Abstract
Objectives:
The objectives of this study were to investigate psychosocial outcomes in a sample of prelingually deaf, early-implanted children, adolescents, and young adults who are long-term cochlear implant (CI) users and to examine the extent to which language and executive functioning predict psychosocial outcomes.
Design:
Psychosocial outcomes were measured using two well-validated, parent-completed checklists: the Behavior Assessment System for Children and the Conduct Hyperactive Attention Problem Oppositional Symptom. Neurocognitive skills were measured using gold standard, performance-based assessments of language and executive functioning.
Results:
CI users were at greater risk for clinically significant deficits in areas related to attention, oppositional behavior, hyperactivity–impulsivity, and social-adaptive skills compared with their normal-hearing peers, although the majority of CI users scored within average ranges relative to Behavior Assessment System for Children norms. Regression analyses revealed that language, visual–spatial working memory, and inhibition–concentration skills predicted psychosocial outcomes.
Conclusions:
Findings suggest that underlying delays and deficits in language and executive functioning may place some CI users at a risk for difficulties in psychosocial adjustment.
Keywords: Cochlear implants, Executive functioning, Hearing loss, Language, Psychosocial outcomes
INTRODUCTION
Most research concerning outcomes after cochlear implantation in prelingually deaf children has focused on auditory and proximal spoken language skills (Young & Kirk 2016). Consequently, much less is known about the effects of early auditory deprivation, language delay, and cochlear implantation on critical quality-of-life (QoL) outcomes such as psychosocial functioning. Psychosocial functioning includes social (e.g., self-esteem, leadership, adaptability, isolation), emotional (e.g., responses to challenges and problem solving, anxiety, depression), and behavioral (e.g., aggression, conduct problems) components. Overt behaviors primarily directed toward the external world and characterized by aggression, overactivity, impulsivity, disruptiveness, defiance, and antisocial features that violate age-appropriate social rules are termed as externalizing behavioral problems. Inward behaviors primarily affecting the child’s internal world and characterized by depression, anxiety, and somatic complaints are termed as internalizing behavioral problems (Reynolds & Kamphaus 2015).
Prelingually deaf, cochlear implant (CI) users display highly variable psychosocial outcomes, with some children demonstrating excellent adjustment while others struggle with emotional–behavioral problems or social deficits or delays. Certain domains of psychosocial functioning may be at higher risk in CI users compared with typically developing normal-hearing (NH) children (Dammeyer 2009; Punch & Hyde 2011), suggesting that characteristics associated with a period of early deafness, language delay, and subsequent cochlear implantation present significant challenges to these critical areas of development. For example, many pediatric CI users find forming friendships, socializing with peers, and exerting emotional control to be challenging (Bat-Chava et al. 2005, 2013; Dammeyer 2009; Huber 2005; Punch & Hyde 2011).
Differences in psychosocial functioning between prelingually deaf children and NH peers may begin to emerge even before implantation, when children are CI candidates. Using observational and parent report data, Barker et al. (2009) found that prelingually deaf CI candidates 1.5 to 5 years of age display significantly greater problems with internalizing behaviors (emotional reactivity, anxious/depressed, somatic complaints, and withdrawn) and negativity during play, with a higher proportion falling within the at-risk range, than their NH age-matched peers (Barker et al. 2009). Social competence (the ability to use social skills to interact with others in a flexible manner) and adaptability (the ability to adjust to change and challenge in the environment) have also been reported by preschool students’ teachers to be significantly delayed in a sample of CI candidates 2.5 to 5.3 years of age when compared with NH age-matched controls (Hoffman et al. 2015). Of the demographic and hearing history variables analyzed, Hoffman et al. (2015) report age at diagnosis and amplification to be negatively associated with higher teacher-reported social competence and adaptability scores, suggesting that early hearing intervention may serve as one possible protective factor against developing delays in psychosocial functioning. Similarly, Stika et al. (2015) describe the benefits of early identification, amplification, and intervention services for psychosocial outcomes of 12- to 18-month-old children with hearing loss. Parent reports revealed that children with bilateral mild-to-severe hearing loss displayed externalizing (impulsivity, defiance, peer aggression) and internalizing (depression, anxiety, separation distress, inhibition to novelty) behaviors, and communication and social skills comparable to a sample of NH peers. However, one cannot draw direct comparisons between this and previous work, because Stika et al. collected parent-reported data on younger children with milder degrees of hearing loss (68% of the sample were diagnosed with mild-to-moderate hearing loss), whereas Quittner and colleagues (Barker et al. 2009; Hoffman et al. 2015) collected teacher-reported data on older children with severe-to-profound hearing loss who were CI candidates.
Studies examining the effects of deafness on psychosocial functioning also report group differences between deaf children without CIs and their NH peers. For example, Van Eldik et al. (2016) asked the parents of 238 profoundly deaf children and adolescents 4- to 18-year-olds to complete the Child Behavior Checklist (Achenbach 1991), a questionnaire that assessed 10 domains of psychosocial functioning including internalizing and externalizing behaviors, and provided an aggregate total problem score. On the basis of parent reports, a greater percentage of deaf children and adolescents (41% of the sample) displayed total problem scores within the borderline to clinically significant range, indicating that the deaf children were 2.6 times more likely than the NH normative sample to have psychosocial problems. Chronological age and intellectual functioning were also found to be associated with deaf children and adolescents psychosocial outcomes. Deaf children and adolescents with lower intelligence scores were reported to have more attention, thought, and social problems, while deaf adolescents were reported to have more anxiety, depression, and social problems than their younger deaf peers.
Of the studies examining psychosocial outcomes after cochlear implantation, most have focused on CI users during school age and adolescence. For example, Hoffman et al. (2016) created a social competence composite score from the adaptability and social skills subscales of the parent-completed Behavior Assessment System for Children (BASC-2; Reynolds & Kamphaus 2004) and the parent-completed Social Skills Rating System (Gresham & Elliott 1990) and found that across the first 8 years after implantation, school-age CI users displayed significantly lower social competencies than their NH peers. Further, Huber (2005) investigated school-age and adolescent CI users’ health-related QoL, including psychological well being, self-esteem, and social functioning. CI users 8 to 12 years of age self-reported significantly lower (poorer) levels of QoL than their NH peers, whereas no differences were found on a global score of QoL between CI users 13 to 16 years of age and their NH peers.
Warner-Czyz et al. (2009) conducted one of the few studies to examine aspects of psychosocial functioning in younger, preschool CI users 4 to 7 years of age. They compared preschool CI users’ self- and parent-reported QoL using the Kiddy KINDL. The Kiddy KINDL assesses six health-related domains of QoL, including physical health, emotional well being, selfesteem, family, friends, and everyday school functioning. The interview version of the Kiddy KINDL consists of 12 items rated by children on a three-point scale (never, sometimes, very often), while the parent version consists of 46 items rated on a five-point scale (never, seldom, sometimes, often, all the time). In both versions of the assessment, domain scores are summed to create a total QoL score. Results revealed that preschool CI users and NH peers did not differ on their self-reported total QoL scores. However, parent-reported ratings of QoL were significantly lower (poorer) than those self-reported by preschool CI users, perhaps suggesting that abstract concepts such as proud and bored were interpreted differently or may reflect differences between parental and self-expectations. Freeman et al. (2017) also examined psychosocial functioning in a sample of preschool CI users. Using the parent-completed BASC-2, CI users 3 to 7 years of age displayed significantly higher (poorer) levels of hyperactivity, somatization, attention problems, atypicality, and withdrawal, and lower (poorer) levels of adaptability, social skills, and functional communication when compared with their NH peers. However, preschool CI users did not differ from their NH peers on domains of aggression, anxiety, depression, and activities of daily living.
Not all studies report maladaptive psychosocial functioning in CI users. Nicholas and Geers (2003) examined self-competence in a large group of school-aged CI users (implanted under the age of 5.5 years and 8 to 9 years at the time of testing) and obtained parent ratings of child adjustment. Although a NH sample was not obtained for comparison, using the Picture Assessment of Self-Image for Children with CIs, CI users selfreported competence across domains of cognitive, physical, social, school, and communication. Similarly, parent reports revealed competence in the domains of social adjustment, selfimage, and emotional adjustment.
Because hearing loss does not seem to affect all domains of psychosocial functioning equally and because of the large individual variability in outcomes, Moeller (2007) urged the field to move from reporting group differences toward identifying and explaining sources of variability in psychosocial outcomes and the underlying processes that lead to them. It is likely that atrisk underlying neurocognitive processes, such as language and executive functioning (EF; the self-regulation of thought, behavior, and emotion in the service of goal attainment), account for a large portion of unexplained individual variability in psychosocial outcomes in CI users. Cognitive–behavioral theory and research suggest that language plays a direct and central role in how young children develop schema-based assumptions and processing strategies for how they interpret and react (either internalize or externalize behaviors) to individuals and events around them (Kendall 2011; Villabø et al. 2013). Furthermore, EF and language are robustly connected via feedback loops that include attention and working memory, which are stronger in CI users than in NH peers (Kronenberger et al. 2014).
Previous research has revealed associations between language and psychosocial adjustment in prelingually deaf children. In one study, young CI candidates with better language and attentional skills had better psychosocial outcomes as indexed by observational and parent-reported measures (Barker et al. 2009). Other research also indicates that CI users with better language skills during elementary school have better self- and parent-reported psychosocial outcomes during adolescence (Moog et al. 2011). CI users with higher speech perception, speech intelligibility, and reading scores were rated by their parents during adolescence as displaying average or better levels of assertive (e.g., asking questions, introducing oneself) and cooperative (e.g., helping others, following rules and directions) behaviors (Moog et al. 2011).
EF skills may also help to explain the heterogeneity of CI users’ psychosocial strengths and difficulties. Caspi et al. (1995) found that behavioral ratings by an examiner based on observations of NH children’s self-control at age 3 were predictive of parent- and teacher-reported externalizing problems (hyperactivity, inattention, antisocial behavior) in adolescence. Similarly, Snyder et al. (2004) studied a large cohort of NH children and found that a composite measure of EF, comprised of both behavioral and questionnaire data, was predictive of parent- and teacher-reported conduct problems at school entry and change in conduct problems over the first 2 years of formal schooling. Social maturity, a construct that includes the understanding and use of age-appropriate social skills, has also been linked with EF. More recently, Marschark et al. (2017) found that poor self-reported EF skills were associated with more immature behaviors in high school and college-aged deaf students with and without CIs. Taken together, the studies reviewed earlier suggest that individual variability in psychosocial functioning is high among CI candidates and young CI users, and that children and adolescents with language and EF delays appear to be more vulnerable to psychosocial difficulties than their typically developing NH peers.
In the present study, we investigated the association between psychosocial outcomes and neurocognitive functioning (language, verbal working memory, visual–spatial working memory, fluency–speed, inhibition–concentration) in prelingually deaf, early-implanted, school-age children, adolescents, and young adults who are long-term CI users (averaged 10.41 years of CI use). Two primary questions concerning the psychosocial functioning of school-age and adolescent CI users were investigated: first, do prelingually deaf, early-implanted, long-term CI users display deficits in psychosocial functioning, compared to their typically developing NH peers? Second, can individual differences in psychosocial functioning be explained by underlying language and EF skills? We predicted that underlying deficits and delays in neurocognitive skills place CI users, compared with their NH peers, at a higher risk for maladaptive psychosocial outcomes. The present study is the first to examine how language and a broad range of EF skills may underlie differences in critical QoL outcomes and identify potential domains of psychosocial functioning that may be at higher relative risk in long-term CI users across the lifespan when compared with their NH peers.
MATERIALS AND METHODS
Participants
CI Sample †
Fifty-seven children, adolescents, and young adults with CIs were recruited from a large university hospital– based CI clinic and local advertisements. CI users were required to meet the following inclusionary criteria: (1) have prelingual severe-to-profound sensorineural hearing loss (>70 dB HL in the better-hearing ear before 2 years of age); (2) have received their CI before 7 years of age; (3) have used their CI for 7 years or more; (4) use a currently available state-of-the-art multichannel CI system; (5) live in a household with spoken English as the primary language; and (6) pass a screening performed by licensed speech–language pathologists before testing, confirming no additional developmental, neurologic, or cognitive conditions were present other than hearing loss.
Demographics and hearing history variables obtained for the CI sample are provided in Table 1 and include age at onset of deafness (defined as the age at which deafness was identified or age at the time of a known event causing deafness, mean = 1.32 months), age at the time of implantation (mean = 30.78 months), preimplant residual hearing (mean unaided pure-tone average = 106.62 in the better-hearing ear for the frequencies 500, 1000, and 2000 Hz in dB HL), duration of CI use at testing (mean = 10.41 years), communication mode at testing [coded on a 1 (mostly sign) to 6 (auditory verbal) scale, with values of 1 to 3 reflecting simultaneous communication strategies (sign and speech to varying degrees of emphasis) and 4 to 6 reflecting oral communication strategies (speech used exclusively with no formal sign language other than gestures); Geers & Brenner 2003], and etiology of deafness. At testing, 86% of the CI users reported using oral communication, while 14% reported using simultaneous communication strategies. Etiology of deafness included unknown (N = 38, 66.7%), familial (at least one immediate family member also had deafness of unknown etiology, N = 10, 17.5%), meningitis (N = 3, 5.3%), Mondini malformation (N = 3, 5.3%), auditory neuropathy (N = 2, 3.5%), and large vestibular aqueduct (N = 1, 1.8%).
TABLE 1.
Participant demographics and hearing history
| Hearing Status |
|||||||
|---|---|---|---|---|---|---|---|
| CI |
NH |
||||||
| 57 |
53 |
||||||
| N | M (SD) | Range | M (SD) | Range | |||
| Onset of deafness (mos) | 1.32 (4.76) | 0.00–24.00 | — | — | |||
| Child | 0.08 (0.41) | 0.00–2.00 | |||||
| Adolescent | 2.21 (6.12) | 0.00–24.00 | |||||
| Age at implantation (mos) | 30.78 (16.85) | 8.28–75.76 | — | — | |||
| Child | 21.30 (9.96) | 8.28–54.54 | |||||
| Adolescent | 37.67 (17.59) | 17.25–75.76 | |||||
| Age at testing (yrs) | 12.98 (3.07) | 7.80–19.13 | 13.08 (2.77) | 7.08–19.80 | |||
| Child | 10.15 (1.17) | 7.80–11.79 | 10.05 (1.27) | 7.08–11.85 | |||
| Adolescent | 15.04 (2.27) | 12.08–19.13 | 14.63 (1.90) | 12.02–19.80 | |||
| Duration of CI use (yrs) | 10.41 (2.44) | 7.08–15.70 | — | — | |||
| Child | 8.37 (1.26) | 7.08–10.63 | |||||
| Adolescent | 11.90 (1.97) | 8.18–15.70 | |||||
| Preimplant PTA* | 106.62 (11.79) | 85.00–118.43 | — | — | |||
| Child | 107.41 (11.78) | 85.00–118.43 | |||||
| Adolescent | 106.02 (11.95) | 85.00–118.43 | |||||
| CMRS | 4.63 (0.96) | 1.00–5.00 | — | — | |||
| Child | 4.67 (0.96) | 1.00–5.00 | |||||
| Adolescent | 4.61 (0.97) | 2.00–5.00 | |||||
| Nonverbal Intelligence† | 54.75 (7.67) | 32.00–68.00 | 55.51 (7.58) | 38.00–70.00 | |||
| Child | 57.46 (7.31) | 32.00–68.00 | 58.67 (8.42) | 47.00–70.00 | |||
| Adolescent | 52.79 (7.43) | 35.00–65.00 | 53.89 (6.66) | 38.00–66.00 | |||
| Count (% of Sample) |
|||||||
| Age at testing (yrs)‡ | |||||||
| Child: 6–11 | 24 (42.10) | 18 (34.0) | |||||
| Adolescent: 12–21 | 33 (57.9) | 35 (66.0) | |||||
| Hearing device | — | ||||||
| Bilateral CI | 23 (40.35) | ||||||
| Unilateral CI | 31 (54.39) | ||||||
| CI and HA | 3 (5.26) | ||||||
| Etiology of hearing loss | — | ||||||
| Meningitis | 3 (5.3) | ||||||
| Other/unknown | 54 (94.7) | ||||||
| Gender | |||||||
| Female | 26 (45.6) | 28 (52.8) | |||||
| Male | 31 (54.4) | 25 (47.2) | |||||
| Race | |||||||
| Black | — | 8 (15.1) | |||||
| Multiracial | 1 (1.8) | 4 (7.5) | |||||
| Asian | 2 (3.5) | 2 (3.8) | |||||
| White | 54 (94.7) | 39 (73.6) | |||||
| Ethnicity | |||||||
| Hispanic | 2 (3.5) | 1 (1.9) | |||||
| Not Hispanic | 55 (96.5) | 52 (98.1) | |||||
| Income level | |||||||
| <$5000 | — | 1 (1.9) | |||||
| $5–9999 | — | — | |||||
| $10–14,999 | 2 (3.5) | 1 (1.9) | |||||
| $15–24,999 | 3 (5.3) | 2 (3.8) | |||||
| $25–34,999 | 6 (10.5) | 3 (5.7) | |||||
| $35–49,999 | 6 (10.5) | 10 (18.9) | |||||
| $50–64,999 | 5 (8.8) | 8 (15.1) | |||||
| $65–79,999 | 6 (10.5) | 5 (9.4) | |||||
| $80–94,999 | 11 (19.3) | 1 (1.9) | |||||
| >$95,000 | 13 (22.8) | 18 (34) | |||||
Preimplant unaided PTA in the better ear for the frequencies 500, 1000, and 2000 Hz in dB HL.
WASI matrix reasoning subtest t score for nonverbal intelligence.
We adhered to the age breakdown as presented in the BASC manual. Parents of participants 6–11 years of age received the child form of the BASC, while parents of participants 12–21 years of age received the adolescent form of the BASC.
BASC, Behavior Assessment System for Children; CI, cochlear implant; CMRS, Communication Mode Rating Scale; HA, hearing aid; NH, normal hearing; PTA, pure-tone average; SD, standard deviation; WASI, Wechsler Abbreviated Scale of Intelligence.
NH Control Sample †
Participants in the NH control sample were 53 children, adolescents, and young adults who passed a basic audiometric hearing screening (headphones were used to test each ear individually at frequencies of 500, 1000, 2000, and 4000 Hz at 20 dB HL), and reported no significant developmental, neurologic, or cognitive delays. NH peers were recruited from advertisements placed in the community. Characteristics of the NH sample are also summarized in Table 1. Demographic variables coded for the CI and NH samples included chronological age (CI users’ mean age = 12.98 years, NH peers’ mean age = 13.08 years), gender (49.1% female, 50.9% male), race/ethnicity (97.3% not Hispanic, 2.7% Hispanic), and family income.
Procedure
All study procedures were reviewed and approved by the local Institutional Review Board, and written informed consent was obtained for all participants or parents before initiation of study procedures. All behavioral and questionnaire assessments were selected to be age appropriate for all children and adolescents in our study. Licensed speech–language pathologists evaluated all CI users and administered the language tests in the participant’s mode of communication used at school or (for those not in school) in the participant’s preferred mode of communication (either oral or total communication). Speech–language pathologists or experienced psychometric technicians evaluated the NH participants. A licensed clinical psychologist (W.G.K) supervised all examiners.
Measures
Nonverbal Intelligence †
The matrix reasoning subtest of the Wechsler Abbreviated Scale of Intelligence (WASI; Wechsler 1999), which is applicable for children as young as 6 years, was used to assess global nonverbal intelligence. The WASI matrix reasoning subtest presents geometric designs in a matrix where each design either remains constant or changes in each cell. Below the matrix are five possible response boxes, each containing a design. Participants must complete the pattern of geometric designs contained in the matrix by selecting one of the five response boxes. Raw scores were converted into t scores to provide an age-standardized measure of nonverbal intelligence.
Psychosocial Outcomes †
Two parent-completed checklists, the BASC-2 (N = 57 CI users and N = 53 NH peers; Reynolds & Kamphaus 2004) and the Conduct Hyperactive Attention Problem Oppositional Symptom (CHAOS; N = 57 CI users and N = 52 NH peers; Levy et al. 2017) scales, were used to assess psychosocial (social, emotional, and behavioral) outcomes. Parents were provided with one of two forms of the BASC-2 scale: child (applicable for 6 to 11 years of age) or adolescent (applicable for 12 to 21 years of age). Forty-two (38.2%) parents completed the 160-item child version of the BASC-2 (N = 24 CI users and N = 18 NH peers), while 68 (61.8%) parents completed the 150-item adolescent version of the BASC-2 (N = 33 CI users, N = 35 NH peers).
BASC-2 items are divided into clinical and adaptive scales that are aggregated to create four indices: externalizing problems index (composite of hyperactivity, aggression, and conduct problems scales), internalizing problems index (composite of anxiety, depression, and somatization scales), behavioral symptoms index (composite of hyperactivity, aggression, depression, atypicality, withdrawal, and attention problems scales), and an adaptive skills index (composite of adaptability, social skills, leadership, activities of daily living, and functional communication skills scales). BASC-2 scale and index scores are compared separately by gender to a normative group of nonreferred children, adolescents, and young adults (although the adolescent form of the parent-completed BASC-2 is applicable for 12–21 years of age, the manual only provides norms up to 18 years. Consequently, N = 1 CI user 19 years of age was compared against the gender-specific norms for 18-year-old young adults). Higher t scores on BASC clinical scales constituting the externalizing problem index, the internalizing problem index, and the behavioral symptoms index indicate behavioral deficits (at-risk: t score range 60 to 69; clinically significant: t scores ≥70). Lower t scores on BASC adaptive scales constituting the adaptive skills index indicate maladaptive deficits (at-risk: t score range 31 to 40; clinically significant: t scores ≤30).
The CHAOS contains 22 items divided into four scales: conduct problems (antisocial and rule-breaking behavior such as stealing), hyperactivity–impulsivity (fidgeting, interrupting), attention problems (inability to maintain attention), and oppositional behavior (irritable mood, defiance). Parents rate the child’s frequency of behavior on a four-point scale, ranging from 0 (never) to 3 (almost always), such that higher raw scores on CHAOS scales indicate greater behavioral problems. Instead of norm-referenced scores, the CHAOS provides criterion-referenced scores that yield information about the degree to which psychosocial behaviors cause problems in everyday functioning (borderline problem: raw score range 5 to 9; problem: raw scores ≥10; Levy et al. 2017). The psychometrics of the CHAOS scale were validated in a sample of 205 children and adolescents 6 to 17 years of age and indicate medium-to-high internal consistency, medium-to-high interrater reliability, and satisfactory test–retest reliability over 10 to 26 weeks (Levy et al. 2017). Validity of CHAOS subscales was shown by strong correlations with another well-established behavior checklist as well as modest correlations with neurocognitive tests of EF. CHAOS subscale scores also differentiated children with diagnoses of attention-deficit/hyperactivity disorder, conduct or oppositional-defiant disorder, and no psychiatric diagnosis (Levy et al. 2017).
Neurocognitive Composite Scores †
A broad range of gold standard neurocognitive tests with strong psychometrics including internal consistency, test–retest reliability, and construct validity were administered in their standardized format using spoken instructions when appropriate.
Five composite scores were created from individual neurocognitive assessments: (1) language; (2) verbal working memory; (3) visual–spatial working memory; (4) fluency–speed; and (5) inhibition–concentration.
Language †
Standard scores on the Peabody Picture Vocabulary Test, Fourth edition (PPVT-4; Dunn & Dunn 2007) and core language standard scores from the Clinical Evaluation of Language Fundamentals, Fourth edition (CELF-4; Semel et al. 2003) were used to assess language skills. The PPVT-4 is applicable for children as young as 2 years 6 months, and the CELF-4 is applicable for children as young as 5 years. The PPVT-4 is a measure of receptive vocabulary skills, while the core language score of the CELF-4 is a measure of general receptive and expressive language skills. For CI users using total communication (N = 8, 14%), signed exact English accompanied the administration of these language tests.
Verbal Working Memory †
Scaled scores on the “digit span” subtest of the Wechsler Intelligence Scale for Children, Third Edition (WISC-III; Wechsler 1991) and scaled scores on the “visual digit span” subtest of the WISC, Fourth Edition, Integrated (WISC-IV-I; Wechsler et al. 2004) were used to assess verbal working memory capacity. The WISC is applicable for children as young as 6 years. The digit span subtest of the WISC-III requires participants to verbally reproduce a sequence of spoken digits presented in forward (digit span forward) or backward (digit span backward) order, while the visual digit span subtest of the WISC-IV-I requires participants to verbally reproduce a sequence of visually presented digits in forward order.
Visual–Spatial Working Memory †
Scaled scores on the spatial span subtest of the WISC-IV-I (Wechsler et al. 2004) were used to assess visual–spatial working memory capacity. The spatial span subtest of the WISC-IV-I, which is applicable to children as young as 6 years, requires participants to reproduce a sequence of blocks tapped by the experimenter in forward (spatial span forward) or backward (spatial span backward) order.
Fluency–Speed †
Standard scores on the “pair cancellation” subtest of the Woodcock–Johnson Tests of Cognitive Abilities, Third Edition (Woodcock et al. 2001) and scaled scores on the “coding” and “coding copy” subtests of the WISC-IV-I (Wechsler et al. 2004) were used to assess fluency–speed skills. The pair cancellation subtest of the Woodcock–Johnson Tests of Cognitive Abilities, Third Edition, which is applicable for children as young as 2 years, requires participants to rapidly identify pictures within visual stimulus arrays. The coding subtest of the WISC-IV-I, which is applicable for children as young as 6 years, requires participants to rapidly reproduce a sequence of visually unique symbols based on corresponding numerals, while the coding copy subtest requires participants to rapidly reproduce visual symbols (from the coding subtest), without the corresponding numerals.
Inhibition–Concentration †
Omissions, commissions, and response time variability standard scores from the Test of Variables of Attention (TOVA; Leark et al. 1996) were used to assess inhibition–concentration skills. The TOVA, which is applicable for children as young as 4 years, requires participants to press a button when presented with a target stimulus (a square at the top of the screen) but not when presented with a distractor stimulus (a square at the bottom of the screen). Measures of omissions (failing to respond to the target), commissions (responding inaccurately to the distractor), and response time variability (variability in speed of button press in response to the target) were collected from the TOVA.
Data Analysis
Composite Score Derivation †
Composite scores for language, verbal working memory, visual–spatial working memory, fluency–speed, and inhibition–concentration were created by summing z-transformed scores (based on the means and standard deviations in the present study sample) on the individual neurocognitive assessments (see Geers, Brenner, & Davidson, 2003; Kronenberger, Colson et al., 2014 for support of this technique). Composite scores were then used for all correlation and regression analyses.
Relations Between Psychosocial Outcomes and Neurocognitive Skills †
Two-tailed independent sample t tests were used to compare CI and NH participants on scores from the BASC and CHAOS. Next, to examine the relations between neurocognitive skills and psychosocial outcomes, composite scores of language, verbal working memory, visual–spatial working memory, fluency–speed, and inhibition–concentration were correlated with scores from the BASC and CHAOS with nonverbal intelligence (WASI matrix reasoning) statistically controlled. These partial correlational analyses were carried out separately for the CI and NH participants. Last, to evaluate the independent contribution of neurocognitive skills to psychosocial outcomes, while also accounting for demographic and hearing history variables, hierarchical regression analyses were conducted with each BASC index and CHAOS subscale score as the criterion variable and blocks of variables entered sequentially as follows: block 1 consisted of demographic variables (chronological age and income); block 2 consisted of hearing status (CI, NH); and block 3 consisted of neurocognitive skills (language, verbal working memory, visual–spatial working memory, fluency– speed, and inhibition–concentration). Because of the large number of variables in block 3, variables were entered using a forward stepwise entry technique.
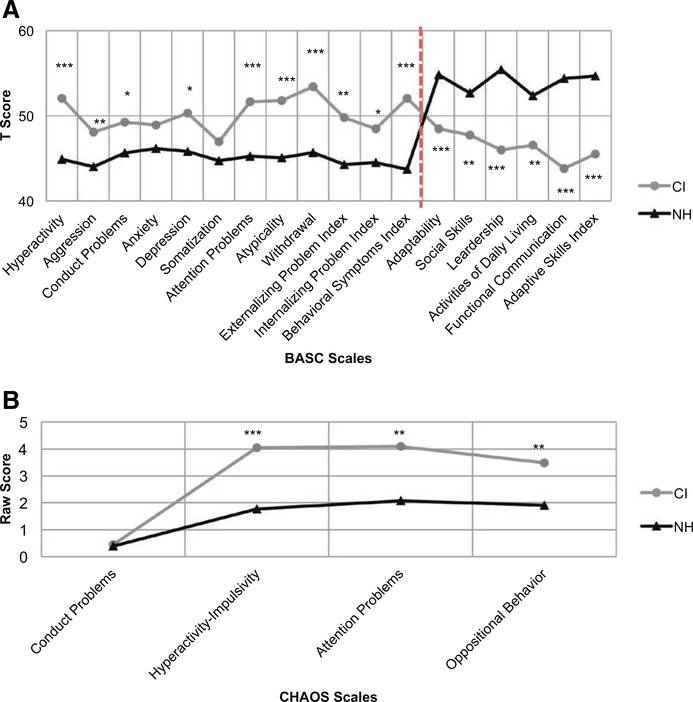
RESULTS
CI and NH samples did not differ on nonverbal intelligence scores [t(108) = −0.52, p = 0.61, d = −0.10], age [t(108) = −0.18, p = 0.86, d = −0.03), gender (p = 0.57 by Fisher exact test), or family income [t(99) = 0.05, p = 0.96, d = 0.01; Table 1]. Psychosocial outcomes for CI users and NH controls are shown in Figure 1. CI users differed significantly from the NH controls on all subscales of the BASC (Fig. 1A) except on the anxiety [t(108) = 1.50, p = 0.17, d = 0.26] and somatization [t(108) = −0.18, p = 0.14, d = 0.29] subscales. When comparing scores on the four BASC indices, CI users displayed significantly greater levels of behavior problems [externalizing problem index, t(108) = 3.58, p = 0.001, d = 0.69; internalizing problem index, t(108) = 2.27, p = 0.03, d = 0.43; and behavioral symptoms index, t(108) = 5.01, p < 0.000, d = 0.96], and significantly lower adaptive skills [adaptive skills index, t(108) = −4.93, p < 0.000, d = −0.94] than NH peers. CI users also differed significantly from NH peers on the CHAOS (Fig. 1B) subscales of hyperactivity–impulsivity [t(107) = 3.95, p < 0.000, d = 0.77], oppositional behavior [t(107) = 2.64, p = 0.01, d = 0.51], and attention problems [t(107) = 3.36, p = 0.001, d = 0.65]. Descriptive statistics for psychosocial and neurocognitive skills are reported in Table 2.
Figure 1.
Group difference in psychosocial outcomes. A, BASC parent-reported scales that significantly differ between CI and NH participants (collapsed across age). N = 57 CI users and N = 53 NH peers. Higher t scores on scales constituting the externalizing problem index, the internalizing problem index, and the behavioral symptoms index indicate behavioral deficits (scales to the left of vertical dashed line). Lower t scores on scales constituting the adaptive skills index indicate maladaptive behaviors (scales to the right of vertical dashed line). ***p < 0.001; **p < 0.01; *p < 0.05. B, CHAOS parent-reported scales that significantly differ between CI and NH participants (collapsed across age). N = 57 CI users and N = 52 NH peers. Higher raw scores indicate greater behavioral problems. ***p < 0.001; **p < 0.01. BASC indicates Behavior Assessment System for Children; CHAOS, Conduct Hyperactive Attention Problem Oppositional Symptom; CI, cochlear implant; NH, normal hearing.
TABLE 2.
Descriptive statistics for psychosocial outcomes and neurocognitive skills
| Hearing Status |
||||||
|---|---|---|---|---|---|---|
| CI |
NH |
|||||
| Measures | N | M (SD) | Range | N | M (SD) | Range |
| Psychosocial questionnaires | ||||||
| BASC indices | ||||||
| Externalizing problem | 57 | 49.81 (9.39) | 36.00–76.00 | 53 | 44.26 (6.45) | 35.00–61.00 |
| Internalizing problem | 57 | 48.47 (9.87) | 34.00–78.00 | 53 | 44.49 (8.44) | 34.00–77.00 |
| Behavioral symptoms | 57 | 52.05 (10.48) | 33.00–85.00 | 53 | 43.72 (6.29) | 34.00–59.00 |
| Adaptive skills | 57 | 45.49 (10.63) | 16.00–69.00 | 53 | 54.66 (8.72) | 38.00–69.00 |
| CHAOS subscales | ||||||
| Conduct problems | 57 | 0.44 (1.50) | 0.00–10.00 | 52 | 0.38 (1.12) | 0.00–7.00 |
| Hyperactivity–impulsivity | 57 | 4.05 (3.61) | 0.00–13.00 | 52 | 1.77 (2.17) | 0.00–9.00 |
| Attention problems | 57 | 4.09 (3.68) | 0.00–15.00 | 52 | 2.08 (2.37) | 0.00–10.00 |
| Oppositional behavior | 57 | 3.49 (3.55) | 0.00–15.00 | 52 | 1.90 (2.60) | 0.00–12.00 |
| Neurocognitive composite scores | ||||||
| Language | ||||||
| PPVT-4 | 57 | 89.91 (20.66) | 42.00–124.00 | 53 | 113.96 (16.07) | 79.00–146.00 |
| CELF-core | 52 | 88.75 (24.52) | 42.00–124.00 | 53 | 112.34 (10.95) | 81.00–129.00 |
| Verbal working memory | ||||||
| WISC-III digit span forward | 56 | 7.00 (2.78) | 2.00–12.00 | 53 | 10.26 (3.13) | 4.00–15.00 |
| WISC-III digit span backward | 56 | 8.41 (3.04) | 1.00–16.00 | 53 | 10.15 (3.44) | 5.00–17.00 |
| WISC-IV-I visual digit span forward | 57 | 8.51 (3.02) | 1.00–15.00 | 53 | 11.87 (2.30) | 2.00–15.00 |
| Visual–spatial working memory | ||||||
| WISC-IV-I spatial span forward | 57 | 9.77 (2.67) | 5.00–16.00 | 53 | 10.98 (2.81) | 6.00–17.00 |
| WISC-IV-I spatial span backward | 56 | 10.89 (2.71) | 5.00–16.00 | 53 | 11.49 (2.51) | 5.00–16.00 |
| Fluency–speed | ||||||
| WJ-III pair cancellation | 57 | 99.02 (11.36) | 66.00–127.00 | 53 | 102.60 (8.50) | 73.00–120.00 |
| WISC-IV-I coding | 57 | 8.58 (2.87) | 2.00–15.00 | 53 | 9.74 (2.94) | 5.00–17.00 |
| WISC-IV-I coding copy | 57 | 9.40 (2.95) | 2.00–16.00 | 52 | 10.49 (3.14) | 4.00–18.00 |
| Inhibition–concentration | ||||||
| TOVA omissions | 53 | 83.91 (22.64) | 40.00–136.00 | 51 | 97.86 (13.65) | 63.00–123.00 |
| TOVA commissions | 53 | 78.04 (26.87) | 40.00–113.00 | 51 | 92.51 (19.48) | 40.00–113.00 |
| TOVA response time variability | 53 | 83.68 (22.75) | 40.00–119.00 | 51 | 95.12 (16.65) | 40.00–123.00 |
BASC index scores are expressed as t scores (M = 50, SD = 10), and CHAOS subscale scores are expressed as raw scores. The PPVT-4, CELF-core, WJ-III pair cancellation, TOVA omissions, TOVA commissions, and TOVA response time variability scores are expressed as standard scores (M = 100, SD = 15), while all other neurocognitive assessments are expressed as scaled scores (M = 10, SD = 3).
BASC, Behavior Assessment System for Children; CELF, Clinical Evaluation of Language Fundamentals; CHAOS, Conduct Hyperactive Attention Problem Oppositional Symptom; CI, cochlear implant; NH, normal hearing; PPVT-4, Peabody Picture Vocabulary Test, Fourth edition; SD, standard deviation; TOVA, Test of Variables of Attention; WJ-III, Woodcock–Johnson Tests of Cognitive Abilities, Third Edition; WISC-III, Wechsler Intelligence Scale for Children, Third Edition; WISC-IV-I, Wechsler Intelligence Scale for Children, Fourth Edition, Integrated.
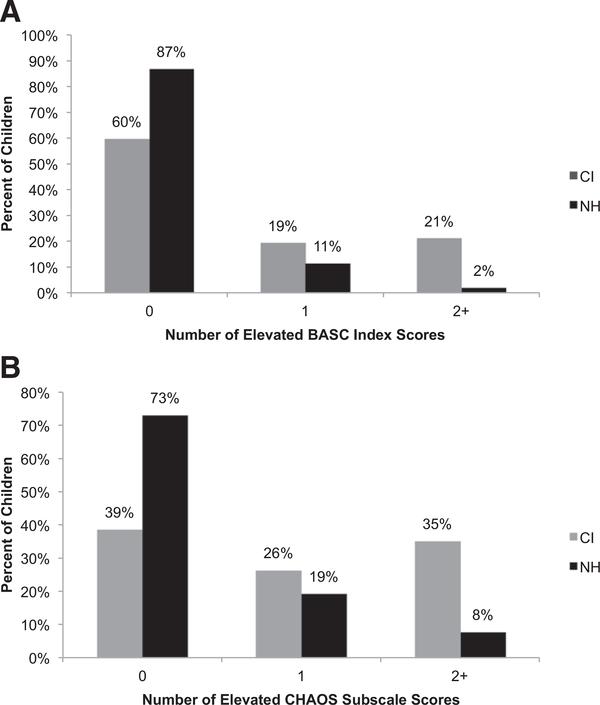
The percent of children with elevated BASC and CHAOS scores (elevated scores are defined in this article as BASC t scores falling within the at-risk to clinically significant range and CHAOS raw scores falling within the borderline problem-to-problem range) and their relative risk for problems in psychosocial outcomes are shown in Table 3. CI users were 2.35 to 4.56 times more likely than their NH peers to display elevations in adaptive skills, hyperactivity–impulsivity, oppositional behavior, and attention problems. On the BASC, a greater percentage of CI users fell within the atrisk to clinically significant range on the externalizing problem index (14.04% of the CI users versus 1.89% of the NH controls, p = 0.03), the behavioral symptoms index (17.54% of the CI users versus 0% of the NH controls, p = 0.001), and the adaptive skills index (29.82% of the CI users versus 7.55% of the NH controls, p = 0.003, all by Fisher exact test). On the CHAOS, a significantly greater percentage of CI users fell within the borderline problem-to-problem range on the hyperactivity–impulsivity scale (35.09% CI users versus 7.69% NH controls, p = 0.001), the oppositional behavior scale (31.58% CI users versus 13.46% NH controls, p = 0.04), and on the attention problems scale (43.86% CI users versus 17.31% NH controls, p = 0.002, all by Fisher exact test). Additionally, the mean number of elevated BASC indices and CHAOS subscales in the CI sample was significantly higher than in the NH sample [t(108) = 3.74, p < 0.000, d = 0.72; t(108) = 3.83, p < 0.000, d = 0.74, respectively). The number of elevated indices/subscales per participant on the BASC (Fig. 2A) and CHAOS (Fig. 2B) are shown in Figure 2.
TABLE 3.
Percent of children with elevated psychosocial scores
| Percentage of Elevated Scores |
Relative Risk (95% Confidence Interval) | ||
|---|---|---|---|
| Questionnaires | CI | NH | |
| N | 57 | 53 | |
| BASC indices | |||
| Externalizing problem | 14.04 | 1.89 | 7.44 (0.96–57.49) |
| Internalizing problem | 17.54 | 5.66 | 3.10 (0.90–10.66) |
| Behavioral symptoms | 17.54 | 0.00 | |
| Adaptive skills | 29.82 | 7.55 | 3.95 (1.42–10.99) |
| N | 57 | 52 | |
| CHAOS subscales | |||
| Conduct problems | 3.51 | 1.92 | 1.82 (0.17–19.54) |
| Hyperactivity-impulsivity | 35.09 | 7.69 | 4.56 (l.67–12.47) |
| Attention problems | 43.86 | 17.31 | 2.53 (1.31–4.92) |
| Oppositional behavior | 31.58 | 13.46 | 2.35 (1.07–5.16) |
Percentages represent children with BASC t scores within the at-risk to clinically significant range and CHAOS raw scores within the borderline problem to problem range. Appearing in bold are relative risks that are statistically significant at p < 0.05.
BASC, Behavior Assessment System for Children; CHAOS, Conduct Hyperactive Attention Problem Oppositional Symptom; CI, cochlear implant; NH, normal hearing.
Figure 2.
Number of elevated psychosocial scores. A, Number of elevated BASC index scores. The BASC contains 4 indices: externalizing problem, internalizing problem, behavioral symptoms, and adaptive skills. Percentages represent children with BASC t scores within the at-risk to clinically significant range. Externalizing problem index, internalizing problem index, and behavioral symptoms index (at-risk: t scores of 60–69; clinically significant: t scores ≥70); adaptive skills index (at-risk: t scores of 31–40; clinically significant: t scores ≤30). B, Number of elevated CHAOS subscale scores. The CHAOS contains 4 subscales: hyperactivity–impulsivity, oppositional behavior, conduct problems, and attention problems. Percentages represent children with CHAOS raw scores within the borderline problem (raw scores of 5–9) to problem (raw scores ≥10) range. BASC indicates Behavior Assessment System for Children; CHAOS, Conduct Hyperactive Attention Problem Oppositional Symptom.
Correlational Analyses
Partial correlations between psychosocial outcomes and neurocognitive skills, controlling for nonverbal intelligence, are shown in Table 4. Results revealed dissociations in the patterns of correlations between the BASC and CHAOS scales and neurocognitive skills for CI users and NH controls. Better language skills were correlated with stronger adaptive skills, fewer attention problems, fewer oppositional behaviors, and fewer global behavioral symptoms (composite of hyperactivity, aggression, depression, atypicality, withdrawal, and attention problems scales) in CI users. Better working memory (verbal and visual– spatial) skills were correlated with fewer attention problems in CI users. Whereas better working memory skills were correlated with fewer internalizing problems and fewer global behavioral symptoms in NH controls. Better inhibition–concentration skills were correlated with fewer global behavioral symptoms, fewer symptoms of hyperactivity–impulsivity, fewer conduct problems, and fewer oppositional behaviors in NH controls. Better fluency–speed skills were correlated with fewer global behavioral symptoms and fewer attention problems in NH controls. Additionally, the correlations between language and adaptive skills and language and attention problems were stronger in the CI sample (r = 0.50; r = −0.39) than in the NH sample (r = 0.17; r = −0.01; Z test comparing the magnitude of these correlations p < 0.05), whereas the correlation between inhibition– concentration and conduct problems was stronger in the NH sample (r = −0.41) than in the CI sample (r = 0.02; p < 0.05).
TABLE 4.
Correlations between BASC and CHAOS psychosocial outcomes, and neurocognitive composite scores for CI and NH participants, controlling for nonverbal intelligence
| Neurocognitive Composite Scores |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Language |
Verbal Working Memory |
Visual–Spatial Working Memory |
Fluency–Speed |
Inhibition–Concentration |
||||||
| Questionnaires | CI | NH | CI | NH | CI | NH | CI | NH | CI | NH |
| df | 54 | 50 | 54 | 50 | 54 | 50 | 54 | 50 | 50 | 48 |
| BASC indices | ||||||||||
| Externalizing problems | −0.20 | −0.15 | −0.13 | −0.26 | −0.10 | −0.20 | −0.24 | −0.10 | −0.24 | −0.26 |
| Internalizing problems | −0.22 | −0.21 | −0.21 | −0.18 | −0.23 | −0.28* | −0.12 | −0.20 | −0.12 | −0.09 |
| Behavioral symptoms | −0.39† | −0.20 | −0.24 | −0.31* | −0.21 | −0.24 | −0.22 | −0.29* | −0.26 | −0.31* |
| Adaptive skills | 0.50‡ | 0.17 | 0.19 | 0.13 | 0.26 | 0.12 | 0.06 | 0.18 | 0.15 | 0.04 |
| df | 54 | 49 | 54 | 49 | 54 | 49 | 54 | 49 | 50 | 47 |
| CHAOS subscales | ||||||||||
| Conduct problems | −0.15 | 0.02 | −0.16 | −0.28* | 0.19 | −0.06 | −0.02 | 0.02 | 0.02 | −0.41† |
| Hyperactivity–impulsivity | −0.08 | −0.12 | −0.12 | −0.13 | −0.06 | −0.05 | −0.12 | 0.04 | −0.22 | −0.35* |
| Attention problems | −0.39† | −0.01 | −0.33† | −0.27 | −0.30* | −0.14 | −0.10 | −0.28* | −0.24 | −0.15 |
| Oppositional behavior | −0.28* | −0.05 | −0.13 | −0.23 | 0.05 | −0.11 | −0.14 | −0.13 | −0.10 | −0.41† |
p < 0.05.
p < 0.01.
p < 0.001.
BASC, Behavior Assessment System for Children; CHAOS, Conduct Hyperactive Attention Problem Oppositional Symptom; CI, cochlear implant; Df, degrees of freedom; NH, normal hearing.
Regression Models Predicting Psychosocial Outcomes
Table 5 displays a summary of results from the regression analyses using demographic factors (chronological age, gender, and income), hearing status (CI, NH), and neurocognitive composite scores (language, verbal working memory, visual–spatial working memory, fluency–speed, and inhibition–concentration) as predictors of psychosocial (BASC, CHAOS) outcomes. For most of the equations, the regression coefficients of the traditional demographic and hearing history variables were attenuated after the entry of neurocognitive composite scores. Better language skills significantly predicted stronger adaptive skills and the overall equation, which included demographic and hearing history variables, accounted for 30% of the variance in BASC adaptive skills index scores (p < 0.001). Better language and inhibition–concentration skills predicted significantly fewer global behavioral symptoms, and the overall equation with demographic and hearing history variables (which were significantly attenuated) accounted for 35% of the variance in BASC behavioral symptoms index scores (p < 0.001). Better inhibition–concentration skills predicted significantly fewer oppositional behaviors, with the overall equation accounting for 12% of the variance in CHAOS oppositional behavior scores (p < 0.05). Additionally, better visual–spatial working memory skills predicted significantly fewer internalizing problems as indexed by the BASC internalizing problems index score, with the overall equation accounting for 16% of the variance. The overall equation with visual–spatial working memory, language, demographic, and hearing history variables predicted 25% of the variance in CHAOS attention problem scores (p < 0.001), such that better visual–spatial working memory and language skills predicted fewer parent-reported attention problems.
TABLE 5.
Regression models predicting BASC and CHAOS psychosocial outcomes
| BASC Psychosocial Indices |
CHAOS Psychosocial Subscales |
|||||||
|---|---|---|---|---|---|---|---|---|
| Externalizing Problems |
Internalizing Problems |
Behavioral Symptoms |
Adaptive Skills |
Conduct Problems |
Hyperactivity–Impulsivity |
Attention Problems |
Oppositional Behavior |
|
| β | β | β | β | β | β | β | β | |
| Block 1: demographics | ||||||||
| Chronological age | −0.20* | 0.16 | −0.05 | 0.01 | −0.03 | −0.32† | −0.12 | −0.17 |
| Gender | −0.06 | 0.00 | −0.05 | 0.02 | −0.10 | −0.02 | −0.15 | −0.13 |
| Income | −0.20 | −0.17 | −0.26* | 0.19 | −0.15 | −0.00 | 0.17 | −0.14 |
| R2 | 0.08* | 0.05 | 0.07 | 0.03 | 0.02 | 0.07* | 0.06 | 0.07 |
| Block 2: hearing status | ||||||||
| Chronological age | −0.20* | 0.16 | −0.06 | 0.01 | — | −0.32† | −0.12 | — |
| Gender | −0.03 | 0.02 | −0.01 | −0.02 | — | 0.01 | −0.13 | — |
| Income | −0.19 | −0.16 | −0.25* | 0.17 | — | 0.01 | −0.15 | — |
| Hearing status | −0.29† | −0.21* | −0.42† | 0.42‡ | — | −0.34‡ | −0.29† | — |
| R2 | 0.17† | 0.10 | 0.25‡ | 0.21‡ | — | 0.18‡ | 0.15† | — |
| Block 3: neurocognitive skills | ||||||||
| Chronological age | −0.19 | 0.15 | −0.09 | 0.08 | — | −0.30† | −0.17 | −0.16 |
| Gender | −0.06 | 0.01 | −0.05 | −0.01 | — | −0.02 | −0.14 | −0.14 |
| Income | −0.15 | −0.12 | −0.15 | 0.09 | — | 0.06 | −0.06 | −0.10 |
| Hearing status | −0.21* | −0.14 | −0.17 | 0.20 | — | −0.24* | −0.07 | — |
| Language | — | — | −0.31† | 0.39† | — | — | −0.30* | — |
| Visual–spatial WM | — | −0.27† | — | — | — | — | −0.20* | — |
| Inhibition–concentration | −0.21* | — | −0.21* | — | — | −0.25* | — | −0.24* |
| R2 | 0.20† | 0.16† | 0.35‡ | 0.30‡ | — | 0.23‡ | 0.25‡ | 0.12* |
p < 0.05.
p < 0.01.
p < 0.001.
BASC, Behavior Assessment System for Children; CHAOS, Conduct Hyperactive Attention Problem Oppositional Symptom; WM, working memory.
In only two regression equations did traditional demographic and hearing history variables remain as significant predictors of psychosocial outcomes after the addition of neurocognitive variables to the equation. Hearing status and inhibition–concentration skills predicted significantly lower BASC externalizing problems index scores, such that NH and better inhibition–concentration skills predicted better scores on the BASC externalizing problems index, with the overall equation accounting for 20% of the variance. Hearing status (NH), chronological age (older), and better inhibition–concentration predicted significantly fewer scores on CHAOS hyperactivity– impulsivity, and the overall equation including gender and income accounted for 23% of the variance in these scores (p < 0.001). Last, conduct problems as indexed by the CHAOS were not predicted using traditional demographic and hearing history variables, and neurocognitive composite scores, likely because these behaviors occurred infrequently in both of our NH and CI samples.
DISCUSSION
In this study, we examined psychosocial adjustment and the extent to which language and EF skills were associated with psychosocial outcomes in school-age, adolescent, and young adult CI users, using two well-validated, parent-completed behavior checklists. Our findings indicate that long-term CI users were at elevated risk relative to a NH control sample for developing clinically significant problems in several areas of psychosocial functioning, including adaptive skills, hyperactivity–impulsivity, oppositional behavior, and attention problems. Additionally, a greater percent of CI users than NH controls displayed more than one elevated index/subscale score, suggesting that some CI users experience comorbid psychosocial problems that span across varying domains of functioning (21 to 35% of CI users displayed two or more elevated index/subscale scores on the BASC and CHAOS).
The largest differences in psychosocial functioning between the CI and NH samples were found on BASC and CHAOS subscales assessing hyperactivity–impulsivity, attention problems, atypical behaviors, and social/adaptive competence including withdrawal behaviors. On subscales assessing these areas of psychosocial functioning, the mean score for the CI sample was significantly higher (in the case of behavior problems) or lower (in the case of social-adaptive behaviors) than in the NH sample. Findings of elevated attention problems and hyperactivity– impulsivity scores in CI users are consistent with prior reports of EF delays in samples of CI users (Kronenberger et al. 2014, 2013), and EF has been demonstrated to underlie these types of behaviors in NH children (Barkley 2012). It appears likely that EF delays found to occur in the behaviors of about 30 to 40% of children with CIs (Kronenberger et al. 2014) also influence psychosocial functioning in the form of attention problems and hyperactivity–impulsivity reported by parents. The association between neurocognitive measures of EF and parent-reported attention problems and hyperactivity–impulsivity in the present sample provide further support for this hypothesis.
It is important to note that the current results indicate that not all areas of psychosocial functioning are equally at risk in CI users. CI users did not differ from NH peers in anxiety or somatization scores. Furthermore, on measures of conduct problems and aggression, differences between CI and NH samples were either absent (on the CHAOS) or the CI sample scored, on average, below the normed mean (on the BASC). Thus, for severe externalizing problems and for anxiety-related internalizing problems, there was no consistent evidence that CI users were at greater risk. Even in the case of attention problems, hyperactivity–impulsivity, and social-adaptive behaviors, 56 to 70% of children, adolescents, and young adults with CIs did not fall in at-risk/borderline or clinically significant/problem ranges. Hence, the elevated risk of these problems found in the CI sample reflects an increase in incidence relative to NH peers, but not a certainty of poor outcomes. Rather, high variability and individual differences in psychosocial outcomes in the CI sample suggest that within-group factors are at least as important in affecting psychosocial outcomes as the presence of early hearing loss, language delays, and subsequent implantation. Thus, these results suggest that vigilance about attention problems, hyperactivity–impulsivity, and social-adaptive delays is warranted in the population of children, adolescents, and young adults with CIs. Additionally, the results suggest that the understanding, explanation, and remediation of these psychosocial problems should focus on within-group factors associated with individual differences in social, emotional, and behavioral adjustment.
Because significant variability in psychosocial outcomes was observed in the CI sample, identifying factors predicting individual differences in psychosocial adjustment is crucial in understanding the elevated psychosocial risk encountered by a large minority (as much as 30 to 44% for adaptive skills, inattentive, or hyperactive–impulsive behaviors) of CI users. As a first step toward explaining this variability, we found that several neurocognitive skills, including language and some executive functions, were associated with individual differences in psychosocial functioning.
To understand these within-group factors in explaining individual differences in psychosocial outcomes in children, adolescents, and young adults with CIs, partial correlations were carried out between psychosocial outcomes and neurocognitive composite scores of language, verbal working memory, visual–spatial working memory, fluency–speed, and inhibition– concentration while controlling for nonverbal IQ. Unlike the correlations between CHAOS raw scores and neurocognitive skills, correlations using BASC t scores also accounted for age, as these scores were norm referenced. Different patterns of correlations between neurocognitive composite scores and psychosocial outcomes were found for CI users and NH controls, indicating differences in how these domains of functioning may be associated in CI users relative to NH peers.
In CI users, language scores were significantly associated with two indices of the BASC (adaptive skills and global behavioral problems) and two subscales of the CHAOS (attention problems and oppositional behavior), whereas language scores were not associated with BASC or CHAOS scores in NH peers. In particular, the observed correlations between language and adaptive skills and language and attention problems in CI users were substantially greater than the observed correlations in the NH group. Similarly, verbal and visual–spatial working memory scores were significantly associated with CHAOS measures of attention problems only in CI users. In contrast, inhibition–concentration scores were associated with one index of the BASC (global behavioral problems) and three subscales of the CHAOS (conduct problems, hyperactivity–impulsivity, and oppositional behavior) only in NH peers. In particular, the observed correlation between inhibition–concentration and conduct problems in CI users was substantially greater than the observed correlation between inhibition–concentration and conduct problems in the NH group.
Our findings of a different pattern of relations between neurocognitive processes and psychosocial outcomes in CI users compared with NH peers are revealing because they suggest that psychosocial risks in CI users may be further amplified by language and EF delays. Adopting a developmental neurocognitive perspective, we approach the study of psychosocial functioning as the result of the complex and bidirectional interaction between language and EF skills at multiple points in development, beginning with early mother–infant interactions and progressing through the social–cultural (Castellanos, Pisoni, Kronenberger & Beer, 2016). Language and EF skills are intrinsically linked, and research suggests that reaction time (a core EF) in toddlers 25 months of age is predictive of later lexical and grammatical development (Marchman & Fernald 2008). Similarly, early language skills in young children 2 to 6 years of age are predictive of EF outcomes, an average of 11 years later (Castellanos et al. 2016). Language is a critical tool for developing and managing foundational beliefs about the self and world that are used to appraise, interpret, and respond to challenging situations, both behaviorally and emotionally. Previous research indicates that language processing is often slow and effortful, and not highly automatized in CI users (AuBuchon et al. 2015; Kronenberger et al. 2014); therefore, language dysfluencies provide insufficient support to EF, resulting in inefficient deployment of EF. When this EF processing is necessary for coping with situational or emotional challenges or stress, psychosocial outcomes may also be affected.
With the exception of the verbal working memory tests, all other EF tests used in this study involved visual stimuli with no demands for hearing or spoken responses. Furthermore, all EF tests (other than verbal working memory tests) used nonverbal symbols or spatial locations with the exception of the pair cancellation test, which used simple pictures (dog, ball). Thus, the stimuli and tasks for the EF tests (with the exception of verbal working memory) were designed to minimize verbal loadings. Although we carefully selected EF tasks that reduced the contribution of language, it is possible that some participants in our sample may have used language to mediate their performance on the EF tasks by labeling items (which would be inefficient, but possible) or by using self-talk for self-regulation. Language skills are part of most aspects of EF or self-regulation, but by minimizing the verbal components of the EF tasks, we also sought to reduce the contribution of language. Similarly, EF skills are necessary during language processing. Language tests not only measure language skills but are also influenced by EF components such as controlled attention, concentration, concept formation, and working memory.
Associations between psychosocial functioning and EF have been previously reported in studies of children, adolescents, and young adults with CIs. For example, Barker et al. (2009) and Marschark et al. (2017) found that EF delays may underlie specific areas of maladaptive psychosocial functioning. Parents of pediatric CI candidates report that their deaf children (under 5 years of age and on track for cochlear implantation) display aggressive behaviors within age-appropriate limits (Barker et al. 2009). However, CI candidates’ parents reported that their deaf children display greater problems with internalizing behaviors and attention problems when compared with NH peers. Barker et al. (2009) also found that behavioral measures of sustained attention (a core executive function) significantly predicted parent-reported internalizing behaviors. Marschark et al. (2017) reports that deaf adolescents and young adults (with and without CIs) do not significantly differ from their NH peers with respect to social maturity. However, these deaf individuals did differ on several domains of EF, and delays in attention and visual–spatial organization specifically were related to social immaturity in CI users. Taken together with the present results, these findings suggest that adaptive psychosocial functioning is variable among CI users such that some individuals experience no issues while others are at high risk for developing disturbances in specific areas of psychosocial functioning. Moreover, for the portion of CI users with maladaptive psychosocial outcomes, their delays may be partially attributed to underlying executive dysfunction (e.g., attention, visual–spatial organization).
In our regression analyses, language, visual–spatial working memory, and inhibition–concentration skills were all found to be significantly related to psychosocial outcomes in the combined CI and NH samples even after accounting for hearing status and demographic variables such as age, gender, and income. These results replicate and extend previous findings indicating that proficient use of language and skilled self-control are extremely important for psychosocial functioning (Barker et al. 2009; Caspi et al. 1995; Moog et al. 2011). Barkley (2012) and others have suggested that visual–spatial working memory skills allow individuals to create mental representations and interpret information before action; indeed our findings provide some preliminary support for this premise as poor visual–spatial working memory skills significantly predicted internalizing (anxiety, depression, and somatization) and attention problems.
Several limitations should be considered when interpreting the present results. First, CI users’ psychosocial functioning was measured using parent-completed checklists. Although parent report behavior checklists have been extensively validated (Levy et al. 2017; Reynolds & Kamphaus 2004) and previous studies have shown that parent-completed checklists have good predictive validity of CI users’ psychosocial functioning (Snyder et al. 2004), factors such as parent experiences, bias, and awareness of child behavior can affect behavior ratings and contribute to error in these scores. The risk of these factors affecting parent ratings is particularly great when children are embedded in different cultures or settings with different expectations for behaviors, because parent ratings might reflect child behavior relative to cultural norms or expectations, which may differ from one culture or setting to the next. Because our sample was drawn from deaf children embedded in mainstream schools and contexts with NH children, this risk of biased parent report is substantially reduced, but studies of deaf children who are not embedded in mainstream schools and contexts with NH children would be likely to suffer from this parental bias/expectation effect. Another point to consider is the potential difference between self and parental expectations, which affect behavioral ratings of social, emotional, and physical skills (Eiser & Morse 2001a, 2001b). As such, studies are currently underway in our lab to examine CI users’ psychosocial functioning using behaviorally based tests and self-report checklists.
Second, the purpose of the present study was to investigate psychosocial functioning after long-term CI use, and therefore our sample consisted of participants with a wide age range (from 7.80 to 19.13). Although we found no differences between groups even when accounting for age in our regression analyses, it is likely that developmental influences and differences exist in psychosocial adjustment. Future research with larger samples may provide additional information about these developmental differences. Third, we correlated all subscales from the BASC and CHAOS with the long-term neurocognitive assessments, thereby providing clinicians with comprehensive information about psychosocial functioning across several domains after prelingual deafness and subsequent cochlear implantation. However, by conducting these additional correlations, we increased our risk of experimentwise error and correlational results should be interpreted with caution. Last, we strategically prioritized employing a multimethod approach, using both performance- and questionnaire-based data, to obtain a broader snapshot of psychosocial abilities and behavioral adjustment in deaf children, adolescents, and young adults after cochlear implantation. In doing so, we obtained five neurocognitive composite scores and eight psychosocial index scores thus limiting our ability to perform mediating analyses because following Baron & Kenny’s (1986) model for testing mediating effects, over 100 regressions would be necessary.
In summary, we found that several critical areas of psychosocial functioning, particularly attention problems, hyperactivity–impulsivity, and social-adaptive competence are at elevated risk for problems in children, adolescents, and young adults with CIs, compared with NH peers. On the other hand, the 56 to 70% of CI users showed no at-risk/borderline or clinically significant/problems in these or other areas of psychosocial adjustment. Individual differences in these areas of psychosocial adjustment in CI users were associated with language and several areas of EF, particularly working memory, suggesting that language and EF might explain some of the individual differences observed in psychosocial adjustment within the population of CI users. The present findings are consistent with evidence from prior studies, indicating that a period of early auditory deprivation has proximal effects on language, cascading effects on EF (Castellanos et al., 2015; 2013; Kronenberger, Beer, et al., 2014; Kronenberger, Colson, et al., 2014), and distal effects on QoL outcomes such as psychosocial functioning. These new findings have clinical implications for the early identification and potential intervention to improve psychosocial adjustment in prelingually deaf, early-implanted CI users. Given our findings, it is possible that the large minority of CI users at risk for psychosocial delays (especially the 21 to 35% of CI users who exhibit comorbid psychosocial problems) may benefit from specific interventions targeting language and EF growth during early development (Blair & Diamond 2008; Diamond 2013; Diamond & Lee 2011).
ACKNOWLEDGMENTS
This work was supported by grants from the National Institute on Deafness and Other Communication Disorders: R01 DC009581, R01 DC015257, R21 DC016134, and T32 DC00012, and the National Center for Advancing Translational Sciences TL1 TR001107.
Footnotes
The authors have no conflicts of interest to disclose.
REFERENCES
- Achenbach TM (1991). Integrative Guide for the 1991 CBCL/4–18, YSR, and TRF Profiles. Burlington, VT: University of Vermont, Department of Psychiatry. [Google Scholar]
- AuBuchon AM, Pisoni DB, Kronenberger WG (2015). Verbal processing speed and executive functioning in long-term cochlear implant users. J Speech Lang Hear Res, 58, 151–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker DH, Quittner AL, Fink NE, et al. ; The CDaCI Investigative Team. (2009). Predicting behavior problems in deaf and hearing children: The influences of language, attention, and parent–child communication. Dev Psychopathol, 21, 373–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barkley RA (2012). Executive Functions: What They Are, How They Work, and Why They Evolved. New York, NY: The Guildford Press. [Google Scholar]
- Baron RM, & Kenny DA (1986). The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol, 51, 1173–1182. [DOI] [PubMed] [Google Scholar]
- Bat-Chava Y, Martin D, Imperatore L (2013). Long-term improvements in oral communication skills and quality of peer relations in children with cochlear implants: Parental testimony. Child Care Health Dev, 40, 870–881. [DOI] [PubMed] [Google Scholar]
- Bat-Chava Y, Martin D, Kosciw JG (2005). Longitudinal improvements in communication and socialization of deaf children with cochlear implants and hearing aids: Evidence from parental reports. J Child Psychol Psychiatry, 46, 1287–1296. [DOI] [PubMed] [Google Scholar]
- Blair C, & Diamond A (2008). Biological processes in prevention and intervention: The promotion of self-regulation as a means of preventing school failure. Dev Psychopathol, 20, 899–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Henry B, McGee RO, et al. (1995). Temperamental origins of child and adolescent behavior problems: From age three to age fifteen. Child Dev, 66, 55–68. [DOI] [PubMed] [Google Scholar]
- Castellanos I, Kronenberger WG, Beer J, et al. (2015). Concept formation skills in long-term cochlear implant users. J Deaf Stud Deaf Educ, 20, 27–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castellanos I, Kronenberger WG, Beer J, et al. (2013). Preschool speech intelligibility and vocabulary skills predict long-term speech and language outcomes following cochlear implantation in early childhood. Cochlear Implants Int, 15, 200–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castellanos I, Pisoni DB, Kronenberger WG, et al. (2016). Neurocognitive function in deaf children with cochlear implants: Early development and long-term outcomesIn Marschark M, & Spencer PE (Eds.), The Oxford Handbook of Deaf Studies in Language (pp. 264–275). New York: Oxford University Press. [Google Scholar]
- Dammeyer J (2009). Psychosocial development in a Danish population of children with cochlear implants and deaf and hard-of-hearing children. J Deaf Stud Deaf Educ, 15, 50–58. [DOI] [PubMed] [Google Scholar]
- Diamond A (2013). Executive functions. Annu Rev Psychol, 64, 135–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamond A, & Lee K (2011). Interventions shown to aid executive function development in children 4 to 12 years old. Science, 333, 959–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn LM, & Dunn DM (2007). Peabody Picture Vocabulary Test, Fourth Edition Manual. Bloomington, MN: Pearson. [Google Scholar]
- Eiser C, & Morse R (2001a). Can parents rate their child’s healthrelated quality of life? Results of a systematic review. Qual Life Res, 10, 347–357. [DOI] [PubMed] [Google Scholar]
- Eiser C, & Morse R (2001b). The measurement of quality of life in children: Past and future perspectives. J Dev Behav Pediatr, 22, 248–256. [DOI] [PubMed] [Google Scholar]
- Freeman V, Pisoni DB, Kronenberger WG, et al. (2017). Speech intelligibility and psychosocial functioning in deaf children and teens with cochlear implants. J Deaf Stud Deaf Educ, 22, 278–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geers A, & Brenner C (2003). Background and educational characteristics of prelingually deaf children implanted by five years of age. Ear Hear, 24(Suppl), 2S–14S. [DOI] [PubMed] [Google Scholar]
- Geers A, Brenner C, & Davidson L (2003). Factors associated with development of speech perception skills in children implanted by age five. Ear Hear, 24(Supplement), 24S–35S. [DOI] [PubMed] [Google Scholar]
- Gresham FM, & Elliott SN (1990). Social Skills Rating System: Manual. Circle Pines, MN: American Guidance Service. [Google Scholar]
- Hoffman MF, Cejas I, Quittner AL, et al. (2016). Comparisons of longitudinal trajectories of social competence: Parent ratings of children with cochlear implants versus hearing peers. Otol Neurotol, 37, 152–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman MF, Quittner AL, Cejas I (2015). Comparisons of social competence in young children with and without hearing loss: A dynamic systems framework. J Deaf Stud Deaf Educ, 20, 115–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huber M (2005). Health-related quality of life of Austrian children and adolescents with cochlear implants. Int J Pediatr Otorhinolaryngol, 69, 1089–1101. [DOI] [PubMed] [Google Scholar]
- Kendall PC (2011). Child and Adolescent Therapy: Cognitive-Behavioral Procedures. New York, NY: Guilford Press. [Google Scholar]
- Kronenberger WG, Beer J, Castellanos I, et al. (2014). Neurocognitive risk in children with cochlear implants. JAMA Otolaryngol Head Neck Surg, 140, 608–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kronenberger WG, Colson BG, Henning SC, et al. (2014). Executive functioning and speech-language skills following long-term use of cochlear implants. J Deaf Stud Deaf Educ, 19, 456–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kronenberger WG, Pisoni DB, Henning SC, et al. (2013). Executive functioning skills in long-term users of cochlear implants: A case control study. J Pediatr Psychol, 38, 902–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leark RA, Dupuy TR, Greenberg, et al. (1996). Test of Variables of Attention Professional Manual Version 7.0. Los Alimitos, CA: Universal Attention Disorders, Inc. [Google Scholar]
- Levy JD, Kronenberger WG, Dunn DW (2017). Development of a very brief measure of ADHD: The CHAOS scale. J Atten Disord, 21, 575–586. [DOI] [PubMed] [Google Scholar]
- Marchman VA, & Fernald A (2008). Speed of word recognition and vocabulary knowledge in infancy predict cognitive and language outcomes in later childhood. Dev Sci, 11, F9–F16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marschark M, Kronenberger WG, Rosica M, et al. (2017). Social maturity and executive function among deaf. J Deaf Stud Deaf Educ, 22, 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moeller MP (2007). Current state of knowledge: Psychosocial development in children with hearing impairment. Ear Hear, 28, 729–739. [DOI] [PubMed] [Google Scholar]
- Moog JS, Geers AE, Gustus C, et al. (2011). Psychosocial adjustment in adolescents who have used cochlear implants since preschool. Ear Hear, 32, 75S–83S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholas JG, & Geers AE (2003). Personal, social, and family adjustment in school-aged children with a cochlear implant. Ear Hear, 24(Suppl), 69S–81S. [DOI] [PubMed] [Google Scholar]
- Punch R, & Hyde M (2011). Social participation of children and adolescents with cochlear implants: A qualitative analysis of parent, teacher, and child interviews. J Deaf Stud Deaf Educ, 16, 474–493. [DOI] [PubMed] [Google Scholar]
- Reynolds CR, & Kamphaus RW (2004). Behavior Assessment System for Children, Second Edition (BASC-2). Circle Pines, MN: American Guidance Service. [Google Scholar]
- Reynolds CR, & Kamphaus RW (2015). BASC-3: Behavioral Assessment System for Children. Bloomington, MN: PsychCorp. [Google Scholar]
- Semel EM, Wiig EH, & Secord W (2003). Clinical Evaluation of Language Fundamentals (CELF-4). San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Snyder J, Prichard J, Schrepferman L (2004). Child impulsiveness-inattention, early peer experiences, and the development of early onset conduct problems. J Abnorm Child Psychol, 32, 579–594. [DOI] [PubMed] [Google Scholar]
- Stika CJ, Eisenberg LS, Johnson KC, et al. (2015). Developmental outcomes of early-identified children who are hard of hearing at 12 to 18months of age. Early Hum Dev, 91, 47–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Eldik T, Treffers DA, Veerman JW, et al. (2016). Mental health problems of deaf Dutch children as indicated by parents’ responses to the child behavior checklist. Am Ann Deaf, 148, 390–395. [DOI] [PubMed] [Google Scholar]
- Villabø MA, Gere MK, Torgersen S, et al. (2013). Anxious self-statements in clinic-referred U.S. and Norwegian anxiety-disordered youth. Cognit Ther Res, 37, 840–850. [Google Scholar]
- Warner-Czyz AD, Loy B, Roland PS, et al. (2009). Parent versus child assessment of quality of life in children using cochlear implants. Int J Pediatr Otorhinolaryngol, 73, 1423–1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D (1991). Wechsler Intelligence Scale for Children, Third Edition. San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Wechsler D (1999). Wechsler Abbreviated Scale of Intelligence (WASI). New York, NY: The Psychological Corporation. [Google Scholar]
- Wechsler D, Kaplan E, Fein D, et al. (2004). Wechsler Intelligence Scale for Children – Fourth Edition – Integrated. San Antonio, TX: Harcourt Assessment. [Google Scholar]
- Woodcock RW, McGrew KS, Mather J (2001). Woodcock-Johnson-III. Itasca, IL: Riverside Publishing. [Google Scholar]
- Young NM, & Kirk KI (Eds.). (2016). Pediatric Cochlear Implantation: Learning and the Brain. New York, NY: Springer. [Google Scholar]