Abstract
Background
Patients with uncontrolled type 1 diabetes mellitus (T1DM) are at a high risk for Ramadan fasting and are exempt from fasting; however, most still insist on fasting. The aim of this study was to examine glucose level fluctuations in those patients during Ramadan fasting using a real-time continuous glucose monitoring system (RT-CGMS).
Methods
This pilot study involved adult patients with uncontrolled T1DM (HbA1c > 7%) who insisted on fasting during Ramadan in 2014 from Maternity and Children’s Hospital, Medina, Saudi Arabia. A Medtronic RT-CGMS was used to monitor the participants’ glucose levels for 3 consecutive days during fasting.
Results
The study included 22 patients (mean age 22 ± 6 years, duration of diabetes 10.9 ± 7.2 years, HbA1c level 9.3 ± 1.2). All participants were using the basal-bolus insulin regimen, except for one patient who was on an insulin pump. Sensor glucose (SG) profiles typically followed a pattern that was characterized by an exaggerated increase after iftar, which was sustained overnight, and a second rapid rise after suhoor, with a prolonged glucose decay over the daylight hours. The average SG was 199 ± 104.1 mg/dl, which was lower during fasting 188.4 ± 103.41 mg/dl than during the eating hours 212.5 ± 103.51 mg/dl (P = 0.00). There was a higher rate of hyperglycemia (48%) than hypoglycemia (10%).
Conclusions
Patients with uncontrolled T1DM who fasted during Ramadan experienced a wide fluctuation of glucose levels between fasting and eating hours, exhibiting a greater tendency toward hyperglycemia. The long-term effects for this finding are not known and warrant further investigation.
Abbreviations: T1DM, type 1 diabetes mellitus; RT-CGMS, real time continuous glucose monitoring system; SMBG, self-glucose monitoring; SD, standard deviation; SG, sensor glucose
Keywords: Real time continuous glucose monitoring system, T1DM, Ramadan fasting, Hyperglycemia
1. Introduction
Millions of Muslims all over the world fast during the month of Ramadan. This month is a time when Muslims fast from dawn till sunset each day. Ramadan is the ninth month of the Islamic lunar calendar, based on the cycles of the moon. The duration of the fasting varies according to the season of year and geographical location. The typical mean fasting duration is 12–14 h, whereas in some regions it can extend to 18–20 h (Adawi et al., 2017). All adults Muslims are required to fast the whole month of Ramadan with few exceptions such as acutely ill people and those with serious chronic medical conditions.
Ramadan fasting consists of fasting alternating with feasting (re-feeding) periods with a major shift in meal times and prolongation of time between meals. This leads to disruption of the normal glucose homeostasis which carries the risk for hypoglycaemia, hyperglycaemia, diabetic ketoacidosis (DKA), and dehydration during the month of Ramadan among patients with diabetes (Ahmed et al., 2017).
Type 1 diabetes mellitus (T1DM) patients, particularly those with uncontrolled disease, are listed as a high-risk group for Ramadan fasting and are exempt from fasting by Islamic rules and medical recommendations (Hassanein et al., 2017), however, majority of them insist on fasting. The Epidemiology of Diabetes and Ramadan (EPIDIAR) study found that 42.8% of patients with T1DM fasted for at least 15 days during Ramadan (Salti et al., 2004). Interestingly, the safety of Ramadan fasting in patients with diabetes was described by many studies when correct guidance was used (Alabbood et al., 2017, AlAlwan and Banyan, 2010).
To avoid the risk of hypoglycemia and/or hyperglycemia, patients with T1DM need to monitor their glucose frequently during fasting (Hassanein et al., 2017). Multiple-point capillary glucose measurement by a glucometer, the traditional method for glucose monitoring, gives only snapshots for glucose levels during the day and do not reflect the real fluctuation of glucose levels during fasting. A continuous glucose monitoring (CGM) provides an incessant record for glucose during the day and, hence, detects glucose levels variability between fasting and eating. Data on glucose levels fluctuation during Ramadan fasting in patients with T1DM using CGM among are scanty (Kaplan and Afandi, 2015, Lessan et al., 2015). The present study intended to examine glucose level fluctuations during Ramadan fasting in patients with uncontrolled T1DM using a real-time continuous glucose monitoring system (RT-CGMS).
2. Methods
An invitation to participate in the study was sent to a WhatsApp group of patients with T1DM who were fasting during the month of Ramadan in 2014 in Medina City, Saudi Arabia. Thirty patients agreed to participate. Patients were excluded if they had controlled T1DM (HbA1c ≤ 7%), type 2 diabetes, pregnant women, and unwilling to perform self-glucose monitoring (SMBG). Twenty-four patients met the inclusion criteria and were included. All patients provided signed consent after receiving a detailed description of the study. The ethical committee of the Maternity and Children’s Hospital, Medina, Saudi Arabia approved the study.
Demographic data were obtained from the participants, including age, duration of diabetes and insulin regimen pre-Ramadan and if any modifications were made during Ramadan. The insulin dose adjustments during Ramadan were left to each participant’s health care provider (HCP). Weight and height were measured, and blood samples were collected for the HbA1c measurements.
Real-time CGMS was applied for all participants for 3 consecutive days during Ramadan fasting. Patients came to the clinic after fasting for at least 4 h for CGMS insertion. The glucose sensor was inserted into the abdominal subcutaneous tissue by a single skilled nurse. All participants were supplied with a glucometer to perform SMBG four to six times per day: upon waking, pre-iftar, 2-h after iftar, pre-suhoor, 2-h after suhoor, and when they felt the symptoms of hypoglycemia or hyperglycemia at any time. For CGMS calibration, the patients were instructed to enter at least two glucose values directly into the system. In addition, the participants were required to record in a logbook the contents and time of meals and insulin injections, and to report if they broke their fasting for any reason, or if they visited the emergency room for diabetic ketoacidosis or severe hypoglycemia during the study period. The participants were given the contact information of the support team in case of any medical or technical problems. At the end of the monitoring period, the results were downloaded from CGMS and a glucose profile was generated for each patient. The average sensor glucose (SG) and the standard deviation (SD) were recorded from the CGMS report. The average SG levels during fasting hours and eating hours were compared. The total fasting time during the year of 2014 in Madina city was 15 h per day (from 4 am until 7 pm).
The hyperglycemia and hypoglycemia rates were calculated. Hypoglycemia was defined as a glucose level ≤70 mg/dl, and hyperglycemia was defined as glucose level ≥180 mg/dl, (American Diabetes Association, 2018) and significant hyperglycemia was as a glucose level ≥300 mg/dl (Kaplan and Afandi, 2015).
2.1. Statistics
SPSS software (v 20.0, SPSS Inc, Chicago, IL, USA) was used to perform the statistical analyses. Normality tests was done using Shapiro–wilk test besides graphical assessment of normality and data was normally distributed, so we used mean and standard deviations for continuous data, and percentages were used for categorical variables. Student’s t-test was used to determine the significance of differences between two continuous variables, and the chi-squared test was used to assess for differences in the categorical variables. P < 0.05 was considered to be the cut-off value indicating significance.
3. Results
A total of 24 patients were enrolled, two participants were excluded because of sensor failure in one patient, and the electrodes fell off in the other patient. All participants were women, as the study was conducted at women hospital, with a mean age of 22 ± 6 years; the mean duration of diabetes was 10.9 ± 7.2 years, and the mean HbA1c value was 9.3 ± 1.2. Twenty-one participants were on a basal-bolus insulin regimen (glargine and rapid-acting insulin analogs), and a single participant was on an insulin pump.
During the study period, there were no episodes of diabetic ketoacidosis, severe hypoglycemia associated with seizure or coma, or any emergency room visits. However, four patients needed to break their fasts because of mild hypoglycemia; three patients broke their fasts for 1 day, and one patient broke the fast for the entire 3 days of the study.
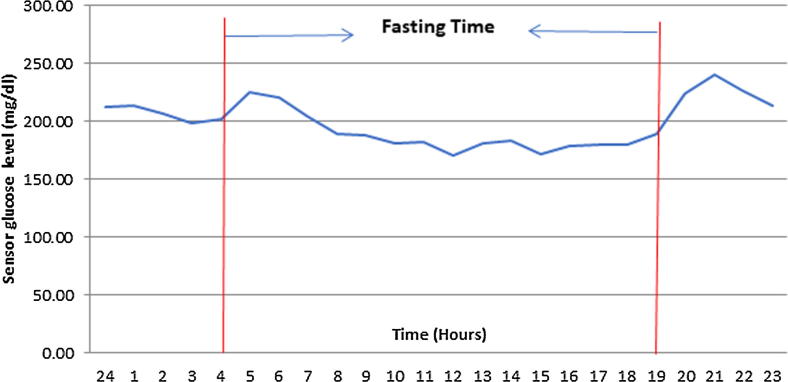
Sensor glucose profile typically followed a pattern that was characterized by a quick rise post iftar meal that sustained overnight and a second rapid rise after the suhoor meal, with prolonged glucose decay during daylight hours until it reached the nadir at 12 noon (i.e., after 8 h from fasting), Fig. 1. The average SG was 199 ± 104.1 mg/dl, which was lower during fasting (188.4 ± 103.41 mg/dl) than that during eating hours (212.5 ± 103.51 mg/dl, P 0.00). The average SG levels during different points of the day are presented in Table 1.
Fig. 1.
Mean 24-h sensor glucose levels during Ramadan fasting in 22 patients with uncontrolled T1DM.
Table 1.
Sensor glucose levels at different points of the day in 22 patients with uncontrolled T1DM during Ramadan fasting.
| Time | Sensor glucose level (mg/dl) Mean ± SD |
|---|---|
| During the whole day | 199 ± 104.1 |
| During Fasting hours | 188.4 ± 103.41 |
| During Eating hours | 212.5 ± 103.51 |
| During mid-fasting time | 170.54 ± 89 |
| At pre-iftar | 189.9 ± 97.1 |
| 2 h post-iftar | 240.2 ± 104.7 |
| 2 h after the beginning of fasting | 220.9 ± 110.7 |
In general, there was a higher rate of hyperglycemia than hypoglycemia (48% vs. 10%, respectively, Fig. 2). Hyperglycemia was observed in 53.3% of the time during eating hours and 44% during fasting hours (P 0.002), whereas hypoglycemia was observed in 13.4% of the time during fasting hours versus 5.9% during eating hours (P 0.000), (Fig. 3). There was no significant difference in the prevalence of significant hyperglycemia (SG > 300 mg/dl) between the eating hours and fasting hours (14.9% vs. 11.8%, respectively, P 0.135). The average time spent in hyperglycemia was 4.96 ± 4.8 h, whereas the average time of hypoglycemia was 0.60 ± 1.5 h. The average time of hyperglycemia post-suhoor (3.63 ± 4.3 h) was significantly longer than that post iftar (2.76 ± 2.5 h, P = 0.00).
Fig. 2.
Glycemic control during Ramadan fasting in 22 patients with uncontrolled T1DM.
Fig. 3.
Differences in the glycemic control between the fasting and eating hours during Ramadan fasting in 22 patients with uncontrolled T1DM. *P value <0.001, **P value <0.002.
4. Discussion
The key finding of the present study was the presence of wide fluctuation of glucose levels between the fasting and eating hours in patients with uncontrolled T1DM. In addition, there was higher rate of hyperglycemia than hypoglycemia. These results are similar to the findings of previous studies that assessed glucose level fluctuations during Ramadan fasting using CGM in patients with controlled diabetes (Kaplan and Afandi, 2015, Lessan et al., 2015).
Glucose levels typically increased immediately after iftar and were sustained overnight. Then, there was a second rapid rise in SG after the suhoor meal, with prolonged glucose decay over the daylight hours until it reached the nadir at the mid-fasting time. Later, glucose levels increased slightly before iftar, which could be attributed to an increase in the counter regulatory hormones and to decrease in the level of the administered insulin. This typical glucose profile during fasting was reported in the aforementioned studies that used CGM in patients with controlled T1DM (Kaplan and Afandi, 2015, Lessan et al., 2015). The best glucose profile observed in the current study with a minimal variability was in the single patient on an insulin pump, a finding that concurs with other studies that compared glucose profile between T1DM patients on insulin pumps vs. those on MDI (Alamoudi et al., 2017, Bin-Abbas, n.d.)
Although, it is generally assumed that there is a greater tendency for hypoglycemia in patients with diabetes during fasting, we found a higher rate of hyperglycemia than hypoglycemia, a finding that concurs with many previous studies (Kaplan and Afandi, 2015, Lessan et al., 2015, Alamoudi et al., 2017, Al-Agha et al., 2017). In a recent systematic review that investigated the effect of Ramadan fasting on glycemic control in patients with insulin dependence, postprandial hyperglycemia was the main concern (Alabbood et al., 2017). In the current study, the mean glucose level was 199 ± 104 mg/dl, and approximately half of the time, the patients were in the hyperglycemic range (SG ≥ 180 mg/dL), and in 13% of the time, they were experiencing significant hyperglycemia (SG ≥ 300 mg/dL). The factors contributing to the higher risk of hyperglycemia during Ramadan fasting included meals eaten during iftar, are often carbohydrate-heavy meals with fried food, which has high saturated fats, along with sweet drinks and desserts. In addition, patients may eat more at suhoor to avoid hypoglycemia during fasting. Moreover, as many guidelines and experts recommend reduction of the basal and the short acting insulin before suhoor (Hassanein et al., 2017), this action may further increases the risk of hyperglycemia during fasting hours in patients with uncontrolled diabetes. Physical activity levels usually fall during the daytime of Ramadan, which could be another reason for the increased hyperglycemia observed during fasting (Hassanein et al., 2017).
The hypoglycemia rate was low during fasting in this cohort of patients, and there were no reports of severe hypoglycemia associated with seizure or coma. Only four patients needed to break their fasts prematurely for mild hypoglycemia, which aligned with several studies in which the rate of severe hypoglycemia was negligible during Ramadan fasting (Alabbood et al., 2017, Alamoudi et al., 2017, Al-Agha et al., 2017). However, Lessan et al. reported short episodes of minor hypoglycemia that went unrecognized but were recorded by CGM in a significant number of patients with diabetes during Ramadan fasting (Lessan et al., 2015).
Despite the significant hyperglycemia encountered in the current study, there were no reports of diabetic ketoacidosis or major adverse events, and most patients were able to fast for most of the days during the study period. This finding is in agreement with previous reports that demonstrated the safety of Ramadan fasting in patients with diabetes, if correct guidance is used (Alabbood et al., 2017, AlAlwan and Banyan, 2010). In the Multi-country retrospective study of the management and outcomes of patients with Type 2 diabetes during Ramadan (CREED), majority of Muslim population were able to fast for the whole month of Ramadan (Babineaux et al., 2015). Nevertheless, the long-term consequences of fasting on patients with uncontrolled T1DM are not known and warrant further investigations.
Although International Diabetes Federation and the Diabetes and Ramadan International Alliance (IDF-DAR) guidelines advise patients to break their fasting if their blood glucose levels fall to 70 mg/dl or increase to 300 mg/dl (Hassanein et al., 2017), many patients in the current study did not follow these recommendations, which highlights the need for more intensive education before Ramadan.
Finally, it should be emphasized that, as fasting is a deeply spiritual practice to the Muslims; majority of Muslim patients with T1DM choose to fast even against medical advice. Those patients represent a challenge to the HCPs; hence, physicians are required to be familiar in dealing with them to provide the best care. They should counsel every patient individually, deliver intensive education, and advise on healthy nutrition and insulin dosing adjustments if needed. A trial of pre-Ramadan fasting may guide the HCP for proper management of diabetes during Ramadan. Questioning the patient’s insulin dose and whether any changes made during last Ramadan or if any complications were experienced could help HCPs determine an insulin-dosing adjustment for the current Ramadan period. In addition, patients should be encouraged to maintaining a logbook on glucose levels and their insulin regimen during Ramadan to guide the HCP to make the best insulin dosing adjustments for the next Ramadan. Contrary to IDF-DAR recommendations for patients with type 1 diabetes to reduce the doses of the basal insulin and the short acting insulin before suhoor (Hassanein et al., 2017), we feel this practice may not be appropriate for patients with uncontrolled diabetes. Insulin dosing adjustments should be individualized, and for those patients with uncontrolled diabetes and at low risk of hypoglycemia, keeping the same doses of the basal and short acting insulin before suhoor, while increasing the pre iftar short-acting insulin may be more appropriate. Patients should be encouraged to use CHO counting for insulin dose estimation before meals. In addition, they should be advised to follow a healthy balanced diet and to reduce their caloric intake during iftar and suhoor meals and to divide the total daily calories intake between suhoor and iftar, in addition to having 1–2 snacks to avoid marked hyperglycemia post meals (Hassanein et al., 2017). Iftar should begin with water and 1–2 dates to increase blood glucose levels followed by a meal that has fewer carbohydrate and less fried food, sugary drinks and desserts (Hassanein et al., 2017). Suhoor should be delayed, and it should consist of food with low glycemic index and high fiber, which helps to release energy slowly during fasting. An adequate amount of protein and fat at suhoor induces satiety better than carbohydrates, while not increasing blood glucose levels (Hassanein et al., 2017). Patients should be encouraged to check their blood glucose levels regularly many times during the day, as it allows them to better treat their blood glucose and prevent hypo- and/or hyper-glycaemia (Hassanein et al., 2017). As recommended by IDF-DAR, patients should be advised to break their fast if their glucose levels drop to <70 mg/dl or increase to 300 mg/dl (Hassanein et al., 2017).
The small sample size was the primary limitation of our study, and future studies with larger sample sizes are needed to confirm our findings. However, our study was a pilot study that examined the glucose profiles of patients with uncontrolled T1DM during Ramadan fasting using RT-CGMS. Previous studies have primarily examined patients with controlled disease and excluded high-risk group with poorly controlled diabetes. In addition, the current study provides some insights on insulin dose adjustments during Ramadan fasting for this high-risk group of patients.
5. Conclusions
Patients with uncontrolled T1DM who fast during Ramadan experience a wide fluctuation of glucose levels between fasting and eating hours, exhibiting a higher rate of hyperglycemia than hypoglycemia. Although there were no short-term major complications, the long-term effects of the marked hyperglycemia are not known and warrant further investigation.
The use of RT-CGMS by patients with diabetes during Ramadan provides a continuous record for glucose during fasting and non-fasting periods which enlightens them with the episodes of hypo and hyperglycemia and hence could improve patients’ safety during fasting. Randomized controlled trials are needed to confirm the value of using RT-CGMS during Ramadan fasting in patients with diabetes.
During Ramadan fasting, insulin dosing adjustment should be individualized for patients with uncontrolled T1DM, and well-designed randomized controlled trials are required to determine the best insulin dose adjustments for those patients.
Funding source
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest disclosure
None.
Acknowledgments
Acknowledgements
The author gratefully acknowledges Mrs. Khadijah AbuTalib for her contribution in this research by applying RT-CGMS to the participants.
Footnotes
Peer review under responsibility of King Saud University.
References
- Adawi M., Watad A., Brown S., Aazza K., Aazza H., Zouhir M., Sharif K., Ghanayem K., Farah R., Mahagna H., Fiordoro S., Sukkar S.G., Bragazzi N.L., Mahroum N. Ramadan fasting exerts immunomodulatory effects: insights from a systematic review. Front. Immunol. 2017;8:1144. doi: 10.3389/fimmu.2017.01144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed M., Husain N., Elmadhoun W., Noor S., Khalil A., Almobarak A. Diabetes and Ramadan: a concise and practical update. J. Fam. Med. Prim. Care. 2017;6:11. doi: 10.4103/2249-4863.214964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Agha A.E., Kafi S.E., Zain Aldeen A.M., Khadwardi R.H. Flash glucose monitoring system may benefit children and adolescents with type 1 diabetes during fasting at Ramadan. Saudi Med. J. 2017;38:366–371. doi: 10.15537/smj.2017.4.18750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alabbood M.H., Ho K.W., Simons M.R. The effect of Ramadan fasting on glycaemic control in insulin dependent diabetic patients: a literature review. Diabet. Metab. Syndr. Clin. Res. Rev. 2017;11:83–87. doi: 10.1016/j.dsx.2016.06.028. [DOI] [PubMed] [Google Scholar]
- AlAlwan I., Banyan A. Al. Effects of Ramadan fasting on children with Type 1 diabetes. Int. J. Diabet. Mellit. 2010;2:127–129. [Google Scholar]
- Alamoudi R., Alsubaiee M., Alqarni A., Saleh Y., Aljaser S., Salam A., Eledrisi M. Comparison of insulin pump therapy and multiple daily injections insulin regimen in patients with type 1 diabetes during Ramadan fasting. Diabetes Technol. Ther. 2017;19:349–354. doi: 10.1089/dia.2016.0418. [DOI] [PubMed] [Google Scholar]
- American Diabetes Association 6. Glycemic targets: standards of medical care in diabetes-2018. Diabet. Care. 2018;41:S55–S64. doi: 10.2337/dc18-S006. [DOI] [PubMed] [Google Scholar]
- Babineaux S.M., Toaima D., Boye K.S., Zagar A., Tahbaz A., Jabbar A., Hassanein M. Multi-country retrospective observational study of the management and outcomes of patients with Type 2 diabetes during Ramadan in 2010 (CREED) Diabet. Med. 2015;32:819–828. doi: 10.1111/dme.12685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bin-Abbas, B.S., n.d. Insulin pump therapy during Ramadan fasting in type 1 diabetic adolescents. Ann. Saudi Med. 28, 305–306. [DOI] [PMC free article] [PubMed]
- Hassanein M., Al-Arouj M., Hamdy O., Bebakar W.M.W., Jabbar A., Al-Madani A., Hanif W., Lessan N., Basit A., Tayeb K., Omar M., Abdallah K., Al Twaim A., Buyukbese M.A., El-Sayed A.A., Ben-Nakhi A. Diabetes and Ramadan: practical guidelines. Diabet. Res. Clin. Pract. 2017;126:303–316. doi: 10.1016/j.diabres.2017.03.003. [DOI] [PubMed] [Google Scholar]
- Kaplan W., Afandi B. Blood glucose fluctuation during ramadan fasting in adolescents with type 1 diabetes: findings of continuous glucose monitoring. Diabet. Care. 2015 doi: 10.2337/dc15-1108. [DOI] [PubMed] [Google Scholar]
- Lessan N., Hannoun Z., Hasan H., Barakat M.T. Glucose excursions and glycaemic control during Ramadan fasting in diabetic patients: Insights from continuous glucose monitoring (CGM) Diabet. Metab. 2015;41:28–36. doi: 10.1016/j.diabet.2014.11.004. [DOI] [PubMed] [Google Scholar]
- Salti I., Bénard E., Detournay B., Bianchi-Biscay M., Le Brigand C., Voinet C., Jabbar A., EPIDIAR study group A population-based study of diabetes and its characteristics during the fasting month of Ramadan in 13 countries: results of the epidemiology of diabetes and Ramadan 1422/2001 (EPIDIAR) study. Diabet. Care. 2004;27:2306–2311. doi: 10.2337/diacare.27.10.2306. [DOI] [PubMed] [Google Scholar]