Abstract
Hawai‘i has the lowest rate of community water fluoridation in the nation, which has contributed to poor oral health for children statewide. When properly prescribed, the benefits of fluoride supplementation for oral health outweigh any potential side effects to the body. Official recommendations give pediatric healthcare providers the authority to prescribe fluoride supplements and guide parents in daily usage. However, knowledge of actual practice and adherence for both providers and patients have never been examined in Hawai‘i. This study aims to evaluate pediatric healthcare providers' attitudes, knowledge, and practices, regarding fluoride supplementation. A 37-item survey was developed investigating these domains, and was distributed to pediatric dentists, family practitioners, and pediatricians in the state. One hundred and three responses were collected during the time period of May 2014 through May 2015. Descriptive and bivariate associations with several outcomes were assessed. The majority (87%) reported at least some knowledge of the official guidelines. There was uncertainty in knowledge of fluorosis and the seriousness of the health risk. A recent educational session on fluoride was associated with more knowledge of the guidelines and the signs and symptoms of fluorosis. The majority of providers started fluoride at the recommended age whereas there was more variablility on stopping fluoride. On the patient side, providers reported that 67% of the parents forget to administer and 53% reported that their child does not like the taste. This study provides some information regarding the clinical use of fluoride supplementation in children. More efforts are needed to raise awareness in a consistent manner by both the dental and medical communities on the importance of fluoride supplementation to promote oral health in children while addressing concerns of professionals and the community.
Introduction
The effects of dental caries on the overall health and wellbeing of children are still being identified. Evidence points to a sharp decline in quality of life for children with caries,1,2 as well as a potential for adversely affecting the child's academic success with an increase in school absenteeism and decrease academic performance.3,4 Caries commonly present with pain and discomfort but cause more serious sequelae as well, including abscesses, granulomas, or suppurating lesions.5 Depending on the virulence of the organism(s) and/or delay in proper treatment, osteomyelitis, cellulitis, and/or septic thrombophlebitis could also result.5
Fluoride prevents oral caries in children when administered at optimal levels.6–9 These optimal levels can be reached through a variety of sources including community water flouridations, fluoridated toothpaste, fluoride varnishes, fluoride rinses, and dietary fluoride supplements, all of which should be considered in clinical recommendations.10 Incorporation of the element into the tooth enamel and dentin forms fluorohydroxyapatite, which is more resistant to the acidic conditions that precipitate dental caries.11 In 2014, 74.4% of United States (U.S.) citizens on community water systems, received fluoridated water,12 a cost-effective method of improving oral health and one of the greatest public health achievements of the past century.13–15
In the State of Hawai‘i, community water fluoridation has been controversial. As of 2014, the state remains last in the U.S. in water fluoridation availability at 11.7% of the population — predominantly found in federally governed military installations.16–19 Additionally, efforts to increase fluoridation in Hawai‘i have been met with considerable community resistance. Moloka‘i, Lana‘i, O‘ahu, the State Senate, and the State House of Representatives have all rejected fluoridation proposals, despite vocal support from agencies and organizations including the Dental Health Division of the Hawai‘i State Department of Health (DOH), the Hawai‘i Chapter of the American Academy of Pediatrics (AAP), the Hawai‘i Dental Association, the Hawai‘i Medical Service Association, and the Centers for Disease Control and Prevention.20–24 A review of the online archives of The Honolulu Advertiser (records available from March 15th, 2001 to June 6th, 2010) and The Honolulu Star-Bulletin (March 18th, 1996 to June 6th, 2010) reveal dozens of editorials expressing negative opinions on systemic fluoridation in Hawai‘i. Fluoride was misrepresented as “medication,” a “pollutant,” “toxic,” “highly corrosive,” and causing “negative health effects.”22,25–29 Even some members of the healthcare community have voiced their opposition.20, 30–32 Many dissenters cite “good dental hygiene” as the most important method of preventing dental caries, while pointing to the “pure and sacred” nature of Hawaii's water supply in its current condition.33,34 As a result, school-aged children in Hawai‘i have disproportionately higher rates of dental caries when compared with their peers on the mainland.35 The Pew Center gave Hawai‘i a failing grade in 2011 for not meeting seven out of eight policy benchmarks aimed at improving children's dental health.36 The State's 2014–2015 data from a screening survey done among third grade children revealed a 70.6% rate (last among the 47 reporting states, the national average being 52%) of tooth decay in third graders with significant disparities found among low income, Micronesian, and Native Hawaiian populations.37
In the absence of community water fluoridation, the responsibility for providing fluoride to children falls to pediatric healthcare providers including both dental and medical providers. Dietary supplements delivering systemic fluoride in the form of tablets, drops, or lozenges have been shown to safely and effectively prevent dental caries in children, particularly in their permanent teeth.38 Recommendations endorsed by the AAP, American Dental Association, American Academy of Pediatric Dentistry (AAPD), and American Academy of Family Physicians (AAFP), advise their usage from six months of age to 16 years with dosages adjusted according to the presence of other sources of fluoride in the child's lifestyle, such as in infant waters, fluoride varnish, fluoridated toothpaste or rinses, or in naturally occurring mineral fluoride.10,39–41
The practice and adherence to supplementation guidelines for both providers and patients have not previously been reported in Hawai‘i. Thus, the purpose of this study was to assess attitudes towards pediatric oral fluoride supplementation, knowledge levels and gaps, prescribing habits, and clinician assessments of patient concerns among healthcare providers.
Methods
A preliminary cross-sectional survey was developed by the authors, which included representation from community pediatricians, epidemiology, public health, and pediatric oral health. The electronic survey was peer reviewed by non-author specialists in family medicine, pediatrics, and pediatric dentistry to ensure clarity, resulting in a final 37-item questionnaire. Information on the first page of the electronic survey included: a description of the study; aims of the study; voluntary nature of the survey; assurance that answers would remain confidential and anonymous; and included contact information for questions or concerns. The survey included sections on the recommended fluoride prescribing guidelines, provider prescribing practices, awareness of health impacts of fluoride supplementation, provider awareness of patient use and attitudes towards supplementation, and general demographics of providers and their practices. Two items were free-text response sections allowing participants to provide suggestions “to improve fluoride supplementation rates and awareness in Hawai‘i” as well as other feedback. The study received exempt status from the University of Hawai‘i Committee on Human Subjects and Hawai‘i State DOH Institutional Review Boards.
Awareness of the current ADA recommendations for daily fluoride supplementation was assessed through the question “Do you know the current ADA recommendations for daily fluoride supplementation” with options of “Yes,” “No,” and “I have some knowledge.” Fluorosis as a potential barrier to recommending supplementation was assessed by two questions: Knowledge of the fluorosis was asked with “Do you know the signs and symptoms of fluorosis?” with “Yes,” “Somewhat,” and “No” as possible responses and “Do you think that fluorosis poses a serious health risk in general?” with “Yes,” “No,” and “Unsure” as possible responses. To assess recent education on fluoride, providers were asked if they had attended an educational session on fluoride supplementation and/or oral health education which included fluoride supplementation in the past 5 years.
Prescribing habits were assessed by the question: “Do you prescribe or recommend fluoride supplements to your patients?” with options of “Yes” or “No.” To check knowledge, providers were then asked about the age they started and stopped recommending fluoride with options of “Birth to 6 months,” “6 months to 3 years,” “3 years to 6 years,” “6 years to 16 years,” “After 16 years,” and “I do not recommend fluoride supplementations to any of my patients.” Starting at the age range of “6 months to 3 years” and stopping “After 16 years” were considered the appropriate times for knowledge of the recommendations.
Patient concerns were addressed by the question “How often do patients ask you about fluoridation concerns?” with options of “Never (0% of visits),” “Rarely (1–24% of visits),” “Sometimes (25–49% of visits),” “Often (50–74% of visits),” “Almost Always (75–99% of visits),” and “Always (100% of visits).” These responses were grouped in pairs and categorized as Rarely/Never, Occasionally, and Frequently/Always. Perceived barriers were assessed by the question “If applicable, what issues do your patients raise about fluoride supplementation?” (choose all that apply: conflicting advice when another healthcare provider said not to use, side effects, child does not like taste, cost, and forget to administer).
The questionnaire also elicited provider characteristics for analysis and included: area of training (dentistry, family medicine, pediatrics), year(s) since training completion, main clinical practice type (community health center, military, private practice of 1–2 person(s), private practice of 3+ persons, ‘other’—which included health maintenance organizations, private hospitals, and residency clinics), and practice location which was grouped as O‘ahu or Neighbor Island (Big Island, Kaua‘i, Maui, Moloka‘i, and Lana‘i) due to small numbers of respondents serving neighbor islands. Also, included in the questionnaire were: provider gender, location of training, main type of insurance seen in practice, years of practice in Hawai‘i average number of pediatric patients per week (1–25, 26–50, 51–75, 76+), and number of caries cases diagnosed in the past 30 days (quartiles).
The survey was administered through the Hawai‘i Chapters of the AAP, AAFP, and AAPD with an electronic link to the survey, hosted on Google Forms. The survey was initially distributed to pediatricians (n=250); followed by pediatric dentists (n=34), and then family physicians (n=326). To improve response rates, a reminder was sent 30 days after initial contact to each group. In all, 49 pediatricians, 20 pediatric dentists, and 34 family practitioners inputted valid responses, for a total n=103. Excluded from the study were answers from subspecialists not providing primary care (n=1), adult-only providers (n=1), and inactive providers (n=1).
Descriptive and bivariate analysis between outcomes and characteristics were completed. Measures of associations were based on chi-square testing with all analyses conducted at a significance level (P< .05). All analyses were done with SAS, version 9.4 (SAS Institute, Inc, Cary, North Carolina).
Results
The overall survey response rate was 16.9% (103/610). Nearly 1 in 5 respondents were dentists, 1 in 3 were family medicine, and nearly 1 in 2 were pediatricians (Table 1). Nearly 1 in 4 had been in practice 25 or more years. Private practice of any size was the largest group in the sample at 43%, followed by community health centers and ‘other’—both at 22%. More than 8 out of 10 practiced on O‘ahu. About 2 in 3 reported not having attended an educational session on fluoride in the last 5 years. The most common insurance seen in the practice among respondents was Medicaid/QUEST (51%), followed by private insurance (36%) and military/Tricare plans (13%). About half of the respondents were female. About 1 in 3 reported seeing 0–1 caries in the past 30 days (31%) and nearly 1 in 3 reported more than 20 cases in the past 30 days. A large proportion of respondents saw only 1–25 pediatric patients per week (41%) whereas over a quarter (28%) saw more than 75 pediatric patients per week.
Table 1.
Characteristics of Respondents (N=103) in Fluoride Supplementation Survey
| n | Percent (%) | |
| Specialty | ||
| Dentistry | 20 | 19 |
| Family Medicine | 34 | 33 |
| Pediatrics | 49 | 48 |
| Number of Years Since Training Completion | ||
| Trainee to 6 years | 26 | 25 |
| 7–14 years | 27 | 26 |
| 15–24 years | 26 | 25 |
| 25+ years | 24 | 23 |
| Practice Type | ||
| Community Health Center | 23 | 22 |
| Military | 13 | 13 |
| Private Practice (1–2) | 29 | 28 |
| Private Practice (3+) | 15 | 15 |
| Other | 23 | 22 |
| Practice Location | ||
| O‘ahu | 88 | 85 |
| Neighbor Island | 15 | 15 |
| Educational Session | ||
| Yes | 36 | 35 |
| No | 67 | 65 |
| Main Patient Insurer | ||
| Medicaid/QUEST | 52 | 51 |
| Private | 37 | 36 |
| Military/Tricare | 13 | 13 |
| Uninsured | 1 | 1 |
| Number of Years of Practice in Hawai‘i | ||
| 0 to 3 years | 24 | 23 |
| 4–9 years | 25 | 24 |
| 10–17 years | 28 | 27 |
| 18+ years | 26 | 25 |
| Gender | ||
| Female | 52 | 51 |
| Male | 51 | 50 |
| Number of Caries Cases in Last 30 Days | ||
| 0 to 1 case | 32 | 31 |
| 2–5 cases | 26 | 25 |
| 6–20 cases | 20 | 19 |
| 21+ cases | 29 | 28 |
| Average Number of Pediatric Patients Per Week | ||
| 1–25 patients | 42 | 41 |
| 26–50 patients | 22 | 21 |
| 51–75 patients | 10 | 10 |
| 76+ patients | 29 | 28 |
| Total | 103 | 100 |
Note: percentage totals may not sum to 100 based on rounding.
Overall, 72% of respondents reported knowing the current ADA fluoride supplementation guidelines and 16% reported some knowledge of the fluoride guidelines (Table 2). All dentists reported at least some knowledge of the recommendations with 95% reporting they knew the recommendations and 5% reporting some knowledge of the recommendations. Nearly 80% of family medicine providers reported at least some knowledge of the guidelines (53% reported knowing and 27% reported some knowledge). Nearly 90% of pediatric medical providers reported at least some knowledge of the guidelines (76% reported knowing and 12% reported some knowledge). Nearly all providers recommended fluoride (97%; n=100; Figure 1). Of the 100 respondents that recommended fluoride, almost all (95%) reported starting between 6 months and 3 years of age (Figure 1). Information on age to stop recommending fluoride was available for 90 respodents with 60% stopping after 16 years of age, 37% between 6 and 16 years of age, and 3% between 3 and 6 years of age.
Table 2.
Fluoride Supplementation Knowledge and Educational Session Attendance by Selected Characteristics
| Do you know the current ADA recommendations for daily fluoride supplementation? (N=103) | Have you attended an educational session on fluoride supplementation in the past 5 years? (N=103) | ||||||
| Characteristics | Yes Percent (%) | Some Knowledge Percent (%) | No Percent (%) | P-value | Yes Percent (%) | No Percent (%) | P-value |
| Specialty | |||||||
| Dentistry | 95 | 5 | 0 | .21 | 65 | 35 | .001 |
| Family Medicine | 53 | 27 | 21 | 29 | 71 | ||
| Pediatrics | 76 | 12 | 12 | 27 | 75 | ||
| Number of Years Since Training Completion | |||||||
| Trainee to 6 years | 77 | 19 | 4 | .81 | 46 | 54 | .45 |
| 7–14 years | 56 | 15 | 30 | 26 | 74 | ||
| 15–24 years | 77 | 15 | 8 | 31 | 69 | ||
| 25+ years | 79 | 13 | 8 | 38 | 63 | ||
| Practice Type | |||||||
| Community Health Center | 74 | 13 | 13 | .89 | 44 | 57 | .87 |
| Military | 54 | 8 | 9 | 39 | 62 | ||
| Private Practice (1–2) | 86 | 14 | 0 | 31 | 69 | ||
| Private Practice (3+) | 67 | 20 | 13 | 33 | 67 | ||
| Other | 65 | 22 | 13 | 30 | 70 | ||
| Practice Location | |||||||
| O‘ahu | 69 | 16 | 15 | .35 | 33 | 14 | .30 |
| Neighbor Island | 87 | 13 | 0 | 47 | 53 | ||
| Educational Session | |||||||
| Yes | 92 | 8 | 0 | .003 | — | — | — |
| No | 61 | 19 | 19 | — | — | ||
| Total | 72 | 16 | 13 | 35 | 65 | ||
Figure 1.
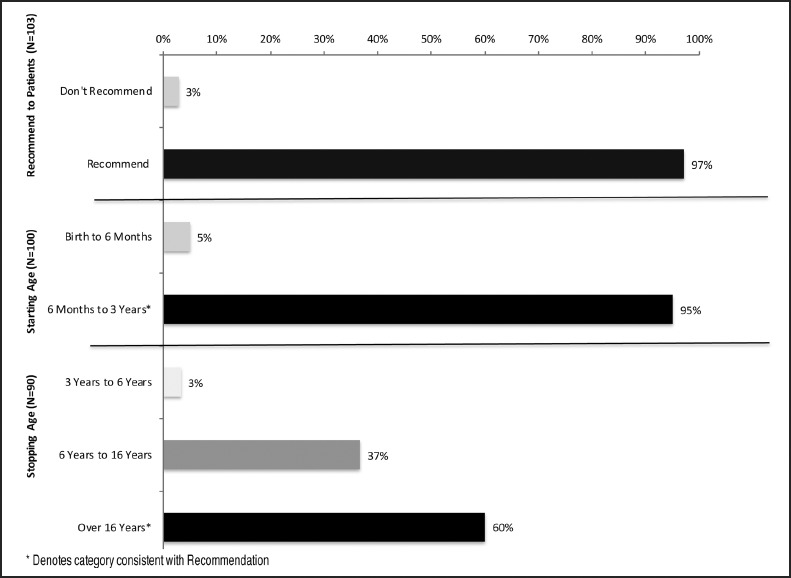
Percent of Providers Recommending Fluoride Supplementation and Associated Start and Stop Ages
Overall, 35% of respondents reported having attended an educational session on fluoride in the past 5 years (Table 2). Nearly two-thirds of dentists (65%) reported attendance compared to less than a third of those in the family medicine (29%) and pediatric medical providers (27%). Of those who had an educational session on fluoride in the past 5 years, 92% reported knowing and 8% reported some knowledge of the recommendations compared with about 80% of those who had not attended a session (61% reported knowing and 19% reported some knowledge).
Ninety-five percent of providers reported at least some knowledge of the signs and symptoms of fluorosis versus 5% who reported no knowledge (Table 3). This varied, with nearly all (93%) neighbor island providers reporting knowing compared to just 56% of O‘ahu providers. Those who had attended a recent educational session on fluoride were more likely to report knowledge (81%) compared to those who had not attended a session (51%). Concerning whether providers perceived fluorosis to be a serious health risk, 27% of family medicine and 16% of pediatric medical providers reported being unsure on the risk. Similarly, 29% of family medicine providers reported fluorosis as a serious health risk compared to 18% of pediatric and 15% of dentists.
Table 3.
Knowledge and Perceived Health Risk of Fluorosis by Selected Characteristics
| Knowledge of Fluorosis (N=103) | Think Fluorosis is a Serious Health Risk (N=103) | |||||||
| Characteristics | Yes Percent (%) | Somewhat Percent (%) | No Percent (%) | P-value | Yes Percent (%) | No Percent (%) | Unsure Percent (%) | P-value |
| Specialty | ||||||||
| Dentistry | 95 | 5 | 0 | .006 | 15 | 85 | 0 | .03 |
| Family Medicine | 59 | 32 | 9 | 29 | 44 | 27 | ||
| Pediatrics | 49 | 47 | 4 | 18 | 65 | 16 | ||
| Number of Years Since Training Completion | ||||||||
| Trainee to 6 years | 46 | 46 | 8 | .17 | 31 | 46 | 23 | .20 |
| 7–14 years | 52 | 41 | 7 | 22 | 56 | 22 | ||
| 15–24 years | 65 | 32 | 4 | 19 | 65 | 15 | ||
| 25+ years | 83 | 17 | 0 | 13 | 83 | 4 | ||
| Practice Type | ||||||||
| Community Health Center | 48 | 48 | 4 | .07 | 30 | 44 | 26 | .01 |
| Military | 77 | 23 | 0 | 39 | 54 | 8 | ||
| Private Practice (1–2) | 66 | 35 | 0 | 10 | 86 | 4 | ||
| Private Practice (3+) | 60 | 40 | 0 | 27 | 67 | 7 | ||
| Other | 61 | 22 | 9 | 13 | 52 | 35 | ||
| Practice Location | ||||||||
| O‘ahu | 56 | 39 | 6 | .02 | 23 | 59 | 18 | .29 |
| Neighbor Island | 93 | 7 | 0 | 13 | 80 | 7 | ||
| Educational Session | ||||||||
| Yes | 81 | 17 | 3 | .01 | 19 | 72 | 8 | .20 |
| No | 51 | 43 | 6 | 22 | 57 | 21 | ||
| Total | 61 | 34 | 5 | 21 | 62 | 17 | ||
Most providers (67%) reported rarely/never being asked about fluoride supplementation by their patients and only 14% reported being asked by patients frequently/always (Figure 2). About half of providers stated that their patients across all age groups were taking fluoride ‘regularly’, with about a quarter taking it ‘sometimes’, and a quarter ‘not taking’ fluoride at all (data not shown). The most common barriers to fluoride supplement use as reported by providers about their patients were parent forgetfulness (67%), followed by taste issues (53%) and potential side effects (33%; Figure 3). About a quarter of respondents (23%) reported that their patients were being told by another healthcare provider not to use fluoride.
Figure 2.
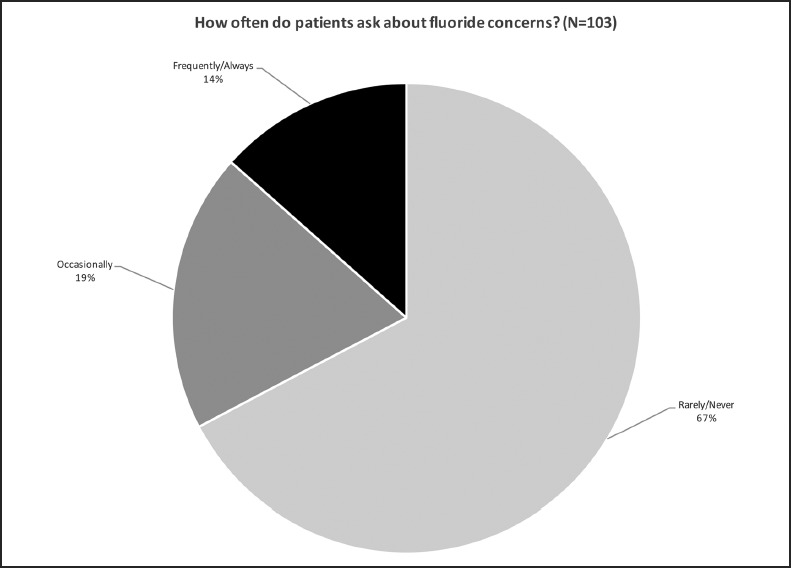
Frequency in which Patients Express Fluoride Concerns as Reported by Providers
Figure 3.
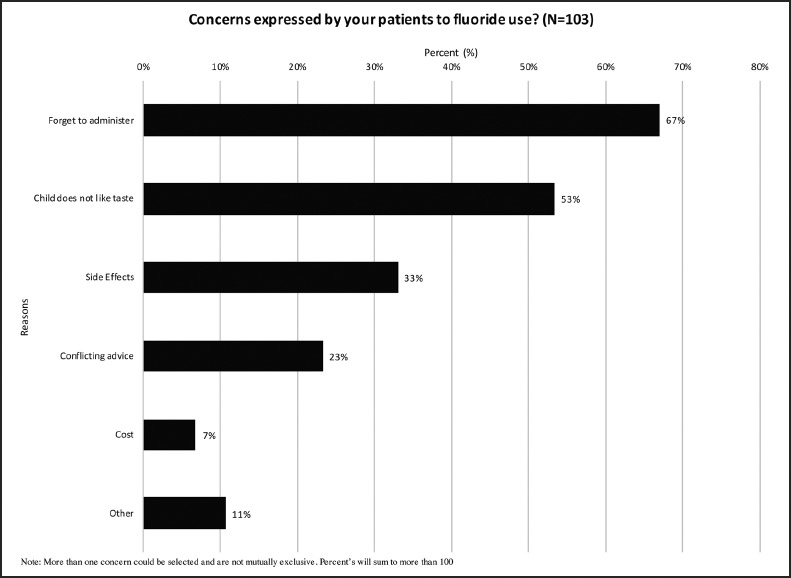
Specific Fluoride Concerns Expressed by Patients as Reported by Providers
Discussion
This study shows that while most pediatric healthcare providers (dental and medical) in Hawai‘i surveyed support and prescribe fluoride supplements, knowledge and clinical practice vary from official recommendations and guidelines. Dentists and medical providers both see children and families early on and collaboration and consistent messaging related to fluoride has the potential to improve the oral health of children.
Primary care providers are more likely to see a child in the first two years of life due to frequent well-child visits and thus have opportunities to discuss fluoride supplementation with parents. Whereas dentists are likely to see a child up to twice a year, once established as a patient, compared to a primary care physician who will typically see a child only once a year after the 24 month well-child visit other than during sick visits. Thus, there is significant overlap and consistent messages across disciplines could minimize confusion and potentially raise adherence and acceptance of fluoride among young children. In this study, pediatric dentists were more likely to report knowing the current ADA recommendations compared to family medicine and pediatric physicians. This could be due to the greater focus on oral health in dentistry training and reinforcement through ongoing training compared to medical training. The lower and uncertain knowledge in pediatricians and family medicine providers could also be due to the different focus of training as well as that they were less likely to have attended a recent education session on fluoride compared to dentists. Fortunately, there are several online sources of education and recommendations on oral health including those from AAP and AAFP that can be accessed and provide additional guidance and training on oral health for medical providers.42, 43
Knowledge of the guidelines was further assessed by looking at recommended start and stop times in the survey. Unfortunately, interpretation is severly limited due to broad ranges listed in the survey instrument but does grossly represent a high agreement for the likely age to start fluoride supplements after 6 months. There was more variability in stopping with 40% recommending stopping before 16 years of age which represents an area where further education could provide clearer recommendations on age of stopping. However, a more refined range of start/stop years would better characterize knowledge of the guidelines. Pediatric healthcare professionals need to learn about important patient concerns as presented here and be better prepared to counsel on fluoride supplementation and other sources of fluoride. Moreover, further education will hopefully make the issue a more common clinic visit topic, as parental forgetfulness is by far the most-cited reason for patients not taking fluoride. A standardized message—particularly in dosage and age—put forth across provider types will allow for quality oral health care consistent with clinical standards statewide.
This study had several limitations. First, over 80% of surveys sent out did not produce a response, introducing a selection bias that limits the generalizability. It is unclear if those who did not answer the survey would answer in a similar manner, and the very low response rate limits the conclusions. Nonetheless, in the absence of a more focused survey representative of all providers in the state, which would include other health providers caring for young children such as nurse practitioners and physician assistants, this study can help inform the promotion of fluoride supplements in children. Due to the low response rate and small sample numbers, it was necessary to combine all the responses from dentists, pediatric physcians, and family medicine physicians together even though they are very different in their education and timing of contacts with children. In addition, provider assessment of patient concerns may not truly reflect attitudes in the community regarding fluoride supplementation. Lastly, other methods to provide fluoride such as administering fluoride varnish in a primary care setting that has recently been promoted was not included in the survey.10,44,45
To gain some qualitative input into ways to improve fluoride supplementation rates and its awareness in Hawai‘i, a free response section was included at the end of the survey. In total, 42% of the 103 respondents provided input that can inform efforts on places to raise awareness and educate (eg, patient outreach in daycare centers, schools, media outlets, and social media). Of particular interest is that some discussed the ineffective coordination of care between primary care physicians and dentists with regards to fluoride supplements. The literature has supported fluoride supplementation due to its overwhelming benefits to oral health and lack of associated side effects to the body.11–14 This study shows some uncertainty in providers knowing the signs and symptoms of fluorosis and in perceived risk. The medical and dental community can work in partnership to raise awareness in the state so providers are comfortable recommending supplementation and patients are comfortable taking the supplements. For example, standardized training in educational programs and through the membership organizations of the various specialties and collaboration with stakeholders involved in oral health could help promote the use of fluoride by providers and ensure the public hears consistent messages on the safety and benefits of fluoride supplementation in children.
Conclusion
Fluoride supplementation is an integral component of oral health care for children in the State of Hawai‘i. This study provides some information based on those who responded to the survey regarding clinical use of fluoride supplementation in children. More efforts are needed to raise awareness on the importance of fluoride supplementation in a consistent manner in both the dental and medical communities to effectively promote oral health of children in Hawai‘i.
Acknowledgements
We thank Lee Buenconsejo-Lum, MD and Lynn Fujimoto, DMD for their assistance in disseminating this survey.
Conflict of Interest
None of the authors identify a conflict of interest.
References
- 1.Filstrup SL, Briskie D, da Fonseca M, Lawrence L, Wandera A, Inglehart MR. Early childhood caries and quality of life: child and parent perspectives. Pediatr Dent. 2003;25:431–440. [PubMed] [Google Scholar]
- 2.Low W, Tan S, Schwartz S. The effect of severe caries on the quality of life in young children. Pediatric Dent. 1999;21:325–326. [PubMed] [Google Scholar]
- 3.Jackson SL, Vann WF, Jr, Kotch JB, Pahel BT, Lee JY. Impact of poor oral health on children's school attendance and performance. Am J Public Health. 2011;101(10):1900–1906. doi: 10.2105/AJPH.2010.200915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seirawan H, Faust S, Mulligan R. The impact of oral health on the academic performance of disadvantaged children. Am J Public Health. 2012;102(9):1729–1734. doi: 10.2105/AJPH.2011.300478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ryan KJ, Ray CG, Sherris JC, editors. Sherris Medical Microbiology. 5th ed. New York: McGraw-Hill; 2010. [Google Scholar]
- 6.Dean HT, Arnold JFA, Elvove E. Domestic Water and Dental Caries: V. Additional Studies of the Relation of Fluoride Domestic Waters to Dental Caries Experience in 4,425 White Children, Aged 12 to 14 Years, of 13 Cities in 4 States. Public Health Rep. 1942;57(32):1155–1179. [Google Scholar]
- 7.McDonagh MS, Whiting PF, Wilson PM, Sutton AJ, Chestnutt I, Cooper J, Misso K, Bradley M, Treasure E, Kleijnen J. Systematic review of water fluoridation. BMJ. 2000;321(7265):855–859. doi: 10.1136/bmj.321.7265.855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yeung CA. A systematic review of the efficacy and safety of fluoridation. Evid Based Dent. 2008;9(2):39–43. doi: 10.1038/sj.ebd.6400578. [DOI] [PubMed] [Google Scholar]
- 9.Burt BA. The changing patterns of systemic fluoride intake. J Dent Res. 1992;71(5):1228–1237. doi: 10.1177/00220345920710051601. [DOI] [PubMed] [Google Scholar]
- 10.Clark MB, Slayton RL. Fluoride use in caries prevention in the primary care setting. Pediatrics. 2014;134(3):626–633. doi: 10.1542/peds.2014-1699. [DOI] [PubMed] [Google Scholar]
- 11.Buzalaf MA, Pessan JP, Honorio HM, ten Cate JM. Mechanisms of action of fluoride for caries control. Monogr Oral Sci. 2011;22:97–114. doi: 10.1159/000325151. [DOI] [PubMed] [Google Scholar]
- 12.Division of Oral Health, National Center for Chronic Disease Prevention and Health Promotion, author. 2014 Fluoridation Statistics. Community Water Fluoridation. [April 28, 2017]. https://www.cdc.gov/fluoridation/statistics/2014stats.htm.
- 13.Burt BA, editor. Proceedings for the workshop: cost effectiveness of caries prevention in dental public health. J Public Health Dent. 1989;49(5):251–344. [Google Scholar]
- 14.Brown LJ, Beazoglou T, Heffley D. Estimated savings in U.S. dental expenditures, 1979–89. Public Health Rep. 1994;109(2):195–203. [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention (CDC), author Achievements in Public Health, 1900–1999: Fluoridation of Drinking Water to Prevent Dental Caries. MMWR Morb Mortal Wkly Rep. 1999;48(41):933–940. [Google Scholar]
- 16.Conger J. Fluoridation at DoD Owned or Operated Potable Water Treatment Plants. Department of Defense; 2013. Mar 18, [September 10, 2014]. http://www.ilikemyteeth.org/wp-content/uploads/2013/05/DoD-Fluoridation-Memo-March-2013.pdf. [Google Scholar]
- 17.Board of Water Supply, City and County of Honolulu, author. Water Quality FAQ. Board of Water Supply. [December 20, 2014]. http://www.boardofwatersupply.com/cssweb/display.cfm?sid=1163.
- 18.U.S. Army Garrison-Hawaii, author. Drinking Water. U.S. Army Garrison-Hawaii, Sustainability and Environmental Management. [December 22, 2015]. www.garrison.hawaii.army.mil/sustainability/DrinkingWater.aspx#PrgrmDocs. Updated July 1, 2015.
- 19.Division of Oral Health, National Center for Chronic Disease Prevention and Health Promotion, author. 2010 Water Fluoridation Statistics. Community Water Fluoridation. [November 10, 2014]. http://www.cdc.gov/fluoridation/statistics/20 10stats.htm. Updated May 11, 2011.
- 20.Hurley T. Lana'i dentist wary of plan to fluoridate. [November 10, 2014];The Honolulu Advertiser. 2001 Aug 16; http://the.honoluluadvertiser.com/article/2001/Aug/16/ln/ln32a.html. [Google Scholar]
- 21.Kubota GT. Lanai drinking water will not be fluoridated. Honolulu Star-Bulletin. 2002. Jan 12, [November 10, 2014]. http://archives.starbulletin.com/2002/01/12/news/index5.html.
- 22.Shapiro T. Council vote bans fluoride in water. [November 10, 2014];The Honolulu Advertiser. 2004 Jan 29; http://the.honoluluadvertiser.com/article/2004/Jan/29/ln/ln20a.html. [Google Scholar]
- 23.Omandam P. Fluoridation splits, Hemmeter loses. Honolulu Star-Bulletin. 2000. May 17, [November 10, 2014]. http://archives.starbulletin.com/2000/05/17/news/story3.html.
- 24.Hoover W. Fluoride wording deleted from bill. [November 10, 2014];The Honolulu Advertiser. 2002 Feb 10; http://the.honoluluadvertiser.com/article/2002/Feb/10/ln/ln07a.html. [Google Scholar]
- 25.McCulloch B. European countries join ‘banana republics’. The Honolulu Advertiser. 2004. Feb 13, [November 10, 2014]. http://the.honoluluadvertiser.com/article/2004/Feb/13/op/op12aletters.html.
- 26.Welch V. Lana'i citizens weren't brought in on decision. The Honolulu Advertiser. 2001. Sep 29, [November 10, 2014]. http://the.honoluluadvertiser.com/article/2001/Sep/29/op/op03aletters.html.
- 27.Carvalho G. Good dental hygiene is the only answer. The Honolulu Advertiser. 2001. Jan 20, [November 10, 2014]. http://th e.honoluluadvertiser.com/2001/Jan/20/letters.html.
- 28.Bradford M. Forget fluoridation; make school kids brush. The Honolulu Advertiser. 2002. Feb 8, [November 10, 2014]. http://the.honoluluadvertiser.com/article/2002/Feb/08/op/op03a.html.
- 29.Lehman C. Case studies show downside of fluoride. Honolulu Star-Bulletin. 2000. Feb 22, [November 10, 2014]. http://archives.starbulletin.com/2000/02/22/editorial/letters.html.
- 30.Carlson R. Evidence does not support fluoride use. Honolulu Star-Bulletin. 2001. Nov 26, [November 10, 2014]. http://archives.starbulletin.com/2001/11/26/editorial/letters.html.
- 31.Lao C. Fluoride in water would be wasted. Honolulu Star-Bulletin. 2000. Feb 21, [November 10, 2014]. http://archives.starbulletin.com/2000/02/21/editorial/letters.html.
- 32.Martindale T. Government mustn't mandate fluoridation. Honolulu Star-Bulletin. 2000. Dec 9, [November 10, 2014]. http://archives.starbulletin.com/2000/12/09/editorial/letters.html.
- 33.Altonn H. Health chief makes quiet impact. Honolulu Star-Bulletin. 2003. Mar 6, [November 10, 2014]. http://archives.starbulletin.com/2003/03/06/news/index10.html.
- 34.Terri HK. Let kids drink bottled water with fluoride. Honolulu Star-Bulletin. 2000. Oct 19, [November 10, 2014]. http://archives.starbulletin.com/2000/10/19/editorial/letters.html.
- 35.Greer MH, Tengan SL, Hu KI, Takata JT. Early childhood caries among Hawaii public school children, 1989 vs. 1999. Pac Health Dialog. 2003;10(1):17–22. [PubMed] [Google Scholar]
- 36.Urahn SK, editor. The State of Children's Dental Health: Making Coverage Matter. The Pew Charitable Trusts, Children's Dental Policy. 2011. May 23, [December 22, 2015]. http://www.pewtrusts.org/en/research-and-analysis/ reports/2011/05/23/the-state-of-childrens-dental-health-making-coverage-matter.
- 37.Division of Oral Health, National Center for Chronic Disease Prevention and Health Promotion, author. Explore Oral Health Data by Locations. [April 12, 2016]. http://www.cdc.gov/oralhealthdata/index.html.
- 38.Ismail AI, Hasson H. Fluoride supplements, dental caries and fluorosis: a systematic review. J Am Dent Assoc. 2008;139(11):1457–1468. doi: 10.14219/jada.archive.2008.0071. [DOI] [PubMed] [Google Scholar]
- 39.Rozier RG, Adair S, et al. Evidence-based clinical recommendations on the prescription of dietary fluoride supplements for caries prevention: a report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2010;141(12):1480–1489. doi: 10.14219/jada.archive.2010.0111. [DOI] [PubMed] [Google Scholar]
- 40.American Academy on Pediatric Dentistry, Liaison with Other Groups Committee, author. Guideline on fluoride therapy. Pediatr Dent. 2014;37(6):15–16. [Google Scholar]
- 41.American Academy of Family Physicians, author. Dental Caries. Clinical Preventive Service Recommendation. 2014. [December 22, 2015]. http://www.aafp.org/patient-care/clinical-recommendations/all/dental-caries.html.
- 42.American Academy of Pediatricians, author. Section on Oral Health. [May 23, 2018]. https://www.aap.org/en-us/about-the-aap/Committees-Councils-Sections/Oral-Health/Pages/Oral-Health.aspx.
- 43.American Academy of Family Physicians, author. Oral Health. [May 23, 2018]. https://www.aafp.org/patient-care/public-health/oral-health.html.
- 44.Chou R, Cantor A, Zakher B, Mitchell JP, Pappas M. Prevention of Dental Caries in Children Younger Than 5 Years Old: Systematic Review to Update the U.S. Preventive Services Task Force Recommendation [Internet] Rockville (MD): Agency for Healthcare Research and Quality (US); 2014. May, [May 10, 2017]. Available from http://www.ncbi.nlm.nih.gov/books/NBK202090/ [PubMed] [Google Scholar]
- 45.Bader JD, Rozier RG, Lohr KN, Frame PS. Physicians' roles in preventing dental caries in preschool children: a summary of the evidence for the U.S. Preventive Services Task Force. Am J Prev Med. 2004 May;26(4):315–325. doi: 10.1016/j.amepre.2003.12.001. [DOI] [PubMed] [Google Scholar]


