Abstract
Occurrence of bone metastases is a common event in oncology. Bone metastases are associated with pain, functional impairment, and fractures, particularly when weight-bearing bones are involved. Management of bone metastases has been improved by the development of various interventional radiology consolidation techniques. Cementoplasty is based on injection of acrylic cement into a weakened bone to reinforce it and to control pain. This minimally invasive technique has proven its efficacy for flat bone submitted to compression forces. However, resistance to torsion forces is limited and, thus, treatment of long bones should be considered with caution. In recent years, variant techniques of percutaneous bone consolidation have emerged, including expansion devices for vertebral augmentation and percutaneous screw fixation for pelvic bone and proximal femur tumors. Research projects are ongoing to develop drug-loaded cements to use them as therapeutic vectors. However, release of drugs is still poorly controlled and conventional polymethylmethacrylate cement remains the gold standard in oncology. Image-guided consolidation techniques enhance the array of treatments in bone oncology. Multidisciplinary approach is mandatory to select the best indications.
Keywords: cementoplasty, vertebroplasty, bone metastasis, screw fixation, interventional radiology
Objectives : Upon completion of this article, the reader will be able to identify patient selection, technical considerations, and periprocedural management of the patient undergoing interventional radiologic procedures for oncologic musculoskeletal lesions.
Bone metastases are a common event in cancer patients. 1 Their incidence keeps growing as overall survival of cancer patients is improving. Bone metastases are associated with pain and pathological fractures. Bone loss is commonly due to tumoral osteolysis; however, benign fractures related to osteoporosis can also occur in cancer patients, particularly when prolonged steroid or hormone therapies are required. The impact of skeletal-related events in cancer patients is major, causing functional impairment and increasing morbidity and mortality. Moreover, bone complications often imply interruption or postponement of systemic therapies. 2
Although surgical approach offers an excellent mechanical fixation, the choice of the technique has to be adapted to the general status of the patient and the speed of growth of the cancer disease. Thus, image-guided minimally invasive techniques have been developed. Cementoplasty is the cornerstone of percutaneous bone consolidation. Initially limited to vertebrae, it can also be used in extraspinal tumors in well-selected cases. Other techniques using vertebral augmentation devices or percutaneous screw fixation have also been reported. For more complex cases, percutaneous bone consolidation can be combined with other interventional radiology methods such as embolization or thermal ablation. The choice of the technique depends on the therapeutic intent (palliative or curative), on the risk of fracture or neurological compression. 3 Multidisciplinary strategy remains mandatory.
Cementoplasty
Principle and Indications
Cementoplasty includes injecting cement through a trocar, into a weakened bone, to achieve consolidation and pain management. This technique was first described by Galibert and Deramond to treat a cervical aggressive hemangioma. 4 The field of vertebroplasty has extended to vertebral compression fractures in various indications: osteoporosis, metastases and myeloma, and traumatology. 5 In oncology, such a procedure has proved to be efficient for myeloma and painful osteolytic metastases ( Fig. 1 ). Benign fractures can also occur in cancer patients, due to longer life expectancy, but also due to faster bone resorption secondary to steroids and hormone therapy. For cases where imaging is equivocal to differentiate benign or malignant fracture, coaxial bone biopsy can be performed during the cementoplasty procedure.
Fig. 1.
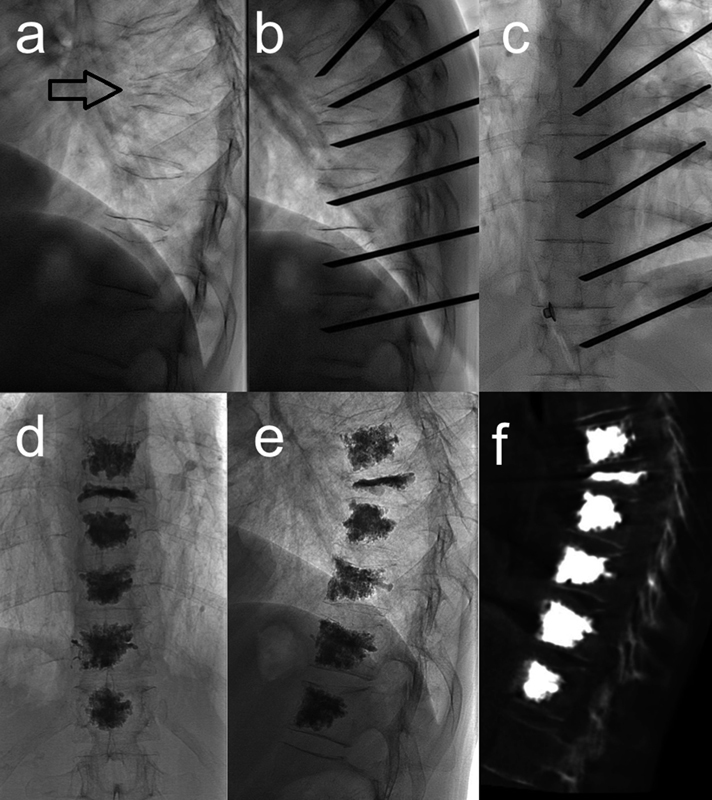
Thoracic multilevel vertebroplasty in a 58-year-old patient treated for myeloma. ( a ) Lateral fluoroscopic view demonstrates a major T8 pathological collapse (arrow) and several adjacent minor fractures. ( b and c ) Six levels are cemented under cone beam-CT guidance, using unilateral intercostopedicular approach. ( d–f ) Control after procedure confirms proper cement distribution without leakage.
As bone metastases are mostly multifocal, radical surgery is seldom indicated. 6 Radiation therapy is often needed, but it does not guarantee a fast and durable consolidation. On the contrary, cementoplasty is effective to rapidly improve pain and to restore mechanical strength. Polymerization of polymethylmethacrylate (PMMA) cement produces exothermic reaction with transient peak of temperature reaching 80°C; despite this raise of temperature, thermal necrosis at the bone–cement interface is not a common histological finding. 7 Thus, cementoplasty as a standalone technique remains palliative. When treatment strategy implies complete tumor control, combination with other therapies (surgery, radiotherapy, thermal ablation, and systemic therapy) should be considered. 8 9
Although less frequent, symptomatic osteoblastic metastases can sometimes be treated with cementoplasty if bone is not too dense and if fissures are present. In case of massive osteoblastic reaction, proper bone filling with cement is no longer feasible and may be associated with periosseous leakage. When bone metastases are associated with symptomatic soft-tissue invasion, cementoplasty can be combined with thermal ablation (radiofrequency, cryoablation). 3 10 11 Notably, metallic surgical device close to the target tumor is a contraindication for radiofrequency ablation, as electrical conductivity of the metal may lead to severe burning.
For vertebroplasty, rupture of the posterior wall is not a contraindication, although particular caution should be taken to avoid perineural cement leakage. 12 13 On the contrary, neurological compression and sagittal spinal instability are strict contraindications for vertebroplasty as a standalone technique; for those cases, urgent surgical decompression and fixation is required. Other contraindications for percutaneous cementoplasty include acute infections and irreversible coagulopathy.
Vertebroplasty
Lumbar levels are treated by transpedicular oblique approach. Mid- and low thoracic levels can be treated via bilateral transpedicular route or ideally via unilateral intercostopedicular approach ( Fig. 1 ). For upper thoracic levels, the bone trocar can be inserted with an oblique route through the transverse process, keeping a craniocaudal axis parallel to the head of the rib, to stay away from the spinal canal and the foraminal nerves. For mid- and low cervical levels, the trocar is inserted via anterolateral approach, just medial to the carotid jugular complex, which is moved laterally by the opposite hand. For upper cervical levels (C1 and C2), the transoral route is preferred, using an oral retractor ( Fig. 2 ).
Fig. 2.
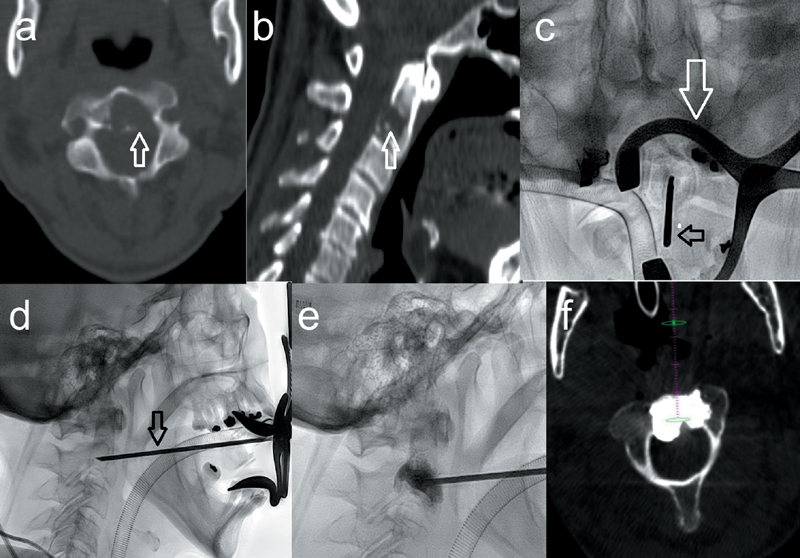
C2 transoral vertebroplasty of osteolytic painful metastasis of leiomyosarcoma. Axial ( a ) and sagittal ( b ) CT demonstrating a major osteolysis of the base of C2 (arrows). ( c and d ) Using an oral retractor (white arrow), a 13-gauge bone trocar (black arrow) is inserted via transoral route. ( e and f ) Lateral fluoroscopy ( e ) and axial cone beam CT reconstruction ( f ) show proper cement distribution.
For the sacrum, sacral wings are treated via direct posterior approach. Less often, if the body of S1 has to be consolidated, posterolateral route through the sacroiliac joint can be used, ensuring to keep away from the first sacral nerves.
Vertebroplasty can be performed under general anesthesia or under conscious sedation, 14 15 depending on the general status of the patient, his or her positioning during intervention, and the estimated procedural time. Strict sterility is mandatory. Under fluoroscopic guidance or under CT guidance for some complex cases, a 10- to 13-gauge bone trocar is inserted into the weakened bone. If needed, coaxial biopsy can be performed just before cement injection. Cement is then mixed and when it reaches a slightly pasty consistency, injection is slowly performed under continuous fluoroscopic control. Cements certified for percutaneous use are loaded with a radio-opacifier to control distribution and to avoid extraosseous leakages, particularly intravascular leakages. Although polymerization of acrylic cements produces exothermic reaction that may play an additional role for pain management, the major therapeutic effect of cementoplasty is related to mechanical stabilization of the pathological bone.
After intervention, a brief surveillance is needed before mobilizing the patient. Most cementoplasties are performed in short hospital stay or even outpatient. Pain control and functional improvement are often rapidly achieved. If applicable, systemic therapy or radiation therapy can be resumed in the next few days.
Vertebroplasty is efficient to treat symptomatic spine metastases or myeloma. Many studies report early and durable pain management on 75 to 85% of cases. 6 13 16 17 In a meta-analysis pooling 23 studies with 923 myeloma patients, Khan et al reported a decrease of visual analogic pain score of 4.8 points after 1 week, and 4.6 points after 1 year. 18 Rupture of the posterior vertebral wall is not a strict contraindication for vertebroplasty ( Fig. 3 ); however, in case of neurological compression, radiotherapy or surgical decompression has to be considered.
Fig. 3.
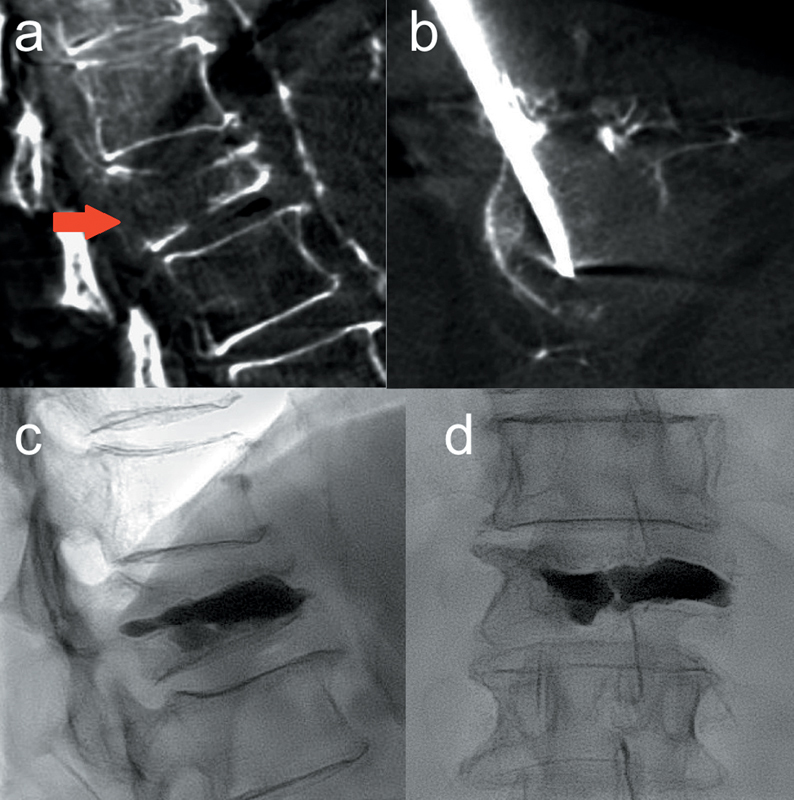
Lumbar vertebroplasty with posterior wall rupture in a metastatic lung cancer patient. ( a ) Cone beam CT aquisition with sagittal reconstruction shows a L1 pathological fracture with posterior wall osteolysis (arrow). No neurological symptoms. ( b ) An 11-gauge bone trocar is inserted via transpedicular oblique approach. ( c and d ) Image after cement injection shows no extraosseous leakage. Additional radiotherapy was performed.
Symptomatic complications due to vertebroplasty remain rare. They are mainly due to foraminal cement leakage that may cause transient radiculopathy. Anterior venous leakages can lead to lung embolism; if minor, it is generally asymptomatic and does not require any specific anticoagulation. Multilevel vertebroplasty in oncology does not seem to increase the rate of complications. 19
Extra-Spinal Cementoplasty
Polymethylmethacrylate cement has a good resistance to compression forces, but limited resistance to torsion forces. For this reason, flat bones such as acetabular roof, 20 femoral condyles, tibial endplates, or talus can be treated effectively with percutaneous cementoplasty ( Fig. 4 ). However, when subchondral bone is destroyed or fractured, the risk of cement leakage into the joint is high; although mainly asymptomatic, rapid chondrolysis secondary to intra-articular cement leakage has been reported. 21
Fig. 4.
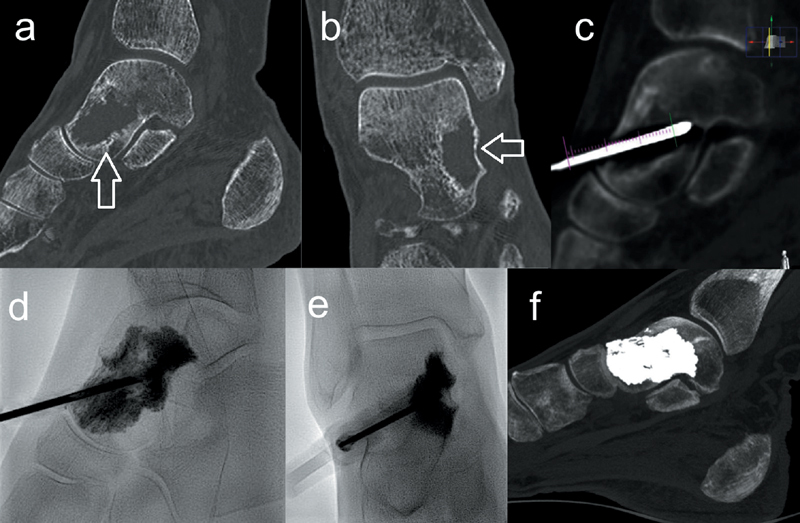
Painful talar metastasis of rhabdomyosarcoma. ( a and b ) Sagittal and coronal CT show a talar osteolysis (arrow) with risk of fracture. ( c–e ) Cone beam CT-guided cementoplasty is performed to consolidate the weakened bone. ( f ) CT with sagittal reconstruction shows filling of the bone defect. Excellent pain control.
Cementoplasty of long bone diaphysis should be considered only in selected nonsurgical patients. Indeed, the quality of bone consolidation is limited due to the fact that optimal cement distribution within the lesion is often difficult to be achieved. Moreover, the mechanical properties of PMMA with poor resistance to torsion lead to increased risk of secondary fracture. For this reason, surgical intramedullary nail remains the gold standard technique for long bone stabilization. In a series of 50 extra-spinal cementoplasties, Anselmetti et al reported two cases of femoral diaphysis cementoplasty where fracture occurred 1 month after treatment. 22 In a more recent series focused only on long bone limb cementoplasty in 51 nonsurgical patients, Cazzato et al reported pain improvement after 1 month in 89.4% cases, and limb functional improvement in 71.8% cases. 23 Secondary fracture of the cemented bone occurred in 9.1% cases. However, external surgical plaque screwed into the previously injected cement was still feasible.
Cements in Oncology
PMMA cement remains the gold standard in oncology, and offers many advantages: good mechanical resistance to compression forces, stability over time, easy to inject, low cost.
Composite cements or biocompatible calcium-phosphate cements show no benefit in oncology due to lower stability over time with less mechanical resistance.
Several studies report research projects using loaded cements as therapeutic vectors. Methotrexate and cisplatin are the most studied chemotherapies. However, many problems remain unsolved: the release of the drugs is poorly controlled and may lead to toxic rates; some drugs may be altered by the exothermic reaction during polymerization of PMMA. One study mentioned the use of zoledronate-loaded cement after surgical curettage of giant cell tumors of the sacrum in four patients; the authors found bone reconstruction without tumor recurrence. 24 There is actually no evidence to prove if this approach is beneficial, compared with conventional intravenous use of zoledronate.
Other studies tried to load PMMA with radionuclide to reinforce focal antitumoral effect. 25 Potential problems are numerous: risk of excessive dose to cortical bone causing secondary osteonecrosis; poor control of the release of radionuclide; and risk of inadvertent irradiation of vulnerable tissues in case of cement leakage.
Other Pecutaneous Consolidation Techniques
Vertebral Expansion
Since the early 2000s, intravertebral expansion devices have been developed. Kyphoplasty using balloons was the first one. The principle is to inflate one or two balloons into the fractured vertebra to create a cavity, which is thereafter filled with cement. 26 27 However, height restoration and reduction of kyphosis are often limited. Creation of an intra-vertebral cavity allows injection of cement with lower pressure; thus, the risk of cement leakage may be reduced. Other devices have been developed, based on permanent expandable implants: stents, jacks, and preformed polymers. 28 Compared with conventional vertebroplasty, expandable devices have not proven to be more effective for pain management. Their use in the field of oncology remains limited, as procedural time and cost are increased. Moreover, in a palliative situation, multiple vertebral levels often have to be treated in a single session ( Fig. 1 ). Balloon kyphoplasty is increasing intravertebral pressure and is associated with a much greater release of tumoral cells into the blood circulation, compared with conventional vertebroplasy. 29 Further studies are required to evaluate the clinical impact.
Percutaneous Screw Fixation
Peripheral bone fixation is an efficient and generally low invasive technique. On the contrary, pelvic bone surgery in the field of oncology is a complex and aggressive surgery, often associated with major blood loss. When bone destruction is advanced, extensive surgery of the pelvic bone implies complex reconstruction to achieve proper functional result. Thus, for polymetastatic patients, surgical approach is often rejected, considering the general status of the patient and his or her life expectancy. Moreover, prior radiotherapy or antiangiogenic treatments impair wound healing.
Thanks to the improvements of image guidance, screw fixation with minimally invasive interventional radiology approach has recently emerged. 30 31 Navigation softwares integrated with computed tomography (CT) or cone beam CT allow precise screw insertion, even if bone landmarks are altered by tumor destruction. If needed, screw fixation can easily be combined with cementoplasty to achieve optimal anchorage and to avoid secondary screw displacement. Cementoplasty of the iliac wing is a simple and effective technique for most pathological symptomatic fractures. However, in case of fractures involving the sacral holes, it is difficult to achieve proper consolidation without risk of perineural cement leakage. In such scenarios, trans-sacro-iliac screw fixation can achieve safer pelvic bone stabilization ( Fig. 5 ).
Fig. 5.
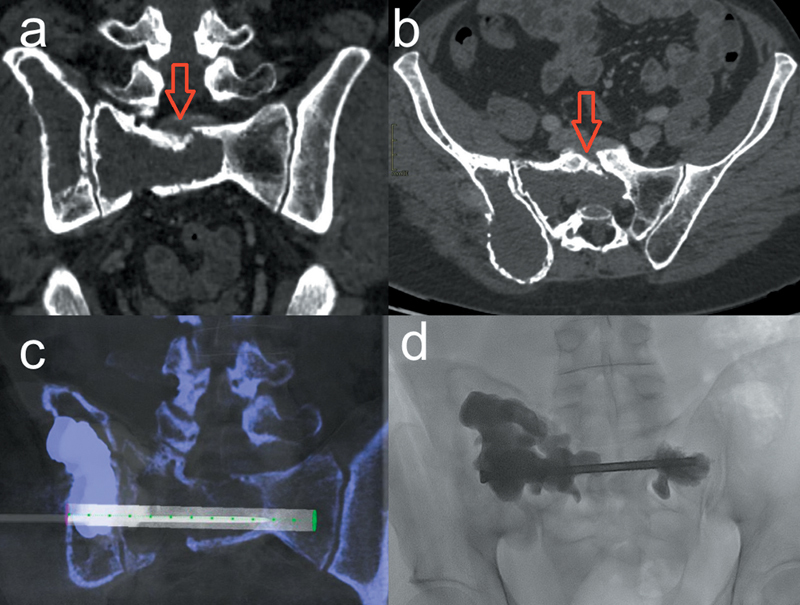
Percutaneous screw fixation and cementoplasty in a 42-year-old patient with multiple metastases of Ewing's sarcoma. Acute mechanical left sciatic pain while standing. ( a and b ) Coronal and axial CT shows a large osteolysis of the sacrum and the right iliac wing. Note the vertical fracture of the sacrum involving the first left sacral hole (arrows). ( c and d ) Cone beam CT-guided consolidation is performed; A trans-sacro-iliac 12-cm screw is inserted. Additional cementoplasty of the iliac wing and the sacral wings is performed to reinforce the bone and to avoid secondary screw displacement.
Complications associated with percutaneous screw fixation remain rare. In a series of 36 pelvic bone and proximal femur metastases, Cazzato et al reported pain and functional improvement in 87.1% of cases. 30 Three patients had unfavorable outcome because of insufficient consolidation ( n = 1) or secondary screw displacement ( n = 2).
Combination of Cementoplasty and Surgery
For complex spine metastases, vertebroplasty can sometimes be combined with posterior surgical fixation: posterior surgical approach achieves neurological decompression with laminectomy, and sagittal stabilization with osteosynthesis; but vertebroplasty can consolidate the vertebral body and thus avoids complex anterior surgical approach.
Cementoplasty can also be performed after prior fixation, if surgical material becomes loose. The aim is then to preserve the osteosynthesis and thus to avoid major salvage surgery associated with high morbidity ( Fig. 6 ).
Fig. 6.
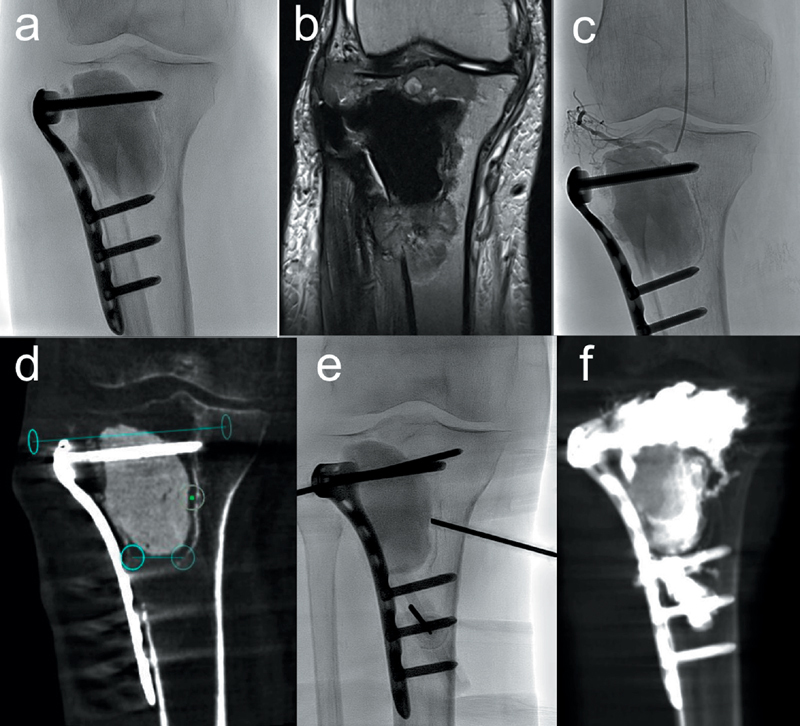
Proximal painful tibial metastasis of renal cancer in a 62-year-old patient. ( a and b ) Plain film ( a ) and proton density–weighted MRI sequence show tumor recurrence around surgical material. ( c ) Selective embolization is first performed, using microparticles. ( d–f ) Cone beam CT-guided cementoplasty is then performed to reinforce the proximal tibia and to avoid secondary rupture of the surgical fixation. Planning of the bone trocar trajectories ( d ); insertion of three 11-gauge bone trocars ( e ); control after cement injection ( f ).
Conclusion
Bone metastases have a dramatic impact on patient's quality of life, because of pain and functional impairment. Moreover, improved life expectancy in cancer patients is associated with an increased rate of benign fractures due to osteoporosis. Interventional radiology plays a major role for bone consolidation in oncology. Cementoplasty remains the major technique, as it achieves a fast and durable stabilization of weight-bearing bones submitted to compression strength. This minimally invasive technique does not contraindicate other focal therapies such as radiotherapy or surgery. Moreover, systemic treatment can rapidly be resumed after cementoplasty, if needed. Vertebral expandable devices did not prove clinical benefit in the field of oncology. For complex pelvic bone destruction or in case of sacral radio-necrosis with fractures involving sacral holes, cementoplasty as a standalone technique may provide insufficient consolidation. In such circumstances, percutaneous screw fixation can expand the field of image-guided bone consolidation.
Multidisciplinary approach remains mandatory for optimal patient selection.
Note
For an overview of the use of vertebroplasty and kyphoplasty for the palliation of pain in the cancer patient, the reader is referred to a prior publication by Shaibani et al in Seminars in Interventional Radiology . 32
References
- 1.Coleman R E.Clinical features of metastatic bone disease and risk of skeletal morbidity Clin Cancer Res 200612(20, Pt 2):6243s–6249s. [DOI] [PubMed] [Google Scholar]
- 2.Piccioli A, Spinelli M S, Maccauro G. Impending fracture: a difficult diagnosis. Injury. 2014;45 06:S138–S141. doi: 10.1016/j.injury.2014.10.038. [DOI] [PubMed] [Google Scholar]
- 3.Gangi A, Tsoumakidou G, Buy X, Quoix E. Quality improvement guidelines for bone tumour management. Cardiovasc Intervent Radiol. 2010;33(04):706–713. doi: 10.1007/s00270-009-9738-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Galibert P, Deramond H, Rosat P, Le Gars D. [Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty] Neurochirurgie. 1987;33(02):166–168. [PubMed] [Google Scholar]
- 5.Gangi A, Kastler B A, Dietemann J L. Percutaneous vertebroplasty guided by a combination of CT and fluoroscopy. AJNR Am J Neuroradiol. 1994;15(01):83–86. [PMC free article] [PubMed] [Google Scholar]
- 6.Cotten A, Dewatre F, Cortet B et al. Percutaneous vertebroplasty for osteolytic metastases and myeloma: effects of the percentage of lesion filling and the leakage of methyl methacrylate at clinical follow-up. Radiology. 1996;200(02):525–530. doi: 10.1148/radiology.200.2.8685351. [DOI] [PubMed] [Google Scholar]
- 7.McMahon S, Hawdon G, Baré J, Yu Y, Bertollo N, Walsh W R. In vivo response of bone defects filled with PMMA in an ovine model. Hip Int. 2011;21(05):616–622. doi: 10.5301/HIP.2011.8704. [DOI] [PubMed] [Google Scholar]
- 8.Brahimi Y, Antoni D, Buy X, Gangi A, Noël G. [Bone metastases relapse after cementoplasty: Case report and discussion about the combination of radiotherapy and cementoplasty] Cancer Radiother. 2016;20(02):109–114. doi: 10.1016/j.canrad.2015.09.012. [DOI] [PubMed] [Google Scholar]
- 9.Aebli N, Goss B G, Thorpe P, Williams R, Krebs J.In vivo temperature profile of intervertebral discs and vertebral endplates during vertebroplasty: an experimental study in sheep Spine 200631151674–1678., discussion 1679 [DOI] [PubMed] [Google Scholar]
- 10.Sabharwal T, Katsanos K, Buy X, Gangi A. Image-guided ablation therapy of bone tumors. Semin Ultrasound CT MR. 2009;30(02):78–90. doi: 10.1053/j.sult.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 11.Tsoumakidou G, Koch G, Caudrelier J et al. Image-guided spinal ablation: a review. Cardiovasc Intervent Radiol. 2016;39(09):1229–1238. doi: 10.1007/s00270-016-1402-6. [DOI] [PubMed] [Google Scholar]
- 12.Gangi A, Guth S, Imbert J P, Marin H, Dietemann J L. Percutaneous vertebroplasty: indications, technique, and results. Radiographics. 2003;23(02):e10. doi: 10.1148/rg.e10. [DOI] [PubMed] [Google Scholar]
- 13.Weill A, Chiras J, Simon J M, Rose M, Sola-Martinez T, Enkaoua E. Spinal metastases: indications for and results of percutaneous injection of acrylic surgical cement. Radiology. 1996;199(01):241–247. doi: 10.1148/radiology.199.1.8633152. [DOI] [PubMed] [Google Scholar]
- 14.Mathis J M. Percutaneous vertebroplasty: complication avoidance and technique optimization. AJNR Am J Neuroradiol. 2003;24(08):1697–1706. [PMC free article] [PubMed] [Google Scholar]
- 15.McGraw J K, Cardella J, Barr J Det al. Society of Interventional Radiology quality improvement guidelines for percutaneous vertebroplasty J Vasc Interv Radiol 200314(9, Pt 2):S311–S315. [DOI] [PubMed] [Google Scholar]
- 16.Alvarez L, Pérez-Higueras A, Quiñones D, Calvo E, Rossi R E. Vertebroplasty in the treatment of vertebral tumors: postprocedural outcome and quality of life. Eur Spine J. 2003;12(04):356–360. doi: 10.1007/s00586-003-0525-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shimony J S, Gilula L A, Zeller A J, Brown D B. Percutaneous vertebroplasty for malignant compression fractures with epidural involvement. Radiology. 2004;232(03):846–853. doi: 10.1148/radiol.2323030353. [DOI] [PubMed] [Google Scholar]
- 18.Khan O A, Brinjikji W, Kallmes D F. Vertebral augmentation in patients with multiple myeloma: a pooled analysis of published case series. AJNR Am J Neuroradiol. 2014;35(01):207–210. doi: 10.3174/ajnr.A3622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang J J, Zhou Y, Hu H Y et al. Safety and efficacy of multilevel vertebroplasty for painful osteolytic spinal metastases: a single-centre experience. Eur Radiol. 2017;27(08):3436–3442. doi: 10.1007/s00330-016-4683-x. [DOI] [PubMed] [Google Scholar]
- 20.Marcy P Y, Palussière J, Descamps B et al. Percutaneous cementoplasty for pelvic bone metastasis. Support Care Cancer. 2000;8(06):500–503. doi: 10.1007/s005200000138. [DOI] [PubMed] [Google Scholar]
- 21.Leclair A, Gangi A, Lacaze F et al. Rapid chondrolysis after an intra-articular leak of bone cement in treatment of a benign acetabular subchondral cyst: an unusual complication of percutaneous injection of acrylic cement. Skeletal Radiol. 2000;29(05):275–278. doi: 10.1007/s002560050607. [DOI] [PubMed] [Google Scholar]
- 22.Anselmetti G C, Manca A, Ortega C, Grignani G, Debernardi F, Regge D. Treatment of extraspinal painful bone metastases with percutaneous cementoplasty: a prospective study of 50 patients. Cardiovasc Intervent Radiol. 2008;31(06):1165–1173. doi: 10.1007/s00270-008-9396-3. [DOI] [PubMed] [Google Scholar]
- 23.Cazzato R L, Buy X, Eker O, Fabre T, Palussiere J. Percutaneous long bone cementoplasty of the limbs: experience with fifty-one non-surgical patients. Eur Radiol. 2014;24(12):3059–3068. doi: 10.1007/s00330-014-3357-9. [DOI] [PubMed] [Google Scholar]
- 24.Chen K H, Wu P K, Chen C F, Chen W M. Zoledronic acid-loaded bone cement as a local adjuvant therapy for giant cell tumor of the sacrum after intralesional curettage. Eur Spine J. 2015;24(10):2182–2188. doi: 10.1007/s00586-015-3978-y. [DOI] [PubMed] [Google Scholar]
- 25.Cardoso E R, Ashamalla H, Weng L et al. Percutaneous tumor curettage and interstitial delivery of samarium-153 coupled with kyphoplasty for treatment of vertebral metastases. J Neurosurg Spine. 2009;10(04):336–342. doi: 10.3171/2008.11.SPINE0856. [DOI] [PubMed] [Google Scholar]
- 26.Schroeder J E, Ecker E, Skelly A C, Kaplan L. Cement augmentation in spinal tumors: a systematic review comparing vertebroplasty and kyphoplasty. Evid Based Spine Care J. 2011;2(04):35–43. doi: 10.1055/s-0031-1274755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li Z, Ni C, Chen L et al. Kyphoplasty versus vertebroplasty for the treatment of malignant vertebral compression fractures caused by metastases: a retrospective study. Chin Med J (Engl) 2014;127(08):1493–1496. [PubMed] [Google Scholar]
- 28.Anselmetti G C, Manca A, Tutton S et al. Percutaneous vertebral augmentation assisted by PEEK implant in painful osteolytic vertebral metastasis involving the vertebral wall: experience on 40 patients. Pain Physician. 2013;16(04):E397–E404. [PubMed] [Google Scholar]
- 29.Mohme M, Riethdorf S, Dreimann M et al. Circulating tumour cell release after cement augmentation of vertebral metastases. Sci Rep. 2017;7(01):7196. doi: 10.1038/s41598-017-07649-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cazzato R L, Koch G, Buy X et al. Percutaneous image-guided screw fixation of bone lesions in cancer patients: double-centre analysis of outcomes including local evolution of the treated focus. Cardiovasc Intervent Radiol. 2016;39(10):1455–1463. doi: 10.1007/s00270-016-1389-z. [DOI] [PubMed] [Google Scholar]
- 31.Deschamps F, de Baere T, Hakime A et al. Percutaneous osteosynthesis in the pelvis in cancer patients. Eur Radiol. 2016;26(06):1631–1639. doi: 10.1007/s00330-015-3971-1. [DOI] [PubMed] [Google Scholar]
- 32.Shaibani A, Ali S, Bhatt H. Vertebroplasty and kyphoplasty for the palliation of pain. Semin Intervent Radiol. 2007;24(04):409–418. doi: 10.1055/s-2007-992329. [DOI] [PMC free article] [PubMed] [Google Scholar]


