Abstract
Head and neck squamous cell carcinoma (HNSCC) is responsible for a large number of deaths each year. Oral cancer is the most frequent subtype of HNSCC. Historically, oral cancer has been associated with an increase in the consumption of tobacco and alcohol products, seen especially in the Asian subcontinent. It has also been associated with infection by the human papilloma virus (HPV), particularly strain HPV16. Treatment usually involves a multidisciplinary approach of surgery combined with chemotherapy and radiation. The advent of immunotherapy has broadened the scope for treatment. A better immune response to the tumour can also elicit the action of other therapeutic approaches. A heightened immune response, on the other hand, can lead to resistant tumour formation through the process of immunoediting. Molecular profiling of the tumour microenvironment (TME) can provide us with better insight into the mechanism and progression of the disease, ultimately opening up new therapeutic options. High-throughput molecular profiling techniques over the past decade have enabled us to appreciate the heterogeneity of the TME. In this review, we will be describing the clinicopathological role of the immune and genomic landscape in oral cancer. This study will update readers on the several immunological and genetic factors that can play an important function as predictive and prognostic biomarkers in various forms of head and neck cancer, with a special emphasis on oral carcinoma.
Keywords: Oncology, Cancer research, Immunology, Genetics
1. Introduction
Immunotherapy in the field of oncobiology has been rapidly advancing over the past decade. The role of tumour-infiltrating lymphocytes (TILs) in the tumour microenvironment (TME) gives a predefined definition of cancer being an immunological disease apart from its genetic basis [1, 2, 3]. Tumours have the ability to organize an immunosuppressive microenvironment that is dependent on the reciprocal interactions between the tumour and its host. Generally, the released tumour antigens are processed and presented by antigen-presenting cells (APCs) to the effector T cells. The effector T cells, thus activated, can mount an antitumour response [4, 5]. Tumour cells develop resistance via induced T cell tolerance, leading to an immune escape condition due to alterations in immunity. This creates an immunosuppressive environment through complex signalling between tumours and their associated cells.
Head and neck squamous cell carcinoma (HNSCC) represents cancer of the squamous cells that line the moist, mucosal surfaces inside the head and neck. It includes the oral cavity, pharynx, larynx, salivary glands, paranasal sinuses and nasal cavity. HNSCC is the most aggressive malignant neoplasm arising in the mucosa of the upper aerodigestive tract [6]. Patients suffering from HNSCC have myriad alterations in their immune cell population. They demand a potential therapeutic approach to be highlighted for the proper recovery and lower recurring outcomes. HNSCC immunobiology is essentially linked to the immune system of the host. Immunological surveillance is a monitoring process of the immune system to detect and destroy invading pathogens and neoplastically transformed cells in the body. The escape of the tumour-associated antigens (TAA) from host immunity signifies a failure of immune surveillance to control tumour progression. Although molecular and cellular immunology has gained immense advances in the last few decades, the biotherapy of cancer, including antitumour vaccines, still needs a satisfactory outcome. The major reason for this drawback is that tumours in general, especially HNSCC, can evade and escape host immunity through multiple strategies. Tumours are also known to express immunoinhibitory molecules [7, 8, 9, 10] and, as a result, both the local and systemic immunity are suppressed. Finally, in advanced HNSCC death of the immune effector cells is profound [11]. The mechanisms for immune suppression are yet to be revealed and several large investigations are already in progress.
Alterations of the genome are among the main factors that have been implicated in the etiology of cancer. These alterations can be observed as the insertion, deletion or substitution of nucleotides or chromosomal abnormalities leading to the manifestation of a defective phenotype [12, 13, 14]. Therefore, genomic biomarkers can be very useful to predict changes in tumour biology in response to treatment and can be potential therapeutic targets. The presence of oncogenes and their expression at very high levels contribute to tumourigenesis. In the case of tumour suppressor genes, the scenario is exactly the opposite, and a loss of expression is generally associated with progression to cancer. The genes involved and their degree of change in expression varies according to different tumour types. Several techniques have been employed to pinpoint the genetic instabilities taking place inside a tumour cell, which can help to characterize different subsets of tumours. Approaches ranging from oncogene arrays to comparative genome hybridization (CGH), BAC end sequencing and quantitative microsatellite analysis have provided oncology researchers with useful experimental strategies for mapping the genomic markers involved in oncogenesis [15, 16]. Modern techniques such as RNA-seq technology have been successfully used to identify global gene expression patterns in tongue squamous cell carcinoma [17]. This RNA-seq study identified several genetic alterations that can explain the highly invasive behavioural pattern of tongue squamous cell carcinoma.
This review aims to identify the mechanisms involved in the immunosuppression of HNSCC biology and to demonstrate a few experimental and therapeutic approaches implemented to surmount the tumour associated immune dysfunction in HNSCC. Critical genetic signatures have also been described in detail, which are known to play an important role in the development of oral cancer. This would finally be supportive for the proper developmental immunotherapy approaches.
2. Main text
2.1. Immune markers/profile in HNSCC
In HNSCC, an increase in regulatory T cells (Tregs) and myeloid-derived suppressor cells (MDSCs), as well as a decrease in the absolute number of T cells and CD8+ effector T cell dysfunction, has already been reported [18, 19, 20]. This profiling of the immune cells can correlate to the treatment efficacy and prediction of prognosis. Activation of T cells requires two simultaneous signals from APCs. The ‘first signal’ is the direct interaction of the T cell receptor (TCR) on a T cell with the major histocompatibility complex (MHC) on APCs. The second is the ‘co-stimulatory signal’ that aids in the interaction of B7 on the APC surface to CD28 on the T cell [3]. A third signal made up of immune-activating cytokines such as IL-12 and type I (IFNα/β) or type II (IFNγ) interferon [21] must be involved in the context of the previous two signals.
Recently, researchers have been investigating the expression of tumour infiltrating lymphocytes (TILs), including T cells, B cells, macrophages and neutrophils in solid tumours [22, 23]. Tregs in general control the autoreactive lymphocytes, but they can also downregulate the immune system response to tumour-associated antigen (TAA). In many solid tumours these Tregs are found especially in the TILs as well as in peripheral circulation [24, 25, 26, 27]. Although, the reason for their accumulation is still not clear. The enrichment of Tregs in tumours could be induced by the conversion of FOXP3- T cells into FOXP3+ T cells in the presence of TGFβ1 and retinoic acid [28, 29]. Inversely, in tumour sites, the CD44hi memory Tregs specific for self-antigen are expanded and that protects the tumour against the immune response of the host [30]. Hence, the conclusion can be drawn that Treg activation and expansion takes place in the TME. In patients with HNSCC, severe immune disruption is found; hence, the antitumour response is impaired [31], but few effector immune cells are reported to have favourable outcome [32].
A strong correlation between the density and location of TILs may lead to better prognosis of cancer and can be implemented in quantitative pathology. The ‘immunoscore’ is one such method based upon a standardized algorithm, where CD3+ and CD8+ TILs are quantified in the tumour core (CT) and invasive margin (IM). This proved to be an established prognostic tool in colorectal cancer [33, 34].
2.2. Role of immune marker expression in tumour progression
Subsets of immune and non-immune cells interact with each other and are required for an efficient functioning of the immune system. Leukocyte migration and trafficking to their destined tissues or sites is specially regulated by chemokines. Chemokines are mostly produced during infection or inflammation, except for CCL19 and CCL21, which are constitutively produced and control cell movement during homeostasis [35]. All these interactions are important for protective immunity but peripheral tolerance and regulations by Tregs are also essential. On the basis of these discoveries, we will discuss the involvement of the most significant signature markers and their role in immune development.
2.2.1. CCR7
CC-chemokine receptor 7 (CCR7) is expressed by different immune cell subsets [36] and is mainly involved in the homing (through its ligands CCL19 andCCL21) of many T cell subpopulations and antigen presenting dendritic cells (DC) to the lymph node. CCR7 is an indispensable mediator for tranquil thymic T cell development and behaves as negative selection for self-reactive T cells. A seven-transmembrane-spanning domain protein that mediates its signal through heterotrimeric G proteins and is generally involved in the homing of the immune cells to their secondary lymphoid organs and positioning them to defined functional compartments. They are expressed by a number of cells such as semi-mature and mature DCs [37], thymocytes during defined stages of their development [38], naïve B and T cells [39, 40], Tregs [41] and a subpopulation of memory T cells known as central memory T (TCM) cells [40]. CCR7 is critical in its functional status at subcellular level and its expression on transformed and metastatic cells has been reported in different cancer types. CCR7 in combination with CD45RA+ (naive) and CD45RA− (memory) subtypes can be sorted into: CD45RA−CCR7+ (central memory), CD45RA−CCR7− (effector/memory), CD45RA+CCR7− (terminally differentiated). CD45RA−CCR7− effector memory subtypes are mostly increased in the invading TILs that could significantly influence their fate in comparison to conventional T cells, indicating immunosuppressive consequences in gastric cancers [42]. It has been reported that invasive breast cancer cells may undergo targeted migration towards lymphatics induced by tumour cell expression of CCR7 bound to its ligands called the lymphoid homing chemokines CCL19/CCL21. Hence, CCR7 play crucial role in lymphatic migration of tumour cells similarly to lymph nodes draining dendritic cell immigration. This can be also explained as a hijack of physiological chemokine driven leucocyte migration by CCR7 in lymphatic migration of tumor cells during metastasis. This highlights the significant role of tumour microenvironment during immune cell mediated inflammation in determining the repertoire of expression of chemokines on immune cell infiltrate and developing tumour [43]. Although these facts indicate an abundant chemokine expression within the tumour mass to retain immune cells, but expression on tumour-associated leucocytes in its microenvironment still needs a global informative panel designing research on immune subset analysis. In HNSCC, elevated CCR7 expression is found to correlate with lymph node metastasis and tumour tissue histological differentiation status [44]. Tongue squamous cell carcinoma tissues and different cell lines detected the expression of CCR7 when compared to normal oral mucosa with no CCR7 expression [45]. With many such similar reports, CCR7 may be conferred to play an important role in predicting metastasis and prognosis in HNSCC patients.
2.2.2. T cell
Naive T (TN) cells harbouring a given epitope specificity are released from the thymus as mature cells after following either a positive or a negative selection. TN cells proliferate and differentiate into effector cells after a cognate antigen (Ag) encounter. Most of them migrate to peripheral tissues and infected sites to facilitate their destruction [46]. After Ag clearance, effector cells die, and few develop into long-lived memory T cells.
The development of high-throughput technologies such as multiplexing and flow cytometry has paved a unique contribution to immunology. With the use of monoclonal antibodies and spectral immunohistochemistry, phenotypic identification and characterization of a heterogeneous population of cells could be quantified using conjugated fluorochromes. Although, identification of different subsets of lymphocytes and other cells under flow cytometry can be done with a designed panel of eight colour fluorochrome conjugated antibodies (Table 1), the simultaneous detection of upto seventeen different markers is possible [47]. TN, T central memory (TCM) and T effector memory (TEM) cells could be separated on the basis of expression of CD45, CD45 RA and CD45 RO, respectively [48]. At the single cell level both the phenotype and functional properties of T cells could also be recognized. For instance, CD27 (a member of the tumour necrosis factor receptor-TNF superfamily) and CCR7 both mediate homing and can be used in combination with CD45 RA to define the phenotypical subsets of CD8+ memory cells on the effector function basis. Antigen-specific T cell activation is mainly mediated by the human leukocyte antigen HLA-DR. Low HLA-DR expression significantly indicates impaired host defence [49, 50]. Among the cytolytic molecules, Granzyme (Gr) A and B and perforin are the most common. Gr B production depends on the production of Gr A. Henceforth, perforin-positive cells that are positive for both Gr A and B can be a good choice of marker for the assessment of cytological property.
Table 1.
Flow cytometry panel design with 8 colour fluorochromes for immune subset analysis includes lymphocyte (T & B), monocytes, macrophages and dendritic cells in resected tumour samples from HNSCC patients and matched peripheral blood samples.
| Cell Type | Tube | BV421 | V500/BV510 | FITC/BB 515 | PE/PE-CF594 | PerCp-Cy5.5 | PE-Cy7 | APC/Alexa647 | APC-H7 |
|---|---|---|---|---|---|---|---|---|---|
| T cell | T1 | CD45RA | CD3 | CD8 | CCR7 | CD4 | CD45RO | CD38 | HLA-DR |
| T2 | Perforin | CD3 | CD8 | Granzyme B | CD4 | CD16 + CD56 | CD103 | - | |
| T3 | GARP | CD3 | CD8 | LAP | CD4 | CD278 | - | ||
| T4 | TIM-3 | CD3 | CTLA4 | CD4 | PD-1 | PDL-1 | - | ||
| Treg | T1 | CD3 | CD25 | FoxP3 | CD4 | CD127 | - | ||
| B cell | T1 | CD24 | CD138 | CD27 | CD10 | CD19 | IgD | CD38 | CD20 |
| MDSC, Monocyte, DC | T1 | CD200 | CD3 | CD16 | CD1c | CD11c | CD14 | CD169 | HLA-DR |
| T2 | CD141 | - | CD15 | - | CD11c | - | CD123 | HLA-DR | |
| Macro-phage | T1 | CD40 | HLA-DR | CD206 | CD81 | - | CD33 | CD192 | CD11b |
| T2 | CD141 | CD86 | CD163 | CD80 | - | PD-1 | PDL-1 | CD11b |
2.2.3. Tregs
Suppressor Tregs that prevent autoimmunity contain a subpopulation of CD4+ T cells and have CD25, CTLA4, and CD39 marker expression [51, 52]. Tregs have multiple functions, including promoting cancer progression by causing anergy, apoptosis and cell cycle arrest of activated T cell with the production of IL-10, TGF-β and direct cell-cell contact. The inhibitory action of Tregs is also applied to DCs, natural killer (NK) and B cells [53, 54]. In HNSCC, an increased Treg population is found in the peripheral blood and T cell infiltrating tumour, suggesting an immune-suppressed status [55, 56, 57, 58]. Indoleamine 2, 3-dioxygenase (IDO) activity in antigen-presenting cells (APCs) can be induced by Tregs through CTLA-4 and CD80/CD86 interaction. Tryptophan is generally catabolized by IDO and its supply to immune cell is depleted, leading to an inhibition of effector T and NK cell functions [59, 60]. A recent study found a gene signature of 32 genes in Treg enriched tumours that are likely to be associated with favourable prognosis [61]. Two genes have been selected for special mention. The TRAF3IP1 gene expresses the TRAF3IP1 protein, which interacts with another protein, TRAF3, to inhibit the type I interferon response. As expected, lower expression of this gene has been associated with a favourable outcome. Another gene, LTB, coding for the lymphotoxin beta has been shown to be elevated in patients showing a better response to therapy. The role of lymphotoxin beta is to stimulate Tregs so that they migrate away to lymph nodes from the tissue. Although these data point toward the immunosuppressive role of Tregs within the tumour microenvironment, it requires further validation through in vivo studies.
On the other hand, it has been found that after treatment Treg frequency gets elevated in HNSCC patients, indicating a correlation between oncologic treatment and Treg elevation. In several solid tumours, the role of FOXP3+ is associated with favourable outcomes. Data from 278 patients' formalin-fixed paraffin-embedded (FFPE) samples suggest that elevated FOXP3+ cells are associated with favourable prognosis and positively correlated to superior loco regional control [62, 63]. Thus, it seems that the opinion on the clinical relevance of intratumoural Tregs can be polarized. The heterogeneous property of Tregs can be influenced by the tumour site, molecular subtype and tumour stage. Indeed, biomarkers are not reliable indicators of the functional capacity of Tregs, since Tregs found in TME and that circulating to the periphery may not be the same in their functional repertoire [64]. The origin and phenotypic characteristics of Tregs that infiltrates human tumours are yet to be unfolded. Enhancement of Tregs can be beneficial to some patient groups while being detrimental to others. Additional studies are required to better understand the myriad roles of Tregs in the TME [65, 66].
2.2.4. MDSCs
Myeloid-derived suppressor cells (MDSCs) are emerging as important markers of the myeloid cell lineage and play a major role in tumour-mediated immunosuppression [67]. In healthy individuals, immature myeloid cells in the bone marrow differentiate into mature granulocyte, macrophages or dendritic cells. However, in pathological conditions such as cancer, a block during differentiation leads to an accumulation of the population. At this stage, they lack the expression of markers for monocytes, macrophages and dendritic cells. Monocytes are one of the myeloid-derived cell types that have different expression of CD markers on their surface, especially CD14 and CD16, and can differentiate into both macrophages and dendritic cells. Both macrophages and dendritic cells play a crucial role in disease pathogenesis, including cancer [68, 69, 70, 71]. MDSCs can migrate to the tumour site, upregulating expression of arginase1 and iNOS (induced nitric oxide synthetase) but downregulating production of reactive oxygen intermediates (ROS), and/or can be rapidly differentiated to tumour associated macrophages (TAMS) [72, 73]. Cytokines are produced by the TAMS, which can induce T cell suppression non-specifically. Tumour-associated neutrophils (TANS), like TAMS, have distinct activation and differentiation states, and they develop a pro-tumourigenic phenotype largely driven by the presence of TGF-β [74]. The depletion of TANS reduces tumour growth and inhibits immunosuppression in the tumour microenvironment, thus leading to increased CD8+ cytotoxic T lymphocytes.
MDSCs are responsible for angiogenesis in HNSCC, and inhibition of the JAK/STAT pathway has been shown to reduce both MDSCs and angiogenesis [75]. Alterations of myelopoiesis-associated tumour growth leads to the recruitment of immunosuppressive MDSCs. Hence, MDSCs are induced by markers (TGFβ, VEGF and IL-6) associated with inflammation [76]. MDSCs isolated from some ovarian cancer patients have been found to exhibit hypermethylation [77]. Prostaglandin-E2 (PGE2)-induced upregulation of DNA methyltransferase 3A (DNMT3A) is responsible for the observed hypermethylation, which is also replicated in in vitro models. This MDSC-specific methylation is responsible for the downregulation of S1PR4, RUNX1, AQP9, LMO2 or FYN genes. Most of these genes encode factors to prevent the suppressive activity of MDSCs. Hence, characterization of myeloid gene hypermethylation mediated by DNMT3A under the induction of PGE2 can be implemented in their identification under different inflammatory perspectives. It can also be a useful target for therapeutic intervention.
2.2.5. Immune checkpoint molecules
Activated immune cells express some inhibitory checkpoint receptors (ICRs) on their surface. The receptors may be cytotoxic T lymphocyte-associated antigen 4(CTLA-4), programmed cell death-1(PD-1), T-cell immunoglobulin and mucin protein-3 (TIM-3) and lymphocyte activation gene-3 (LAG-3) that play an important role in the TME [3, 78]. Activated CD8+ T cells, NK cells, B cells, monocytes, and DCs express PD-1, a cell surface protein that, when bound by its ligand PD-L1, provides an inhibitory signal. The upregulation of PD-1 may even cause T cell exhaustion and tolerance [79]. Exhausted T cells can also be marked with another inhibitory receptor such as TIM-3, which is selectively expressed on activated interferon gamma (IFN-γ) produced by CD4+ and CD8+ T cells. Autologous TIL and peripheral blood samples may be compared for intratumoural and circulating immune cell expression, and then correlating them with the ICR expression would result in their expansion and/or suppression property in the TME.
2.3. Genomic signatures
Band q13 of chromosome 11 in humans harbours many candidate genes implicated in oral cancer. Several genetic drivers that function to confer a malignant phenotype to the host cell have been mapped to this locus [80]. The specialty of this locus is that a set of neighbouring gene are often co-amplified. It has been observed that amplification of this particular chromosomal band is often associated with worse prognosis during the investigation of cell lines obtained from oral cancer patients [81]. Within the 11q13.2-q13.4sub-region, an amplicon core has been identified that is responsible for oral squamous cell carcinoma (OSCC). This amplicon shows a high degree of complexity in both structure and composition [82]. Discontinuities are observed, suggestive of preferential re-amplification or counter selection. A study by Natrajan et al. [83] has shown that it is possible for an amplicon to be associated with more than one amplicon driver. By limiting candidates to the smallest regions of amplification, many drivers associated with this amplicon have been identified. It is quite possible that the observed phenotypes in oral cancer are a result of a co-operative interaction between the genetic markers of locus 11q13.
CCND1 (encodes cyclin D1 that promotes the G1-S phase transition during the cell cycle) and CTTN (coding for cortactin, an F-actin binding protein that permit various protein interactions) are two of the most frequently associated drivers of locus 11q13. The amplification of CTTN confers resistance to the anticancer drug gefitinib, while amplification of CCND1 is associated with resistance to cisplatin [84]. The presence of these oncogenes influencesthe clinicopathological characteristics, such as lymph node involvement, poor tumour differentiationand low survival, observed in OSCC [85]. Strong expression of cortactin is a predicting factor for increased cancer risk in oral premalignant lesions [86]. Epigallocatechin-3 gallate, an active polyphenol component of green tea, has various beneficial biological effects. Actin cytoskeleton remodelling through activation of FAK/Src signalling and a decrease in cortactin phosphorylation due to epigallocatechin-3 gallate treatment resulted in inhibition of oral cancer cell invasiveness and motility [87]. Expression levels of the CCND1 gene could be used as a biomarker to select oral cancer patients who could benefit from induction chemotherapy. Although, lower cyclin D1 expression in the pretreatment biopsy samples is generally considered a favourable prognostic biomarker, Zhong et al. found that the higher the expression of cyclin D1 is, the better is the response of the patients towards chemotherapy [88]. In synergy with CCND1, overexpression of the PPP1CA gene, coding for the catalytic subunit of protein phosphatase 1α (PP1α), is responsible for the progression of oral cancer [89]. The RNA-binding protein quaking 5 (QKI-5) regulates the growth of the human oral cancer cell line CAL-27. This regulative function is attributed to its ability to regulate the mitogen-activated protein kinase (MAPK) pathway, leading to decreased expression of cyclin D1 [90]. The antagonistic effect of FOXO3a on the phosphoinositide-3-kinase (PI3K)/Akt pathway can also regulate the level of cyclin D1 in OSCC [91]. For this reason, FOXO3a activation has even been proposed as a therapeutic strategy for OSCC.
2.4. Markers located on other loci
Apart from 11q13, a gain of chromosome 8q has also been implicated in the development of OSCC [92]. A majority of structural rearrangements observed are isochromosomes or whole arm translocations. FAK/PTK2 is one of the most important genes located within the chromosomal region 8q23–24, encoding the intracellular protein focal adhesion kinase (FAK) located in cellular structures called “focal adhesions”. Overexpression of this particular protein was detected in premalignant oral mucosa lesions at early stages of oral tumourigenesis [86]. The frequency of amplification of this particular locus increases with the grade of dysplasia. It is an important determinant in the pathogenesis, development and progression of a significant subset of oral squamous cell carcinomas. OSCC had higher frequencies of gain of chromosome arms 1q and 8q and chromosome region 11q1, and loss of genetic material from 3p and 8p2 [92].
2.5. Genes involved in oral carcinoma of the tongue and gingivo-buccal
In oral carcinoma located in the tongue, the expression of FADD (Fas-associated death domain-containing protein) was higher than that in adjacent areas [93]. This phenomenon can be attributed to genomic amplification in 11q13.3, impacting the regulation of the FADD gene. FADD acts as an adaptor to relay apoptotic signals initiated by death receptors such as Fas. FADD amplification was found to correlate with gender distinction, possibly accounting for the observed twofold increased frequency of oral cancer occurrence in males compared with females. Overexpression of FADD is more likely to make the carcinoma metastatic. ORAOV1 (Oral Cancer Overexpressed 1) is another oncogene located at this locus, whose gain of function has been attributed to the inhibition of apoptosis, progression through the cell cycle and angiogenesis [94, 95]. Whole-exome sequencing of 120 OSCCs from male individuals in Taiwan has identified several mutational signatures [96]. Novel driver genes, such as CHUK and ELAVL1, have been identified that are involved in promoting or repressing the functions of various oncogenes and tumour suppressor genes. Two important genes mutated less frequently are ASXL1 (coding for a transcription factor) and RPTN (related to epithelial differentiation). A significant group of genes involved in cell cycle regulation, including TP53, CDKN2A, and CCND1, were also present. Loss of theTP53 allele has long been associated with defects in cell cycle regulation, leading to uncontrolled amplification [97]. Tumours predominantly located in the tongue could be targeted by drugs against theTP53 and CCND1 genes of the p53-cell cycle pathway. More than 50% of the tumours were found to carry at least one aberrant event potentially targeted by US Food and Drug Administration approved agents.
Gingivo-buccal oral squamous cell carcinoma (OSCC-GB) is a clinical subtype of OSCC, prevalent in the Asian sub-continent, where tobacco chewing is common. A synergistic contribution of related major OSCC driver genes, such as MAP4K2, FAT1, EPHA2, NOTCH1, CASP8, HRAS, RASA1, and PIK3CA, has been found to contribute to tumourigenesis, with the most common anatomical site being the buccal mucosa. Genetic signatures indicate that mutations in several cancer genes, including USP9X, MLL4, ARID2, UNC13C and TRPM3, are specific to OSCC-GB [96, 98]. These specific genes are functionally involved in the suppression of tumours. Some genetic markers, such as TP53, FAT1, CASP8, HRAS and NOTCH1, are shared between OSCC-GB and HNSCC. Alterations in some new genes, for example, DROSHA, YAP1 and DDX3X, have been discovered in OSCC-GB. An enrichment of alterations in Wnt signalling, dorso-ventral axis formation and axon guidance pathways was also discovered. A very high proportion of C4G mutations, especially among tobacco users, was observed by the India Project Team of the International Cancer Genome Consortium [98]. It seems that mutations in tumour suppressor genes are more prevalent than mutations of oncogenes in oral cancer. Some of the important genetic markers for oral cancer are listed in Table 2.
Table 2.
List of some genes, which have been found to play a significant role in the development of oral carcinoma.
| Gene | Locus | Function | Reference |
|---|---|---|---|
| CCND1 | 11q13 | Cell cycle regulation | [72, 76, 77, 78, 79, 86] |
| CTTN | 11q13 | F-actin binding protein | [72, 74, 75] |
| FADD | 11q13 | Regulation of apoptosis | [83] |
| ORAOV1 | 11q13 | Regulation of apoptosis and angiogenesis | [84, 85] |
| TP53 | 17p13 | Regulation of cell cycle and apoptosis | [87] |
| FAK/PTK2 | 8q23–24 | Cellular adhesion and spreading | [74] |
| PIK3CA | 3q26 | Regulation of receptor- mediated extracellular stimuli | [86] |
| SOX2 | 3q26 | Transcription factor | [86] |
| EGFR | 7p12 | Receptor for epidermal growth factor protein ligands | [90, 91, 92] |
2.6. Gene expression studies and the role of HPV
Gene expression analyses can be used to predict lymph node metastasis and the extracapsular spread of metastatic nodes in patients of OSCC [99]. CTTN and MMP9 have been found to be two important biomarkers whose overexpression can be used to predict the lymph node metastasis and extracapsular spread. MMP9 is a zinc metalloprotease that can degrade the collagen of the extracellular matrix. Other candidates are BMP2, a member of the transforming growth factor-β superfamily, and epidermal growth factor receptor (EGFR). Fluorescence in situ hybridization (FISH) and immunohistochemistry (IHC) studies on OSCC samples by Martin-Ezquerra et al. have detected genetic abnormalities in a set of cell cycle markers, includingTP53, MYC, CCND1, ERBB2 and EGFR [100]. As expected, loss of the tumour suppressor gene TP53 and copy number gains of the oncogenes MYC, CCND1, ERBB2 and EGFR were detected in tumoural lesions. These same genetic abnormalities were infrequent in precursor lesions and totally absent in inflammatory lesions. Thus, evaluation of these genes can act as a diagnostic tool to distinguishing benign from malignant oral lesions. Since, multiple genetic alterations are involved in the pathogenesis of OSCC, monoclonal antibody targeted therapies are unlikely to be very effective.
A CGH study on primary OSCCs obtained from 97 patients by Pathare et al. [101] identified several genomic alterations caused mainly by tobacco use. A strong correlation of 7p gain and 8p loss with node-positive OSCC was observed. Activation of the oncogene EGFR on 7p12 and loss of the tumour suppressor genes on 8p may contribute to the lymph node involvement of primary OSCC. Loss of the q arm of chromosome 18 was also found to decrease survival. Their findings revealed the importance of simultaneous 11q13 gain and 18q loss as a predictor of poor prognosis. An array comparative genomic hybridization analysis of progressive oral potential malignant lesions and same-site OSCCs identified copy number alterations that may be associated with disease progression [102]. A majority of them were amplifications observed on chromosomes 1p, 11q13.4, 9q34.13, 21q22.3, 6p21, 6q25, 10q24, 19q13.2, 22q12, 5q31.2, 7p13, 10q24 and 14q22. DNA losses were observed at a lesser frequency on 5q31.2, 16p13.2, 9q33.1, 9q33.29, 17q11.2, 3p26.2, 18q21.1, 4q34.1 and 8p23.2. Some of the associated genes identified and validated by quantitative real-time polymerase chain reaction are BTBD7, KHDRBS1, PARP1 and RAB1A, indicating changes in transcriptional and post-transcriptional control mechanisms as important factors for disease progression. By combining array-CGH with mRNA expression and tissue microarray analysis, Freier et al. found SOX2 in 3q26.33 coding for a transcription factor and CCNE1 in 19q12, a member of the cyclin family, as important candidate genes on OSCC specimens [103]. Using array-based comparative genomic hybridization on microdissected OSCCs, Chen et al. have observed copy number gains in TP63, Serpine1, FGF4/FGF3, c-Myc, EGFR, CCND1, EMS1, AIB1 and DMD genes clustering mainly on 3q27–29, 7p, 17q21–tel, 11q13, 20q and the X chromosome [104]. Among them, gains of EGFR at 7p, FGF4/FGF3, CCND1and EMS1at 11q13, and AIB1 at 20q were significantly associated with lymph node metastasis. On the other hand, deletions were detected for Caspase8 and MTAP. An areca quid (AQ) chewing habit linked to Asian countries differentially affect the genomic profiles of FHIT at 3p14.2 and EXT1 at 8q24.11-13.
It is very important to differentiate between HPV-related and HPV-unrelated OSCC because of competing treatment strategies. The number of chromosomal alterations to form tumours is lower in the presence of HPV due to the inactivation of the tumour suppressor proteins p53 and pRb by the viral E6 and E7 oncoproteins, respectively. Copy number gain at 3q26.3 and 11q13 was present irrespective of HPV status, although its effect was more severe in HPV-negative tumours [105, 106]. OSCC in the presence of HPV showed significantly more losses at chromosomes 3p, 5q, 9p, 15q, and 18q and, less often, Xp gains. Loss of 16q in HPV-related OSCC was found to be a strong indicator of favourable outcome with no recurrence. This information should be considered to improve treatment decisions.
3. Conclusions
Among the various categories of HNSCC, cancer of the oral cavity is the most common malignancy and has a high morbidity rate (37.8%) five years after diagnosis [107, 108]. With late detection and poor prognosis, OSCC has been the most relevant epithelial malignancy for dental surgeons [109]. OSCC is a highly heterogeneous, complex subtype of cancer [110]. Tobacco, alcohol, viruses and diet are several of the risk factors involved. These factors, along with genetic inheritance, may have a carcinogenic effect on the respiratory and digestive system's normal cells. This can occur in regions such as the mouth, and the tongue, lower lip and mouth floor are the most affected regions [107, 111].
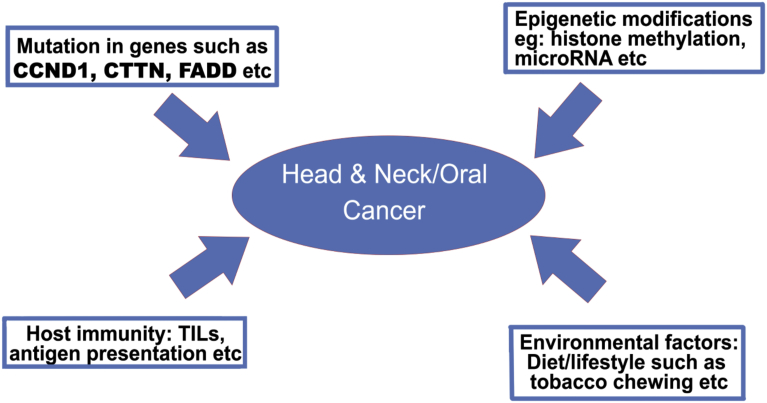
This review article sheds light on the role of various immune factors involved in HNSCC and the genetic markers responsible for the development of OSCC (Fig. 1). As seen from this review, several genetic signatures specific to OSCC are available. In contrast to immunological markers, a plethora of research work has been directed towards the broader purview of HNSCC, but the same data specific for OSCC are very limited. That is exactly where our group is planning to contribute in the near future. A histological analysis of tumours from the oral cavity has shown a correlation between increased intratumoural or stromal TILs and a better prognosis [112]. The identification of genetic abnormalities is becoming easier with the rapid progress in detection technologies. Emerging technologies that can provide both genetic and epigenetic information have the potential to provide an overall picture of tumour progression. Recently, a group from China reported a set of twenty-four genes that are postulated to be important for the classification and prognosis of OSCC [113].
Fig. 1.
Various factors contributing to the occurrence of head and neck/oral carcinoma. TILs: Tumour infiltrating lymphocytes.
Along with genomic aberrations, regulation of the immune profile and the interplay between them can also have a significant effect on the pathological features and treatment outcome of a particular patient. An example of this interplay can be seen in the loss or down-regulation of HLA genes belonging to the MHC on chromosome 6 that provides tumour cells an opportunity to evade the host immune response [114, 115]. Recognition of TAA by HLA-restricted T cells is fundamental for the detection and destruction of malignant cells [116]. Alterations in MHC can be reversible regulatory defects or irreversible structural defects that can influence the outcome of cancer immunotherapy [117]. When there is a loss of expression due to transcriptional regulation, it can be reversed by cytokine treatment, and T-cell-based therapy can be successfully applied. However, immunotherapy aimed at augmenting a T-cell-specific anti-tumour response may not be effective in cases of structural damage to HLA genes that is irreversible. Therefore, immunotherapy needs to include precise identification of the HLA genotype. Analysis of HLA-A, B, and C genes on microdissected tumours correlated loss of expression to metastasis [118]. Loss of heterozygosity on chromosome 15, which codes for β-2 microglobulin, is quite prevalent in some cancers [119]. This could represent one of the early events in malignant cells showing a normal HLA-pattern, leading to the generation of precommitted tumours to become HLA escape variants. Another example of the integrity between genomic alterations and immunomodulation in many different types of cancer can be observed in copy number gains of chromosome 9p involving PD-L1 [120]. Apart from PD-L1, chromosome 9p also harbours PD-L2 and the Janus Kinase 2 gene (JAK2) adjacent to one another and localized exactly to 9p24.1. JAK2 is a transcriptional activator of both PD-1 ligands and amplification of this locus provides a distinct molecular subtype in breast cancer, gastric cancer and lymphomas [121, 122, 123, 124]. The PDJ amplicon in tumours seems to represent a biomarker that can be used to advance personalized therapies for cancer patients. The genetic basis of PD-1 ligand deregulation and overexpression in Hodgkin's lymphoma suggests that a blockade with an anti-PD-1 antibody could be used to treat this disease. In fact, Ansell et al. have shown that Nivolumab (a PD-1 blocking antibody) can be used as a therapeutic agent in patients suffering from relapsed Hodgkin's lymphoma [125].
It is quite obvious that increased neoantigen diversity caused by genomic alterations will have an effect on the immune infiltrate within TME. Future research related to both the positive and negative effects of gene amplification and the effectiveness of combined therapies that target both genetic and immune markers is warranted. One of the main challenges will be to integrate the staggering amount of data that is being generated in cancer research for better management.
Declarations
Author contribution statement
All authors listed have significantly contributed to the development and the writing of this article.
Funding statement
This work was supported by Department of Biotechnology, India.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
References
- 1.Hanahan D., Weinberg R.A. Hallmarks of cancer: the next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 2.Beatty G.L., Gladney W.L. Immune escape mechanisms as a guide for cancer immunotherapy. Clin. Cancer Res. 2015;21:687–692. doi: 10.1158/1078-0432.CCR-14-1860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ferris R.L. Immunology and immunotherapy of head and neck cancer. J. Clin. Oncol. 2015;33:3293–3304. doi: 10.1200/JCO.2015.61.1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boon T., Cerottini J.C., Van den Eynde B., van der Bruggen P., Van Pel A. Tumor antigens recognized by T lymphocytes. Annu. Rev. Immunol. 1994;12:337–365. doi: 10.1146/annurev.iy.12.040194.002005. [DOI] [PubMed] [Google Scholar]
- 5.Fuertes M.B., Kacha A.K., Kline J., Woo S.R., Kranz D.M., Murphy K.M. Host type I IFN signals are required for antitumor CD8+ T cell responses through CD8{alpha}+ dendritic cells. J. Exp. Med. 2011;208:2005–2016. doi: 10.1084/jem.20101159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sanderson R.J., Ironside J.A.D. Squamous cell carcinomas of the head and neck. BMJ. 2002;325:822–827. doi: 10.1136/bmj.325.7368.822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pak A.S., Wright M.A., Matthews J.P., Collins S.L., Petruzzelli G.J., Young M.R. Mechanisms of immune suppression in patients with head and neck cancer: presence of CD34(+) cells which suppress immune functions within cancers that secrete granulocyte-macrophage colony-stimulating factor. Clin. Cancer Res. 1995;1:95–103. Published January 1995. [PubMed] [Google Scholar]
- 8.Marincola F.M., Jaffee E.M., Hicklin D.J., Ferrone S. Escape of human solid tumors from T-cell recognition: molecular mechanisms and functional significance. Adv. Immunol. 2000;74:181–273. doi: 10.1016/s0065-2776(08)60911-6. [DOI] [PubMed] [Google Scholar]
- 9.Whiteside T.L. Apoptosis of immune cells in the tumor microenvironment and peripheralcirculation of patients with cancer: implications for immunotherapy. Vaccine. 2002;20:A46–A51. doi: 10.1016/s0264-410x(02)00387-0. [DOI] [PubMed] [Google Scholar]
- 10.Whiteside T.L. Immunobiology of head and neck cancer. Cancer Metastasis Rev. 2005;24:95–105. doi: 10.1007/s10555-005-5050-6. [DOI] [PubMed] [Google Scholar]
- 11.Hoffmann T.K., Dworacki G., Tsukihiro T., Meidenbauer N., Gooding W., Johnson J.T. Spontaneous apoptosis of circulating T lymphocytes in patients with headand neckcancer and its clinical importance. Clin. Cancer Res. 2002;8:2553–2562. Published August 2002. [PubMed] [Google Scholar]
- 12.Lengauer C., Kinzler K.W., Vogelstein B. Genetic instabilities in human cancers. Nature. 1998;396:643–649. doi: 10.1038/25292. [DOI] [PubMed] [Google Scholar]
- 13.Albertson D.G., Collins C., McCormick F., Gray J.W. Chromosome aberrations in solid tumors. Nat. Genet. 2003;34:369–376. doi: 10.1038/ng1215. [DOI] [PubMed] [Google Scholar]
- 14.Tang Y.C., Amon A. Gene copy-number alterations: a cost-benefit analysis. Cell. 2013;152:394–405. doi: 10.1016/j.cell.2012.11.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Savelyeva L., Schwab M. Amplification of oncogenes revisited: from expression profiling to clinical application. Cancer Lett. 2001;167:115–123. doi: 10.1016/s0304-3835(01)00472-4. [DOI] [PubMed] [Google Scholar]
- 16.Garnis C., Campbell J., Zhang L., Rosin M.P., Lam W.L. OCGR array: an oral cancer genomic regional array for comparative genomic hybridization analysis. Oral Oncol. 2004;40:511–519. doi: 10.1016/j.oraloncology.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 17.Zhang H.X., Liu O.S., Deng C., He Y., Feng Y.Q., Ma J.A. Genome-wide gene expression profiling of tongue squamous cell carcinoma by RNA-seq. Clin. Oral Investig. 2018;22:209–216. doi: 10.1007/s00784-017-2101-7. [DOI] [PubMed] [Google Scholar]
- 18.Kuss I., Donnenberg A.D., Gooding W., Whiteside T.L. Effector CD8+CD45RO-CD27-Tcells have signalling defects in patients with squamous cell carcinoma of the head and neck. Br. J. Cancer. 2003;88:223–230. doi: 10.1038/sj.bjc.6600694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chikamatsu K., Sakakura K., Toyoda M., Takahashi K., Yamamoto T., Masuyama K. Immunosuppressive activity of CD14+ HLA-DR- cells in squamous cell carcinoma of the head and neck. Cancer Sci. 2012;103:976–983. doi: 10.1111/j.1349-7006.2012.02248.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sun W., Li W.J., Wu C.Y., Zhong H., Wen W.P. CD45RA-Foxp3high but not CD45RA+Foxp3low suppressive T regulatory cells increased in the peripheral circulation of patients with head and neck squamous cell carcinoma and correlated with tumor progression. J. Exp. Clin. Cancer Res. 2014;25:33–35. doi: 10.1186/1756-9966-33-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Curtsinger J.M., Mescher M.F. Inflammatory cytokines as a third signal for T cell activation. Curr. Opin. Immunol. 2010;22:333–340. doi: 10.1016/j.coi.2010.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shimabukuro-Vornhagen A., Schlößer H.A., Gryschok L., Malcher J., Wennhold K., Garcia-Marquez M. Characterization of tumor-associated B-cell subsets in patients with colorectal cancer. Oncotarget. 2014;5:4651–4664. doi: 10.18632/oncotarget.1701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schlößer H.A., Drebber U., Kloth M., Thelen M., Rothschild S.I., Haase S. Immunecheckpoints programmed death 1 ligand 1 and cytotoxic T lymphocyte associatedmolecule 4 in gastric adenocarcinoma. OncoImmunology. 2015;5 doi: 10.1080/2162402X.2015.1100789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Woo E.Y., Chu C.S., Goletz T.J., Schlienger K., Yeh H., Coukos G. Regulatory CD4(+)CD25(+) T cells in tumors from patients with early-stage non-small cell lung cancer and late-stage ovarian cancer. Cancer Res. 2001;61:4766–4772. Published June 2001. [PubMed] [Google Scholar]
- 25.Woo E.Y., Yeh H., Chu C.S., Schlienger K., Carroll R.G., Riley J.L. Cutting edge: regulatory T cells from lung cancer patients directly inhibit autologous T cell proliferation. J. Immunol. 2002;168:4272–4276. doi: 10.4049/jimmunol.168.9.4272. [DOI] [PubMed] [Google Scholar]
- 26.Liyanage U.K., Moore T.T., Joo H.G., Tanaka Y., Herrmann V., Doherty G. Prevalence of regulatory T cells is increased in peripheral blood and tumor microenvironment of patients with pancreas or breast adenocarcinoma. J. Immunol. 2002;169:2756–2761. doi: 10.4049/jimmunol.169.5.2756. [DOI] [PubMed] [Google Scholar]
- 27.Wolf A.M., Wolf D., Steurer M., Gastl G., Gunsilius E., Grubeck-Loebenstein B. Increase of regulatory T cells in the peripheral blood of cancer patients. Clin. Cancer Res. 2003;9:606–612. Published February 2003. [PubMed] [Google Scholar]
- 28.Coombes J.L., Siddiqui K.R., Arancibia-Cárcamo C.V., Hall J., Sun C.M., Belkaid Y. A functionally specialized population of mucosal CD103+ DCs induces Foxp3+ regulatory T cells via a TGF-beta and retinoic acid-dependent mechanism. J. Exp. Med. 2007;204:1757–1764. doi: 10.1084/jem.20070590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sun C.M., Hall J.A., Blank R.B., Bouladoux N., Oukka M., Mora J.R. Small intestine lamina propria dendritic cells promote de novo generation of Foxp3 T reg cells via retinoic acid. J. Exp. Med. 2007;204:1775–1785. doi: 10.1084/jem.20070602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Darrasse-Jèze G., Bergot A.S., Durgeau A., Billiard F., Salomon B.L., Cohen J.L. Tumor emergence is sensed by self-specific CD44hi memory Tregs that create a dominant tolerogenic environment for tumors in mice. J. Clin. Invest. 2009;119:2648–2662. doi: 10.1172/JCI36628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Whiteside T.L. Down-regulation of zeta-chain expression in T cells: a biomarker of prognosis in cancer? Cancer Immunol. Immunother. 2004;53:865–878. doi: 10.1007/s00262-004-0521-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wallis S.P., Stafford N.D., Greenman J. Clinical relevance of immune parameters in the tumor microenvironment of head and neck cancers. Head Neck. 2015;37:449–459. doi: 10.1002/hed.23736. [DOI] [PubMed] [Google Scholar]
- 33.Pagès F., Kirilovsky A., Mlecnik B., Asslaber M., Tosolini M., Bindea G. In situ cytotoxic and memory T cells predict outcome in patients with early-stage colorectal cancer. J. Clin. Oncol. 2009;27:5944–5951. doi: 10.1200/JCO.2008.19.6147. [DOI] [PubMed] [Google Scholar]
- 34.Galon J., Mlecnik B., Bindea G., Angell H.K., Berger A., Lagorce C. Towards the introduction of the ‘Immunoscore’ in the classification of malignant tumours. J. Pathol. 2014;232:199–209. doi: 10.1002/path.4287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Förster R., Davalos-Misslitz A.C., Rot A. CCR7 and its ligands: balancing immunity andtolerance. Nat. Rev. Immunol. 2008;8:362–371. doi: 10.1038/nri2297. [DOI] [PubMed] [Google Scholar]
- 36.Rot A., von Andrian U.H. Chemokines in innate and adaptive host defense: basic chemokinese grammar for immune cells. Annu. Rev. Immunol. 2004;22:891–928. doi: 10.1146/annurev.immunol.22.012703.104543. [DOI] [PubMed] [Google Scholar]
- 37.Ohl L., Mohaupt M., Czeloth N., Hintzen G., Kiafard Z., Zwirner J. CCR7 governs skin dendritic cell migration under inflammatory and steady-state conditions. Immunity. 2004;21:279–288. doi: 10.1016/j.immuni.2004.06.014. [DOI] [PubMed] [Google Scholar]
- 38.Misslitz A., Pabst O., Hintzen G., Ohl L., Kremmer E., Petrie H.T. Thymic T cell development and progenitor localization depend on CCR7. J. Exp. Med. 2004;200:481–491. doi: 10.1084/jem.20040383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Reif K., Ekland E.H., Ohl L., Nakano H., Lipp M., Förster R. Balanced responsiveness to chemoattractants from adjacent zones determines B-cell position. Nature. 2002;416:94–99. doi: 10.1038/416094a. [DOI] [PubMed] [Google Scholar]
- 40.Sallusto F., Lenig D., Förster R., Lipp M., Lanzavecchia A. Two subsets of memory T lymphocytes with distinct homing potentials and effector functions. Nature. 1999;401:708–712. doi: 10.1038/44385. [DOI] [PubMed] [Google Scholar]
- 41.Szanya V., Ermann J., Taylor C., Holness C., Fathman C.G. The subpopulation of CD4+CD25+ splenocytes that delays adoptive transfer of diabetes expresses L-selectin and high levels of CCR7. J. Immunol. 2002;169:2461–2465. doi: 10.4049/jimmunol.169.5.2461. [DOI] [PubMed] [Google Scholar]
- 42.Mao F.Y., Kong H., Zhao Y.L., Peng L.S., Chen W., Zhang J.Y. Increased tumor-infiltrating CD45RA-CCR7- regulatory T-cell subset with immunosuppressive properties foster gastric cancer progress. Cell Death Dis. 2017;8 doi: 10.1038/cddis.2017.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mburu Y.K., Wang J., Wood M.A., Walker W.H., Ferris R.L. CCR7 mediates inflammation-associated tumor progression. Immunol. Res. 2006;36:61–72. doi: 10.1385/IR:36:1:61. [DOI] [PubMed] [Google Scholar]
- 44.Ueda M., Shimada T., Goto Y., Tei K., Nakai S., Hisa Y. Expression of CC-chemokine receptor 7 (CCR7) and CXC-chemokine receptor 4 (CXCR4) in head and neck squamous cell carcinoma. Auris Nasus Larynx. 2010;37:488–495. doi: 10.1016/j.anl.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 45.Xia X., Liu K., Zhang H., Shang Z. Correlation between CCR7 expression and lymph node metastatic potential of human tongue carcinoma. Oral Dis. 2015;21:123–131. doi: 10.1111/odi.12228. [DOI] [PubMed] [Google Scholar]
- 46.Zhang N., Bevan M.J. CD8(+) T cells: foot soldiers of the immune system. Immunity. 2011;35(2):161–168. doi: 10.1016/j.immuni.2011.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Perfetto S.P., Chattopadhyay P.K., Roederer M. Seventeen-colour flow cytometry: unravelling the immune system. Nat. Rev. Immunol. 2004;4:648–655. doi: 10.1038/nri1416. [DOI] [PubMed] [Google Scholar]
- 48.Sanders M.E., Makgoba M.W., Shaw S. Human naive and memory T cells: reinterpretation of helper-inducer and suppressor-inducer subsets. Immunol. Today. 1988;9:195–199. doi: 10.1016/0167-5699(88)91212-1. [DOI] [PubMed] [Google Scholar]
- 49.Holling T.M., van der Stoep N., Quinten E., van den Elsen P.J. Activated human T cellsaccomplish MHC class II expression through T cell-specific occupation of class II transactivator promoter III. J. Immunol. 2002;168:763–770. doi: 10.4049/jimmunol.168.2.763. [DOI] [PubMed] [Google Scholar]
- 50.Birle A., Nebe C.T., Gessler P. Age-related low expression of HLA-DR molecules on monocytes of term and preterm newborns with and without signs of infection. J. Perinatol. 2003;23:294–299. doi: 10.1038/sj.jp.7210906. [DOI] [PubMed] [Google Scholar]
- 51.Sakaguchi S., Sakaguchi N., Asano M., Itoh M., Toda M. Immunologic self-tolerance maintained by activated T cells expressing IL-2 receptor alpha-chains (CD25). Breakdown of a single mechanism of self-tolerance causes various autoimmune diseases. J. Immunol. 1995;155:1151–1164. [PubMed] [Google Scholar]
- 52.Cosmi L., Liotta F., Lazzeri E., Francalanci M., Angeli R., Mazzinghi B. Human CD8+CD25+ thymocytes share phenotypic and functional features with CD4+CD25+ regulatory thymocytes. Blood. 2003;102:4107–4114. doi: 10.1182/blood-2003-04-1320. [DOI] [PubMed] [Google Scholar]
- 53.Ralainirina N., Poli A., Michel T., Poos L., Andrès E., Hentges F. Control of NK cell functions by CD4+CD25+ regulatory T cells. J. Leukoc. Biol. 2007;81:144–153. doi: 10.1189/jlb.0606409. [DOI] [PubMed] [Google Scholar]
- 54.Alhamarneh O., Amarnath S.M., Stafford N.D., Greenman J. Regulatory T cells: what role do they play in antitumor immunity in patients with head and neck cancer? Head Neck. 2008;30:251–261. doi: 10.1002/hed.20739. [DOI] [PubMed] [Google Scholar]
- 55.Strauss L., Bergmann C., Szczepanski M., Gooding W., Johnson J.T., Whiteside T.L. A unique subset of CD4+CD25highFoxp3+ T cells secreting interleukin-10 and transforming growth factor-beta1 mediates suppression in the tumor microenvironment. Clin. Cancer Res. 2007;13:4345–4354. doi: 10.1158/1078-0432.CCR-07-0472. [DOI] [PubMed] [Google Scholar]
- 56.Strauss L., Bergmann C., Whiteside T.L. Functional and phenotypic characteristics ofCD4+CD25highFoxp3+ Treg clones obtained from peripheral blood of patients with cancer. Int. J. Cancer. 2007;121:2473–2483. doi: 10.1002/ijc.23001. [DOI] [PubMed] [Google Scholar]
- 57.Strauss L.1, Bergmann C., Gooding W., Johnson J.T., Whiteside T.L. The frequency and suppressor function of CD4+CD25highFoxp3+ T cells in the circulation of patients with squamous cell carcinoma of the head and neck. Clin. Cancer Res. 2007;13:6301–6311. doi: 10.1158/1078-0432.CCR-07-1403. [DOI] [PubMed] [Google Scholar]
- 58.Jie H.B., Gildener-Leapman N., Li J., Srivastava R.M., Gibson S.P., Whiteside T.L. Intratumoral regulatory T cells upregulate immunosuppressive molecules in head and neck cancer patients. Br. J. Cancer. 2013;109:2629–2635. doi: 10.1038/bjc.2013.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Muller A.J., Prendergast G.C. Indoleamine 2, 3-dioxygenase in immune suppression and cancer. Curr. Cancer Drug Targets. 2007;7:31–40. doi: 10.2174/156800907780006896. [DOI] [PubMed] [Google Scholar]
- 60.Pietra G., Manzini C., Rivara S., Vitale M., Cantoni C., Petretto A. Melanoma cells inhibit natural killer cell function by modulating the expression of activating receptors and cytolytic activity. Cancer Res. 2012;72:1407–1415. doi: 10.1158/0008-5472.CAN-11-2544. [DOI] [PubMed] [Google Scholar]
- 61.Givechian K.B., Wnuk K., Garner C., Benz S., Garban H., Rabizadeh S. Identification of an immune gene expression signature associated with favorable clinical features in Treg-enriched patient tumor samples. NPJ Genom. Med. 2018;3:14. doi: 10.1038/s41525-018-0054-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Badoual C., Hans S., Rodriguez J., Peyrard S., Klein C., Agueznay Nel H. Prognostic value of tumor-infiltrating CD4+ T-cell subpopulations in head and neck cancers. Clin. Cancer Res. 2006;12:465–472. doi: 10.1158/1078-0432.CCR-05-1886. [DOI] [PubMed] [Google Scholar]
- 63.Nguyen N., Bellile E., Thomas D., McHugh J., Rozek L., Virani S. Tumor infiltrating lymphocytes and survival in patients with head and neck squamous cell carcinoma. Head Neck. 2016;38:1074–1084. doi: 10.1002/hed.24406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Whiteside T.L. The role of regulatory T cells in cancer immunology. Immunotargets Ther. 2015;4:159–171. doi: 10.2147/ITT.S55415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.deLeeuw R.J., Kost S.E., Kakal J.A., Nelson B.H. The prognostic value of FoxP3+ tumor-infiltrating lymphocytes in cancer: a critical review of the literature. Clin. Cancer Res. 2012;18:3022–3029. doi: 10.1158/1078-0432.CCR-11-3216. [DOI] [PubMed] [Google Scholar]
- 66.Shang B., Liu Y., Jiang S.J., Liu Y. Prognostic value of tumor-infiltrating FoxP3+ regulatory T cells in cancers: a systematic review and meta-analysis. Sci. Rep. 2015;5:15179. doi: 10.1038/srep15179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Damuzzo V., Pinton L., Desantis G., Solito S., Marigo I., Bronte V. Complexity and challenges in defining myeloid-derived suppressor cells. Cytometry Part B (Clin. Cytometry) 2015;88B:77–91. doi: 10.1002/cyto.b.21206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gill M.A. The role of dendritic cells in asthma. J. Allergy Clin. Immunol. 2012;129:889–901. doi: 10.1016/j.jaci.2012.02.028. [DOI] [PubMed] [Google Scholar]
- 69.Singh A.K., Gaur P., Shukla N.K., Das S.N. Differential dendritic cell-mediated activation and functions of invariant NKT-cell subsets in oral cancer. Oral Dis. 2015;21:e105–e113. doi: 10.1111/odi.12238. [DOI] [PubMed] [Google Scholar]
- 70.Mantovani A., Sozzani S., Locati M., Allavena P., Sica A. Macrophage polarization: tumor-associated macrophages as a paradigm for polarized M2 mononuclear phagocytes. Trends Immunol. 2002:549–555. doi: 10.1016/s1471-4906(02)02302-5. [DOI] [PubMed] [Google Scholar]
- 71.Lambrecht B.N., Hammad H. Lung dendritic cells in respiratory viral infection and asthma: from protection to immunopathology. Annu. Rev. Immunol. 2012;30:243–270. doi: 10.1146/annurev-immunol-020711-075021. [DOI] [PubMed] [Google Scholar]
- 72.Kusmartsev S., Nefedova Y., Yoder D., Gabrilovich D.I. Antigen-specific inhibition of CD8+ T cell response by immature myeloid cells in cancer is mediated by reactive oxygen species. J. Immunol. 2004;172:989–999. doi: 10.4049/jimmunol.172.2.989. [DOI] [PubMed] [Google Scholar]
- 73.Kusmartsev S., Gabrilovich D.I. STAT1 signaling regulates tumor-associated macrophage-mediated T cell deletion. J. Immunol. 2005;174:4880–4891. doi: 10.4049/jimmunol.174.8.4880. [DOI] [PubMed] [Google Scholar]
- 74.Fridlender Z.G., Sun J., Kim S., Kapoor V., Cheng G. Polarization of tumor-associated neutrophil phenotype by TGF-beta: “N1” versus “N2” TAN. Cancer Cell. 2009;16:183–194. doi: 10.1016/j.ccr.2009.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Liu J.F., Deng W.W., Chen L., Li Y.C., Wu L., Ma S.R. Inhibition of JAK2/STAT3 reduces tumor-induced angiogenesis and myeloid-derived suppressor cells in head and neck cancer. Mol. Carcinog. 2018;57:429–439. doi: 10.1002/mc.22767. [DOI] [PubMed] [Google Scholar]
- 76.Lechner M.G., Liebertz D.J., Epstein A.L. Characterization of cytokine-induced myeloid-derived suppressor cells from normal human peripheral blood mononuclear cells. J. Immunol. 2010;185:2273–2284. doi: 10.4049/jimmunol.1000901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Rodríguez-Ubreva J., Català-Moll F., Obermajer N., Álvarez-Errico D., Ramirez R.N., Company C. Prostaglandin E2 leads to the acquisition of DNMT3A-dependent tolerogenic functions in human myeloid-derived suppressor cells. Cell Rep. 2017;21:154–167. doi: 10.1016/j.celrep.2017.09.018. [DOI] [PubMed] [Google Scholar]
- 78.Bauman J.E., Ferris R.L. Integrating novel therapeutic monoclonal antibodies into the management of head and neck cancer. Cancer. 2014;120:624–632. doi: 10.1002/cncr.28380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zitvogel L., Kroemer G. Targeting PD-1/PD-L1 interactions for cancer immunotherapy. OncoImmunology. 2012;1:1223–1225. doi: 10.4161/onci.21335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ramos-García P., Ruiz-Ávila I., Gil-Montoya J.A., Ayén Á., González-Ruiz L., Navarro-Triviño F.J. Relevance of chromosomal band 11q13 in oral carcinogenesis: an update of current knowledge. Oral Oncol. 2017;72:7–16. doi: 10.1016/j.oraloncology.2017.04.016. [DOI] [PubMed] [Google Scholar]
- 81.Martin C.L., Reshmi S.C., Ried T., Gottberg W., Wilson J.W., Reddy J.K. Chromosomal imbalances in oral squamous cell carcinoma: examination of 31 cell lines and review of the literature. Oral Oncol. 2008;44:369–382. doi: 10.1016/j.oraloncology.2007.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gaudray P., Szepetowski P., Escot C., Birnbaum D., Theillet C. DNA amplification at 11q13 in human cancer: from complexity to perplexity. Mutat. Res. 1992;276:317–328. doi: 10.1016/0165-1110(92)90018-5. [DOI] [PubMed] [Google Scholar]
- 83.Natrajan R., Mackay A., Wilkerson P.M., Lambros M.B., Wetterskog D., Arnedos M. Functional characterization of the 19q12 amplicon in grade III breast cancers. Breast Cancer Res. 2012;14:R53. doi: 10.1186/bcr3154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhang P., Zhang Z., Zhou X., Qiu W., Chen F., Chen W. Identification of genes associated with cisplatin resistance in human oral squamous cell carcinoma cell line. BMC Cancer. 2006;6:224. doi: 10.1186/1471-2407-6-224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wilkerson P.M., Reis-Filho J.S. The 11q13-q14 amplicon: clinicopathological correlationsand potential drivers. Genes Chromosomes Cancer. 2013;52:333–355. doi: 10.1002/gcc.22037. [DOI] [PubMed] [Google Scholar]
- 86.de Vicente J.C., Rodrigo J.P., Rodriguez-Santamarta T., Lequerica-Fernández P., Allonca E., García-Pedrero J.M. Cortactin and focal adhesion kinase as predictors of cancer risk inpatients with premalignant oral epithelial lesions. Oral Oncol. 2012;48:641–646. doi: 10.1016/j.oraloncology.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 87.Hwang Y.S., Park K.K., Chung W.Y. Epigallocatechin-3 gallate inhibits cancer invasion by repressing functional invadopodia formation in oral squamous cell carcinoma. Eur. J. Pharmacol. 2013;715:286–295. doi: 10.1016/j.ejphar.2013.05.008. [DOI] [PubMed] [Google Scholar]
- 88.Zhong L.P., Zhu D.W., William W.N., Jr., Liu Y., Ma J., Yang C.Z. Elevated cyclin D1expression is predictive for a benefit from TPF induction chemotherapy in oral squamous cell carcinoma patients with advanced nodal disease. Mol. Cancer Therapeut. 2013;12:1112–1121. doi: 10.1158/1535-7163.MCT-12-1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hsu L.C., Huang X., Seasholtz S., Potter D.M., Gollin S.M. Gene amplification and overexpression of protein phosphatase 1 alpha in oral squamous cell carcinoma cell lines. Oncogene. 2006;25:5517–5526. doi: 10.1038/sj.onc.1209563. [DOI] [PubMed] [Google Scholar]
- 90.Fu X., Feng Y. QKI-5 suppresses cyclin D1 expression and proliferation of oral squamous cell carcinoma cells via MAPK signalling pathway. Int. J. Oral Maxillofac. Surg. 2015;44:562–567. doi: 10.1016/j.ijom.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 91.Fang L., Wang H., Zhou L., Yu D. Akt-FOXO3a signaling axis dysregulation in human oral squamous cell carcinoma and potent efficacy of FOXO3a-targeted gene therapy. Oral Oncol. 2011;47:16–21. doi: 10.1016/j.oraloncology.2010.10.010. [DOI] [PubMed] [Google Scholar]
- 92.Jin C., Jin Y., Wennerberg J., Annertz K., Enoksson J., Mertens F. Cytogenetic abnormalities in 106 oral squamous cell carcinomas. Cancer Genet. Cytogenet. 2006;164:44–53. doi: 10.1016/j.cancergencyto.2005.06.008. [DOI] [PubMed] [Google Scholar]
- 93.Prapinjumrune C., Morita K., Kuribayashi Y., Hanabata Y., Shi Q., Nakajima Y. DNA amplification and expression of FADD in oral squamous cell carcinoma. J. Oral Pathol. 2010;39:525–532. doi: 10.1111/j.1600-0714.2009.00847.x. [DOI] [PubMed] [Google Scholar]
- 94.Xia J., Chen Q., Li B., Zeng X. Amplifications of TAOS1 and EMS1 genes in oral carcinogenesis: association with clinicopathological features. Oral Oncol. 2007;43:508–514. doi: 10.1016/j.oraloncology.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 95.Jiang L., Zeng X., Yang H., Wang Z., Shen J., Bai J. Oral cancer overexpressed 1 (ORAOV1): a regulator for the cell growth and tumor angiogenesis in oral squamous cell carcinoma. Int. J. Cancer. 2008;123:1779–1786. doi: 10.1002/ijc.23734. [DOI] [PubMed] [Google Scholar]
- 96.Su S.C., Lin C.W., Liu Y.F., Fan W.L., Chen M.K., Yu C.P. Exome sequencing of oral squamous cell carcinoma reveals molecular subgroups and novel therapeutic opportunities. Theranostics. 2017;7:1088–1099. doi: 10.7150/thno.18551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Livingstone L.R., White A., Sprouse J., Livanos E., Jacks T., Tlsty T.D. Altered cell cycle arrest and gene amplification potential accompany loss of wild-type p53. Cell. 1992;70:923–935. doi: 10.1016/0092-8674(92)90243-6. [DOI] [PubMed] [Google Scholar]
- 98.Maitra A., Biswas N.K., Amin K., Kowtal P., Kumar S., Das S. Mutational landscape of gingivo-buccal oral squamous cell carcinoma reveals new recurrently-mutated genes and molecular subgroups. Nat. Commun. 2013;4:2873. doi: 10.1038/ncomms3873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Zhou X., Temam S., Oh M., Pungpravat N., Huang B.L., Mao L. Global expression-based classification of lymph node metastasis and extracapsular spread of oral tongue squamous cell carcinoma. Neoplasia. 2006;8:925–932. doi: 10.1593/neo.06430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Martín-Ezquerra G., Salgado R., Toll A., Gilaberte M., Baró T., Alameda Quitllet F. Multiple genetic copy number alterations in oral squamous cell carcinoma: study of MYC,TP53, CCDN1, EGFR and ERBB2 status in primary and metastatic tumours. Br. J. Dermatol. 2010;163:1028–1035. doi: 10.1111/j.1365-2133.2010.09947.x. [DOI] [PubMed] [Google Scholar]
- 101.Pathare S.M., Gerstung M., Beerenwinkel N., Schäffer A.A., Kannan S., Pai P. Clinicopathological and prognostic implications of genetic alterations in oral cancers. Oncol. Lett. 2011;2:445–451. doi: 10.3892/ol.2011.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Cervigne N.K., Machado J., Goswami R.S., Sadikovic B., Bradley G., Perez-Ordonez B. Recurrent genomic alterations in sequential progressive leukoplakia and oral cancer:drivers of oral tumorigenesis? Hum. Mol. Genet. 2014;23:2618–2628. doi: 10.1093/hmg/ddt657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Freier K., Knoepfle K., Flechtenmacher C., Pungs S., Devens F., Toedt G. Recurrent copy number gain of transcription factor SOX2 and corresponding high protein expression in oral squamous cell carcinoma. Genes Chromosomes Cancer. 2010;49:9–16. doi: 10.1002/gcc.20714. [DOI] [PubMed] [Google Scholar]
- 104.Chen Y.J., Lin S.C., Kao T., Chang C.S., Hong P.S., Shieh T.M. Genome-wide profiling of oral squamous cell carcinoma. J. Pathol. 2004;204:326–332. doi: 10.1002/path.1640. [DOI] [PubMed] [Google Scholar]
- 105.Klussmann J.P., Mooren J.J., Lehnen M., Claessen S.M., Stenner M., Huebbers C.U. Genetic signatures of HPV-related and unrelated oropharyngeal carcinoma and their prognostic implications. Clin. Cancer Res. 2009;15:1779–1786. doi: 10.1158/1078-0432.CCR-08-1463. [DOI] [PubMed] [Google Scholar]
- 106.Hübbers C.U., Akgül B. HPV and cancer of the oral cavity. Virulence. 2015;6:244–248. doi: 10.1080/21505594.2014.999570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Chi A.C., Day T.A., Neville B.W. Oral cavity and oropharyngeal squamous cell carcinoma-an update. CA Cancer J. Clin. 2015;65:401–421. doi: 10.3322/caac.21293. [DOI] [PubMed] [Google Scholar]
- 108.Rivera C. Essentials of oral cancer. Int. J. Clin. Exp. Pathol. 2015;8:11884–11894. eCollection 2015. [PMC free article] [PubMed] [Google Scholar]
- 109.Rivera C. Opportunities for biomarkers with potential clinical use in oral cancer. Medwave. 2015;15 doi: 10.5867/medwave.2015.06.6186. [DOI] [PubMed] [Google Scholar]
- 110.Bavle R.M., Venugopal R., Konda P., Muniswamappa S., Makarla S. Molecular classification of oral squamous cell carcinoma. J. Clin. Diagn. Res. 2016;10:18–21. doi: 10.7860/JCDR/2016/19967.8565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Rivera C., Venegas B. Histological and molecular aspects of oral squamous cell carcinoma (Review) Oncol. Lett. 2014;8:7–11. doi: 10.3892/ol.2014.2103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Hendry S., Salgado R., Gevaert T., Russell P.A., John T., Thapa B. Assessing tumor-infiltrating lymphocytes in solid tumors: a practical review for pathologists and proposal for a standardized method from the international immuno-oncology biomarkers working group: part 2: TILs in melanoma, gastrointestinal tract carcinomas, non-small cell lung carcinoma and mesothelioma, endometrial and ovarian carcinomas, squamous cell carcinoma of the head and neck, genitourinary carcinomas, and primary brain tumors. Adv. Anat. Pathol. 2017;24:311–335. doi: 10.1097/PAP.0000000000000161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Gao J., Tian G., Han X., Zhu Q. Twenty-four signature genes predict the prognosis of oral squamous cell carcinoma with high accuracy and repeatability. Mol. Med. Rep. 2018;17:2982–2990. doi: 10.3892/mmr.2017.8256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Aptsiauri N., Cabrera T., Mendez R., Garcia-Lora A., Ruiz-Cabello F., Garrido F. Role of altered expression of class I MHC molecules in cancer progression. Adv. Exp. Med. Biol. 2007;601:123–131. doi: 10.1007/978-0-387-72005-0_13. [DOI] [PubMed] [Google Scholar]
- 115.Chang C.C., Campoli M., Ferrone S. Classical and nonclassical HLA class I changes in malignant cells: current challenges and future directions. Adv. Cancer Res. 2005;93:189–234. doi: 10.1016/S0065-230X(05)93006-6. [DOI] [PubMed] [Google Scholar]
- 116.van der Bruggen P., Traversari C., Chomez P., Lurquin C., De Plaen E., Van den Eynde B. A gene encoding an antigen recognized by cytolytic T lymphocytes on a human melanoma. Science. 1991;254:1643–1647. doi: 10.1126/science.1840703. [DOI] [PubMed] [Google Scholar]
- 117.Garrido F., Cabrera T., Aptsiauri N. “Hard” and “soft” lesions underlying the HLA class I alterations in cancer cells: implications for immunotherapy. Int. J. Cancer. 2010;127:249–256. doi: 10.1002/ijc.25270. [DOI] [PubMed] [Google Scholar]
- 118.Carretero R., Wang E., Rodriguez A.I., Reinboth J., Ascierto M.L., Engle A.M., Liu H., Camacho F.M., Marincola F.M., Garrido F., Cabrera T. Regression of melanoma metastases after immunotherapy is associated with activation of antigen presentation and interferon-mediated rejection genes. Int. J. Cancer. 2012;131:387–395. doi: 10.1002/ijc.26471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Maleno I., Aptsiauri N., Cabrera T., Gallego A., Paschen A., López-Nevot M.A. Frequent loss of heterozygosity in the β2-microglobulin region of chromosome 15 in primary human tumors. Immunogenetics. 2011;63:65–71. doi: 10.1007/s00251-010-0494-4. [DOI] [PubMed] [Google Scholar]
- 120.Budczies J., Denkert C., Győrffy B., Schirmacher P., Stenzinger A. Chromosome 9p copy number gains involving PD-L1 are associated with a specific proliferation and immune-modulating gene expression program active across major cancer types. BMC Med. Genom. 2017;10:74. doi: 10.1186/s12920-017-0308-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Comprehensive molecular characterization of gastric adenocarcinoma. Nature. 2014;513:202–209. doi: 10.1038/nature13480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Green M.R., Monti S., Rodig S.J., Juszczynski P., Currie T., O’Donnell E. Integrative analysis reveals selective 9p24.1 amplification, increased PD-1 ligand expression, and further induction via JAK2 in nodular sclerosing Hodgkin lymphoma and primary mediastinal large B-cell lymphoma. Blood. 2010;116:3268–3277. doi: 10.1182/blood-2010-05-282780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Barrett M.T., Anderson K.S., Lenkiewicz E., Andreozzi M., Cunliffe H.E., Klassen C.L. Genomic amplification of 9p24.1 targeting JAK2, PD-L1, and PD-L2 is enriched in high-risk triple negative breast cancer. Oncotarget. 2015;6:26483–26493. doi: 10.18632/oncotarget.4494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Chen M., Pockaj B., Andreozzi M., Barrett M.T., Krishna S., Eaton S. JAK2 and PD-L1 amplification enhance the dynamic expression of PD-L1 in triple-negative breast cancer. Clin. Breast Cancer. 2018;18:e1205–e1215. doi: 10.1016/j.clbc.2018.05.006. [DOI] [PubMed] [Google Scholar]
- 125.Ansell S.M., Lesokhin A.M., Borrello I., Halwani A., Scott E.C., Gutierrez M. PD-1 blockade with nivolumab in relapsed or refractory Hodgkin's lymphoma. N. Engl. J. Med. 2015;372:311–319. doi: 10.1056/NEJMoa1411087. [DOI] [PMC free article] [PubMed] [Google Scholar]