Abstract
Purpose
Carpal tunnel release (CTR) is a common surgical procedure, representing a financial burden to the health care system. The purpose of this study is to test whether the choice of CTR technique (open [OCTR] versus endoscopic [ECTR]), surgical setting (operating room [OR] versus procedure room [PR]), and anesthetic type (local, monitored anesthesia care [MAC], Bier block, general) affect costs or payments.
Methods
Consecutive adult patients undergoing isolated unilateral CTR between 5/13/2014 – 10/27/2017 at a single academic medical center were identified. Patients undergoing ECTR converted to OCTR, revision surgery, or additional procedures, were excluded. Using our institution’s information technology value tools, we calculated total direct costs (TDC), total combined payment (TCP), hospital payment, surgeon payment, and anesthesia payment for each surgical encounter. Cost data were normalized using each participant’s surgical encounter cost divided by the average cost in the data set and compared across 8 groups (defined by surgery type, operation location and anesthesia type).
Results
Of 479 included patients, the mean age was 55.3 ± 16.1 years, and 68% were female. Payer mix included commercial (45%), Medicare (37%), Medicaid (13%), workers compensation (2%), self-pay (1%) and other (3%) insurance types. TDC and TCP both differed significantly between each CTR release group, and OCTR in the PR under local anesthesia was the lowest. OCTR/local/OR, OCTR/MAC/OR, and ECTR/OR, were associated with 6.3-fold, 11.0-fold, and 12.4–16.6-fold greater TDC than OCTR/local/PR, respectively.
Conclusions
Performing open carpal tunnel release under local anesthetic in the procedure room setting significantly minimizes direct surgical encounter costs relative to other surgical methods (endoscopic), anesthetic methods (Bier block, MAC, general), and surgical settings (OR).
Clinical Relevance Statement
This study identifies modifiable factors that may lead to cost reductions for CTR surgery.
Keywords: Carpal tunnel release, cost, payment, procedure room, WALANT
Introduction
The value of health care delivered in the United States has received increased attention in the past decade, in part due to policy changes that have included value-based payment models.1,2 Carpal tunnel syndrome (CTS) is one of the most common clinical entities involving the hand and wrist, and treatment costs attributed to CTS represent a burden to the health care system.3
Hand surgeons have several options to consider when performing CTR surgery for appropriately indicated patients, including use of open (OCTR) or endoscopic (ECTR) techniques, choice of surgical setting, and anesthetic type. Each of these decisions may have cost implications. OCTR and ECTR techniques have been described as both safe and effective with equivalent results in the short-term,4–7 although ECTR may be costlier.8,9 With regard to anesthetic type, performing CTR under local anesthetic without sedation has been shown to be effective,10–14 while other anesthetic methods including Bier block, monitored anesthesia care (MAC), or general anesthesia are also well-established options.
Performing CTR under local anesthetic in a procedure room may provide an opportunity to reduce costs by eliminating the need for an anesthesia team, by reducing need for routine preoperative medical testing,15 and allowing for “Wide-awake local anesthesia no tourniquet” (WALANT) surgery in ambulatory- or clinic-based procedure rooms. WALANT has been utilized successfully for CTR,16–18 yielding significant cost-reductions in the context of the United States Military Health Care System16 and in Canada.18 It remains unclear whether these results are generalizable to the majority of the United States population covered by commercial and non-military government payers.
A study utilizing 2007 cost and payment data demonstrated cost-savings for CTR performed in a PR, as compared to the hospital-based OR, at a United States tertiary care center.19 Although these data are promising, use of a hospital-based OR as the comparison group rather than an ambulatory surgical center (ASC) is a limitation, because performing CTR in the ASC setting has been shown to be less costly than a hospital-based OR for CTR.3 Therefore, generalizing the observed PR cost-savings to practices predominantly utilizing an ASC may overestimate potential savings. A recent study utilizing payment data from United Health Group insurance records concluded that OCTR performed under local anesthetic was less costly than other methods of CTR.9 However, surgical setting (OR versus PR) was not included as a study variable.9
Although superior short-term outcomes and greater rates of nerve injury have been demonstrated with ECTR than OCTR, mid- to long-term results are similar between these two surgical methods.4–7 Additionally, surgical setting and anesthetic type have cost implications without proven impact on overall patient outcomes in the current literature. Therefore, costs should be considered in the surgical treatment of CTS. Our institution has developed a “Value Driven Outcomes” (VDO) database containing detailed patient- and item-level total direct cost and payment data for a variety of health care services. This has successfully identified areas of high variability in cost, leading to improved value of care delivered.1 In the current study, the VDO tool was utilized to test our null hypothesis that choice of CTR technique, surgical setting, and anesthetic type do not affect total direct costs or total combined payments.
Methods
This IRB-approved retrospective cost analysis study included all adult (≥ 18 years of age) patients undergoing isolated unilateral carpal tunnel release between July 2014 and October 2016 by fellowship-trained hand surgeons at a single tertiary academic institution. Patients were identified by CPT code (64721 and 29848), and corresponding basic demographic and surgical data were tabulated. Manual chart review of all operative, anesthesia, and clinic notes was performed to confirm the surgery type, surgical setting, and anesthesia type. Patients undergoing additional simultaneous procedures including other surgeries, injections, or bilateral CTR, were excluded. Also excluded were patients undergoing revision CTR, ECTR converted to OCTR, or those undergoing surgery prior to July 2014 (corresponding with initiation of WALANT hand surgery at our institution).
Total direct cost and payment data were collected from the Value Driven Outcomes (VDO) database for each individual surgical encounter. The VDO information technology tool draws prospectively-collected payment data and patient- and item-level total direct cost data from our institution’s data warehouse for specific patient encounters. VDO costing methods have been previously described, yielding total direct costs for materials used for patient care, facility utilization direct costs (including sterile processing costs), and time-based cost allocations including procedure/operative time and cost of staff involved in care (nursing, surgical technicians, medical assistants).1 Total direct cost categories, as tabulated by the VDO tool, are further described in Appendix I.
Using the VDO tool, total combined payments were calculated as the sum of hospital payment, surgeon payment, and anesthesia payment. All reported cost or payment data were normalized using each individual’s cost divided by the average cost in the data set, to comply with institutional guidelines prohibiting the public reporting of any financial data related to the details of non-publically disclosed contractual agreements. At our institution, both the OR and procedure room are located within an orthopaedic ambulatory surgery center, and the procedure room is considered a “site of service 22” (a procedure room within a hospital). Both the procedure room and OR incur a facility cost (OR costs are 8.4-fold greater than the procedure room per minute of use for CTR surgeries).
Each unique combination of surgery technique (OCTR, ECTR), operation location (OR, PR), and anesthesia type (local, MAC, Bier block, general) was defined as a distinct group. Continuous variables were summarized as mean ± standard deviation (SD), and categorical variables were summarized as count and percentage (%). Relative costs (or payments) were calculated relative to the lowest group by dividing each distinct group average by the lowest group mean. Total direct costs and total combined payments were compared between groups using Kruskal-Wallis tests, followed by Nemenyi post-hoc tests to adjust for multiple comparisons.20 Statistical significance was assessed at the 0.05 level and all tests were two-tailed.
We based our sample size calculations on a medium effect size of 0.35 in SD units. We expect a 1:1.5 ratio of procedure room versus OR cases for open CTR surgeries based on prior experience. With a two-sided, two-sample t-test, we required a total sample size of 270 (108 procedure room and 162 OR) to detect a medium effect size of 0.35 for cost between groups with 80% power at a 0.05 alpha level.
Results
After excluding 168 patients undergoing other simultaneous procedures (122 bilateral simultaneous CTR, and 46 patients with other additional procedures) and 34 patients treated by non-fellowship trained surgeons, 479 patients remained for analysis. Mean age was 55.2 ± 16.2 years, and 68% were female. Payer mix is summarized in Table 1. Nearly half of patients were covered by commercial insurance and half covered by non-military government insurance. All but three patients were treated in the procedure room or ambulatory surgery center. The three patients treated at a main hospital operating room setting declined treatment in the procedure room and had medical comorbidities that precluded treatment in the ambulatory surgery center setting: two had cardiac comorbidities, and one had diabetes, morbid obesity and obstructive sleep apnea. Due to insufficient sample size representation of the main hospital OR, these three patients were excluded. The breakdown of CTR surgeries performed by surgical method, surgical setting, and anesthesia type is illustrated in Table 2 with associated sample sizes - a total of 8 unique groups were identified.
Table 1.
Summary of payer mix.
| Insurance Type | Percentage (%) |
|---|---|
| Commercial | 45.1 |
| Medicare | 37.0 |
| Medicaid | 12.7 |
| Other | 2.9 |
| Workers Compensation | 2.1 |
| Self Pay | 0.6 |
Table 2.
Summary of unique study groups based upon surgical method, surgical setting, and anesthesia type.
| Sample Size (n) | Surgical Method | Surgical Setting | Anesthesia Type |
|---|---|---|---|
| 135 | Open CTR | Procedure Room (WALANT) | Local Only |
| 122 | Open CTR | Operating Room | MAC |
| 100 | Endoscopic CTR | Operating Room | MAC |
| 57 | Endoscopic CTR | Operating Room | Bier Block and MAC |
| 42 | Open CTR | Operating Room | Bier Block and MAC |
| 14 | Open CTR | Operating Room | General |
| 5 | Open CTR | Operating Room | Local Only |
| 4 | Endoscopic CTR | Operating Room | General |
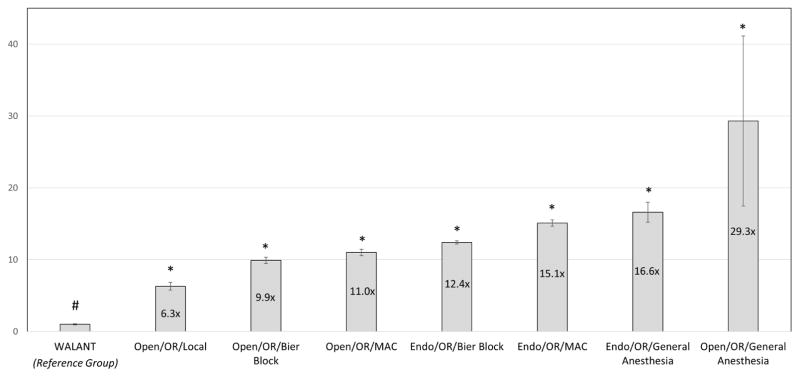
Total direct costs differed significantly between each CTR release group (p < 0.05; Figure 1). CTR performed under WALANT (OCTR in the PR under local anesthesia) was associated with the lowest total direct costs (relative cost of 1.0). Performing OCTR in the OR under local anesthesia was associated with 6.3-fold higher total direct costs than an OCTR using WALANT in a procedure room setting, and using MAC anesthesia for OCTR in the OR was 11.0-fold higher. Depending on the chosen anesthesia type, performing ECTR in the OR was associated with 12.4 – 16.6-fold greater total direct costs than WALANT.
Figure 1.
Data represent mean ± standard error of the mean (SEM). # Reference group, normalized to 1.0. *p<0.05 as compared to left-sided neighboring value per Kruskal-Wallis tests and Nemenyi post-hoc multiple comparison tests. Values over graph bars represent fold-change differences relative to the reference group (WALANT).
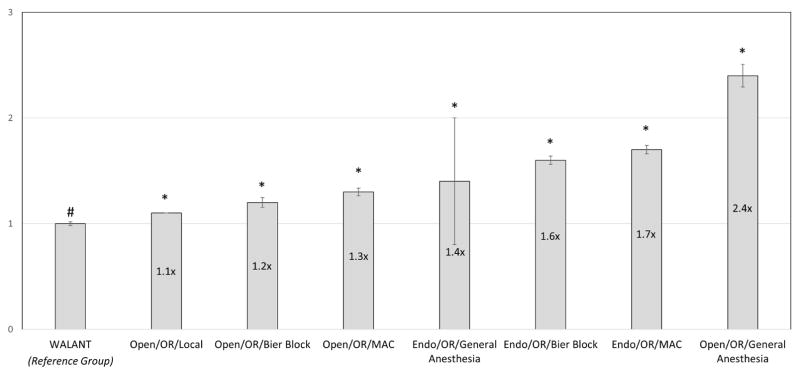
Total combined payments differed significantly between each CTR release group (p < 0.05; Figure 2). WALANT was associated with the lowest total combined payment (relative payment of 1.0). Performing OCTR in the OR was associated with 1.1 – 2.4-fold greater total combined payments, depending on anesthesia type, as compared to WALANT. ECTR was associated with 1.4 – 1.7-fold greater total combined payments, depending on anesthesia type, as compared to WALANT.
Figure 2.
Data represent mean ± standard error of the mean (SEM). # Reference group, normalized to 1.0. *p<0.05 as compared to left-sided neighboring value per Kruskal-Wallis tests and Nemenyi post-hoc multiple comparison tests. Values over graph bars represent fold-change differences relative to the reference group (WALANT).
Discussion
The main finding of this study is that performing open CTR using local anesthetic only in a procedure room setting was the least costly CTR method at our institution. We observed differing total direct costs and total combined payments between each of 8 carpal tunnel release groups, and therefore reject our null hypothesis that choice of CTR technique (OCTR versus ECTR), surgical setting (OR versus PR), and anesthetic type (local, MAC, Bier block, general) do not affect costs or payments.
Surgical setting contributed significantly to surgical costs independent of anesthesia type or surgical method, as performing OCTR under local in the PR versus the OR significantly affected both total direct costs and total combined payments (6.3- and 1.1-fold greater in the OR, respectively). Similarly, we conclude that anesthesia type independently influences CTR surgery costs. Total direct costs differed significantly based upon anesthesia type for OCTR performed in the OR (MAC, Bier block, and local were 62.6%, 66.4%, and 78.5% lower than general), and for ECTR performed in the OR (MAC and Bier block were 8.8% and 25.3% lower than general). Total combined payments also differed significantly based upon anesthesia type when controlling for surgical method.
Our findings regarding the cost-saving potential of WALANT and the impact of surgical setting on cost are congruent with previous literature. Chatterjee et al. demonstrated cost-savings for CTR performed in a procedure room, as compared to the hospital-based OR.19 Limitations of that study include possible overestimation of savings through use of a hospital-based OR as the comparison group rather than an ambulatory surgical center, the latter of which incur lower costs for CTR surgery. Rhee et al. observed significant cost-savings related to performing small hand surgery procedures under WALANT, 34% of which were CTR.16 The authors projected nearly $400,000 in savings to the Military Health Care System by performing 100 surgeries in a clinic-based procedure room rather than the OR. A study by LeBlanc et al. considered differences in material and personnel costs between OR and clinic-based carpal tunnel release surgery and arrived at a similar conclusion in Canada.18 Limitations include questionable generalizability to the non-military population in the United States.
Although procedure room surgery was not studied specifically, Foster et al. concluded that OCTR performed under local was the least costly method of those studied.9 ECTR cost $794 more than OCTR, and general/regional anesthesia was $654 more expensive than local – subjectively these results parallel our findings. Limitations include use of United Health Group insurance records, which do not quantify direct costs, do not allow differentiation between general and regional anesthesia, or identify revision surgeries or bilateral simultaneous CTR patients for exclusion. Failure to exclude revision open CTR may bias the results by underestimating actual cost discrepancies between OCTR and ECTR. An additional critical limitation was the inability to differentiate costs based on operative setting (procedure room versus operating room). Generalizability of the results may be affected by the homogeneous payer mix, as no Medicare or Medicaid patients were included in that database.
In addition, we conclude that ECTR led to significantly greater total direct costs and total combined payments than OCTR when performed in the OR under Bier block (20.5% and 23.8% greater, respectively) or in the OR under MAC (33.5% and 23.1%, respectively). These results are also consistent with previous literature. Zhang et al. used payer fees to define cost, and concluded that ECTR was associated with greater fees than OCTR when considering facility fees, surgeon fees, and occupational therapy fees ($2602 versus $1751, respectively).8 However, specific anesthesia fees and total direct cost data were not evaluated, and the authors were limited in precisely identifying the sources of cost differences.8 Thoma et al. performed a cost-effectiveness analysis to compare OCTR to ECTR using direct cost data at a Canadian academic institution, and concluded that ECTR was not cost-effective based upon their calculated incremental cost-utility ratio of $124,311 per quality-adjusted life years.21
Limitations of the current study deserve mention. Initial identification of patients by procedure code and the retrospective study design introduce potential for selection bias. Generalizability of our results may be limited by our observed payer mix, or unique pricing agreements between our institution and suppliers, which may affect payments and total direct costs, respectively. Given that we identified only three patients undergoing CTR in a main hospital operating room setting, we could not analyze cost or payment differences based upon this variable. Nonetheless, it has been previously established that CTR surgery is more expensive when performed in the hospital-based setting as compared to an ambulatory surgery setting.3 We believe that excluding this costlier surgical setting does not curtail the goal of the current investigation, which is to highlight opportunities for cost-savings for CTR surgery. We are unable to comment on costs associated with CTR treatment strategies beyond those performed at our institution, including endoscopic release under WALANT. Prior studies have described cost-savings of bilateral simultaneous carpal tunnel release, as compared to staged unilateral releases, for those with bilateral disease.21,22 However, our study did not evaluate the potential additional cost-savings of performing bilateral simultaneous releases in the procedure room setting. Since we did not evaluate costs or payments related to preoperative or postoperative care following carpal tunnel release, our results are not intended to reflect cost savings beyond the surgical encounter itself. We speculate that it is possible that evaluating costs for the treatment process in its entirety may uncover even greater cost savings afforded by WALANT, through minimization of the need for preoperative medical evaluation.15 We did not evaluate the opportunity cost associated with procedure room utilization, which may afford the ability to perform more CTR surgeries per unit time through increased efficiency.19 The VDO database does not include indirect cost data such as housekeeping, electricity, or property rent/depreciation. Although the relative dollar amounts reported in this manuscript allow for comparison of costs and payments between groups, an additional limitation is that our institution does not allow raw cost or payment data to be presented. Despite literature supporting similar clinical outcomes regardless of how the transverse carpal ligament is cut, and paucity of literature supporting differences in outcomes based upon anesthesia type or operative setting, it deserves emphasis that we did not perform a true cost-effectiveness analysis. Therefore, our results describe only cost differences rather than differences in value.
We think it is critical to recognize that although we did not observe any nerve or vascular transections in our series, this study was not designed nor adequately powered to make any conclusions or comments on the relative safety of carpal tunnel release performed in various settings or with differing anesthetic choices, including WALANT in a procedure room. We did not observe any catastrophic complications such as nerve transections in our series, which precludes a number-needed-to-treat (NNT) analysis to determine whether CTR method, surgical setting, or anesthetic type contribute to such complications. Although not demonstrated in the current literature, we recognize the possibility that use of sedation or general anesthesia may reduce the risk of nerve transections by keeping the patient relaxed and reducing the chance that they unexpectedly withdraw the operative limb. The increased direct and indirect costs to both patient and society resulting from iatrogenic neurovascular injury during carpal tunnel surgery are likely extraordinary. A single median nerve transection may lead to costly additional operations to address the injury (nerve repair or grafting) or its sequelae (opponensplasty tendon transfer, sensory nerve transfer), additional costs attributable to provider visits and nerve conduction studies, loss of productivity from time off of work or decreased efficiency from the resulting functional disability, and intangible costs of patient morbidity. Potential risks of nerve transection must be considered when choosing a surgical method, anesthesia method, and procedure setting for CTR.
Despite the cost-reducing potential of a procedure room for carpal tunnel surgery, barriers to implementation do exist. Regulatory and compliance issues may make it difficult to establish a procedure room in a surgery center or office setting. The need for sterile processing and limited space in the office may pose as logistical barriers. For surgeons who currently derive compensation through facility fees of a surgical center or other operational setting, changing the paradigm for CTR by transitioning into the procedure room setting may have implications for surgeon reimbursement, as profit-sharing groups may be incentivized to perform CTR in the OR which is associated with greater facility fees than the procedure room. Surgeon concern regarding costs of supplies and personnel for office-based procedure room cases may also pose as a barrier, although the Place of Service Code 11 for Professional Claims modifier may offset some of these expenses.22 Additional potential barriers include concerns that cost-savings may not be realized at the patient level, patient refusal of treatment in a procedure room, or surgeon concerns for safety in the procedure room setting. We also acknowledge that surgeon preference and training background influence choices in how to perform CTR, and we are not advocating that the least costly way is the best or only way to perform CTR. Lastly, we acknowledge potential safety concerns arising from lack of anesthesia monitoring or preoperative medical workup for these surgical patients, and further investigation is warranted to determine the safety effects of this practice particularly for high-risk patients with extensive comorbidities such as newly placed coronary stent or other major active medical problems.
In conclusion, this study demonstrates substantial cost-savings for carpal tunnel release surgery performed under WALANT (open carpal tunnel release under local anesthesia, in the procedure room setting) for a United States non-military population. Compared to WALANT, other variations of CTR are associated with 6.3 – 29.3-fold and 1.1 – 2.4-fold greater total direct costs and total combined payments, respectively, depending on the chosen surgical technique, surgical setting, and anesthesia type.
Supplementary Material
Acknowledgments
This investigation was supported by the University of Utah Study Design and Biostatistics Center, with funding in part from the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant 5UL1TR001067-02 (formerly 8UL1TR000105 and UL1RR025764).
Appendix I. Breakdown of Value-Driven Outcomes database categories for total direct costs
IMAGING COST: All imaging, scans and radiology services used.
SUPPLY COST: All supplies and devices used, excluding implants.
IMPLANT COST: All supply costs who are grouped as an Other Implant Supply
PHARMACY COST: Total cost of all medication used during the patients stay.
LAB COST: All lab work associated with visit, including blood work, urinalysis, hematology and all other lab or chemistry related costs.
OTHER SERVICES COST: Services that don’t fall into one of the other categories. Services include Physical Therapy, Occupational Therapy, Speech Pathology, Respiratory Service, EKG, Recovery Room nursing/staff, and Other Therapeutic Services.
FACILITY UTILIZATION COST: Time and labor costs for patients stay in each unit (excluding Professional costing). Cost is mapped to the individual patient level based on time spent on specific unit (surgery minutes, patient hours) or by completed visit.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lee VS, Kawamoto K, Hess R, et al. Implementation of a value-driven outcomes program to identify high variability in clinical costs and outcomes and association with reduced cost and improved quality. JAMA. 2016;316:1061–1072. doi: 10.1001/jama.2016.12226. [DOI] [PubMed] [Google Scholar]
- 2.Kawamoto K, Martin CJ, Williams K, et al. Value driven outcomes (vdo): A pragmatic, modular, and extensible software framework for understanding and improving health care costs and outcomes. J Am Med Inform Assoc. 2015;22:223–235. doi: 10.1136/amiajnl-2013-002511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nguyen C, Milstein A, Hernandez-Boussard T, Curtin CM. The effect of moving carpal tunnel releases out of hospitals on reducing united states health care charges. J Hand Surg Am. 2015;40:1657–1662. doi: 10.1016/j.jhsa.2015.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sayegh ET, Strauch RJ. Open versus endoscopic carpal tunnel release: A meta-analysis of randomized controlled trials. Clin Orthop Relat Res. 2015;473:1120–1132. doi: 10.1007/s11999-014-3835-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Trumble TE, Diao E, Abrams RA, Gilbert-Anderson MM. Single-portal endoscopic carpal tunnel release compared with open release : A prospective, randomized trial. J Bone Joint Surg Am. 2002;84-A:1107–1115. doi: 10.2106/00004623-200207000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Kang HJ, Koh IH, Lee TJ, Choi YR. Endoscopic carpal tunnel release is preferred over mini-open despite similar outcome: A randomized trial. Clin Orthop Relat Res. 2013;471:1548–1554. doi: 10.1007/s11999-012-2666-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thoma A, Veltri K, Haines T, Duku E. A meta-analysis of randomized controlled trials comparing endoscopic and open carpal tunnel decompression. Plast Reconstr Surg. 2004;114:1137–1146. doi: 10.1097/01.prs.0000135850.37523.d0. [DOI] [PubMed] [Google Scholar]
- 8.Zhang S, Vora M, Harris AH, Baker L, Curtin C, Kamal RN. Cost-minimization analysis of open and endoscopic carpal tunnel release. J Bone Joint Surg Am. 2016;98:1970–1977. doi: 10.2106/JBJS.16.00121. [DOI] [PubMed] [Google Scholar]
- 9.Foster BD, Sivasundaram L, Heckmann N, et al. Surgical approach and anesthetic modality for carpal tunnel release: A nationwide database study with health care cost implications. Hand (N Y) 2017;12:162–167. doi: 10.1177/1558944716643276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lichtman DM, Florio RL, Mack GR. Carpal tunnel release under local anesthesia: Evaluation of the outpatient procedure. J Hand Surg Am. 1979;4:544–546. doi: 10.1016/s0363-5023(79)80007-6. [DOI] [PubMed] [Google Scholar]
- 11.Rozanski M, Neuhaus V, Reddy R, Jupiter JB, Rathmell JP, Ring DC. An open-label comparison of local anesthesia with or without sedation for minor hand surgery. Hand (N Y) 2014;9:399–405. doi: 10.1007/s11552-014-9670-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lalonde D, Martin A. Epinephrine in local anesthesia in finger and hand surgery: The case for wide-awake anesthesia. J Am Acad Orthop Surg. 2013;21:443–447. doi: 10.5435/JAAOS-21-08-443. [DOI] [PubMed] [Google Scholar]
- 13.Lalonde D, Martin A. Tumescent local anesthesia for hand surgery: Improved results, cost effectiveness, and wide-awake patient satisfaction. Arch Plast Surg. 2014;41:312–316. doi: 10.5999/aps.2014.41.4.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lalonde DH, Wong A. Dosage of local anesthesia in wide awake hand surgery. J Hand Surg Am. 2013;38:2025–2028. doi: 10.1016/j.jhsa.2013.07.017. [DOI] [PubMed] [Google Scholar]
- 15.Davison PG, Cobb T, Lalonde DH. The patient’s perspective on carpal tunnel surgery related to the type of anesthesia: A prospective cohort study. Hand (N Y) 2013;8:47–53. doi: 10.1007/s11552-012-9474-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rhee PC, Fischer MM, Rhee LS, McMillan H, Johnson AE. Cost savings and patient experiences of a clinic-based, wide-awake hand surgery program at a military medical center: A critical analysis of the first 100 procedures. J Hand Surg Am. 2017;42:e139–e147. doi: 10.1016/j.jhsa.2016.11.019. [DOI] [PubMed] [Google Scholar]
- 17.Leblanc MR, Lalonde DH, Thoma A, et al. Is main operating room sterility really necessary in carpal tunnel surgery? A multicenter prospective study of minor procedure room field sterility surgery. Hand (N Y) 2011;6:60–63. doi: 10.1007/s11552-010-9301-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leblanc MR, Lalonde J, Lalonde DH. A detailed cost and efficiency analysis of performing carpal tunnel surgery in the main operating room versus the ambulatory setting in canada. Hand (N Y) 2007;2:173–178. doi: 10.1007/s11552-007-9043-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chatterjee A, McCarthy JE, Montagne SA, Leong K, Kerrigan CL. A cost, profit, and efficiency analysis of performing carpal tunnel surgery in the operating room versus the clinic setting in the united states. Ann Plast Surg. 2011;66:245–248. doi: 10.1097/SAP.0b013e3181db7784. [DOI] [PubMed] [Google Scholar]
- 20.Pohlert T. The pairwise multiple comparison of mean ranks package (pmcmr) 2014 [cited 2017 07/01/2017]; Available from: http://CRAN.R-project.org/package=PMCMR.
- 21.Thoma A, Wong VH, Sprague S, Duku E. A cost-utility analysis of open and endoscopic carpal tunnel release. Can J Plast Surg. 2006;14:15–20. doi: 10.1177/229255030601400101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cpt 2017 professional edition. Chicago, IL USA: American Medical Association; 2016. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.