Abstract
Objectives: Depression and other mental disorders are more prevalent among individuals living with spinal cord injury (SCI) than in the community at large, and have a strong association with quality of life. Yet little is known about the prevalence and predictors of mental disorders among U.S. military Veterans living with SCI. The primary aim of this study was to present an estimate of mental disorder point prevalence in this population. The secondary aim was to examine the relationship of mental disorders to demographics, injury characteristics, and other clinically relevant features such as impairment from mental health problems and life satisfaction.
Design: Cross-sectional.
Setting: A SCI & Disorders Center at a U.S. Veterans Affairs Medical Center.
Participants/Methods: Administrative and medical records of 280 Veterans who attended annual comprehensive SCI evaluations were evaluated. Demographics, injury characteristics, self-reported mental and emotional functioning (i.e. SF-8 Health Survey), and clinician-determined mental disorder diagnoses were attained.
Results: Overall, 40% of patients received at least one mental disorder diagnosis, most commonly depressive disorders (19%), posttraumatic stress disorder (12%), and substance or alcohol use disorders (11%). Several patient characteristics predicted mental disorders, including age, racial minority identity, non-traumatic SCI etiology, and incomplete (i.e. AIS D) vs. complete injury. Mental disorders were associated with greater impairment from health and mental health-related problems and less satisfaction with life.
Conclusions: Mental disorders are common among outpatients receiving VA specialty care for SCI. These findings highlight the importance of having adequate and effective available mental health services available for Veterans with SCI.
Keywords: Spinal cord injuries, Social adjustment, Depression, Mental disorders, Veterans
Introduction
Spinal cord injury (SCI) is a life-changing event, often resulting in chronic physical impairment and challenges to maintaining good quality of life. Difficulties associated with SCI (SCI) include increased risk of secondary health conditions and mortality,1,2 less vocational and community integration,3,4 disturbance of romantic relationships,5 and lower quality of life.6 Individuals with SCI are at greater risk of mental health difficulties as well.7,8 For example, depression affects about 19–26% of individuals living with SCI,9 about 3 times higher than in the general population (Table 1).10 Prevalence estimates of posttraumatic stress disorder (PTSD) in SCI range widely from 6% to 44%.8,11–15 Rates of anxiety, substance abuse, and other mental health problems in SCI also tend to be higher than found in the general population.8,16–19
Table 1. Summary of select studies of mental health prevalence rates among spinal cord injury patients.
| Study | Population | Methods and Measures for Assessing Mental Health | Mental Health Prevalence Rates |
|---|---|---|---|
| Current Study | Veterans with SCI (N =280) receiving outpatient care at an SCI clinic. | Review of electronic medical records for diagnoses determined by team psychologist interviews. (Point Prevalence) | 40%=Any disorder 19%=Depressive disorders 12%=PTSD 8%=Alcohol use disorder 5.3%=Substance use disorders |
| Banerjea et al., 20097 | Veterans with SCI (N=8338) receiving VA health care from 1999–2002. | Retrospective observational study of VA and Medicare billing data for Veterans with SCI/D. Mental disorders were indicated by ICD-9 codes recorded by providers over a 2-year period. (Period prevalence) | 46% = At least one mental health diagnosis 27%=Depressive disorders 6%=PTSD 10%=Anxiety disorder 9%= Alcohol use disorder 8%=Drug use disorder |
| Craig et al., 20158 | Adults with SCI (N=88) recruited while receiving inpatient rehabilitation and followed for up to 6 months post-discharge. | Mini International Neuropsychiatric Interview (DSM-IV). (Point prevalence) | 25% = Any mental health or substance use disorder at 6-months post-discharge |
| Findley et al., 201112 | Veterans with SCI (N=8334) receiving health care through the Veterans Affairs Health Clinics from 2000–2003. | Retrospective observational study of VA and Medicare billing data for Veterans with SCI/D. Mental disorders were indicated by ICD-9 codes recorded by providers over a 3-year period. (Period prevalence) | 38%=Any mental disorder 26%=Mental disorder but no SUD 12%=SUD but no mental disorder 8%=Both mental disorder and SUD 26%=Depressive disorders 10%=Anxiety disorders 6%=PTSD |
| Krause et al., 201075 | Adults with SCI (N=927) recruited from a longitudinal study comprised of patients from three rehabilitation hospitals. | Self-report measures of PTSD (Purdue Post-traumatic Stress Disorder Scale-Revised) and depression (Patient Health Questionnaire-9). (Point prevalence) | 18%=Major depressive disorder 10%=PTSD |
| Otis et al., 201211 | Outpatients with SCI (N=83) receiving care at a rehabilitation institute. | Structured Clinical Interview for the DSM-IV. | 11%= PTSD at some point after SCI |
| Radnitz et al., 199628 | Veterans with SCI (N = 138) recruited from health clinics of three VA medical centers. | Structured Clinical Interview for the DSM-III-R (point prevalence) | 54%=Lifetime mental disorder 15%=Current mental disorder 10%=Mood disorder (current) 3%=SUD 2%=Anxiety disorder |
| Radnitz et al., 199814 | Veterans with SCI (N=125) at three VA medical centers. | Clinician Administered PTSD Scale (CAPS). (Point prevalence) | 22%=PTSD for patients with paraplegia 2%=PTSD for patients with quadriplegia |
| Smith et al., 200726 | Veterans with SCI/D (N=3678) who received health care at VA medical centers from 1999–2001. Veterans with multiple sclerosis were excluded. | Retrospective observational study of VA Allocation Resource Center (ARC) data on Veterans with SCI/D. Depression was indicated by ICD-9 codes recorded by providers over a 3-year period. (Period prevalence) | 22%=Depressive disorder |
| Ullrich et al., 201420 | Veterans with SCI (N=41,213) who received care at VA medical centers from 1997–2007. | Retrospective observational study of Veterans Health Administration National Registry for Depression (NARDEP) data on Veterans with SCI/D. Depression was indicated by ICD-9 codes recorded by providers over a 10-year period. (Period prevalence) | 28%=Depressive disorders 70%=Individuals with depression and at least one other co-morbid mental health diagnosis |
DSM, Diagnostic and Statistical Manual; ICD, International Classification of Diseases; SCI, spinal cord injury; SUD, substance use disorder.
The elevated rate of mental health problems among individuals with SCI is of concern, given their deleterious impact on daily functioning and well-being. Psychosocial problems such as higher levels of stress, difficulty coping with SCI-related challenges, less enjoyment of daily activities such as hobbies, and lower quality of life are all more common among those with SCI and comorbid mental disorders.20,21 Further, individuals with SCI and psychopathology are more likely to experience health complications,7 more frequent hospitalizations,20 increased suicidality,22,23 and greater mortality.12,24 Additionally, mental health concerns increase the utilization of health care and health care costs and20 reduce rehabilitation engagement.25 Thus, the detection and effective treatment of psychopathology is important for promoting well-being and reducing health comorbidity and costs for patients with SCI.
Few studies have examined rates of mental disorders among military Veterans with SCI, and most of those have reported period prevalence from system-wide Department of Veterans Affairs (VA) administrative billing data (Table 1). In one study combining VA and Medicare claims data, 46% of 8,338 Veterans with SCI had a mental health diagnosis in a 2-year period, most commonly depressive disorders (27%), substance use disorders (SUD; including alcohol, drug, and tobacco use; 26%), anxiety disorders (10%), and PTSD (6%).7 Another study of 8,334 Veterans with SCI using the same data source reported a 38%, 3-year period prevalence of mental disorders, with depressive disorders (26%), substance use disorders (SUD; including alcohol, drug, and tobacco use; 20%), anxiety disorders (10%), and PTSD (6%) most common.12 Two other studies using VA administrative data (N = 41,213 and 3,678) found 2 and 10-year period prevalence of depressive disorders to be 22% and 28%, respectively.20,26 The 38–46% prevalence rate for Veterans with SCI from VA administrative data is considerably higher than the 29%, 5-year estimate of mental disorders for all Veterans.27 In contrast, an earlier, smaller study by Radnitz et al. (N = 125), employing a structured diagnostic interview to determine point prevalence of current mental disorders among Veterans with SCI across three VA medical centers, found a much lower rate (15%).28
No studies have focused on mental disorder prevalence specifically among patients using the VA Spinal Cord Injury and Disorders (SCI/D) system of care, the largest single network of SCI care in the nation. About half of the 27,000 VA patients with SCI/D receive specialty VA SCI/D services.29,30 Although the studies utilizing VA administrative data reviewed above provide important information about mental disorder prevalence among Veterans with SCI/D, it is unclear whether their findings represent those patients seen in SCI/D specialty clinics today. If the findings of Radnitz et al.28 with structured diagnostic interviews offered an accurate, clinic-level view of mental disorder prevalence in SCI/D specialty clinics; administrative data may substantially overestimate the prevalence of mental disorders.
Given mixed findings and the limitations of extant prevalence estimates of mental disorders, further research is needed to inform patient-centered resource allocation to ensure the mental health needs of Veterans with SCI are met. Thus, the primary aim of this study was to estimate the point prevalence of mental disorder among U.S. military Veterans receiving outpatient care in the VA Spinal Cord Injury and Disorders (SCI/D) system of care. The secondary aim was to examine the relationship of mental disorders to demographics, injury characteristics, and other clinically relevant features such as impairment from mental health problems and life satisfaction.
Methods
Participants
The current study used retrospective clinical data from an outpatient sample of military Veterans scheduled at a mid-Atlantic VA SCI/D Center for annual SCI/D evaluations across 24 months during the 2011–2013 calendar years. The SCI/D Centers provide outpatient, home-based and inpatient services including primary care, comprehensive rehabilitation services, specialized mental health services, and acute medical care for over Veterans with SCI/D. The “hub and spoke” VA SCI/D System of Care is comprised of 24 SCI Centers (“hubs”) and over a hundred Patient Aligned Care Teams (PACTs; “spokes”). The study site is the SCI/D Center for Veterans and Service Members residing in Virginia, North Carolina, Maryland, Delaware, West Virginia and the District of Columbia. In fiscal year 2015, this center conducted 662 annual evaluations, 348 (52.6%) during outpatient visits.
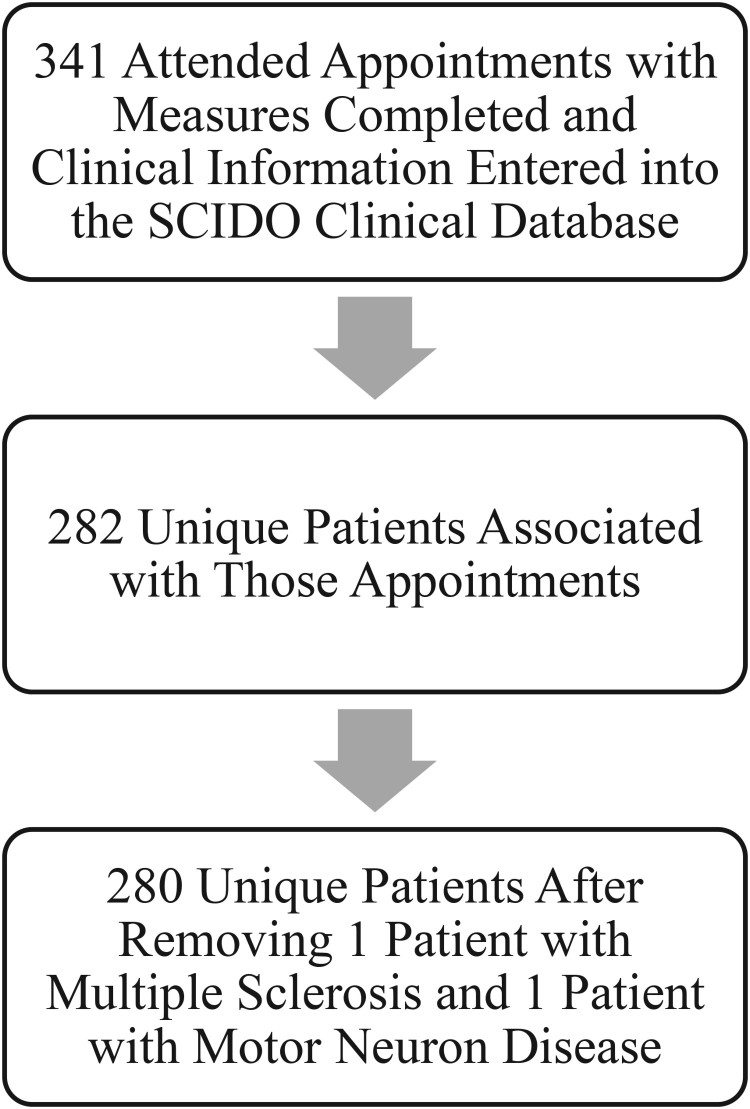
Inclusion criteria were attending the appointment and completion of a health-functioning questionnaire (Fig. 1). For patients with multiple visits during the 24-month period (N = 59), data from their first visit was analyzed. Two patients with primary diagnoses of multiple sclerosis or motor neuron disease were excluded resulting in a final sample of 280.25 Four patients with no appreciable neurologic deficits due to SCI (i.e. American Spinal Injury Association Impairment Scale [AIS] E rating) were excluded for the analyses involving SCI completeness (i.e. AIS rating). Thirteen did not have mental health diagnostic data available, and thus were not included in principal analyses of mental health prevalence rates and predictors.
Figure 1.
Flowchart of appointments and patient data used in this study.
Procedures
SCI/D annual evaluations include a complete review of physical systems, functioning and psychosocial adjustment. Physical health, functional independence, and disability are assessed by appropriate healthcare professionals including a physician, clinical psychologist, occupational therapist, physical therapist, recreational therapist and social worker. Team psychologists meet with each patient to assess mental and behavioral health, examine mental status, administer pertinent mental health screenings, and solicit treatment preferences and needs. Most mental health evaluations were unstructured clinical interviews conducted by four SCI/D clinic team psychologists (including M.E. and B.M.) and informed by other interdisciplinary team members, collateral information from family members or care providers, findings from screening tests, and chart review. The remainder was conducted by another SCI/D psychologist (S.M.) or advanced clinical psychology trainees under close supervision of a licensed team psychologist. Patients completed psychological questionnaires as part of their evaluation. When upper-extremity motor functioning or low vision limited self-completion of forms, patients were assisted by a clinic team member or care provider (about 26%). A waiver of informed consent and the study protocol were approved by the local Institutional Review Board.
Measures
Patient characteristics
Demographic variables were extracted from VA administrative data and the VA Spinal Cord Injury and Disorders Outcomes (SCIDO) clinical database. Injury completeness was rated by SCI team physicians using the AIS grading system. Injury etiology, including both traumatic (e.g. assault, falls, motor vehicle collisions) and non-traumatic (e.g. spinal stenosis, tumor, and ischemia) injuries were extracted from the SCIDO database.
Mental disorder diagnoses
An unstructured diagnostic interview was conducted as part of the mental and behavioral health assessment by team psychologists. Consistent with recommended assessment practices, team psychologists generally began with open-ended questions leading to more structured inquiry about specific problems and events and informed by supplemental information from informants (e.g. care providers) and medical records.31 For the purpose of this study, a mental disorder was coded as present if the SCI psychologist recorded a diagnosis per the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR)32 in a chart note associated with the clinic visit. Recorded diagnoses with the DSM-IV-TR specifier of “provisional,” indicating that the clinician has a strong presupposition that full diagnostic criteria are met but more information would be needed (e.g. unclear date of onset so duration criterion is not met) were considered present due to the detection of a clinically meaningful condition and pertinent to the patient's treatment plan, despite diagnostic uncertainty. Diagnoses with the informal specifier “rule out” were considered provisional when no primary and exclusive mental disorder diagnosis was recorded (n = 5). Personality disorders were considered present if any associated “features” or “traits” were listed as clinically relevant in the clinical note. Conditions “in full remission” were considered present if the patient continued to receive treatment for the condition (e.g. antidepressants for depression or participation in a relapse prevention program for alcohol dependence). Antidepressant use in the absence of a history of depression, anxiety, or PTSD was not coded as indicating a mental disorder, given its frequent use to treat neuropathic pain. Cognitive disorders were not considered for the current study. In a small number of cases (1.5%) the note mentioned continued symptoms and/or treatment but not a specific diagnosis. In those cases, the established, current mental health diagnosis listed in the VA medical records problem list was used. Information was extracted by medical record review by a clinical psychologist (S.M.) or an advanced clinical psychology graduate student (L.L.).
Satisfaction with life scale (SWLS)
The SWLS is a five-item, self-report measure of life satisfaction. 33 Using a 7-point scale, respondents are asked to rate the degree to which the respondent agrees or disagrees with five statements such as “my life is close to my ideal.” Higher scores indicate higher life satisfaction.
SF-8™ Health Survey
The SF-8™ Health Survey (SF-8, VA version),34 a short form of the SF-36 Health Survey,35 is an eight-item self-report measure of patient health within the past four weeks. The VA version of the SF-8 has an extra item that asks non-ambulatory patients to mark how much physical health problems limit physical activities, not considering walking and climbing stairs. That item was not used in analyses. The Physical (PCS) and Mental Component Summary (MCS) variables were calculated from weighted sums of all items using appropriate algorithms. Higher scores on PCS and MCS indicate better physical and mental health, respectively. Scores below 40 indicate impaired functioning whereas scores from 40 to 44 indicate a need for further investigation.
Analyses
Percentages or measures of central tendency and variability were used to describe variables as applicable. Missing data was managed by listwise deletion of cases. Independent-samples t-tests were employed to compare group means where appropriate. Standard binary logistic regression analyses were conducted with mental disorder category as an outcome and patient characteristics as predictors. In addition to the planned contrasts, for statistically significant predictors with three or more levels, comparisons of proportions among levels were compared using a modified Bonferroni procedure.36 Primary analyses were conducted using IBM® SPSS® Statistics (Version 21, IBM Corp., Armonk, NY, USA).
Results
Patient characteristics
The 280 patients included in this study (Table 2) were representative of the 455 patients with appointments in this time period on demographic and injury characteristics such as age (M = 58.0), sex (96.0% male), race (51.2% White/Caucasian), rates of traumatic etiology (70.1%), rates of AIS D (incomplete) injury (48.1%), and rates of paraplegia (45.0%). Compared with a national cohort of patients with SCI treated by the VA37 this sample had a greater percentage of ethnic and racial minority patients (52% vs. 39%) and lower percentage with paraplegia vs. tetraplegia (42% vs. 54%). However, this sample was similar regarding percentage of females (4% vs. 3%) and percentage of patients over 65 years of age (29% vs. 30%).
Table 2. Demographic, injury, and other patient characteristics (N = 280).
| Characteristic | Mean (SD) or % |
|---|---|
| Age | |
| Mean (SD) years | 58.13 (13.02) |
| Median | 59 |
| Range | 24 to 90 |
| Years since SCI | |
| Mean (SD) years | 16.94 (13.30) |
| Median | 13 |
| Range | 1 to 67 |
| Age at SCI | |
| Mean (SD) years | 41.19 (15.13) |
| Median | 40 |
| Range | 19 to 84 |
| Sex (% male) | 96.1% |
| Race/ethnicity | |
| White/Caucasian | 48.2% |
| Black/African American | 46.4% |
| Other | 2.2% |
| Unknown/Declined to Answer | 3.3% |
| Married† | 49.3% |
| College graduate† | 29.2% |
| Employed† | 14.4% |
| VA Service Connected Disability | |
| 70–100% | 55.0% |
| 30–60% | 5.0% |
| 0–20% | 2.9% |
| None | 37.1% |
| SCI Etiology (% traumatic) | 70.0% |
| Level of Injury | |
| High tetraplegia (C1–C4) | 26.1% |
| Low tetraplegia (C5–C8) | 32.5% |
| Paraplegia | 41.4% |
| ASIA Impairment Scale (AIS) | |
| A | 30.1% |
| B | 9.1% |
| C | 9.4% |
| D | 51.4% |
| SF-8™ Health Survey: Physical Component Summary | 39.25 (11.20) |
| Average or greater | 31.9% |
| Requires further investigation | 13.8% |
| Impaired functioning | 54.2% |
| SF-8™ Health Survey: Mental Component Summary | 49.58 (11.43) |
| Average or greater | 70.8% |
| Requires further investigation | 11.2% |
| Impaired functioning | 18.1% |
†n=138.
Prevalence of mental disorders
In all, 39.9% of patients with SCI had at least one mental disorder (Table 3). The most common diagnoses were depressive disorders (19.3%), PTSD (11.7%), substance use disorders (5.3%), alcohol use disorders (8.0%), adjustment disorders (6.8%), pain disorders (4.5%), anxiety disorders (sans PTSD; 3.0%), and personality disorders (3.0%). A small percentage presented with other conditions including schizophrenia/psychotic disorders, bipolar disorders, sleep disorders, and sexual disorders (5.7%). Comorbidity was common: 66.7% of patients with depressive disorders, 71.0% with PTSD, and 63.3% with a substance use or alcohol use disorder had at least one diagnosis from another diagnostic category.
Table 3. Percentages of mental disorders per demographic or clinical characteristic.
| Characteristic | n† | Depressive Disorders | PTSD | Substance/Alcohol Use Disorders | Any‡ |
|---|---|---|---|---|---|
| Age | |||||
| 18 to 45 years of age | 43 | 23.3 | 7.0 | 11.6 | 34.9 |
| 46 to 60 years of age | 105 | 21.0 | 6.7 | 14.4 | 41.3 |
| 61 to 70 years of age | 73 | 24.7 | 27.4 | 12.3 | 50.7 |
| 71 years of age or older | 43 | 2.3 | 2.3 | 2.3 | 23.3 |
| Years since SCI | |||||
| 1 to 5 | 61 | 24.6 | 13.1 | 16.4 | 52.5 |
| 6 to 10 | 53 | 17.0 | 11.3 | 7.5 | 37.7 |
| 11 to 20 | 62 | 19.4 | 14.5 | 11.5 | 36.1 |
| 21 or greater | 88 | 17.0 | 9.1 | 10.2 | 35.2 |
| Age at SCI | |||||
| 18 to 30 years of age | 86 | 19.8 | 8.1 | 12.8 | 37.2 |
| 31 to 45 years of age | 76 | 18.4 | 11.8 | 6.7 | 38.7 |
| 46 to 60 years of age | 69 | 26.1 | 15.9 | 17.4 | 47.8 |
| 61 years of age or older | 33 | 6.1 | 12.1 | 6.1 | 33.3 |
| Race/ethnicity | |||||
| White/Caucasian | 128 | 14.1 | 6.3 | 3.1 | 28.3 |
| Black/African American and other Minority groups | 129 | 24.8 | 17.1 | 20.2 | 51.9 |
| Marital Status | |||||
| Never married | 19 | 5.6 | 5.6 | 11.1 | 22.2 |
| Married | 68 | 22.2 | 9.5 | 7.9 | 41.3 |
| Divorced/separated | 48 | 11.4 | 11.4 | 18.2 | 36.4 |
| Education | |||||
| High school or GED | 45 | 22.2 | 8.9 | 17.8 | 46.7 |
| Some college or 2-year degree | 39 | 20.5 | 12.8 | 7.7 | 38.5 |
| College graduate or higher | 36 | 5.6 | 5.6 | 8.3 | 22.2 |
| Employment | |||||
| Unemployed | 46 | 19.6 | 8.7 | 13.0 | 34.8 |
| Employed | 18 | 11.1 | 0 | 0 | 16.7 |
| Retired | 59 | 15.3 | 11.9 | 13.6 | 42.4 |
| VA Service Connected Disability | |||||
| None | 96 | 11.5 | 1.0 | 14.6 | 31.3 |
| 0–20% | 8 | 25.0 | 0 | 12.5 | 37.5 |
| 30–60% | 14 | 21.4 | 7.1 | 21.4 | 50.0 |
| 70–100% | 146 | 24.0 | 19.9 | 8.3 | 44.8 |
| SCI Etiology | |||||
| Non-Traumatic | 78 | 30.8 | 19.2 | 11.5 | 57.7 |
| Traumatic | 186 | 14.5 | 8.6 | 11.4 | 32.4 |
| Level of Injury | |||||
| Paraplegia | 108 | 16.7 | 9.3 | 6.5 | 35.2 |
| Low tetraplegia (C5–C8) | 88 | 17.0 | 14.8 | 13.6 | 38.6 |
| High tetraplegia (C1–C4) | 68 | 26.5 | 11.8 | 16.4 | 49.3 |
| ASIA Impairment Scale | |||||
| D | 133 | 25.6 | 18.8 | 15.2 | 50.8 |
| C | 24 | 12.5 | 8.3 | 4.2 | 33.3 |
| B | 24 | 12.5 | 4.2 | 4.2 | 29.2 |
| A | 79 | 11.4 | 2.5 | 7.6 | 24.1 |
| All | 266 | 19.3 | 11.7 | 11.4 | 39.9 |
†Group sizes may be smaller in this table vs. Table 1 due to missing diagnostic data.
‡Includes depressive disorders, PTSD, other anxiety disorders, substance use disorders, alcohol use disorders, schizophrenia/psychotic disorders, pain disorders, adjustment disorders, and personality disorders.
Mental health and health functioning
Those with a mental health diagnosis (M = 40.8 [12.2]) reported significantly worse mental health functioning than those without (M = 55.3 [6.6]), t(242) = 11.99, P < 0.001, and were substantially more likely to report impaired functioning (44%) in comparison to those with no diagnosis (1%) (Tables 2 and 4). Among the most prevalent disorders, percentage of impaired functioning was highest for PTSD (67%), followed by depressive disorders (55%), then substance/alcohol use disorders (41%).
Table 4. Severity of mental health impairment by mental disorder diagnosis.
| SF-8 Mental Component Summary | |||
|---|---|---|---|
| Diagnosis | Average or Greater | Requires Further Investigation | Impaired Functioning |
| Depressive Disorders | 16 (34.0%) | 5 (10.6%) | 26 (55.3%) |
| PTSD | 7 (23.3%) | 3 (10.0%) | 20 (66.7%) |
| Substance/Alcohol Use Disorders | 10 (37.0%) | 6 (22.2%) | 11 (40.7%) |
| Any Diagnosis† | 39 (40.6%) | 15 (15.6%) | 42 (43.8%) |
| No Diagnosis | 134 (90.5%) | 12 (8.1%) | 2 (1.4%) |
†Includes depressive disorders, PTSD, other anxiety disorders, substance use disorders, alcohol use disorders, schizophrenia/psychotic disorders, pain disorders, adjustment disorders, and personality disorders.
Those with a mental health diagnosis (M = 34.2 [9.7]) reported significantly worse health functioning than those without (M = 42.7 [11.0]), t(242) = 6.15, P < 0.001, and were substantially more likely to report impaired functioning (75%) in comparison to those with no diagnosis (41%) (Table 5). Among the most prevalent disorders, percentage of impaired functioning was highest for PTSD (97%), followed by depressive disorders (79%), then substance/alcohol use disorders (63%).
Table 5. Severity of physical health impairment by mental disorder diagnosis.
| SF-8 Physical Component Summary | |||
|---|---|---|---|
| Diagnosis | Average or Greater | Requires Further Investigation | Impaired Functioning |
| Depressive Disorders | 5 (10.6%) | 5 (10.6%) | 37 (78.7%) |
| PTSD | 1 (3.3%) | 0 (0%) | 29 (96.7%) |
| Substance/Alcohol Use Disorders | 6 (22.2%) | 4 (14.8%) | 17 (63.0%) |
| Any Diagnosis† | 13 (13.5%) | 12 (12.5%) | 71 (74.0%) |
| No Diagnosis | 66 (44.6%) | 22 (14.9%) | 60 (40.5%) |
†Includes depressive disorders, PTSD, other anxiety disorders, substance use disorders, alcohol use disorders, schizophrenia/psychotic disorders, pain disorders, adjustment disorders, and personality disorders.
Satisfaction with life
The SWLS was available for a subset of 69 patients. Group mean satisfaction with life (M = 21.6 [6.9]) was in range of those with SCI in the community (M = 19.4 [7.9]),38 corresponding to “average” life satisfaction.39 Those with mental disorders (M = 18.5 [6.3]) had significantly lower life satisfaction than those without (M = 24.5 [5.8]), t(64) = 4.04, P < 0.001. Life satisfaction for those with mental disorders was in the “slightly below average” range.
Predictors of mental disorders
Unadjusted odds ratios with 95% confidence intervals of mental disorders per demographic or clinical characteristic are presented in Table 6. Of note, the term “predictor” is used in this text for variables thought to predict group membership but does not suggest causality. Marital status, education, and employment were not displayed in Table 6, as none of these variables were significant predictors of mental disorders.
Table 6. Unadjusted odds ratios with 95% confidence intervals of mental disorders per demographic or clinical characteristic.
| Unadjusted Odds Ratio (95% CI) | ||||
|---|---|---|---|---|
| Characteristic | Depressive Disorders | PTSD | Substance/Alcohol Use Disorders | Any‡ |
| Age | ||||
| 18 to 45 years of age | .93 (.38, 2.24) | .20 (.06,.72)* | .94 (.29, 3.00) | .52 (.24, 1.13) |
| 46 to 60 years of age | .81 (.40, 1.65) | .19 (.08,.48)*** | 1.20 (.49, 2.91) | .69 (.38, 1.25) |
| 61 to 70 years of age | 1.0 | 1.0 | 1.0 | 1.0 |
| 71 years of age or older | .07 (.01,.57)* | .06 (.01,.49)** | .17 (.02, 1.39) | .30 (.13,.69)* |
| Wald | 6.35† | 19.67*** | 3.52 | 8.72* |
| χ2 | 13.66** | 22.59*** | 5.95 | 9.35* |
| Years since SCI | ||||
| 1 to 5 | 1.0 | 1.0 | 1.0 | 1.0 |
| 6 to 10 | .63 (.25, 1.58) | .85 (.27, 2.62) | .42 (.12, 1.42) | .55 (.26, 1.16) |
| 11 to 20 | .74 (.31, 1.74) | 1.13 (.40, 3.14) | .66 (.23, 1.87) | .51 (.25, 1.06) |
| 21 or greater | .63 (.28, 1.41) | .66 (.23, 1.87) | .58 (.22, 1.53) | .49 (.25,.96) |
| Wald | 1.55 | 1.16 | 2.34 | 5.20 |
| χ2 | 1.52 | 1.19 | 2.34 | 5.21 |
| Age at SCI | ||||
| 18 to 30 years of age | 1.0 | 1.0 | 1.0 | 1.0 |
| 31 to 45 years of age | .92 (.42, 2.01) | 1.52 (.54, 4.29) | .49 (.16,1.47) | 1.06 (.56, 2.01) |
| 46 to 60 years of age | 1.43 (.67, 3.05) | 2.14 (.78, 5.86) | 1.44 (.59,3.49) | 1.55 (.81, 2.94) |
| 61 years of age or older | .26 (.06, 1.20) † | 1.56 (.42, 5.71) | .44 (.09,2.10) | .84 (.36, 1.97) |
| Wald | 5.14 | 2.20 | 4.91 | 2.69 |
| χ2 | 6.72† | 2.27 | 5.34 | 2.69 |
| Race/ethnicity | ||||
| White/Caucasian | 1.0 | 1.0 | 1.0 | 1.0 |
| Black/African American (95%) and other Minority groups | 2.02 (1.06, 3.82)* | 3.08 (1.32, 7.22)** | 7.76 (2.62, 22.97)*** | 2.73 (1.63, 4.59)*** |
| χ2 | 4.79* | 7.54** | 19.79*** | 14.99*** |
| SCI Etiology | ||||
| Non-Traumatic | 1.0 | 1.0 | 1.0 | 1.0 |
| Traumatic | .38 (.20,.72)** | .40 (.19,.85)* | .98 (.43, 2.25) | .35 (.20,.61)*** |
| χ2 | 8.76** | 5.56* | .002 | 14.43*** |
| Level of Injury | ||||
| Paraplegia | 1.0 | 1.0 | 1.0 | 1.0 |
| Low tetraplegia (C5–C8) | 1.03 (.49, 2.18) | 1.70 (.71, 4.09) | 2.28 (.86, 6.06) | 1.16 (.65, 2.08) |
| High tetraplegia (C1–C4) | 1.80 (.86, 3.77) | 1.31 (.49, 3.49) | 2.83 (1.04, 7.72) | 1.79 (.96, 3.33) |
| Wald | 2.96 | 1.40 | 4.44 | 3.47 |
| χ2 | 2.86 | 1.42 | 4.92 | 3.47 |
| ASIA Impairment Scale | ||||
| D | 1.0 | 1.0 | 1.0 | 1.0 |
| C | .42 (.12, 1.48) | .39 (.09, 1.78) | .24 (.03, 1.91) | .49 (.19, 1.21) |
| B | .42 (.12, 1.48) | .19 (.02, 1.46) | .24 (.03, 1.91) | .40 (.16, 1.03)† |
| A | .37 (.17,.83)* | .11 (.03,.49)** | .46 (.18, 1.20) | .31 (.17,.57)*** |
| Wald | 7.72† | 11.31* | 5.15 | 15.85*** |
| χ2 | 8.26* | 16.68*** | 6.06 | 16.75*** |
†P < 0.10; *P < 0.05; **P < 0.01; ***P ≤ 0.001.
‡Includes depressive disorders, PTSD, other anxiety disorders, substance use disorders, alcohol use disorders, schizophrenia/psychotic disorders, pain disorders, adjustment disorders, and personality disorders.
Depressive disorders
Increasing the risk of depressive disorders were age, minority status, non-traumatic SCI etiology, and SCI completeness (AIS D > AIS A, P = 0.013, critical value =.01). Regarding age, those 71 years or older had significantly lower risk of depression when compared to each of the other age groups (P < 0.01 for each).
PTSD
Increasing the risk of PTSD were age, minority status, non-traumatic SCI etiology, and SCI completeness (AIS D > AIS A, P < 0.001, critical value = 0.01). Regarding age, those 61 to 70 years of age had significantly higher risk of PTSD when compared to each of the other age groups (P < 0.01 for each).
Substance/alcohol use disorders
Minority status increased the risk of substance/alcohol use disorders.
Any mental disorder
Increasing the risk of any of the mental disorders examined in this study were age, years since injury (planned contrasts were all ns), minority status, non-traumatic SCI etiology, and SCI completeness (AIS D > AIS A, P < 0.001, critical value = 0.01). Regarding age, those 71 years of age or older had significantly lower risk of any mental disorder when compared to those 61 to 70 years of age (P = 0.004).
Discussion
Prevalence of mental disorders
Overall, 40% of patients received at least one mental disorder diagnosis from SCI team psychologists during outpatient evaluations. Consistent with prior studies, mental disorders were associated with lower life satisfaction and greater impairment in daily activities from health and mental health problems.12,40 These findings highlight the commonness of mental disorders and the associated reduction in quality of life for many patients with SCI.
The 40% point prevalence of mental disorders in this population was considerably higher than the 19–26% estimated 12-month prevalence in the general population10,41 and 29% 5-year prevalence among Veterans receiving VA health care.27 It was also higher than point prevalence estimates of mental disorders among patients with SCI from structured diagnostic interviews in a community sample in Australia (25%)8 and U.S. military Veterans with SCI (15%). However, despite methodological differences, it was similar to 2-year and 3-year period prevalence estimates informed by administrative data for patients with SCI receiving VA care.7,12 Regarding specific disorders, the point prevalence of depressive disorders (19%), PTSD (12%), and substance or alcohol use disorders (11%) were higher than in the general population10 and overall VA health care27 but within expectations for patients with SCI.7,9,12,20 Comorbidity was common, affecting between 63–71% across specific diagnoses.
It is unclear why the point prevalence of mental disorders reported in this study was more similar to period prevalence estimates from VA administrative data than with other point prevalence estimates from structured diagnostic interviews. One possibility is that structured diagnostic interviews may underestimate the prevalence of mental disorders among patients with SCI. Although structured interviews have the advantage of improved reliability across multiple raters, they also tend to sacrifice breadth of assessment for depth in specific areas,42 limit clinical judgment that is afforded in the classification system used to diagnose mental disorders,43 and may not capture the waxing and waning symptoms that are common in chronic mental disorders.44,45 In contrast, the unstandardized mental health evaluations conducted by team psychologists in this clinic are less structured but more likely to entrust clinical judgment while integrating multiple sources of clinical information. Thus, the flexibility afforded by unstructured clinical interviews may have been beneficial in capturing clinically significant information that reflects actual treatment needs and practices. Accordingly, unstandardized clinical interviews may be more likely to reflect the actual practices of VA providers reflected in VA administrative billing data.
On the other hand, the finding that 41% of those with a mental health diagnosis did not self-report significant mental health-related impairment may suggest that clinical interviews overestimated mental disorder prevalence. As significant distress or impairment is a defining feature of a mental disorder,32 it may seem unusual that many patients with SCI with diagnoses did not self-report impairment. However, there are several possible reasons why that was not the case. First, the family of Short Form health surveys is only moderately sensitive to psychopathology.46–48 Second, since mental health diagnoses included conditions in remission, not all patients should be expected to report current mental health impairment. To better understand how methods and settings impact mental disorder prevalence estimates and associated clinical needs, more cross-method, and preferably prospective, studies are needed.
Predictors of mental disorders
Patient characteristics that increased the risk of a depressive disorder and PTSD include age, racial minority group membership, non-traumatic SCI etiology, and incomplete (i.e. AIS D) vs. complete injury. In contrast, only racial minority group membership increased the risk of substance and alcohol use disorders.
Those over 70 years old had the lowest risk of psychopathology, consistent with findings of community epidemiological studies.41,49 Rates of depression were consistent until the eighth decade, after which rates plummeted. The relative consistency of lower rates of depression among older adults may reflect higher mortality rates for depressed individuals, the relatively good health of patients with SCI who have survived to the eighth decade of life or increased acceptance of health declines with age. The elevated rate of PTSD among 61- to 70-year-olds was in contrast to the null findings reported by most other studies,11,14,50 (cf.15) likely reflecting the cohort that served during the Vietnam War era (61 to 70 years old). This suggests that trauma screenings are particularly important for Vietnam-era Veterans with SCI and highlights the impact of life events beyond SCI on mental health.
Minority status was a significant predictor of depressive disorders, PTSD, substance/alcohol use disorders, and mental disorders overall. In other studies conducted in the U.S., racial and ethnic disparities in SCI outcomes such as subjective well-being, community participation, career opportunities, and mental health have been observed.7,14,51,52 It is possible that minority status acts as a proxy for socioeconomic factors52, 53that are associated with mental health54 although other interactive cultural and institutional factors should also be considered.
Regarding SCI injury characteristics, the higher rates of depressive disorders and PTSD among those with non-traumatic injuries are in stark contrast to earlier studies that found no differences by etiology.6,55–57 It is possible that variation in defining “non-traumatic” SCI across studies, such as the exclusion of patients with more common progressive conditions including multiple sclerosis and motor neuron diseases in this study, contributed to disparate findings.58,59
Incomplete SCI with persevered motor and sensory functioning below the level of injury (i.e. AIS D) significantly increased the risk of depression and PTSD (but not substance/alcohol use disorders). In contrast, level of injury was not predictive of mental disorders. Most studies have found no more than a weak relationship between SCI injury characteristics and subsequent mental health in chronic SCI,8,11,40,60 although exceptions can be found.14,19,61 Patients with incomplete injury are often ambulatory, which can lead others to misperceive their SCIs as less severe than those with visible signs of SCI such as wheelchairs or other aids for mobility.62 Yet patients with incomplete injury often endure functional limitations, fatigue, and pain that significantly impacts confidence in abilities, daily functioning and community engagement.62,63 Given the associations between pain, fatigue, and depression, it is possible that AIS D incomplete SCI serves as a proxy for the impact of these variables on mental health outcomes.64
Limitations
Findings may not generalize to all patients with SCI treated by the VA nor patients treated outside the VA. Although patients were not taken from consecutive appointments nor randomly selected, the sample was largely representative of the facility's SCI/D outpatient evaluation clinic and a close match with national VA SCI/D patients. Further, the SCI/D Center conducts annual evaluations for patients living across five states and the District of Columbia, enhancing heterogeneity. However, the findings may not be applicable to women and minority subgroups that were too small to be explored separately.
Use of unstandardized clinical interviews by SCI team psychologists to indicate mental disorders rather than a standardized interview could limit generalizability. However, clinical interviews informed by supplemental clinical information appear representative of typical VA clinical practices and allows more breadth in assessment that most structured diagnostic interviews. Further, the inclusion of data from multiple providers of diverse backgrounds may have limited bias from idiosyncratic clinical judgment. Additional studies are needed to examine regional and institutional differences as well as the impact of clinician-driven diagnoses on health and mental health outcomes.
Finally, the secondary aim of examining predictors of mental disorders was limited to variables that were available to the research team, and may impart relatively small risk compared with other factors such as premorbid mental disorders,8,65 social support,21 psychological variables such as coping,66 and socioeconomic factors.60 Future studies that examine the relative impact of protective and risk factors for psychopathology in SCI, and directions for intervention, are needed.
Conclusions
Spinal cord injury is a life-changing event that is accompanied by an increased prevalence of depression, PTSD, substance and alcohol abuse, and other mental disorders. The 40% of Veterans with SCI and mental disorders are likely to have the additional burdens of secondary health comorbidities, lower quality of life, and higher caregiver stress. Early detection through efficient screening programs, awareness of risk factors, and readily available mental health resources for assessment and treatment are essential for the management of SCI and its psychosocial outcomes.67,68 Further, the finding of high mental health comorbidity in SCI highlights the importance of assessment and treatment planning that accounts for complex clinical needs.20 Although a challenging endeavor, mental health in SCI would benefit from standardizing definitions and methodology69 and consider matching measurement to clinical practice. At the same time, clinical practice should employ standardized measures that offer opportunity for meaningful comparison between institutions and across patient subgroups.
We hope that this study will inform resource allocation, highlight the need for seamless care coordination across “hub and spoke” sites in the VA SCI/D system of care, and invigorate research on mental health assessment and treatment in this population. More work is needed to understand the foundations of SCI adjustment such as interrelationships between risk and protective factors, determine the best ways to honor patient preferences,70 build patient skills and resources to foster well-being,71,72 and promote the efficient application of treatments that work.73,74
Funding Statement
This project was supported by a VA Career Development Award-2 (K2RX000703; PI: McDonald).
Acknowledgements
We are grateful to Stephen Trapp, Cheonte’ Harding, Anne Simmons, and Judy Pulliam for their assistance with for this study. The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs or other author affiliations.
Disclaimer statements
Contributor statement Drs. McDonald, Ellwood, and Mutchler contributed to the design of the work. Drs. McDonald and Mickens and Ms. Goldberg-Looney contributed to data acquisition and data entry. All authors contributed to interpretation of the data, drafting and revising the manuscript, gave final approval of the version to be submitted, and agreed to be accountable for the accuracy and integrity of the data.
Conflicts of interest Dr. McDonald's work has been funded by the Department of Veteran's Affairs. Drs. Mickens, Mutchler, Ellwood, and Castillo and Ms. Goldberg-Looney declare no conflicts of interest.
Ethics approval A waiver of informed consent and the study protocol were approved by the local Institutional Review Board. All applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
ORCID
Scott D. McDonald http://orcid.org/0000-0003-1490-0096
Melody N. Mickens http://orcid.org/0000-0002-7126-8456
Brian J. Mutchler http://orcid.org/0000-0002-0347-0054
References
- 1. Whiteneck GG, Charlifue SW, Frankel HL, Fraser MH, Gardner BP, Gerhart KA et al. , Mortality, morbidity, and psychosocial outcomes of persons spinal cord injured more than 20 years ago. Paraplegia 1992;30(9):617–30. [DOI] [PubMed] [Google Scholar]
- 2. Krause JS, Devivo MJ, Jackson AB.. Health status, community integration, and economic risk factors for mortality after spinal cord injury. Arch Phys Med Rehabil 2004;85(11):1764–73. doi: 10.1016/j.apmr.2004.06.062 [DOI] [PubMed] [Google Scholar]
- 3. Ottomanelli L, Lind L.. Review of critical factors related to employment after spinal cord injury: implications for research and vocational services. J Spinal Cord Med 2009;32(5):503–31. doi: 10.1080/10790268.2009.11754553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hammell KR. Psychosocial outcome following spinal cord injury. Paraplegia 1994;32(11):771–9. [DOI] [PubMed] [Google Scholar]
- 5. Kreuter M. Spinal cord injury and partner relationships. Spinal Cord 2000;38(1):2–6. doi: 10.1038/sj.sc.3100933 [DOI] [PubMed] [Google Scholar]
- 6. Migliorini CE, New PW, Tonge BJ.. Quality of life in adults with spinal cord injury living in the community. Spinal Cord 2011;49(3):365–70. doi: 10.1038/sc.2010.102 [DOI] [PubMed] [Google Scholar]
- 7. Banerjea R, Findley PA, Smith B, Findley T, Sambamoorthi U.. Co-occurring medical and mental illness and substance use disorders among veteran clinic users with spinal cord injury patients with complexities. Spinal Cord 2009;47(11):789–95. doi: 10.1038/sc.2009.42 [DOI] [PubMed] [Google Scholar]
- 8. Craig A, Nicholson Perry K, Guest R, Tran Y, Dezarnaulds A, Hales A et al. , Prospective study of the occurrence of psychological disorders and comorbidities after spinal cord injury. Arch Phys Med Rehabil 2015;96(8):1426–34. doi: 10.1016/j.apmr.2015.02.027 [DOI] [PubMed] [Google Scholar]
- 9. Williams R, Murray A.. Prevalence of depression after spinal cord injury: A meta-analysis. Arch Phys Med Rehabil 2015;96(1):133–40. doi: 10.1016/j.apmr.2014.08.016 [DOI] [PubMed] [Google Scholar]
- 10. Kessler RC, Chiu WT, Demler O, Walters EE.. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005;62(6):617–27. doi: 10.1001/archpsyc.62.6.617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Otis C, Marchand A, Courtois F.. Risk factors for posttraumatic stress disorder in persons with spinal cord injury. Top Spinal Cord Inj Rehabil 2012;18(3):253–63. doi: 10.1310/sci1803-253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Findley PA, Banerjea R, Sambamoorthi U.. Excess mortality associated with mental illness and substance use disorders among veteran clinic users with spinal cord injury. Disabil Rehabil 2011;33(17–18):1608–15. doi: 10.3109/09638288.2010.540294 [DOI] [PubMed] [Google Scholar]
- 13. Kennedy P, Evans MJ.. Evaluation of post traumatic distress in the first 6 months following SCI. Spinal Cord 2001;39(7):381–6. doi: 10.1038/sj.sc.3101172 [DOI] [PubMed] [Google Scholar]
- 14. Radnitz CL, Hsu L, Tirch DD, Willard J, Lillian LB, Walczak S et al. , A comparison of posttraumatic stress disorder in veterans with and without spinal cord injury. J Abnorm Psychol 1998;107(4):676–80. doi: 10.1037/0021-843X.107.4.676 [DOI] [PubMed] [Google Scholar]
- 15. Nielsen MS. Post-traumatic stress disorder and emotional distress in persons with spinal cord lesion. Spinal Cord 2003;41(5):296–302. doi: 10.1038/sj.sc.3101427 [DOI] [PubMed] [Google Scholar]
- 16. Craig A, Tran Y, Middleton J.. Psychological morbidity and spinal cord injury: A systematic review. Spinal Cord 2009;47(2):108–14. doi: 10.1038/sc.2008.115 [DOI] [PubMed] [Google Scholar]
- 17. Craig AR, Hancock KM, Dickson HG.. A longitudinal investigation into anxiety and depression in the first 2 years following a spinal cord injury. Paraplegia 1994;32(10):675–9. [DOI] [PubMed] [Google Scholar]
- 18. Radnitz CL, Tirch D.. Substance misuse in individuals with spinal cord injury. Int J Addict 1995;30(9):1117–40. doi: 10.3109/10826089509055831 [DOI] [PubMed] [Google Scholar]
- 19. Tate DG, Forchheimer MB, Krause JS, Meade MA, Bombardier CH.. Patterns of alcohol and substance use and abuse in persons with spinal cord injury: risk factors and correlates. Arch Phys Med Rehabil 2004;85(11):1837–47. doi: 10.1016/j.apmr.2004.02.022 [DOI] [PubMed] [Google Scholar]
- 20. Ullrich PM, Smith BM, Blow FC, Valenstein M, Weaver FM.. Depression, healthcare utilization, and comorbid psychiatric disorders after spinal cord injury. J Spinal Cord Med 2014;37(1):40–5. doi: 10.1179/2045772313Y.0000000137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kraft R, Dorstyn D.. Psychosocial correlates of depression following spinal injury: A systematic review. J Spinal Cord Med 2015;38(5):571–83. doi: 10.1179/2045772314Y.0000000295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. DeVivo MJ, Black KJ, Richards JS, Stover SL.. Suicide following spinal cord injury. Paraplegia 1991;29(9):620–7. [DOI] [PubMed] [Google Scholar]
- 23. Judd FK, Brown DJ.. Suicide following acute traumatic spinal cord injury. Paraplegia 1992;30(3):173–7. [DOI] [PubMed] [Google Scholar]
- 24. Krause JS, Carter RE, Pickelsimer EE, Wilson D.. A prospective study of health and risk of mortality after spinal cord injury. Arch Phys Med Rehabil 2008;89(8):1482–91. doi: 10.1016/j.apmr.2007.11.062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kortte KB, Falk LD, Castillo RC, Johnson-Greene D, Wegener ST.. The Hopkins Rehabilitation Engagement Rating Scale: development and psychometric properties. Arch Phys Med Rehabil 2007;88(7):877–84. doi: 10.1016/j.apmr.2007.03.030 [DOI] [PubMed] [Google Scholar]
- 26. Smith BM, Weaver FM, Ullrich PM.. Prevalence of depression diagnoses and use of antidepressant medications by veterans with spinal cord injury. Am J Phys Med Rehabil 2007;86(8):662–71. doi: 10.1097/PHM.0b013e318114cb6d [DOI] [PubMed] [Google Scholar]
- 27. United States Government Accountability Office VA mental health: Number of veterans receiving care, barriers faced, and efforts to increase access (GAO-12–12): U.S. Government Accountability Office; 2011.
- 28. Radnitz CL, Broderick CP, Perez-Strumolo L, Tirch DD, Festa J, Schlein IS et al. , The prevalence of psychiatric disorders in veterans with spinal cord injury: a controlled comparison. J Nerv Ment Dis 1996;184(7):431–3. doi: 10.1097/00005053-199607000-00006 [DOI] [PubMed] [Google Scholar]
- 29. VA Office of Research and Development, HSR&D Quality Enhancement Research Initiative Spinal Cord Injury: Fact Sheet 2014. Available from: http://www.queri.research.va.gov/about/factsheets/sci_factsheet.pdf.
- 30. Office of Public Affairs, Media Relations VA and Spinal Cord Injury 2009. Available from: http://www.va.gov/opa/publications/factsheets/fs_spinal_cord_injury.pdf.
- 31. American Psychiatric Association Practice Guidelines for the Psychiatric Evaluation of Adults, Third Edition 2015. Available from: http://psychiatryonline.org/doi/abs/10.1176/appi.books.9780890426760.pe02. [DOI] [PubMed]
- 32. American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders - Text Revision. 4th ed Washington, D.C.: American Psychiatric Association; 2000. [Google Scholar]
- 33. Diener E, Emmons RA, Larsen RJ, Griffin S.. The Satisfaction with Life Scale. J Pers Assess 1985;49(1):71–5. doi: 10.1207/s15327752jpa4901_13 [DOI] [PubMed] [Google Scholar]
- 34. QualityMetric Quick start guide for the SF-8 Health Survey. Lincoln, RI: QualityMetric Incorporated; 2011. [Google Scholar]
- 35. Ware JE, Sherbourne CD.. The MOS 36-Item Short-Form Health Survey (SF-36): I. Conceptual framework and item selection. Med Care 1992;30(6):473–83. doi: 10.1097/00005650-199206000-00002 [DOI] [PubMed] [Google Scholar]
- 36. Jaccard J, Becker M.. Statistics for the behavioral sciences. 4th ed. Belmont, CA: Wadsworth; 2002. [Google Scholar]
- 37. Curtin CM, Suarez PA, Di Ponio LA, Frayne SM.. Who are the women and men in Veterans Health Administration's current spinal cord injury population? J Rehabil Res Dev 2012;49(3):351–60. doi: 10.1682/JRRD.2010.11.0220 [DOI] [PubMed] [Google Scholar]
- 38. Dijkers MP. Correlates of life satisfaction among persons with spinal cord injury. Arch Phys Med Rehabil 1999;80(8):867–76. doi: 10.1016/S0003-9993(99)90076-X [DOI] [PubMed] [Google Scholar]
- 39. Diener E. Understanding scores on the Satisfaction with Life Scale 2006. Available from: http://internal.psychology.illinois.edu/∼ediener/Documents/Understanding%20SWLS%20Scores.pdf.
- 40. Bombardier CH, Richards JS, Krause JS, Tulsky D, Tate DG.. Symptoms of major depression in people with spinal cord injury: Implications for screening. Arch Phys Med Rehabil 2004;85(11):1749–56. doi: 10.1016/j.apmr.2004.07.348 [DOI] [PubMed] [Google Scholar]
- 41. Narrow WE, Rae DS, Robins LN, Regier DA.. Revised prevalence estimates of mental disorders in the United States: using a clinical significance criterion to reconcile 2 surveys’ estimates. Arch Gen Psychiatry 2002;59(2):115–23. doi: 10.1001/archpsyc.59.2.115 [DOI] [PubMed] [Google Scholar]
- 42. Segal DL, Williams KN.. Structured and semistructured interviews for differential diagnosis: fundamental issues, applications, and features. In: Beidel DC, Frueh BC, Hersen M, editors. Adult psychopathology and diagnosis. 7th ed. Hoboken, NJ: John Wiley & Sons; 2014. [Google Scholar]
- 43. Brugha TS, Bebbington PE, Jenkins R.. A difference that matters: comparisons of structured and semi-structured psychiatric diagnostic interviews in the general population. Psychol Med 1999;29(5):1013–20. doi: 10.1017/S0033291799008880 [DOI] [PubMed] [Google Scholar]
- 44. Gilchrist G, Gunn J.. Observational studies of depression in primary care: what do we know? BMC Fam Pract 2007;8:28. doi: 10.1186/1471-2296-8-28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Chopra MP, Zhang H, Pless Kaiser A, Moye JA, Llorente MD, Oslin DW et al. , PTSD is a chronic, fluctuating disorder affecting the mental quality of life in older adults. Am J Geriatr Psychiatry 2014;22(1):86–97. doi: 10.1016/j.jagp.2013.01.064 [DOI] [PubMed] [Google Scholar]
- 46. Choi Y, Mayer TG, Williams MJ, Gatchel RJ.. What is the best screening test for depression in chronic spinal pain patients? Spine J 2014;14(7):1175–82. doi: 10.1016/j.spinee.2013.10.037 [DOI] [PubMed] [Google Scholar]
- 47. Vilagut G, Forero CG, Pinto-Meza A, Haro JM, de Graaf R, Bruffaerts R et al. , The mental component of the short-form 12 health survey (SF-12) as a measure of depressive disorders in the general population: results with three alternative scoring methods. Value Health 2013;16(4):564–73. doi: 10.1016/j.jval.2013.01.006 [DOI] [PubMed] [Google Scholar]
- 48. Silveira E, Taft C, Sundh V, Waern M, Palsson S, Steen B.. Performance of the SF-36 health survey in screening for depressive and anxiety disorders in an elderly female Swedish population. Qual Life Res 2005;14(5):1263–74. doi: 10.1007/s11136-004-7753-5 [DOI] [PubMed] [Google Scholar]
- 49. Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S et al. , Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry 1994;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002 [DOI] [PubMed] [Google Scholar]
- 50. Hatcher MB, Whitaker C, Karl A.. What predicts post-traumatic stress following spinal cord injury? Br J Health Psychol 2009;14(Pt 3):541–61. doi: 10.1348/135910708X373445 [DOI] [PubMed] [Google Scholar]
- 51. Krause JS, Broderick L.. Outcomes after spinal cord injury: comparisons as a function of gender and race and ethnicity. Arch Phys Med Rehabil 2004;85(3):355–62. doi: 10.1016/S0003-9993(03)00615-4 [DOI] [PubMed] [Google Scholar]
- 52. Krause JS, Saladin LK, Adkins RH.. Disparities in subjective well-being, participation, and health after spinal cord injury: a 6-year longitudinal study. Neurorehabilitation 2009;24(1):47–56. [DOI] [PubMed] [Google Scholar]
- 53. Putzke JD, Hicken BL, Richards JS.. Race: predictor versus proxy variable? Outcomes after spinal cord injury. Arch Phys Med Rehabil 2002;83(11):1603–11. doi: 10.1053/apmr.2002.35115 [DOI] [PubMed] [Google Scholar]
- 54. Hudson CG. Socioeconomic status and mental illness: tests of the social causation and selection hypotheses. Am J Orthopsychiatry 2005;75(1):3–18. doi: 10.1037/0002-9432.75.1.3 [DOI] [PubMed] [Google Scholar]
- 55. Migliorini CE, New PW, Tonge BJ.. Comparison of depression, anxiety and stress in persons with traumatic and non-traumatic post-acute spinal cord injury. Spinal Cord 2009;47(11):783–8. doi: 10.1038/sc.2009.43 [DOI] [PubMed] [Google Scholar]
- 56. Kennedy P, Chessell ZJ.. Traumatic versus non-traumatic spinal cord injuries: are there differential rehabilitation outcomes? Spinal Cord 2013;51(7):579–83. doi: 10.1038/sc.2013.27 [DOI] [PubMed] [Google Scholar]
- 57. Lude P, Kennedy P, Evans M, Lude Y, Beedie A.. Post traumatic distress symptoms following spinal cord injury: a comparative review of European samples. Spinal Cord 2005;43(2):102–8. doi: 10.1038/sj.sc.3101688 [DOI] [PubMed] [Google Scholar]
- 58. New PW, Cripps RA, Bonne Lee B.. Global maps of non-traumatic spinal cord injury epidemiology: towards a living data repository. Spinal Cord 2014;52(2):97–109. doi: 10.1038/sc.2012.165 [DOI] [PubMed] [Google Scholar]
- 59. Devivo MJ. Epidemiology of traumatic spinal cord injury: trends and future implications. Spinal Cord 2012;50(5):365–72. doi: 10.1038/sc.2011.178 [DOI] [PubMed] [Google Scholar]
- 60. Krause JS, Kemp B, Coker J.. Depression after spinal cord injury: Relation to gender, ethnicity, aging, and socioeconomic indicators. Arch Phys Med Rehabil 2000;81(8):1099–109. doi: 10.1053/apmr.2000.7167 [DOI] [PubMed] [Google Scholar]
- 61. Arango-Lasprilla JC, Ketchum JM, Starkweather A, Nicholls E, Wilk AR.. Factors predicting depression among persons with spinal cord injury 1 to 5 years post injury. Neurorehabilitation 2011;29(1):9–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Martin Ginis KA, Papathomas A, Perrier MJ, Smith B.. Psychosocial factors associated with physical activity in ambulatory and manual wheelchair users with spinal cord injury: a mixed-methods study. Disabil Rehabil 2017;39(2):187–92. doi: 10.3109/09638288.2015.1045991 [DOI] [PubMed] [Google Scholar]
- 63. Freixes O, Rivas ME, Agrati PE, Bochkezanian V, Waldman SV, Olmos LE.. Fatigue level in spinal cord injury AIS D community ambulatory subjects. Spinal Cord 2012;50(6):422–5. doi: 10.1038/sc.2011.175 [DOI] [PubMed] [Google Scholar]
- 64. Dipiro ND, Saunders LL, Brotherton S, Kraft S, Krause JS.. Pain and fatigue as mediators of the relationship between mobility aid usage and depressive symptomatology in ambulatory individuals with SCI. Spinal Cord 2014;52(4):316–21. doi: 10.1038/sc.2013.164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Fann JR, Bombardier CH, Richards JS, Tate DG, Wilson CS, Temkin N.. Depression after spinal cord injury: Comorbidities, mental health service use, and adequacy of treatment. Arch Phys Med Rehabil 2011;92(3):352–60. doi: 10.1016/j.apmr.2010.05.016 [DOI] [PubMed] [Google Scholar]
- 66. Galvin LR, Godfrey HP.. The impact of coping on emotional adjustment to spinal cord injury (SCI): Review of the literature and application of a stress appraisal and coping formulation. Spinal Cord 2001;39(12):615–27. doi: 10.1038/sj.sc.3101221 [DOI] [PubMed] [Google Scholar]
- 67. Elliott TR. Studying depression following spinal cord injury: Evidence, policy and practice. J Spinal Cord Med 2015;38(5):584–6. doi: 10.1179/2045772315Y.0000000046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Migliorini C, Tonge B, Taleporos G.. Spinal cord injury and mental health. Aust N Z J Psychiatry 2008;42(4):309–14. doi: 10.1080/00048670801886080 [DOI] [PubMed] [Google Scholar]
- 69. DeVivo MJ, Biering-Sorensen F, New P, Chen Y.. Standardization of data analysis and reporting of results from the International Spinal Cord Injury Core Data Set. Spinal Cord 2011;49(5):596–9. doi: 10.1038/sc.2010.172 [DOI] [PubMed] [Google Scholar]
- 70. Fann JR, Crane DA, Graves DE, Kalpakjian CZ, Tate DG, Bombardier CH.. Depression treatment preferences after acute traumatic spinal cord injury. Arch Phys Med Rehabil 2013;94(12):2389–95. doi: 10.1016/j.apmr.2013.07.004 [DOI] [PubMed] [Google Scholar]
- 71. Guest R, Craig A, Nicholson Perry K, Tran Y, Ephraums C, Hales A et al. , Resilience following spinal cord injury: A prospective controlled study investigating the influence of the provision of group cognitive behavior therapy during inpatient rehabilitation. Rehabil Psychol 2015;60(4):311–21. doi: 10.1037/rep0000052 [DOI] [PubMed] [Google Scholar]
- 72. Kennedy P, Duff J, Evans M, Beedie A.. Coping effectiveness training reduces depression and anxiety following traumatic spinal cord injuries. Br J Clin Psychol 2003;42:41–52. doi: 10.1348/014466503762842002 [DOI] [PubMed] [Google Scholar]
- 73. Dorstyn D, Mathias J, Denson L.. Efficacy of cognitive behavior therapy for the management of psychological outcomes following spinal cord injury: a meta-analysis. J Health Psychol 2011;16(2):374–91. doi: 10.1177/1359105310379063 [DOI] [PubMed] [Google Scholar]
- 74. Fann JR, Bombardier CH, Richards JS, Wilson CS, Heinemann AW, Warren AM et al. , Venlafaxine extended-release for depression following spinal cord injury: a randomized clinical trial. JAMA Psychiatry 2015;72(3):247–58. doi: 10.1001/jamapsychiatry.2014.2482 [DOI] [PubMed] [Google Scholar]
- 75. Krause JS, Saunders LL, Newman S.. Posttraumatic stress disorder and spinal cord injury. Arch Phys Med Rehabil 2010;91(8):1182–7. doi: 10.1016/j.apmr.2010.05.012 [DOI] [PubMed] [Google Scholar]