Abstract
Spinal pain is a common condition leading to significant disability and high cost. Spinal injections have been demonstrated to be effective short-term treatments with cost–utility superior to numerous other treatments, including surgical procedures. Appropriate patient selection—based on clinical and imaging finding—and the use of image guidance associated with technical precautions improve the safety and effectiveness of spinal injection and overall patient outcomes.
Keywords: spinal injection, epidural infiltration, foraminal infiltration, back pain, interventional radiology
Objectives : Upon completion of this article, the reader will be able to (1) explain the rationale of spinal injections; (2) identify the indication and the technique of epidural and transforaminal injection for spinal injection; (3) describe the indication and the technique for facet join syndrome treatment.
Spinal pain is the most common of all chronic pain disorders and it is associated with enormous economic, societal, and health impact. 1 The lifetime prevalence of spinal pain has been reported as 54 to 80% with a recurrence rate ranging from 24 to 80%, with low back pain (LBP) as the leading condition and neck pain (NP) as the fourth highest condition leading to disability. 2 3 4 The estimated cost of spinal pain in the United States has been calculated ranging from $560 billion to $630 billion per year, but it could also be higher as the incidence of spinal pain is growing up with the cost of spine-related care. 5 6 Patients having persistent LBP and NP are initially managed conservatively with medical therapies and physical therapy; however, the nonresponders are frequently treated with spinal steroid injections, although the efficacy of those treatments is still controversial. 6 7
General Principle
The zygapophysial joints (also called facet joints or l-z joints) and the intervertebral disc represent the anatomical unit of the spine able to support and stabilize the spine and prevent injury by limiting motion. 8 The discogenic pain is a painful condition due to alteration of the internal structure of the spinal disc (nucleus pulpous and annulus fibrosus) because of dehydration of the nucleus pulposus associated with radial fissures, conditioning disruption of the inner lamella of the annulus lending to internal disc disruption (IDD). 8 Phospholipase A2 and other enzymes have been described within the epidural space in IDD 9 ; those inflammation mediators recruit macrophages able to secrete cytokines and catalyze the inflammatory cascade, subsequently sustained by prostaglandins and leukotrienes. 10 The nerve endings, in this setting, are exposed to enzymes and breakdown products, causing pain. 10
Moreover, as a result of spinal disc dehydration and subsequent narrowing of the disc space, the pressure between l-z joint is increased significantly leading to zygapophysial joints degeneration associated with capsulitis, effusion, and periarticular edema resulting in change of facet joint positioning to sagittal plane, as aging occurs 11 ; this phenomenon is known as “tropism” which demonstrates a positive relation with intervertebral disc degeneration and herniation. 12 13 Corticosteroids inhibit the phospholipase A2 and thus the release of cytokines and the synthesis of prostaglandins, thereby reducing the inflammation. 14 15 Injectable corticosteroids are divided into two groups based on their chemical structure and subsequent effect 16 :
Nonparticulate corticosteroids , fully soluble and clear in appearance with rapid-onset but short-lived anti-inflammatory effects: nonparticulate preparation includes dexamethasone sodium phosphate and betamethasone sodium phosphate.
Particulate corticosteroids , suspensions contain corticosteroid ester insoluble in saline with delayed-onset and sustained anti-inflammatory effects: particulate preparation includes methylprednisolone acetate, triamcinolone acetonide, and betamethasone acetate.
The particulate corticosteroids have been associated with neurologic damage during transforaminal cervical and lumbar injections. The most widely accepted mechanism is thought to be direct intra-arterial administration into radicular arteries supplying the spinal cord resulting in embolic occlusion followed by ischemia or infarction of neural tissue. 17 18 Other mechanisms proposed include iatrogenic arterial injury from needle transection, dissection, vasospasm, or perforation.
In April 2014, the Food and Drug Administration (FDA) posted a safety announcement requiring manufacturers to add a warning about adverse neurologic events for spinal injection; however, no differences in risks and benefits of transforaminal versus interlaminar routes of administration and particulate versus nonparticulate formulations of steroids have been reported in that alert 19 20 ; because no neurologic complications due to nonparticulate corticosteroid use have been reported, some authors advocated the use of this preparation for whole site transforaminal procedures. 21 In a follow-up article in the New England Journal of Medicine outlining the FDA's risk assessment, the advisory committee concluded that all locations, approaches, and formulations of steroids used was associated with some risk of neurological injury. 22 Moreover, there was insufficient data to support contraindication of particulate steroids, even for cervical transforaminal injections that are considered to have the highest risk of neurological injury. 22
Indications
Although the efficacy of spinal injection is controversial and a comprehensive guideline is still not available, spinal infiltrations are widely used in the treatment of spinal pain. The perfect candidate for periradicular steroid injection is a patient with medical therapy–resistant radicular symptoms (positive Laseque's sign, decreased tendon reflex, sensation and motor response, and specific dermatomal pain distribution) due to disc decompression demonstrated with computed tomography (CT)/magnetic resonance imaging (MRI) at the corresponding level 23 ( Fig. 1 ).
Fig. 1.

Lumbar intraforaminal infiltration. ( a ) Sagittal reformatted CT image and axial CT image scan show a right intraforaminal disc herniation ( arrow ) at L5–S1 level, responsible for sciatic pain. ( B ) A 22-gauge needle ( arrow ) is inserted using CT guidance at the lower level of the foramina posteriorly to the nerve root.
Lumbar facet joint syndrome—characterized by median lumbar pain, with possible irradiation to gluteal regions and in the tight (never below the knee) without dermatomeric distribution, generally worst in the morning and after rest but also after hyperextension and torsion movements at the level of involved side—is a classical indication for steroid injection on zygapophysial joints 24 ( Fig. 2 ).
Fig. 2.

Facet joint syndrome and infiltration. ( a ) Sagittal T2w STIR MRI and axial T2w STIR MRI demonstrate bright signal at the level of the paravertebral muscles compatible with edema ( arrow ); note the bright signal at the level of FJ as fluid distension. Axial T1w postcontrast MRI depicts enhancement at the level of FJ and paravertebral muscles ( arrow ). ( b ) Oblique view demonstrates correct placement of needle during the facet joint infiltration.
Segmental instability poorly responds to spinal injection: when LBP is superimposed to neurogenic claudication and radiculopathy, the surgical treatment is often necessary. 14 In patients with chronic nonlocalizing LBP without specific MRI findings to support the level of the injection, an epidural L4–L5 spinal injection should be preferred because the preparation typically flows cranially and caudally. 14 Contraindications to corticosteroid spinal injections include hypersensitivity to the medication, uncorrectable coagulation disorders, local infections, diabetes, gastric ulcers, and pregnancy. Relative contraindications include hypersensitivity to steroids or iodine contrast agent (that could be avoided or substituted with gadolinium). 14 23 25 26
Technique
Patients are interviewed before the procedure to select and plan the treatment. It is mandatory to obtain a focused clinical history and to correlate the symptoms with the imaging findings. 14 The details of the procedure and expected results must be described to the patient to obtain the requested procedure approval, with a written informed consent signed at the end of the interview. 14
The procedure can be performed in an outpatient basis. 23 Strict sterilization of the area of interest with iodine solution (the use of extra solution containing alcohol varies among different centers) is used for rigorous and extensive skin disinfection to prevent infection 25 ( Fig. 3 ). Image-guided injections are preferred to blind procedures to avoid needle displacement 26 27 ; treatment can be performed under fluoroscopy or CT guidance. Moreover, the MR guidance and ultrasound guidance have been described in the literature 28 29 ( Fig. 4 ). Recently, the introduction of fusion imaging has been allowed a perfect match between CTI/MRI with the most available and inexpensive US images ( Fig. 5 ). CT guidance may improve the accuracy and safety of needle placement especially in the case of overlapping bones or in the presence of previous surgical treatment, whereas fluoroscopy can reduce the level of radiation exposure of the patient and the operator and it is less expansive 14 ( Fig. 1 ).
Fig. 3.

Materials for spinal infiltration. ( a , from the right top) needles' holder; sterile cloths, sterile dressings, and box with iodine solution to allow strict sterilization of the area of interest; syringes for anesthesia (10 mL) and for spinal injection (5 mL). The detail shows the 22-gauge needles are able to avoid the spinal structure.( b ) Needle placement. ( c ) Syringe with a mixture of particulate corticosteroid and anesthetic for lumbar injection. Note the needle holder with the needle used for operator safety.
Fig. 4.

Facet joint ecoguidance. ( a ) The needle placement under ultrasound guidance. ( b ) The needles placement. ( c ) The injection of corticosteroid at the level of FJ.
Fig. 5.
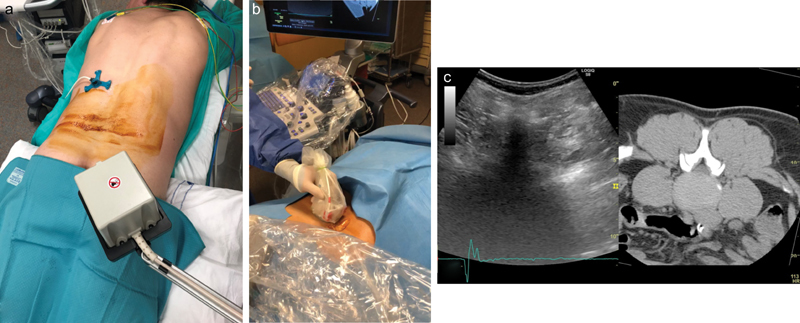
Fusion imaging for spinal infiltration. ( a ) The magnetic detector able to calibrate the images, previously acquired with CT exam in prone position with dedicated radiopaque tracking system. ( b ) The ultrasound scan during calibration of fusion imaging. ( c ) The ultrasound images (in the right) fused with CT images (on the left).
In the case of lumbar level injections, patient lays supine on the bed. The epidural lateral space is the target for posterolateral disc herniations, whereas the foramen is the landmark for foraminal and extraforaminal disc herniations 23 30 ( Fig. 6 ).
Fig. 6.

Spinal infiltration. ( a ) Facet joint infiltration: the needle could be inserted within the facet joint or at the level of median nerve pathway basing on patient symptom. ( b ) Lumbar infiltration: epidural lateral infiltration performed via interlaminar puncture or foraminal infiltration performed via an oblique posterolateral approach.
The epidural lateral infiltration is performed via interlaminar puncture with posterior approach using a 22-gauge needle; after passing the ligamentum flavum, an epidurogram with 1 mL of iodine contrast is necessary to confirm the needle tip position within the epidural space. The use of flash or positive blood aspirate is poorly sensitive to predict intravascular injection 23 30 ( Figs. 6 and 7 ).
Fig. 7.

Epidural infiltration with fluoroscopic guidance. ( a ) Anteroposterior view demonstrates the correct placement of 22-gauge needle at the level of L4–L5 with right translaminar approach. ( b ) Lateral view confirms the correct placement of 22-gauge needle at the level of L4–L5 with right translaminar approach.
In the case of correct needle position, 1.5 mL of long-acting steroid solution mixed with local anesthetic is injected; equal efficacy for local anesthetic with steroids and local anesthetic alone has been demonstrated in multiple spinal conditions except for disc herniation where the superiority of local anesthetic with steroids was seen over local anesthetic alone. 31 The exact mixture for the injectate varies widely among proceduralists. Long-acting synthetic steroids should be avoided for intrathecal injection because of the risk of chemical arachnoiditis. 32 In case of severe spinal canal stenosis, hydrocortisone is preferred, as long-acting synthetic steroids may transiently worsen the symptoms due to their hyperosmotic effect. 23
The foraminal infiltration is performed via an oblique posterolateral approach, slipping along the lateral border of l-z joints, targeting the lower part of the foramen to avoid the nerve root and the arterial vessel 23 30 ( Figs. 1 and 6 ).
Thoracic steroid injections are rarely performed; thus, intercostal radicular pain due to disc herniation is infrequent. Injection of long-acting steroids mixed with 1 mL of local anesthetic can be safely done with posterolateral approach via foraminal approach avoiding the nerve root and the vessels or via interlaminar approach in case of proximal thoracic level with large transverse processes. 23
In case of cervical steroid injection, the patient is positioned in supine with the head turned to the opposite side and with a cushion under the lower neck and upper thoracic spine to hyperextend the neck. 23 30 33
For periradicular infiltration, the 22-gauge is inserted via lateral approach with the needle tip reaching the anterior side of facet joint behind the nerve root, avoiding the vertebral artery. Subsequently, the tip position is checked with 1 to 2 mL of iodine contrast and 1.5 mL of long-acting steroid (3.75-mg cortivazol) solution is injected. 33 The injection of lidocaine should be avoided within the foramen, as it may diffuse around the spinal cord and induce transient phrenic nerve palsy. 23 33
In case of facet joint syndrome, treatment can be performed under CT guidance ( Fig. 8 ) or under fluoroscopy ( Fig. 9 ) with the C-arm positioned approximately 30 to 40 degrees on the side of the target joint to have the X-ray beam perpendicular to the zygapophysial joint 23 ; a 22-gauge needle is advanced and its position is checked with 0.5 mL of iodine contrast, assuming fluoroscopy guidance. Subsequently, 1.5 mL of long-acting steroid solution mixed with 1 mL of lidocaine 1% is injected slowly. 23
Fig. 8.

Facet joint infiltration. ( a ) Axial CT image demonstrates the correct placement of 22-gauge needle at the level of L4–L5 facet joint. ( b ) Axial CT image demonstrates the correct placement of 22-gauge needle at the level of L5–S1 facet joint and at the level of medial branch. ( c ) Axial CT image demonstrates the correct placement of 22-gauge needle at the level of L4–L5 medial branch.
Fig. 9.

Facet joint infiltration with fluoroscopic guidance. ( a ) Oblique view shows the correct placement of 22-gauge needle at the level of L5 facet joint; note the facet joint degeneration. ( b ) Oblique view shows the correct placement of 22-gauge needle at the level of L5 and S1 medial branches ( arrows ).
Results
Although there is no evidence-based synthesis on spinal injection, in Medicare population from 2000 to 2013 there was an overall increase in epidural injections of 102% with an annual increase of 5.6%, in particular for lumbar transforaminal epidural injections. 34
Strong evidence for short-term efficacy of spinal injection has been demonstrated from multiple high-quality trials, and moderate evidence for long-term efficacy from at least one high-quality trial for fluoroscopically guided caudal, lumbar interlaminar, and lumbar transforaminal epidural injections in managing lumbar disc herniation in terms of pain relief and functional improvement. 6 7 Moreover, a limited evidence suggested that epidural corticosteroid injections are not effective for spinal stenosis or nonradicular back pain. 35
A recent meta-analysis demonstrated a level II evidence for long-term management for cervical disc herniation treated with interlaminar epidural injections, for caudal and lumbar interlaminar epidural injections. The evidence of levels II to III in managing thoracic disc herniation with an interlaminar approach has been stated and a level III evidence for lumbar transforaminal epidural injections for lumbar spinal stenosis has been described. 6
While the effectiveness of steroid injection is still debated with short-term pain relief followed by a relapse of symptoms in an average 50% of treated patients at 6-month follow-up, the cost–utility of steroid injections is superior to numerous other modalities of treatments including spinal cord stimulation and surgical intervention. 36
However, severe complications after epidural injection have been reported in the literature with an incidence rate of less than 0.05%. 32 37 38 39 Major neurological complications—including stroke and spinal cord injury—seem to be related to particulate steroids administered via the cervical transforaminal route 31 36 37 ; there have been no known permanent neurological complications after nonparticulate steroid injections. 21
Needle displacement has been described as possible cause of nerve damage and bleeding; those events could be reduced with image-guided procedures and the use of blunt tip needles connected with catheters to avoid needle displacement during the injection. 36 37
Arachnoiditis is more common with the interlaminar technique and it may originate from inadvertent introduction of particulate steroid in the intrathecal space, which can be limited with the image guidance. 31 36 37 Fast injection of large injectable with subsequent increase in retinal venous pressures has been related to some cases of blindness. 38 A maximum of four infiltrations per year should be performed at the same level to avoid secondary lipodistrophy. 22
Although rare in occurrence, infectious complications after steroid spinal injection—as meningitis and epidural abscess—are related to contamination especially because of fungal infections, which could be avoid with strict sterilization. 36 37 40
Conclusion
Image guidance in spinal injection plays an important role for spinal pain management. The knowledge of anatomic landmarks and pathophysiology is mandatory to obtain an effective spinal injection and to avoid complications. CT and fluoroscopy—and also ultrasound and magnetic resonance—can be used to precise target and delivery of the injectable to relieve the pain caused by spinal disorder, allowing low-dose drug administration and reducing the risk of complications. The choice of injection site and injectate must be carefully planned before the procedure, after clinical examination and image review.
Spinal injections have been demonstrated with strong evidence only for short-term efficacy and it is probably related to the intrinsic mechanism of corticosteroid action, that is, to reduce the inflammation but not to treat the spinal disorder. Thus, image guidance is essential to reduce the dose of injectate and to precisely target its injection at the site of inflammation. The cost–utility of spinal injection has been demonstrated to be superior to numerous other treatments, including surgery, resulting in the recent growth of image-guided steroid spinal injections. The reader is referred to a previous article by Iannuccilli et al for further information regarding steroid injections for pain management. 41
References
- 1.Abdi S, Datta S, Trescot A M et al. Epidural steroids in the management of chronic spinal pain: a systematic review. Pain Physician. 2007;10(01):185–212. [PubMed] [Google Scholar]
- 2.Murray C J, Atkinson C, Bhalla K et al. The state of US health, 1990-2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310(06):591–608. doi: 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hoy D, March L, Brooks P et al. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73(06):968–974. doi: 10.1136/annrheumdis-2013-204428. [DOI] [PubMed] [Google Scholar]
- 4.Hoy D, March L, Woolf A et al. The global burden of neck pain: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73(07):1309–1315. doi: 10.1136/annrheumdis-2013-204431. [DOI] [PubMed] [Google Scholar]
- 5.Gaskin D J, Richard P. The economic costs of pain in the United States. J Pain. 2012;13(08):715–724. doi: 10.1016/j.jpain.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 6.Kaye A D, Manchikanti L, Abdi S et al. Efficacy of epidural injections in managing chronic spinal pain: a best evidence synthesis. Pain Physician. 2015;18(06):E939–E1004. [PubMed] [Google Scholar]
- 7.Manchikanti L, Buenaventura R M, Manchikanti K N et al. Effectiveness of therapeutic lumbar transforaminal epidural steroid injections in managing lumbar spinal pain. Pain Physician. 2012;15(03):E199–E245. [PubMed] [Google Scholar]
- 8.Cavanaugh J M, Ozaktay A C, Yamashita H T, King A I. Lumbar facet pain: biomechanics, neuroanatomy and neurophysiology. J Biomech. 1996;29(09):1117–1129. doi: 10.1016/0021-9290(96)00023-1. [DOI] [PubMed] [Google Scholar]
- 9.Saal J S, Franson R C, Dobrow R, Saal J A, White A H, Goldthwaite N. High levels of inflammatory phospholipase A2 activity in lumbar disc herniations. Spine. 1990;15(07):674–678. doi: 10.1097/00007632-199007000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Olmarker K, Blomquist J, Strömberg J, Nannmark U, Thomsen P, Rydevik B. Inflammatogenic properties of nucleus pulposus. Spine. 1995;20(06):665–669. doi: 10.1097/00007632-199503150-00006. [DOI] [PubMed] [Google Scholar]
- 11.Dunlop R B, Adams M A, Hutton W C. Disc space narrowing and the lumbar facet joints. J Bone Joint Surg Br. 1984;66(05):706–710. doi: 10.1302/0301-620X.66B5.6501365. [DOI] [PubMed] [Google Scholar]
- 12.Murtagh F R, Paulsen R D, Rechtine G R. The role and incidence of facet tropism in lumbar spine degenerative disc disease. J Spinal Disord. 1991;4(01):86–89. [PubMed] [Google Scholar]
- 13.Farfan H F, Huberdeau R M, Dubow H I. Lumbar intervertebral disc degeneration: the influence of geometrical features on the pattern of disc degeneration--a post mortem study. J Bone Joint Surg Am. 1972;54(03):492–510. [PubMed] [Google Scholar]
- 14.Palmer W E. Spinal injections for pain management. Radiology. 2016;281(03):669–688. doi: 10.1148/radiol.2016152055. [DOI] [PubMed] [Google Scholar]
- 15.Lee H M, Weinstein J N, Meller S T, Hayashi N, Spratt K F, Gebhart G F. The role of steroids and their effects on phospholipase A2. An animal model of radiculopathy. Spine. 1998;23(11):1191–1196. doi: 10.1097/00007632-199806010-00001. [DOI] [PubMed] [Google Scholar]
- 16.Derby R, Lee S H, Date E S, Lee J H, Lee C H. Size and aggregation of corticosteroids used for epidural injections. Pain Med. 2008;9(02):227–234. doi: 10.1111/j.1526-4637.2007.00341.x. [DOI] [PubMed] [Google Scholar]
- 17.Scanlon G C, Moeller-Bertram T, Romanowsky S M, Wallace M S. Cervical transforaminal epidural steroid injections: more dangerous than we think? Spine. 2007;32(11):1249–1256. doi: 10.1097/BRS.0b013e318053ec50. [DOI] [PubMed] [Google Scholar]
- 18.Okubadejo G O, Talcott M R, Schmidt R E et al. Perils of intravascular methylprednisolone injection into the vertebral artery. An animal study. J Bone Joint Surg Am. 2008;90(09):1932–1938. doi: 10.2106/JBJS.G.01182. [DOI] [PubMed] [Google Scholar]
- 19.U.S. Food and Drug Administration.Drug Safety Communications. FDA Drug Safety Communication: FDA requires label changes to warn of rare but serious neurologic problems after epidural corticosteroid injections for painAvailable:http://www.fda.gov/downloads/Drugs/DrugSafety/UCM394286.pdf. Accessed September 15, 2018
- 20.American Society of Anesthesiologists.ASA Formally Responding to FDA Warning on Injection of Corticosteroids into Epidural SpaceAvailable:https://www.asahq.org/advocacy/fda-and-washington-alerts/washington-alerts/2014/07/asa-formally-responding-to-fda-warning-on-injection-of-corticosteroids-into-epiduralspace?page=5. Accessed September 15, 2018
- 21.Rathmell J P, Benzon H T, Dreyfuss P et al. Safeguards to prevent neurologic complications after epidural steroid injections: consensus opinions from a multidisciplinary working group and national organizations. Anesthesiology. 2015;122(05):974–984. doi: 10.1097/ALN.0000000000000614. [DOI] [PubMed] [Google Scholar]
- 22.Racoosin J A, Seymour S M, Cascio L, Gill R. Serious neurologic events after epidural glucocorticoid injection--the FDA's risk assessment. N Engl J Med. 2015;373(24):2299–2301. doi: 10.1056/NEJMp1511754. [DOI] [PubMed] [Google Scholar]
- 23.Buy X, Gangi A. Percutaneous treatment of intervertebral disc herniation. Semin Intervent Radiol. 2010;27(02):148–159. doi: 10.1055/s-0030-1253513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lilius G, Laasonen E M, Myllynen P, Harilainen A, Grönlund G. Lumbar facet joint syndrome. A randomised clinical trial. J Bone Joint Surg Br. 1989;71(04):681–684. doi: 10.1302/0301-620X.71B4.2527856. [DOI] [PubMed] [Google Scholar]
- 25.Bogduk N. International Spinal Injection Society guidelines for the performance of spinal injection procedures. Part 1: Zygapophysial joint blocks. Clin J Pain. 1997;13(04):285–302. doi: 10.1097/00002508-199712000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Kelekis A D, Filippiadis D K, Martin J B, Brountzos E. Standards of practice: quality assurance guidelines for percutaneous treatments of intervertebral discs. Cardiovasc Intervent Radiol. 2010;33(05):909–913. doi: 10.1007/s00270-010-9952-5. [DOI] [PubMed] [Google Scholar]
- 27.Renfrew D L, Moore T E, Kathol M H, el-Khoury G Y, Lemke J H, Walker C W. Correct placement of epidural steroid injections: fluoroscopic guidance and contrast administration. AJNR Am J Neuroradiol. 1991;12(05):1003–1007. [PMC free article] [PubMed] [Google Scholar]
- 28.Deli M, Fritz J, Mateiescu S et al. Saline as the sole contrast agent for successful MRI-guided epidural injections. Cardiovasc Intervent Radiol. 2013;36(03):748–755. doi: 10.1007/s00270-012-0489-7. [DOI] [PubMed] [Google Scholar]
- 29.Provenzano D A, Narouze S. Sonographically guided lumbar spine procedures. J Ultrasound Med. 2013;32(07):1109–1116. doi: 10.7863/ultra.32.7.1109. [DOI] [PubMed] [Google Scholar]
- 30.Shim E, Lee J W, Lee E, Ahn J M, Kang Y, Kang H S. Fluoroscopically guided epidural injections of the cervical and lumbar spine. Radiographics. 2017;37(02):537–561. doi: 10.1148/rg.2017160043. [DOI] [PubMed] [Google Scholar]
- 31.Manchikanti L, Nampiaparampil D E, Manchikanti K N et al. Comparison of the efficacy of saline, local anesthetics, and steroids in epidural and facet joint injections for the management of spinal pain: a systematic review of randomized controlled trials. Surg Neurol Int. 2015;6 04:S194–S235. doi: 10.4103/2152-7806.156598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Manchikanti L, Hirsch J A. Neurological complications associated with epidural steroid injections. Curr Pain Headache Rep. 2015;19(05):482. doi: 10.1007/s11916-015-0482-3. [DOI] [PubMed] [Google Scholar]
- 33.Gangi A, Tsoumakidou G, Buy X, Cabral J F, Garnon J. Percutaneous techniques for cervical pain of discal origin. Semin Musculoskelet Radiol. 2011;15(02):172–180. doi: 10.1055/s-0031-1275601. [DOI] [PubMed] [Google Scholar]
- 34.Manchikanti L, Pampati V, Falco F JE, Hirsch J A. An updated assessment of utilization of interventional pain management techniques in the Medicare population: 2000 - 2013. Pain Physician. 2015;18(02):E115–E127. [PubMed] [Google Scholar]
- 35.Chou R, Hashimoto R, Friedly J . Rockville, MD: Agency for Healthcare Research and Quality (US); 2015. Pain Management Injection Therapies for Low Back Pain. [PubMed] [Google Scholar]
- 36.Manchikanti L, Falco F JE, Pampati V, Cash K A, Benyamin R M, Hirsch J A. Cost utility analysis of caudal epidural injections in the treatment of lumbar disc herniation, axial or discogenic low back pain, central spinal stenosis, and post lumbar surgery syndrome. Pain Physician. 2013;16(03):E129–E143. [PubMed] [Google Scholar]
- 37.Manchikanti L, Benyamin R M. Key safety considerations when administering epidural steroid injections. Pain Manag. 2015;5(04):261–272. doi: 10.2217/pmt.15.17. [DOI] [PubMed] [Google Scholar]
- 38.Bicket M C, Chakravarthy K, Chang D, Cohen S P. Epidural steroid injections: an updated review on recent trends in safety and complications. Pain Manag. 2015;5(02):129–146. doi: 10.2217/pmt.14.53. [DOI] [PubMed] [Google Scholar]
- 39.Kim W, Kim J S, Lim S C, Kim Y I, Moon D E. Reversible posterior leukoencephalopathy syndrome after cervical transforaminal epidural steroid injection presenting as transient blindness. Anesth Analg. 2011;112(04):967–970. doi: 10.1213/ANE.0b013e31820bff7e. [DOI] [PubMed] [Google Scholar]
- 40.Chiller T M, Roy M, Nguyen D et al. Clinical findings for fungal infections caused by methylprednisolone injections. N Engl J Med. 2013;369(17):1610–1619. doi: 10.1056/NEJMoa1304879. [DOI] [PubMed] [Google Scholar]
- 41.Iannuccilli J D, Prince E A, Soares G M. Interventional spine procedures for management of chronic low back pain-a primer. Semin Intervent Radiol. 2013;30(03):307–317. doi: 10.1055/s-0033-1353484. [DOI] [PMC free article] [PubMed] [Google Scholar]


