This study tested newer, single-cycle adenovirus vaccines that amplify Ebola virus antigen genes thousands of times in infected cells. This work shows that these vaccines can generate protective and persistent antibody responses against Ebola virus after a single immunization.
Keywords: Ebola virus, adenovirus, single cycle, vaccine, animal models
Abstract
Recent West African Ebola virus (EBOV) epidemics have led to testing different anti-EBOV vaccines, including a replication-defective adenovirus (RD-Ad) vector (ChAd3-EBOV) and an infectious, replication-competent recombinant vesicular stomatitis virus expressing the EBOV glycoprotein (rVSV-EBOV; also known as rVSV-ZEBOV). While RD-Ads elicit protection, when scaled up to human trials, the level of protection may be much lower than that of vaccines containing viruses that can replicate. Although a replication-competent Ad (RC-Ad) vaccine might generate a level of protection approximating that of rVSV, this infectious vector would also risk causing adenovirus disease. We recently described a “single-cycle” adenovirus (SC-Ad) vector that amplifies antigen genes like RC-Ad, but that avoids the risk of adenovirus infection. Here we have tested an SC-Ad6 vector expressing the glycoprotein (GP) from a 2014 EBOV strain in mice, hamsters, and rhesus macaques. We show that SC-Ad6-EBOV GP induces a high level of serum antibodies in all species and mediates significant protection against pseudo-challenge with rVSV-EBOV expressing luciferase in mice and hamsters. These data suggest that SC-Ad6-EBOV GP may be useful during future EBOV outbreaks.
(See the Editorial Commentary by Holbrook on pages 1858–60.)
Ebola virus (EBOV) is a cause of fatal hemorrhagic fever in humans [1, 2]. EBOV was the causative agent of the most recent and largest documented Ebola virus disease (EVD) epidemic, which occurred during 2013–2016 and had a 39.5% case-fatality rate [3, 4]. EBOV displays glycoprotein GP1,2, which mediates membrane attachment and fusion on its surface [5, 6]. GP1,2 is the primary target for neutralizing antibodies and is thought to be an ideal antigen candidate for EBOV vaccines.
Thirteen vaccine candidates were tested in 2014–2015, during the epidemic [7]. The 2 leading EBOV vaccines were a replication-defective (RD) recombinant chimpanzee adenovirus type 3 vectored vaccine (ChAd3-EBOV; National Institute of Allergy and Infectious Diseases [NIAID] and GlaxoSmithKline) and a replication-competent, recombinant vesicular stomatitis virus vaccine (rVSV-EBOV; also known as rVSV-ZEBOV; NIAID, Public Health Agency of Canada, and Merck) [8].
rVSV-EBOV generated EBOV binding antibodies regardless of dose in phase 1 trials [9–11]. While rVSV-EBOV showed efficacy, it is a live replication-competent virus [8, 11–13]. It infects a cell, replicates its transgene many times, expresses large amounts of antigen, but also produces infectious progeny viruses. Intramuscularly administered rVSV-EBOV was shown to replicate in peripheral tissues and can lead to vaccine-associated arthritis, vasculitis, and dermatitis in both low- and high-dose vaccinations [14, 15].
ChAd3 was effective in nonhuman primate models and also progressed into clinical trials [8, 16–20]. Phase 1 trials suggested no vaccine-elicited serious adverse events, immunogenicity in high-dose groups, and promising humoral and cell-mediated responses within the range associated with protection in primates [16–18, 20].
Although ChAd3 generated EBOV-specific antibody and T-cell responses, its efficacy is limited by the fact that it is a RD vaccine [21]. Unlike rVSV-EBOV, ChAd3-EBOV does not amplify, so it infects 1 cell, delivers 1 viral genome, and expresses only “1X” of the EBOV GP antigen. In primates, EBOV-specific responses generated by ChAd3 were only transient and required boosting with modified vaccinia Ankara to retain durable protection [8, 16, 18, 19].
Given the lack of antigen replication and amplification by RD-Ads, we developed “single-cycle” Ad (SC-Ad6) vectors that replicate transgenes thousands of times, like replication-competent Ad (RC-Ad), but cannot produce infectious viruses [22–24]. SC-Ad generates 100-fold more protein than RD-Ads when used at equal doses and equal amounts of antigen as RD-Ad, with 33–100 times fewer viral particles [23, 24]. As an influenza vaccine, SC-Ad6 mediated superior levels of hemagglutination inhibition antibodies and protection after a single intranasal vaccination [22].
Given the better vaccine effects of SC-Ad and the absence of a safe, Food and Drug Administration–approved, replicating Ad vaccine for EBOV, we tested a SC-Ad6-EBOV GP vaccine expressing a 2014 EBOV GP in mice, hamsters, and rhesus macaques.
MATERIALS AND METHODS
Cell Culture
293 human embryonic kidney cells (Microbix), Vero cells (American Type Culture Collection), and A549 lung carcinoma cells (American Type Culture Collection) were maintained at 37°C in Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 10% fetal bovine serum (FBS; HyClone) and penicillin/streptomycin at 100 U/mL (Gibco). 293-IIIA-LacI cells were generated by transfection of 293-IIIA cells [24] with the p3’SS plasmid that expresses nuclear targeted LacI repressor [25]. 293-IIIA-LacI cells were cloned after selection in 100 µg/mL hygromycin B.
SC-Ad6 Expressing EBOV Glycoprotein
A codon-optimized GP complementary DNA encoding EBOV-Makona isolate KJ660346 [3] (Genscript) was recombined into SC-Ad6 to generate SC-Ad6-EBOV GP as described elsewhere [22–24]. Control Ad6 viruses expressing human immunodeficiency virus type 1 (HIV) GP160 (Env) or influenza virus hemagglutinin (HA) were also used. Viruses were rescued, amplified, and purified as previously described [22–24]. Virus comparisons were performed using virus particles as recommended by Nyberg-Hoffman et al [26].
rVSV Vectors Pseudotyped With EBOV GP
Recombinant rVSVs expressing the EBOV-Mayinga GP and luciferase (rVSV-EBOV-Luc) were produced as described previously [27].
Western Blotting
A549 cells were infected with SC-Ad6-EBOV GP or rVSV-EBOV-Luc at different multiplicities of infection, determined in virus particles/cell or plaque-forming units (PFU)/cell, respectively. Twenty-four hours later, cell lysates were analyzed by Western blotting with primary Syrian hamster antibody against EBOV GP (1:500) and Protein A/G–horseradish peroxidase (1:10 000). SuperSignal West Dura (Thermo Scientific) was added, and blots were imaged on an In Vivo F Station (Kodak).
Animals
CD-1 mice (Charles River Laboratories) and Syrian hamsters (Harlan Sprague-Dawley) were housed in the Mayo Clinic Animal Facility. Adult female rhesus macaques (Macaca mulatta) of Indian origin were maintained in the specific-pathogen-free breeding colony at the Michael Keeling Center for Comparative Medicine and Research at the University of Texas M. D. Anderson Cancer Center (Bastrop, TX). All animal handling and experiments were performed according to the provisions of the Animal Welfare Act, the Public Health Service Animal Welfare Policy, the principles of the National Institutes of Health Guide for the Care and Use of Laboratory Animals, and the policies and procedures of the Institutional Animal Care and Use Committee at Mayo Clinic (for rodents) and the University of Texas M. D. Anderson Cancer Center (for nonhuman primates).
Immunizations and Sample Collection
Hamsters were anesthetized with isoflurane and immunized by the indicated routes with the indicated amounts of vaccine. Rhesus macaques were anesthetized with ketamine and immunized by the intranasal or intramuscular route with the indicated amounts of Ad vaccine. At various time points, hamsters were anesthetized, and serum was collected from submandibular veins. In rhesus macaques, plasma samples were collected at each time point before any immunization via peripheral vein.
Pseudo-Challenge With rVSV-EBOV-Luc
Mice (n = 10) were immunized intranasally with 1 × 109 viral particles/mL of SC-Ad6-influenza virus HA, SC-Ad6-EBOV GP, or phosphate-buffered saline (PBS). Serum was collected 1 month and 28 days after immunization, before intranasal challenge with 2.5 × 105 PFU/mL of rVSV-EBOV-Luc. Serum was also collected 2 and 6 weeks after challenge. Animals were imaged using a Xenogen IVIS instrument on days 1, 3, and 6 after pseudo-challenge, to quantify rVSV-EBOV-Luc infection. In brief, animals were anesthetized with a 100-μL intraperitoneal injection of a solution of ketamine and xylazine. Animals then received a 150-μL intraperitoneal injection and 10 μL per nostril of D-luciferin. Animals were imaged 10 minutes later, and images were analyzed using the Living Image 4.5.2 software. Aged Syrian hamsters were challenged in the same way.
Enzyme-Linked Immunosorbent Assay (ELISA)
Immulon 4 HBX plates (Thermo) were coated with 100 ng/well of recombinant EBOV GP (EBOV rGPdTM; IBT Bioservices) in 1X PBS overnight. Wells were washed and blocked with 200 μL blocking buffer (5% milk and 1X Tris-buffered saline with Tween 20) at room temperature for 2 hours. Wells were washed, and 100 μL of 1:200 dilutions of each sample were added to plates and incubated for 3 hours at room temperature. Wells were washed 4 times, and 100 μL of rabbit anti-hamster anti–immunoglobulin M, immunoglobulin A, and immunoglobulin G–horseradish peroxidase (Brookwood Biomedical, Birmingham, AL) diluted 1:10000 were added to each well. Plates were incubated for 2 hours at room temperature. Wells were washed 4 times, and 50 μL of 1 step Ultra TMB ELISA (Thermo Fisher Scientific) was added. When color developed, 50 μL of 2 mol/L H2SO4 were added. OD450 was determined with a Beckman Coulter DTX 880. Assays were conducted similarly for end point–titer ELISAs. Reciprocal titers were statistically defined on the basis of 95% confidence intervals, as determined elsewhere [28].
rVSV-EBOV-Luc Neutralization Assay
One hundred–microliter serum samples were incubated at 56°C for 0.5 hours. A total of 65 μL of heat-inactivated sera was added to serum-free DMEM to make a 1:10 dilution. A total of 200 μL of each sample was added to the first column of empty 96-well plates (Corning) in triplicate. The remaining wells received 100 μL of serum-free DMEM. A total of 100 μL of diluted plasma was serially transferred from the first column onto the next. rVSV-EBOV-Luc was diluted to 500 PFU/mL in serum-free DMEM. One hundred microliters (50 PFU) of rVSV-EBOV-Luc was added to each well (except the negative control wells), and samples were incubated for 1 hour at 37°C with rotating at 50 rpm. One hundred microliters of the mixtures was added to 96-well, black-walled, clear-bottomed plates (Corning) containing 80% confluent Vero cells and incubated for 24 hours at 37°C. Luminescence was measured with a Bright-Glo Luciferase Assay System (Promega) on the Beckman Coulter DTX 880 Multimode Detector system.
Statistical Analysis
Prism 7 graphical software was used for all statistical analyses.
RESULTS
Plasmid and SC-Ad6 Expressing EBOV GP
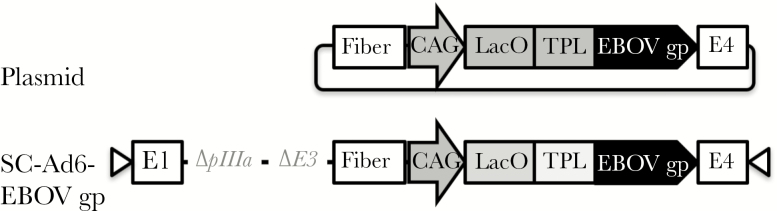
We previously demonstrated that SC-Ad6 vectors expressing green fluorescent protein–luciferase or influenza virus hemagglutinin generate more-robust protein expression and immune responses than RD-Ad6 vectors in vitro and in vivo [22–24, 29]. We generated a SC-Ad6-EBOV GP vector as previously described [22–24, 30] (Figure 1).
Figure 1.
Schematic of shuttle and single-cycle adenovirus 6 (SC-Ad6) plasmids expressing Ebola virus glycoprotein (EBOV GP). CAG, cytomegalovirus/β-actin promoter; LacO, binding site transcriptional repression; TPL, tripartate leader.
To compare plasmid DNA and Ad gene–based vaccination approaches for EBOV, groups of 5 mice each were immunized intramuscularly. After a single immunization, SC-Ad induced significantly higher EBOV GP–specific antibodies than those generated by the plasmid (P < .01; Supplementary Figure 1). Plasmid and Ad vaccines are frequently used in prime-boost immunizations [31]. We tested several combinations of plasmid and Ad prime-boosts. At 14 days and 47 days after boost (68 days after priming), the EBOV GP–specific antibody levels in Ad-primed groups were significantly higher than in plasmid-primed animals (Supplementary Figure 1).
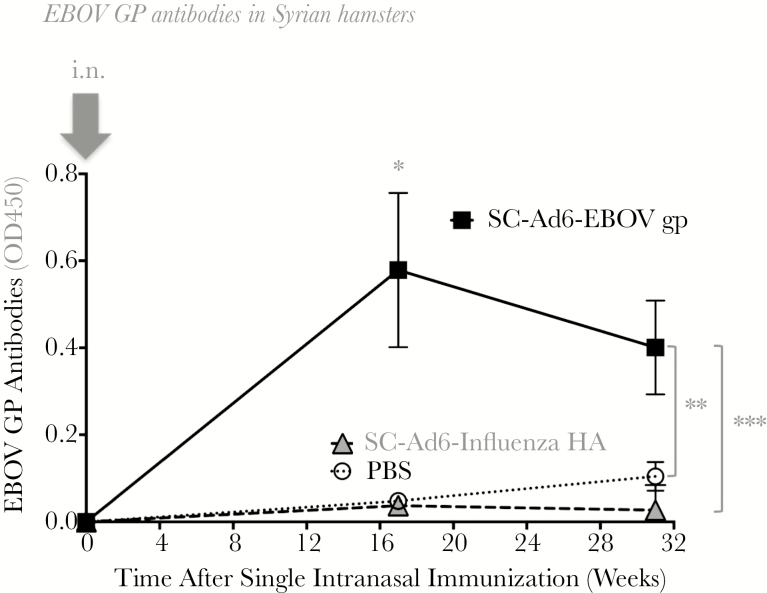
Single Intranasal Vaccination With Low-Dose SC-Ad6-EBOV GP Induces Persistent Antibodies in Syrian Hamsters
Unlike mice, Syrian hamsters can support the human Ad life cycle and are better models to accurately investigate transgene expression from SC-Ad vaccines [32]. To test SC-Ad in a more permissive animal model, 5 Syrian hamsters were immunized intranasally with PBS or 1 × 109 viral particles of SC-Ad6-EBOV GP or SC-Ad6-influenza virus HA (Figure 2). This intranasal immunization generated EBOV GP–specific antibodies at titers that peaked 17 weeks (P < .01) after a single vaccination and remained significantly elevated beyond 6 months as compared to controls (at week 31, P < .05 and P < .01 for comparisons of SC-Ad6-EBOV GP recipients to PBS recipients and SC-Ad6-influenza virus HA recipients, respectively).
Figure 2.
Intranasal vaccination with a single-cycle adenovirus 6 (SC-Ad6) vector expressing Ebola virus glycoprotein (SC-Ad6-EBOV GP) elicits robust immune responses. Groups of 5 hamsters received a single immunization of phosphate-buffered saline (PBS) or a low dose of 1 × 109 viral particles of SC-Ad6-EBOV GP or SC-Ad6-influenza virus hemagglutinin (HA) (negative control). EBOV GP–binding antibodies were examined at weeks 17 and 31 after immunization. *P < .01, compared with PBS recipients and SC-Ad6-influenza virus HA recipients (week 17); **P < .05, compared with PBS recipients (week 31); and ***P < .01, compared with SC-Ad6-influenza virus HA recipients (week 31) by 1-way analysis of variance.
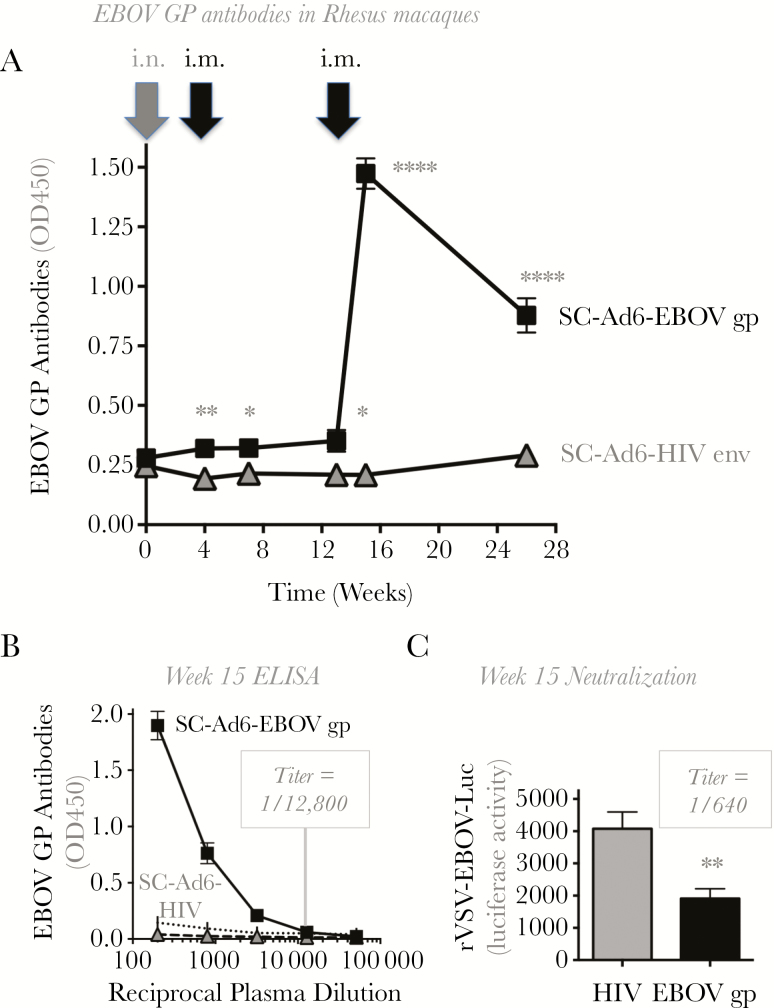
SC-Ad6-EBOV GP Immunization Generates Robust Immune Responses in Rhesus Macaques
Groups of 4 female rhesus macaques were immunized intranasally with 2 × 1010 viral particles of either SC-Ad6-EBOV GP or SC-Ad6 vector expressing HIV GP160. One mucosal immunization generated significant EBOV GP–specific antibodies in plasma within 1 week of vaccination (Figure 3A).
Figure 3.
Serum antibody responses in immunized rhesus macaques. A, Four female rhesus macaques were vaccinated by the intranasal route (gray arrow) with 2 × 1010 viral particles of a single-cycle adenovirus 6 (SC-Ad6) vector expressing Ebola virus glycoprotein (SC-Ad6-EBOV GP) or a SC-Ad6 vector expressing human immunodeficiency virus type 1 (HIV) gp160 (negative control). Macaques were then boosted intramuscularly at weeks 4 and 13 (black arrows). Plasma was collected at weeks 4, 7, 13, 15, and 26 and evaluated by enzyme-linked immunosorbent assay. *P < .0112 (week 13), *P < .0257 (week 7), **P < .0081, and ****P < .0001. B, Plasma end point titers at peak antibody response. P < .0001, by the t test, at a 1:12800 dilution for comparison of HIV Env and EBOV GP recipients. C, Week 15 plasma neutralization assay. P < .01, by 1-way analysis of variance, at a 1:640 dilution for comparison of HIV Env and EBOV GP recipients.
One challenge with viral-vectored vaccines is the generation of antivector immune responses that may prevent or reduce immune responses if the vaccine is used a second time. Previous work in mice indicated that anti-Ad antibodies can be evaded by switching between the intramuscular route and the mucosal oral route [33]. To test this, macaques were immunized a second time with SC-Ad6, at week 4, using the intramuscular route. No obvious increases in titers of antibodies against the EBOV GP were observed through week 13, although antibody titers in the SC-Ad6-EBOV GP group remained statistically higher than those in the control Ad group (Figure 3A). The animals were immunized a third time with SC-Ad6 at week 13, via the intramuscular route. The third immunization increased EBOV GP–specific antibodies significantly in the SC-Ad6-EBOV GP group (P < .0001). The antibody titers remained elevated in plasma after this last boost through 26 weeks after the first immunization (P < .0001). Plasma from the week 15 peak antibody response was serially diluted to calculate end point titers. The 3 immunizations with SC-Ad6-EBOV GP elicited an antibody titer of 1:12800 (Figure 3B). Week 15 peak antibody plasma samples from SC-Ad6-HIV Env recipients and SC-Ad6-EBOV GP recipients were tested for their ability to neutralize rVSV-EBOV-Luc (Figure 3C). Plasma from SC-Ad6-EBOV GP had a rVSV-EBOV-Luc neutralizing titer of 1:640 when compared to SC-Ad6-HIV Env samples (P < .01).
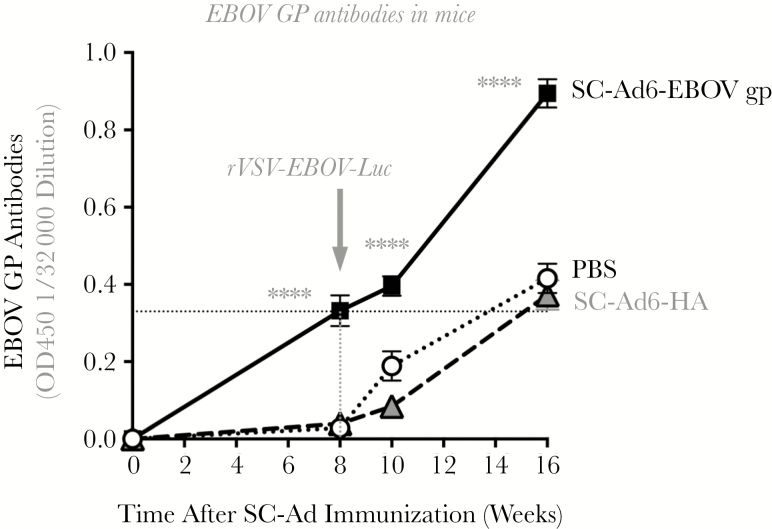
SC-Ad6-EBOV GP Immunization Inhibits rVSV-EBOV-Luc Infection after Intranasal Pseudo-Challenge
Groups of 10 CD1 mice were immunized intranasally a single time with 109 viral particles of SC-Ad6-EBOV GP, SC-Ad6-influenza virus HA, or PBS. This single vaccination of SC-Ad6-EBOV GP generated strong antibody responses (Figure 4 and Supplementary Figures 2 and 3), with an end point titer >1:32000 at 8 weeks and 1:16000 at 10 and 16 weeks.
Figure 4.
Vaccination with a single-cycle adenovirus 6 (SC-Ad6) vector expressing Ebola virus glycoprotein (SC-Ad6-EBOV GP) induces high antibodies after rVSV-EBOV-Luc pseudo-challenge. Sera from CD-1 outbred mice immunized with phosphate-buffered saline or the indicated SC-Ads from weeks 8, 10, and 16 were titrated (Supplementary Figures 2 and 3). Representative findings of enzyme-linked immunosorbent assays of EBOV GP–binding antibody in sera diluted 1:32000 are shown. ****P < .0001, by 1-way analysis of variance, for comparison of the SC-Ad6-EBOV GP group to the other groups at each time point.
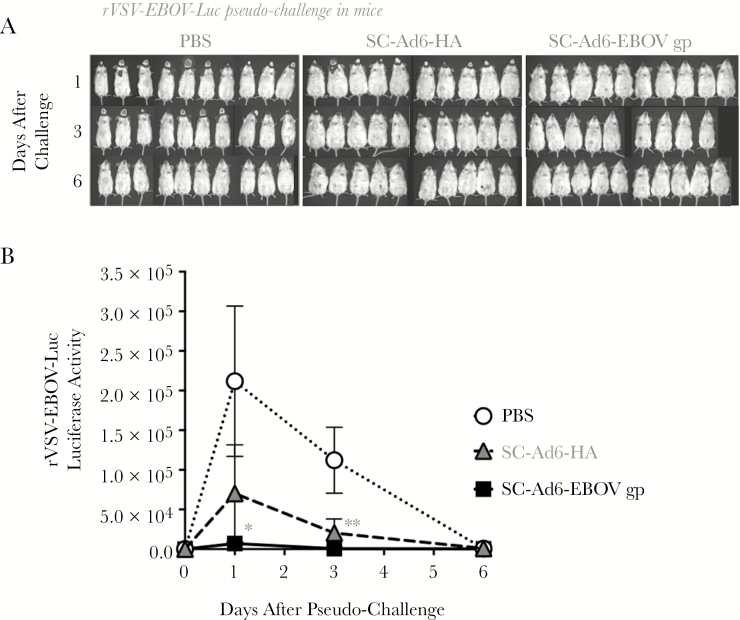
At 8 weeks, the animals were pseudo-challenged intranasally with 2.5 × 105 PFU of rVSV-EBOV-Luc (Figure 5). rVSV-driven luciferase activity was monitored over time (Figure 5A). Under these conditions, SC-Ad mediated significant reductions in rVSV-driven luciferase activity 1 and 3 days after challenge (P < .05; Figure 5B). Single SC-Ad6-EBOV GP immunization generated antibody levels over 8 weeks that were similar to those generated by the rVSV-EBOV-Luc challenge over 8 weeks in PBS or SC-Ad-influenza virus HA immunized mice (Figure 4).
Figure 5.
Vaccination with a single-cycle adenovirus 6 (SC-Ad6) vector expressing Ebola virus glycoprotein (SC-Ad6-EBOV GP) protects mice against intranasal rVSV-EBOV-Luc pseudo-challenge. Ten CD-1 outbred mice were intranasally immunized with 1 × 109 viral particles of SC-Ad6-EBOV GP, SC-Ad6-influenza virus hemagglutinin (HA), or phosphate-buffered saline (PBS). Eight weeks later, the animals were challenged intranasally with 2.5 × 105 plaque-forming units of rVSV-EBOV-Luc. Average luciferase activity was assessed with Xenogen IVIS imaging (A) and quantified (B) on days 1, 3, and 6 after challenge. *P < .05, by 1-way analysis of variance, for comparison of the SC-Ad-EBOV group to the other groups at day 1; **P < .05, by 1-way analysis of variance, for comparison of the SC-Ad6-influenza virus HA and SC-Ad6-EBOV GP groups to the other groups at day 3.
SC-Ad6-EBOV GP Protects Aged Hamsters >1 Year After a Single Vaccination
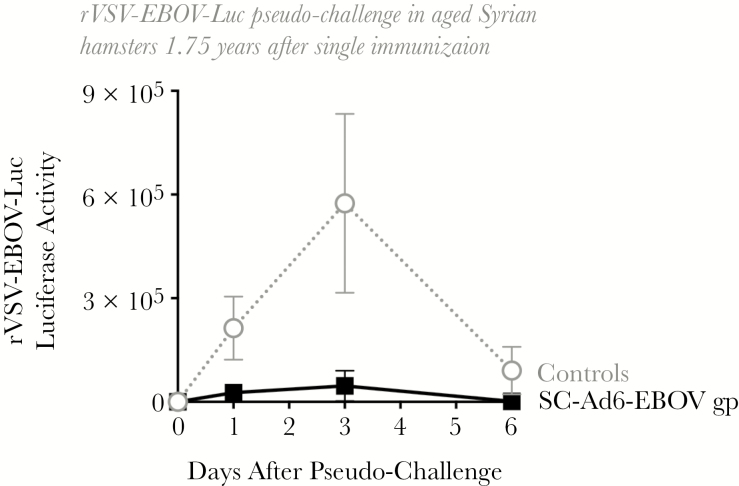
The PBS control and 3 aged hamsters from Figure 2 survived for 21 months after the single vaccination with 1 × 109 viral particles of SC-Ad6-EBOV GP. Considering their age, these remaining 2-year-old hamsters were challenged intranasally with rVSV-EBOV-Luc, and luciferase activity was measured (Figure 6). Under these conditions, SC-Ad reduced rVSV-luciferase activity after challenge when compared to controls, although this did not reach significance (P = .055 and .057, by the 1-tailed t test on days 1 and 3, respectively).
Figure 6.
Syrian hamsters are protected against recombinant vesicular stomatitis virus–Ebola virus (EBOV)–Luc pseudo-challenge over 1 year after single intranasal immunization with single-cycle adenovirus 6 (SC-Ad6) expressing EBOV glycoprotein (GP). Groups of 3 hamsters that had received a single intranasal vaccination of SC-Ad6-EBOV GP or SC-Ad6-influenza virus hemagglutinin (HA; negative control) 1.75 years prior underwent pseudo-challenge with 2.5 × 105 plaque-forming units of rVSV-EBOV-Luc. rVSV-driven luciferase activity was examined on days 1, 3, and 6 after challenge. P = .055 (day 1) and P = .057 (day 3), by 1-way analysis of variance.
DISCUSSION
EBOV vaccines ChAd3-EBOV and rVSV-EBOV both generated promising immune responses in preclinical and human trials [8, 11, 13]. While rVSV-EBOV shows good promise, some vaccinated individuals had side effects and persistent viral loads in peripheral tissues [14, 15]. In contrast, ChAd3-EBOV produced durable responses with no adverse effects, but its immune responses were weaker than those achieved with rVSV-EBOV [8].
This observation was not particularly surprising given that ChAd3-EBOV is a replication-defective vaccine whereas rVSV-EBOV is fully replication competent. Unlike ChAd3-EBOV, rVSV-EBOV amplifies antigen expression via replication and generates infectious progeny virus that can infect an increasing number of cells.
In this study, we explored the usefulness of a replicating, single-cycle Ad (SC-Ad) vector as an alternate EBOV vaccine. Unlike ChAd3-EBOV, SC-Ad vectors retain their E1 gene and their ability to replicate viral DNA up to 10000 times the initial levels, but they fail to form infectious progeny owing to a deletion of the critical virion cement protein IIIa [22–24]. Previous work showed that SC-Ads generate significantly higher transgene expression and antibody levels than RD-Ads [22–24, 29] (data not shown).
We initially compared the ability of naked DNA injection to SC-Ad vaccination for their ability to drive anti-Ebola GP antibodies. Consistent with previous observations, the Ad-vectored vaccine generated markedly stronger immune responses against GP after only 1 immunization. When the animals were boosted with the same or alternate vaccine, antibody titers increased only in the SC-Ad–primed group. For the DNA-primed group, it is unclear why neither vector boosted these responses. Nonetheless, these data suggested that the SC-Ad vaccine was more robust to proceed to testing as a single vaccine.
We showed that single mucosal intranasal immunization of mice or Ad-permissive hamsters with SC-Ad6-EBOV GP generated robust antibodies that persisted for >6 months after 1 mucosal vaccination. We also showed that a single intranasal Ad vaccination with SC-Ad6-EBOV GP generated significant levels of EBOV GP–specific antibodies in rhesus macaques. A single systemic intramuscular boost with the same Ad6 serotype vaccine did not boost these responses, but a second intramuscular dose with the same Ad6 serotype markedly amplified EBOV binding and neutralizing antibodies. Notably, these antibodies persisted for 6 months after priming. This suggests that one may be able to administer 1 SC-Ad serotype by different immunization routes to avoid the expense of generating multiple GMP grade vaccines for prime-boost strategies.
We next tested the vaccine for its ability to resist replication-competent rVSV-EBOV-Luc displaying the EBOV GP that expresses luciferase. This demonstrated that SC-Ad6-EBOV GP mediated significant protection against challenge with this rVSV-EBOV-Luc. SC-Ad and rVSV-EBOV-Luc generated similar kinetics and levels of antibody responses against EBOV GP after 1 exposure to either vector.
Another side benefit of the pseudo-challenge study is that it provides proof of principle for the use of SC-Ad and rVSV-EBOV-Luc as prime-boost vaccines, a strategy already used by the Russian licensed EBOV vaccines, albeit not with replicating Ad as a platform [34, 35]. Mice primed with SC-Ad6-EBOV GP and then boosted with rVSV-EBOV-Luc generated stronger antibody responses than those only vaccinated with rVSV-EBOV-Luc or with SC-Ad. This suggests a potential coupling of these 2 replicating vaccines to induce possibly stronger and longer-lasting immunity.
Since mice do not support adenovirus replication, these results may underestimate the relative potency of SC-Ad. Likewise, the addition of luciferase to rVSV-EBOV attenuates but does not ablate VSV replication. This leads to an unfair comparison of potency to that observed in vaccine trials with rVSV-EBOV and is not reflective of a true EBOV challenge. We should also emphasize that comparison of the 2 viruses may always be unfair, because they are titered by different methods and choosing an ideal vaccine dose for either will be complicated when comparing in vivo. Ultimately, the best comparisons or combinations of SC-Ad and rVSV will be in human vaccine trials where both viruses can replicate.
These data suggest that SC-Ads may be useful as a vaccine against EBOV in humans. SC-Ad may be useful alone or as a prime-boost strategy perhaps with replication-competent rVSV.
Supplementary Data
Supplementary materials are available at The Journal of Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Acknowledgments. We thank Mary Barry and Laura Evgin, for their invaluable technical assistance, and Dr Heinz Feldmann (National Institute of Allergy and Infectious Diseases, National Institutes of Health), for his insight and for generously providing the rVSV-EBOV-Luc vector.
Disclaimer. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official view of National Institutes of Health.
Financial support. This work was supported by NIH/NIAID grants R01 AI096967 and R01 AI136718 and the Walter & Lucille Rubin Fund in Infectious Diseases Honoring Michael Camilleri, M.D. at Mayo Clinic, and the Discovery Translation Fund at Mayo Clinic (to M.A.B). This work was supported by the National Center for Advancing Translational Sciences (Clinical and Translational Science award UL1 TR000135 to S. S. A. Z.), National Institutes of Health; and by the Initiative for Maximizing Student Development (to S. S. A. Z.) at Mayo Clinic. This work was supported by the NIAID Intramural Research Fund (to A. M.).
Potential conflicts of interest. All authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Doukas T. Analysis of Ebola glycoprotein sequences from strains of varying lethality. Stanford, CA: Stanford University, 2002. [Google Scholar]
- 2. Sanchez A, Khan AS, Zaki SR, Nabel GJ, Ksiazek TG, Peters CJ. Filoviridae: Marburg and Ebola viruses. In: Knipe DM, Howley PM, eds. Fields virology. 1. 4th ed. Philadelphia, PA: Lippincott Williams and Wilkins, 2001:1279–304. [Google Scholar]
- 3. Baize S, Pannetier D, Oestereich L, et al. Emergence of Zaire Ebola virus disease in Guinea. N Engl J Med 2014; 371:1418–25. [DOI] [PubMed] [Google Scholar]
- 4. Dixon MG, Schafer IJ; Centers for Disease Control and Prevention (CDC) Ebola viral disease outbreak–West Africa, 2014. MMWR Morb Mortal Wkly Rep 2014; 63:548–51. [PMC free article] [PubMed] [Google Scholar]
- 5. Yoshihiro K. How ebola virus infects cells. N Engl J Med 2005; 352:2645–6. [DOI] [PubMed] [Google Scholar]
- 6. Mohan GS, Ye L, Li W, et al. Less is more: Ebola virus surface glycoprotein expression levels regulate virus production and infectivity. J Virol 2015; 89:1205–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. World Health Organization (WHO). Ebola R&D landscape of clinical candidates and trials. Geneva: WHO, 2015. [Google Scholar]
- 8. Widdowson MA, Schrag SJ, Carter RJ, et al. Implementing an Ebola vaccine study—Sierra Leone. MMWR Suppl: Centers for Disease Control 2016. [DOI] [PubMed] [Google Scholar]
- 9. Agnandji ST, Huttner A, Zinser ME, et al. Phase 1 trials of rVSV Ebola vaccine in Africa and Europe. N Engl J Med 2016; 374:1647–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Regules JA, Beigel JH, Paolino KM, et al. ; rVSVΔG-ZEBOV-GP Study Group A Recombinant Vesicular Stomatitis Virus Ebola Vaccine. N Engl J Med 2017; 376:330–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Skrip LA, Galvani AP. Next steps for Ebola vaccination: deployment in non-epidemic, high-risk settings. PLoS Negl Trop Dis 2016; 10:e0004802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Henao-Restrepo AM, Camacho A, Longini IM, et al. Efficacy and effectiveness of an rVSV-vectored vaccine in preventing Ebola virus disease: final results from the Guinea ring vaccination, open-label, cluster-randomised trial (Ebola Ça Suffit!). Lancet 2017; 389:505–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. World Health Organization. Ebola vaccines, therapies, and diagnostics 2015 http://www.who.int/medicines/emp_ebola_q_as/en/. Accessed 5 September 2017.
- 14. Huttner A, Dayer JA, Yerly S, et al. ; VSV-Ebola Consortium The effect of dose on the safety and immunogenicity of the VSV Ebola candidate vaccine: a randomised double-blind, placebo-controlled phase ½ trial. Lancet Infect Dis 2015; 15:1156–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ledgerwood JE. Use of low dose rVSV-ZEBOV: safety issues in a Swiss cohort. Lancet Infect Dis 2015; 15:1117–9. [DOI] [PubMed] [Google Scholar]
- 16. Ewer K, Rampling T, Venkatraman N, et al. A monovalent Chimpanzee adenovirus Ebola vaccine boosted with MVA. N Engl J Med 2016; 374:1635–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ledgerwood JE, DeZure AD, Stanley DA, et al. ; VRC 207 Study Team Chimpanzee adenovirus vector Ebola vaccine. N Engl J Med 2017; 376:928–38. [DOI] [PubMed] [Google Scholar]
- 18. Sridhar S. Clinical development of Ebola vaccines. Ther Adv Vaccines 2015; 3:125–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Stanley DA, Honko AN, Asiedu C, et al. Chimpanzee adenovirus vaccine generates acute and durable protective immunity against ebolavirus challenge. Nat Med 2014; 20:1126–9. [DOI] [PubMed] [Google Scholar]
- 20. Tapia MD, Sow SO, Lyke KE, et al. Use of ChAd3-EBO-Z Ebola virus vaccine in Malian and US adults, and boosting of Malian adults with MVA-BN-Filo: a phase 1, single-blind, randomised trial, a phase 1b, open-label and double-blind, dose-escalation trial, and a nested, randomised, double-blind, placebo-controlled trial. Lancet Infect Dis 2016; 16:31–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Maeda K, West K, Hayasaka D, Ennis FA, Terajima M. Recombinant adenovirus vector vaccine induces stronger cytotoxic T-cell responses than recombinant vaccinia virus vector, plasmid DNA, or a combination of these. Viral Immunol 2005; 18:657–67. [DOI] [PubMed] [Google Scholar]
- 22. Crosby CM, Matchett WE, Anguiano-Zarate SS, et al. Replicating single-cycle adenovirus vectors generate amplified influenza vaccine responses. J Virol 2017; 91:e00720–00716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Crosby CM, Nehete P, Sastry KJ, Barry MA. Amplified and persistent immune responses generated by single-cycle replicating adenovirus vaccines. J Virol 2015; 89:669–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Crosby CM, Barry MA. IIIa deleted adenovirus as a single- cycle genome replicating vector. Virology 2014; 462-463:158–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Fieck A, Wyborski DL, Short JM. Modifications of the E.coli Lac repressor for expression in eukaryotic cells: effects of nuclear signal sequences on protein activity and nuclear accumulation. Nucleic Acids Res 1992; 20:1785–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nyberg-Hoffman C, Shabram P, Li W, Giroux D, Aguilar-Cordova E. Sensitivity and reproducibility in adenoviral infectious titer determination. Nat Med 1997; 3:808–11. [DOI] [PubMed] [Google Scholar]
- 27. Marzi A, Ebihara H, Callison J, et al. Vesicular stomatitis virus-based Ebola vaccines with improved cross-protective efficacy. J Infect Dis 2011; 204(Suppl 3):S1066–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Frey A, Di Canzio J, Zurakowski D. A statistically defined endpoint titer determination method for immunoassays. J Immunol Methods 1998; 221:35–41. [DOI] [PubMed] [Google Scholar]
- 29. Crosby CM, Barry MA. Transgene expression and host cell responses to replication-defective, single-cycle, and replication-competent adenovirus vectors. Genes 2017; 8(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Piedra PA, Poveda GA, Ramsey B, McCoy K, Hiatt PW. Incidence and prevalence of neutralizing antibodies to the common adenoviruses in children with cystic fibrosis: implication for gene therapy with adenovirus vectors. Pediatrics 1998; 101:1013–9. [DOI] [PubMed] [Google Scholar]
- 31. Lasaro MO, Ertl HC. New insights on adenovirus as vaccine vectors. Mol Ther 2009; 17:1333–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Thomas MA, Spencer JF, Wold WS. Use of the Syrian hamster as an animal model for oncolytic adenovirus vectors. Methods Mol Med 2007; 130:169–83. [DOI] [PubMed] [Google Scholar]
- 33. Xiang ZQ, Gao GP, Reyes-Sandoval A, Li Y, Wilson JM, Ertl HC. Oral vaccination of mice with adenoviral vectors is not impaired by preexisting immunity to the vaccine carrier. J Virol 2003; 77:10780–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Dolzhikova IV, Tokarskaya EA, Dzharullaeva AS, et al. Virus-Vectored Ebola Vaccines. Acta Naturae 2017; 9:4–11. [PMC free article] [PubMed] [Google Scholar]
- 35. Dolzhikova IV, Zubkova OV, Tukhvatulin AI, et al. Safety and immunogenicity of GamEvac-Combi, a heterologous VSV- and Ad5-vectored Ebola vaccine: An open phase I/II trial in healthy adults in Russia. Hum Vaccin Immunother 2017; 13:613–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.