Abstract
Background
To develop a modified transforaminal endoscopic spine system (TESSYS®) technique for treating intracanalicular combining foraminal and/or extraforaminal lumbar disc herniation (ICFE-LDH), and evaluate the technical efficacy and safety.
Methods
Twenty-three patients with ICFE-LDH underwent the modified TESSYS technique were enrolled. Magnetic resonance imaging (MRI) was used to verify the reduction of herniated disc. Pre- and post-operative neurological functions were compared by visual analogue scale (VAS) score, Oswestry disability index (ODI) and the modified MacNab criteria. The technical safety was evaluated by surgical complications.
Results
MRI demonstrated reductions of disc herniations in 22 patients (95.7%) after surgeries. The VAS scores were significantly improved at 1 year follow-up (low back: P=0.001, lower limbs: P<0.001), as well as ODI scores (P<0.001). 22 patients had achieved excellent and good recovery postoperatively according to the modified MacNab criteria. One patient (4.3%) underwent a reoperation due to postoperative recurrence of disc herniation. Another patient complained postoperative causalgia in 8 weeks, the symptom alleviated after conservative treatment at 1 year follow-up (VAS: back, 3, lower limbs, 0; ODI: 20%). The incidence rate of surgical complication was 8.7%.
Conclusions
The modified TESSYS technique is a minimally-invasive, effective and safe surgery for treating ICFE-LDHs in selected patients.
Keywords: Modified transforaminal endoscopic spine system (modified TESSYS), lumbar disc herniation, efficacy, safety
Introduction
Lumbar disc herniation (LDH) is a very common spinal disorder with a variety of subtypes, which are classified as central, paracentral, foraminal and extraforaminal herniations according to protrusion’s position on spinal horizontal plane (1). Of these subtypes, Chang defined the central and paracentral herniations as intracanalicular LDH, and extraforaminal herniation was defined as far-lateral LDH (2). While intracanalicular combining foraminal and/or extraforaminal LDH (ICFE-LDH) at one segment is a special and complicated type of LDH (3). Patients with ICFE-LDH often suffer multiple and unbearable radiculopathy since compressions on exiting and traversing nerve roots simultaneously (4), and it is easily to be missed in diagnosis.
Surgery was recommended to treat ICFE-LDH since conservative treatments were unavailable to achieve good curative effect sometimes (5). Of the surgical treatments applying to ICFE-LDH, traditional open discectomy requires a large surgical field due to muscle detachment, exposure of nerve root and excision of facet joint. These processes not only lead to extensive intraoperative traumas but also may result in postoperative atrophies of lumbosacral muscles, lumbar discomfort and instability, even accelerate degeneration in adjacent segments (6).
Then endoscopic spine surgery was developed to minimize above complications. More and more literatures revealed that percutaneous endoscopic discectomy (PED) was effective to treat lumbar pathologies including central, paracentral, lateral, and extruded disc herniations in addition to lateral recess stenosis (7-9). Of the PED techniques, Yeung endoscopy spine system (YESS) and transforaminal endoscopic spine system (TESSYS) techniques are typically associated with less iatrogenic trauma and surgical complications (10). YESS technique is able to treat far-lateral or intracanalicular LDH (11), but it is unsafe to treat ICFE-LDH. For example, Lever technique on behalf of YESS may generate impairments in normal disc (12,13). Although the TESSYS technique is safer to treat LDH, it can’t efficiently treat ICFE-LDH due to defective inside-out approach. With a revised approach, we developed a modified TESSYS technique to treat ICFE-LDH (Figure 1): our working cannula is initially positioned at extracanalicular herniation and removed the outside protrusion, then, we shifted the cannula and headed into intracanalicular herniation for excising the inside protrusion (Figure 2). Through this outside-in technique assisted with endoscopy, we could completely decompress both of the exiting and traversing nerve roots. In this study, we aimed to investigate the efficacy and safety of the modified TESSYS technique in treatment of ICFE-LDH.
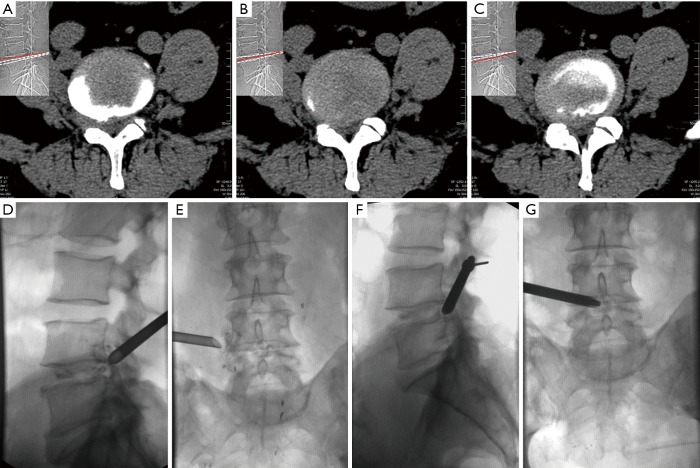
Figure 1.
The modified TESSYS technique in treating ICFE-LDH. (A-C) The ICFE-LDH occurs at L4/5; (D,E) the fluoroscopic trajectory of working cannula for removing foraminal and/or extraforaminal herniated disc; (F,G) the fluoroscopic trajectory of working cannula for removing intracanalicular herniated disc. TESSYS, transforaminal endoscopic spine system; ICFE-LDH, intracanalicular combining foraminal and/or extraforaminal lumbar disc herniation.
Figure 2.
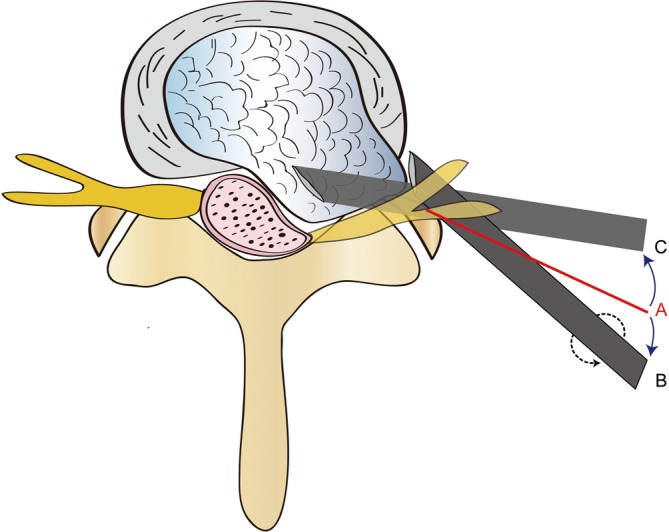
The intracanalicular combining foraminal lumbar herniated discs are removed by the modified TESSYS approach. A: puncture trajectory of the modified TESSYS technique; B: the trajectory of working cannula to remove foraminal herniated disc; C: the trajectory of working cannula to remove intracanalicular herniated disc. TESSYS, transforaminal endoscopic spine system.
Methods
Thirty-one patients were diagnosed as ICFE-LDH by clinical symptoms, neurological examinations, and imaging studies. Of these, 6 rejected surgery and 2 underwent previous lumbar surgeries had not been enrolled in this prospective study (25.8%). To decrease outcome’s bias and clinical heterogeneity, consistent surgical procedures and instrumentations were performed by an experienced surgeon (Y Zhang) in our department from October 2015 to January 2017 (Table 1). This study was designed to conform to the Declaration of Helsinki and approved by the ethics committee of our hospital, all participants had signed informed consents.
Table 1. Demographic characteristics.
| Characteristic | Value |
|---|---|
| Gender | |
| Female | 7 |
| Male | 16 |
| Age (years)† | 58 [45–61] |
| BMI (kg/cm2)§ | 24.1±3.6 |
| Operative segment | |
| L2/3 | 2 |
| L3/4 | 1 |
| L4/5 | 14 |
| L5/S1 | 6 |
†, in deviation distribution, data was presented as median (P25, P75) (P, percentile); §, in normal distribution, data was presented as mean ± standard deviation (SD). BMI, body mass index.
The patient inclusion criteria were: (I) symptoms and signs result from one segmental compressions on exiting and transversing nerve roots. Such as low back pain, lower limbs’ pain, and/or paralysis; (II) positive straight leg raising test or femoral nerve stretch test, with or without relevant muscle’s weakness; (III) magnetic resonance imaging (MRI) and/or computed tomographic (CT) scan indicate ICFE-LDH at the same lumbar segment; (IV) failure of appropriate conservative treatment with no less than 6 weeks. The exclusion criteria were: (I) surgical history at the affected lumbar segment; (II) calcified herniated disc; (III) lumbar instability; (IV) cauda equina syndrome; (V) patients with severe comorbidities such as severe cardiovascular diseases, hemorrhagic disease, tumour or inflammation, etc.
Surgical procedure
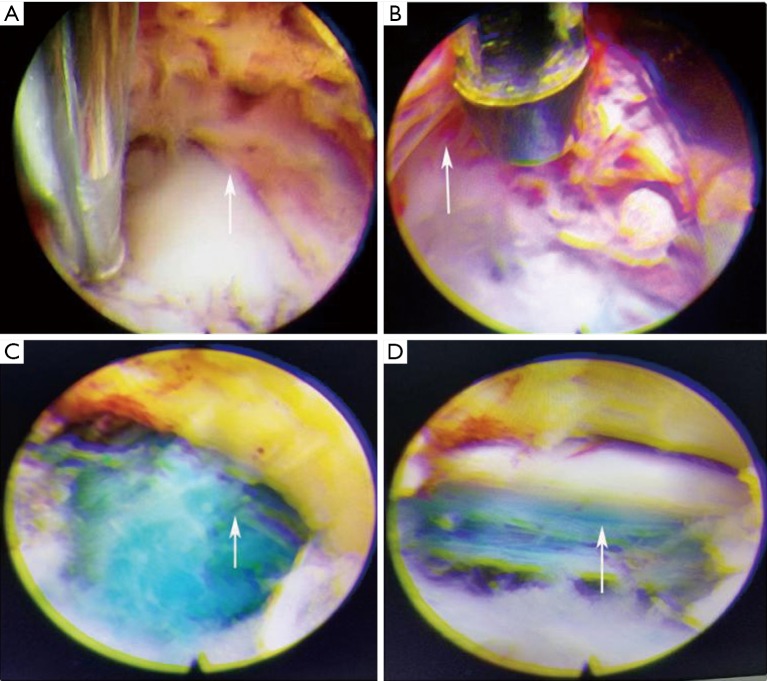
To control clinical confounding factors, all cases were performed by the consistent modified TESSYS technique with MaxMore Spine system (GmbH, Hoogland Spine Products, Germany). Patient was fixed on an operating table in a lateral decubitus position with the affected side upwards. Prior to the surgery, C-arm fluoroscopy was used to verify the herniated segment. Entry point on skin was determined according to traditional TESSYS technique. After sterilization, local infiltration anesthesia with 1% lidocaine was performed to encourage patient communicate with surgeon in real time and avoid neural injury. Whereafter, 0.5 mL mixture containing iohexol and coeruleum methylenum were applied for fluoroscopic localization and blue-staining degenerated nucleus pulposus. Then the anesthetic needle was replaced by a guidewire with its tip touching the superior articular facet, following a skin incision with 8 mm in diameter was made around the guidewire. The surgical pathway was expanded to 6 mm by dilators. Then increased the horizontal angle of the dilator and advanced it till its tip reaching the foraminal or extraforaminal ruptured nuclear tissue. The dilator was replaced by a 7.5 mm working tube afterwards (Figure 1D,E). Under the endoscope, a trigger-flex bipolar radiofrequency (DTF-40, Elliquence, LLC. American) was used to disclose the extracanalicular degenerative disc. Therewith the exiting nerve root was decompressed after the blue-stained disc was removed by a grasping forceps (Figure 3A,B).
Figure 3.
Intraoperative endoscopic imaging. (A) An existing nerve root is compressed by extraforaminal herniated disc. Arrowhead is pointing to the position of nerve root, same hereinafter; (B) revealing the existing nerve root after removal of the extraforaminal herniated disc; (C) a traversing nerve root is compressed and covered by intracanalicular herniated disc (blue-stained); (D) the traversing nerve root is free after removal of the intracanalicular herniated disc.
Next, the working cannula was replaced by a dilator. Based on fluoroscopy, the surgeon shifted and rotated a dilator for sliding the dilator into foramen intervertebrale along with ventral side of superior facet. Meanwhile decreased the dilator’s horizontal angle and headed to intracanalicular herniated disc (Figure 2). Then the dilator was changed by working tube, and surgeon placed the tube’s tip closed to spinous process line at anterior-posterior view on fluoroscopy, and reached posterior line of the intervertebral space at lateral view (Figure 1F,G). Following removed intracanalicular disc herniation and decompressed the traversing nerve root (Figure 3C,D) via intervertebral foramen (foraminoplasty should be conducted in case of foraminal stenosis. Generally, widening the caudal part of intervertebral foramen by reamer was used to avoid nerve’s irritation in the foramen). Finally skin incision was sutured after adequate hemostasis with the radiofrequency bipolar.
Perioperative care and follow-up
Preoperative cefazolin on the day of surgery, as well as painkiller and dehydrant were routinely administrated for patients in postoperative 3 days. Out-of-bed with a lumbar brace on the next day after surgery and maintained one month was suggested. MRI and CT scans were used to monitor postoperative recurrence of LDH. Individual follow-up was regularly performed at postoperative 3 months and 1 year.
Outcome assessment
The technical safety was assessed by operative time, hospital stay, surgical complications and reoperation. The technical efficacy was evaluated by patients’ neurological recovery after surgery such as symptoms and signs as well as imaging examinations. Specifically, pre- and postoperative pains were assessed by visual analogue scale (VAS) score (0–10), improvements in neurological function were measured by Oswestry disability index (ODI, 0–100%) and modified MacNab criteria. There were four grades in modified MacNab criteria: “Excellent” means no pain, no restriction of mobility, patients could return to normal work and activity; “Good” indicates occasional non-radicular pain, relief of presenting symptoms, patients could return to modified work; “Fair” signifies some improved functional capacity, still handicapped and/or unemployed; “Poor” intends continued objective symptoms of root involvement.
Statistical analysis
All statistical analyses were performed by SPSS 19.0 statistical software (SPSS Inc., Chicago, USA). A probability less than 0.05 was considered statistically significant. In normal distribution, the data were presented as mean ± standard deviation (SD). In deviation distribution, pre- and post-operative data were analyzed by Wilcoxon test and the data were presented as median (percentile 25, percentile 75).
Results
Surgical efficacy and safety
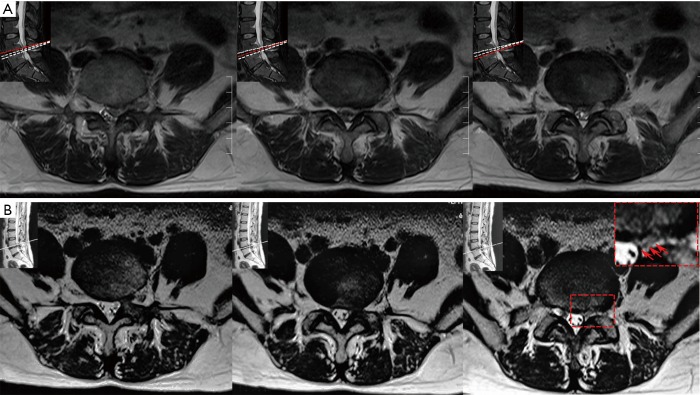
Twenty-three patients (85.2%) with ICFE-LDH performed the modified TESSYS technique and accomplished no less than 1 year follow-up were finally enrolled to this study (Table S1). All cases’ incisions primarily healed. There was no intraspinal canal infection, dural laceration and cerebrospinal fluid leakage occurred. One patient complained causalgia due to intraoperative irritation on L5 exiting nerve root by radiofrequency bipolar. After treatment with gabapentin and mecobalamin, the patient’s symptom was obviously improved in postoperative 10 weeks and recovered at 1 year follow-up (VAS: back, 3, lower limbs, 0; ODI: 20%). Additionally, MRI indicated patients’ LDH were reduced after surgeries in 22 patients (95.7%). One patient (4.3%) recurred pains on lateral crus and foot dorsum at postoperative 15 months, which resulted from recurrence of disc herniation at L4/5 (Figure 4). Remission of the patients’ symptoms were acquired by reoperation (VAS: back, decreased from 2 to 1, lower limbs, from 7 to 2; ODI: from 75% to 9%). The early and late incidence rate of surgical complication was 4.3% respectively. Moreover, a mean of 72±31 min operative time [95% confidence interval (CI): 58–83 min] and a mean of 5.6±3.2 days (95% CI: 4.2–6.8 days) of hospital stay were recorded in present study.
Figure 4.
Recurrence of lumbar disc herniation after surgery. (A) Preoperative intracanalicular combining foraminal disc herniation at L4/5; (B) an existing nerve root is compressed by the postoperative recurrent herniated disc.
Improvements in postsurgical neurological function
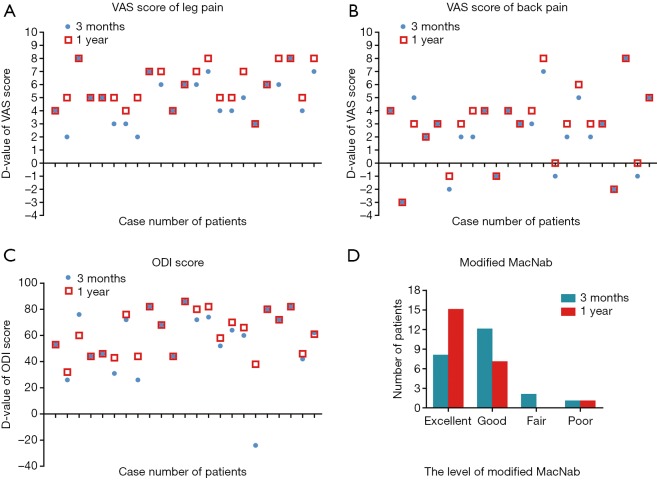
Patients neurological recoveries were summarized in Table 2. The mean VAS score of low back pain and lower limbs pain were 3 [0–5] and 5 [5–7] before operation, decreased to 0 [0–1] and 0 [0–0] (low back: P=0.001, lower limbs: P<0.001) at 1 year follow-up, respectively (Figure 5A,B). The average ODI score was decreased from preoperative 71% (47–82%) to postoperative 0 (0–8%) (P<0.001) at 1 year follow-up (Figure 5C). With the outcomes based on modified MacNab criteria at 1 year follow-up, 8 cases (34.8%) were excellent, 14 cases (60.9%) were good, while 1 case (4.3%) was poor. The success rate was 95.7% (22/23) which including excellent and good curative effects (Figure 5D). In addition, we found VAS score and ODI at postoperative 1 year were a little better than postoperative 3 months but without significant difference between the two durations (all P>0.05, Table 2).
Table 2. Pre- and postoperative VAS score and ODI.
| Variable | Pre-op | Follow-up | P value | |||
|---|---|---|---|---|---|---|
| 3-month | 1-year | 3-month vs. 1 year | Pre-op vs. 1 year | |||
| VAS score† (low back) | 3 (0–5) | 1 (0–1) | 0 (0–1) | 0.239 | 0.001 | |
| VAS score† (lower limbs) | 5 (5-7) | 0 (0–0) | 0 (0–0) | 0.909 | <0.001 | |
| ODI† | 71% (47–82%) | 4% (0–12%) | 0 (0–8%) | 0.615 | <0.001 | |
†, in deviation distribution, data was presented as median (P25, P75) (P, percentile). VAS, visual analogue scale; ODI, Oswestry disability index; Pre-op, pre-operation.
Figure 5.
Neurofunctional outcomes at postoperative 3 months and 1 year follow-up. D-values are defined as measurement value difference, positive value is considered as improvement, negative value is considered as deterioration. At postoperative 3 months and 1 year follow-up: (A) D-value of VAS scores shows the improvements in lower limbs pain; (B) D-value of VAS scores indicates the remissions in most patients with low back pain; (C) D-value of ODI scores reveals the relief in most patients with lumbar dysfunctions; (D) 22 patients achieve neurofunctional improvements according to the modified MacNab criteria. VAS, visual analogue scale; ODI, Oswestry disability index.
Discussion
Techniques’ selection
Surgical treatment for vertebral disease and disc pathology has evolved over time from traditional open surgery to minimally invasive approaches including TESSYS technique. Open surgery for lumbar disorders has a number of challenging factors such as advanced age, osteoporosis and loss of lordosis, which may lead to poor clinical outcomes. In addition to open surgery may result in some severe complications such as low back pain, nonunion and instability, etc. Take the case of most frequent complication of traditional open surgery, transient lower extremity dysesthesia or hypesthesia induced by irritation on nerve root, which is relatively rare in TESSYS though (14). Moreover, TESSYS approach not only reduced the injury to lumbar tissues but also preserve the biomechanical structure of affected segment (15). Even compared with conservative surgeries, TESSYS has fewer postoperative complications as well (16). In summary, aside from TESSYS technique seems as effective as open discectomy in selected patients (17), TESSYS has the benefits of an minimally invasive spine surgery including less trauma, small incision, faster recovery and lower blood loss while still achieving equally clinical outcomes compared to traditional open surgeries (18,19). So, minimally invasive spinal surgery is more and more popular in treating LDH recently. But since Lee et al. reported a limited view and deficient access to extruded disc fragments which could lead to a failure in treating LDH by PED (20). Many researchers found that it was important to select an available approach for intracanal and extracanal herniated fragments when treating ICFE-LDH by spinal endoscopy (21,22). Currently, although some endoscopic operations are useful for either intracanalicular or far-lateral LDH, few literature has reported that ICFE-LDH could be treated by PED except “lever technique”. On basis of YESS technique, Gore et al. developed the “Lever technique” which added decompression for intracanalicular herniated disc by undercutting the facet to visualize epidural and subarticular areas (12). Although this technique also could treat ICFE-LDH through the decompression inside disc, it generates unnecessary iatrogenic trauma since intradiscal operation is unavoidable to injure normal disc (13). In addition, inserting the working channel into intervertebral disc before removal of extracanal herniated disc may result in a risk of the injury on exiting nerve root due to disc migration (23). Hence, we designed the outside-in approach to treat ICFE-LDH, and it was also inversed to hand-down technique with the inside-out approach (24). By this way, we developed a less invasive and practical endoscopic technique by shifting the working tube out of disc, and demonstrated the technical efficiency and safety according to the recovery of neurological function and surgical complications.
In this study, we found that patients’ ODI and VAS scores had significantly improved after treatment by the modified TESSYS technique, which may indicate the technique was effective to ICFE-LDH. Pan et al. compared surgical outcomes between TESSYS technique and traditional fenestration discectomy in treating LDH (25), and found a lower complication rate of 6.3% in TESSYS group (all P<0.001), as well as lower VAS score and lower ODI (VAS score: osphyalgia, 1.6±0.4, skelalgia, 0.9±0.3; ODI: 8.6%±2.9%, at 1 year follow-up) in TESSYS group. Additionally, a relative low incidence of 8.7% in complications revealed the technical safety.
The feasibility, advantages and disadvantages of the modified TESSYS technique
Even though TESSYS is a minimal invasive technique, some complications are unavoidable in the surgeries. Literatures reported that an incidence of 1% in sensory deficits, 10% in dysesthesias, and 0.3% in dural tears respectively occurred in TESSYS surgeries (18,26). Any operation contacts nerve root might injure nerve tissues intraoperatively, but with local anesthesia, patient could immediately complain any pain or numbness in case of neurostimulus. This intraoperative feedback from patient could minimize nerve injury. In addition, we used fluoroscopy to precisely manipulate surgical instruments at pathological level, and which assisted to place the instruments in a safe approach (Kambin safety triangle) and avoid approach-related complications.
Although TESSYS could be used in non-inclusive herniation, traditional TESSYS technique can’t effectively remove ICFE-LDH due to its limited approach. With the modified TESSYS technique, we could shift the head of working tube from extracanal area to intracanalicular area and extract protrusion. In present case series, the surgical success rate of treating ICFE-LDH was 95.7% (22/23) according to the modified MacNab criteria. Correspondingly, a success rate of 95.84% was revealed by traditional TESSYS technique in treating LDH with simplex protrusion (25). There was one patient (4.3%) occurred recurrent disc herniation in this study, it was within microdiscectomy reherniation rates range from 2.3% to 11.8% (26). The recurrent disc herniation rate experienced in this study was similar to Kosztowski et al.’s reherniation rates of 4.76% after transforaminal lumbar endoscopic discectomy (18).
Suggestions to application of the modified TESSYS technique
In this cohort, to appropriately manipulate instruments with the modified approach, we performed foraminoplasty for 8 cases with facet joints suffering osteophyte and hypertrophy. In the process of foraminoplasty, there was a risk of nerve root injury caused by using driller, trephine or laser. We found it was more easy to avoid facet’s obstruction and expose intracanalicular herniated disc by pushing down horizontal puncture angle. But we did not recommend insert working tube into intracanalicular structures through intervertebral foramen in horizontal approach since the risk of injury to abdominal organs. So we suggested that puncture angle should be kept about 30°, and we used the “underdraught” technique to shift working tube ventrally and decrease the horizontal angulation since it was an easy way to access spinal canal.
In present study, one patient complained postoperative dermatomal causalgia due to the injury of L5 exiting nerve root. It is a common and transient complication when employing endoscopy to treat extracanal disc herniations, the symptom often results from the irritation on dorsal root ganglion by working tube or frequency bipolar (27). Patients’ symptom ultimately disappeared after taking analgesic and neurotrophic drugs. This complication reminded us to pay close attention to patients’ response during surgery and minimize intraoperative neural injury. Additionally, although TESSYS technique is a practical and minimally invasive method to treat a part of LDH, we should strictly make operation plan for each patient since TESSYS is unsuitable for some LDH cases such as lumbar instability, severe spinal canal stenosis or intervertebral space stenosis.
Limitations
There were some limitations in this study. Firstly, with the small sample size and single center data, the clinical data was not so powerful to support our investigative results. And an inclusion rate of 74.2% in participants may lead to result’s bias. In addition, the data in this case series were just compared pre- and post-operatively but lacking appropriate control group for comparison since the rare cases of ICFE-LDH. Secondly, patients’ disease courses and involved segments were not controlled, which might lead to data bias. Thirdly, the follow-up period was not so long but intervertebral disc collapse may occur as time goes on. In addition, only the protruded disc was removed by this technique but degenerative intervertebral disc was remained after surgery. So maybe, higher recurrence rate of LDH would be observed in longer follow-up. Hence, a large-sample, randomized controlled trial with long follow-up period is required in future study.
Conclusions
The modified TESSYS technique is a minimally-invasive, effective and safe surgery for treating ICFE-LDHs in selected patients. Also it may provide a potential method to treat patients with similar herniations in cervical or thoracic disc.
Table S1. Patients’ characteristics and clinical outcomes.
| Case No. | Age (year) | Sex | Surgical segment | VAS score (low back) | VAS score (lower limbs) | ODI score (%) | Modified MacNab criteria (1 year) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-op | Post-op (3 months) | Post-op (1 year) | Pre-op | Post-op (3 months) | Post-op (1 year) | Pre-op | Post-op (3 months) | Post-op (1 year) | |||||||
| 1 | 52 | F | L4/5 | 4 | 0 | 0 | 4 | 0 | 0 | 53 | 0 | 0 | Excellent | ||
| 2 | 55 | M | L4/5 | 0 | 3 | 3 | 5 | 1 | 0 | 52 | 26 | 20 | Good | ||
| 3 | 67 | F | L4/5 | 5 | 0 | 2 | 8 | 0 | 0 | 76 | 0 | 16 | Excellent | ||
| 4 | 61 | M | L4/5 | 2 | 0 | 0 | 5 | 0 | 0 | 44 | 0 | 0 | Excellent | ||
| 5 | 59 | M | L4/5 | 3 | 0 | 0 | 5 | 0 | 0 | 46 | 0 | 0 | Excellent | ||
| 6 | 55 | F | L4/5 | 0 | 2 | 1 | 5 | 0 | 0 | 47 | 16 | 4 | Good | ||
| 7 | 34 | M | L4/5 | 3 | 1 | 0 | 4 | 0 | 0 | 76 | 4 | 0 | Excellent | ||
| 8 | 42 | M | L5/S1 | 5 | 3 | 1 | 5 | 0 | 0 | 50 | 24 | 6 | Good | ||
| 9 | 67 | F | L4/5 | 4 | 0 | 0 | 7 | 0 | 0 | 82 | 0 | 0 | Excellent | ||
| 10 | 31 | M | L5/S1 | 0 | 1 | 1 | 7 | 0 | 0 | 72 | 4 | 4 | Good | ||
| 11 | 68 | M | L3/4 | 4 | 0 | 0 | 4 | 0 | 0 | 44 | 0 | 0 | Excellent | ||
| 12 | 51 | M | L5/S1 | 3 | 0 | 0 | 6 | 0 | 0 | 86 | 0 | 0 | Excellent | ||
| 13 | 59 | M | L2/3 | 4 | 1 | 0 | 7 | 0 | 0 | 80 | 8 | 0 | Excellent | ||
| 14 | 39 | M | L5/S1 | 8 | 1 | 0 | 8 | 0 | 0 | 82 | 8 | 0 | Excellent | ||
| 15 | 60 | F | L4/5 | 0 | 1 | 0 | 5 | 0 | 0 | 58 | 6 | 0 | Excellent | ||
| 16 | 45 | M | L2/3 | 3 | 1 | 0 | 5 | 0 | 0 | 70 | 6 | 0 | Excellent | ||
| 17 | 61 | M | L4/5 | 7 | 2 | 1 | 7 | 0 | 0 | 74 | 14 | 8 | Good | ||
| 18 | 68 | M | L4/5 | 3 | 1 | 2 | 4 | 6 | 7 | 38 | 62 | 75 | Poor | ||
| 19 | 61 | M | L4/5 | 3 | 0 | 0 | 6 | 1 | 0 | 84 | 4 | 4 | Excellent | ||
| 20 | 58 | M | L5/S1 | 0 | 2 | 2 | 8 | 0 | 0 | 84 | 12 | 12 | Good | ||
| 21 | 27 | M | L5/S1 | 8 | 0 | 0 | 8 | 0 | 0 | 82 | 0 | 0 | Excellent | ||
| 22 | 45 | F | L4/5 | 0 | 1 | 0 | 5 | 0 | 0 | 46 | 4 | 0 | Excellent | ||
| 23 | 66 | F | L4/5 | 6 | 1 | 1 | 8 | 0 | 0 | 71 | 9 | 10 | Good | ||
VAS, visual analogue scale; ODI, Oswestry disability index; Pre-op, pre-operation; Post-op, post-operation; F, female; M, male.
Acknowledgements
We thank the reviewers and editors for their helpful comments on this article, and thank Sun Kyu Choi (who is a biostatistician works at Yonsei University College of Medicine) for his statistical suggestions.
Funding: The present study was financially supported by the grants of China Scholarship Council (2017-3109/201708260068), and 5511 Innovation-driven Program of Jiangxi Province Department of Science and Technology (20165BCB18017).
Ethical Statement: The study was registered and carried out with the approvals of Ethical Institutional Review Boards of the First Affiliated Hospital of Nanchang University. Written informed consents were obtained from eligible patients and the study was designed to conform to the Declaration of Helsinki.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Jackson RP, Glah JJ. Foraminal and extraforaminal lumbar disc herniation: diagnosis and treatment. Spine (Phila Pa 1976) 1987;12:577-85. 10.1097/00007632-198707000-00014 [DOI] [PubMed] [Google Scholar]
- 2.Chang CW, Lai PH, Yip CM, Hsu SS. Spontaneous regression of lumbar herniated disc. J Chin Med Assoc 2009;72:650-3. 10.1016/S1726-4901(09)70449-6 [DOI] [PubMed] [Google Scholar]
- 3.Covaro A, Vila-Canet G, de Frutos AG, Ubierna MT, Ciccolo F, Caceres E. Management of degenerative lumbar spinal stenosis: an evidence-based review. EFORT Open Rev 2017;1:267-74. 10.1302/2058-5241.1.000030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Joswig H, Richter H, Haile SR, Hildebrandt G, Fournier JY. Introducing interlaminar full-endoscopic lumbar diskectomy: a critical analysis of complications, recurrence rates, and outcome in view of two spinal surgeons' learning curves. J Neurol Surg A Cent Eur Neurosurg 2016;77:406-15. 10.1055/s-0035-1570343 [DOI] [PubMed] [Google Scholar]
- 5.Genevay S, Courvoisier DS, Konstantinou K, Kovacs FM, Marty M, Rainville J, Norberg M, Kaux JF, Cha TD, Katz JN, Atlas SJ. Clinical classification criteria for radicular pain caused by lumbar disc herniation: the radicular pain caused by disc herniation (RAPIDH) criteria. Spine J 2017;17:1464-71. 10.1016/j.spinee.2017.05.005 [DOI] [PubMed] [Google Scholar]
- 6.En'Wezoh DC, Leonard DA, Schoenfeld AJ, Harris MB, Zampini JM, Bono CM. Relationship between size of disc and early postoperative outcomes after lumbar discectomy. Arch Orthop Trauma Surg 2017;137:805-11. 10.1007/s00402-017-2699-6 [DOI] [PubMed] [Google Scholar]
- 7.Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective, randomized, controlled study. Spine (Phila Pa 1976) 2008;33:931-9. 10.1097/BRS.0b013e31816c8af7 [DOI] [PubMed] [Google Scholar]
- 8.Choi G, Lee SH, Lokhande P, Kong BJ, Shim CS, Jung B, Kim JS. Percutaneous endoscopic approach for highly migrated intracanal disc herniations by foraminoplastic technique using rigid working channel endoscope. Spine (Phila Pa 1976) 2008;33:E508-15. 10.1097/BRS.0b013e31817bfa1a [DOI] [PubMed] [Google Scholar]
- 9.Ruetten S, Komp M, Merk H, Godolias G. Surgical treatment for lumbar lateral recess stenosis with the full-endoscopic interlaminar approach versus conventional microsurgical technique: a prospective, randomized, controlled study. J Neurosurg Spine 2009;10:476-85. 10.3171/2008.7.17634 [DOI] [PubMed] [Google Scholar]
- 10.Yokosuka J, Oshima Y, Kaneko T, Takano Y, Inanami H, Koga H. Advantages and disadvantages of posterolateral approach for percutaneous endoscopic lumbar discectomy. J Spine Surg 2016;2:158-66. 10.21037/jss.2016.09.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yeung AT, Yeung CA. Advances in endoscopic disc and spine surgery: foraminal approach. Surg Technol Int 2003;11:255-63. [PubMed] [Google Scholar]
- 12.Gore S, Yeung A. The "inside out" transforaminal technique to treat lumbar spinal pain in an awake and aware patient under local anesthesia: results and a review of the literature. Int J Spine Surg 2014;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sasani M, Ozer AF, Oktenoglu T, Canbulat N, Sarioglu AC. Percutaneous endoscopic discectomy for far-lateral lumbar disc herniations: prospective study and outcome of 66 patients. Minim Invasive Neurosurg 2007;50:91-7. 10.1055/s-2007-984383 [DOI] [PubMed] [Google Scholar]
- 14.Xin G, Shi-Sheng H, Hai-Long Z. Morphometric analysis of the YESS and TESSYS techniques of percutaneous transforaminal endoscopic lumbar discectomy. Clin Anat 2013;26:728-34. 10.1002/ca.22286 [DOI] [PubMed] [Google Scholar]
- 15.Xiong C, Li T, Kang H, Hu H, Han J, Xu F. Early outcomes of 270-degree spinal canal decompression by using TESSYS-ISEE technique inpatients with lumbar spinal stenosis combined with disk herniation. Eur Spine J 2018. [Epub ahead of print]. 10.1007/s00586-018-5655-4 [DOI] [PubMed] [Google Scholar]
- 16.Nellensteijn J, Ostelo R, Bartels R, Peul W, van Royen B, van Tulder M. Transforaminal endoscopic surgery for symptomatic lumbar disc herniations: a systematic review of the literature. Eur Spine J 2010;19:181-204. 10.1007/s00586-009-1155-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gadjradj PS, van Tulder MW, Dirven CM, Peul WC, Harhangi BS. Clinical outcomes after percutaneous transforaminal endoscopic discectomy for lumbar disc herniation: a prospective case series. Neurosurg Focus 2016;40:E3. 10.3171/2015.10.FOCUS15484 [DOI] [PubMed] [Google Scholar]
- 18.Kosztowski TA, Choi D, Fridley J, Galgano M, Gokaslan Z, Oyelese A, Telfeian AE. Lumbar disc reherniation after transforaminal lumbar endoscopic discectomy. Ann Transl Med 2018;6:106. 10.21037/atm.2018.02.26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jasper GP, Francisco GM, Telfeian AE. Clinical success of transforaminal endoscopic discectomy with foraminotomy: a retrospective evaluation. Clin Neurol Neurosurg 2013;115:1961-5. 10.1016/j.clineuro.2013.05.033 [DOI] [PubMed] [Google Scholar]
- 20.Lee JS, Woo JY, Jang JS, Jang IT. Combined interlaminar and paraisthmic approach for co-existing intracanal and foraminal lesion. Korean J Spine 2015;12:256-60. 10.14245/kjs.2015.12.4.256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kong W, Liao W, Ao J, Cao G, Qin J, Cai Y. The strategy and early clinical outcome of percutaneous full-endoscopic interlaminar or extraforaminal approach for treatment of lumbar disc herniation. Biomed Res Int 2016;2016:4702946. 10.1155/2016/4702946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sairyo K, Higashino K, Yamashita K, Tezuka F, Morimoto M, Terai T, Chikawa T, Yonezu H, Nagamachi A, Fukui Y. A new concept of transforaminal ventral facetectomy including simultaneous decompression of foraminal and lateral recess stenosis: Technical considerations in a fresh cadaver model and a literature review. J Med Invest 2017;64:1-6. 10.2152/jmi.64.1 [DOI] [PubMed] [Google Scholar]
- 23.Strömqvist F, Stromqvist B, Jonsson B, Karlsson MK. Surgical treatment of lumbar disc herniation in different ages-evaluation of 11,237 patients. Spine J 2017;17:1577-85. 10.1016/j.spinee.2017.03.013 [DOI] [PubMed] [Google Scholar]
- 24.Sairyo K, Egawa H, Matsuura T, Takahashi M, Higashino K, Sakai T, Suzue N, Hamada D, Goto T, Takata Y, Nishisho T, Goda Y, Sato R, Tsutsui T, Tonogai I, Kondo K, Tezuka F, Mineta K, Sugiura K, Takeuchi M, Dezawa A. State of the art: Transforaminal approach for percutaneous endoscopic lumbar discectomy under local anesthesia. J Med Invest 2014;61:217-25. 10.2152/jmi.61.217 [DOI] [PubMed] [Google Scholar]
- 25.Pan Z, Ha Y, Yi S, Cao K. Efficacy of transforaminal endoscopic spine system (TESSYS) technique in treating lumbar disc herniation. Med Sci Monit 2016;22:530-9. 10.12659/MSM.894870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fakouri B, Shetty NR, White TC. Is sequestrectomy a viable alternative to microdiscectomy? A systematic review of the literature. Clin Orthop Relat Res 2015;473:1957-62. 10.1007/s11999-014-3904-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tu Z, Li YW, Wang B, Lu G, Li L, Kuang L, Dai Y. Clinical outcome of full-endoscopic interlaminar discectomy for single-level lumbar disc herniation: a minimum of 5-year follow-up. Pain Physician 2017;20:E425-30. [PubMed] [Google Scholar]