Abstract
Objective
Understanding how individuals with mental illness who receive services at peer support agencies use technology can inform the development of online and mobile health interventions tailored for users in these non-traditional mental health settings. The purpose of this study was to assess the use of technology among individuals with mental illness at peer support agencies.
Methods
A survey delivered within peer support agencies (PSAs) in one state assessed technology use among individuals ages 18 and over with a self-identified mental illness receiving services at these agencies.
Results
In total, 195 individuals from 10 PSAs completed the survey. Eighty-two percent of respondents used the internet, with 63% of respondents connected to the internet at the PSAs. Eighty one percent of respondents owned a cell phone, 70% used text messaging, 58% owned smartphones, 61% used mobile applications, and 72% used social media. PSA users under age 55 were significantly more likely to own a smartphone than PSA users age 55 and older. Among internet users, 71% had searched for health information online and 57% had searched for mental health information online
Conclusions
Many individuals who receive services at PSAs have access to online and mobile technologies. These technologies may be leveraged to expand the reach of evidence-based health and mental health programs to individuals in these non-traditional mental health settings. Future research should explore the feasibility of intervention strategies that involve PSAs as a resource for linking people with mental illness to online and mobile support for their health and wellness goals.
Keywords: Mental illness, peer support, technology, mobile health, social media
Introduction
Internet and mobile technologies provide a unique opportunity to deliver cost-effective interventions with on demand information and support for health and wellness. Approximately nine-in-ten American adults use the internet, 93% own cell phones, 77% own smartphones, and 79% of adults who are online use popular social media such as Facebook [1–3]. Lower income adults are making gains in technology adoption, though a digital divide between lower and upper income individuals persists [4]. Increasing internet use and mobile device ownership among lower-income adults is generating enthusiasm for the potential to reach vulnerable groups with evidence-based therapeutic tools for health and mental health promotion [5]. Considering the many barriers to receiving evidence-based behavioral interventions, digital technology is a promising solution to reaching the millions of people worldwide with mental illness with potentially cost-effective and accessible interventions to advance physical and mental health [6, 7].
Most prior research on technology use among persons with mental illness in the US has been conducted in outpatient psychiatric clinics and community mental health centers [8–11], where patients are engaged in formal mental health care services. Researchers exploring the potential of technology use in psychiatry have primarily focused on developing evidence-based tools for use in clinical settings delivered by clinical providers to improve mental health diagnosis and psychiatric treatment and rehabilitation [12]. To date surprisingly little attention has been given to the potential for online and mobile technologies to address the health and mental health needs of persons with mental illness in non-traditional mental health settings, such as self-help organizations, consumer-run services, and mental health advocacy organizations.
National estimates indicate that over one million people in the US receive services from self-help and consumer-run organizations that offer complementary and alternative mental health services for individuals with mental illness and their family members [13]. A primary objective of consumer-run services is to promote recovery outcomes, such as quality of life and social and personal functioning, in contrast to treating or preventing clinical features of mental illness [14]. Technology-based therapeutic tools that target constructs such as empowerment, self-efficacy, self-determination, and social connections [15–18] may be particularly appealing in non-clinical peer support settings. A first step in exploring the feasibility of intervening with digital health technologies in peer support settings is to understand how individuals served in these non-traditional mental health settings use online and mobile technologies.
In a prior study we conducted preliminary research on the use of computers and the internet among people with mental illness who were users of peer support agencies (PSAs) [19]. PSAs provide non-clinical mental health services that are augments to, referral sources for, or alternatives to public mental health centers for individuals who self-identify as a person with mental illness. Our survey results showed that over three quarters (79%) of PSA users had gone online in the past year, and 49% were interested in learning more about online forums that provide information and support for mental health issues [19]. The objective of the present study was to expand on our prior work and to conduct a more comprehensive assessment of technology use among PSA users that included use of mobile technologies, such as smartphones, mobile applications, and social media.
Methods
The New Hampshire Bureau of Behavioral Health facilitated a survey of technology use among consumers receiving services at NH Peer Support Agencies (PSAs). NH PSAs are operated by and for people with a mental illness and are designed to promote mental health recovery. PSA services include, but are not limited to: face-to-face and telephone peer support; outreach; monthly educational events; activities that promote self-advocacy; wellness training; after hours warm line; and crisis respite (24 hours, short-term, non-medical crisis program). Thirteen PSAs have contracted with the NH Department of Health and Human Services, Bureau of Behavioral Health to provide services to people with mental illness who are 18 years of age or older and self-identify as a recipient, former recipient, or at significant risk of becoming a recipient of publicly funded mental health services.
The technology use survey in the present study was administered over a 60-day period starting in July 2016. At the time of the survey there were 1064 active members of the PSAs. PSA leadership and staff invited all participants of the PSAs to complete a 15-question survey. The survey was anonymous and was completed electronically on a web-based platform (i.e. Survey Monkey) using a computer located at the PSA or on paper. This format made it possible to survey members of the PSAs regardless of their current access to or familiarity with using the internet or other technology. PSA leadership and staff provided support to complete the survey if needed.
Survey respondents were asked to report their age and race, and to identify which of the 13 PSAs they belonged to. The technology use survey was adapted from our prior research assessing technology use among individuals with serious mental illness at community mental health centers [10]. Four questions focused on internet use: 1) Do you use the internet? 2) Please tell me about all the ways you connect to the internet choosing from a list of common ways to access it (e.g., home computer, cell phone with internet access, at the peer support agency) 3) Have you ever used the internet to access information about your health? 4) Have you ever used the internet to access information about your mental health? Four questions focused on cell phone ownership and use: 1) Do you own a cell phone? 2) Is your phone a smartphone (in other words, does it let you make telephone calls but also send text and receive emails and texts)? 3) Do you ever use your phone to send and receive text messages? 4) Please tell me from the following list what type of mobile devices you use regularly (e.g., iPhone, Android phone, or other smartphone).
Four questions focused on assessing use of mobile applications: 1) Do you use apps (e.g., for email, music, games, maps, checking the weather)? 2) What is your favorite app? 3) Have you ever used a health or fitness app? 4) Have you ever used a mental health app? Three questions focused on use of social media: 1) Do you use any of these popular sites, check all that apply (e.g., Facebook, Twitter, Instagram, Snapchat, YouTube)? 2) Have you ever searched for information about your physical health on these sites? 3) Have you ever searched for information about your mental health on these sites? The survey did not collect any personally identifiable information and thus was exempt from review by the NH Department of Health and Human Services Institutional Review Board. We followed the guidelines for maintaining the safety of humans subjects as outlined by the Declaration of Helsinki.
Data Analysis
Descriptive statistics were used to characterize the sample and chi-square tests of independence were used to examine whether there was a significant relationship between mobile phone ownership and age. Specifically, we compared cell phone and smartphone ownership among PSA users ages 18 to 54 to users ages 55 and older. We hypothesized that PSA users under age 55 would be more likely to own cell phones and smartphones than PSA users age 55 and older. We also compared participants’ online and mobile technology use with findings reported in a prior published survey of individuals with serious mental illness receiving services from community mental health centers in New Hampshire [10], as well as national surveys of the general adult population conducted by the Pew Research Center on internet, smartphone, and social media use [2, 3, 1]. Data analyses were conducted using SPSS version 23.
Results
In 2016, NH PSAs provided services to over 2,300 adults with mental illness. During the 60-day survey period, 195 of the 1064 people participating in peer support services (18%) during the first quarter responded to the survey. PSA survey respondents were predominately White (86%). Only 7% of PSA users were under age 25 years, 32% were age 25–44 years, 53% were age 45–64 years, and 8% were over age 65 years.
Over three quarters (82%) of respondents used the internet, 80% owned a cell phone, 70% used text messaging, 58% owned smartphones, 61% used mobile applications, and 72% used social media. Among participants who owned a smartphone, 59% owned an Android phone, 29% owned an iPhone, and 12% owned another type of smartphone. PSA users under age 55 (n = 112) were significantly more likely to own a cell phone (86% vs. 71%, respectively) than PSA users age 55 and older (n = 65), χ2 (1, N = 177) = 5.79, p <.05. PSA users under age 55 (n = 112) were also significantly more likely to own a smartphone (67% vs. 43%, respectively) than PSA users age 55 and older (n = 63), χ2 (1, N = 175) = 9.64, p <.01.
Seventy-one percent of respondents who used the internet had searched for health information online and 57% had searched for mental health information online. Forty percent of respondents who used mobile applications used a health or fitness app and 23% used a mental health app. Table 1 highlights characteristics of respondents’ use of technology, including the different ways they connected to the internet and the social media sites they used. Table 2 shows mobile phone ownership by population density of the cities where the PSAs were located. Mobile phone ownership did not appear to vary by population density of PSA location.
Table 1.
Characteristics of PSA Users’ Technology Use
| Survey Responses | Participants n (%) |
|---|---|
| Ways respondents access internet among the 156 (82%) respondents who used the Internet | |
| Peer support agency | 96 (62%) |
| Cell phone | 90 (58%) |
| Personal computer | 84 (54%) |
| Library | 55 (35%) |
| Tablet computer (e.g., iPad) | 41 (26%) |
| Workplace | 38 (24%) |
| Family or friend’s computer | 34 (22%) |
| Mental health agency | 12 (8%) |
| School | 6 (4%) |
| Senior center | 4 (3%) |
| Types of social Media use among the 141 (72%) respondents who used social media | |
| 109 (77%) | |
| 16 (11% | |
| 21 (15%) | |
| Snapchat | 17 (12%) |
| YouTube | 115 (82%) |
| 20 (14%) | |
| Tumblr | 5 (4%) |
| 28 (20%) | |
| 5 (4%) | |
| Google Plus | 52 (37%) |
| 4 (2%) | |
| Myspace | 1 (0.7%) |
Table 2.
Mobile Phone Ownership by Population Density of Peer Support Agency Location
| NH PSA Location | (N) | Population Density (per SQMI) | Cell Phone Ownership | Smartphone Ownership |
|---|---|---|---|---|
|
| ||||
| % | % | |||
| Claremont city and Lebanon city | 36 | 312 | 82.4% | 73.5% |
| Conway town, Carroll County | 37 | 326 | 75.7% | 51.4% |
| Laconia city, Belknap County | 24 | 404 | 91.7% | 66.7% |
| Keene city, Cheshire County | 16 | 621 | 86.7% | 71.4% |
| Concord city, Merrimack County | 20 | 630 | 85.0% | 55.0% |
| Rochester city, Strafford County | 4 | 653 | 75.0% | 75.0% |
| Portsmouth city, Rockingham County | 12 | 1,268 | 50.0% | 11.1% |
| Derry town, Rockingham County | 13 | 1,430 | 84.7% | 46.2% |
| Nashua city, Hillsborough County | 12 | 2,722 | 70.0% | 45.5% |
| Manchester city, Hillsborough County | 9 | 3,148 | 77.8% | 77.8% |
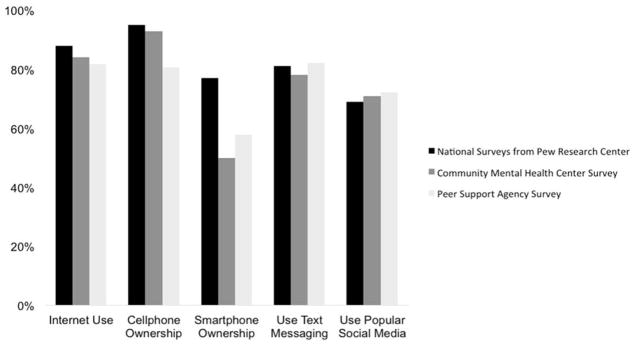
Figure 1 shows participants reported rates of internet, text messaging, and social media use compared to a survey of individuals with serious mental illness at community mental health centers and national surveys of technology use in the general adult population conducted by the Pew Research Center. Respondents with mental illness receiving services at PSAs and community mental health centers reported lower rates of smartphone ownership when compared to the general population. However, rates of other online and mobile technologies among PSA service users are comparable to adults in the general population.
Figure 1.
Technology Use Among PSA Respondents Compared to General Population and Community Mental Health Centersa,b
aData was obtained from a sample (n=70) of people living with serious mental illness surveyed in community mental health centers [10]
bNational survey data was obtained from the Pew Research Center reports on Internet, smartphone, and social media use [2, 3, 1]
Discussion
The objective of this study was to assess how individuals with mental illness who are PSA service users in one state use online and mobile technologies. Current knowledge about how people with mental illness use technology is based largely on research conducted with individuals recruited from clinical mental health treatment settings. However, over one million people with mental illness across the US participate in non-clinical self-help and consumer-run and consumer-controlled organizations [13]. The present study was a preliminary step in assessing the potential promise and possible challenges of disseminating scalable online and mobile technologies for promoting the health and well being of persons with mental illness in non-clinical peer support settings.
We found that most PSA users have access to online and mobile technologies, and report use of technology that is comparable to adults in the general population. These data are consistent with findings from prior surveys of technology use among adults with serious mental illness in formal mental health care treatment settings [20, 10, 21], which suggests that there may be comparable access to technology among individuals with mental illness who receive services at either PSAs or formal clinical settings. This is valuable insight because it suggests that emerging digital interventions aimed at supporting the health and mental health of individuals living with mental illness may have more widespread reach than previously considered, with potential applicability across both formal and informal settings.
While we found that smartphone ownership was lower among persons with mental illness compared to adults in the general population, this gap does not appear to be as wide among younger age groups given that sixty-seven percent of PSA users under age 55 reported owning a smartphone. These data add to mounting empirical evidence supporting the promise of using online and mobile technologies to reach individuals with mental illness, and provide a novel contribution by suggesting that online and mobile technologies may also be promising approaches for reaching those who receive services in non-traditional mental health settings.
There are many potential benefits of the internet as a source of information and support that are consistent with the philosophy and spirit of peer support services which embrace empowerment, shared decision making, and peer exchanges of information and social support [22]. We found that 71% of PSA respondents who used the internet had searched for health information online and 57% had searched for mental health information online. Thus, online health and mental health information-seeking behavior was moderately high among PSA service users, suggesting that online interventions that address health and mental health may be appealing to PSA consumers. While the Internet is the single largest source of information worldwide, the quality of health and mental health information online varies between sources [23]. In the future peers may play an important role in helping one another effectively use online health and mental health information sources and gain access to evidence-based online and mobile interventions that support health goals and promote well-being.
Social media is increasingly used as a platform for people with mental health conditions to share their illness experiences or seek advice from others with similar lived experiences with mental illness [24]. In the present study 72% of PSA respondents used social media: 77% used Facebook and 82% used YouTube. These rates are comparable to use of social media among persons with SMI reported in prior studies [10]. Research by our group and others has explored naturally occurring peer support among persons with mental illness on social media platforms [25, 26] and the feasibility and preliminary effectiveness of interventions that leverage social media to facilitate peer support for health behavior change in this population [24, 15, 27]. The majority of respondents (85%) to a survey of Twitter users who self-identified as having a mental illness expressed interest in mental health programs delivered through social media, especially to promote overall health and well-being (72%) and for coping with mental health symptoms (90%) [28]. There is significant potential for using social media as a platform for connecting PSA users who wish to engage in mutually beneficial support for accessing evidence-based health and mental health interventions.
Future research exploring the potential to intervene with online and mobile health technologies in PSAs and other consumer-operated services will need to consider the role of peers in the design, delivery, and evaluation of such interventions. Individuals often turn to peer support services seeking non-clinical, non-hierarchical and reciprocal support for recovery goals outside of or in addition to traditional mental health services. A challenge for the field will be to design effective ways to implement evidence-based health promotion and mental health interventions in PSAs and other consumer-operated services that acknowledges and leverages established peer relationships based on trust, respect, and mutual support. Peer navigators have played a role in helping people with mental illness gain access to formal health and mental health care services [29–31]. A peer technology navigator model implemented in PSAs may be useful for linking persons with mental illness to evidence-based online and mobile interventions in these non-clinical mental health settings. Future research should seek input from peer support stakeholders, including leadership, staff, and members, on feasible and desirable roles for peers in the delivery of technology based interventions to promote the health and well-being of persons with mental illness.
Limitations
The present report provides a snapshot of technology use among people with mental illness who use PSA services in non-clinical mental health settings in one state. The results should be interpreted with caution. PSA users who do not use technology or do not like it may have not completed the survey. Nonresponse bias among PSA users can negatively impact both the reliability and validity of survey study findings. Although PSAs are designed and funded to support people with diagnoses of mental illnesses, to maintain anonymity in our survey we did not obtain information about respondents’ mental health diagnoses or symptoms. Additionally, this survey was completed on computers or by paper located at the PSA. It is possible that respondents’ experience with computers and the internet is not representative of the entire population of people with mental illness who use peer support centers. However, since the survey could be completed either on paper or via computer, it is unlikely that respondents were more or less likely to be computer and Internet users than those who did not complete the survey. Finally, we did not explore privacy and security concerns among survey respondents even though these concerns may be a barrier to implementing online and mobile interventions at PSAs. Despite these limitations, the current study provides preliminary insight about technology use among people with mental illness who attend peer support agencies.
Conclusions
Many individuals who receive services at PSAs report having access to online and mobile technologies. Online and mobile technologies may be leveraged to expand the reach of evidence-based health and mental health promotion programs to individuals in these non-clinical mental health settings. Peers may play an important role in helping one another effectively use online health and mental health information sources and gain access to evidence-based technology interventions that support health goals and promote wellness. Future research should explore the feasibility and acceptability of intervention strategies that involve PSAs as a resource for linking people with mental illness to online and mobile interventions.
Acknowledgments
Funding: This study was supported in part by the Dartmouth Health Promotion and Disease Prevention Research Center supported by Cooperative Agreement Number U48DP005018 from the Centers for Disease Control and Prevention. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Conflict of Interest: The authors declare that they have no conflicts of interest.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- 1.Greenwood S, Perrin A, Duggan M. Social Media Update 2016. Washington, D. C: Pew Research Center; 2016. [Google Scholar]
- 2.Internet/Broadband Fact Sheet. Vol. 2017 Washington, D.C: Pew Research Center; 2017. Oct 22, [Google Scholar]
- 3.Mobile Fact Sheet. Washington, D. C: Pew Research Center; 2017. [Google Scholar]
- 4.Anderson M. Digital divide persists even as lower-income Americans make gains in tech adoption. Vol. 2017 Wasington, D. C: Pew Research Center; 2017. Mar 22, [Google Scholar]
- 5.Bonevski B, Randell M, Paul C, Chapman K, Twyman L, Bryant J, et al. Reaching the hard-to-reach: a systematic review of strategies for improving health and medical research with socially disadvantaged groups. BMC Medical Research Methodology. 2014;14:42. doi: 10.1186/1471-2288-14-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhugra D, Tasman A, Pathare S, Priebe S, Smith S, Torous J, et al. The WPA-Lancet Psychiatry Commission on the Future of Psychiatry. The Lancet Psychiatry. 2017;4(10):775–818. doi: 10.1016/s2215-0366(17)30333-4. [DOI] [PubMed] [Google Scholar]
- 7.Naslund JA, Aschbrenner KA, Araya R, Marsch LA, Unützer J, Patel V, et al. Digital technology for treating and preventing mental disorders in low-income and middle-income countries: a narrative review of the literature. The Lancet Psychiatry. 2017;4(6):486–500. doi: 10.1016/S2215-0366(17)30096-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Firth J, Cotter J, Torous J, Bucci S, Firth JA, Yung AR. Mobile Phone Ownership and Endorsement of “mHealth” Among People With Psychosis: A Meta-analysis of Cross-sectional Studies. Schizophrenia bulletin. 2016;42(2):448–55. doi: 10.1093/schbul/sbv132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Glick G, Druss B, Pina J, Lally C, Conde M. Use of mobile technology in a community mental health setting. Journal of telemedicine and telecare. 2016;22(7):430–5. doi: 10.1177/1357633x15613236. [DOI] [PubMed] [Google Scholar]
- 10.Naslund JA, Aschbrenner KA, Bartels SJ. How people with serious mental illness use smartphones, mobile apps, and social media. Psychiatric rehabilitation journal. 2016;39(4):364–7. doi: 10.1037/prj0000207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Naslund JA, Marsch LA, McHugo GJ, Bartels SJ. Emerging mHealth and eHealth interventions for serious mental illness: a review of the literature. Journal of mental health. 2015;24(5):321–32. doi: 10.3109/09638237.2015.1019054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tal A, Torous J. The digital mental health revolution: Opportunities and risks. Psychiatric rehabilitation journal. 2017;40(3):263–5. doi: 10.1037/prj0000285. [DOI] [PubMed] [Google Scholar]
- 13.Goldstrom ID, Campbell J, Rogers JA, Lambert DB, Blacklow B, Henderson MJ, et al. National estimates for mental health mutual support groups, self-help organizations, and consumer-operated services. Administration and policy in mental health. 2006;33(1):92–103. doi: 10.1007/s10488-005-0019-x. [DOI] [PubMed] [Google Scholar]
- 14.Segal SP, Hayes SL. Consumer-run services research and implications for mental health care. Epidemiology and psychiatric sciences. 2016;25(5):410–6. doi: 10.1017/s2045796016000287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Naslund JA, Aschbrenner KA, Marsch LA, Bartels SJ. Feasibility and acceptability of Facebook for health promotion among people with serious mental illness. Digital health. 2016:2. doi: 10.1177/2055207616654822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aschbrenner KA, Naslund JA, Bartels SJ. Technology-Supported Peer-to-Peer Intervention for People With Serious Mental Illness. Psychiatric services (Washington, DC) 2016;67(8):928–9. doi: 10.1176/appi.ps.670801. [DOI] [PubMed] [Google Scholar]
- 17.Brunette MF, Ferron JC, McHugo GJ, Davis KE, Devitt TS, Wilkness SM, et al. An electronic decision support system to motivate people with severe mental illnesses to quit smoking. Psychiatric services (Washington, DC) 2011;62(4):360–6. doi: 10.1176/ps.62.4.pss6204_0360. [DOI] [PubMed] [Google Scholar]
- 18.Brunette MF, Gunn W, Alvarez H, Finn PC, Geiger P, Ferron JC, et al. A pre-post pilot study of a brief, web-based intervention to engage disadvantaged smokers into cessation treatment. Addiction science & clinical practice. 2015;10:3. doi: 10.1186/s13722-015-0026-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brunette MF, Aschbrenner KA, Ferron JC, Ustinich L, Kelly M, Grinley T. Use of Computers and Internet Among People With Severe Mental Illnesses at Peer Support Centers. Psychiatric rehabilitation journal. 2017 doi: 10.1037/prj0000247. [DOI] [PubMed] [Google Scholar]
- 20.Glick G, Druss B, Pina J, Lally C, Conde M. Use of mobile technology in a community mental health setting. Journal of telemedicine and telecare. 2015 doi: 10.1177/1357633x15613236. [DOI] [PubMed] [Google Scholar]
- 21.Ben-Zeev D, Davis KE, Kaiser S, Krzsos I, Drake RE. Mobile technologies among people with serious mental illness: opportunities for future services. Administration and policy in mental health. 2013;40(4):340–3. doi: 10.1007/s10488-012-0424-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Villani M, Kovess-Masfety V. How Do People Experiencing Schizophrenia Spectrum Disorders or Other Psychotic Disorders Use the Internet to Get Information on Their Mental Health? Literature Review and Recommendations. JMIR Mental Health. 2017;4(1):e1. doi: 10.2196/mental.5946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fahy E, Hardikar R, Fox A, Mackay S. Quality of patient health information on the Internet: reviewing a complex and evolving landscape. The Australasian Medical Journal. 2014;7(1):24–8. doi: 10.4066/AMJ.2014.1900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Naslund JA, Aschbrenner KA, Marsch LA, Bartels SJ. The future of mental health care: peer-to-peer support and social media. Epidemiology and psychiatric sciences. 2016;25(2):113–22. doi: 10.1017/s2045796015001067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Naslund JA, Grande SW, Aschbrenner KA, Elwyn G. Naturally occurring peer support through social media: the experiences of individuals with severe mental illness using YouTube. PLoS One. 2014;9(10):e110171. doi: 10.1371/journal.pone.0110171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Parikh SV, Huniewicz P. E-health: an overview of the uses of the Internet, social media, apps, and websites for mood disorders. Current opinion in psychiatry. 2015;28(1):13–7. doi: 10.1097/yco.0000000000000123. [DOI] [PubMed] [Google Scholar]
- 27.Valimaki M, Athanasopoulou C, Lahti M, Adams CE. Effectiveness of Social Media Interventions for People With Schizophrenia: A Systematic Review and Meta-Analysis. Journal of medical Internet research. 2016;18(4):e92. doi: 10.2196/jmir.5385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Naslund JA, Aschbrenner KA, McHugo GJ, Unutzer J, Marsch LA, Bartels SJ. Exploring opportunities to support mental health care using social media: A survey of social media users with mental illness. Early intervention in psychiatry. 2017 doi: 10.1111/eip.12496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kelly E, Fulginiti A, Pahwa R, Tallen L, Duan L, Brekke JS. A pilot test of a peer navigator intervention for improving the health of individuals with serious mental illness. Community mental health journal. 2014;50(4):435–46. doi: 10.1007/s10597-013-9616-4. [DOI] [PubMed] [Google Scholar]
- 30.Corrigan PW, Pickett S, Schmidt A, Stellon E, Hantke E, Kraus D, et al. Peer navigators to promote engagement of homeless African Americans with serious mental illness in primary care. Psychiatry research. 2017;255:101–3. doi: 10.1016/j.psychres.2017.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Corrigan PW, Kraus DJ, Pickett SA, Schmidt A, Stellon E, Hantke E, et al. Using Peer Navigators to Address the Integrated Health Care Needs of Homeless African Americans With Serious Mental Illness. Psychiatric services (Washington, DC) 2017;68(3):264–70. doi: 10.1176/appi.ps.201600134. [DOI] [PMC free article] [PubMed] [Google Scholar]