Abstract
Percutaneous vertebral augmentation/consolidation techniques are varied. These are vertebroplasty, kyphoplasty, and several methods with percutaneous introduction of an implant (associated or not with cement injection). They are proposed in painful osteoporotic vertebral fractures and traumatic fractures. The objectives are to consolidate the fracture and, if possible, to restore the height of the vertebral body to reduce vertebral and regional kyphosis. Stabilization of the fracture leads to a reduction in pain and thus restores the spinal support function as quickly as possible, which is particularly important in the elderly. The effectiveness of these interventions on fracture pain was challenged once by two randomized trials comparing vertebroplasty to a sham intervention. Since then, many other randomized studies in support of vertebroplasty efficacy have been published. International recommendations reserve vertebroplasty for medical treatment failures on pain, but earlier positioning may be debatable if the objective is to limit kyphotic deformity or even reexpand the vertebral body. Recent data suggest that in osteoporotic fracture, the degree of kyphosis reduction achieved by kyphoplasty and percutaneous implant techniques, compared with vertebroplasty, is not sufficient to justify the additional cost and the use of a somewhat longer and traumatic procedure. In young patients with acute traumatic fractures and a significant kyphotic angle, kyphoplasty and percutaneous implant techniques are preferred to vertebroplasty, as in these cases a deformity reduction has a significant positive impact on the clinical outcome.
Keywords: vertebral fracture, vertebroplasty, kyphoplasty, vertebral augmentation techniques, interventional radiology
Objectives : Upon completion of this article, the reader will be able to describe the role of vertebral augmentation techniques in the treatment of vertebral fractures, patient selection for these procedures, and the potential complications associated with the fractures.
Percutaneous vertebral augmentation/consolidation techniques are varied. These are vertebroplasty, kyphoplasty, and several methods with percutaneous introduction of an implant (associated or not with cement injection). They are proposed in painful osteoporotic vertebral fractures and traumatic fractures. The objectives are to consolidate the fracture and, if possible, to restore the height of the vertebral body to reduce vertebral and regional kyphosis. Stabilization of the fracture leads to a reduction in pain and thus restores the spinal support function as quickly as possible, which is particularly important in the elderly. The effectiveness of these interventions on fracture pain was challenged once by two randomized trials comparing vertebroplasty to a sham intervention. Since then, many other randomized studies in support of vertebroplasty efficacy have been published. International recommendations reserve vertebroplasty for medical treatment failures on pain, but earlier decision may be debatable if the objective is to limit kyphotic deformity or even reexpand the vertebral body. Recent data suggest that in osteoporotic fracture, the degree of kyphosis reduction achieved by kyphoplasty or percutaneous implant techniques, compared with vertebroplasty, is not sufficient to justify the additional cost and the use of a somewhat longer and traumatic procedure. The data are different for traumatic fractures with vertebral and regional deformity where there is a larger consensus favoring kyphoplasty or percutaneous implant techniques, as in these cases a deformity reduction has a significant positive impact on the clinical outcome. However, the long-term benefit/safety balance is not well established in younger subjects.
Epidemiology and Consequences of Vertebral Fractures
Osteoporotic Vertebral Fractures
Osteoporotic vertebral fractures are very frequent in women after menopause, but also occur in men and younger subjects carrying risk factors for bone fragility. One postmenopausal woman in four will suffer from osteoporotic vertebral fractures. According to the classification of Genant, the loss of height of the fractured vertebra may be mild (20–25%), moderate (25–40%), or severe (>40%). The thoracolumbar region is the dominant location of vertebral fractures. 1 About two-thirds of vertebral fractures are asymptomatic, but others are responsible for a significant and disabling spinal pain. Often, the pain resolves spontaneously in a few weeks, and this spontaneous favorable outcome is an essential factor in interpreting the results of controlled trials. However, some patients remain handicapped for several months with severe pain that can justify the use of morphine and force the patient to a prolonged bed rest with increased risk of subsequent complications, especially the elderly persons. Three events can explain that intense pain persists beyond a few weeks: an increased loss of height of the vertebral body ( Fig. 1 ), an absence of consolidation of the fracture with pseudarthrosis ( Fig. 2 ), or the fracture of another vertebra ( Fig. 3 ). Indeed, in some cases, the fracture gradually increases, which can lead to a significant loss of height of the vertebral body with an increase in the kyphosis and its detrimental consequences on the vertebral column static, especially for fractures at the thoracolumbar junction ( Fig. 1 ). Sometimes, the fracture does not consolidate and a real pseudarthrosis is formed. In these cases, a linear intracorporeal cavity can be observed which may contain gas or liquid on the X-rays, computed tomography (CT), and magnetic resonance imaging (MRI; Fig. 2 ). This cavity materializes the absence of consolidation of the fracture site. Sometimes the gas or fluid accumulation is not spontaneously visible but may be suspected on the presence of a horizontal split in the vertebral body corresponding to pseudarthrosis. In these cases, an X-ray of the spinal profile in extension or a scanner may unmask the intrasomatic “void” image. Finally, osteoporotic vertebral fractures tend to cluster over time ( Fig. 3 ), and also in the same segment, worsening the spine deformities. In a cohort of osteoporotic women (mean age: 74 years) who recently had an osteoporotic vertebral fracture, the risk of a new vertebral fracture within a year increases from 3.6% if the patient has no prevalent vertebral fracture to 24% in those with at least two prevalent vertebral fractures. 2
Fig. 1.

Time course of an osteoporotic L1 fracture in a 72-year-old patient. On the initial T1-weighted MRI ( a ), the regional kyphosis angle was 17 degrees. The treatment was medical. The patient had an MRI 6 months later (b) for persistent thoracolumbar junction pain. The fracture increased, especially anteriorly, and the regional kyphosis angle increased from 17 to 22 degrees in the supine position (b).
Fig. 2.
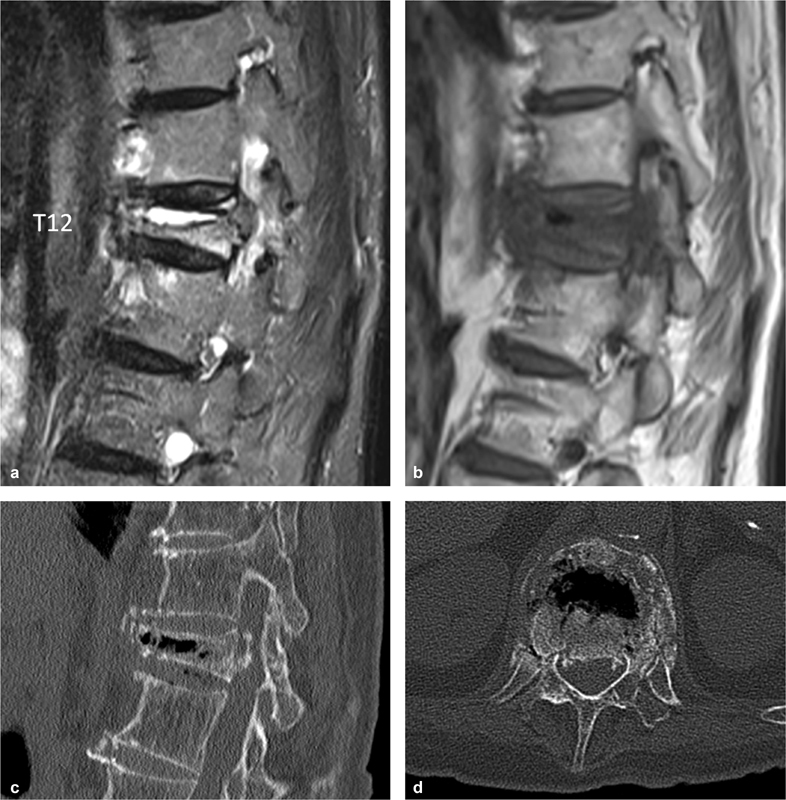
Osteoporotic fracture of T12 in a 78-year-old patient. Intracorporeal fluid cavity on T2-weighted MRI ( a ), mixed liquid and gas on T1-weighted MRI (b), and gas on CT scan ( c and d ). This cavity corresponds to a pseudarthrosis.
Fig. 3.

Cascade of osteoporotic fractures in a 76-year-old patient. The initial MRI ( a and b ) shows a recent or semi-recent fracture of the T10 and L2 vertebrae, and a discrete fracture of the lower L4 endplate. The persistence of pain leads the physician to propose a vertebroplasty. The new MRI ( c and d ), performed 2 months after the first one, shows four new fractures, T11, T12, upper endplate of L4, and L5.
Spinal fractures are accompanied by a loss of lumbar lordosis and an increase in thoracic kyphosis. In particular, fractures of the thoracolumbar level, the preferred site of osteoporotic fractures, at the junction between a relatively fixed spinal segment, and a mobile segment, often result in significant and functionally damaging angular kyphosis ( Fig. 4 ). Roux et al prospectively evaluated over 3 years the influence of thoracic kyphosis on the risk of incident vertebral fracture and on the quality of life in a population of 1,624 untreated osteoporotic postmenopausal women. 3 Increased kyphosis (whatever the cause) was a significant independent risk factor of a new vertebral fracture and altered quality of life. 3 Recent epidemiological studies have shown that osteoporotic vertebral fractures are also associated with excessive mortality. 4
Fig. 4.

T12 fracture with marked regional kyphosis. CT, sagittal image ( a ); radiography in flexion (b) .
Traumatic Vertebral Fractures
Fractures of the thoracolumbar spine can have very varied consequences, ranging from simple painful discomfort to paraplegia or even death. In young patients, the main causes are traffic accidents, falls from high places, sports accidents, and accidents at work. But traumatic thoracolumbar vertebral fractures are a heterogeneous group in terms of patient age, morphology, and severity of the fracture. It encompasses traumatic fractures in osteoporotic patients.
Several classification systems have been developed to better define the injury and help treatment decision making. These classifications are based on anatomical structures (Denis three-column system), mechanisms of injury (AO–Magerl classification 5 ), or commonly identified clinical and radiographic parameters (the thoracolumbar injury classification and severity score system, TLICS 6 7 ).
The AO-Magerl classification is based on the mechanism of injury, and has three main groups. 5 Group A corresponds to a compression mechanism (lesions mainly in the vertebral body) ranging from a simple fracture of the upper plate (A1) to a comminuted fracture (A3). Group B corresponds to distraction fractures. It is divided into three distinct groups: posterior flexion-distraction lesions with ligament predominance B1, posterior flexion-distraction lesions with bone predominance B2, and hyperextension lesions with anterior distraction B3. Finally, group C corresponds to lesions resulting from a rotating mechanism added to mechanisms of types A and B. This classification has a prognostic significance, the subdivisions from A to C being of increasing severity.
The TLICS system assigns a numerical score for three subcategories: morphology of injury, neurological involvement, and integrity of the posterior ligamentous complex. The individual scores for each subcategories are added to provide a global score used to guide treatment. 6 7 Management strategies will be discussed in a next paragraph.
Technique and Indications of Vertebroplasty and Kyphoplasty and Introduction of Implants into the Vertebral Body
Technique
Vertebroplasty was invented by Galibert and Deramond in 1987. 8 It consists of injecting an acrylic cement (polymethylmethacrylate) into the fractured vertebral body, which is of the same nature as that used to seal joint prostheses, and whose biological tolerance is well established. The vertebrae are approached posteriorly at the thoracic and lumbar levels. Most operators use a transpedicular route which has the advantage of containing any cement reflux within the vertebral body. The bipedicular approach requires more time but allows a better distribution of the cement in the vertebra at the lower thoracic and lumbar levels. At the upper and middle thoracic levels, a one-sided approach is often sufficient because the vertebral bodies are narrower. At the upper thoracic level, a suprapedicular or parapedicular pathway in the costovertebral space should be used. At the cervical level, the approach is anterolateral. Once the trocar is in place in the vertebral body, depending on the size of the vertebrae, 2 to 8 cm 3 of polymethylmethacrylate is slowly injected under continuous fluoroscopic control to ensure that there is no extravertebral cement leakage. Efforts should be made to fill the vertebral body from one vertebral plate to the other to form a forestay and prevent the risk of refracture of the same vertebral body. It is also necessary to try to have some filling of the posterior third of the vertebral body to avoid fracture at the cement–bone junction because refracture would be associated with a displacement of the posterior wall with the risk of neurological compression.
In balloon kyphoplasty ( Fig. 5 ), two balloons are inserted transpedicularly into the fractured vertebral body, then inflated under pressure to raise the vertebral endplates, and create an intracorporal cavity. The balloons are then deflated and removed, and the cement can be injected at low pressure to fill the created cavity which reduces the risk of extravertebral cement leakage. 9 To limit the loss of correction after balloon deflation, several reexpansion devices were further designed, for example, porous vessel balloon, titanium expansible supports, or coil filled systems, which are used to push the fractured vertebral endplates, and are left in place and embedded into the cement, or removed ( Fig. 6 ). The objective of these devices is to reduce, at least partially, the angle of vertebral and regional kyphosis sometimes important in certain fractures with cuneiform deformity of the vertebral body, and stabilize the reduction.
Fig. 5.

L1 vertebral kyphoplasty in a 68-year-old patient. The fractured L1 vertebra is the site of a pseudarthrosis on the T2 sagittal sequence ( a ) and radiograph ( b ). The steps of the intervention are introduction of the trocars ( c ), introduction of the drill ( d ), introduction of the balloons ( e ), the balloons are inflated ( f , g ) and then removed. Cement injection gradually filled the cavity ( h ). Control X-rays ( i and j ), and CT ( k and l ).
Fig. 6.
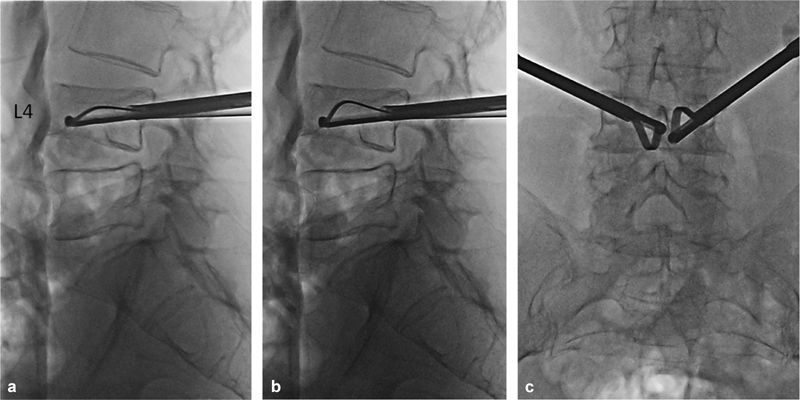
( a–c ) L4 vertebral fracture and reduction instruments. Gradual spreading of the slats under the upper left and lower right endplates.
Percutaneous fixation ( Fig. 7 ) of the spine consists of inserting pedicular screws and connecting them by two rods through centimeter-size incisions. This technique is a little more invasive than the previous ones. It is common to add a vertebroplasty or other vertebral augmentation technique to restore the height of the fractured vertebral body and reduce kyphosis, and moreover maintain kyphosis correction. The vertebroplasty/spinal augmentation technique stabilizes the anterior column and has an analgesic effect; fixation provides a stabilization of the middle and posterior columns. However, in patients with poor bone stock, mechanical failures of implants and rates of pseudarthrosis and screws pullout are high. Consequently, the combination of percutaneous fixation with cement-augmented screws can be a valuable option. Recently developed partially fenestrated screws allow a cement injection in the first anterior third of the screw, increasing the pullout strength with a minimized risk of cement leakage. 10 11 12 13
Fig. 7.

Kyphoplasty and percutaneous fixation for a traumatic fracture of L4 in a 55-year-old patient. The radiograph ( a ) and the CT scan ( b ) show a fracture of L4, type Magerl A3, with regional traumatic angulation of about 30 degrees. Partial restoration of vertebral body height by balloon kyphoplasty ( c ). Radiographs ( d, e ) showing the result of kyphoplasty coupled with percutaneous fixation L3–L5, with restoration of a relatively satisfactory lumbar lordosis.
Indications of Vertebroplasty and Other Vertebral Augmentation Techniques in Osteoporotic Fractures
The American and English recommendations (FDA and NICE, respectively) on the indication of vertebroplasty in osteoporotic fractures are precise: it should be reserved for cases where pain does not yield to medical analgesic treatment. However, should we always go through the medical treatment step in recent osteoporotic vertebral fractures? The answer to this question depends on the angle one adopts with regard to osteoporotic vertebral disease. Indeed, if we consider the fracture episode in isolation, since the pain amends spontaneously and the fracture consolidates in most cases in a few weeks or months, it seems logical to reserve vertebroplasty for failures of conservative treatment or in the elderly persons, in whom prolonged bed rest and pain-relieving drugs of level 2 or 3 carry significant risks. The point of view is different if we consider the vertebral statics as a whole and its consequences on the future of the patient. First, a significant percentage of recent fractures continue to increase after their occurrence, resulting in an increase in kyphosis angle ( Fig. 1 ). 14 A wedge-shaped fracture of the thoracolumbar junction or thoracic spine can generate 15 to 20 degrees of kyphosis, which is far from nonsignificant. Observation of such cases makes it regrettable that the patient could not benefit from vertebroplasty before the deformity became worse. Above all, some patients will develop new vertebral fractures whose accumulation in the same spinal segment will lead to the development of a severe angular kyphosis. Antiosteoporotic treatment, which must be systematic from the first fracture, reduces the risk of a new fracture by 50 to 70% but does not cancel it. The advanced age, spontaneous occurrence of the fracture, low bone mineral density, risk factors integrated in the FRAX score, 15 and especially the location of the fracture at the thoracolumbar junction and the number of prevalent vertebral fractures make it possible to predict, to a certain extent, the occurrence of new vertebral fractures. But the occurrence, number, and location of subsequent vertebral fractures remain largely unpredictable. However, vertebral kyphosis is a marker of physiological aging and a morbidity factor, due to the sagittal imbalance of the spine, the decrease in functional and respiratory capacities, the increased risk of falling and therefore new fractures; it also increases the risk of mortality. Kyphosis also creates a mechanical vicious circle: each vertebral fracture increases it and increases the anterior imbalance of the spine and the mechanical stresses on the other vertebrae and therefore the risk of a new fracture. The risk of complications due to vertebroplasty must also be taken into account. With the technological developments in the materials used (rheological qualities of polymethylmethacrylate cements mainly) and the experience of operators, the risks of venous leakage and symptomatic pulmonary embolism, and of passage in the spinal canal or intervertebral foramen responsible for nerve compression, have become rare. However, such risks exist as well as the risk of secondary infection. In addition, if the patient has more than two or three vertebrae to cement, general anesthesia is most often necessary carrying its own additional risk.
Considering all these elements, what is the attitude to adopt for a recent osteoporotic vertebral fracture with vertebral edema at MRI? In practice, the patient should be explained with the respective benefits and risks of conservative treatment and vertebroplasty. The patient usually chooses vertebroplasty when pain remains severe and disabling despite analgesic treatment. The patient should also be referred to vertebroplasty when the risk of new vertebral fractures and the risk of a spinal kyphosis creating a sagittal imbalance appear high: advanced age, spontaneous nature of the fracture, low bone mineral density, personal and family history of osteoporotic fractures, location of the fracture at the thoracolumbar level, and the presence of other vertebral fractures. The evaluation of the sagittal equilibrium of the spine by images of the entire spine (EOS system in particular) must also be systematically taken into account; its interest in guiding vertebroplasty indications linked to the risk of static deformity is currently being evaluated.
Not all persistent vertebral pain after an osteoporotic fracture needs a vertebroplasty. In most cases, the pain directly related to the fracture improves in a few weeks with consolidation of the fracture site. However, the deformity induced by the fracture can trigger joint, ligament, or muscle pain. It is important to bear in mind other potential static cause of pain, especially when it lasts longer than 6 to 8 weeks when the fracture has not increased in the meantime and the medullary “edema” of the fractured vertebra has been resolved by MRI. This is a very important confounding factor in published trials of vertebroplasty in osteoporotic fractures, particularly when the authors failed to perform an MRI shortly before vertebroplasty to verify the persistence of a medullary “edema” signal in the fractured vertebral body. 16 17 It is a good rule, moreover, when the fracture is no longer recent or the edema is not very marked on MRI, to start with an infiltration of cortisonic derivatives in the posterior joints because they can be responsible for persistent pain. 18 Muscle pain secondary to the static disorder induced by a severe fracture or iterative vertebral fractures is another cause of persistent pain. The induced kyphosis projects forward the top of the trunk and the head, and the patient must permanently contract his extensors of the spine to straighten the trunk and maintain a horizontal gaze. This spinal pain by muscular effort does not appear at the beginning of the passage to an erect position but after a certain period of time.
Indications of Vertebroplasty and Other Vertebral Augmentation Techniques in Traumatic Vertebral Fractures
The management of traumatic thoracolumbar fractures has evolved in recent years, mainly due to advances in surgical instrumentation. Minimally invasive techniques have developed in the face of an economic rationale to reduce the length of hospitalization, and a shift in mentalities toward shorter and less restrictive treatments with a desire to resume activities rapidly. The therapeutic possibilities are numerous, functional, orthopaedic, or surgical treatment. Four essential factors guide the therapeutic choice:
Neurological status : In case of neurological damage, treatment is usually a surgical procedure.
Spinal stability : Type C fractures are always unstable, always requiring a posterior surgical procedure more or less associated with fusion. Type B fractures with predominantly discoligamentary involvement are considered “permanently unstable,” requiring a surgical stabilization procedure with fusion. Type B fractures with predominant bone damage are considered “temporary unstable,” and orthopaedic treatment may be conceivable as well as fixation (percutaneous or not) without fusion on a short segment. Type A fractures do not affect the discoligamentary structures, and stability depends only on the extent of comminution of the vertebral body. Percutaneous vertebral augmentation techniques may be an option.
Impact on spinal statics : The deformity induced by the fracture can cause an imbalance of the spine in the frontal plane (asymmetric compression fracture), in the sagittal plane (local kyphosis caused by the fracture), or a rotational deformity which can induce a true secondary scoliosis. The sagittal deformity of the vertebra is measured by the vertebral kyphosis angle (VKA). The regional deformity assessed by the regional kyphosis angle (RKA) takes into account the deformity of the fractured vertebra but also the deformity caused by any associated disc or ligament lesions. The RKA allows the calculation of the regional traumatic angle (RTA) which is the RKA minus the regional physiological angulation of the fractured vertebral level. The RTA guides the therapeutic choice and the need for fracture reduction. The limit of 15 degrees imposes a reduction of the fracture (Boehler-type reduction brace, open reduction via internal fixation, reduction by external maneuvers for percutaneous fixation).
The “long-term outcome” : The clinical result is worsened by the importance of regional kyphosis and by vertebral comminution, although local kyphosis is compensated by changes in thoracic and lumbar curvatures and pelvic version. An attempt should also be made to assess the risk of pseudarthrosis (predominant ligament injury, “diabolo” fracture), and the risk of loss of correction due to fracture comminution or correction of kyphosis in the discs adjacent to the fracture.
Most of the therapeutic discussions concern type A fractures ( Figs. 5 and 6 ). In these cases, the extent of deformity, subtypes of fractures, locally available means (percutaneous fixation, kyphoplasty, implants), and root canal stenosis enter the discussion to choose the best option. Vertebral fractures A1.1 (endplate impaction), A1.2 (wedge impaction), A1.3 (vertebral body collapse), and A3.1 (incomplete burst fracture) can be managed with percutaneous vertebral augmentation technique, for analgesic and bone consolidation purposes. These techniques replace advantageously the orthopaedic management of fractures by brace, allowing quick recovery of the spinal function, and ideally a restoration and a maintenance of the normal angulation of the vertebra. When there is a traumatic regional angulation (regional kyphosis minus physiological angulation) greater than 15 degrees, it makes sense to prefer to vertebroplasty, a kyphoplasty, or the introduction of implants to perfectly restore height to the vertebral body ( Fig. 6 ). The choice to insert an implant and the type of implant also depends on the bone quality (normal bone mineral density or impaired bone quantity/quality). The use of percutaneous fixation is studied on a case-by-case basis. 19 20 Percutaneous fixation can be performed in normal bone or in fragile bone; in the latter case, cemented screws can provide valuable contribution. 12 13
Short- and Middle-Term Results
Efficacy of Vertebral Augmentation Techniques on Pain in Osteoporotic Fractures
The numerous open series on the efficacy of vertebroplasty 21 22 23 24 25 or kyphoplasty 26 27 28 29 reported a rapid analgesic effect in 60 to 100% of patients. These data were confirmed in reviews 29 30 and meta-analyses. 31 In a recent retrospective analysis of a series of 78 consecutive patients with vertebroplasty in our center, a significant reduction of pain was observed in 61.5% of cases. Predictive factors of a favorable outcome included an early procedure (performed within 2 months after fracture) and the absence of intravertebral cleft on preintervention imaging. 32
The results of the various randomized trials are apparently contradictory. However, these trials differ in many methodological aspects. At least six randomized trials compared vertebroplasty 33 34 35 36 37 38 or balloon kyphoplasty 39 with medical treatment. Their quality and methodological characteristics are unequal. In all but one of these trials, 36 vertebroplasty was superior in pain criteria. One of the best trials is the VERTOS 2 study which randomized 101 patients in a vertebroplasty group and 101 in a conventional medical treatment group with very strict inclusion criteria: pain evolving for less than 6 weeks, intensity of pain greater than or equal to 5 (as evaluated on a 10-grade VAS), osteopenia attested by bone densitometry, and especially the presence of a spinal fracture with bone marrow edema on a T2 MRI sequence. Under these methodological conditions, the authors observed a decrease in pain of more than 3 degrees on the VAS at 1 month and 1 year, and a decrease in analgesic consumption that went hand in hand with an improvement in quality of life. The tolerance was excellent with few immediate side effects and no increased risk of adjacent vertebral fractures. 35
In August 2009, the publication in the same issue of the New England Journal of Medicine of two multicenter double-blind controlled trials, one conducted by an Australian team from Melbourne 16 and the other by the Mayo Clinic team 17 had a great impact. The two trials compared percutaneous vertebroplasty and a sham vertebroplasty procedure with anesthesia of the skin and subcutaneous planes (lidocaine 1%) and periosteum (bupivacaine 0.25%), insertion of a needle against the spine, and opening of an acrylic cement bottle with a characteristic odor. These two studies did not show any superiority of vertebroplasty over the sham intervention on the pain. The Australian study randomized 71 patients with spinal pain for less than 12 months in relation to one or two “recent” osteoporotic vertebral fractures. Vertebroplasty did not improve any of the evaluation criteria compared with the sham procedure during the 6 months of follow-up. 16 The format of the second trial is very similar but with an additional methodological refinement since patients could ask to receive the other technique in a second time if they were dissatisfied with the first treatment. 17 Sixty-eight patients over the age of 50 with one to three painful fractures less than 1 year old were included in the vertebroplasty group and 63 patients in the sham group. MRI, the only way to establish the “recent” nature of the fracture, was done only if there was clinical doubt about its age and could be replaced by a bone scan. Neither difference was observed on the main criterion which was the evolution of the spinal handicap score on the Roland-Morris index nor any significant difference in terms of pain intensity between the two groups. Pain decreased from the first few days in both groups and the mean difference in pain at 3 months between the two groups was very small: 0.7 degrees on the VAS (−0.3 to 1.7; p = 0.19). It should be noted, however, that 43% of patients in the placebo group requested a change in treatment during the 3-month evaluation—that is, the “real” procedure—compared with only 12% in the vertebroplasty group. A first explanation for the negativity of these randomized trials is the importance of the “placebo effect” on pain of a sham procedure whose execution is very similar to that of a real intervention. The analysis of these two controlled trials also reveals several methodological limitations. The age of the fracture was very heterogeneous and a significant proportion of the patients had had pain for more than 3 months. Including patients up to 1 year after the occurrence of their osteoporotic vertebral fracture goes against clinical common sense, especially since the guarantees provided by the authors on the relationship between the fracture and persistent pain are insufficient. These trials have other technical limitations: the trocar was small, the approach was unipedicular and therefore the amount of cement injected into the vertebral bodies was relatively small. There is no medically managed fracture control group, so the trial conditions are far removed from clinical practice. Last but not least, two major limitations of these studies should be highlighted. The pain intensity required to include these patients was very moderate since the minimum threshold on the VAS required as inclusion criteria was only 3 11 or 4/10, 16 which is unfavorable to the demonstration of a clinically relevant therapeutic effect. In addition, patients were included without formally checking for the presence of a medullary edema signal on MRI, a major criterion for defining the recent nature of an osteoporotic vertebral fracture and its responsibility in vertebral pain.
Recently, a new randomized, multicenter, double-blind Australian trial (VAPOR study) concluded that vertebroplasty (mean amount of cement injected: 7.5 ± 2.8 mL) was superior to a sham procedure in 120 patients with one or two vertebral fractures less than 6 weeks old with edema at MRI and a pain intensity of at least 7/10. The primary endpoint was the proportion of patients with pain of less than 4/10 at day 14. Forty-four percent of patients in the vertebroplasty group versus 21% in the sham intervention group met this criterion with intent to treat. 40 Table 1 summarizes the main differences between the three randomized trials that compared vertebroplasty to a sham procedure. 16 17 40
Table 1. Main differences between three randomized trials comparing vertebroplasty to a sham procedure.
|
Buchbinder et al
16
n = 71 |
Kallmes et al
17
n = 131 |
Clark et al
40
n = 120 |
|
|---|---|---|---|
| Control group | Sham procedure (deep) | Sham procedure (deep) | Sham procedure (superficial) |
| Age of the fracture | < 1 year | < 1 year | < 6 wk |
| Medullary edema at MRI | Medullary edema or fracture line at MRI | MRI in some cases | 100% |
| Pain (visual analogic scale, VAS) | VAS ≥ 4 | VAS ≥ 3 | VAS ≥ 7 |
| Main criteria (D = day; M = month) |
VAS at D7, M1, M3, M6 | VAS at M1 | VAS < 4 at D14 |
Comparison of Vertebroplasty and Percutaneous Implant Techniques in Osteoporotic Fractures
Four randomized trials compared vertebroplasty and balloon kyphoplasty. 41 42 43 44 None of the four trials found any difference in the effect on pain and functional abilities. In one study, there were fewer new fractures within 2 years after kyphoplasty, but the difference was not significant. 41 There are more extravertebral cement leaks that remain asymptomatic with vertebroplasty but no more complications. 41
What about the correction of spinal deformity among techniques? The question is relevant because as mentioned earlier, the correction of kyphosis induced by the fracture could have a preventive action on the occurrence of new vertebral fractures. 3 Vertebroplasty, by hyperlordosing patients during the procedure 45 and by injecting the cement under pressure, can recover some of the vertebral height loss ( Fig. 8 ). But kyphoplasty aims at achieving better correction through the expansion of balloons or intracorporal devices ( Figs. 5 and 6 ). However, this gain suggested by the open trial data 29 46 and put forward by the firms developing these devices is not observed in randomized studies. 41 In reality, the gain in kyphosis angle of the cemented vertebra obtained by vertebroplasty or kyphoplasty is modest (the average correction of vertebral kyphosis angle is 2 to 3 degrees) and not significantly different between the two treatments, except in very recent fractures (first week of evolution) ( Fig. 8 ) and in pseudarthrotic fractures with split or intrasomatic void ( Fig. 9 ). 47 Furthermore, the small gain in vertebral kyphosis angle is not accompanied by a gain in regional kyphosis angle, which takes into account the discs and two adjacent vertebrae. 47 In fact, balloon kyphoplasty or, to a lesser degree, vertebroplasty (but with no significant difference) only reduces the increase in regional kyphosis that occurs in the year or 2 years following fracture. 41 47 However, various percutaneous implants exist and their potential to restore and maintain deformity correction is not equivalent. With balloon kyphoplasty, it incurs a loss of restored height when the balloon is deflated and removed. Spine Jack device, left in the vertebral body after its expansion, avoids the loss of correction before the cement injection and consequently allows a higher cement volume to be injected and maintenance of height restoration and kyphosis reduction. 48 49 50 Indeed several cadaveric and in vivo studies compared the percutaneous titanium-expandable device (Spine Jack) to balloon kyphoplasty, and concluded that the Spine Jack device was more able to reduce mechanically compressed vertebral bodies and maintain height restoration than balloon kyphoplasty. 48 49 50
Fig. 8.

L1 vertebral body height gain after cementoplasty of a traumatic fracture less than 1 week old in a 74-year-old patient. ( a–c ) X-ray and CT scan immediately before cementoplasty; ( d–f ) X-ray and CT scan immediately after cementoplasty.
Fig. 9.

Vertebroplasty of L1 and L2 vertebrae site of osteoporotic fractures in a 78-year-old male with Parkinson's disease. MRI ( a ) shows a large pseudarthrosis cavity. The X-ray before cementoplasty shows the reduced vertebral body height of L1 ( b ). After insertion of the trocars ( c ), when the L1 mandrel was removed, the cavity was filled with gas ( d ). L1 and L2 cementoplasty with L1 vertebral body height gain ( e and f ).
To conclude, in osteoporotic vertebral fractures, as it stands, it does not seem that the small gain in height and angle obtained by the kyphoplasty devices compared with vertebroplasty is sufficient to justify an additional expense and an increased duration of the intervention.
Does Vertebroplasty or Other Vertebral Augmentation Techniques Promote Fracture of Adjacent Vertebrae in Osteoporotic Patients?
A possible increase in the risk of a new vertebral fracture adjacent to a cemented vertebra has caused much discussion. The introduction of hard material between fragile vertebrae would precipitate their fracture. This risk of adjacent fracture sometimes encourages multiple injections of cement into vertebral bodies adjacent to the cemented vertebrae either when the MRI reveals a discrete edematous signal in an adjacent vertebra or when a healthy vertebra is interposed between two fractured vertebrae. It is obvious that this approach, intuitively logical, must be evaluated ( Figs. 10 and 11 ).
Fig. 10.

Successive fractures and vertebroplasties in an 87-year-old male. Osteoporotic fracture of L1 ( a ) treated with cementoplasty ( b, c ); fracture of T12 (vertebra above cementoplasty) 1 month after L1 cementoplasty ( d ); cementoplasty of T12 ( e ); fracture of T11 (vertebra above cementoplasty) 3 weeks after T12 cementoplasty ( f ).
Fig. 11.

Successive fractures and vertebroplasties in a 68-year-old female. Fractures of T11 and L1 ( a ); vertebroplasty of T11, L1, and T12 preventively ( b ); 15 days later, occurrence of a fracture of T10 (adjacent to vertebroplasty) and L3 (distant from vertebroplasty) ( c ).
Many open studies support an increased risk of fracture of adjacent vertebrae after vertebroplasty. 23 51 52 53 54 Grados et al 55 estimated that the risk of fracture of adjacent vertebrae was doubled in the year following vertebroplasty (relative risk: 2.27; 95% confidence interval [CI]: 1.1–4.56) when compared with the risk of fracture on a vertebra located at a distance from the vertebra injected (relative risk: 1.44; 95% CI: 0.82–2.55). However, it is important to remember that the natural evolution of the osteoporotic disease suggests that vertebral fractures tend to cluster over time and in the same spinal segment, and that the incidence of new vertebral fractures in the year following a medically treated osteoporotic fracture is of the same order as that observed after vertebroplasty. Of nine randomized trials comparing vertebroplasty and medical treatment, there was no significant difference in the incidence of new fractures after vertebroplasty or under medical treatment in seven studies, 16 17 35 36 38 39 40 an increased incidence in the vertebroplasty group in one trial 33 and an increased incidence in the medical treatment group in another trial. 34 Similarly, there does not appear to be any significant difference in the incidence of new fractures following balloon kyphoplasty or vertebroplasty. 41 However, recurrence of cemented vertebra fracture may be more frequent in vertebroplasty than in kyphoplasty 41 and, conversely, kyphoplasty may cause slightly more fractures of adjacent vertebrae, 56 but these data must be confirmed.
If osteoporotic fractures deserve a careful management, one should not forget to treat the underlying disease, osteoporosis. There are now effective medical treatments for osteoporosis. Since vertebral fractures are considered as severe (i.e., associated with increased mortality in epidemiologic studies), 4 the presence of such a fracture requires the prescription of an antiosteoporotic drug. Additional measures are also useful: normalization of vitamin D status, adequate calcium intake, advice on physical activity, fall prevention in elderly patients, and correction of associated risk factors. 57 Additionally, the patient must be informed to consult quickly in the event of new vertebral pain or loss of height to treat a new vertebral fracture in time.
What Are the Results of Vertebroplasty and Percutaneous Implant Techniques in Traumatic Vertebral Compression Fractures?
Unfortunately, most studies investigating the outcomes of conservative or percutaneous treatment after stable traumatic thoracolumbar vertebral fractures usually failed to address underlying bone mineral density and characteristics of the trauma, and consequently do not really separate osteoporotic and nonosteoporotic traumatic vertebral fracture. In a study addressing specifically nonosteoporotic patients, percutaneous vertebroplasty was shown to be a safe and effective technique for the treatment of stable traumatic thoracolumbar fractures, allowing a good pain control, beginning at the 2-hour follow-up, and early return to normal working activity and social life. 58 It was also demonstrated that balloon kyphoplasty was able to provide significant reduction in traumatic vertebral deformity while conserving free and healthy adjacent discs. 59 In a long-term investigation of the results related to nonsurgical treatment 60 or surgical treatment 61 of thoracolumbar burst fractures, the authors demonstrated the impact of long-lasting residual regional deformity and global imbalance on clinical outcomes. In particular, the large number of global, thoracic, and lumbosacral compensatory mechanisms that aim to balance the regional deformity was shown to have a negative impact on clinical outcomes. The maintenance of a close-to-physiological sagittal alignment with restoration of the regional kyphosis angle and thoracolumbar junction angle influences the clinical outcome measures. 60 61 This is in agreement with other studies indicating that sagittal imbalance caused by adult degenerative deformity or posttraumatic deformity promote increasing pain, worse clinical outcomes, and a loss of health-related quality of life. 62 63 To summarize, the traumatic fracture probably raises a greater demand for maintenance of correction than the osteoporotic fractures because the patients are younger.
What Are the Complications of Vertebroplasty and Other Spinal Augmentation Techniques?
The complications of vertebroplasty or other vertebral augmentation techniques are well known. 64 They are similar for osteoporotic or traumatic fractures. They are, on the whole, infrequent and operator dependent. Cement leakage may occur in the epidural space, foramens, pre- or laterovertebral soft tissues, adjacent intervertebral discs, and perivertebral vessels. Epidural or foraminal leakage can cause nerve compressions, but fortunately this complication is exceptional. Small asymptomatic venous leaks are common and are explained by the density of the perivertebral venous plexuses. 65 Distant cement vascular migrations are rare, but perhaps underestimated. Cement microembols in pulmonary vascularization are not uncommon if a noninjection chest CT is routinely performed after a vertebroplasty performed with low or medium viscosity cements. These cement microembolisms are exceptionally symptomatic, but warrant close monitoring in patients with respiratory insufficiency. Studies comparing vertebroplasty and balloon kyphoplasty suggest that the latter carries less risk of leakage. 66 Finally, the use of highly viscous cements is recommended to reduce this risk of leakage. 22 51 52 53 66
Conclusion
Osteoporotic vertebral fractures are associated with increased morbidity which is important to prevent by appropriate management of osteoporosis, but also to treat when a symptomatic vertebral fracture is responsible for significant pain and disability. In this context, vertebroplasty techniques could have several advantages—obtaining rapid analgesia, improving spinal support function, partial restoration of spinal statics—at low risk if the operator is experienced, and guidance imaging of sufficient quality. The superiority of kyphoplasty by balloon and other spinal expansion techniques still raises questions, even though its cost is much higher: this justifies continuing an evaluation effort, in particular with regard to the accuracy of the indications, while taking care to avoid any conflict of interest in this evaluation with the manufacturers of these devices. For the recent traumatic fracture, the reexpansion of the vertebral body using balloon kyphoplasty or implant devices seems more legitimate as sagittal imbalance caused by posttraumatic deformity and adult degenerative deformity has been shown to promote increasing pain, worse clinical outcomes, and a loss of health-related quality of life.
The reader is referred to several prior Seminars in Interventional Radiology articles for further information regarding vertebral augmentation techniques. 67 68 69 70 71
References
- 1.Fechtenbaum J, Cropet C, Kolta S, Verdoncq B, Orcel P, Roux C. Reporting of vertebral fractures on spine X-rays. Osteoporos Int. 2005;16(12):1823–1826. doi: 10.1007/s00198-005-1939-8. [DOI] [PubMed] [Google Scholar]
- 2.Lindsay R, Silverman S L, Cooper C et al. Risk of new vertebral fracture in the year following a fracture. JAMA. 2001;285(03):320–323. doi: 10.1001/jama.285.3.320. [DOI] [PubMed] [Google Scholar]
- 3.Roux C, Fechtenbaum J, Kolta S, Said-Nahal R, Briot K, Benhamou C-L. Prospective assessment of thoracic kyphosis in postmenopausal women with osteoporosis. J Bone Miner Res. 2010;25(02):362–368. doi: 10.1359/jbmr.090727. [DOI] [PubMed] [Google Scholar]
- 4.Edidin A A, Ong K L, Lau E, Kurtz S M. Life expectancy following diagnosis of a vertebral compression fracture. Osteoporos Int. 2013;24(02):451–458. doi: 10.1007/s00198-012-1965-2. [DOI] [PubMed] [Google Scholar]
- 5.Magerl F, Aebi M, Gertzbein S D, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3(04):184–201. doi: 10.1007/BF02221591. [DOI] [PubMed] [Google Scholar]
- 6.Vaccaro A R, Lehman R A, Jr, Hurlbert R J et al. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine. 2005;30(20):2325–2333. doi: 10.1097/01.brs.0000182986.43345.cb. [DOI] [PubMed] [Google Scholar]
- 7.Patel A A, Dailey A, Brodke D S et al. Thoracolumbar spine trauma classification: the Thoracolumbar Injury Classification and Severity Score system and case examples. J Neurosurg Spine. 2009;10(03):201–206. doi: 10.3171/2008.12.SPINE08388. [DOI] [PubMed] [Google Scholar]
- 8.Galibert P, Deramond H, Rosat P, Le Gars D. [Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty] Neurochirurgie. 1987;33(02):166–168. [PubMed] [Google Scholar]
- 9.Phillips F M, Todd Wetzel F, Lieberman I, Campbell-Hupp M.An in vivo comparison of the potential for extravertebral cement leak after vertebroplasty and kyphoplasty Spine 200227192173–2178., discussion 2178–2179 [DOI] [PubMed] [Google Scholar]
- 10.Cook S D, Salkeld S L, Stanley T, Faciane A, Miller S D. Biomechanical study of pedicle screw fixation in severely osteoporotic bone. Spine J. 2004;4(04):402–408. doi: 10.1016/j.spinee.2003.11.010. [DOI] [PubMed] [Google Scholar]
- 11.Sarzier J S, Evans A J, Cahill D W.Increased pedicle screw pullout strength with vertebroplasty augmentation in osteoporotic spines J Neurosurg 200296(3, Suppl):309–312. [DOI] [PubMed] [Google Scholar]
- 12.Pesenti S, Graillon T, Mansouri N et al. [Use of pedicle percutaneous cemented screws in the management of patients with poor bone stock] Neurochirurgie. 2016;62(06):306–311. doi: 10.1016/j.neuchi.2016.06.009. [DOI] [PubMed] [Google Scholar]
- 13.Pesenti S, Blondel B, Peltier E, Adetchessi T, Dufour H, Fuentes S. Percutaneous cement-augmented screws fixation in the fractures of the aging spine: is it the solution? BioMed Res Int. 2014;2014:610675. doi: 10.1155/2014/610675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cankaya D, Yilmaz S, Deveci A et al. Clinical and radiological outcomes of conservative treatment after stable post-traumatic thoracolumbar fractures in elderly: Is it really best option for all elderly patients? Ann Med Surg (Lond) 2015;4(04):346–350. doi: 10.1016/j.amsu.2015.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kanis J A, Johnell O, Oden A, Johansson H, McCloskey E. FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int. 2008;19(04):385–397. doi: 10.1007/s00198-007-0543-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Buchbinder R, Osborne R H, Ebeling P R et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med. 2009;361(06):557–568. doi: 10.1056/NEJMoa0900429. [DOI] [PubMed] [Google Scholar]
- 17.Kallmes D F, Comstock B A, Heagerty P J et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med. 2009;361(06):569–579. doi: 10.1056/NEJMoa0900563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wilson D J, Owen S, Corkill R A. Facet joint injections as a means of reducing the need for vertebroplasty in insufficiency fractures of the spine. Eur Radiol. 2011;21(08):1772–1778. doi: 10.1007/s00330-011-2115-5. [DOI] [PubMed] [Google Scholar]
- 19.Pishnamaz M, Oikonomidis S, Knobe M, Horst K, Pape H-C, Kobbe P. Open versus percutaneous stabilization of thoracolumbar spine fractures: a short-term functional and radiological follow-up. Acta Chir Orthop Traumatol Cech. 2015;82(04):274–281. [PubMed] [Google Scholar]
- 20.Cimatti M, Forcato S, Polli F, Miscusi M, Frati A, Raco A. Pure percutaneous pedicle screw fixation without arthrodesis of 32 thoraco-lumbar fractures: clinical and radiological outcome with 36-month follow-up. Eur Spine J. 2013;22 06:S925–S932. doi: 10.1007/s00586-013-3016-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cortet B, Cotten A, Boutry N et al. Percutaneous vertebroplasty in the treatment of osteoporotic vertebral compression fractures: an open prospective study. J Rheumatol. 1999;26(10):2222–2228. [PubMed] [Google Scholar]
- 22.Cyteval C, Sarrabère M P, Roux J O et al. Acute osteoporotic vertebral collapse: open study on percutaneous injection of acrylic surgical cement in 20 patients. AJR Am J Roentgenol. 1999;173(06):1685–1690. doi: 10.2214/ajr.173.6.10584820. [DOI] [PubMed] [Google Scholar]
- 23.Diamond T H, Bryant C, Browne L, Clark W A. Clinical outcomes after acute osteoporotic vertebral fractures: a 2-year non-randomised trial comparing percutaneous vertebroplasty with conservative therapy. Med J Aust. 2006;184(03):113–117. doi: 10.5694/j.1326-5377.2006.tb00148.x. [DOI] [PubMed] [Google Scholar]
- 24.Heini P F, Wälchli B, Berlemann U. Percutaneous transpedicular vertebroplasty with PMMA: operative technique and early results. A prospective study for the treatment of osteoporotic compression fractures. Eur Spine J. 2000;9(05):445–450. doi: 10.1007/s005860000182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zoarski G H, Snow P, Olan W Jet al. Percutaneous vertebroplasty for osteoporotic compression fractures: quantitative prospective evaluation of long-term outcomes J Vasc Interv Radiol 200213(2, Pt 1):139–148. [DOI] [PubMed] [Google Scholar]
- 26.Coumans J V, Reinhardt M K, Lieberman I H.Kyphoplasty for vertebral compression fractures: 1-year clinical outcomes from a prospective study J Neurosurg 200399(1, Suppl):44–50. [DOI] [PubMed] [Google Scholar]
- 27.Lieberman I H, Dudeney S, Reinhardt M K, Bell G. Initial outcome and efficacy of “kyphoplasty” in the treatment of painful osteoporotic vertebral compression fractures. Spine. 2001;26(14):1631–1638. doi: 10.1097/00007632-200107150-00026. [DOI] [PubMed] [Google Scholar]
- 28.Theodorou D J, Theodorou S J, Duncan T D, Garfin S R, Wong W H. Percutaneous balloon kyphoplasty for the correction of spinal deformity in painful vertebral body compression fractures. Clin Imaging. 2002;26(01):1–5. doi: 10.1016/s0899-7071(01)00350-3. [DOI] [PubMed] [Google Scholar]
- 29.Taylor R S, Fritzell P, Taylor R J. Balloon kyphoplasty in the management of vertebral compression fractures: an updated systematic review and meta-analysis. Eur Spine J. 2007;16(08):1085–1100. doi: 10.1007/s00586-007-0308-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pateder D B, Khanna A J, Lieberman I H.Vertebroplasty and kyphoplasty for the management of osteoporotic vertebral compression fractures Orthop Clin North Am 20073803409–418., abstract vii [DOI] [PubMed] [Google Scholar]
- 31.Eck J C, Nachtigall D, Humphreys S C, Hodges S D. Comparison of vertebroplasty and balloon kyphoplasty for treatment of vertebral compression fractures: a meta-analysis of the literature. Spine J. 2008;8(03):488–497. doi: 10.1016/j.spinee.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 32.Denoix E, Viry F, Ostertag A et al. What are the predictors of clinical success after percutaneous vertebroplasty for osteoporotic vertebral fractures? Eur Radiol. 2018;28(07):2735–2742. doi: 10.1007/s00330-017-5274-1. [DOI] [PubMed] [Google Scholar]
- 33.Blasco J, Martinez-Ferrer A, Macho J et al. Effect of vertebroplasty on pain relief, quality of life, and the incidence of new vertebral fractures: a 12-month randomized follow-up, controlled trial. J Bone Miner Res. 2012;27(05):1159–1166. doi: 10.1002/jbmr.1564. [DOI] [PubMed] [Google Scholar]
- 34.Farrokhi M R, Alibai E, Maghami Z. Randomized controlled trial of percutaneous vertebroplasty versus optimal medical management for the relief of pain and disability in acute osteoporotic vertebral compression fractures. J Neurosurg Spine. 2011;14(05):561–569. doi: 10.3171/2010.12.SPINE10286. [DOI] [PubMed] [Google Scholar]
- 35.Klazen C A, Lohle P N, de Vries Jet al. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial Lancet 2010376(9746):1085–1092. [DOI] [PubMed] [Google Scholar]
- 36.Rousing R, Hansen K L, Andersen M O, Jespersen S M, Thomsen K, Lauritsen J M. Twelve-months follow-up in forty-nine patients with acute/semiacute osteoporotic vertebral fractures treated conservatively or with percutaneous vertebroplasty: a clinical randomized study. Spine. 2010;35(05):478–482. doi: 10.1097/BRS.0b013e3181b71bd1. [DOI] [PubMed] [Google Scholar]
- 37.Voormolen M H, Mali W P, Lohle P N et al. Percutaneous vertebroplasty compared with optimal pain medication treatment: short-term clinical outcome of patients with subacute or chronic painful osteoporotic vertebral compression fractures. The VERTOS study. AJNR Am J Neuroradiol. 2007;28(03):555–560. [PMC free article] [PubMed] [Google Scholar]
- 38.Yang E-Z, Xu J-G, Huang G-Z et al. Percutaneous vertebroplasty versus conservative treatment in aged patients with acute osteoporotic vertebral compression fractures: a prospective randomized controlled clinical study. Spine. 2016;41(08):653–660. doi: 10.1097/BRS.0000000000001298. [DOI] [PubMed] [Google Scholar]
- 39.Wardlaw D, Cummings S R, Van Meirhaeghe Jet al. Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a randomised controlled trial Lancet 2009373(9668):1016–1024. [DOI] [PubMed] [Google Scholar]
- 40.Clark W, Bird P, Gonski Pet al. Safety and efficacy of vertebroplasty for acute painful osteoporotic fractures (VAPOUR): a multicentre, randomised, double-blind, placebo-controlled trial Lancet 2016388(10052):1408–1416. [DOI] [PubMed] [Google Scholar]
- 41.Dohm M, Black C M, Dacre A, Tillman J B, Fueredi G; KAVIAR Investigators.A randomized trial comparing balloon kyphoplasty and vertebroplasty for vertebral compression fractures due to osteoporosis AJNR Am J Neuroradiol 201435122227–2236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Evans A J, Kip K E, Brinjikji W et al. Randomized controlled trial of vertebroplasty versus kyphoplasty in the treatment of vertebral compression fractures. J Neurointerv Surg. 2016;8(07):756–763. doi: 10.1136/neurintsurg-2015-011811. [DOI] [PubMed] [Google Scholar]
- 43.Liu J T, Liao W J, Tan W C et al. Balloon kyphoplasty versus vertebroplasty for treatment of osteoporotic vertebral compression fracture: a prospective, comparative, and randomized clinical study. Osteoporos Int. 2010;21(02):359–364. doi: 10.1007/s00198-009-0952-8. [DOI] [PubMed] [Google Scholar]
- 44.Barr J D. Randomized controlled trial of vertebroplasty versus kyphoplasty in the treatment of vertebral compression fractures. J Neurointerv Surg. 2016;8(07):765–766. doi: 10.1136/neurintsurg-2016-012279. [DOI] [PubMed] [Google Scholar]
- 45.Carlier R Y, Gordji H, Mompoint D M, Vernhet N, Feydy A, Vallée C. Osteoporotic vertebral collapse: percutaneous vertebroplasty and local kyphosis correction. Radiology. 2004;233(03):891–898. doi: 10.1148/radiol.2333030400. [DOI] [PubMed] [Google Scholar]
- 46.Ledlie J T, Renfro M B. Kyphoplasty treatment of vertebral fractures: 2-year outcomes show sustained benefits. Spine. 2006;31(01):57–64. doi: 10.1097/01.brs.0000192687.07392.f1. [DOI] [PubMed] [Google Scholar]
- 47.Bossard P, Tran O, Vicaut E, Laredo J D.Vertebroplasty versus balloon kyphoplasty in osteoporotic fractures: results from a prospective randomized clinical trialPersonal communication
- 48.Krüger A, Baroud G, Noriega D et al. Height restoration and maintenance after treating unstable osteoporotic vertebral compression fractures by cement augmentation is dependent on the cement volume used. Clin Biomech (Bristol, Avon) 2013;28(07):725–730. doi: 10.1016/j.clinbiomech.2013.06.007. [DOI] [PubMed] [Google Scholar]
- 49.Krüger A, Oberkircher L, Figiel J et al. Height restoration of osteoporotic vertebral compression fractures using different intravertebral reduction devices: a cadaveric study. Spine J. 2015;15(05):1092–1098. doi: 10.1016/j.spinee.2013.06.094. [DOI] [PubMed] [Google Scholar]
- 50.Lin J H, Wang S H, Lin E Y, Chiang Y H. Better height restoration, greater kyphosis correction, and fewer refractures of cemented vertebrae by using an intravertebral reduction device: a 1-year follow-up study. World Neurosurg. 2016;90:391–396. doi: 10.1016/j.wneu.2016.03.009. [DOI] [PubMed] [Google Scholar]
- 51.Fribourg D, Tang C, Sra P, Delamarter R, Bae H.Incidence of subsequent vertebral fracture after kyphoplasty Spine 200429202270–2276., discussion 2277 [DOI] [PubMed] [Google Scholar]
- 52.Grafe I A, Da Fonseca K, Hillmeier J et al. Reduction of pain and fracture incidence after kyphoplasty: 1-year outcomes of a prospective controlled trial of patients with primary osteoporosis. Osteoporos Int. 2005;16(12):2005–2012. doi: 10.1007/s00198-005-1982-5. [DOI] [PubMed] [Google Scholar]
- 53.Mudano A S, Bian J, Cope J U et al. Vertebroplasty and kyphoplasty are associated with an increased risk of secondary vertebral compression fractures: a population-based cohort study. Osteoporos Int. 2009;20(05):819–826. doi: 10.1007/s00198-008-0745-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Uppin A A, Hirsch J A, Centenera L V, Pfiefer B A, Pazianos A G, Choi I S. Occurrence of new vertebral body fracture after percutaneous vertebroplasty in patients with osteoporosis. Radiology. 2003;226(01):119–124. doi: 10.1148/radiol.2261011911. [DOI] [PubMed] [Google Scholar]
- 55.Grados F, Depriester C, Cayrolle G, Hardy N, Deramond H, Fardellone P. Long-term observations of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. Rheumatology (Oxford) 2000;39(12):1410–1414. doi: 10.1093/rheumatology/39.12.1410. [DOI] [PubMed] [Google Scholar]
- 56.Frankel B M, Monroe T, Wang C. Percutaneous vertebral augmentation: an elevation in adjacent-level fracture risk in kyphoplasty as compared with vertebroplasty. Spine J. 2007;7(05):575–582. doi: 10.1016/j.spinee.2006.10.020. [DOI] [PubMed] [Google Scholar]
- 57.Briot K, Cortet B, Thomas T et al. 2012 update of French guidelines for the pharmacological treatment of postmenopausal osteoporosis. Joint Bone Spine. 2012;79(03):304–313. doi: 10.1016/j.jbspin.2012.02.014. [DOI] [PubMed] [Google Scholar]
- 58.Knavel E M, Thielen K R, Kallmes D F. Vertebroplasty for the treatment of traumatic nonosteoporotic compression fractures. AJNR Am J Neuroradiol. 2009;30(02):323–327. doi: 10.3174/ajnr.A1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Teyssédou S, Saget M, Gayet L E, Pries P, Brèque C, Vendeuvre T. Radiologic study of disc behavior following compression fracture of the thoracolumbar hinge managed by kyphoplasty: a 52-case series. Orthop Traumatol Surg Res. 2016;102(01):61–65. doi: 10.1016/j.otsr.2015.11.011. [DOI] [PubMed] [Google Scholar]
- 60.Koller H, Acosta F, Hempfing A et al. Long-term investigation of nonsurgical treatment for thoracolumbar and lumbar burst fractures: an outcome analysis in sight of spinopelvic balance. Eur Spine J. 2008;17(08):1073–1095. doi: 10.1007/s00586-008-0700-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mayer M, Ortmaier R, Koller H et al. Impact of sagittal balance on clinical outcomes in surgically treated T12 and L1 burst fractures: analysis of long-term outcomes after posterior-only and combined posteroanterior treatment. BioMed Res Int. 2017;2017:1.568258E6. doi: 10.1155/2017/1568258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Glassman S D, Bridwell K, Dimar J R, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine. 2005;30(18):2024–2029. doi: 10.1097/01.brs.0000179086.30449.96. [DOI] [PubMed] [Google Scholar]
- 63.Mac-Thiong J M, Transfeldt E E, Mehbod A A et al. Can c7 plumbline and gravity line predict health related quality of life in adult scoliosis? Spine. 2009;34(15):E519–E527. doi: 10.1097/BRS.0b013e3181a9c7ad. [DOI] [PubMed] [Google Scholar]
- 64.Laredo J D, Hamze B. Complications of percutaneous vertebroplasty and their prevention. Skeletal Radiol. 2004;33(09):493–505. doi: 10.1007/s00256-004-0776-8. [DOI] [PubMed] [Google Scholar]
- 65.Venmans A, Klazen C A, Lohle P N et al. Percutaneous vertebroplasty and pulmonary cement embolism: results from VERTOS II. AJNR Am J Neuroradiol. 2010;31(08):1451–1453. doi: 10.3174/ajnr.A2127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hulme P A, Krebs J, Ferguson S J, Berlemann U. Vertebroplasty and kyphoplasty: a systematic review of 69 clinical studies. Spine. 2006;31(17):1983–2001. doi: 10.1097/01.brs.0000229254.89952.6b. [DOI] [PubMed] [Google Scholar]
- 67.Kasper D M. Kyphoplasty. Semin Intervent Radiol. 2010;27(02):172–184. doi: 10.1055/s-0030-1253515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jay B, Ahn S H. Vertebroplasty. Semin Intervent Radiol. 2013;30(03):297–306. doi: 10.1055/s-0033-1353483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Prince E A, Ahn S H. Interventional management of vertebral body metastases. Semin Intervent Radiol. 2013;30(03):278–281. doi: 10.1055/s-0033-1353480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wang D T, Dubois M, Tutton S M. Complications in musculoskeletal intervention: important considerations. Semin Intervent Radiol. 2015;32(02):163–173. doi: 10.1055/s-0035-1549447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lea W, Tutton S. Decision making: osteoplasty, ablation, or combined therapy for spinal metastases. Semin Intervent Radiol. 2017;34(02):121–131. doi: 10.1055/s-0037-1602707. [DOI] [PMC free article] [PubMed] [Google Scholar]


