Abstract
Background
Streptococcus pneumoniae is capable of causing multiple infectious syndromes and occasionally causes outbreaks. The objective of this review is to update prior outbreak reviews, identify control measures, and comment on transmission.
Methods
We conducted a review of published S. pneumoniae outbreaks, defined as at least two linked cases of S. pneumoniae.
Results
A total of 98 articles (86 respiratory; 8 conjunctivitis; 2 otitis media; 1 surgical site; 1 multiple), detailing 94 unique outbreaks occurring between 1916 to 2017 were identified. Reported serotypes included 1, 2, 3, 4, 5, 7F, 8, 12F, 14, 20, and 23F, and serogroups 6, 9, 15, 19, 22. The median attack rate for pneumococcal outbreaks was 7.0% (Interquartile range: 2.4%, 13%). The median case-fatality ratio was 12.9% (interquartile range: 0%, 29.2%). Age groups most affected by outbreaks were older adults (60.3%) and young adults (34.2%). Outbreaks occurred in crowded settings, such as universities/schools/daycares, military barracks, hospital wards, and long-term care facilities. Of outbreaks that assessed vaccination coverage, low initial vaccination or revaccination coverage was common. Most (73.1%) of reported outbreaks reported non-susceptibility to at least one antibiotic, with non-susceptibility to penicillin (56.0%) and erythromycin (52.6%) being common. Evidence suggests transmission in outbreaks can occur through multiple modes, including carriers, infected individuals, or medical devices. Several cases developed disease shortly after exposure (< 72 h). Respiratory outbreaks used infection prevention (55.6%), prophylactic vaccination (63.5%), and prophylactic antibiotics (50.5%) to prevent future cases. PPSV23 covered all reported outbreak serotypes. PCV13 covered 10 of 16 serotypes. For conjunctival outbreaks, only infection prevention strategies were used.
Conclusions
To prevent the initial occurrence of respiratory outbreaks, vaccination and revaccination is likely the best preventive measure. Once an outbreak occurs, vaccination and infection-prevention strategies should be utilized. Antibiotic prophylaxis may be considered for high-risk exposed individuals, but development of antibiotic resistance during outbreaks has been reported. The short period between initial exposure and development of disease indicates that pneumococcal colonization is not a prerequisite for pneumococcal respiratory infection.
Electronic supplementary material
The online version of this article (10.1186/s41479-018-0055-4) contains supplementary material, which is available to authorized users.
Keywords: Streptococcus pneumoniae, Pneumococcus, Outbreaks, Transmission, Epidemic, Cluster, Pneumococcal vaccine
Background
Discovered in 1881 independently by Louis Pasteur and George Sternberg [1], Streptococcus pneumoniae is a Gram-positive bacterial pathogen that may asymptomatically colonize the upper respiratory tract and is capable of causing infections including conjunctivitis, otitis media, lower respiratory tract infections, bacteremia, and meningitis [2]. Those at particularly high risk for invasive disease are young children, older adults, and persons with underlying comorbidities [3, 4]. Among United States (US) adults ≥50 years, it is estimated that S. pneumoniae causes ≥500,000 cases of pneumonia and ≥ 25,000 deaths each year [5]. Previous publications describing pneumococcal disease state that nasopharyngeal colonization is a prerequisite for disease [2, 6, 7]. Colonization is “the presence and multiplication of microorganisms without tissue invasion or damage” [8]. Conversely, infection involves tissue invasion.
The objective of this review was to summarize the publications on outbreaks and inform the understanding of S. pneumoniae transmission in these outbreaks. The most recent review of general pneumococcal outbreaks was conducted in 2010 [9]. Since then, the Advisory Committee on Immunization Practices (ACIP) has revised its recommendations to include the use of 13-valent pneumococcal conjugate vaccine (PCV13) in adults [10]. Our review represents an important update to previous reviews, includes additional pneumococcal disease manifestations, and has over double the number of included articles from the previous review. This review informs the understanding of Streptococcus pneumoniae outbreak serotypes, transmission, and effective control measures.
Methods
A search of PubMed was conducted on July 18, 2017, for publications describing outbreaks of disease caused by S. pneumoniae. The following search terms were used: (“streptococcus pneumoniae” OR “pneumococcus”) AND (“outbreak” OR “epidemic”) with no date restrictions. Articles not available in the English language were excluded. All types of pneumococcal disease, year of outbreak, or location of outbreak were eligible for inclusion. To be considered an outbreak, at least one transmission event of pneumococcal disease had to occur. Pneumococcal carriage or surveillance studies were included if details of a pneumococcal outbreak were described. Each included article’s references and previous reviews [9, 11, 12] were screened for additional articles not identified.
The following information was extracted from publications. Case-patient ages were groups into five categories; toddler (0–2 years old), children (3–17), young adults (18–25), adults (26–49) and older adults (50+). S. pneumoniae were considered antibiotic susceptible or non-susceptible, where non-susceptible refers to intermediate or resistant. Specific antibiotic susceptibility information was extracted for penicillin, cefotaxime, erythromycin, tetracycline, levofloxacin, and vancomycin. The three general control measures considered were antibiotic prophylaxis, prophylactic vaccination, and infection prevention (i.e., hand-hygiene, isolation of cases, isolation of carriers, social distancing). Outbreak settings were categorized as occurring in hospitals, military, long term care facilities (LTCF), daycares, schools, jails, or workplaces. Settings falling outside these categories were grouped as “community” outbreaks. Pneumococcal lower respiratory tract infections were divided into three eras; pre-vaccine (pre-1977), pneumococcal polysaccharide vaccine (PPSV) only (1977–1999), and PPSV and PCV vaccines (2000–2017).
Results
The search identified 629 potential articles. After screening, 83 articles were identified as meeting the inclusion criteria. From references of included articles and other reviews an additional 15 articles were identified. A total of 98 publications detailing 94 unique S. pneumoniae outbreaks were identified (Table 1, Additional file 1: Figure S1). Thirteen reports were published from 1916 to 1946, and the remainder were published after 1980. Unique outbreaks by disease syndrome were as follows; 80 lower respiratory tract infection [12–97], 9 conjunctivitis [98–105], 3 otitis media [106, 107], 1 surgical site infection [108], and 1 lower respiratory tract infection and otitis media [109] (Fig. 1).
Table 1.
Characteristics of included pneumococcal publications
| Author | Year published | Country | Type | Setting | Age Categories | Linkage | Serotype | Number colonized (%) | Number infected (%) | Case-Fatality Ratio |
|---|---|---|---|---|---|---|---|---|---|---|
| McCrae T | 1916 | Canada | Respiratory | Community | ||||||
| Miller JL | 1918 | United States | Respiratory | Military | 346 | 0.325 | ||||
| Schroder MC | 1930 | United States | Respiratory | School | Children | 5 | 150 | |||
| Smillie WG | 1936 | United States | Respiratory | Hospital | 2 | 21 | 17 | 0.471 | ||
| Tilghman RC | 1936 | United States | Respiratory | Community | Toddler, Children, Young Adult, Adult, Older Adult | Variety | ||||
| Gilman BB | 1938 | United States | Multiple | Community | Neufeld | 1 | 35 (7.0%) | 0.114 | ||
| Smillie WG | 1938 | United States | Respiratory | Hospital | 1 | (10.0%) | 110 | |||
| Mackenzie GM | 1940 | United States | Respiratory | Community | Neufeld | 1 | 43 (18.0%) | 4 (1.6%) | ||
| Hodges RG* | 1946 | United States | Respiratory | Military | Neufeld | Variety | 1644 | 0 | ||
| Hodges RG* | 1946 | United States | Respiratory | Military | Neufeld | Variety | 1644 | 0 | ||
| Hodges RG* | 1946 | United States | Respiratory | Military | Neufeld | Variety | 1644 | 0 | ||
| Hodges RG* | 1946 | United States | Respiratory | Military | Neufeld | Variety | 1644 | 0 | ||
| Hodges RG* | 1946 | United States | Respiratory | Military | Neufeld | Variety | 1644 | 0 | ||
| DeMaria A | 1980 | United States | Respiratory | Community | Quelleng | 1 | 10 (10%) | 39 | ||
| Shayegani M | 1982 | United States | Conjunctivis | Community | Nontypeable | 1567 | 0 | |||
| Shayegani M | 1983 | United States | Conjunctivis | Military | Nontypeable | 80 | 0 | |||
| Fenton PA | 1983 | United Kingdom | Respiratory | Community | 1 | |||||
| Shayegani M | 1984 | United States | Conjunctivis | Community | Adult, Older Adult | Nontypeable | 1189 | 0 | ||
| Davies AJ | 1984 | United Kingdom | Respiratory | Hospital | Immunoelectrophoresis | 9 | 4 | |||
| Berk SL | 1985 | United States | Respiratory | Hospital | Older Adult | Quelleng | 8 | 0 (0%) | 4 (18.0%) | 0.500 |
| Collingham KE | 1985 | United States | Respiratory | Community | Older Adult | 12 | 2 | 0.500 | ||
| Mehtar S | 1986 | United Kingdom | Respiratory | Hospital | Toddler | 6 | 3 | 0.333 | ||
| Davies AJ | 1987 | United Kingdom | Respiratory | Hospital | Older Adult | Quelleng | 3 | 8 | 0.250 | |
| Gould FK | 1987 | United Kingdom | Respiratory | Hospital | Older Adult | 23 | 6 | |||
| Moore EP | 1988 | United Kingdom | Respiratory | Hospital | Older Adult | 23 | 4 | 0.250 | ||
| CDC* | 1989 | United States | Respiratory | Jail | Young Adult, Adult | Quelleng | 12F | 11 (7.0%) | 17 (0.5%) | 0.043 |
| Rauch AM | 1990 | United States | Respiratory | Daycare | Toddler | 14 | 10 (9.3%) | 2 (2.4%) | 0 | |
| Bain M | 1990 | United Kingdom | Respiratory | Hospital | Older Adult | Quelleng | 4 | 4 | ||
| Mercat A | 1991 | France | Respiratory | Community | Young Adult, Adult, Older Adult | Quelleng | 1 | 1 (2.0%) | 39 | 0.040 |
| Cartmill TDI | 1992 | United Kingdom | Respiratory | Hospital | Older Adult | 6 | 1 | 4 | 0.250 | |
| Dawson S | 1992 | United Kingdom | Respiratory | Hospital | Older Adult | 6 | 1 | 5 | ||
| PHLS | 1992 | United Kingdom | Respiratory | Hospital | 9 | 7 | 0.143 | |||
| Quick RE | 1993 | United States | Respiratory | Long-term care facility | Older Adult | Quelleng | 9 V | 2 (3.0%) | 7 (7.4%) | 0.710 |
| Gratten M | 1993 | Australia | Respiratory | Community | Young Adult, Adult, Older Adult | Antisera | 1 | 13 (17.3%) | 18 | |
| Denton M | 1993 | United Kingdom | Respiratory | Hospital | Older Adult | 14 | 8 | 0.125 | ||
| Hoge CW* | 1994 | United States | Respiratory | Jail | Young Adult, Adult | Quelleng | 12F | 11 (7.0%) | 46 (0.5%) | 0.043 |
| Cherian T | 1994 | United States | Respiratory | Daycare | Toddler | Ribotyping | 12F | 6 (100%) | 4 (66.7%) | 0 |
| Millar MR | 1994 | United Kingdom | Respiratory | Hospital | Older Adult | 9 | 0 (0%) | 10 (5.7%) | ||
| Mandigers CMPW | 1994 | Netherlands | Respiratory | Hospital | Older Adult | Quelleng | 9 | 18 | 0.556 | |
| Nims L | 1994 | United States | Respiratory | Daycare | Toddler | PCR | 19 | 3 | 14 | 0.500 |
| Raymond J | 1995 | France | Respiratory | Hospital | Toddler | RAPD | 23F | 2 | ||
| Ertugrul N | 1997 | United States | Conjunctivis | Military | PFGE, PCR | Nontypeable | 561 | 0 | ||
| Marton A | 1997 | Hungary | Otitis Media | Hospital | Toddler | 0 | 6 | |||
| Marton A | 1997 | Hungary | Otitis Media | Hospital | Toddler | 3 | ||||
| Gillespie SH | 1997 | United Kingdom | Respiratory | Hospital | Older Adult | RFLP | 9 | 3 | 9 | 0.444 |
| CDC* | 1997 | United States | Respiratory | Long-term care facility | Older Adult | PCR | 14 | 10 (14.9%) | 0.200 | |
| CDC* | 1997 | United States | Respiratory | Long-term care facility | Older Adult | PFGE | 23F | 17 (23.0%) | 11 (13.0%) | 0.270 |
| CDC | 1997 | United States | Respiratory | Long-term care facility | Older Adult | PCR | 4 | 14 (11.7%) | 0.290 | |
| Musher DM | 1997 | United States | Respiratory | Military | Young Adult | 1 | 128 (3.2%) | |||
| Musher DM | 1997 | United States | Respiratory | Military | Young Adult | 7F / 8 | 44 (28.4%) | 14 (6.4%) | ||
| Fiore AE* | 1998 | United States | Respiratory | Long-term care facility | Older Adult | PCR | 14 | 10 (14.9%) | 0.200 | |
| Nuorti JP* | 1998 | United States | Respiratory | Long-term care facility | Older Adult | PFGE | 23F | 17 (23.0%) | 11 (13.0%) | 0.27 |
| Sheppard DC | 1998 | United States | Respiratory | Long-term care facility | Older Adult | PFGE | 14 | 0 (0%) | 15 (12.5%) | |
| Razzaq N | 1998 | United Kingdom | Respiratory | Community | Toddler, Older Adult | 12F | 2 | |||
| Craig AS | 1999 | United States | Respiratory | Daycare | Toddler | PFGE | 14 | 15 (19%) | 3 (3.4%) | 0 |
| de Galan BE | 1999 | Netherlands | Respiratory | Hospital | Older Adult | Quelleng, RFEL | 15 | 36 | 0.297 | |
| Kellner JD | 1999 | Canada | Respiratory | Community | Adult, Older Adult | PFGE | 6 | 0.167 | ||
| Leggiadro RJ | 1999 | United States | Respiratory | Long-term care facility | Older Adult | 4 | 3 | |||
| Gleich S | 2000 | United States | Respiratory | Long-term care facility | Older Adult | PFGE | 4 | 11 (5.5%) | ||
| Dagan R | 2000 | Israel | Respiratory | Community | Ribotyping, PCR | 1 | 31 (4.8%) | 5 | ||
| Nakashima T | 2001 | Japan | Otitis Media | Daycare | Children | Antisera, RAPD | 19, 23, 6 | 7 | ||
| CDC* | 2001 | United States | Respiratory | Long-term care facility | Older Adult | PFGE | 14 | 9 | 0.444 | |
| Weiss K | 2001 | Canada | Respiratory | Hospital | Older Adult | PFGE | 23F | 23 | 0.087 | |
| CDC | 2002 | United States | Conjunctivis | School | Children, Young Adult, Adult | PFGE | Nontypeable | 144 | ||
| Melamed R | 2002 | Israel | Respiratory | Hospital | Toddler | RAPD | 5 | 0 | 3 | |
| Martin M | 2003 | United States | Conjunctivis | Community | Young Adult | PFGE, MLST | Nontypeable | 20 (8.1%) | 698 (13.8%) | |
| Tan CG* | 2003 | United States | Respiratory | Long-term care facility | Older Adult | PFGE | 14 | 9 | 0.444 | |
| Crum NF | 2003 | United States | Respiratory | Military | Young Adult | Quelleng, Latex Agglutination | 9 V / 4 | 13 (11.0%) | 52 (1.5%) | 0 |
| Subramanian D | 2003 | United Kingdom | Respiratory | Hospital | PFGE | 9 V | 3 (5.5%) | 9 | ||
| Sanchez JL | 2003 | United States | Respiratory | Military | Young Adult | PCR | 3, 6, 9, 14, 20, 22, 23 | 30 (13.6%) | 30 (12.1%) | |
| Crum NF | 2004 | United States | Conjunctivis | Military | Young Adult, Adult | MLST | Nontypeable | 15 (9.9%) | 80 (2.3%) | 0 |
| Banerjee A | 2005 | India | Respiratory | Military | RAPD | 0 | ||||
| CDC | 2005 | United States | Respiratory | Hospital | Adult | PFGE | 23F, 3 | 6 (9.0%) | 7 | 0.290 |
| CDC* | 2005 | United States | Respiratory | Community | Toddler, Children, Young Adult, Adult, Older Adult | PFGE, MLST, MLBT | 12F | 46 (2.4%) | 14 (0.1%) | |
| Birtles A | 2005 | United Kingdom | Respiratory | Community | Adult | MLST | 8 | 2 | 1 | |
| Buck JM | 2006 | United States | Conjunctivis | Community | Toddler, Children, Young Adult, Adult, Older Adult | PFGE, MLST | Nontypeable | 735 | 0 | |
| Hennick M | 2006 | Canada | Conjunctivis | Community | Toddler, Children, Young Adult, Adult, Older Adult | AFLP | Nontypeable | 47 | ||
| Hansmann Y | 2006 | France | Respiratory | Long-term care facility | Older Adult | Antisera, Urine | 4 | 1 (1.2%) | 11 (11.7%) | 0.273 |
| Singh PMP | 2006 | India | Respiratory | Military | Young Adult | 316 | 0 | |||
| Cashman P | 2007 | Australia | Respiratory | School | Children | 1 | 25 | |||
| Sheppard CL | 2008 | United Kingdom | Respiratory | Community | Children, Young Adult, Adult | PCR, MLST | 1 | 11 | 0.182 | |
| Romney MG | 2008 | Canada | Respiratory | Community | Toddler, Children, Young Adult, Adult, Older Adult | Latex Agglutination | 5 | 137 | 0.080 | |
| Zegans ME | 2009 | United States | Conjunctivis | Community | Young Adult | PFGE, MLST | Nontypeable | 20 (8.1%) | 698 (13.8%) | |
| Vainio A | 2009 | Finland | Respiratory | Military | MLST | 7F | 9 (20.9%) | 5 (12.0%) | 0 | |
| Gupta A | 2009 | United Kingdom | Respiratory | School | Children | ELISA, Urine | 1 | 1 (1.2%) | 5 | |
| Mehiri-Zghal E | 2010 | Tunisia | Respiratory | Jail | PFGE | 1 | 9 (45.0%) | 150 (3.8%) | ||
| Balicer RD | 2010 | Israel | Respiratory | Military | Young Adult | PFGE, MLST | 5 | 35 (24.1%) | 34 | 0 |
| Pichon B | 2010 | United Kingdom | Respiratory | Community | MLST | 5 | 8 | |||
| Dawood FS | 2011 | United States | Respiratory | Military | Young Adult | Quelleng | 7F | 16 (4.3%) | 74 (0.3%) | 0.027 |
| Vanderkooi OG | 2011 | Canada | Respiratory | Community | Children, Young Adult, Adult, Older Adult | Quelleng, MLST | 5, 8 | 207 | ||
| Skoczynska A | 2012 | Poland | Respiratory | Hospital | Older Adult | PFGE, MLST | 14 | 6 | ||
| Fleming-Dutra K | 2012 | United States | Respiratory | Hospital | Children, Young Adult | PCR, MLST | 15A | 6 | 11 | |
| Guillet M | 2012 | France | Surgical Site | Hospital | 3 | 1 | 4 | |||
| Zulz T* | 2013 | United States | Respiratory | Community | Toddler, Children, Young Adult, Adult, Older Adult | PFGE, MLST, MLBT | 12F | 46 (2.4%) | 14 (0.1%) | |
| CDC | 2013 | United States | Respiratory | Long-term care facility | Adult, Older Adult | 3 | 7 (50.0%) | 0.430 | ||
| Kuroki T | 2014 | Japan | Respiratory | Hospital | Older Adult | PFGE, MLST | 3 | 16 (83.9%) | 0.063 | |
| Ben-David D | 2014 | Israel | Respiratory | Hospital | Young Adult, Older Adult | PFGE, MLST | 19F, 23F | 21 (20.2%) | 66 | |
| Schillberg E | 2014 | Canada | Respiratory | Community | Children, Young Adult, Adult, Older Adult | Quelleng, PFGE, MLST, MLVA | 12F | 32 | ||
| Suryam V | 2015 | India | Respiratory | Military | 52 | 0 | ||||
| Thomas HL | 2015 | United Kingdom | Respiratory | Long-term care facility | Older Adult | Urinary, MLST | 8 | 15 (65.0%) | 0.133 | |
| Kunwar R | 2015 | India | Respiratory | Military | Young Adult | 58 (1.1%) | 0 | |||
| Sheppard CL | 2016 | United Kingdom | Respiratory | Hospital | Older Adult | Urinary | 6C | 13 | 0.231 | |
| Ewing J | 2017 | United Kingdom | Respiratory | Workplace | Young Adult, Adult, Older Adult | WGS, MLST | 4 | 25 | 0 | |
| Jauneikaite E | 2017 | United Kingdom | Respiratory | Hospital | Older Adult | WGS, MLST | 9 V | 4 |
PCR polymerase chain reaction, RAPD random amplified polymorphic DNA, PFGE pulse-field gel electrophoresis, RFLP restriction fragment length polymorphism, RFEL restriction fragment end labeling, MLST multilocus sequence type, AFLP amplified fragment length polymorphism, ELISA enzyme-linked immunosorbent assay, MLBT multilocus boxB sequence typing, MLVA multiple loci variable-number tandem repeat analysis, WGS whole genome sequencing
Age categories are defined as follows; toddler (0–2 years old), children (3–17), young adult (18–25), adult (26–49), and older adult (50+)
Settings falling outside the other indicated categories were considered as “Community” settings. These included transmission among families, homeless shelter outbreaks, outbreaks in socially disadvantaged groups, and transmission occurring generally within geographical regions
*Outbreaks that were described in multiple publications. See supplement data set containing unique identifiers for each outbreak report
Fig. 1.
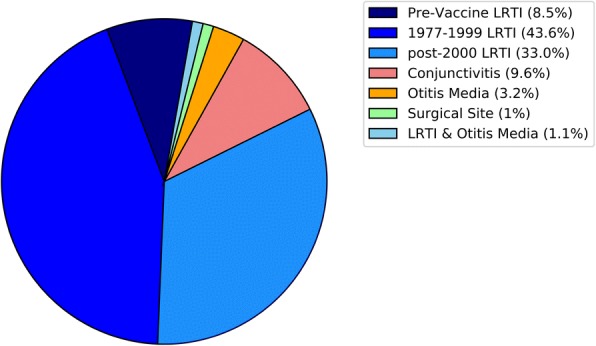
Reported Streptococcus pneumoniae outbreaks by anatomical site. LRTI: Lower respiratory tract infection. LRTI was divided into three eras; pre-vaccine (pre-1977), pneumococcal polysaccharide vaccine only (1977–1999), and pneumococcal polysaccharide and conjugate vaccines (2000–2017)
A majority of reported outbreaks occurred in hospitals (33.0%), community (26.6%), or military buildings (17.0%) (Fig. 2). The most common age categories for case-patients in outbreaks (n = 73) were older adults (60.3%), young adults (34.2%) and adults (28.8%). Case-patients were less commonly toddlers (20.5%) or children (19.2%). Most reported outbreaks were reported in the US (43.6%), the United Kingdom (24.5%), or Canada (7.4%). France, India, and Israel each reported four outbreaks (4.3%); Japan, Australia, Netherlands, and Hungary each reported two outbreaks (2.1%); and Tunisia, Poland, and Finland each reported one outbreak (1.1%).
Fig. 2.
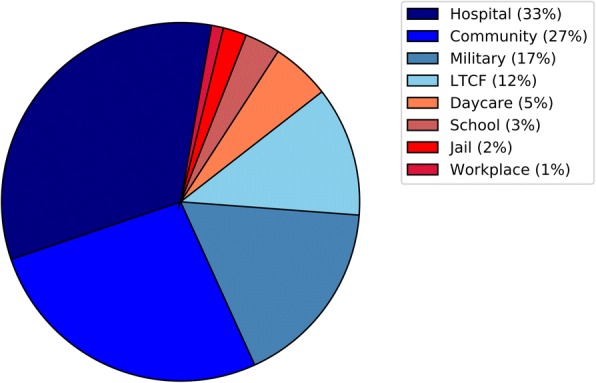
Streptococcus pneumoniae outbreaks by setting. LTCF: Long-term care facility. Graphic includes outbreaks from all anatomical sites (94 outbreaks)
Sixty-one outbreak investigations reported assessing S. pneumoniae strains by molecular typing. The most common methods used were pulse-field-gel-electrophoresis (PFGE) (23.2%), antisera methods (23.2%), and multi-locus-sequence-typing (MLST) (22.0%). Of outbreak reports published since 2007 (n = 18), MLST (40.6%) and PFGE (18.8%) were most commonly used. Of 52 outbreaks assessing antibiotic resistance, 73.1% of outbreaks reported some antibiotic non-susceptibility. Antibiotics chosen for susceptibility testing were inconsistent. Non-susceptibility to penicillin (28/50 outbreaks), erythromycin (20/38), and tetracycline (11/20) were reported. Fewer outbreaks reported non-susceptibility to cefotaxime (5/13) or levofloxacin (3/11). Non-susceptibility to vancomycin was not reported for any outbreak (n = 17).
Disease types
Lower respiratory tract infection
A total of 81 unique reported outbreaks involved lower respiratory tract infection with pneumococcus, with 9 in the pre-vaccine era, 41 in the PPSV era and 31 in the PPSV/PCV era.
Pre-vaccine era
Within the pre-vaccine era, outbreaks occurred in community (4/9), military (2/9), hospital (2/9), and a school (1/9) settings. Interestingly, 3 of the outbreak reports mentioned concocting a vaccine from pneumococcal polysaccharides [16, 18, 20].
PPSV era
During the PPSV era, reported outbreaks occurred in hospitals (43.9%), community (19.5%), LTCF (17.1%), daycares (9.8%), military (7.3%) or jail (2.4%) settings. Within hospital settings, outbreaks occurred in geriatric, pulmonary, oncology, maternity, and “AIDS-care” units. Community outbreaks included homeless shelter outbreaks, transmission between family members, and outbreaks occurring within socially disadvantaged groups. Of the 39 outbreaks that reported serotypes, the most common pneumococci were serogroup 9 (15.4%), serotype 1 (15.4%), serotype 23F (12.8%), and serotype 14 (12.8%) (Fig. 3). Of the 17 studies that reported colonization data, the median percent of colonized individuals was 9.3% (IQR: 3.0%, 19.0%). For 15 studies with a denominator, the median attack rate was 7.4% (IQR: 4.4%, 12.8%) with a median case-fatality ratio of 25.0% (IQR: 11.5%, 36.1%) from 24 studies. Twenty-six studies reported conducting testing for resistance to at least one antibiotic. Non-susceptibility was reported for the following antibiotics; penicillin (18/25), cefotaxime (5/9), erythromycin (9/19), tetracycline (8/11), levofloxacin (2/3), and other antibiotics (13/17). No vancomycin non-susceptibility was reported in 13 publications. Seven outbreaks reported sufficient information to calculate the vaccination coverage of the source population with the following coverages; 2% [110], 3% [55], two with 4% [52, 110], 7% [42], and 24% [70]. One study reported an unadjusted vaccine effectiveness (VE) of 0.87 (95% CI: -0.03, 0.98) for those who received PPSV before the outbreak [70]. For hospital outbreaks with reported control measures (11/18), infection-prevention practices alone (54.5%), vaccination alone (9.1%), infection-prevention and vaccination (18.2%), infection-prevention and prophylactic antibiotics (9.1%), and all three (9.1%) were used to mitigate outbreaks. Only two outbreaks (infection control alone [64], all three control measures [70]) reported control measures as unsuccessful. Both outbreaks described the development of antibiotic resistance over the course of the outbreak [64, 70]. LTCF reported infection-prevention and vaccination (2), infection-prevention and antibiotics (1), and all three (1) as control measures with cases discontinuing after implementation. Two of three daycares that used antibiotics alone reported failure of control measures to eradicate carriage of the outbreak strain. For outbreaks designated as within communities, a homeless men’s shelter controlled an outbreak successfully using vaccination. None of the other community outbreaks reported using control measures.
Fig. 3.
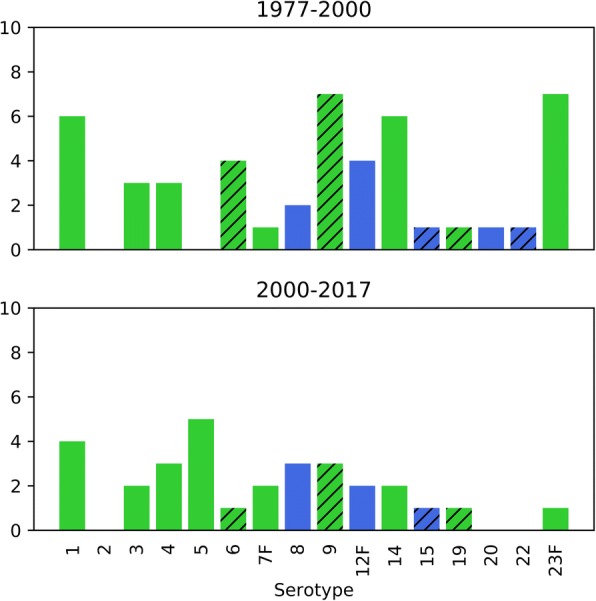
Pneumococcal lower respiratory tract infection outbreak serotypes and coverage by pneumococcal vaccines. Green: both the 13-valent pneumococcal conjugate vaccine (PCV13) and 23-valent pneumococcal polysaccharide vaccine (PPSV23) cover the indicated serotype. Blue: only PPSV23 covers the indicated serotype. Hatched bars indicate serogroups that have subtypes covered by the vaccines, but the specific serotype within the serogroup was not consistently reported across publications. The graph is subdivided by vaccine era; PPSV only (1977–1999) and PPSV/PCV (2000–2017)
PPSV/PCV era
From 2000 to 2017, outbreaks were reported in hospitals (25.8%), military settings (25.8%), communities (22.6%), LTCF (12.9%), schools (6.5%), a workplace (3.2%), and a jail (3.2%). Hospital outbreaks occurred in geriatric, pulmonary, ear/nose/throat, and a pediatric psychiatry ward. Community outbreaks included a homeless shelter outbreak, transmission among children, and a socially disadvantaged group. Of outbreaks with recorded case-patient ages (n = 29), 55.2% were older adults, 48.3% were young adults, 37.9% were adults, 27.6% were children, and 10.3% were toddlers. Twenty-seven outbreaks reported serotypes, with serotype 5 (18.5%) and serotype 1 (14.8%) most commonly reported (Fig. 3). Of 10 outbreaks with a denominator for colonization, the median colonization percentage was 8.2% (IQR: 2.9%, 20.7%). The median attack rate was 7.7% (IQR: 1.2%, 40.5%) for the ten outbreaks that provided attack rates. The case-fatality ratio was 4.5% (IQR: 0%, 21.9%) for 18 reports. Seventeen studies reported testing for antibiotic resistance with 64.7% reporting resistance to at least one antibiotic. Reported antibiotic non-susceptibility included; penicillin (5/16), erythromycin (5/11), tetracycline (2/5), levofloxacin (1/4), and other antibiotics (5/9). No non-susceptibility was reported for cefotaxime (n = 3) and vancomycin (n = 2). Twelve studies assessed whether case-patients had ever received either pneumococcal vaccine before the outbreak [62, 66, 67, 71, 73, 74, 82, 88, 89, 91, 93, 97]. Of the studies that provided enough information to calculate vaccination coverage of the source population of cases, two reported 0% coverage [66, 88], one reported 7% [89], and one reported 57% [93]. At least one vaccine failure was reported for 6 studies [71, 74, 88, 91, 93, 97]. Two reports described one case-patient vaccine failure of a vaccine received within five years of the outbreak [71, 74]. Two studies reported PPSV VE among older adults; 1.00 (95% CI: 0.30, 1.00) [63] and − 0.41 (95% CI: -2.33, 0.40) [93]. The poor VE and the outbreak occurring despite 57% vaccination coverage was partially attributed to “waning immunity” by the authors, since all case-patients received the vaccine more than 7 years prior to the outbreak [93]. Of hospital outbreaks with reported control measures (6/8), the following measures were used; infection-prevention alone (16.7%), vaccination alone (16.7%), infection-prevention and prophylactic antibiotics (50.0%), and vaccination and prophylactic antibiotics (16.7%). None of the six outbreaks reported the control measures failing to control the outbreak. Military outbreaks were effectively controlled by antibiotics alone (1), infection control alone (1), antibiotics and vaccination (3), infection-prevention and antibiotics (3) or all three (1). All five LTCF outbreaks were controlled with vaccination paired with infection control (2), antibiotics (2), or both (1). Community outbreaks reporting control measures (5/7), all used vaccination alone. All outbreaks except one were reported as being successfully controlled.
Conjunctivitis
Eight publications describing nine conjunctivitis outbreaks have been published since 1982. All of these outbreaks are attributed to non-typeable strains. Two pneumococcal outbreaks were MLST sequence type 448 [101, 104]. Interestingly, this pneumococcal strain, identified in the 2002 Dartmouth and 2003 Minnesota outbreaks, was related to a strain isolated in 1980’s outbreaks in New York, California, and Illinois [98, 99, 101, 104]. Noteworthy is the development of non-susceptibility to penicillin, erythromycin, and tetracycline between 1980 to 2003 in this strain. Four of six outbreaks reported non-susceptibility to at least one antibiotic [98, 100, 103, 104]. Non-susceptibility was observed for erythromycin (4/6), penicillin (2/6) and tetracycline (1/4). Outbreaks occurred in the community (N = 6) or military settings (N = 3). Three of the community outbreaks were associated with universities, with two large outbreaks occurring in this setting. Furthermore, all outbreaks with reported ages (n = 5) included young adult case-patients. Outbreaks of conjunctivitis were generally larger than respiratory outbreaks (median: 561 cases; range 80, 735). There was no reported mortality associated with these outbreaks. Five outbreaks reported using infection-prevention to control outbreaks and led to a subsequent decline in cases [100, 101, 103–105]. However, for three of the four outbreaks related to schools, the decline occurred after school breaks [100, 101, 105], complicating the attribution of infection-prevention strategies as ending the outbreak.
Otitis media
There were four reported otitis media outbreaks in three publications. The first was an otitis media outbreak occurring simultaneously with a pneumococcal lower respiratory tract infection outbreak in a US community in 1937 [109]. This study was unable to directly link the two manifestations of pneumococcal disease. Two outbreaks occurred in hospitals in Hungary during 1993–1994 and 1996 [106]. No carriers were reported among healthcare personnel and transmission was believed to occur between patients in the hospital since case-patients shared rooms. The other outbreak occurred in 1997 in a Japanese daycare center among seven children with serogroup 6 (n = 1), and serotypes 19 (n = 4), and 23F (n = 2) [107]. Otitis media occurred in at least one case-patient during two pneumococcal lower respiratory tract infection outbreaks [48, 61]. Non-susceptibility was reported for penicillin (3/3) and erythromycin (2/2). None of the publications reported instituting control measures.
Surgical-site
One publication detailed four surgical site infections transmitted by a surgeon with nasopharyngeal carriage to four prostatic surgery patients [108]. Pneumococcal infection occurred at skin and soft tissue near the surgical site of case-patients. Transmission was attributed to the surgeon persistently wearing a poorly fitting mask.
Transmission
In the reviewed outbreak articles, we found evidence for multiple modes of transmission. Aside from transmission attributable to nasopharyngeal carriers, there were pneumococcal lower respiratory tract infection outbreaks suggestive of device-associated transmission (infant resuscitation device [30]; inhaler [50, 97]), and infection transmission without any carriers detected [27, 28, 33, 39, 46, 65, 97]. While it is near impossible to ever fully rule out transient nasopharyngeal colonization as the source, these outbreaks found no evidence that carriers contributed to transmission. There is also evidence that droplet transmission occurs for S. pneumoniae. In a neonatal intensive care unit, transmission occurred between two neonates 2 meters apart who had no overlapping nursing staff, no contact between families, no carriage among family member, and infection of the transmitting neonate occurred before admission [65]. Studies also reported co-circulation of other viral [51, 76, 87, 91, 95] or bacterial respiratory tract pathogens [44, 59, 84, 87] preceding or during a pneumococcal outbreak. For conjunctivitis outbreaks, direct droplet, or indirect (i.e. environment or hand contamination) transmission may also have occurred, because having a roommate with conjunctivitis was associated with developing conjunctivitis [101]. In four outbreaks, time from exposure to infection in several outbreaks was less 72 hours for at least one case-patient [27, 28, 65, 97]. Serotype 1, 5, and 9 V exhibited short times between exposure and disease.
Discussion
In our review, we found multiple outbreaks attributable to S. pneumoniae reported in the first half of the 1900s. In the beginning of the antibiotic area, there were no publications regarding pneumococcal outbreaks. One explanation for this observation is that outbreaks went unreported or unrecognized due to widespread antibiotic use while antibiotics were exquisitely effective. After the 1980’s, outbreaks began being reported regularly, with most reporting non-susceptibility to at least one antibiotic. A majority of pneumococcal outbreaks are linked to lower respiratory tract infection but several large conjunctivitis outbreaks due to non-typeable strains have recently occurred. Most reported lower respiratory tract infection outbreaks have occurred in hospitals, perhaps due to observation bias. Conjunctivitis outbreaks have mostly occurred in community settings, specifically universities. Regarding transmission, this review supported the view of S. pneumoniae transmission as a complicated process occurring by multiple modes (Fig. 4), and droplet precautions may be warranted for symptomatic patients due to the evidence of droplet transmission occurring [65]. Recommendation for droplet precautions is in line with American Public Health Association for patients with antibiotic-resistant pneumococcus [111], but differs from US Centers for Disease Control and Prevention’s (CDC) and Red Book’s recommendation of standard precautions for pneumococcus cases [112, 113]. For infection progression in individuals, we reviewed several studies that development of pneumococcal disease occurred with 72 h of initial exposure to S. pneumoniae [27, 28, 65, 97]. Such a short time between exposure and infection suggests that colonization is not a prerequisite for pneumococcal disease, and infection can progress directly from initial exposure. Based on these observations, we propose a new conceptual model for pneumococcal lower respiratory tract infection progression within an individual (Fig. 5). After initial exposure, an individual may develop infection directly or become colonized. A colonized individual can either develop disease or develop immunity to the pneumococcal serotype. After this point, pneumococcal respiratory infection progresses as has been described previously [2].
Fig. 4.

Modes of person-to-person transmission of Streptococcus pneumoniae
Fig. 5.
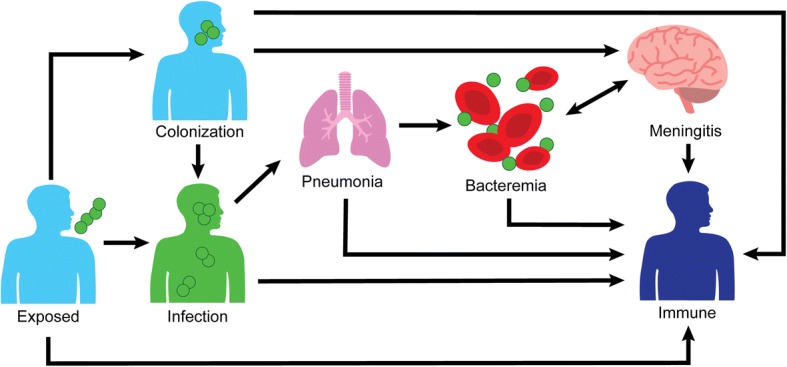
Simplified description of serious Streptococcus pneumoniae infections, with a focus on initial respiratory tract disease. Death, not represented in the figure, can occur at any illness stage with varying survival probability based on disease stage
Of the serotypes reported in pneumococcal lower respiratory tract infection outbreaks, the reported strains are considered high risk for serious disease manifestation [114]. Specifically, increased empyema/parapneumonic effusion (serotype 1), meningitis (serotypes 12, 23F), and fatality (serotypes 14, 23F). These strains have continued to be reported in the PPSV/PCV era. Outbreak strains in lower respiratory tract infection outbreaks are included within PCV13 but are covered more fully by PPSV23 (Fig. 3) [115]. Along with the observation that most outbreaks occurred where vaccination/revaccination rates were low suggests that effective vaccination programs play a key role in preventing outbreaks. Providing vaccination is particularly vital in highly susceptible populations, like individuals in LTCF. Primary adult pneumococcal vaccination is recommended for healthy adults 65 years or older, immunocompromised individuals, and those with certain chronic diseases [115, 116]. Providing a 5-year PPSV23 revaccination, if indicated per US CDC recommendations, should be considered to retain sufficient immunity [117–121]. In regards to conjunctivitis, vaccination likely has no role in prevention since these strains do not express capsules, the antigenic target of the current vaccines.
The nasopharyngeal carrier state is an important feature in transmission of S. pneumoniae strains both within households and across regions. There is recognition that carrier-attributed transmission is important among families, with children acting as a reservoir [122–125]. In a global view, large events offer opportunities for widespread dissemination of S. pneumoniae strains. Events like the Hajj, the annual Islamic pilgrimage to Mecca, can lead to acquisition of new S. pneumoniae strains in attendees [126]. While the colonization has been important in dissemination of S. pneumoniae, in outbreaks we found evidence of additional transmission from other sources. Furthermore, there is a need to explore the transmission dynamics of S. pneumoniae with other respiratory pathogens, and the role of the time-order of co-infections [127]. Pneumococcal infection severity has been observed to increase with influenza in murine models [128], and influenza and other respiratory viruses have been associated with increased pneumococcal colonization and infection [129, 130]. In outbreak settings, interventions targeted at preventing or treating co-infections has potential to interrupt transmission. The CDC provided an interim recommendation for the use of PPSV23 as an adjunctive intervention during the 2009 influenza pandemic [131]. Data supports the use of pneumococcal vaccine in future influenza pandemics [132]. Additionally, annual influenza vaccination has potential to mitigate pneumococcal risk [133]. However, interventions targeted specifically for pneumococcus are still required to prevent pneumococcal outbreaks, as evidenced by a pneumococcal outbreak occurring in a military barrack with comprehensive influenza vaccination coverage [82].
Compared to the US CDC’s Active Bacterial Core Surveillance 2015 report for S. pneumoniae [134], reported outbreaks are much more likely to involve non-susceptible pneumococcal strains. The difference is likely related to publication bias favoring non-susceptible outbreak strains. Multitudes of pneumococcal disease outbreaks probably occur but are undetected due to inadequate diagnostic methods or effective antibiotic treatments, and we likely only see a fraction of the full burden of pneumococcal disease. If antibiotic resistance increases in the future, recognized pneumococcal outbreaks may occur with increasing frequency. However, childhood pneumococcal vaccination programs have been associated with a decrease in antibiotic resistance for vaccine serotypes in both children and adults [135], and may provide a way to reduce antibiotic resistance.
In future pneumococcal outbreaks, efforts should be made to rapidly identify cases and carriers to isolate them. For case linkage, we recommend using molecular typing methods, such as whole-genome sequencing (WGS), PFGE, or MLST, rather than serotyping alone. WGS is preferred over PFGE/MLST, but when not possible PFGE/MLST should be used. Recent outbreak investigations have been moving in this direction. When an outbreak is recognized, prompt vaccination or revaccination is important, but due to the delay until immunity occurs, infection-prevention measures are imperative. There is evidence that S. pneumoniae may be transmitted via droplets, so appropriate infection prevention measures should be taken (i.e. droplet precautions). While use of prophylactic antibiotics have had success in controlling outbreaks, the risk of antibiotic resistance developing should be considered carefully. Antibiotic non-susceptibility has previously developed secondary to antibiotic prophylaxis [70]. Rather, it may be appropriate to limit antibiotic prophylaxis to exposed contacts who are at high-risk of disease. Use of prophylactic antibiotics should be evaluated in light of the outbreak size, the pace of new cases, existing antibiotic resistances, and other contextual features. In conjunctivitis outbreaks, prevention efforts should focus on infection-prevention, since vaccination confers no protection against this disease manifestation.
The major strength of our review involves fewer restrictions on inclusion, allowing a more expansive assessment compared to prior pneumococcal outbreak reviews. We updated prior reviews with more recently published outbreaks. Our review also explored features of transmission and infection dynamics in S. pneumoniae, which has not previously been commented on in prior outbreak reviews. Lastly, since we could not report every possible combination of variables that may be of interest to readers, we have provided a data file containing all of the information extracted from the articles (Additional file 2: Table S1).
There are several limitations to our review. While our search terms were general, it is possible that our review missed articles of interest. We attempted to minimize this by searching through the references of included articles and other review articles. Some of these further identified articles were in journals not indexed by PubMed and would not have been identified regardless of search terms. One article not identified by our search reported a serotype 5 outbreak among unaccompanied minors in the US during 2014 [136]. Our conclusions are consistent with the unidentified article and this article provides further evidence for co-infection transmission. Our search was limited to only including articles available in English, but only 8 non-English were identified as eligible via abstracts. Lastly, our review is limited to published outbreaks. However, our conclusions regarding transmission and infection progression remain valid, because only one example is needed to show this can occur.
Conclusion
S. pneumoniae causes outbreaks of various clinical manifestations. There is sufficient evidence that S. pneumoniae colonization is not an obligate prerequisite for disease. To prevent the initial occurrence of outbreaks, maintaining high vaccination rates and revaccination per US CDC/ACIP recommendations is likely to be effective. Once an outbreak occurs, efforts should be directed to infection-prevention strategies, like droplet precautions, and vaccination. The usage of prophylactic antibiotics for exposed individuals may lead to development of antibiotic resistance, and is not currently recommended by the CDC. In scenarios of pneumococcal infection co-circulating with another pathogen, interventions targeted at the co-circulating infections may mitigate pneumococcal transmission. Interestingly, conjunctival pneumococcal outbreaks have been linked to bacteria that do not express a capsule and would therefore not be covered by the currently-licensed pneumococcal vaccines. Despite being discovered over 100 years ago, there is still much to uncover regarding S. pneumoniae.
Additional files
Figure S1. Article exclusion flow diagram. (PNG 22 kb)
Table S1. Data extracted from reviewed articles. (XLSX 28 kb)
Acknowledgments
Funding
PNZ is supported by National Institute of Child Health and Human Development T32-HD091058. No funding support was provided for this article.
Availability of data and materials
The data extracted from publications and analyzed for the systematic review are available in the supplement of this article and is available upon request from the corresponding author.
Author’s contributions
Literature search: PNZ, JDG. Article review: PNZ. Data extraction: PNZ. Drafting of Manuscript: PNZ, JDG, SIB-D, DJW. All authors performed a critical review of the manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
JDG is an employee of Merck & Co., Inc. SIB-D received investigator-initiated research funding and served as a consultant for Pfizer. DJW consults for Merck & Co., Inc. and Pfizer Inc., and received payment as part of Merck’s Speaker’s Bureau.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Watson DA, Musher DM, Jacobson JW, Verhoef J. A brief history of the pneumococcus in biomedical research: a panoply of scientific discovery. Clin Infect Dis. 1993;17:913–924. doi: 10.1093/clinids/17.5.913. [DOI] [PubMed] [Google Scholar]
- 2.Henriques-Normark B., Tuomanen E. I. The Pneumococcus: Epidemiology, Microbiology, and Pathogenesis. Cold Spring Harbor Perspectives in Medicine. 2013;3(7):a010215–a010215. doi: 10.1101/cshperspect.a010215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ortqvist A, Hedlund J, Kalin M. Streptococcus pneumoniae: epidemiology, risk factors, and clinical features. Semin Respir Crit Care Med. 2005;26:563–574. doi: 10.1055/s-2005-925523. [DOI] [PubMed] [Google Scholar]
- 4.Torres A, Blasi F, Dartois N, Akova M. Which individuals are at increased risk of pneumococcal disease and why? Impact of COPD, asthma, smoking, diabetes, and/or chronic heart disease on community-acquired pneumonia and invasive pneumococcal disease. Thorax. 2015;70:984–989. doi: 10.1136/thoraxjnl-2015-206780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weycker D, Strutton D, Edelsberg J, Sato R, Jackson LA. Clinical and economic burden of pneumococcal disease in older US adults. Vaccine. 2010;28:4955–4960. doi: 10.1016/j.vaccine.2010.05.030. [DOI] [PubMed] [Google Scholar]
- 6.Tan TQ. Pediatric invasive pneumococcal disease in the United States in the era of pneumococcal conjugate vaccines. Clin Microbiol Rev. 2012;25:409–419. doi: 10.1128/CMR.00018-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Simell B, Auranen K, Kayhty H, Goldblatt D, Dagan R, O'Brien KL. The fundamental link between pneumococcal carriage and disease. Expert Rev Vaccines. 2012;11:841–855. doi: 10.1586/erv.12.53. [DOI] [PubMed] [Google Scholar]
- 8.Mosby's. Mosby's medical dictionary. 7th edn. St. Louis: Elsevier; 2006.
- 9.Ihekweazu C, Basarab M, Wilson D, Oliver I, Dance D, George R, Pebody R. Outbreaks of serious pneumococcal disease in closed settings in the post-antibiotic era: a systematic review. J Inf Secur. 2010;61:21–27. doi: 10.1016/j.jinf.2010.03.032. [DOI] [PubMed] [Google Scholar]
- 10.Nuorti JP, Whitney CG. Prevention of pneumococcal disease among infants and children - use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine - recommendations of the advisory committee on immunization practices (ACIP) MMWR Recomm Rep. 2010;59:1–18. [PubMed] [Google Scholar]
- 11.Basarab M, Ihekweazu C, George R, Pebody R. Effective management in clusters of pneumococcal disease: a systematic review. Lancet Infect Dis. 2011;11:119–130. doi: 10.1016/S1473-3099(10)70281-4. [DOI] [PubMed] [Google Scholar]
- 12.Gleich S, Morad Y, Echague R, Miller JR, Kornblum J, Sampson JS, Butler JC. Streptococcus pneumoniae serotype 4 outbreak in a home for the aged: report and review of recent outbreaks. Infect Control Hosp Epidemiol. 2000;21:711–717. doi: 10.1086/501717. [DOI] [PubMed] [Google Scholar]
- 13.McCrae T. An epidemic of pneumococcus infection. Can Med Assoc J. 1916;6:769–774. [PMC free article] [PubMed] [Google Scholar]
- 14.Miller JL, Lusk FB. Epidemic of streptococcus pneumonia and empyema at camp dodge, Iowa. J Am Med Assoc. 1918;71:702–704. doi: 10.1001/jama.1918.02600350006003. [DOI] [Google Scholar]
- 15.Schroder MC, Cooper G. An epidemic of colds, bronchitis and pneumonia due to type V pneumococci. J Infect Dis. 1930;46:384–392. doi: 10.1093/infdis/46.5.385. [DOI] [Google Scholar]
- 16.Smillie WG. A study of an outbreak of type ii pneumococcus pneumonia in the VETERANS' administration hospital at BEDFORD, MASSACHUSETTS1. Am J Epidemiol. 1936;24:522–535. doi: 10.1093/oxfordjournals.aje.a118281. [DOI] [Google Scholar]
- 17.Tilghman RC, Finland M. PNEUMOCOCCIC infections in families. J Clin Investig. 1936;15:493–499. doi: 10.1172/JCI100799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smillie WG, Warnock GH, White HJ. A study of a type I pneumococcus epidemic at the state Hospital at Worcester, mass. Am J Public Health Nations Health. 1938;28:293–302. doi: 10.2105/AJPH.28.3.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mackenzie G, McKee T, Tepperman J. Epidemiology of an outbreak of pneumococcal pneumonia in a rural community. Trans Assoc Am Phys. 1940;55:199–208. [Google Scholar]
- 20.Hodges RG, Macleod CM. EPIDEMIC PNEUMOCOCCAL PNEUMONIAI. Description of the EPIDEMIC12. Am J Epidemiol. 1946;44:183–192. doi: 10.1093/oxfordjournals.aje.a119088. [DOI] [PubMed] [Google Scholar]
- 21.Hodges RG, Mac LC. Epidemic pneumococcal pneumonia; the influence of population characteristics and environment. Am J Hyg. 1946;44:193–206. [PubMed] [Google Scholar]
- 22.Hodges RG, Macleod CM, Bernhard WG. EPIDEMIC PNEUMOCOCCAL PNEUMONIAIII. Pneumococcal carrier STUDIES12. Am J Epidemiol. 1946;44:207–230. doi: 10.1093/oxfordjournals.aje.a119090. [DOI] [PubMed] [Google Scholar]
- 23.Hodges RG, Macleod CM. EPIDEMIC PNEUMOCOCCAL PNEUMONIAIV. The relationship of nonbacterial respiratory disease to pneumococcal PNEUMONIA12. Am J Epidemiol. 1946;44:231–236. doi: 10.1093/oxfordjournals.aje.a119091. [DOI] [PubMed] [Google Scholar]
- 24.Hodges RG, Mac LC. Epidemic pneumococcal pneumonia; final consideration of the factors underlying the epidemic. Am J Hyg. 1946;44:237–243. doi: 10.1017/S0022172400013450. [DOI] [PubMed] [Google Scholar]
- 25.DeMaria A, Jr, Browne K, Berk SL, Sherwood EJ, McCabe WR. An outbreak of type 1 pneumococcal pneumonia in a men's shelter. Jama. 1980;244:1446–1449. doi: 10.1001/jama.1980.03310130024022. [DOI] [PubMed] [Google Scholar]
- 26.Fenton PA, Spencer RC, Savill JS, Grover S. Pneumococcal bacteraemia in mother and son. Br Med J (Clin Res Ed) 1983;287:529–530. doi: 10.1136/bmj.287.6391.529-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Davies A J, Hawkey P M, Simpson R A, O'Connor K M. Pneumococcal cross infection in hospital. BMJ. 1984;288(6425):1195–1195. doi: 10.1136/bmj.288.6425.1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Berk SL, Gage KA, Holtsclaw-Berk SA, Smith JK. Type 8 pneumococcal pneumonia: an outbreak on an oncology ward. South Med J. 1985;78:159–161. doi: 10.1097/00007611-198502000-00010. [DOI] [PubMed] [Google Scholar]
- 29.Collingham KE, Littlejohns PD, Anfilogoff N, Wiggins J. Pneumococcal meningitis in a husband and wife. J Infect. 1985;10:256–258. doi: 10.1016/S0163-4453(85)92663-5. [DOI] [PubMed] [Google Scholar]
- 30.Mehtar S, Drabu YJ, Vijeratnam S, Mayet F. Cross infection with Streptococcus pneumoniae through a resuscitaire. Br Med J (Clin Res Ed) 1986;292:25–26. doi: 10.1136/bmj.292.6512.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Davies AJ, Lockley MR. A prospective survey of hospital cross-infection with Streptococcus pneumoniae. J Hosp Infect. 1987;9:162–168. doi: 10.1016/0195-6701(87)90055-7. [DOI] [PubMed] [Google Scholar]
- 32.Gould FK, Magee JG, Ingham HR. A hospital outbreak of antibiotic-resistant Streptococcus pneumoniae. J Inf Secur. 1987;15:77–79. doi: 10.1016/s0163-4453(87)91576-3. [DOI] [PubMed] [Google Scholar]
- 33.Moore EP, Williams EW. Hospital transmission of multiply antibiotic-resistant Streptococcus pneumoniae. J Infect. 1988;16:199–200. doi: 10.1016/S0163-4453(88)94147-3. [DOI] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention. Outbreak of invasive pneumococcal disease in a jail--Texas, 1989. MMWR Morb Mortal Wkly Rep. 1989;38:733–734. [PubMed]
- 35.Hoge CW, Reichler MR, Dominguez EA, Bremer JC, Mastro TD, Hendricks KA, Musher DM, Elliott JA, Facklam RR, Breiman RF. An epidemic of pneumococcal disease in an overcrowded, inadequately ventilated jail. N Engl J Med. 1994;331:643–648. doi: 10.1056/NEJM199409083311004. [DOI] [PubMed] [Google Scholar]
- 36.Rauch AM, O'Ryan M, Van R, Pickering LK. Invasive disease due to multiply resistant streptococcus pneumoniae in a Houston, tex, day-care center. Am J Dis Child. 1990;144:923–927. doi: 10.1001/archpedi.1990.02150320087033. [DOI] [PubMed] [Google Scholar]
- 37.Bain M, Ahmad N, Elder AT. Pneumococcal cross-infection in hospitalized elderly patients. Br J Hosp Med. 1990;44:416. [PubMed] [Google Scholar]
- 38.Mercat A, Nguyen J, Dautzenberg B. An outbreak of pneumococcal pneumonia in two men's shelters. Chest. 1991;99:147–151. doi: 10.1378/chest.99.1.147. [DOI] [PubMed] [Google Scholar]
- 39.Cartmill TD, Panigrahi H. Hospital outbreak of multiresistant Streptococcus pneumoniae. J Hosp Infect. 1992;20:130–132. doi: 10.1016/0195-6701(92)90121-2. [DOI] [PubMed] [Google Scholar]
- 40.Dawson S, Pallett A, Davidson A, Tuck A. Outbreak of multiresistant pneumococci. J Hosp Infect. 1992;22:328–329. doi: 10.1016/0195-6701(92)90020-M. [DOI] [PubMed] [Google Scholar]
- 41.A nosocomial outbreak of Streptococcus pneumoniae infection. Commun Dis Rep CDR Wkly 1992, 2:29. [PubMed]
- 42.Quick RE, Hoge CW, Hamilton DJ, Whitney CJ, Borges M, Kobayashi JM. Underutilization of pneumococcal vaccine in nursing home in Washington state: report of a serotype-specific outbreak and a survey. Am J Med. 1993;94:149–152. doi: 10.1016/0002-9343(93)90176-P. [DOI] [PubMed] [Google Scholar]
- 43.Gratten M, Morey F, Dixon J, Manning K, Torzillo P, Matters R, Erlich J, Hanna J, Asche V, Riley I. An outbreak of serotype 1 Streptococcus pneumoniae infection in Central Australia. Med J Aust. 1993;158:340–342. doi: 10.5694/j.1326-5377.1993.tb121794.x. [DOI] [PubMed] [Google Scholar]
- 44.Denton M, Hawkey PM, Hoy CM, Porter C. Co-existent cross-infection with Streptococcus pneumoniae and group B streptococci on an adult oncology unit. J Hosp Infect. 1993;23:271–278. doi: 10.1016/0195-6701(93)90144-O. [DOI] [PubMed] [Google Scholar]
- 45.Cherian T, Steinhoff MC, Harrison LH, Rohn D, McDougal LK, Dick J. A cluster of invasive pneumococcal disease in young children in child care. Jama. 1994;271:695–697. doi: 10.1001/jama.1994.03510330073037. [DOI] [PubMed] [Google Scholar]
- 46.Millar MR, Brown NM, Tobin GW, Murphy PJ, Windsor AC, Speller DC. Outbreak of infection with penicillin-resistant Streptococcus pneumoniae in a hospital for the elderly. J Hosp Infect. 1994;27:99–104. doi: 10.1016/0195-6701(94)90002-7. [DOI] [PubMed] [Google Scholar]
- 47.Mandigers CM, Diepersloot RJ, Dessens M, Mol SJ, van Klingeren B. A hospital outbreak of penicillin-resistant pneumococci in the Netherlands. Eur Respir J. 1994;7:1635–1639. doi: 10.1183/09031936.94.07091635. [DOI] [PubMed] [Google Scholar]
- 48.Centers for Disease Control and Prevention. Hemorrhage and shock associated with invasive pneumococcal infection in healthy infants and children--New Mexico, 1993–1994. MMWR Morb Mortal Wkly Rep. 1995;43:949–952. [PubMed]
- 49.Raymond J, Bingen E, Doit C, Brahimi N, Bergeret M, Badoual J, Gendrel D. Failure of cefotaxime treatment in a patient with penicillin-resistant pneumococcal meningitis and confirmation of nosocomial spread by random amplified polymorphic DNA analysis. Clin Infect Dis. 1995;21:234–235. doi: 10.1093/clinids/21.1.234. [DOI] [PubMed] [Google Scholar]
- 50.Gillespie SH, McHugh TD, Hughes JE, Dickens A, Kyi MS, Kelsey M. An outbreak of penicillin resistant Streptococcus pneumoniae investigated by a polymerase chain reaction based genotyping method. J Clin Pathol. 1997;50:847–851. doi: 10.1136/jcp.50.10.847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fiore AE, Iverson C, Messmer T, Erdman D, Lett SM, Talkington DF, Anderson LJ, Fields B, Carlone GM, Breiman RF, Cetron MS. Outbreak of pneumonia in a long-term care facility: antecedent human parainfluenza virus 1 infection may predispose to bacterial pneumonia. J Am Geriatr Soc. 1998;46:1112–1117. doi: 10.1111/j.1532-5415.1998.tb06649.x. [DOI] [PubMed] [Google Scholar]
- 52.Nuorti JP, Butler JC, Crutcher JM, Guevara R, Welch D, Holder P, Elliott JA. An outbreak of multidrug-resistant pneumococcal pneumonia and bacteremia among unvaccinated nursing home residents. N Engl J Med. 1998;338:1861–1868. doi: 10.1056/NEJM199806253382601. [DOI] [PubMed] [Google Scholar]
- 53.Centers for Disease Control and Prevention. Outbreaks of pneumococcal pneumonia among unvaccinated residents of chronic-care facilities--Massachusetts, October 1995, Oklahoma, February, 1996, and Maryland, may-June 1996. MMWR Morb Mortal Wkly Rep. 1997;46:60–62. [PubMed]
- 54.Musher DM, Groover JE, Reichler MR, Riedo FX, Schwartz B, Watson DA, Baughn RE, Breiman RF. Emergence of antibody to capsular polysaccharides of Streptococcus pneumoniae during outbreaks of pneumonia: association with nasopharyngeal colonization. Clin Infect Dis. 1997;24:441–446. doi: 10.1093/clinids/24.3.441. [DOI] [PubMed] [Google Scholar]
- 55.Sheppard DC, Bartlett KA, Lampiris HW. Streptococcus pneumoniae transmission in chronic-care facilities: description of an outbreak and review of management strategies. Infect Control Hosp Epidemiol. 1998;19:851–853. doi: 10.2307/30141564. [DOI] [PubMed] [Google Scholar]
- 56.Razzaq N, Riordan T, McNinch AW, Daneshmend TK. A possible secondary case of pneumococcal meningitis. J Inf Secur. 1998;37:290–291. doi: 10.1016/s0163-4453(98)92200-9. [DOI] [PubMed] [Google Scholar]
- 57.Craig AS, Erwin PC, Schaffner W, Elliott JA, Moore WL, Ussery XT, Patterson L, Dake AD, Hannah SG, Butler JC. Carriage of multidrug-resistant Streptococcus pneumoniae and impact of chemoprophylaxis during an outbreak of meningitis at a day care center. Clin Infect Dis. 1999;29:1257–1264. doi: 10.1086/313451. [DOI] [PubMed] [Google Scholar]
- 58.de Galan BE, van Tilburg PM, Sluijter M, Mol SJ, de Groot R, Hermans PW, Jansz AR. Hospital-related outbreak of infection with multidrug-resistant Streptococcus pneumoniae in the Netherlands. J Hosp Infect. 1999;42:185–192. doi: 10.1053/jhin.1999.0580. [DOI] [PubMed] [Google Scholar]
- 59.Kellner JD, Gibb AP, Zhang J, Rabin HR. Household transmission of Streptococcus pneumoniae, Alberta, Canada. Emerg Infect Dis. 1999;5:154–158. doi: 10.3201/eid0501.990120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Leggiadro RJ, Schaberg DR. Nosocomial pneumococcal infection: an outbreak. Hosp Pract (1995) 1999;34:77–78. doi: 10.3810/hp.1999.09.15.166. [DOI] [PubMed] [Google Scholar]
- 61.Dagan R, Gradstein S, Belmaker I, Porat N, Siton Y, Weber G, Janco J, Yagupsky P. An outbreak of Streptococcus pneumoniae serotype 1 in a closed community in southern Israel. Clin Infect Dis. 2000;30:319–321. doi: 10.1086/313645. [DOI] [PubMed] [Google Scholar]
- 62.Centers for Disease Control and Prevention. Outbreak of pneumococcal pneumonia among unvaccinated residents of a nursing home--New Jersey, April 2001. MMWR Morb Mortal Wkly Rep. 2001;50:707–710. [PubMed]
- 63.Tan CG, Ostrawski S, Bresnitz EA. A preventable outbreak of pneumococcal pneumonia among unvaccinated nursing home residents in New Jersey during 2001. Infect Control Hosp Epidemiol. 2003;24:848–852. doi: 10.1086/502148. [DOI] [PubMed] [Google Scholar]
- 64.Weiss K, Restieri C, Gauthier R, Laverdiere M, McGeer A, Davidson RJ, Kilburn L, Bast DJ, de Azavedo J, Low DE. A nosocomial outbreak of fluoroquinolone-resistant Streptococcus pneumoniae. Clin Infect Dis. 2001;33:517–522. doi: 10.1086/322658. [DOI] [PubMed] [Google Scholar]
- 65.Melamed R, Greenberg D, Landau D, Khvatskin S, Shany E, Dagan R. Neonatal nosocomial pneumococcal infections acquired by patient-to-patient transmission. Scand J Infect Dis. 2002;34:385–386. doi: 10.1080/00365540110080241. [DOI] [PubMed] [Google Scholar]
- 66.Crum NF, Wallace MR, Lamb CR, Conlin AM, Amundson DE, Olson PE, Ryan MA, Robinson TJ, Gray GC, Earhart KC. Halting a pneumococcal pneumonia outbreak among United States marine corps trainees. Am J Prev Med. 2003;25:107–111. doi: 10.1016/S0749-3797(03)00114-4. [DOI] [PubMed] [Google Scholar]
- 67.Subramanian D, Sandoe JA, Keer V, Wilcox MH. Rapid spread of penicillin-resistant Streptococcus pneumoniae among high-risk hospital inpatients and the role of molecular typing in outbreak confirmation. J Hosp Infect. 2003;54:99–103. doi: 10.1016/S0195-6701(03)00110-5. [DOI] [PubMed] [Google Scholar]
- 68.Sanchez JL, Craig SC, Kolavic S, Hastings D, Alsip BJ, Gray GC, Hudspeth MK, Ryan MA. An outbreak of pneumococcal pneumonia among military personnel at high risk: control by low-dose azithromycin postexposure chemoprophylaxis. Mil Med. 2003;168:1–6. [PubMed] [Google Scholar]
- 69.Banerjee A, Kalghatgi AT, Saiprasad GS, Nagendra A, Panda BN, Dham SK, Mahen A, Menon KD, Khan MA. Outbreak of pneumococcal pneumonia among military recruits. Med J Armed Forces India. 2005;61:16–21. doi: 10.1016/S0377-1237(05)80111-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Carter RJ, Sorenson G, Heffernan R, Kiehlbauch JA, Kornblum JS, Leggiadro RJ, Nixon LJ, Wertheim WA, Whitney CG, Layton M. Failure to control an outbreak of multidrug-resistant Streptococcus pneumoniae in a long-term-care facility: emergence and ongoing transmission of a fluoroquinolone-resistant strain. Infect Control Hosp Epidemiol. 2005;26:248–255. doi: 10.1086/502534. [DOI] [PubMed] [Google Scholar]
- 71.Centers for Disease Control and Prevention. Outbreak of invasive pneumococcal disease--Alaska, 2003–2004. MMWR Morb Mortal Wkly Rep. 2005;54:72–75. [PubMed]
- 72.Zulz T, Wenger JD, Rudolph K, Robinson DA, Rakov AV, Bruden D, Singleton RJ, Bruce MG, Hennessy TW. Molecular characterization of Streptococcus pneumoniae serotype 12F isolates associated with rural community outbreaks in Alaska. J Clin Microbiol. 2013;51:1402–1407. doi: 10.1128/JCM.02880-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Birtles A, McCarthy N, Sheppard CL, Rutter H, Guiver M, Haworth E, George RC. Multilocus sequence typing directly on DNA from clinical samples and a cultured isolate to investigate linked fatal pneumococcal disease in residents of a shelter for homeless men. J Clin Microbiol. 2005;43:2004–2008. doi: 10.1128/JCM.43.4.2004-2008.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hansmann Y, Doyle A, Remy V, Jaulhac B, Christmann D, Lesens O, Perrocheau A. An outbreak of pneumococcal pneumonia among residents of a retirement home in France during October 2003. Infect Control Hosp Epidemiol. 2006;27:1252–1254. doi: 10.1086/508842. [DOI] [PubMed] [Google Scholar]
- 75.Singh P, Jaiswal A, Handa S, Bhalwar R, Wankhede V, Banerjee A, Bhatnagar D, Kumar H. Outbreak of pneumococcal pneumonia in Military Barracks. Indian J Community Med. 2006;31:160–163. [Google Scholar]
- 76.Cashman P, Massey P, Durrheim D, Islam F, Merritt T, Eastwood K. Pneumonia cluster in a boarding school--implications for influenza control. Commun Dis Intell Q Rep. 2007;31:296–298. doi: 10.33321/cdi.2007.31.30. [DOI] [PubMed] [Google Scholar]
- 77.Sheppard CL, Salmon JE, Harrison TG, Lyons M, George RC. The clinical and public health value of non-culture methods in the investigation of a cluster of unexplained pneumonia cases. Epidemiol Infect. 2008;136:922–927. doi: 10.1017/S0950268807009302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Romney MG, Hull MW, Gustafson R, Sandhu J, Champagne S, Wong T, Nematallah A, Forsting S, Daly P. Large community outbreak of Streptococcus pneumoniae serotype 5 invasive infection in an impoverished, urban population. Clin Infect Dis. 2008;47:768–774. doi: 10.1086/591128. [DOI] [PubMed] [Google Scholar]
- 79.Vainio A, Lyytikainen O, Sihvonen R, Kaijalainen T, Teirila L, Rantala M, Lehtinen P, Ruuska P, Virolainen A. An outbreak of pneumonia associated with S. pneumoniae at a military training facility in Finland in 2006. Apmis. 2009;117:488–491. doi: 10.1111/j.1600-0463.2009.02463.x. [DOI] [PubMed] [Google Scholar]
- 80.Gupta A, Khaw FM, Stokle EL, George RC, Pebody R, Stansfield RE, Sheppard CL, Slack M, Gorton R, Spencer DA. Outbreak of Streptococcus pneumoniae serotype 1 pneumonia in a United Kingdom school. Bmj. 2008;337:a2964. doi: 10.1136/bmj.a2964. [DOI] [PubMed] [Google Scholar]
- 81.Mehiri-Zghal E, Decousser JW, Mahjoubi W, Essalah L, El Marzouk N, Ghariani A, Allouch P, Slim-Saidi NL. Molecular epidemiology of a Streptococcus pneumoniae serotype 1 outbreak in a Tunisian jail. Diagn Microbiol Infect Dis. 2010;66:225–227. doi: 10.1016/j.diagmicrobio.2009.05.008. [DOI] [PubMed] [Google Scholar]
- 82.Balicer RD, Zarka S, Levine H, Klement E, Sela T, Porat N, Ash N, Dagan R. Control of Streptococcus pneumoniae serotype 5 epidemic of severe pneumonia among young army recruits by mass antibiotic treatment and vaccination. Vaccine. 2010;28:5591–5596. doi: 10.1016/j.vaccine.2010.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Pichon B, Moyce L, Sheppard C, Slack M, Turbitt D, Pebody R, Spencer DA, Edwards J, Krahe D, George R. Molecular typing of pneumococci for investigation of linked cases of invasive pneumococcal disease. J Clin Microbiol. 2010;48:1926–1928. doi: 10.1128/JCM.02054-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Dawood FS, Ambrose JF, Russell BP, Hawksworth AW, Winchell JM, Glass N, Thurman K, Soltis MA, McDonough E, Warner AK, et al. Outbreak of pneumonia in the setting of fatal pneumococcal meningitis among US Army trainees: potential role of chlamydia pneumoniae infection. BMC Infect Dis. 2011;11:157. doi: 10.1186/1471-2334-11-157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Vanderkooi OG, Church DL, MacDonald J, Zucol F, Kellner JD. Community-based outbreaks in vulnerable populations of invasive infections caused by Streptococcus pneumoniae serotypes 5 and 8 in Calgary, Canada. PLoS One. 2011;6:e28547. doi: 10.1371/journal.pone.0028547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Skoczynska A, Sadowy E, Krawiecka D, Czajkowska-Malinowska M, Ciesielska A, Przybylski G, Zebracka R, Hryniewicz W. Nosocomial outbreak of Streptococcus pneumoniae Spain9VST15614 clone in a pulmonary diseases ward. Pol Arch Med Wewn. 2012;122:361–366. doi: 10.20452/pamw.1353. [DOI] [PubMed] [Google Scholar]
- 87.Fleming-Dutra K, Mbaeyi C, Link-Gelles R, Alexander N, Guh A, Forbes E, Beall B, Winchell JM, Carvalho Mda G, Pimenta F, et al. Streptococcus pneumoniae serotype 15A in psychiatric unit, Rhode Island, USA, 2010-2011. Emerg Infect Dis. 2012;18:1889–1893. doi: 10.3201/eid1811.120454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Centers for Disease Control and Prevention. Notes from the field: Outbreak of severe respiratory illness in an assisted-living facility--Colorado, 2012. MMWR Morb Mortal Wkly Rep. 2013;62:230–1. [PMC free article] [PubMed]
- 89.Kuroki T, Ishida M, Suzuki M, Furukawa I, Ohya H, Watanabe Y, Konnai M, Aihara Y, Chang B, Ariyoshi K, et al. Outbreak of Streptococcus pneumoniae serotype 3 pneumonia in extremely elderly people in a nursing home unit in Kanagawa, Japan, 2013. J Am Geriatr Soc. 2014;62:1197–1198. doi: 10.1111/jgs.12863. [DOI] [PubMed] [Google Scholar]
- 90.Ben-David D, Schwaber MJ, Adler A, Masarwa S, Edgar R, Navon-Venezia S, Schwartz D, Porat N, Kotlovsky T, Polivkin N, et al. Persistence and complex evolution of fluoroquinolone-resistant Streptococcus pneumoniae clone. Emerg Infect Dis. 2014;20:799–805. doi: 10.3201/eid2005.130142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Schillberg E, Isaac M, Deng X, Peirano G, Wylie JL, Van Caeseele P, Pillai DR, Sinnock H, Mahmud SM. Outbreak of invasive Streptococcus pneumoniae serotype 12F among a marginalized inner-city population in Winnipeg, Canada, 2009-2011. Clin Infect Dis. 2014;59:651–657. doi: 10.1093/cid/ciu366. [DOI] [PubMed] [Google Scholar]
- 92.Suryam V, Bhatti VK, Kulkarni A, Mahen A, Nair V. Outbreak control of community acquired pneumonia in a large military training institution. Med J Armed Forces India. 2015;71:33–37. doi: 10.1016/j.mjafi.2014.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Thomas HL, Gajraj R, Slack MP, Sheppard C, Hawkey P, Gossain S, Drew CM, Pebody RG. An explosive outbreak of Streptococcus pneumoniae serotype-8 infection in a highly vaccinated residential care home, England, summer 2012. Epidemiol Infect. 2015;143:1957–1963. doi: 10.1017/S0950268814002490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kunwar R, Sidana N. Mass chemoprophylaxis in control of pneumococcal pneumonia outbreak in a military training Centre. Indian J Public Health. 2015;59:109–114. doi: 10.4103/0019-557X.157526. [DOI] [PubMed] [Google Scholar]
- 95.Sheppard CL, Clark J, Slack MP, Fry NK, Harrison TG. Use of a serotype-specific urine immunoassay to determine the course of a hospital outbreak of Streptococcus pneumoniae complicated by influenza a. JMM Case Rep. 2016;3:e005002. doi: 10.1099/jmmcr.0.005002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ewing J, Patterson L, Irvine N, Doherty L, Loughrey A, Kidney J, Sheppard C, Kapatai G, Fry NK, Ramsay M, Jessop L. Serious pneumococcal disease outbreak in men exposed to metal fume - detection, response and future prevention through pneumococcal vaccination. Vaccine. 2017;35:3945–3950. doi: 10.1016/j.vaccine.2017.06.010. [DOI] [PubMed] [Google Scholar]
- 97.Jauneikaite E, Khan-Orakzai Z, Kapatai G, Bloch S, Singleton J, Atkin S, Shah V, Hatcher J, Samarasinghe D, Sheppard C, et al. Nosocomial outbreak of drug-resistant Streptococcus pneumoniae serotype 9V in an adult respiratory medicine Ward. J Clin Microbiol. 2017;55:776–782. doi: 10.1128/JCM.02405-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Shayegani M, Parsons LM, Gibbons WE, Jr, Campbell D. Characterization of nontypable Streptococcus pneumoniae-like organisms isolated from outbreaks of conjunctivitis. J Clin Microbiol. 1982;16:8–14. doi: 10.1128/jcm.16.1.8-14.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ertugrul N, Rodriguez-Barradas MC, Musher DM, Ryan MA, Agin CS, Murphy SJ, Shayegani M, Watson DA. BOX-polymerase chain reaction-based DNA analysis of nonserotypeable Streptococcus pneumoniae implicated in outbreaks of conjunctivitis. J Infect Dis. 1997;176:1401–1405. doi: 10.1086/517331. [DOI] [PubMed] [Google Scholar]
- 100.Centers for Disease Control and Prevention. Pneumococcal conjunctivitis at an elementary school--Maine, September 20–December 6, 2002. MMWR Morb Mortal Wkly Rep. 2003;52:64–66. [PubMed]
- 101.Martin M, Turco JH, Zegans ME, Facklam RR, Sodha S, Elliott JA, Pryor JH, Beall B, Erdman DD, Baumgartner YY, et al. An outbreak of conjunctivitis due to atypical Streptococcus pneumoniae. N Engl J Med. 2003;348:1112–1121. doi: 10.1056/NEJMoa022521. [DOI] [PubMed] [Google Scholar]
- 102.Zegans ME, Sanchez PA, Likosky DS, Allar RT, Martin M, Schwartzman JD, Pryor JH, Turco JH, Whitney CG. Clinical features, outcomes, and costs of a conjunctivitis outbreak caused by the ST448 strain of Streptococcus pneumoniae. Cornea. 2009;28:503–509. doi: 10.1097/ICO.0b013e3181909362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Crum NF, Barrozo CP, Chapman FA, Ryan MA, Russell KL. An outbreak of conjunctivitis due to a novel unencapsulated Streptococcus pneumoniae among military trainees. Clin Infect Dis. 2004;39:1148–1154. doi: 10.1086/424522. [DOI] [PubMed] [Google Scholar]
- 104.Buck JM, Lexau C, Shapiro M, Glennen A, Boxrud DJ, Koziol B, Whitney CG, Beall B, Danila R, Lynfield R. A community outbreak of conjunctivitis caused by nontypeable Streptococcus pneumoniae in Minnesota. Pediatr Infect Dis J. 2006;25:906–911. doi: 10.1097/01.inf.0000238143.96607.ec. [DOI] [PubMed] [Google Scholar]
- 105.Hennink M, Abbas Z, McDonald RR, Nagle E, Montgomery KL, Diener T, Horsman GB, Levett PN. Streptococcus pneumoniae outbreak in a rural Regina community. Can Commun Dis Rep. 2006;32:181–186. [PubMed] [Google Scholar]
- 106.Marton A, Nagy A, Katona G, Fekete F, Votisky P, Lajos Z. Nosocomial Streptococcus pneumoniae infection causing children's acute otitis media. Int J Antimicrob Agents. 1997;8:29–35. doi: 10.1016/S0924-8579(96)00357-3. [DOI] [PubMed] [Google Scholar]
- 107.Nakashima T, Fukushima K, Tahara M, Sugata KI, Ogawa T, Sugata A, Gunduz M, Ueki Y, Uno Y, Nishizaki K. Random amplified polymorphic DNA analysis applied to acute otitis media caused by penicillin non-susceptible Streptococcus pneumoniae. J Infect Chemother. 2001;7:239–242. doi: 10.1007/s101560170019. [DOI] [PubMed] [Google Scholar]
- 108.Guillet M, Zahar JR, Timsit MO, Grandin L, Carbonnelle E, Join-Lambert O, Quesne G, Nassif X, Mejean A, Carbonne A. Horizontal transmission of Streptococcus pneumoniae in the surgical ward: a rare source of nosocomial wound infection. Am J Infect Control. 2012;40:71–72. doi: 10.1016/j.ajic.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 109.Gilman BB, Anderson GW. A community outbreak of type I pneumococcus infection. Am J Hyg. 1938;28:345–348. [Google Scholar]
- 110.Centers for Disease Control and Prevention. From the Centers for Disease Control and Prevention. Outbreaks of pneumococcal pneumonia among unvaccinated residents in chronic-care facilities--Massachusetts, October 1995, Oklahoma, February 1996, and Maryland, may-June 1996. Jama. 1997;277:452–453. [PubMed]
- 111.Centers for Disease Control and Prevention. Heymann, DL. Control of Communicable Diseases Manual. 20th edn. Washington, DC: American Public Health Association; 2015.
- 112.Siegel JD, Rhinehart E, Jackson M, Chiarello L. Guideline for isolation precautions: preventing transmission of infectious agents in health care settings. Am J Infect Control. 2007;2007(35):S65–164. doi: 10.1016/j.ajic.2007.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Pediatrics AAo . In: In Red Book: 2015 Report of the Committee on Infectious Diseases. 30. Kimberlin D, Brady M, Jackson M, Long S, editors. Elk Grove Village, IL: American Academy of Pediatrics; 2015. p. 633. [Google Scholar]
- 114.Grabenstein JD, Musey LK. Differences in serious clinical outcomes of infection caused by specific pneumococcal serotypes among adults. Vaccine. 2014;32:2399–2405. doi: 10.1016/j.vaccine.2014.02.096. [DOI] [PubMed] [Google Scholar]
- 115.Centers for Disease Control and Prevention. Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine for adults with immunocompromising conditions: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2012;61:816–9. [PubMed]
- 116.Tomczyk S, Bennett NM, Stoecker C, Gierke R, Moore MR, Whitney CG, Hadler S, Pilishvili T. Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine among adults aged >/=65 years: recommendations of the advisory committee on immunization practices (ACIP) MMWR Morb Mortal Wkly Rep. 2014;63:822–825. [PMC free article] [PubMed] [Google Scholar]
- 117.Bridges CB, Woods L, Coyne-Beasley T. Advisory committee on immunization practices (ACIP) recommended immunization schedule for adults aged 19 years and older--United States, 2013. MMWR Suppl. 2013;62:9–19. [PubMed] [Google Scholar]
- 118.Prevention CfDCa: Recommended Immunization Schedule for Adults Aged 19 Years or Older, United States, 2018. (Services UDoHaH ed.; 2018. [DOI] [PubMed]
- 119.Frenck RW, Jr, Fiquet A, Gurtman A, van Cleeff M, Davis M, Rubino J, Smith W, Sundaraiyer V, Sidhu M, Emini EA, et al. Immunogenicity and safety of a second administration of 13-valent pneumococcal conjugate vaccine 5 years after initial vaccination in adults 50 years and older. Vaccine. 2016;34:3454–3462. doi: 10.1016/j.vaccine.2016.04.093. [DOI] [PubMed] [Google Scholar]
- 120.Remschmidt C, Harder T, Wichmann O, Bogdan C, Falkenhorst G. Effectiveness, immunogenicity and safety of 23-valent pneumococcal polysaccharide vaccine revaccinations in the elderly: a systematic review. BMC Infect Dis. 2016;16:711. doi: 10.1186/s12879-016-2040-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Grabenstein JD, Manoff SB. Pneumococcal polysaccharide 23-valent vaccine: long-term persistence of circulating antibody and immunogenicity and safety after revaccination in adults. Vaccine. 2012;30:4435–4444. doi: 10.1016/j.vaccine.2012.04.052. [DOI] [PubMed] [Google Scholar]
- 122.Mosser JF, Grant LR, Millar EV, Weatherholtz RC, Jackson DM, Beall B, Craig MJ, Reid R, Santosham M, O'Brien KL. Nasopharyngeal carriage and transmission of Streptococcus pneumoniae in American Indian households after a decade of pneumococcal conjugate vaccine use. PLoS One. 2014;9:e79578. doi: 10.1371/journal.pone.0079578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Pessoa D, Hoti F, Syrjanen R, Sa-Leao R, Kaijalainen T, Gomes MG, Auranen K. Comparative analysis of Streptococcus pneumoniae transmission in Portuguese and Finnish day-care centres. BMC Infect Dis. 2013;13:180. doi: 10.1186/1471-2334-13-180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Hussain M, Melegaro A, Pebody RG, George R, Edmunds WJ, Talukdar R, Martin SA, Efstratiou A, Miller E. A longitudinal household study of Streptococcus pneumoniae nasopharyngeal carriage in a UK setting. Epidemiol Infect. 2005;133:891–898. doi: 10.1017/S0950268805004012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Shimada J, Yamanaka N, Hotomi M, Suzumoto M, Sakai A, Ubukata K, Mitsuda T, Yokota S, Faden H. Household transmission of Streptococcus pneumoniae among siblings with acute otitis media. J Clin Microbiol. 2002;40:1851–1853. doi: 10.1128/JCM.40.5.1851-1853.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Edouard S, Al-Tawfiq JA, Memish ZA, Yezli S, Gautret P. Impact of the hajj on pneumococcal carriage and the effect of various pneumococcal vaccines. Vaccine. 2017. 10.1016/j.vaccine.2018.09.017. [DOI] [PubMed]
- 127.Davis BM, Aiello AE, Dawid S, Rohani P, Shrestha S, Foxman B. Influenza and community-acquired pneumonia interactions: the impact of order and time of infection on population patterns. Am J Epidemiol. 2012;175:363–367. doi: 10.1093/aje/kwr402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Rudd JM, Ashar HK, Chow VTK, Teluguakula N: Lethal synergism between influenza and Streptococcus pneumoniae. J Infect Pulm Dis 2016, 2:10.16966/12470-13176.16114. [DOI] [PMC free article] [PubMed]
- 129.Launes C, de-Sevilla MF, Selva L, Garcia-Garcia JJ, Pallares R, Munoz-Almagro C. Viral coinfection in children less than five years old with invasive pneumococcal disease. Pediatr Infect Dis J. 2012;31:650–653. doi: 10.1097/INF.0b013e31824f25b0. [DOI] [PubMed] [Google Scholar]
- 130.Wolter N, Tempia S, Cohen C, Madhi SA, Venter M, Moyes J, Walaza S, Malope-Kgokong B, Groome M, du Plessis M, et al. High nasopharyngeal pneumococcal density, increased by viral coinfection, is associated with invasive pneumococcal pneumonia. J Infect Dis. 2014;210:1649–1657. doi: 10.1093/infdis/jiu326. [DOI] [PubMed] [Google Scholar]
- 131.CDC: Interim guidance for use of 23-valent pneumococcal polysaccharide vaccine during novel influenza A (H1N1) outbreak. http://www.cdc.gov/h1n1flu/guidance/ppsv_h1n1.htm 2009.
- 132.Gupta RK, George R, Nguyen-Van-Tam JS. Bacterial pneumonia and pandemic influenza planning. Emerg Infect Dis. 2008;14:1187–1192. doi: 10.3201/eid1408.070751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.McCullers JA. Insights into the interaction between influenza virus and pneumococcus. Clin Microbiol Rev. 2006;19:571–582. doi: 10.1128/CMR.00058-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.ABCs Report: Streptococcus pneumoniae, 2015. (Prevention CfDCa ed.; 2016.
- 135.Dagan R, Klugman KP. Impact of conjugate pneumococcal vaccines on antibiotic resistance. Lancet Infect Dis. 2008;8:785–795. doi: 10.1016/S1473-3099(08)70281-0. [DOI] [PubMed] [Google Scholar]
- 136.Tomczyk S, Arriola CS, Beall B, Benitez A, Benoit SR, Berman L, Bresee J, da Gloria CM, Cohn A, Cross K, et al. Multistate outbreak of respiratory infections among unaccompanied children, June 2014–July 2014. Clin Infect Dis. 2016;63:48–56. doi: 10.1093/cid/ciw147. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Article exclusion flow diagram. (PNG 22 kb)
Table S1. Data extracted from reviewed articles. (XLSX 28 kb)
Data Availability Statement
The data extracted from publications and analyzed for the systematic review are available in the supplement of this article and is available upon request from the corresponding author.


