Abstract
Many adolescents with sickle cell disease (SCD) experience recurrent and chronic pain, which has a negative impact on their health-related quality of life (HRQL). Cognitive-behavioral therapy (CBT) interventions can lead to improvement in pain and HRQL, yet due to barriers to care, most youth with SCD will not receive these interventions. To address this need for innovative programs targeting youth with SCD pain, we developed iCanCope, a tailored smartphone and web-based program that delivers a pain self-management intervention to youth with SCD. We describe the rationale, design, and implementation of a three-site parallel group randomized controlled trial with a sample of 160 adolescents with SCD and their parent caregivers. The iCanCope program includes pain self-management skills training (personalized CBT-based coping skills such as deep breathing, relaxation, and cognitive skills), goal setting, and social support. The attention control group is provided with access to a self-guided website with education about SCD. Assessments will occur at baseline (T1), immediately after completion of the intervention (12 weeks; T2) and at 6 months post-intervention (T3). Primary outcomes include coping strategies and pain intensity; secondary outcomes include physical, social, and emotional functioning, treatment satisfaction, health service use and caregiver response to youth pain behavior. Potential mediators (goal setting, self-management, and perceptions of social support) and moderators (e.g., demographic factors) will also be tested. The objective is to offer an effective, convenient, and low-cost psychosocial intervention to youth with SCD to enhance their self-management of pain.
Keywords: Sickle Cell Disease, pain, pain management, cognitive-behavioral therapy, smartphone application
Introduction
Sickle cell disease (SCD) is the most common genetic blood disease among individualsin North America, most often occurring in individuals of African descent (1). Although episodic acute pain is recognized as the hallmark of this disorder, there is increasing awareness that many individuals experience chronic SCD pain (2). Painful crises are the main reason for SCD-related hospitalization (3), and drive annual healthcare costs of $1.1 billion (4). Similar to other pediatric chronic pain conditions, youth with frequent SCD pain experience negative impact on all aspects of health-related quality of life (HRQL) (5–7) including pain-related functional disability and depressive symptoms (7, 8). Pain becomes more frequent in older adolescence, and by adulthood, almost 30% of patients report daily pain (9).
Although opioid therapy is the most relied upon approach to pain management in SCD, evidence indicates that opioid therapy does not provide adequate pain relief and that its long-term use leads to negative physical and psychological consequences and stigma (10). As such, there is a pressing need for effective, non-pharmacologic interventions to treat chronic pain in patients with SCD.
Cognitive behavioral therapy (CBT) to promote pain self-management can lead to pain reduction, improved coping skills and HRQL, and decreased healthcare use for youth with a range of chronic pain conditions (11–13). However, evidence for the efficacy of psychological therapies in SCD is currently fairly limited (14) due to the small number of studies conducted and very small sample sizes enrolled. A major barrier in implementing CBT in SCD populations is that it is challenging to deliver pain management interventions in traditional office-based visits (15), and investigators have described the critical need to improve feasibility of psychosocial interventions for pediatric SCD pain (16). The use of Internet- and smartphone-delivered interventions is a potential option to overcome barriers to accessing pain management services for youth with SCD and their families. Evidence from a systematic review showed that treatments delivered on the Internet reduce pain and disability in youth with other types of chronic pain (17). In addition, access to Internet and smartphone technologies among African Americans is high (80–85%) (18), even among those of low income (19).
Two prior technology-based interventions have been evaluated in youth with SCD pain (20). In the first study, a sample of children and adolescents with SCD were provided with one in-person session of CBT followed by 8 weeks of home-based practice using a smartphone, with weekly clinician phone contact. In comparison to the waitlist control, participants who received CBT believed they had more control over their pain, but had no change in their negative thinking in response to pain or in their pain intensity. The smartphone application was underutilized (average use of only 12% over the 8-weeks), and the coping skills section of the application was accessed on less than a quarter of the total pain days reported by all youth. However, in the second study, an Internet-delivered CBT program for pain management was piloted with youth in a small randomized controlled trial (RCT), finding that it was feasible to deliver and acceptable to adolescents with SCD and their caregivers and that engagement and adherence were good (21).
Objectives
Our goal is to improve pain self-management and functioning in youth (aged 12–18 years) with SCD by developing and testing a tailored web and smartphone-based application (iCanCope with SC Pain). We aim to evaluate, in a three-site RCT, the efficacy of the intervention with a sample of 160 adolescents with SCD and their parent caregivers. We will also examine mediators and moderators of treatment effects to enhance understanding of who benefits from the intervention and what mechanisms underlie benefit from the pain self-management intervention. The objective is to offer an effective, convenient, and low-cost psychosocial intervention to youth with SCD to enhance their self-management of pain.
Aims and Hypotheses
Aim 1.
To determine feasibility and initial efficacy of iCanCope in youth with SCD pain. We hypothesize that youth who receive iCanCope will achieve significant increases in adaptive coping and reductions in pain (primary outcomes) as well as significant improvements in physical and emotional functioning and disease-specific health-related quality of life (secondary outcomes) at post-treatment and 6-month follow-up compared to youth who receive an attention-control condition. Feasibility and acceptability will be demonstrated by high levels of treatment engagement and high ratings of satisfaction with the intervention.
Aim 2.
To examine possible mediators of the effects of iCanCope to test the hypothesis that changes at post-treatment in youth goal setting, self-efficacy, self-management, and perceptions of social support mediate intervention effects on youth pain intensity, pain-related disability, and adaptive pain coping at 6-months.
Aim 3.
To examine possible moderators of effects of iCanCope through exploratory analyses. Potential moderators will include: engagement with treatment, demographic factors (family income, child age, gender), executive function skills, and disease characteristics (SCD pain burden).
Study Design
This is a parallel group, single blinded randomized controlled trial with stratified randomization based on age and treatment center to intervention vs. active control conditions. The intervention phase will last 12 weeks. Outcome assessment will occur at baseline (T1), immediately after completion of the intervention (12 weeks, T2) and be repeated at 6 months post-intervention (T3). The T3 assessment will capture potential maintenance of treatment gains as youth with SCD may have fluctuations in their disease course that influence pain outcomes.
Participant Eligibility, Recruitment, Enrollment, and Randomization
Youth will be eligible if they: (a) are aged between 12–18 years, (b) are diagnosed with SCD, (c) are able to speak and read English, (d) score at least 4 (indicating some days with pain interference over the past month) on the Sickle Cell Pain Burden Interview (22) and (e) are willing and able to complete online measures. Parent caregivers will be eligible if they: (a) are able to speak and read English and (b) are willing and able to complete online measures. Youth will be excluded if they have significant cognitive limitations that would impair their ability to use and understand the iCanCope program, as per their healthcare provider or parent. Youth will also be excluded if they have received more than 4 sessions of outpatient psychological therapy for pain management in the 6 months prior to the time of screening.
Participants will be recruited from three pediatric centers: Connecticut Children’s Medical Center, Children’s Healthcare of Atlanta/Emory University, and The Hospital for Sick Children in Toronto. Patients listed on the participating clinic registries will be screened for eligibility by the local study investigator. Initial patient contact will be made either through a mailed letter or in-person during scheduled clinic visits. If youth are interested in learning more, study staff will explain the study and seek informed consent or assent. Research staff will track the number of eligible youth approached and reasons for refusal. After obtaining informed consent, study staff at the Seattle site will send out pre-treatment measures to complete online via REDCap. Following completion of pre-treatment measures, participants will be randomized to an intervention condition. Participants will be instructed on the procedures to be followed within the intervention and control groups using standardized manuals. See Figure 1 for study flow.
Figure 1.
CONSORT diagram depicting participant flow
Participants will be randomly allocated using a hidden allocation scheme to either the CBT intervention (iCanCope) or attention control education group. Randomization will be centrally controlled at the Seattle site and will be stratified by study center (i.e., to control for site-specific disease education and treatment approaches) and age (i.e., to control for developmental stage; 12–14 years and 15–18 years). The randomization schedule will be created by the study data manager who is not involved in participant recruitment or intervention assignment. The randomization schedule will be stored in a password-protected document accessible only to study staff involved in intervention assignment.
Description of study Arms
CBT intervention group.
iCanCope includes components from prior pain management interventions. The web based skills and education content is adapted from an Internet-delivered cognitive-behavioral therapy (CBT) pain intervention for teens with general chronic pain conditions that resulted in significant reduction in activity limitations from baseline to 6-month follow-up compared with Internet education. This intervention was piloted in 12 youth with SCD and their parents recruited from two of the sites for this trial (21). Treatment engagement was high for both adolescents and parents. In qualitative interviews, participants reported the CBT program was a helpful tool for coping with pain and indicated a preference for a web program that was designed specifically for youth with SCD.
The iCanCope app platform was initially developed for youth with chronic pain and adapted for this trial for youth with SCD. For more information on the development of the chronic pain platform see (23). Five patient partners with SCD were involved in adapting the platform and content specifically for SCD. The patient partners used the chronic pain platform and provided advice on how to adapt it to SCD. Changes included making the content shorter and more concise, creating video content which includes youth with SCD, and adapting the example scenarios in the content to be more relevant to the population.
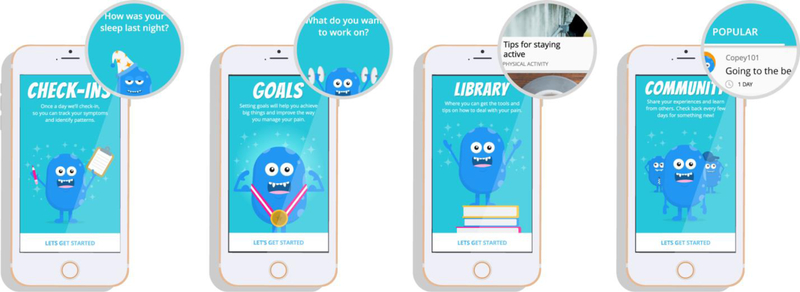
In addition to standard care, youth will receive the iCanCope intervention over a period of 12 weeks. The iCanCope program includes (i) pain self-management skills training, (ii) goal setting, and (iii) social support. See screenshots of the app in Figure 1. The program is designed to enhance self-efficacy. Participants will be encouraged to set SMART (Specific, Measurable, Achievable, Results-focused, and Time-bound) goals. The pain self-management skills include personalized CBT-based coping skills including deep breathing, relaxation, and cognitive skills (e.g., staying positive). The app is developed natively for iOS and Android smartphones while the website is accessible on all modern web browsers. The program is restricted to study participants. Detailed user level and aggregate analytics will be captured to track user engagement.
The app has four key features (see Figure 2): daily symptom tracking, goal setting, self-management skill library, and social community. The daily check-in feature uses adolescent-friendly language and pictorial response options to optimize participant engagement. Pain intensity is self-reported on a 0–10 numerical rating scale with the anchors, “no pain” and “worst pain”. Other symptom categories (pain impact, mood, and sleep quality) are captured via individual 5-point scales where a lower score indicates better function. Participants will receive daily push notification check-in reminders at a time of their choice and be able to view their historical check-in data at any time within the app. The goals feature is designed to support participants in setting and tracking personalized goals to improve their function. Participants can design their own goals or adapt suggested goals within the categories of activity, sleep, and mood. The skills library provides in-the-moment access to pain coping strategies to promote positive changes in mood, behavior, and pain. The library consists of curated articles relevant to different aspects of living with and managing SCD pain. Tailored articles are suggested to participants based on their check-in data (e.g. “developing a wind-down routine” article if participant reports poor sleep quality). The social community is a structured forum where participants can interact with other young people living with SCD pain. Each week, the app poses a new question for discussion, such as, “What’s your favorite distraction from pain?” Participants can post responses to each community question and also “favorite” the posts of other app users.
Figure 2.
Screen shots from the iCanCope app
Youth and their caregiver will also be encouraged to access the iCanCope website, which contains interactive SCD education and self-management strategies. The website is organized into 6 core modules and 2 additional optional modules, which will be assigned based on individual screening measures for depressive symptoms and insomnia. The website uses a multimedia-rich format (e.g., animations, videos, audio clips) to deliver content. Content is: (a) written at a grade 5–6 reading level, (b) developmentally appropriate for the full age range of youth participants [12–18 years], and (c) culturally relevant.
Participants will be instructed to complete one website module per week over the study period. Each module closes with an assignment for the participant to practice the skills taught that week.
Caregivers have access to a website that includes behavioral plans, problem-solving skills, and communication strategies intended to provide instruction in the best ways to support their child’s pain management skills and encourage adaptive coping. The same usage information is collected for the caregiver website. Table 1 provides a summary of the website module content for youth and parent caregivers. Weekly reminders (e.g., text, call, email) will be sent to participants and parents to encourage use of the app and website.
Table 1.
Summary of website module content for iCanCope with SC Pain CBT arm
| Adolescent Intervention Website Content | ||
| Module Number | Module Title | Content/Skills |
| 1 | Introduction | Intro, *SMART Goals, pain education, types of psychological treatments |
| 2 | Managing stress | Reduce negative thoughts: replace with positive thoughts, thought stopping |
| 3 | Relaxation | Relaxation: deep breathing, muscle relaxation, imagery, mini relaxation |
| 4 | Sleep | Pain and sleep, healthy sleep, ways to fall and stay asleep |
| 5 | Communication and self-advocacy | Communication skills, talking with healthcare team and school |
| 6 | Healthy lifestyle | Pacing, graded activity, hydration |
| 7 | Optional: Insomnia | Building healthy sleep habits, using stimulus control and sleep restriction strategies |
| 8 | Optional: Negative emotions | Identify negative emotions, schedule pleasant activities, find the positives |
| Parent Intervention Website Content | ||
| Module Number | Module Title | Content/Skills |
| 1 | Introduction | What your child will learn, *SMART goals to support your child |
| 2 | Behavioral plans | Behavioral plans |
| 3 | Problem solving 1 | Problem solving skills part 1 |
| 4 | Problem solving 2 | Problem solving skills part 2 |
| 5 | Communication | Strategies for parent-child communication, strategies to communicate with health care providers and school staff |
| 6 | Wrap-up | Review |
SMART = Specific, Measurable, Achievable, Results-focused, and Time-bound.
Attention control education group.
The comparator group is designed to account for potential effects on outcomes of time, attention, as well as computer use during the intervention period. In addition to standard medical care, youth and parent caregivers in the attention control group will be provided with access to a self-guided education study website, which will contain static education about SCD (no self-management skills, goal-setting, or social support content). Table 2 provides a summary of the website module content for youth and parent caregivers. The control condition will be delivered over 12 weeks on the same password-protected web-based platform as the intervention group website that will allow us to track usage and engagement. Participants will be encouraged to log onto the control website (i.e., email reminders) and complete all study outcome assessments online at the same time intervals as the experimental group. Program usage data will also be collected for participants in the attention control group.
Table 2.
Summary of website module content for the attention control education group
| Adolescent and Parent Control Website Content | ||
|---|---|---|
| Section Number | Title | Education Content |
| 1 | Introduction | Intro to program |
| 2 | About sickle cell disease | What is SCD, symptoms and complications |
| 3 | Treatments and medication | About medications, transfusions, pain medications, complementary medicines |
| 4 | Acute and chronic pain | Acute pain, chronic pain, factors that influence pain experience |
| 5 | Healthy lifestyle | Diet, exercise, alcohol and drugs, school and hospital stays |
| 6 | Looking ahead and research | Transition to adult care, clinical research |
Study Monitoring Procedures
Treatment fidelity.
Treatment fidelity for both interventions will be assessed in several ways. The administrative interface of the iCanCope application and website will have tracking systems for recording each time a user logs onto the web program, and thus, amount of app and web site usage will be recorded. Assignments and use of different skills will also be recorded.
In order to ensure fidelity to the protocol across sites, study procedures are centrally managed using email and phone by one site for all participants. The Seattle site will conduct all study assessments, randomization, and participant onboarding into the allocated treatment group. We will conduct monthly phone calls across sites to review study management.
Measures.
Outcomes will be assessed across the two intervention groups at T1= pre-treatment; T2 = post-treatment (12 weeks); T3 = follow-up (6 months post-treatment). All measures will be completed online via REDCap. Table 3 provides details on study measures.
Table 3.
Study Measures
| Measure | Description of measure | Respondent | Time point administered | ||
|---|---|---|---|---|---|
| T1 | T2 | T3 | |||
| Screening and background measures | |||||
| Sickle Cell Pain Burden Interview | Screen for SCD pain burden in the past month in six domains (pain, sleep, school, social, emotional, and function). | Youth, Caregiver | ✓ | ✓ | ✓ |
| Background questionnaire | Report on sociodemographic variables (including family income), as well as access, use, and comfort with smartphones and internet technology. | Youth, Caregiver | ✓ | ||
| Treatment expectancies questionnaire | Rate youth/caregivers expectations that the program will be useful and helpful. | Youth, Caregiver | ✓ | ||
| Adolescent Sleep Wake Scale: Insomnia | Two items used to screen for insomnia symptoms in the past month. Used to screen for delivering the optional website module on insomnia. | Youth | ✓ | ||
| Primary outcome measures | |||||
| Coping Strategies Questionnaire for Sickle Cell Disease | Measure use of different strategies to cope with pain. | Youth | ✓ | ✓ | ✓ |
| Daily pain diary (7 day) | Assess daily pain intensity (NRS-11), location, activity limitations, and mood. Completed daily for 7 days. | Youth | ✓ | ✓ | ✓ |
| Secondary outcome measures | |||||
| Treatment Evaluation Inventory | Assess perceptions and acceptability of the intervention. | Youth, Caregiver | ✓ | ||
| Patient’s Global Impression of Change Scale | Assess perception of overall improvements since beginning the intervention. | Youth | ✓ | ✓ | |
| PROMIS Pediatric Profile | Assess physical and emotional functioning including depressive symptoms, anxiety, mobility, pain interference, fatigue, and peer relationships in the past week. Depressive symptoms scale used to screen for delivering the optional website module on negative emotion. | Youth | ✓ | ✓ | ✓ |
| Adult Responses to Child Symptoms | Assess caregiver response to youth pain behavior including protectiveness, minimizing, and encouraging. | Caregiver | ✓ | ✓ | ✓ |
| Bath Adolescent Pain Questionnaire | Caregiver report of youth social functioning, physical functioning, depression, general anxiety, pain specific anxiety, development and femily functioning in the past two weeks. | Caregiver | ✓ | ✓ | ✓ |
| Client Service Receipt Inventory | C ollect youth’s use of various health services (e.g., outpatient visits, emergency room visits, medications) over the past 6 months. | Caregiver | ✓ | ✓ | |
| Symptom Checklist 90 | Assess caregiver psychological symptoms including obsessive compulsive, depression, and anxiety during the past week. | Caregiver | ✓ | ✓ | ✓ |
| Process measures (mediators) | |||||
| iCanCope program usage | App and website usage (e.g., number of logins, activity) at user leveL | Youth, Caregiver | ✓ | ✓ | ✓ |
| Multidimens io nal Scale of Perceived Social Support | Assess social support from femily, friends, and significant others. | Youth | ✓ | ✓ | ✓ |
| Patient Activation Measure | Assesses ability to self-manage health within the context of knowledge, skills, and confidence. | Youth | ✓ | ✓ | ✓ |
| Sickle Cell Self-Efficacy Scale | Measure disease-specific perceptions of self- efficacy. | Youth | ✓ | ✓ | ✓ |
| Behavior Rating Inventory of Executive Function | Report frequency of youth’s problem behaviors associated with executive function in the past 6 months. | Caregiver | ✓ | ||
Primary outcome measures.
We have two primary outcomes, coping strategies and pain. To assess use of strategies to cope with pain, adolescents will complete the Coping Skills Questionnaire (CSQ) (24). The CSQ is an 80-item questionnaire with three primary scales: Coping Attempts, Negative Thinking, and Passive Adherence. The CSQ has demonstrated adequate reliability and validity in pediatric sickle cell disease [31]. To assess pain, adolescents will complete daily pain diaries for 7 days at each measurement period and report pain intensity using an 11-point numerical rating scale (NRS; 0 = no pain, 10 = worst pain possible). The NRS is a widely used measure of pain intensity in adolescents and demonstrates good reliability and validity (25).
Secondary outcome measures.
Secondary outcome measures include an adapted version of the Treatment Evaluation Inventory – Short Form (TEI-SF) (26) to assess satisfaction with the treatment program; the Patient’s Global Impression of Change (PGIC) (27, 28) to assess respondents’ global impressions of change in “activity limitations, symptoms, emotions, and overall quality of life”; the PROMIS Pediatric Profile (29) to assess physical, emotional, and social functioning; the Adult Responses to Child Symptoms (ARCS) (30) to assess parents’ responses to children’s pain behavior; the Bath Adolescent Pain Questionnaire (BAPQ) (31) to assess pain-related functioning; a modified version of the Client Receipt Service Inventory-Pain (32) adapted for sickle cell disease to collect information on use of various health services (e.g., outpatient visits, emergency room visits, medications); and the Symptom Checklist 90 (SCL-90) (33) to assess a range of psychological symptoms in parent caregivers.
Screening and background measures.
Participants will complete three screening measures. The Sickle Cell Pain Burden Interview (SCPBI) (22) will be used to screen for SCD pain burden in the past month in six domains. Youth will complete two items from the Adolescent Sleep Wake Scale (ASWS) (34) to screen for insomnia symptoms in order to deliver optional insomnia content in the iCanCope program. Youth will complete the depressive symptoms scale from the PROMIS Profile [36] in order to deliver optional depression content.
Participants will rate treatment expectancies with a measure adapted for the current study, the Treatment Expectancy Questionnaire (TEQ) (35), which asks respondents to rate how likelyit is that “a sickle cell pain program” will be useful and helpful. Participants will also report on sociodemographic variables (e.g., family income), internet and computer use, and comfort with technology.
Process measures.
Process measures include iCanCope program usage; the Multidimensional Scale of Perceived Social Support (MSPSS) (36) to assess social support from family, friends, and significant others; the Patient Activation Measure (PAM) (37) to assess the ability to self-manage illness; the Sickle Cell Self-Efficacy Scale (SCES) (38) to assess disease-specific perceptions of self-efficacy; and the Behavior Rating Inventory of Executive Function – Parent Form (39) to assess frequency of youth problem behaviors associated with executive function.
Adverse events.
Adverse events will be collected at post-treatment and follow-up using a child and parent self-report scale developed for this study.
Retention and Adherence
We will over-recruit by 20% to account for potential dropouts and loss to follow-up. An intent-to-treat approach will be used for the analysis. However, every effort will be made to maintain participation in the study groups and to obtain post-treatment measures on all participants. Participants will receive a gift card for each outcome assessment completed (T1–3). We will ask for multiple phone numbers, which will aid in follow-up. We will use emails and text messages to remind participants of the various online assessments. Every effort will be made to maintain participation in the study groups and to obtain post-treatment measures on all participants who are enrolled in the study.
Strategies for dealing with nonadherence will include: designing an appealing and engaging program as per user-centered methodology, gamification elements (e.g., positive feedback loops, short-term and meta goals), and social elements (e.g., peer support). Characteristics of adherent versus non-adherent youth will be examined for systematic differences. When found, sensitivity analyses will determine effect on outcomes.
Sample Size and Power Estimations.
Based on our prior and current study experience, and the pool of available study candidates, we are expecting to enroll a total of 160 subjects into the RCT. With attrition conservatively estimated at 20% we expect a final sample size of 128. Based on preliminary data from our prior trials and other published trials in SCD, power estimates are based on expected differences in pain intensity. Group sample sizes of 49 and 49 achieve 80% power to detect a difference of 0.75 in pain intensity (average over three time points) in a design with 3 repeated measurements having an autoregressive (1) covariance structure, SD=2, ICC=0.2 and 0.05 alpha.
Data Analysis
Distributions of primary and secondary outcome variables at each time point (and on difference scores between time points) will be examined first with summary statistics and graphical tools. For outcome variables with highly skewed distributions, we will either apply transformation or non-parametric test procedures. Preliminary work will also involve computation of scale reliabilities (e.g., internal consistency using Cronbach’s alpha) of all of the self-report measures. The analysis will be an intent-to-treat analysis including all randomized subjects.
Analytic Plan for Aim 1:
Feasibility will be determined by calculating rates of accrual, drop out, compliance, and missing data with 95% CI’s. Criteria for feasibility success will be based on previous studies by our group: accrual rates >70%, attrition rates <20%, minimal technical difficulties (i.e., reported by <10%), high acceptability and satisfaction (score > 27 on TEI), adherence rates >80% (adherence operationalized as completion of at least 50% of the intervention (i.e., 3 of 6 intervention web modules as well as a completed app check-in on 28 of 56 days), and minimal missed responses. In Aim 1, we will also determine preliminary efficacy of the intervention. To account for clustering due to repeated assessments within individuals, we will use generalized estimating equations (GEE). Interaction terms will be used to compare the mean change from pre-treatment to post-treatment for the CBT intervention group with the corresponding mean change for the Attention Control Education group. Single degree of freedom contrasts will test if there is a statistically significant change in pain and coping from pre-treatment to immediate post-treatment for the two groups separately; additional contrasts will be computed to test if there is a statistically significant mean change from baseline to the 6-month follow-up for each group. Secondary treatment outcomes (physical and emotional function, HRQL) will also be examined using GEE to test significant mean changes over time and between groups by using interaction terms and contrasts. Treatment fidelity will be assessed by examining differential attrition (completers vs. non-completers) between and within groups using chi-squared tests and logistic regression models.
Analytic Plan for Aim 2 and 3:
Our working hypothesis related to Specific Aim 2 is that differences in self-efficacy, self-management behaviors, and perceived social support will predict changes in pain intensity and coping strategies in youth with SCD. The test of this hypothesis will follow the recommendations for testing “moderated mediation” models described by Bauer (40), which permits specification of a single equation that furnishes the coefficients necessary for estimating total, direct, and indirect effects in a multilevel mediation model. The single equation is made possible by creating a new outcome variable (“Z”) that comprises both the outcome variable of interest (“Y”) and mediating variable (“M”) simultaneously; the two are distinguished by creating two specification variables (“S”) that take on the value of 0 and 1 depending on whether the new outcome variable “Z” represents the mediating variable or outcome variable. The models will be specified with “time” as a predictor (“X”) of the outcomes pain intensity and coping strategies, with the self-efficacy, self-management behaviors, and perceived social support variables included as mediating variables (“M”). The indirect effect of time will then be specified to be predicted by treatment. As such, this model will allow a test of whether an individual’s changes over time in pain outcomes are partly explained by changes in the hypothesized mediators and whether the strength of this indirect effect varies depending on group.
We will use exploratory analysis to examine possible moderators of effects of iCanCope including engagement with treatment, demographic factors (family income, age, sex), executive function, and disease characteristics (SCD pain burden). To assess the moderation effect we will include an interaction term for each separate moderator variable and key predictor of interest (two-way interaction between moderator and group for cross-sectional analysis and three-way interaction between moderator, group and time for longitudinal analysis) in the regression models and test its significance using Wald t-test.
Discussion
The unique contributions of the proposed research include: (a) establishing the extent to which iCanCope is an efficacious and viable means of disseminating evidence-based pain self-management therapy for youth with SCD; (b) determining the potential impact of this intervention on key health outcomes and processes (e.g., pain, HRQL, and pain coping strategies) that are not optimally addressed with medical treatment alone; (c) conducting the first RCT to evaluate an integrated web- and mobile-based pain self-management app in youth with SCD; (d) optimizing program value by actively engaging youth with SCD and their families through a user-centered design approach to development and evaluation (41); and (e) testing mediators and moderators of treatment effects to begin to understand who benefits from the intervention and through what processes.
A number of barriers can be addressed through using digital technologies to deliver treatment. Specifically, we are able to address the geographic restrictions to CBT pain services, the limited availability of clinicians trained in CBT for SCD pain, the direct and indirect incurred costs of additional healthcare visits to receive CBT (42, 43), and the stigma associated with seeking assistance through mental health services (44).
Several aspects of the intervention and study design are novel. A major strength of our approach to developing the intervention is applying user-centered design principles in order to maximize patient engagement. We have actively engaged youth with SCD (“patient partners”) throughout the process of developing iCanCope with SC Pain. These patient partners have formed a youth advisory panel that provides feedback and guidance. We have facilitated interactive design sessions with the web and app development teams from AboutKidsHealth and eHealth Innovation at the University Health Network and our patient partners from the USA and Canada. These sessions adhere to the principles of human factor design and enabled further definition of user requirements for the app and website (41). This patient engagement has also identified ways that iCanCope with SC Pain can be designed to fit into the daily lives of our target users, which is critical for maximizing engagement and ensuring cultural and linguistic appropriateness (45). While a user-centered design approach has been successfully applied to develop apps for individuals with chronic illnesses such as diabetes (45) and asthma (41), to our knowledge, it has never been used for SCD.
We recognize the significant difficulty in previous SCD clinical trials with obtaining adequate recruitment and retention where prior trials have reported rates of recruitment as low as 13% of available samples (15, 20, 46). Because one of the key barriers to participation in intervention studies by patients with SCD is reaching them by phone and scheduling study visits (21), we have devised multiple strategies for reaching youth and families such as through text and email. Moreover, others have noted the significant challenges of enrolling African-American youth and their parents into intervention research where broader issues such as socioeconomic barriers, mistrust and misunderstanding of research (47), and lack of perceived benefits from research participation may contribute to low enrollment (16). Our use of patient engagement strategies throughout the research process is expected to address some of these participation barriers. In addition, by using an active comparator as opposed to a no treatment control condition we believe the value of research participation to the individual is enhanced.
The results of this trial will have important implications not just for SCD behavioral interventions, but also for other pain self-management interventions more broadly. The knowledge contributions of the proposed research include evaluating an integrated web- and mobile-based pain self-management app in youth and testing mediators and moderators of treatment effects to begin to understand who benefits from the intervention and through what processes. In addition, this intervention represents a cost-effective alternative to traditional CBT that has the potential for widespread dissemination that may inform pain self-management in multiple populations.
Conclusions
This study will evaluate whether a tailored smartphone and web-based application (iCanCope) improves pain self-management and functioning in youth (aged 12–18 years) with SCD. Because SCD morbidity and mortality increase markedly during adolescence and young adulthood (1), intervening during adolescence provides an important opportunity to help youth develop critical pain self-management skills to better cope with SCD pain as adults. Overall, we envision that iCanCope will address an important service gap by delivering pain self-management therapy that is highly appealing, accessible, and engaging to youth. If successful, the iCanCope intervention has the potential for national dissemination in the USA and Canada, via either self-referral or referral from pediatric hematologists.
Acknowledgments
Funding: Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute Of Child Health & Human Development of the National Institutes of Health under Award Number R01HD086978. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hassell KL. Population estimates of sickle cell disease in the U.S. Am J Prev Med 2010;38(4 Suppl):S512–21. [DOI] [PubMed] [Google Scholar]
- 2.Dampier C, Palermo TM, Darbari DS, Hassell K, Smith W, Zempsky W. AAPT Diagnostic Criteria for Chronic Sickle Cell Disease Pain. J Pain. 2017;18(5):490–8. [DOI] [PubMed] [Google Scholar]
- 3.Smith WR, Scherer M. Sickle-cell pain: advances in epidemiology and etiology. Hematology Am Soc Hematol Educ Program. 2010;2010:409–15. [DOI] [PubMed] [Google Scholar]
- 4.Kauf TL, Coates TD, Huazhi L, Mody-Patel N, Hartzema AG. The cost of health care for children and adults with sickle cell disease. Am J Hematol. 2009;84(6):323–7. [DOI] [PubMed] [Google Scholar]
- 5.Dampier C, Shapiro BS. Management of Pain in Sickle Cell Disease. 2003. p. 489–516. [Google Scholar]
- 6.Conner-Warren RL. Pain intensity and home pain management of children with sickle cell disease. Issues Compr Pediatr Nurs. 1996;19(3):183–95. [DOI] [PubMed] [Google Scholar]
- 7.Bonner MJ. Health related quality of life in sickle cell disease: just scratching the surface. Pediatr Blood Cancer. 2010;54(1):1–2. [DOI] [PubMed] [Google Scholar]
- 8.Sil S, Cohen LL, Dampier C. Psychosocial and Functional Outcomes in Youth With Chronic Sickle Cell Pain. Clin J Pain. 2016;32(6):527–33. [DOI] [PubMed] [Google Scholar]
- 9.Smith WR, Penberthy LT, Bovbjerg VE, McClish DK, Roberts JD, Dahman B, et al. Daily assessment of pain in adults with sickle cell disease. Ann Intern Med. 2008;148(2):94–101. [DOI] [PubMed] [Google Scholar]
- 10.Karafin MS, Singavi A, Hussain J, Wandersee N, Heinrich T, Hurley RW, et al. Predictive factors of daily opioid use and quality of life in adults with sickle cell disease. Hematology. 2018:1–8. [DOI] [PubMed] [Google Scholar]
- 11.Fisher E, Heathcote L, Palermo TM, de CWAC, Lau J, Eccleston C. Systematic review and meta-analysis of psychological therapies for children with chronic pain. J Pediatr Psychol. 2014;39(8):763–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Palermo TM, Eccleston C, Lewandowski AS, Williams AC, Morley S. Randomized controlled trials of psychological therapies for management of chronic pain in children and adolescents: An updated meta-analytic review. Pain. 2010;148(3):387–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen E, Cole SW, Kato PM. A review of empirically supported psychosocial interventions for pain and adherence outcomes in sickle cell disease. J Pediatr Psychol. 2004;29(3):197–209. [DOI] [PubMed] [Google Scholar]
- 14.Anie KA, Green J. Psychological therapies for sickle cell disease and pain. Cochrane Database Syst Rev 2015(5):CD001916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barakat LP, Schwartz LA, Salamon KS, Radcliffe J. A family-based randomized controlled trial of pain intervention for adolescents with sickle cell disease. J Pediatr Hematol Oncol 2010;32(7):540–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Daniel LC, Li Y, Smith K, Tarazi R, Robinson MR, Patterson CA, et al. Lessons Learned From a Randomized Controlled Trial of a Family-Based Intervention to Promote School Functioning for School-Age Children With Sickle Cell Disease. J Pediatr Psychol. 2015;40(10):1085–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Velleman S, Stallard P, Richardson T. A review and meta-analysis of computerized cognitive behaviour therapy for the treatment of pain in children and adolescents. Child Care Health Dev. 2010;36(4):465–72. [DOI] [PubMed] [Google Scholar]
- 18.Perrin A Smartphones help blacks, Hispanics bridge some – but not all – digital gaps with whites. 2017. August 31, 2017. Report No.
- 19.Zickuhr K, Smith A. Home Broadband 2013. Washington, DC: Pew Research Center, 2013. [Google Scholar]
- 20.Schatz J, Schlenz AM, McClellan CB, Puffer ES, Hardy S, Pfeiffer M, et al. Changes in coping, pain, and activity after cognitive-behavioral training: a randomized clinical trial for pediatric sickle cell disease using smartphones. Clin J Pain. 2015;31(6):536–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Palermo TM, Dudeney J, Santanelli JP, Carletti A, Zempsky WT. Feasibility and Acceptability of Internet-delivered Cognitive Behavioral Therapy for Chronic Pain in Adolescents With Sickle Cell Disease and Their Parents. J Pediatr Hematol Oncol 2018;40(2):122–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zempsky WT, O’Hara EA, Santanelli JP, Palermo TM, New T, Smith-Whitley K, et al. Validation of the sickle cell disease pain burden interview-youth. J Pain. 2013;14(9):975–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stinson JN, Lalloo C, Harris L, Isaac L, Campbell F, Brown S, et al. iCanCope with Pain (TM) : User-centred design of a web- and mobile-based self-management program for youth with chronic pain based on identified health care needs. Pain Research & Management. 2014;19(5):257–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gil KM, Williams DA, Thompson RJ Jr, Kinney TR. Sickle cell disease in children and adolescents: the relation of child and parent pain coping strategies to adjustment. J Pediatr Psychol. 1991;16(5):643–63. [DOI] [PubMed] [Google Scholar]
- 25.von Baeyer CL, Spagrud LJ, McCormick JC, Choo E, Neville K, Connelly MA. Three new datasets supporting use of the Numerical Rating Scale (NRS-11) for children’s self-reports of pain intensity. Pain. 2009;143(3):223–7. [DOI] [PubMed] [Google Scholar]
- 26.Kelley ML, Heffer R, Gresham F, Elliot S. Development of a modified treatment evaluation inventory. J Psychopathol Behav Assess. 1989;11(3):235–47. [Google Scholar]
- 27.Farrar JT, Young JP, Jr., LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–58. [DOI] [PubMed] [Google Scholar]
- 28.Hurst H, Bolton J. Assessing the clinical significance of change scores recorded on subjective outcome measures. J Manipulative Physiol Ther. 2004;27(1):26–35. [DOI] [PubMed] [Google Scholar]
- 29.Forrest CB, Bevans KB, Tucker C, Riley AW, Ravens-Sieberer U, Gardner W, et al. Commentary: the patient-reported outcome measurement information system (PROMIS(R)) for children and youth: application to pediatric psychology. J Pediatr Psychol. 2012;37(6):614–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Walker LS, Levy RL, Whitehead WE. Validation of a measure of protective parent responses to children’s pain. Clin J Pain. 2006;22(8):712–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jordan A, Eccleston C, McCracken LM, Connell H, Clinch J. The Bath Adolescent Pain--Parental Impact Questionnaire (BAP-PIQ): development and preliminary psychometric evaluation of an instrument to assess the impact of parenting an adolescent with chronic pain. Pain. 2008;137(3):478–87. [DOI] [PubMed] [Google Scholar]
- 32.Larg A, Moss JR. Cost-of-illness studies: a guide to critical evaluation. Pharmacoeconomics. 2011;29(8):653–71. [DOI] [PubMed] [Google Scholar]
- 33.Derogatis LR, Fitzpatrick M. The SCL-90-R, the Brief Symptom Inventory (BSI), and the BSI-18 Maruish Mark E (Ed). (2004). The use of psychological testing for treatment planning and outcomes assessment: Volume 3: Instruments for adults (3rd ed); 2004. xx, 1008 p. [Google Scholar]
- 34.LeBourgeois MK, Giannotti F, Cortesi F, Wolfson AR, Harsh J. The relationship between reported sleep quality and sleep hygiene in Italian and American adolescents. Pediatrics. 2005;115(1 Suppl):257–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tsao JC, Meldrum M, Bursch B, Jacob MC, Kim SC, Zeltzer LK. Treatment expectations for CAM interventions in pediatric chronic pain patients and their parents. Evid Based Complement Alternat Med. 2005;2(4):521–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. J Pers Assess. 1990;55(3–4):610–7. [DOI] [PubMed] [Google Scholar]
- 37.Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004;39(4 Pt 1):1005–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Clay OJ, Telfair J. Evaluation of a disease-specific self-efficacy instrument in adolescents with sickle cell disease and its relationship to adjustment. Child Neuropsychol. 2007;13(2):188–203. [DOI] [PubMed] [Google Scholar]
- 39.Gioia G, Isquith PK, Guy SC, Kenworthy L. Behavior rating inventory of executive function (BRIEF-2). Lutz, FL: Psychological Assessment Resource; 2016. [Google Scholar]
- 40.Bauer D, Preacher KJ, Gil KM. Conceptualizing and testing random indirect effects and moderated mediation in multilevel models: new procedures and recommendations. Psychol Methods. 2006;11(2):142. [DOI] [PubMed] [Google Scholar]
- 41.McCurdie T, Taneva S, Casselman M, Yeung M, McDaniel C, Ho W, et al. mHealth consumer apps: the case for user-centered design. Biomed Instrum Technol. 2012;Suppl:49–56. [DOI] [PubMed] [Google Scholar]
- 42.Peng P, Choiniere M, Dion D, Intrater H, Lefort S, Lynch M, et al. Challenges in accessing multidisciplinary pain treatment facilities in Canada . Can J Anaesth. 2007;54(12):977–84. [DOI] [PubMed] [Google Scholar]
- 43.Peng P, Stinson JN, Choiniere M, Dion D, Intrater H, Lefort S, et al. Dedicated multidisciplinary pain management centres for children in Canada: the current status. Can J Anaesth. 2007;54(12):985–91. [DOI] [PubMed] [Google Scholar]
- 44.Barlow JH, Ellard DR. Psycho-educational interventions for children with chronic disease, parents and siblings: an overview of the research evidence base. Child Care Health Dev. 2004;30(6):637–45. [DOI] [PubMed] [Google Scholar]
- 45.Cafazzo JA, Casselman M, Hamming N, Katzman DK, Palmert MR. Design of an mHealth app for the self-management of adolescent type 1 diabetes: a pilot study. J Med Internet Res. 2012;14(3):e70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schlenz AM, Schatz J, Roberts CW. Examining Biopsychosocial Factors in Relation to Multiple Pain Features in Pediatric Sickle Cell Disease . Journal of Pediatric Psychology. 2016;41(8):930–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stevens EM, Patterson CA, Li YB, Smith-Whitley K, Barakat LP. Mistrust of Pediatric Sickle Cell Disease Clinical Trials Research. Am J Prev Med. 2016;51(1 Suppl 1):S78–86. [DOI] [PMC free article] [PubMed] [Google Scholar]