Every human is born with a certain number of nephrons. Assessing that number (i.e., nephron mass) is important because a low nephron mass at birth is a risk factor for hypertension and/or CKD. A reduced number of nephrons leads to hyperfiltration in the remaining ones, increasing intraglomerular pressure and, in the long term, glomerulosclerosis (1). This mechanism explains why kidney function may continue to decline in patients with CKD even when the primary insult is gone. Unfortunately, estimating nephron mass is not currently possible without kidney biopsy studies.
The level of uromodulin (Tamm–Horsfall protein) in urine is a candidate to estimate nephron mass because the protein is synthesized by the thick ascending limb of the loop of Henle and is essentially released into the urine. We hypothesized that if urinary uromodulin is a proxy of nephron mass, then (1) it should be associated with the known predictors of biopsy-assessed nephron mass in the general population and (2) its excretion should halve after kidney donation.
Urinary uromodulin concentration was measured by a validated ELISA (2) in 24-hour urinary collections of adult participants to the population-based Swiss Kidney Project on Genes in Hypertension (SKIPOGH) study. The study was approved by the institutional ethical review boards of each of the participating hospitals (3). A study visit was performed after an overnight fast, including a questionnaire, a physical examination, blood sampling, and 24-hour urine collection. Birth weight was obtained by self-reporting and birth certificates, if available.
We used a mixed regression multilinear model to assert the association between 24-hour urine uromodulin excretion and all newly identified predictors of the nephron mass as described in a recent biopsy-based study, namely age, female sex, uric acid, and height (4). We also analyzed the association between 24-hour urine uromodulin excretion and birth weight, another predictor of nephron mass. All linear models, including the model presented in Figure 1A, were adjusted for center as a fixed effect and for family clusters as a random effect.
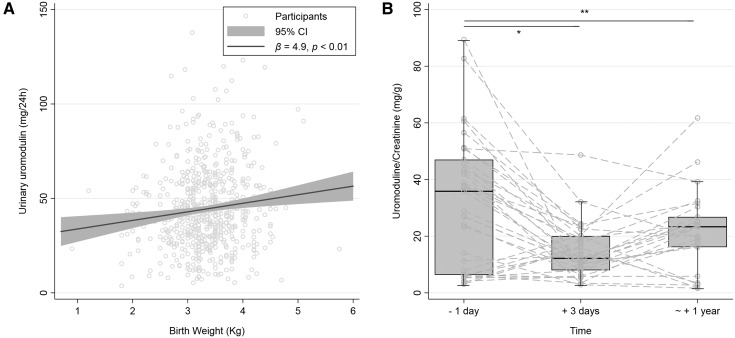
Figure 1.
Urinary uromodulin increases with higher birth weight and decreases after nephrectomy. (A) Scatter plot and linear regression of birth weight and 24-hour urinary uromodulin excretion. (B) Box plot of urine uromodulin-to-creatinine ratio in 35 kidney donors before and after nephrectomy. Paired t test: *P<0.01; **P<0.03. 95% CI, 95% confidence interval.
Urinary uromodulin was also measured in living kidney donors recruited at the University Hospital of Geneva from 2014 to 2016. Uromodulin and creatinine were measured in second morning urine collected 1 day, 3 days, and approximately 1 year after surgery.
A total of 1032 out of 1128 SKIPOGH participants (492 men and 540 women) had a complete 24-hour urine collection (urinary volume ≥300 ml and creatinine excretion ≥0.1 mmol/kg body wt) and were included in the analyses. Mean age was 47±18 years and eGFR was 96±18 ml/min per 1.73 m2. Mean 24-hour urine uromodulin excretion was 43.1±22.5 mg and mean birth weight was (available for 61% of participants) 3.34±0.59 kg. The 24-hour urine uromodulin excretion increased at higher birth weight (Figure 1A). In multiple linear regression analysis, 24-hour urine uromodulin excretion was associated with the same predictors of nephron mass as identified in the study by Denic et al. (4). Age, female sex, and uric acid were negative predictors whereas height and birth weight were positive predictors of 24-hour urine uromodulin excretion.
In 35 living kidney donors (25 women, mean age 53±10 years, eGFR 93±18 ml/min per 1.73 m2), urine uromodulin-to-creatinine ratio decreased from 32±23.1 at 1 day before to 14.6±9.4 mg/g at 3 days after kidney donation (P<0.01). At 1 year, urine uromodulin-to-creatinine ratio was 21.6±2.9 mg/g (paired t test: P=0.03; see Figure 1B). The ratios did not decrease in all donors at day 3, possibly because of the presence of confounding factors (e.g., drugs, perfusions, tubular necrosis) in the postoperative period or, alternatively, to preanalytical factors affecting the stability of uromodulin (e.g., storage, sampling) (2). The rise of the ratio at 1 year could point to tubular hypertrophy occurring after kidney donation.
Taken together, these findings add valuable information to the determinants of urinary uromodulin and suggest that 24-hour urine uromodulin excretion is a proxy of nephron mass. These results complete previous studies demonstrating the association of uromodulin excretion with eGFR, markers of tubular function, and genetic variants. They should be appreciated in the light of recent findings reporting that low urinary uromodulin levels are associated with kidney function decline and total mortality even after adjusting for eGFR and other risk factors (5).
When interpreting the association of uromodulin with birth weight, one should remember that nephron mass varies with gestational age, a parameter that was not available in our study. Although the levels of uromodulin are regulated by nephron mass in the healthy population, the utility of this finding remains uncertain in clinical situations where other factors that affect uromodulin levels such as inflammation, medication, and (pre)diabetes also play a role. In conclusion, urinary excretion of uromodulin correlates with all known predictors of nephron mass, including birth weight, in the healthy population and in living kidney donors. These data substantiate the measurement of urinary uromodulin levels as a useful surrogate marker for nephron mass in the general population.
Disclosures
None.
Acknowledgments
M. Bochud, O.D., and M.P. codirected the study. M.P. is supported by a grant from the Swiss National Science Foundation (FN320030-169191). O.D. is supported by the Swiss National Centre of Competence in Research Kidney Control of Homeostasis (NCCR Kidney.CH) program and the Swiss National Science Foundation (31003A_169850).
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Brenner BM, Meyer TW, Hostetter TH: Dietary protein intake and the progressive nature of kidney disease: The role of hemodynamically mediated glomerular injury in the pathogenesis of progressive glomerular sclerosis in aging, renal ablation, and intrinsic renal disease. N Engl J Med 307: 652–659, 1982 [DOI] [PubMed] [Google Scholar]
- 2.Youhanna S, Weber J, Beaujean V, Glaudemans B, Sobek J, Devuyst O: Determination of uromodulin in human urine: Influence of storage and processing. Nephrol Dial Transplant 29: 136–145, 2014 [DOI] [PubMed] [Google Scholar]
- 3.Pivin E, Ponte B, Pruijm M, Ackermann D, Guessous I, Ehret G, Liu YP, Drummen NE, Knapen MH, Pechere-Bertschi A, Paccaud F, Mohaupt M, Vermeer C, Staessen JA, Vogt B, Martin PY, Burnier M, Bochud M: Inactive matrix gla-protein is associated with arterial stiffness in an adult population-based study. Hypertension 66: 85–92, 2015 [DOI] [PubMed] [Google Scholar]
- 4.Denic A, Mathew J, Lerman LO, Lieske JC, Larson JJ, Alexander MP, Poggio E, Glassock RJ, Rule AD: Single-nephron glomerular filtration rate in healthy adults. N Engl J Med 376: 2349–2357, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garimella PS, Biggs ML, Katz R, Ix JH, Bennett MR, Devarajan P, Kestenbaum BR, Siscovick DS, Jensen MK, Shlipak MG, Chaves PH, Sarnak MJ: Urinary uromodulin, kidney function, and cardiovascular disease in elderly adults. Kidney Int 88: 1126–1134, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]