Abstract
Eagle's syndrome (ES) refers to symptomatic elongation of the ossified styloid process. A styloid process greater than 2.5 cm in length should be considered abnormal; however, an elongated styloid process is not sufficient for a diagnosis of ES; only an abnormal styloid process in association with symptoms can confirm the syndrome. In this case report, we discuss a 54-year-old man who has come to our attention with various symptoms: dysphagia to both solids and liquids, difficulty swallowing, neck pain, and a foreign body sensation during bilateral neck rotation and mouth opening. The diagnosis is performed radiologically because conventional radiographs have many potential disadvantages, whereas, computed tomography (CT) scans and reconstructions allow the length and angulation of the styloid process to be measured and the relationship between the elongated styloid processes and adjacent anatomical structures to be evaluated. Moreover, CT allows for differential diagnosis and provides detailed information needed for surgical planning.
Keywords: Eagle's syndrome, Stylalgia, Styloid process, 3D-CT
Introduction
Eagle's syndrome (ES), or stylalgia, is a syndrome due to an elongated ossified styloid process (SP). In 1652, Marchetti reported the first case of elongated ossified SP [1]. In 1872, Weinlechner described the first surgically treated case of painful elongation of the SP [2]. In 1937, Eagle presented 2 cases of pharyngeal discomfort associated with an elongated SP. Eagle primarily described 2 syndromes: classic styloid syndrome after tonsillectomy and stylocarotid syndrome not related to tonsillectomy [3].
The differential diagnosis of ES should include all conditions that may cause cervicofacial pain. Often, the diagnosis is first performed radiologically, followed by clinical palpation of the tonsillar fossa as confirmation. The aim of this case report is to describe an uncommon syndrome in order to assess the role of 3-dimensional computed tomography (3D-CT) in the evaluation of SP length and angulation.
Case report
A 54-year-old man came to our attention with dysphagia (lasting 2 years) to both solids and liquids, difficulty swallowing, pain on both sides of the face, and a foreign body sensation during bilateral neck rotation and mouth opening. He also complained of weight loss (about 8 kg in the last 2 years) and abdominal pain.
The patient denied any surgical or trauma history. He underwent esophageal-gastric and colon endoscopy examination, esophageal manometry, and barium-contrasted radiographic studies that showed the presence of gastric incontinence, primary peristaltic disorders, and some sigmoid diverticula. He also underwent neck ultrasound and videolaryngoscopic examination that did not show any abnormality. Finally, in the absence of symptom relief after medical therapy, the patient underwent a CT scan of the head and neck.
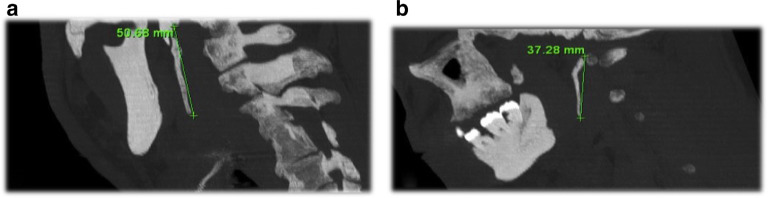
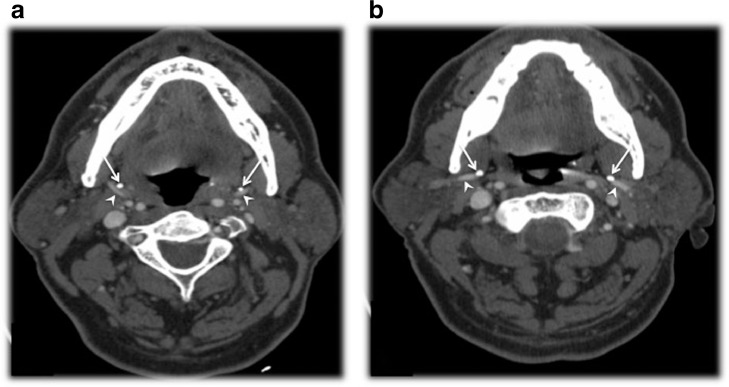
CT examination after intravenous contrast medium administration was performed, with axial, coronal, sagittal, and 3-D volume-rendered reconstructions. The examination showed a bilateral elongation of the SPs. The SPs measured 51 mm on the right side and 37 mm on the left side and presented an anterior angulation (Fig. 1 a-b). The axial images, after intravenous contrast medium administration, showed a contact between the elongated SPs and the internal maxillary arteries (Fig. 2 a-b), causing dysphagia and pain on both sides of the face.
Fig. 1.
(a-b) A 54-year-old man had a 2-year history of dysphagia to both solids and liquids, which made it difficult to swallow. The patient reported neck pain on both sides of the face and a foreign body sensation during neck rotation on both sides and while opening his mouth. CT examination showed a bilateral elongation of the styloid processes, which was less elongated on the left side than on the right. Sagittal planes on the right (A) and left sides (B) and postprocessing MIP reconstruction with bone algorithm are shown. The styloid processes measured 51 and 37 mm on the right and left sides, respectively. The patient underwent resection of the ossified ligament through an extraoral approach and experienced symptom remission.
Fig. 2.
(a-b) CT scan with intravenous injection of iodized contrast made it possible to evaluate the relationship between the elongated styloid processes (white arrows) and the neck vascular structures. Axial slices (a, b) showed that the internal maxillary arteries (white arrowheads) on both sides had been laterally displaced.
Later, a more accurate clinical examination showed palpability of the SPs and pain increasing after palpation. The patient underwent bilateral resection of ossified ligaments under general anaesthesia through an extraoral approach and experienced symptom remission.
Discussion
Embryologically, there are 4 segments of the stylohyoid complex (SP, stylohyoid ligament, lesser cornua of the hyoid, and superior portion of hyoid corpus). These are derived from Reicher's cartilage (second branchial arch), which can be divided into 4 sections based on the subsequent development of the stylohyoid complex. The most proximal, known as the tympanohyaland, gives rise to the tympanic (proximal) portion of the SP as well as the stapes. The second portion is known as the stylohyal and forms the distal portion of the SP. The third portion, the ceratohyal, degenerates in utero, giving rise to the stylohyoid ligament. The fourth and most distal portion is known as the hypohyal and becomes the lesser cornu of the hyoid bone. The SP originates from the temporal bone just medial and anterior to the stylomastoid foramen; it runs anteromedially, with rare anatomic variation in course, and it is delimited on either side by the internal and external branches of the carotid artery. Three muscles (stylopharyngeus, stylohyoid and styloglossus) and 2 ligaments (stylohyoid and stylomandibular) originate from the SP.
Eagle's syndrome is an aggregate of symptoms caused by an elongated ossified SP. SPs greater than 2.5 cm in length should be considered abnormal, but the presence of an elongated SP is not pathognomonic for ES, because many patients with incidental findings of an elongated SP are asymptomatic. ES is a rare entity that is not commonly suspected in clinical practice; in fact, elongation of the SP of the temporal bone occurs in only 4% of the general population [4], [5], but of these, only 4% are symptomatic [6], [7]. The typical patient with an elongated SP is a female between 30 and 50 years old. There is a 3:1 female predominance in ES [8]. This syndrome can occur unilaterally or bilaterally, and the symptoms may include throat pain, dysphagia, odynophagia, dysphasia, otalgia, tinnitus, sensation of a foreign body in the throat, intermittent facial pain, headache, pain on neck rotation, pain on tongue extension, change in voice, clicking upon jaw movement, and a sensation of hypersalivation.
The etiology and pathogenesis of this syndrome are still controversial. Although the actual cause of elongation is poorly understood, several theories have been proposed: (1) congenital elongation of the SP due to persistence of a cartilaginous analogue of the stylohyal, (2) calcification of the stylohyoid ligament by an unknown process, and (3) growth of osseous tissue at the insertion of the stylohyoid ligament [9]. It was suggested that local chronic irritations, surgical trauma, endocrine disorders, and mechanical stress or trauma during development of the SP could result in ossified hyperplasia of the SP. Okabe et al. (2006) found a significant correlation between serum calcium concentration and SP length among 80-year-old subjects [10].
Several pathophysiological mechanisms to explain the symptoms of ES have been proposed: (1) traumatic fracture of the SP causing proliferation of granulation tissue, which determines pressure on the surrounding structures [11]; (2) compression of adjacent nerves, the glossopharyngeal, lower branch of the trigeminal or chorda tympani; (3) degenerative and inflammatory changes in the tendonous portion of the stylohyoid insertion, called insertion tendonitis or “pseudostylohyoid syndrome”; (4) irritation of the pharyngeal mucosa by direct compression or post-tonsillectomy scarring (involves cranial nerves V, VII, IX, and X), and 5) impingement of the arterial vessels producing irritation of the sympathetic nerves in the arterial sheath [9].
Different types of SP mineralization can result in a pathological condition; in the literature there are many classifications systems for SP mineralization [12]. Langlais et al. classify it into 3 types on the basis of radiographic features and patterns of ossification: (1) Elongated – complete mineralization of the SP; (2) Pseudoarticulated – the process is joined to the ossified stylohyoid or stylomandibular ligament; (3) Segmented – the elongated process has multiple interruptions and looks like a segmented mineralized stylohyoid complex. The pathological condition is determined according to these authors by a process length greater than 32 mm [13].
MacDonald Jankowski in their classification considered the centre of calcification involved (tympanohyal, stylohyal, ceratohyal, and hypohyal region) and described 12 different patterns of ossification. Patterns A to D are normal conditions where the process does not extend below the mandibular foramen; pattern E includes an elongated SP that extends below the mandibular foramen; in patterns F to K the process of ossification is segmented and not continuous with the skull base [14].
O'Carroll and Jackson classify SP ossifications into 4 types according to the location of the ossified process: (1) higher than the mandibular foramen (bilateral); (2) on the same level as mandibular foramen (bilateral); (3) lower than mandibular foramen (bilateral); (4) unilateral or having different lengths on the 2 sides [15]. Regarding the last point, Hardy et al. described an unusual unilateral complete ossification of the stylohyoid apparatus, associated with vertebral and laryngeal calcifications [11].
Clinically, the syndrome has been classically categorized into 2 types. The first represents classical ES and is composed of individuals with a former history of tonsillectomy and pain. This pain manifests as neuralgia in the pharynx, odynophagia, and dysphagia. This condition probably results from the organization of fibrotic scar tissue around cranial nerves V, VII, IX, and X [4]. The second group of patients, without history of tonsillectomy, presents pain at the neck and cephalic regions: this condition is known as SP-carotid artery syndrome and is due to impingement of the internal or external carotid artery (or their branches) by a laterally or medially deviated SP. This may be accompanied by referred pain along the distribution of the artery, caused by stimulation of the sympathetic nerve plexus associated with the artery. With lateral deviation and impingement against the external carotid artery, pain can radiate up the face to the level of the eye, whereas with medial deviation and internal carotid impingement, pain will begin in the ophthalmic vessel distribution and radiate back to the occiput. In addition, symptoms related to blood flow interruption within the affected artery, including aphasia, visual symptoms, weakness, and syncope, may occur. Chuang et al. (2007) reported the rare case of a patient who developed left hemispheric ischemia during the 15 seconds in which he turned his head to the left, which completely disappeared on returning the head to the neutral position, without long-term sequelae detected clinically or radiographically [16].
Yavuz et al. (2008) proposed that elongation and abnormal angulation might be responsible for the irritation of a number of structures coursing through the parapharyngeal space. They concluded that anterior angulation of the SP can determine symptoms due to mucosal irritation and high pressure on vital structures in the tonsillar fossa [17]. Camrada et al. (1989) proposed that symptoms similar to stylohyoid syndrome can occur in a nonelongated SP or ossified stylohyoid ligament (absence of radiographic evidence of ossification) due to a tendinosis at the junction of the stylohyoid ligament and the lesser horn of the hyoid bone; they termed this condition “pseudostylohyoid syndrome” [18]. Bareiss et al. (2017) reported the first case of ES apparently resulting from osteoradionecrosis of the SP following head and neck radiation therapy [7].
Often, the diagnosis of SPs is first made radiologically, followed by confirmation by palpation of the tonsillar fossa because, under normal conditions, SP is not palpable [4]. Furthermore, palpation of the tip of the process would exacerbate existing symptoms [5]. After imaging diagnosis of ES and palpation of the lateral tonsillar fossa, the infiltration of local anesthetics allows the final diagnosis to be confirmed.
Various radiological diagnostic criteria are described in the literature. Most authors define a stylohyoid length greater than 2.5 cm as abnormal [8], whereas others suggest 4.0 cm [19]. It is important to keep in mind that the syndrome is not only dependent on the existence of an elongated SP but may occur with an SP of normal length with a deviation of the tip [6,8]. Only the association between symptomatology and demonstration of abnormalities of the SP confirm the syndrome. Since ES is not commonly suspected in clinical practice, the visualization of an elongated SP is often an unusual and incidental finding. In most cases radiographic studies are ordered to seek other possible diseases, which are generally more frequent.
Several imaging modalities have been used for the diagnosis of ES, including lateral head and neck, or anteroposterior head radiography, Towne, or panoramic radiography and lateral-oblique mandible plain film. These conventional radiographs have many potential disadvantages, like the superimposition of several osseous structures (which can cause difficulty viewing the SP, especially if it is not very long) and the impossibility of measuring the definitive SP length. In CT imaging, these disadvantages are eliminated.
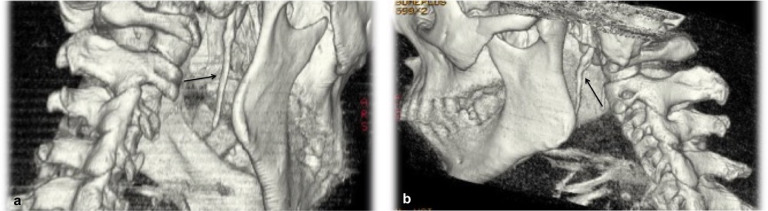
Clinically suspected cases of ES should be studied directly with CT scans, without conventional radiographs, in order to decrease the time to diagnosis of ES. Computed tomography should be performed with thin thickness, preferably submillimetric, with axial, coronal, and sagittal reconstruction images and volume-rendering reconstruction. 3D-CT allows SP length and angulation to be measured and the relationship with nearby anatomical structures to be evaluated (Fig. 3 a-b). CT scans should be performed with intravenous contrast medium administration in order to evaluate the relationship between the elongated SPs and the neck vessels to assess possible vascular compression. In this case, the elongated styloid leads to compression of internal maxillary arteries, the terminal largest branches of the external carotid arteries; these vessels provide a portion of the head vascularization (middle ear, cerebral meninges, dental arches, muscles of the face, mouth pharynx, and temporal muscle), and their terminal branches feed the frontal and maxillary sinuses and nasal septum. CT finally provides detailed information for the surgical plan and eventual excision of the elongated SP through an extraoral or intraoral approach.
Fig. 3.
(a-b) 3D-volume rendering on the right (a) and left (b) sides that show elongated styloid processes (black arrows)
The differential diagnosis of ES should include all conditions possibly causing cervicofacial pain, such as temporomandibular joint diseases; trigeminal, sphenopalatine, or glossopharyngeal neuralgias; temporal arteritis; chronic pharyngotonsillitis; otitis media; external otitis; mastoiditis; dental pain; improperly fitting dental prostheses; submandibular sialadenitis or sialolithiasis; true pharyngeal foreign bodies and tumours of the pharynx or tongue base [18], [20]. In differential diagnosis, we also should consider oesophageal diverticula, cervical vertebral arthritis, hyoid bursitis, Sluder's syndrome, histamine cephalgia, and cluster and migraine type headache [21]. In addition, it is important to exclude cardiovascular and neurological disorders, such as aphasia, syncope, weakness, visual symptoms, or ischemia, associated with interruption of blood flow within the affected vessel in SP-carotid artery syndrome.
The patient in this case is included in the clinical group of patients without a history of tonsillectomy or trauma. CT examination with contrast medium administration and 3-D volume rendered reconstructions demonstrated SP bilateral elongation and medial deviation with impingement of the maxillary arteries. The association of abnormal SPs and related symptoms confirmed ES.
In summary, ES is a rare entity not commonly suspected in clinical practice, whose diagnosis is often first made radiologically. 3D-CT confirms the clinical suspicion and allows the relationship with nearby anatomical structures to be evaluated, providing detailed information for possible surgical planning.
Contributor Information
Giovanni Scavone, Email: gioscavone@hotmail.it.
Daniele Carmelo Caltabiano, Email: daniele.788@gmail.com.
Maria Vittoria Raciti, Email: mariavittoria.raciti@libero.it.
Maria Carla Calcagno, Email: mc.calcagno@gmail.com.
Monica Pennisi, Email: gioscavone81@gmail.com.
Andrea Giovanni Musumeci, Email: musuand@yahoo.it.
Giovanni Carlo Ettorre, Email: gc.ettorre@policlinico.unict.it.
References
- 1.Marchetti P. Anatomia. Patavii. 1652;13:205. [Google Scholar]
- 2.Weinlechner, cited by Kalvin MM. Elongated Styloid processes: their formation and clinical significance. Laryngoscope. 1930;40:907. [Google Scholar]
- 3.Eagle WW. Elongated styloid processes: report of two cases. Arch Otolaryngol. 1937;25:584–587. [Google Scholar]
- 4.Balbuena L, Hayes D, Ramirez SG, Johnson R. Eagle's syndrome (elongated styloid process) South Med J. 1997;90:331–334. doi: 10.1097/00007611-199703000-00014. [DOI] [PubMed] [Google Scholar]
- 5.Okabe S, Morimoto Y, Ansai T. Clinical significance and variation of the advanced calcified stylohyoid complex detected by panoramic radiographs among 80-year-old subjects. Dentomaxillofac Radiol. 2006;35:191–199. doi: 10.1259/dmfr/12056500. [DOI] [PubMed] [Google Scholar]
- 6.Fini G, Gasparini G, Filippini F. The long styloid process syndrome or Eagle's syndrome. J Craniomaxillofac Surg. 2000;28:123. doi: 10.1054/jcms.2000.0128. [DOI] [PubMed] [Google Scholar]
- 7.Prasad KS, Kamath MP, Reddy JM. Elongated styloid process (Eagle's syndrome): a clinical study. J Oral Maxillofac Surg. 2002;60:171. doi: 10.1053/joms.2002.29814. [DOI] [PubMed] [Google Scholar]
- 8.Quereshy FA, Gold ES, Arnold J. Eagle's syndrome in an 11-year-old patient. J Oral Maxillofac Surg. 2001;59:94. doi: 10.1053/joms.2001.19302. [DOI] [PubMed] [Google Scholar]
- 9.Diamond LH, Cottrell DA, Hunter MJ. Eagle's syndrome: A report of 4 patients treated using a modified extraoral approach. J Oral Maxillofac Surg. 2001;59:1420. doi: 10.1053/joms.2001.28276. [DOI] [PubMed] [Google Scholar]
- 10.Ilguy M, Ilguy D, Guler N. Incidence of the type and calcification patterns in patients with elongated styloid process. J Int Med Res. 2005;33(1):96–102. doi: 10.1177/147323000503300110. [DOI] [PubMed] [Google Scholar]
- 11.Balasubramanian S. The ossification of the stylohyoid ligament and its relation to facial pain. Br Dent J. 1964;116:108–111. [Google Scholar]
- 12.Chuang WC, Short JH, McKinney AM, Anker L, Knoll B, McKinney ZJ. Reversible left hemispheric ischemia secondary to carotid compression in eagle syndrome: surgical and CT angiographic correlation. AM J Neuroradiol. 2007;28:143–145. [PMC free article] [PubMed] [Google Scholar]
- 13.Yavuz Y, Caylakli C, Yildirim T, Ozluoglu LN. Angulation of the styloid process in Eagle's syndrome. Eur Arch Otorhinolaryngol. 2008;265:1393–1396. doi: 10.1007/s00405-008-0686-9. [DOI] [PubMed] [Google Scholar]
- 14.Carmada AJ, Deschamps C, Forest D. Stylohyoid chain ossification. A discussion of etiology. Oral Surg Oral Med Oral Pathol. 1989;67:508–514. doi: 10.1016/0030-4220(89)90264-8. [DOI] [PubMed] [Google Scholar]
- 15.Badheya A, Jategaonkara A, Kovacsb AJA, Kadakiaa S, De Deync PP, Ducicd Y. Eagle syndrome: a comprehensive review. Clin Neurol Neurosurg. 2017;159:34–38. doi: 10.1016/j.clineuro.2017.04.021. [DOI] [PubMed] [Google Scholar]
- 16.Ranjan V, Rai S, Misra D, Panjwani S. Eagle's syndrome veiling as pain of odontogenic origin: report of two cases with cone beam computed tomography illustration. Natl J Maxillofac Surg. 2015;6(2):219–223. doi: 10.4103/0975-5950.183863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Langlais RP, Miles DA, Van Dis ML. Elongated and mineralized stylohyoid ligament complex: a proposed classification and report of a case of Eagle's syndrome. Oral Surg Oral Med Oral Pathol. 1986;61:527–532. doi: 10.1016/0030-4220(86)90400-7. [DOI] [PubMed] [Google Scholar]
- 18.MacDonald-Jankowski DS. Calcification of the stylohyoid complex in Londoners and Hong Kong Chinese. Dentomaxillofac Radiol. 2001;30:35–39. doi: 10.1038/sj/dmfr/4600574. [DOI] [PubMed] [Google Scholar]
- 19.Correll RW, Jensen JL, Taylor JB, Rhyne RR. Mineralization of the stylohyoid-stylomandibular ligament complex. A radiographic incidence study. Oral Surg Oral Med Oral Pathol. 1979;48:286–291. doi: 10.1016/0030-4220(79)90025-2. [DOI] [PubMed] [Google Scholar]
- 20.Sivers JE, Johnson GK, Lincoln MS. Diagnosis of Eagle's syndrome. Oral Surg Oral Med Oral Pathol. 1985;59:575. doi: 10.1016/0030-4220(85)90183-5. [DOI] [PubMed] [Google Scholar]
- 21.Harma R. Stylalgia: clinical experiences of 52 cases. Acta Otolaryngol. 1966;224:149. doi: 10.3109/00016486709123570. [DOI] [PubMed] [Google Scholar]