Abstract
Objectives:
Hospital admission during early labor may increase women’s risk for medical and surgical interventions. However, it is unclear which diagnostic guideline is best suited for identifying the active phase of labor among parous women. Dr. Emanuel Friedman, the United Kingdom’s National Institute for Health and Care Excellence (NICE), and the American College of Obstetricians and Gynecologists/Society for Maternal-Fetal Medicine (ACOG/SMFM) support different active labor diagnostic guidelines. Our aims were 1) to determine the proportions of parous women admitted to the hospital before or in active labor per these leading guidelines and 2) to compare associations of labor status at admission (i.e., early labor or active labor) with oxytocin augmentation, cesarean birth, and adverse birth outcomes when using the different active labor diagnostic guidelines.
Design:
Active labor diagnostic guidelines were applied retrospectively to cervical examination data. Binomial logistic regression was used to assess associations of labor status at admission (i.e., early labor relative to active labor) and outcomes.
Setting:
A large, academic, tertiary medical center in the Midwestern United States.
Participants:
Parous women with spontaneous labor onset who gave birth to a single, cephalic-presenting fetus at term gestation between 2006 and 2010 (n = 3,219).
Findings:
At admission, 28.8%, 71.9%, and 24.4% of parous women were in active labor per Friedman, NICE, and ACOG/SMFM diagnostic guidelines, respectively. Oxytocin augmentation was more likely among women admitted in early labor, regardless of the diagnostic strategy used (p<0.001 for each guideline). Cesarean birth was also more likely among women admitted before versus in active labor according to all guidelines (Friedman: adjusted odds ratio [AOR] 3.63 [95% CI 1.46–9.03]), NICE: AOR 2.71 [95% CI 1.47–4.99]), and ACOG/SMFM: AOR 2.11 [95% CI 1.02–4.34]). There were no differences in a composite measure of adverse outcomes within active labor diagnostic guidelines after adjusting for covariates.
Key Conclusions:
Many parous women with spontaneous labor onset are admitted to the hospital before active labor. These women are more likely to receive oxytocin augmentation during labor and are more likely to have a cesarean birth.
Implications for Practice:
Diagnosing active labor prior to admission or prior to intervention aimed at speeding labor after admission may decrease likelihoods for primary cesarean births. The NICE dilation-rate based active labor diagnostic guideline is more inclusive than Friedman or ACOG/SMFM guidelines and its use may be the most clinically-useful for improving the likelihood of vaginal birth among parous women.
Keywords: Cesarean Section, Labor Onset, Labor Stage, First, Oxytocin, Parity, Parturition
INTRODUCTION
Support of normal physiologic childbirth is a tenet of midwifery (International Confederation of Midwives, 2014). The timing of admission to the hospital for a woman with spontaneous labor onset may affect her opportunity for physiologic birth by influencing the interventions she receives during childbirth. Admission early in labor increases likelihoods for intrapartum pharmaceutical and surgical intervention (Bailit et al., 2005; Neal et al., 2017; Neal et al., 2014). The American College of Obstetricians and Gynecologists (2017) recently recommended delaying labor admission for women with reassuring status until active labor begins to improve their opportunity for vaginal birth.
The three most prominent active labor diagnostic guidelines for parous women come from Dr. Emanuel Friedman (1956, 1978), the United Kingdom’s National Institute for Health and Care Excellence (NICE; 2014), and the American College of Obstetricians and Gynecologists/Society for Maternal-Fetal Medicine (ACOG/SMFM) (Caughey et al., 2014). Friedman introduced his approach to the graphic analysis of labor progress among parous women in the mid-1950s (Friedman, 1956). Active labor onset was determined individually for each woman based on progressively more rapid dilation until a maximum slope of dilation was reached, most commonly between 2 and 3 cm (Friedman, 1978; Friedman and Kroll, 1969; Friedman, 1956); the lower limit of normal progress for the majority of active labor was 1.5 cm per hour (Friedman, 1978; Friedman, 1956). The NICE guideline stipulates that active labor can be diagnosed when cervical dilation is progressive from 4 cm or more (National Institute for Health and Care Excellence, 2014). A dilation rate of 2 cm in 4 hours was presented as the lower limit of normal active labor progress. ACOG and the SMFM have jointly endorsed 6 cm dilatation as the threshold for active labor onset for most women as a strategy for safely decreasing the primary cesarean birth rate in the United States and standards for active labor progress should not be applied before this point (Caughey et al., 2014).
The value and use of these various active labor diagnostic guidelines has been explored in a group of nulliparous women with spontaneous labor onset (Neal et al., 2017). Significantly more women met the NICE active labor guideline at the time of hospital admission than met Friedman or ACOG/SMFM guidelines (Neal et al., 2017). The NICE guideline distinguished likelihoods for cesarean birth better than the other guidelines, with women admitted before versus in active labor being more likely to experience cesarean birth (adjusted odds ratio (AOR) 2.55; 95% CI 1.84–3.53; p < 0.001) (Neal et al., 2017). However, which of these guidelines is best suited for clinical use for women with prior births remains unclear.
The aims of our study were (1) to retrospectively determine the proportion of parous women admitted to the hospital before and in active labor when applying Friedman, NICE, and ACOG/SMFM diagnostic guidelines, and (2) to compare associations of labor status at admission (i.e., early labor or active labor) with oxytocin augmentation, cesarean birth, and adverse birth outcomes when using the different active labor diagnostic guidelines.
METHODS
We developed a database of all births between January 1, 2006 and December 31, 2010 at a large, academic, tertiary medical center in the Midwestern United States (N = 21,492). Institutional Review Board approval was obtained for this study and a full waiver of informed consent was granted for data collection. Detailed data were extracted from women’s electronic health records including demographics, medical history, reproductive and prenatal history, labor and birth summary, postpartum and discharge information, newborn information, and International Classification of Diseases-9 codes. Data on labor progression included timestamped cervical dilatation, station, and effacement. Cervical examinations were most often performed by resident physicians who would subsequently contact the attending physician for admission or labor management decisions. Continuous electronic fetal monitoring during labor is predominantly used for fetal assessment at this institution while intermittent auscultation is used rarely. Data cleaning, coding, and logic checking were performed.
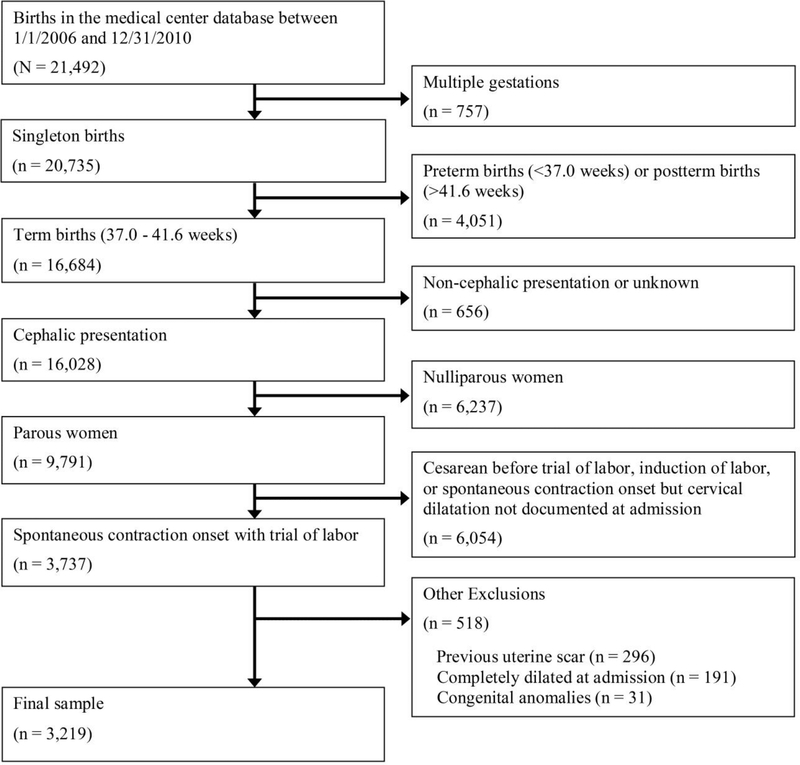
Figure 1 depicts the sample selection process for this study. The sample included 3,219 parous women admitted to the hospital for the indication of spontaneous labor onset and a trial of labor who gave birth to a single, cephalic-presenting fetus at term gestation (37.0 – 41.6 weeks). We defined trial of labor as all vaginal births, cesarean births following labor augmentation, and all other cesarean births with at least two cervical examinations from the time of admission, unless there was documentation that a trial of labor was not attempted. Women with a multiple gestation, preterm or postterm pregnancy, fetus in a non-cephalic or unknown presentation, no prior birth, induction of labor, cesarean birth before a trial of labor, completely dilated cervix at admission, or a fetus with a congenital anomaly were excluded. The dilatation documented at admission served as the baseline value for our retrospective determination if a woman was admitted in active labor per Friedman, NICE, and/or ACOG/SMFM diagnostic guidelines. See Table 1 for a description of the various guidelines.
Figure 1.
Diagram of patient selection.
Table 1.
Operationalized active labor diagnostic criteria for labor state categorization at hospital admission.
| Source | Diagnostic criteria |
|---|---|
| Friedman (1956, 1978) | Cervical dilation rate ≥ 1.5 cm/hour during the first hour after admission that led to dilatation ≥ 3 cm, or progression from an earlier dilatation to complete dilatation within 1 hour of admissiona |
| National Institute for Health and Care Excellence (2014) | Cervical dilation rate ≥ 2 cm in 4 hours (≥ 0.5 cm/hour, on average) post admission that led to dilatation ≥ 4 cm, or progression from an earlier dilatation to complete dilatation within 4 hours of admissionb |
| American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine (Caughey et al., 2014) | Cervical dilatation ≥ 6 cm but not completely dilated and regular uterine contractions at admission |
Slope calculations based on cervical exams immediately prior to and after the 1-hour post-admission time point were used to approximate cervical dilatation (cm) at the 1-hour time point, unless an exam was performed exactly 1 hour after admission. The dilation slope (cm/hour) during the first hour post-admission was then calculated for each woman to determine if she was in active labor.
Slope calculations based on cervical exams immediately prior to and after the 4-hour post-admission time point were used to approximate cervical dilatation (cm) at the 4-hour time point, unless an exam was performed exactly 4 hours after admission. The dilation slope (cm/hour) during the first 4 hours postadmission was then calculated for each woman to determine if she was in active labor.
Frequencies and percentages were used to describe the number of women who were admitted in early labor and in active labor per the three diagnostic guidelines. Labor interventions and birth outcomes were compared using Mann-Whitney U tests for continuous-level data and likelihood ratio tests for categorical-level data. A composite of adverse outcomes was created due to the large sample sizes needed to separately study each outcome. The composite adverse outcome was defined as the presence of an adverse maternal outcome (i.e., maternal fever during labor > 100.4° F; and/or postpartum hemorrhage (> 500 ml for vaginal birth and > 1000 ml for cesarean birth) or an adverse neonatal outcome (i.e., neonatal resuscitation at birth using endotracheal artificial respiration, cardiac compression, and/ or administration of buffers or other resuscitative medications; Apgar score < 7 at 5 minutes; umbilical cord arterial blood pH < 7.1; and/or admission to the neonatal intensive care unit).
Binomial logistic regression was used to assess associations of labor status at admission (i.e., early labor relative to active labor) with oxytocin augmentation, cesarean birth, and the composite adverse outcome. All models were adjusted for maternal age, race, body mass index, gestational age at labor admission, and epidural analgesia use. Models for cesarean birth were also adjusted for hypertensive disorders, diabetes mellitus, oxytocin augmentation, use of amniotomy, and neonatal weight. Finally, models for composite adverse outcome were adjusted for all of the abovementioned variables as well as duration of amniotic membrane rupture and mode of birth. Comparisons of this sample were not made between-guidelines (e.g., women admitted in active labor per the NICE guideline compared to women admitted in active labor per the ACOG/SMFM guideline) because too few women admitted in active labor experienced adverse outcomes (e.g., cesarean birth, composite adverse outcome) to provide meaningful comparisons. Statistical analyses were performed using IBM SPSS Statistics 23 (IBM Corporation, Armonk, NY) and Stata/SE 14.0 (StataCorp LP, College Station, TX). A critical alpha of 0.05 was used for determining statistical significance.
RESULTS
There were 3,219 parous women who met inclusion criteria. Study sample characteristics are presented in Table 2. Rates for amniotomy and oxytocin augmentation were 61.8% and 32.6%, respectively. The cesarean rate was 2.9% (n = 94). An adverse maternal outcome was experienced by 2.8% of women, and an adverse neonatal outcome occurred in 2.4% of births. There were no maternal or neonatal deaths.
Table 2.
Characteristics of parous women with spontaneous labor onset and a trial of labor who gave birth to a single, cephalic-presenting fetus at term gestation from 2006–2010 at [location of study removed per author instructions for blind review] (N = 3,219).
| Characteristic | n (%) or median [5th, 95th percentile] |
|---|---|
| Maternal age (y) | 28 [20, 38] |
| Race | |
| White, non-Hispanic | 1257 (39.0%) |
| Black, non-Hispanic | 1225 (38.1%) |
| Hispanic | 441 (13.7%) |
| Asian/Pacific Islander | 147 (4.6%) |
| Others | 149 (4.6%) |
| Education (highest level) | |
| Post-graduate degree | 267 (8.3%) |
| College graduate | 551 (17.1%) |
| High school graduate | 1253 (38.9%) |
| High school not completed | 866 (26.9%) |
| Not reported | 282 (8.8%) |
| Marital status | |
| Married | 1514 (47.0%) |
| Not married | 1705 (53.0%) |
| Health Insurance | |
| Private | 1085 (33.7%) |
| Public | 1841 (57.2%) |
| Other | 293 (9.1%) |
| Body mass index at labor admission (kg/m2) | 29.2 [22.9, 41.1] |
| Gravidity | 3 [2, 7] |
| Parity | 1 [1, 4] |
| Cervical dilatation at admission (cm) | 4.5 [2.0, 8.0] |
| Cervical effacement at admission (%) | 80 [50, 100] |
| Fetal station at admission | -2 [−3, 0] |
| Amniotomy | 1990 (61.8%) |
| Oxytocin augmentation used | 1049 (32.6%) |
| Epidural analgesia used during labor | 2152 (66.9%) |
| Fetal scalp electrode used | 957 (29.7%) |
| Intrauterine contraction monitor used | 892 (27.7%) |
| Number of cervical exams during labor | 5 [2, 9] |
| Mode of birth | |
| Vaginal - spontaneous | 2893 (89.9%) |
| Vaginal - instrumental | 232 (7.2%) |
| Cesarean | 94 (2.9%) |
| In-hospital labor duration (h) | 5.2 [0.8, 12.6] |
| Duration of membrane rupture (h) | 2.2 [0.1, 11.8] |
| Gestational age at birth (wk) | 39.3 [37.4, 40.7] |
| Birth weight (g) | 3316 [2666, 4065] |
On admission to the hospital in spontaneous labor, 28.8%, 71.9%, and 24.4% of women were in active labor per Friedman, NICE, and ACOG/SMFM diagnostic guidelines, respectively (Table 3). Thus, 28.1% of parous women were admitted to the hospital prior to active labor per the NICE guideline which was, by far, the most inclusive active labor guideline of the three (i.e., the guideline met by the most women); in comparison, 75.6% and 71.2% of women were admitted in early labor when using ACOG/SMFM and Friedman guidelines. Among women admitted prior to 6 cm dilatation (75.6%) (ACOG/SMFM guideline), 19.5% were in active labor per Friedman’s guideline and 65.0% were in active labor per the NICE guideline. Among the 24.4% of women admitted at 6 cm or more, 57.4% and 91.5% were in active labor per these respective guidelines. As compared to women in active labor at admission, the time duration from labor admission until birth among women admitted in early labor was between 4 to 5 hours longer, regardless of the active labor diagnostic guideline used (p < 0.001).
Table 3.
Labor interventions and outcomes for women admitted to the hospital in early labor or active labor based on Friedman, NICE, and ACOG/SMFM guidelines from 2006–2010 at [location of study removed per author instructions for blind review] (N = 3,219).
| Friedman guideline (n = 3,214)a | NICE guideline (n = 3,200)b | ACOG/SMFM guideline (n = 3,219) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Early | Active | P | Early | Active | P | Early | Active | P | |
| Labor | Labor | Labor | Labor | Labor | Labor | ||||
| (n = 2,287) | (n = 927) | (n = 900) | (n = 2,300) | (n = 2,432) | (n = 787) | ||||
| (71.2%) | (28.8%) | (28.1%) | (71.9%) | (75.6%) | (24.4%) | ||||
| In-hospital labor duration (h) | 6.4 [2.7, 13.6] | 1.8 [0.4, 6.7] | <0.001 | 8.8 [5.4, 15.9] | 3.9 [0.7, 8.7] | <0.001 | 6.1 [1.8, 13.4] | 2.1 [0.4, 6.9] | <0.001 |
| Amniotomy | 1502 (65.7%) | 485 (52.3%) | <0.001 | 610 (67.8%) | 1367 (59.4%) | <0.001 | 1488 (61.2%) | 502 (63.8%) | NS |
| Oxytocin augmentation used | 974 (42.6%) | 74 (8.0%) | <0.001 | 587 (65.2%) | 456 (19.8%) | <0.001 | 972 (40.0%) | 77 (9.8%) | <0.001 |
| Epidural analgesia used Mode of birth | 1780 (77.8%) | 370 (39.9%) | <0.001 | 751 (83.4%) | 1391 (60.5%) | <0.001 | 1818 (74.8%) | 334 (42.4%) | <0.001 |
| Vaginal - spontaneous | 2035 (89.0%) | 858 (92.6%) | <0.001c | 788 (87.6%) | 2105 (91.5%) | <0.001c | 2165 (89.0%) | 728 (92.5%) | <0.01c |
| Vaginal - instrumental | 171 (7.5%) | 61 (6.6%) | 70 (7.8%) | 162 (7.0%) | 185 (7.6%) | 47 (6.0%) | |||
| Cesarean | 81 (3.5%) | 8 (0.9%) | 42 (4.7%) | 33 (1.4%) | 82 (3.4%) | 12 (1.5%) | |||
| Indication for cesarean | |||||||||
| Dystocia (1st stage) | 30 (37.0%) | 2 (25.0%) | NS | 19 (45.2%) | 11 (33.3%) | NS | 30 (36.6%) | 2 (16.7%) | NS |
| Arrest of fetal descent (2nd stage) | 6 (7.4%) | 2 (25.0%) | 3 (7.1%) | 5 (15.2%) | 6 (7.3%) | 2 (16.7%) | |||
| Non-reassuring fetal status | 43 (53.1%) | 4 (50.0%) | 19 (45.2%) | 17 (51.5%) | 44 (53.7%) | 7 (58.3%) | |||
| Otherd | 2 (2.5%) | 0 (0%) | 1 (2.4%) | 0 (0%) | 2 (2.4%) | 1 (8.3%) | |||
| Adverse maternal outcomee | 68 (3.0%) | 22 (2.4%) | NS | 41 (4.6%) | 48 (2.1%) | <0.001 | 73 (3.0%) | 17 (2.2%) | NS |
| Adverse neonatal outcomef | 58 (2.5%) | 17 (1.8%) | NS | 23 (2.6%) | 50 (2.2%) | NS | 63 (2.6%) | 14 (1.8%) | NS |
Data are n (%) or median [5th, 95 th percentile]. Percentages may not add to 100% due to rounding. Mann-Whitney U tests performed for continuous level data comparisons due to nonnormal distributions (Kolmogorov-Smirnov test for normality < 0.001). Likelihood ratio tests were performed for categorical level data comparisons. NS = Not statistically significant.
Women delivered by cesarean before the 1-hour assessment point and before complete dilatation were not included in analyses because there was insufficient time for labor status determination (n = 5).
Women delivered by cesarean before the 4-hour assessment point and before complete dilatation were not included in analyses because there was insufficient time for labor status determination (n = 19).
Among women admitted in active labor, likelihood for spontaneous vaginal birth was greater and likelihood for cesarean birth was lower (p < 0.05 after Bonferroni correction).
Umbilical cord prolapse, n = 1; placental abruption, n = 1; suspected macrosomia, n = 1.
Defined as fever during labor > 100.4° F and/or postpartum hemorrhage (i.e., > 500 ml for vaginal birth and > 1000 ml for cesarean birth).
Defined as neonatal resuscitation at birth, Apgar score < 7 at 5 minutes, umbilical cord arterial blood pH < 7.1 (if collected), and/or admission to the neonatal intensive care unit. Umbilical cord arterial blood pH collected from 633 (19.7%) women.
The distributions and within-guideline comparisons of labor interventions and birth outcomes for women admitted to the hospital in early and active labor per ACOG/SMFM, Friedman, and NICE guidelines are presented in Table 3. Unadjusted and adjusted odds (AOR) of oxytocin augmentation, cesarean birth, and composite adverse outcome are in Table 4. Oxytocin for augmentation of labor was more likely among women admitted in early labor, regardless of diagnostic guideline applied (p < 0.001 for each within-guideline contrast). Specifically, oxytocin was received by 42.6%, 65.2%, and 40.0% of parous women admitted before active labor per Friedman, NICE, and ACOG/SMFM guidelines, respectively; among women admitted in active labor per these guidelines, 8.0%, 19.8%, and 9.8%, received oxytocin.
Table 4.
Unadjusted and adjusted odds of oxytocin use, cesarean birth, and composite adverse outcome for women admitted in early labor relative to active labor based on Friedman, NICE, and ACOG/SMFM guidelines from 2006–2010 at [location of study removed per author instructions for blind review] (N = 3,219).
| Group Contrasts | Oxytocin Use | Cesarean | Composite Adverse Outcomea | |||
|---|---|---|---|---|---|---|
| Unadjusted OR (95% CI) | Adjusted OR (95% CI)b | Unadjusted OR (95% CI) | Adjusted OR (95% CI)c | Unadjusted OR (95% CI) | Adjusted OR (95% CI)d | |
| Friedman EL vs. AL | 8.55 (6.64, 11.01)*** | 7.02 (5.31, 9.29)*** | 4.22 (2.03, 8.76)*** | 3.63 (1.46, 9.03)** | 1.31 (0.90, 1.90) | 0.93 (0.59, 1.46) |
| ACOG/SMFM EL vs. AL | 7.58 (6.39, 9.00)*** | 6.53 (5.44, 7.84)*** | 3.36 (2.12, 5.34)*** | 2.71 (1.47, 4.99)*** | 1.59 (1.14, 2.22)** | 1.34 (0.92, 1.94) |
| ACOG/SMFM EL vs. AL | 6.14 (4.79, 7.87)*** | 4.69 (3.61, 6.09)*** | 2.25 (1.22, 4.15)** | 2.11 (1.02, 4.34)* | 1.44 (0.95, 2.18) | 1.29 (0.81, 2.03) |
Data are Odds Ratio (OR) (95th % Confidence Interval). The Active Labor group is the reference group.
AL, Active Labor. EL, Early Labor.
p < 0.05;
p < 0.01;
p < 0.001.
Defined as adverse maternal outcome (i.e., fever during labor > 100.4° F and/or postpartum hemorrhage > 500 ml for vaginal birth and > 1000 ml for cesarean birth) and/or adverse neonatal outcome (i.e., neonatal resuscitation at birth, Apgar score < 7 at 5 minutes, umbilical cord arterial blood pH < 7.1 (if collected), and/or admission to the neonatal intensive care unit). Umbilical cord arterial blood pH collected from 633 (19.7%) women.
Adjusted for maternal age, race, body mass index, gestational age at labor admission, and epidural analgesia use.
Adjusted for maternal age, race, body mass index, hypertensive disorder, diabetes mellitus, gestational age at labor admission, oxytocin augmentation, use of amniotomy, epidural analgesia use, and neonatal weight.
Adjusted for maternal age, race, body mass index, hypertensive disorder, diabetes mellitus, gestational age at labor admission, oxytocin augmentation, use of amniotomy, epidural analgesia use, duration of amniotic membrane rupture, mode of birth, and neonatal weight.
Cesarean birth rates were 3.5%, 4.7%, and 3.4% among parous women admitted in early labor per Friedman, NICE, and ACOG/SMFM guidelines, respectively, and 0.9%, 1.4%, and 1.5% for women admitted in active labor per these guidelines (Table 3). For all guidelines, the likelihood for cesarean birth was higher among women admitted prior to active labor, as contrasted against women admitted in active labor (Table 4). The greatest difference in cesarean rates between women admitted in active versus early labor was found using the NICE guideline. There were no differences in composite adverse outcomes within active labor diagnostic strategies after adjusting for demographic, obstetrical, and neonatal covariates (Table 4).
DISCUSSION
A clinically-useful active labor diagnostic guideline ideally should be inclusive of most women early enough to allow for timely identification and treatment of abnormal active labor progress (Neal et al., 2017). However, the guideline should remain grounded in evidence so that women truly in early labor are not prematurely determined to be in active labor and subsequently held to active labor progress expectations. Likewise, an ideal guideline should not be so stringent that a significant number of laboring women never meet guideline criteria during labor despite progressively advancing in labor and birthing vaginally. The chosen active labor diagnostic guideline should be consistently applied by clinicians when differentiating active labor from earlier labor.
In our study, more than 70% of women were admitted in active labor when NICE active labor criteria were applied, whereas less than 30% of women were admitted in active labor when Friedman or ACOG/SMFM guidelines were used. Friedman’s dilation rate-based guideline (i.e., ≥ 1.5 cm/hour during the first hour after admission) was still not met by 42.6% of parous women who were admitted at 6 cm dilatation or more. Indeed, a large percentage of women will never achieve Friedman active labor dilation rate expectations (Zhang et al., 2010); yet, most parous women will achieve a vaginal birth with normal maternal and neonatal outcomes.
Oxytocin augmentation and cesarean birth rates were increased for those admitted in early versus active labor with each active labor diagnostic guideline. This indicates that timing of hospital admission may be an important predictor of intrapartum intervention and route of birth for parous women with spontaneous labor onset.
The overall cesarean rate in our study of parous women with one or more prior vaginal births and without a prior cesarean was only 2.9%. This indicates that a previous vaginal birth is a strong predictor of subsequent vaginal birth following a trial of labor (Bovbjerg et al., 2017). The NICE guideline showed the greatest difference in cesarean rates between women in our sample who were admitted to the hospital in active versus early labor (1.4% and 4.7%, respectively). Although women admitted in active labor per the ACOG/SMFM guideline (i.e., at 6 cm dilatation or more) had a lower cesarean rate compared to those not at 6 cm (1.5% and 3.4%, respectively), this finding represented the smallest difference in cesarean rates between early labor and active labor groups among the three guidelines evaluated. Prospective studies are needed to evaluate if the NICE guideline is the best approach for distinguishing between likelihoods for cesarean birth among parous women admitted before or in active labor. Studies of parous women undergoing induction of labor are also warranted to evaluate if carefully distinguishing between early induction efforts and active labor improves clinician management and birth outcomes.
Physiologic differences between women in early and active labor may partially explain why cesarean birth is more likely among women admitted earlier (Neal et al., 2017). Labor is an inflammatory event requiring maternal peripheral leukocytes to propagate labor events (Shynlova et al., 2013; Yuan et al., 2009), and women admitted before active labor onset have been shown to be earlier in the labor-associated inflammatory pathway than women admitted in active labor (Neal et al., 2015). Therefore, just as women undergoing induction of labor with an unfavorable cervix have higher cesarean birth rates than women with a favorable cervix (Laughon et al., 2012), women admitted to hospitals in early labor may have higher cesarean rates than women admitted in active labor because physiological changes important to successful labor are less mature (Neal et al., 2017).
There may also be macro-level differences between women who present to hospitals earlier in labor and those who present in active labor that influence birth outcomes (Neal et al., 2017). For example, women presenting earlier may have poor support systems, housing that prevents privacy, lower coping abilities, or physiological differences that may influence labor progression (Carlson et al., 2015; Kawakita et al., 2016; Wray, 2015). Alternatively, higher cesarean birth rates among women admitted to hospitals before active labor may occur simply due to increased time in the medical environment that could lead to higher rates of intervention related to institutional factors. This supports that systems factors, rather than exclusively patient factors, affect birth outcomes and should therefore be examined in maternity care improvement initiatives (Jolles, 2017; Kozhimannil et al., 2017).
Regardless if labor abnormalities result in early presentation to the hospital and subsequent provider intervention or if early presentation and subsequent intervention are the cause of labor abnormalities (Bailit et al., 2005), using a standard, evidence-based approach for diagnosing active labor will aid clinicians in differentiating early from active labor for all women (Neal et al., 2017). Active labor is an appropriate time for admission for women desiring inhospital birth (American College of Obstetricians and Gynecologists, 2017). Women presenting to the hospital in early labor with uncomplicated pregnancies and effective coping may be candidates for in-hospital early labor lounge observation or discharge to home until labor becomes active (Paul et al., 2017). Emerging evidence also suggests that low-risk women might be prepared antenatally to increase coping at home during latent labor, thus delaying hospital admission until active labor (Tilden et al., 2016). Finally, for women admitted to the hospital prior to active labor for legitimate clinical rationale (e.g., pain management, fatigue, severe anxiety, inadequate social support), the active labor diagnostic guideline can guide when progressive cervical dilation should first be expected to prevent premature intervention.
Parous women presenting to the hospital prior to active labor should be counseled on the risks of immediate admission, including more frequent oxytocin augmentation and cesarean births. Research aimed at describing physiological, social, and psychological differences among women admitted to hospitals in pre-active and active labor admission groups would be valuable scientific contributions. Prospective research aimed at evaluating if delaying hospital admission until active labor improves birth outcomes for parous women is also needed.
There were several study limitations. First, the study was a retrospective data analysis of medical record data from a single, large, academic medical center. Timing and frequency of cervical examinations, determinations for labor admission and interventions during labor (e.g., oxytocin augmentation), and diagnostic definitions (e.g., dystocia) were not standardized. These decisions were likely influenced by expectations of labor progress among clinicians at this institution. We were not privy to clinical decision-making processes in this retrospective study. Second, we applied active labor diagnostic guidelines to women admitted in spontaneous labor. Ideally, active labor diagnosis should be made during triage before the woman is officially admitted to the hospital or, at least, before intervention unless there is a maternal or fetal indication for intervention. In our study, some women may have received oxytocin augmentation prior to completion of the 4-hour NICE active labor determination period or even prior to completion of the 1-hour Friedman active labor determination period. This early intervention may have altered natural labor progression and active labor categorization. Finally, labor care at the study institution was predominantly provided within a medical model by resident and attending physicians, thus, findings may not generalize to midwifery models of care.
In summary, more than twice as many parous women with spontaneous labor onset meet the dilation rate-based NICE active labor diagnostic guideline at the time of hospital admission than either Friedman or ACOG/SMFM guidelines. This greater inclusiveness is a function of less stringent diagnostic criteria. Still, the NICE guideline differentiates likelihoods for cesarean birth between women admitted in early versus active labor as well as or better than other guidelines. Regardless of the active labor diagnostic guideline applied, oxytocin augmentation and cesarean birth were more likely among women admitted before active labor. To improve cesarean rates, it is reasonable for clinicians to delay hospital admission for low-risk women in spontaneous labor until active labor is established using the NICE guidelines; instead encouraging women to stay home longer or utilize early labor lounges until labor is established. Prospective research is needed to assess if delaying hospital admission for low-risk women until active labor begins decreases primary cesarean birth rates among parous women.
ACKNOWLEDGEMENTS:
The authors kindly acknowledge the database development support received from Ms. Tara Borlawsky-Payne, MA, Adjunct Instructor within The Ohio State University Department of Biomedical Informatics, Columbus, Ohio and Mr. Vipin Moolchandani from the Information Warehouse at The Ohio State University Wexner Medical Center, Columbus, Ohio.
Dr. Julia Phillippi was supported by grant number K08HS024733 from the Agency for Healthcare Research and Quality during manuscript production. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Dr. Nicole Carlson was supported by grant number K01NR016984 from the National Institute of Nursing Research during manuscript production.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- American College of Obstetricians and Gynecologists, 2017. Committee Opinion No. 687: Approaches to limit intervention during labor and birth. Obstetrics and gynecology 129, e20–8. [DOI] [PubMed] [Google Scholar]
- Bailit JL, Dierker L, Blanchard MH, Mercer BM, 2005. Outcomes of women presenting in active versus latent phase of spontaneous labor. Obstetrics and gynecology 105, 77–9. [DOI] [PubMed] [Google Scholar]
- Bovbjerg ML, Cheyney M, Brown J, Cox KJ, Leeman L, 2017. Perspectives on risk: Assessment of risk profiles and outcomes among women planning community birth in the United States. Birth (Berkeley, Calif.) 44, 209–21. [DOI] [PubMed] [Google Scholar]
- Carlson NS, Hernandez TL, Hurt KJ, 2015. Parturition dysfunction in obesity: time to target the pathobiology. Reproductive biology and endocrinology : RB&E 13, 135,015–0129–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caughey AB, Cahill AG, Guise J, Rouse DJ, 2014. Safe prevention of the primary cesarean delivery. American Journal of Obstetrics and Gynecology 210, 179–93. [DOI] [PubMed] [Google Scholar]
- Friedman EA (Ed.), 1978. Labor: Clinical Evaluation and Management. Appleton-Century-Crofts, New York. [Google Scholar]
- Friedman EA, Kroll BH, 1969. Computer analysis of labour progression. The Journal of obstetrics and gynaecology of the British Commonwealth 76, 1075–9. [DOI] [PubMed] [Google Scholar]
- Friedman EA, 1956. Labor in multiparas: a graphicostatistical analysis. Obstetrics and gynecology 8, 691–703. [PubMed] [Google Scholar]
- International Confederation of Midwives, 2014. Position statement: Keeping birth normal.
- Jolles DR, 2017. Unwarranted variation in utilization of cesarean birth among low-risk childbearing women. Journal of midwifery & women’s health 62, 49–57. [DOI] [PubMed] [Google Scholar]
- Kawakita T, Reddy UM, Landy HJ, Iqbal SN, Huang CC, Grantz KL, 2016. Indications for primary cesarean delivery relative to body mass index. American Journal of Obstetrics and Gynecology 215, 515.e1, 515.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozhimannil KB, Hardeman RR, Henning-Smith C, 2017. Maternity care access, quality, and outcomes: A systems-level perspective on research, clinical, and policy needs. Seminars in perinatology 41, 367–74. [DOI] [PubMed] [Google Scholar]
- Laughon SK, Zhang J, Grewal J, Sundaram R, Beaver J, Reddy UM, 2012. Induction of labor in a contemporary obstetric cohort. American Journal of Obstetrics and Gynecology 206, 486.e1,486.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence., 2014. Intrapartum care: care of healthy women and their babies during childbirth. NICE clinical guideline 190. http://www.nice.org.uk/guidance/cg190. Accessed July 1 2017. [PubMed]
- Neal JL, Lamp JM, Lowe NK, Gillespie SL, Sinnott LT, McCarthy DO, 2015. Differences in inflammatory markers between nulliparous women admitted to hospitals in preactive vs active labor. American Journal of Obstetrics and Gynecology 212, 68.e1,68.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neal JL, Lowe NK, Phillippi JC, Ryan SL, Knupp AM, Dietrich MS, Thung SF, 2017. Likelihood of cesarean delivery after applying leading active labor diagnostic guidelines. Birth (Berkeley, Calif.) 44, 128–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neal JL, Lamp JM, Buck JS, Lowe NK, Gillespie SL, Ryan SL, 2014. Outcomes of nulliparous women with spontaneous labor onset admitted to hospitals in preactive versus active labor. Journal of midwifery & women’s health 59, 28–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul JA, Yount SM, Breman RB, LeClair M, Keiran DM, Landry N, Dever K, 2017. Use of an early labor lounge to promote admission in active labor. Journal of midwifery & women’s health 62, 204–9. [DOI] [PubMed] [Google Scholar]
- Shynlova O, Lee Y, Srikhajon K, Lye SJ, 2013. Physiologic uterine inflammation and labor onset: integration of endocrine and mechanical signals. Reproductive Sciences (Thousand Oaks, Calif.) 20, 154–67. [DOI] [PubMed] [Google Scholar]
- Tilden EL, Emeis CL, Caughey AB, Weinstein SR, Futernick SB, Lee CS, 2016. The Influence of group versus individual prenatal care on phase of labor at hospital admission. Journal of midwifery & women’s health 61, 427–34. [DOI] [PubMed] [Google Scholar]
- Wray S, 2015. Insights from physiology into myometrial function and dysfunction. Experimental physiology 100, 1468–76. [DOI] [PubMed] [Google Scholar]
- Yuan M, Jordan F, McInnes IB, Harnett MM, Norman JE, 2009. Leukocytes are primed in peripheral blood for activation during term and preterm labour. Molecular human reproduction 15, 713–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J, Landy HJ, Branch DW, Burkman R, Haberman S, Gregory KD, Hatjis CG, Ramirez MM, Bailit JL, Gonzalez-Quintero V, Hibbard JU, Hoffman MK, Kominiarek M, Learman LA, Van Veldhuisen P, Troendle J, Reddy UM, 2010. Contemporary patterns of spontaneous labor with normal neonatal outcomes. Obstetrics and gynecology 116, 1281–7. [DOI] [PMC free article] [PubMed] [Google Scholar]