Abstract
Objective:
To characterize physical activity (PA) in individuals with rheumatoid arthritis (RA) and determine the associations between PA participation in light to moderate intensities and cardiovascular risk factors, disability, and disease activity.
Methods:
Cross-sectional study using data from two RA cohorts. PA was measured using an accelerometry-based activity monitor, and characterized as minutes/day in sedentary (≤1 metabolic equivalent-MET), very light (1.1–1.9 METs), light (2–2.9 METs), and moderate activities (≥3 METs). Cardiovascular markers included body mass index, blood pressure, insulin resistance, and lipid profile. Disability and disease activity were measured with the Health Assessment Questionnaire (HAQ) and Disease Activity Score-28 (DAS-28), respectively. Associations between PA at each intensity and health-markers were assessed by multiple linear regression models adjusted by age, sex, and cohort.
Results:
Ninety-eight subjects (58 ± 9 years, 85% female) were included. Subjects spent 9.8 hours/day being sedentary, 3.5 hours/day in very light PA, 2.1 hours/day in light PA and 35 minutes/day in moderate PA. Only 17% were physically active (≥150 minutes/week of moderate PA in 10-minute bouts). Regression models showed that very light, light and moderate PA were inversely associated with most cardiovascular risk factors, the HAQ, and DAS-28 scores (R2Δrange: .04 to .52, p <.05). The associations between PA and cardiovascular markers were either equivalent or stronger at very light- and light-intensities as compared to moderate-intensity.
Conclusions:
Individuals with RA are mostly active at very light and light intensities. PA at these intensities associate favorably with cardiovascular markers, and lower disability and disease activity in RA.
Physical activity (PA) includes both structured and non-structured activities, and is generally classified as light, moderate, or vigorous intensity, depending on the effort or amount of energy expended by an individual during the activity. According to the 2008 PA guidelines from the U.S. Department of Health and Human Services, regular participation in PA of moderate or vigorous intensity improves health and reduces morbidity and mortality.(1) However, individuals with chronic and physically debilitating conditions may not be able to participate in PA of moderate and vigorous intensities as recommended by the guidelines.
Joint disease in rheumatoid arthritis (RA) often limits participation in moderate and vigorous physical activities. Individuals with RA generally tend to be sedentary as a result of poly-articular pain, stiffness, fatigue, and functional limitations (2–4). In a cross-sectional study of patients with RA from 21 countries, around 71% reported being sedentary and not engaging in regular physical activity (2) While a physically active lifestyle in RA is important to decrease the risk of cardiovascular disease, (5) it might be unreasonable to expect that all individuals with RA can shift from their habitual sedentary behavior to regular participation in PA at moderate or higher intensity. Whereas evidence does not suggest any detrimental effects of PA at high intensity on RA disease severity and progression, (6–9) presence of joint pain, swelling, fatigue and discomfort may interfere with the ability to participate in PA at this level. Periods of active RA flares, presence of extensive poly-articular disease or high disease activity may also decrease tolerance to PA at high intensities. On the other hand, light-intensity activities are less demanding and more tolerable than high intensities, thereby making them easier to sustain or accumulate over longer durations. Prolonged periods of inactivity or sedentary behavior are also likely to be broken more frequently with light-intensity PA than with moderate or vigorous PA. Thus, participating in light-intensity PA can serve as a strategy to keep individuals with RA moving throughout the day, and also as a transition step towards activities of greater intensity.
Studies in RA have not investigated the benefits of accruing substantial amounts of time in light-intensity PA, but emerging evidence in non-RA populations suggests promising benefits of light-intensity PA.(10–14) In healthy older adults, light-intensity PA showed similar associations with good physical and psychosocial well-being, (10) and lower odds of being depressed (11) as did moderate-to-vigorous intensity. In adults with diabetes, significant associations between light-intensity PA and lower markers of systemic inflammation (white blood cell and neutrophil count), and lower fasting blood glucose levels were reported.(12, 15) Two studies in individuals with knee osteoarthritis (13, 14) demonstrated that light-intensity PA was associated with reduced incident disability during activities of daily living, (13) and better physical function.(14). Growing evidence also suggests that merely achieving the recommendations of 150 minutes/week in moderate intensity PA is not enough to counteract the deleterious effects of several hours of sedentary behavior accumulated through the remainder of the day.(16) In fact, one randomized trial in sedentary healthy adults demonstrated that spending 6 hours/day in light-intensity PA improved plasma glucose and lipid levels to a greater extent than exercising for one hour/day at vigorous-intensity.(17) These observations thus highlight the benefits of remaining active even at lower intensities.
PA is important for both cardiovascular health and physical function. As those with RA may have difficulty reaping the well-known benefits of moderate or vigorous PA, determining the benefits of light-intensity PA might help encourage participation in activities that are feasible and safe regardless of disability level, and subsequently reduce sedentary behaviors. Therefore, the aim of this study was to characterize PA behavior in individuals with RA, with focus on time spent in PA of light-intensity, and to determine the associations between participation in PA of light to moderate intensities and cardiovascular markers of health, such as body mass index, blood pressure, blood cholesterol and insulin resistance, as well as disability status and RA disease activity.
MATERIAL AND METHODS
Study Design
This is a cross-sectional analysis of PA accelerometry data in adults with RA collected from two research studies conducted at the University of Pittsburgh between 2007 and 2013.(18–21) Both studies were approved by the University of Pittsburgh Institutional Review Board, and informed consent was obtained from all eligible participants prior to study enrollment.
Study Sample
The first study was a prospective cohort study that assessed subclinical cardiovascular disease and associated risk factors in women with RA.(18–20) Participants were at least 30 years old with an established diagnosis of RA in accordance with 1987 American College of Rheumatology criteria (22) for at least two years prior to study enrollment. Individuals with history of cardiovascular events were excluded. PA measures in this study were obtained between November 2007 and July 2008 in 47 subjects who returned for the five-year follow-up visit.
The second study was a randomized clinical study investigating the effect of a 16-week lower extremity strengthening exercise intervention on muscle function.(21) Eligible participants were those at least 21 years of age, diagnosed with RA in accordance with the American College of Rheumatology criteria (22), able to ambulate independently, and without cardiovascular or neuromuscular diseases that would preclude them from participating in muscle strengthening program. This randomized trial was conducted between December 2009 to September 2013, and PA data were collected in 60 subjects during their baseline visit.
Study Procedures and Measurements
In both study cohorts trained personnel collected demographical information, measured height, weight, resting blood pressure, and self-reported disability, assessed RA history and disease severity, and performed phlebotomy. All demographic and clinical data from both studies were obtained during the same time point as the PA measures. Body mass index was calculated from weight and height using formula weight/height2. Blood pressure was measured after 10 minutes of rest. Disability was measured using the Health Assessment Questionnaire (HAQ), which is a widely used and validated tool to assess limitations during activities of daily living. (23) The HAQ includes 20 activities of daily living, and its score ranges from 0 (no disability) to 3 (severe disability).
Measures from fasting blood samples included glucose, insulin, high-density lipoproteins (HDL), low-density lipoproteins (LDL), triglycerides, and erythrocyte sedimentation rate (ESR). Insulin resistance was calculated from glucose and insulin levels using the Oxford formula for Homeostasis Model Assessment (HOMA-IR).(24) Disease activity was measured using the Disease Activity Score (DAS-28), which combines the number of tender and swollen joints, ESR levels, and patient’s rating of global health to produce a score. In the DAS-28, scores < 3.2 indicate low disease activity, scores ≥ 3.2 ≤ 5.1 indicate moderate disease activity and scores > 5.1 indicate high disease activity. (25) The blood assays were run in the Heinz Nutrition Laboratory at the Graduate School of Public Health, University of Pittsburgh. The lab is included in the CDC-NHLBI Lipid Standardization Program and is accredited by the Clinical Laboratory Improvement Amendment.
PA was objectively measured by the Sensewear Armband (SWA, Bodymedia Inc, Pittsburgh PA). The SWA is a multi-sensor portable activity monitor that combines data from biaxial accelerometers, heat flux, skin temperature, and galvanic signals. The SWA has shown to yield reliable and valid measures of PA in older adults and people with disability.(26–28) On the day of the study visit, participants were given the SWA and instructed to wear it on the back of their right arm (over the triceps muscle) for 8 consecutive days, up to 24 hours per day, except during water activities. At the end of the wear period, the SWA was returned to the study site and data were downloaded using Sensewear Professional v6.1 software (Bodymedia Inc, Pittsburgh PA). Participants in whom the monitors recorded at least 5 days with 10 hours of data per day were included in the data analysis. (18)
PA data obtained from the monitors were categorized into four intensity categories based on amount of energy expenditure in metabolic equivalents (METs).(29) Sedentary behavior represented activities that required up to 1 MET that were done while being awake, very light-intensity represented activities between 1.1 and 1.9 METs, light-intensity were activities between 2.0 and 2.9 METs, whereas moderate intensity represented activities equal or above 3 METs. Activities done laying down and while sitting such as watching TV, reading or computer work are examples of sedentary behavior; washing dishes, cleaning windows, or folding laundry are examples of very light-intensity; lawn mowing, vacuuming and slow walking are examples of light-intensity; and swimming, brisk walk, or golfing are examples of moderate-intensity. The time spent in each intensity category per day was recorded in minutes (min/day). The moderate- and vigorous-intensity activities were combined since our sample engaged in negligible vigorous-intensity activities. PA was also characterized as the average daily number of steps, and the proportion of the sample that met the weekly PA recommendation of 150 minutes in moderate-intensity PA in bouts of 10 minutes. (1) Time spent in activities of moderate-to-vigorous intensity in 10-minute bouts was summed across the days included in the analysis.
Statistical Analysis
Subject characteristics and PA behavior at each intensity were described using mean (standard deviation) or median (25–75 quartiles) for continuous data and frequencies for categorical data. Relationships between the number of minutes spent sedentary, on very light-, light- and moderate-intensity PA (independent variables), and cardiovascular risk factors, disability and disease activity (dependent variables) were examined using Pearson or Spearman’s correlation coefficients and linear regression models. The contribution of each number of minutes spent on sedentary, and on very light-, light- and moderate-intensity PA to each dependent variable was assessed using separate linear regression models. Each linear regression model was adjusted by cohort, gender, and age. The contribution of time spent in each PA level with each dependent variable was assessed by the magnitude and significance of the R2 change (R2Δ) statistic. Small magnitude of R2 Δ corresponds to .01, moderate to .09 and large to 0.25. (30) Regression diagnostics were run and data transformations were used as needed in order to not violate the assumptions for linear regression (i.e., normality of the error distribution, linearity, homoscedasticity). All statistical analyses were performed using the IBM SPSS software, version 21. (IBM Corporation)
RESULTS
Of 107 participants in both cohorts, 9 did not have PA data for at least 5 days of 10 hours and were excluded from analysis. The characteristics of the remaining 98 participants are described in Table 1. Participants had an average age of 58 ± 9 years, who were overweight, and mostly female. Participants had a median disease duration of 14 years, median DAS-28 score of 3.4, corresponding to moderate disease activity, (25) and a median HAQ score of 0.75, reflecting relatively low disability.
Table 1.
Demographical and Biomedical Characteristics of the Sample. Values represent Median (25–75 Interquartile range) unless specified otherwise. HOMA-IR: homeostatic model assessment-insulin resistance
| Variables | Sample (n = 98) |
|---|---|
| Mean age, years (SD) | 58 (9) |
| Gender, N of Female (%) | 83 (85) |
| Race, N of Caucasian (%) | 89 (91) |
| Education, N (%) | |
| Less than College Education | 33 (34) |
| College Degree | 65 (66) |
| Height, m | 1.63 (1.6–1.69) |
| Weight, kg | 75.1 (64.0–93.3) |
| Body Mass Index, kg/m2 | 28.4 (24.4–33.8) |
| Systolic Blood Pressure, mmHg | 130 (120–137) |
| Diastolic Blood Pressure, mmHg | 80 (74–86) |
| Disease Activity Score (DAS-28) | 3.44 (2.65–4.31) |
| Disease Duration, years | 14 (6–22) |
| Health Assessment Questionnaire (HAQ) | 0.75 (0.25–1.25) |
| Plasma Glucose, mg/dl | 97 (92–105) |
| Plasma Insulin, μU/ml | 14 (10–19) |
| High Density Lipoprotein, mg/dl | 61 (50–72) |
| Low Density Lipoprotein, mg/dl | 118 (102–132) |
| Triglyceride, mg/dl | 96 (76–147) |
| Insulin Resistance (HOMA-IR) | 1.9 (1.4–2.6) |
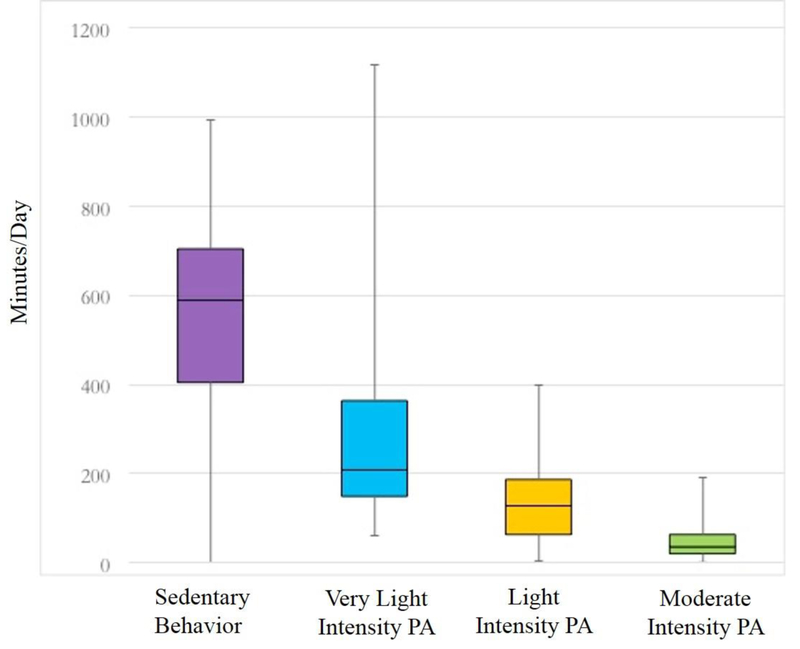
PA behavior in sedentary, very light, light and moderate intensities is characterized in Figure 1. The portable monitors were worn for an average of 23 hours per day for 7 days. Median time spent in sedentary activities performed while awake was 589 min/day (9.8 hours/day), very light-intensity activity was 208 min/day (3.5 hours/day), light-intensity activity was 128 min/day (2.1 hours/day), and moderate-intensity activity was 36 min/day. Median number of steps per day were 6324. Although these data show that participants accumulated more than half-hour a day in moderate-intensity activities, most of these activities were in bouts of less than 10 minutes. Only 17% of subjects achieved the weekly PA guidelines of 150 minutes/week of moderate intensity activity in bouts of at least 10 minutes. For the calculation of those who achieved PA guidelines, 90 of the 98 participants (92%) had PA data for 7 days of the week. For those 8 subjects with less than 7 days of PA data, we observed the pattern of PA per day to adjudicate whether they would have met the guidelines if data for 7 days were available. In our sample, six participants with less than 7 days (5 or 6 days of PA data) had negligible amounts of moderate PA during this period and hence were deemed as not meeting the guidelines, while two participants had 20 ten-minute bouts, and were included in the 17% that met the PA guidelines.
Figure 1.
Whisker Plots showing Physical Activity Characteristics (minutes/day) in the Study Sample Sum of time in several levels of physical activity do not total 24 hours because participants removed the monitors for showering/bathing.
The bivariate correlations between PA levels and cardiovascular risk factors, disability and disease activity are shown in Table 2. PA was inversely associated with cardiovascular risk factors, disability and disease activity, while sedentary behavior directly associated with cardiovascular risk factors, disability and disease activity. PA at all intensities showed moderate to strong inverse associations with BMI, blood pressure, disease activity, disability and insulin resistance (p ≤ .05). PA at very light- and light-intensity showed significant small to moderate inverse associations with HDL, PA at very light-intensity showed a significant but small inverse association with triglycerides (p ≤ .05), and PA did not associate with LDL.
Table 2.
Correlations between Minutes spent in Sedentary Behavior and at Very Light, Light and Moderate Intensity Physical Activity (PA), and Cardiovascular Risk Factors, Disability and Disease Activity.
| Sedentary (min/day) |
Very Light PA (min/day) |
Light PA (min/day) |
Moderate PA (min/day) |
|
|---|---|---|---|---|
| Variables | ||||
| Body Mass Index | .758* | −.651* | −.790* | −.426* |
| Diastolic Blood Pressure | .294* | −.373* | −.239* | −.223* |
| Systolic Blood Pressure | .316* | −.379* | −.200* | −.328* |
| Insulin Resistance (HOMA−IR) | .450* | −.348* | −.507* | −.364* |
| High Density Lipoproteins | −.273* | .246* | .249* | .081 |
| Low Density Lipoproteins | .048 | −.062 | −.019 | −.011 |
| Triglycerides | .137 | −.061 | −.202* | −.064 |
| HAQ score | .433* | −.277* | −.261* | −.384* |
| DAS−28 | .338* | −.274* | −.280* | −.160 |
All correlation coefficients in the table are presented as Spearman Rho (ρ) because data were not normally distributed.
Significant at alpha level of 0.05.
DAS-28: Disease Activity Score; HAQ: Health Assessment Questionnaire; HOMA-IR: homeostatic model assessment-insulin resistance.
The results of the linear regression models are shown in Table 3. For the analyses with cardiovascular risk factors, BMI, systolic blood pressure, insulin resistance, HDL, LDL, and triglycerides were transformed (log-base 10) to meet the assumptions of linear regression. After controlling for age, gender and cohort, greater time spent in PA at very light, light and moderate intensities was significantly associated with lower BMI, lower diastolic and systolic blood pressure, better insulin sensitivity and higher HDL levels (p <.05). In contrast, greater time spent in sedentary behavior was significantly associated with these outcomes in the opposite direction (p < .05). PA was not associated with LDL and triglycerides.
Table 3.
Associations between Minutes spent in Sedentary Behavior and at Very Light, Light, and Moderate Intensity Physical Activity (PA), and Cardiovascular Risk Factors, Disability and Disease Activity from the Regression Analysis. Values represent standardized coefficients (β), R2 change (R2Δ), and p values from adjusted linear regression models of each category of physical activity on each variable. Models are adjusted for age, gender, and cohort.
| Sedentary (min/day) |
Very Light PA (min/day) |
Light PA (min/day) |
Moderate PA (min/day) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β (95% CI) |
R2Δ | p-value | β (95% CI) |
R2Δ | P-value | β (95% CI) |
R2Δ | p-value | β (95% CI) |
R2Δ | p-value | ||
| Variables | |||||||||||||
| BMI (log) | .75 (.65, .82) | .54 | <.001 | −.65 (−.75, −.51) | .40 | <.001 | −.74 (−.81, −.63) | .52 | <.001 | −.45 (−.60, −.28) | .19 | <.001 | |
| Diastolic BP | .34 (.15, .50) | .11 | <.001 | −.40 (−.55, −.22) | .15 | <.001 | −.25 (−.43, −.05) | .06 | .010 | −.21 (−.39, −.01) | .04 | .029 | |
| Systolic BP (log) | .36 (.17, 52) | .13 | <.001 | −.35 (−.51, −.16) | .12 | <.001 | −.28 (−.45, −.09) | .07 | .006 | −.28 (−.45, −.09) | .08 | .006 | |
| HOMA−IR (log) | .40 (.21, 55) | .15 | <.001 | −.32 (−.48, −.12) | .09 | .002 | −.43 (−.57, −.25) | .17 | <.001 | −.29 (−.46, −.10) | .08 | .004 | |
| HDL (log) | −.23 (−.41, −.03) | .05 | .021 | .21 (.01, .39) | .04 | .021 | .30 (.11, .47) | .08 | .001 | .19 (.01, .37) | .03 | .044 | |
| LDL (log) | .12 (−.08, .31) | .01 | .256 | −.17 (−.35, .03) | .03 | .091 | −.13 (−.32, .07) | .02 | .207 | .01 (−.19, .21) | .00 | .916 | |
| Triglycerides (log) | .13 (−.07, 32) | .02 | .212 | −.10 (−.29, .10) | .01 | .318 | −.20 (−.38, −.00) | .04 | .055 | −.12 (−.31,.08) | .01 | .270 | |
| HAQ | .41 (.23, .56) | .16 | <.001 | −.23 (−.38, −.09) | .05 | .027 | −.23 (−.38, −.09) | .05 | .026 | −.34 (−.47, −.20) | .11 | .001 | |
| DAS−28 | .25 (.05, .42) | .06 | .006 | −.20 (−0.35, .02) | .04 | .040 | −.18 (−.35, .03) | .03 | .056 | −.06 (−.24, .10) | <.01 | .511 | |
95% CI: 95% confidence intervals; log: log-10 transformed variable; BMI: Body Mass Index; BP: blood pressure; DAS-28: Disease Activity Score; HAQ: Health Assessment Questionnaire; HOMA-IR: homeostatic model assessment-insulin resistance; HDL: high-density lipoprotein; LDL: low-density lipoprotein.
For BMI, PA at all intensities showed large inverse associations, but the magnitude of effect in very light and light PA was more than double (R2Δ = .40 and .52, respectively) compared to moderate-intensity (R2Δ = .19). In contrast, sedentary behavior showed a large positive association with BMI (R2Δ = .54). Very light-intensity PA also showed greater inverse associations of moderate effect size with diastolic (R2Δ = .15) and systolic blood pressure (R2Δ = .12) compared to light and moderate intensities (R2Δ range: .04 to .08). On the contrary, sedentary behavior showed moderate but positive associations with diastolic and systolic blood pressure (R2Δ = .11 and .13, respectively). PA at all intensities also showed significant small to moderate associations with higher HDL levels (R2Δ range between .03 to .08), and with better insulin sensitivity (R2Δ range: .08 to .17), while sedentary behavior showed significant associations with lower HDL (R2Δ = .05) and lower insulin sensitivity (R2Δ = .16).
The analyses between PA levels, disability and disease activity demonstrated that after controlling for age, gender and cohort, PA was inversely associated with disability and disease activity, while sedentary behavior was positively associated disability and disease activity. Disability was the only outcome in which moderate-intensity PA showed larger associations compared to very light and light intensities. Greater time in moderate PA associated moderately with higher HAQ scores (R2Δ = .11, p <.05), while very light and light PA showed small associations (R2Δ= .05, p <.05). Disease activity was only significantly associated with very light-intensity PA, and the magnitude of the association was small (R2Δ = .04, p =.004).
DISCUSSION
To our knowledge, the current study is the first to characterize objectively measured, free-living PA across the entire spectrum from sedentary behavior to moderate-intensity in individuals with RA. This is in contrast to previous reports in RA that did not characterize or report PA across different intensity categories. (5, 19, 31, 32) The findings confirm that individuals with RA are largely sedentary and spend the majority of their PA in light intensities. Only 17% of participants met the PA guidelines, which is similar to other reports in arthritis, (14, 33, 34) but lower than the reported rate of 44–64% in the general population.(35, 36) The daily number of steps walked by the participants (6234) corresponds to being low-active. (37) The current study is also unique because it investigated the associations between PA at these different intensities and cardiovascular risk factors. To date, only one study in RA assessed the cardiovascular risk profile amongst those who were active and inactive. Metsios et al reported that individuals who were more active had lower blood cholesterol (LDL and triglycerides), lower systolic blood pressure and lower HOMA-IR compared to those who were inactive, which suggest a favorable effect of PA on cardiovascular risk profile. However, the study only compared being active versus inactive, and did not assess PA across the continuum from light to moderate intensities. (5)
Study findings indicate that time spent in very light and light intensities also have beneficial associations with markers of cardiovascular health, as PA at these intensities showed moderate to large associations with more favorable BMI, blood pressure, HDL, and insulin sensitivity. To date, the effect of light-intensities PA on cardiovascular health has not been investigated in adults with RA, but has been examined in two cross-sectional studies in healthy older adults. One study demonstrated that those who participated in less than 300 minutes/week of light intensity PA had higher values of BMI, blood pressure and insulin resistance, and were at higher risk of comorbidity (Relative Risk: 1.35; 95% CI [1.24;1.47]) compared to those who participated in more than 300 minutes/week of light-intensity PA.(38) The second study demonstrated that those who did not participate in 150 minutes/week of moderate to vigorous PA, but spent more time in light PA than being sedentary, had lower triglyceride levels and higher insulin sensitivity compared to those who spent less time in light PA and more time being sedentary. (39) The current study also demonstrated that light PA is significantly associated with lower disability in individuals with RA. While previous studies in RA reported that greater time spent in PA was associated with lower disability, (19, 40) these studies did not specifically assess the contribution of PA at light intensities.
Previous studies in RA that measured PA (5, 18, 19, 31, 32, 41, 42) did not characterize or measure PA across different intensity categories, and data specifically for participation at light intensities is limited. To date, only two studies in RA reported PA at light intensity, and neither investigated the effect of light intensity PA on cardiovascular risk factors. (40) (43) Hernandez et al reported 56 min/day (40) while Semanik et al reported 68 min/day (43), which are considerably lower than our finding of 328 min/day (very-light and light combined). The discrepancy in findings could be attributed to the different methods used to measure PA. Semanik et al measured PA using self-reported questionnaires, which may have contributed to the underestimation of activities of low intensity, while overestimating activities at moderate-intensity. (28) The lesser amount of PA at light intensities reported in Hernandez et al (40) could be due to the waist-mounted accelerometers utilized, which have demonstrated to underestimate PA and not captured upper body movements. (E.g., raking leaves, cooking, or vacuuming). (28) The observation that PA was not accurately captured is further supported by the similar number of steps/day reported in Hernandez et al and in our cohort (6200 vs 6234 steps/day), which suggests that the amount of PA actually performed was not very different between the cohorts.
The study results are relevant to research and clinical practice as PA is generally measured at moderate intensity. However, in a population that spends so little time in moderate intensity PA, it may not be reasonable to track or promote PA participation solely at moderate intensities. According to the current recommendations, at least 150 minutes/week of moderate intensity in bouts of at least 10-minute bouts are necessary for health benefits. Although our sample accrued about 35 minutes of moderate intensity PA per day, majority of PA at this intensity was in very short bouts of 1 to 5 minutes, which falls far below the recommendations for health benefits. On the other hand, our sample spent between two and four hours per day in light activities. Hence, light activities provide a better representation of PA in individuals with RA, and should be considered to accurately track progress toward becoming more active.
Regular PA is necessary not only to improve function and independence during daily activities, but also to reduce cardiovascular mortality, (5–7) which is nearly two-fold greater in RA compared to the general population. (44) Individuals with RA also tend to be more overweight and have higher body fat, (45) and commonly present with co-morbid conditions such as hypertension, infections, and anxiety or depression disorders that worsen their overall health. (44, 46, 47) Thus, the combination of high mortality and morbidity along with the debilitating effects of the RA disease itself underscores the need for effective preventative measures specifically, exercise and PA promotion. While the benefits of structured PA at moderate intensity on cardiovascular health and physical function are recognized, (48–50) the benefits of participating in light-intensity PA are not established. The findings of this study suggest that PA at light intensities may also influence cardiovascular and metabolic health in individuals with RA. Hence, the goals for PA promotion in such individuals should not necessarily focus on increasing participation in moderate intensity activities to meet the current PA guidelines, but should be tailored towards reducing sedentary time and increasing time spent in PA at light intensities.
The current study is not without limitations. The RA population examined in this study were sedentary and overweight. The RA sample studied also consisted of a motivated group of individuals, who were willing to participate in cohort and clinical studies and had no major cardiovascular diseases. While these factors may limit generalizability of results, the study sample is still fairly representative of RA populations studied in most western developed societies, in terms of sedentary behavior, and BMI. Another limitation is the inclusion of an RA cohort with only women, however, the study attempted to minimize this potential confounder by adjusting the regression models for gender and cohort. Further, the overall gender distribution in the current study (85% female) is similar to other studies in RA.(2, 40, 49) The study is also limited due to its cross-sectional design. Thus, even though causal inferences cannot be drawn, the study provides important preliminary information to support the need for future larger and confirmatory longitudinal studies to determine the effect of PA at light intensities in improving cardiovascular health, and reducing disability in more diverse and less selective samples of individuals with arthritis.
CONCLUSION
Individuals with RA are largely sedentary, and most of their PA is at the light intensities levels. While not typically considered to have much health benefit, PA at light intensities were significantly associated with lower disability and disease activity, as well as risk factors for cardiovascular disease, such as lower BMI and blood pressure, higher levels of high-density lipoproteins, and better insulin sensitivity. Increasing participation in light-intensity PA should be considered while promoting PA in individuals with RA.
Significance and Innovation:
Although the health benefits of physical activity at moderate or higher intensity are well-acknowledged, individuals with RA may find it difficult to participate in activities at these intensities due to symptoms and functional limitations. In contrast, these individuals are more likely to engage in very light- or light-intensity activities such as easy domestic duties and leisure walking.
The benefits of physical activity at light intensities are not well established in individuals with RA. To address this gap in knowledge, the current cross-sectional study investigated the associations of physical activity at different intensity levels with cardiovascular risk factors, disability, and disease activity.
Participating in light activities may positively influence health. Study findings demonstrate that greater time spent in very light- and light-intensity activities was associated with favorable markers of cardiovascular and physical health at an equivalent or stronger magnitude as compared to moderate-intensity.
Acknowledgments
Funding Source: Partially supported by Arthritis Foundation - Western Pennsylvania Chapter, MUH-CTRC - NIH/NCRR/CTSA Grant UL1 RR024153, and Mentored Research Scientist Development Award, National Center for Medical Rehabilitation Research, NIH (K01 HD058035).
Footnotes
The authors have no conflicts of interest to disclose.
References
- 1.U.S Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. 2008. [cited 2015 January 5th]; Available from: http://www.health.gov/paguidelines/
- 2.Sokka T, Hakkinen A, Kautiainen H, Maillefert JF, Toloza S, Mork Hansen T, et al. Physical inactivity in patients with rheumatoid arthritis: data from twenty-one countries in a cross-sectional, international study. Arthritis Rheum. 2008;59(1):42–50. [DOI] [PubMed] [Google Scholar]
- 3.Lee J, Dunlop D, Ehrlich-Jones L, Semanik P, Song J, Manheim L, et al. Public health impact of risk factors for physical inactivity in adults with rheumatoid arthritis. Arthritis Care Res (Hoboken). 2012;64(4):488–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Paul L, Rafferty D, Marshall-McKenna R, Gill JM, McInnes I, Porter D, et al. Oxygen cost of walking, physical activity, and sedentary behaviours in rheumatoid arthritis. Scandinavian journal of rheumatology. 2014;43(1):28–34. [DOI] [PubMed] [Google Scholar]
- 5.Metsios GS, Stavropoulos-Kalinoglou A, Panoulas VF, Wilson M, Nevill AM, Koutedakis Y, et al. Association of physical inactivity with increased cardiovascular risk in patients with rheumatoid arthritis. European journal of cardiovascular prevention and rehabilitation : official journal of the European Society of Cardiology, Working Groups on Epidemiology & Prevention and Cardiac Rehabilitation and Exercise Physiology. 2009;16(2):188–94. [DOI] [PubMed] [Google Scholar]
- 6.Plasqui G The role of physical activity in rheumatoid arthritis. Physiology & Behavior. 2008;94(2):270–5. [DOI] [PubMed] [Google Scholar]
- 7.Metsios GS, Stavropoulos-Kalinoglou A, Veldhuijzen van Zanten JJ, Treharne GJ, Panoulas VF, Douglas KM, et al. Rheumatoid arthritis, cardiovascular disease and physical exercise: a systematic review. Rheumatology (Oxford). 2008;47(3):239–48. [DOI] [PubMed] [Google Scholar]
- 8.de Jong Z, Vliet Vlieland TP Safety of exercise in patients with rheumatoid arthritis. Current opinion in rheumatology. 2005;17(2):177–82. [DOI] [PubMed] [Google Scholar]
- 9.van den Ende CH, Breedveld FC, le Cessie S, Dijkmans BA, de Mug AW, Hazes JM. Effect of intensive exercise on patients with active rheumatoid arthritis: a randomised clinical trial. Annals of the rheumatic diseases. 2000;59(8):615–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buman MP, Hekler EB, Haskell WL, Pruitt L, Conway TL, Cain KL, et al. Objective light-intensity physical activity associations with rated health in older adults. Am J Epidemiol. 2010;172(10):1155–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Loprinzi PD. Objectively measured light and moderate-to-vigorous physical activity is associated with lower depression levels among older US adults. Aging & mental health. 2013;17(7):801–5. [DOI] [PubMed] [Google Scholar]
- 12.Loprinzi PD, Ramulu PY. Objectively measured physical activity and inflammatory markers among US adults with diabetes: implications for attenuating disease progression. Mayo Clin Proc. 2013;88(9):942–51. [DOI] [PubMed] [Google Scholar]
- 13.Dunlop DD, Song J, Semanik PA, Sharma L, Bathon JM, Eaton CB, et al. Relation of physical activity time to incident disability in community dwelling adults with or at risk of knee arthritis: prospective cohort study. Bmj. 2014;348:g2472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chmelo E, Nicklas B, Davis C, Miller GD, Legault C, Messier S. Physical activity and physical function in older adults with knee osteoarthritis. Journal of physical activity & health. 2013;10(6):777–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Healy GN, Winkler EA, Brakenridge CL, Reeves MM, Eakin EG. Accelerometer-derived sedentary and physical activity time in overweight/obese adults with type 2 diabetes: cross-sectional associations with cardiometabolic biomarkers. PLoS One. 2015;10(3):e0119140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Owen N, Healy GN, Matthews CE, Dunstan DW. Too Much Sitting: The Population-Health Science of Sedentary Behavior. Exercise and Sport Sciences Reviews. 2010;38(3):105–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Duvivier BM, Schaper NC, Bremers MA, van Crombrugge G, Menheere PP, Kars M, et al. Minimal intensity physical activity (standing and walking) of longer duration improves insulin action and plasma lipids more than shorter periods of moderate to vigorous exercise (cycling) in sedentary subjects when energy expenditure is comparable. PLoS One. 2013;8(2):e55542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Almeida GJ, Wasko MC, Jeong K, Moore CG, Piva SR. Physical activity measured by the SenseWear Armband in women with rheumatoid arthritis. Phys Ther. 2011;91(9):1367–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Piva SR, Almeida GJ, Wasko MC. Association of physical function and physical activity in women with rheumatoid arthritis. Arthritis Care Res (Hoboken). 2010;62(8):1144–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schott LL, Kao AH, Cunningham A, Wildman RP, Kuller LH, Sutton-Tyrrell K, et al. Do carotid artery diameters manifest early evidence of atherosclerosis in women with rheumatoid arthritis? J Womens Health (Larchmt). 2009;18(1):21–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khoja SS, Goodpaster BH, S.R. P. Skeletal Muscle Fat and its Association with Physical Function and Physical Activity in Adults with Rheumatoid Arthritis American College of Rheumatology Annual Meeting. Boston, MA: Arthritis Rheum; 2014. [Google Scholar]
- 22.Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31(3):315–24. [DOI] [PubMed] [Google Scholar]
- 23.Bruce B, Fries JF. The Health Assessment Questionnaire (HAQ). Clin Exp Rheumatol. 2005;23(5 Suppl 39):S14–8. [PubMed] [Google Scholar]
- 24.Levy JC, Matthews DR, Hermans MP. Correct homeostasis model assessment (HOMA) evaluation uses the computer program. Diabetes care. 1998;21(12):2191–2. [DOI] [PubMed] [Google Scholar]
- 25.Makinen H, Kautiainen H, Hannonen P, Mottonen T, Korpela M, Leirisalo-Repo M, et al. Disease activity score 28 as an instrument to measure disease activity in patients with early rheumatoid arthritis. J Rheumatol. 2007;34(10):1987–91. [PubMed] [Google Scholar]
- 26.Machac S, Prochazka M, Radvansky J, Slaby K. Validation of physical activity monitors in individuals with diabetes: energy expenditure estimation by the multisensor SenseWear Armband Pro3 and the step counter Omron HJ-720 against indirect calorimetry during walking. Diabetes technology & therapeutics. 2013;15(5):413–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tierney M, Fraser A, Purtill H, Kennedy N. Study to determine the criterion validity of the SenseWear Armband as a measure of physical activity in people with rheumatoid arthritis. Arthritis Care Res (Hoboken). 2013;65(6):888–95. [DOI] [PubMed] [Google Scholar]
- 28.Almeida GJ, Wert DM, Brower KS, Piva SR. Validity of physical activity measures in individuals after total knee arthroplasty. Arch Phys Med Rehabil. 2015. 96(3):524–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exerc. 1998;30(5):777–81. [DOI] [PubMed] [Google Scholar]
- 30.Cohen J Statistical power analysis for the behavioral sciences. Second ed. Hillsdale,NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 31.Prioreschi A, Hodkinson B, Avidon I, Tikly M, McVeigh JA. The clinical utility of accelerometry in patients with rheumatoid arthritis. Rheumatology (Oxford). 2013;52(9):1721–7. [DOI] [PubMed] [Google Scholar]
- 32.Semanik P, Song J, Chang RW, Manheim L, Ainsworth B, Dunlop D. Assessing physical activity in persons with rheumatoid arthritis using accelerometry. Medicine and science in sports and exercise. 2010;42(8):1493–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wallis JA, Webster KE, Levinger P, Taylor NF. What proportion of people with hip and knee osteoarthritis meet physical activity guidelines? A systematic review and meta-analysis. Osteoarthritis and Cartilage. 2013;21(11):1648–59. [DOI] [PubMed] [Google Scholar]
- 34.Dunlop DD, Song J, Semanik PA, Chang RW, Sharma L, Bathon JM, et al. Objective physical activity measurement in the osteoarthritis initiative: Are guidelines being met? Arthritis Rheum. 2011;63(11):3372–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Prevalence of self-reported physically active adults--United States, 2007. MMWR Morbidity and mortality weekly report. 2008;57(48):1297–300. [PubMed] [Google Scholar]
- 36.Carlson SA, Fulton JE, Schoenborn CA, Loustalot F. Trend and prevalence estimates based on the 2008 Physical Activity Guidelines for Americans. American journal of preventive medicine. 2010;39(4):305–13. [DOI] [PubMed] [Google Scholar]
- 37.Sisson SB, Camhi SM, Tudor-Locke C, Johnson WD, Katzmarzyk PT. Characteristics of step-defined physical activity categories in U.S. adults. American journal of health promotion : AJHP. 2012;26(3):152–9. [DOI] [PubMed] [Google Scholar]
- 38.Loprinzi PD, Lee H, Cardinal BJ. Evidence to Support Including Lifestyle Light-Intensity Recommendations in Physical Activity Guidelines for Older Adults. American journal of health promotion : AJHP. 2014. [DOI] [PubMed] [Google Scholar]
- 39.Loprinzi PD, Lee H, Cardinal BJ. Daily movement patterns and biological markers among adults in the United States. Preventive medicine. 2014;60:128–30. [DOI] [PubMed] [Google Scholar]
- 40.Hernandez-Hernandez V, Ferraz-Amaro I, Diaz-Gonzalez F. Influence of disease activity on the physical activity of rheumatoid arthritis patients. Rheumatology (Oxford). 2014;53(4):722–31. [DOI] [PubMed] [Google Scholar]
- 41.Henchoz Y, Bastardot F, Guessous I, Theler JM, Dudler J, Vollenweider P, et al. Physical activity and energy expenditure in rheumatoid arthritis patients and matched controls. Rheumatology (Oxford). 2012;51(8):1500–7. [DOI] [PubMed] [Google Scholar]
- 42.Munneke M, de Jong Z, Zwinderman AH, Tijhuis GJ, Hazes JM, Vliet Vlieland TP. The value of a continuous ambulatory activity monitor to quantify the amount and intensity of daily activity in patients with rheumatoid arthritis. J Rheumatol. 2001;28(4):745–50. [PubMed] [Google Scholar]
- 43.Semanik P, Wilbur J, Sinacore J, Chang RW. Physical activity behavior in older women with rheumatoid arthritis. Arthritis Rheum. 2004;51(2):246–52. [DOI] [PubMed] [Google Scholar]
- 44.Naz SM, Symmons DP. Mortality in established rheumatoid arthritis. Best practice & research Clinical rheumatology. 2007;21(5):871–83. [DOI] [PubMed] [Google Scholar]
- 45.Giles JT, Ling SM, Ferrucci L, Bartlett SJ, Andersen RE, Towns M, et al. Abnormal body composition phenotypes in older rheumatoid arthritis patients: association with disease characteristics and pharmacotherapies. Arthritis Rheum. 2008;59(6):807–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Center for Disease Control and Prevention. Arthritis Types-Rheumatoid Arthritis. 2011 November 6th 2014. [cited 2015 January 5th]; Available from: http://www.cdc.gov/arthritis/basics/rheumatoid.htm
- 47.Wasko MC. Comorbid conditions in patients with rheumatic diseases: an update. Current opinion in rheumatology. 2004;16(2):109–13. [DOI] [PubMed] [Google Scholar]
- 48.Metsios GS, Stavropoulos-Kalinoglou A, Veldhuijzen van Zanten JJ, Nightingale P, Sandoo A, Dimitroulas T, et al. Individualised exercise improves endothelial function in patients with rheumatoid arthritis. Annals of the rheumatic diseases. 2014;73(4):748–51. [DOI] [PubMed] [Google Scholar]
- 49.Stavropoulos-Kalinoglou A, Metsios GS, Veldhuijzen van Zanten JJ, Nightingale P, Kitas GD, Koutedakis Y. Individualised aerobic and resistance exercise training improves cardiorespiratory fitness and reduces cardiovascular risk in patients with rheumatoid arthritis. Annals of the rheumatic diseases. 2013;72(11):1819–25. [DOI] [PubMed] [Google Scholar]
- 50.Baillet A, Zeboulon N, Gossec L, Combescure C, Bodin LA, Juvin R, et al. Efficacy of cardiorespiratory aerobic exercise in rheumatoid arthritis: meta-analysis of randomized controlled trials. Arthritis Care Res (Hoboken). 2010;62(7):984–92. [DOI] [PubMed] [Google Scholar]