Abstract
Background
Visceral adiposity indicators and the product of triglyceride and fasting plasma glucose (TyG) index-related parameters are effective surrogate markers for insulin resistance (IR) and are predictors of metabolic syndrome and diabetes mellitus. However, their genetic determinants have not been previously reported. Pleiotropic associations of LIPC variants have been observed in lipid profiles and atherosclerotic cardiovascular diseases. We aimed to investigate LIPC polymorphisms as the genetic determinants of adiposity status, visceral adiposity indicators and TyG index-related parameters.
Methods
A total of 592 participants from Taiwan were genotyped for three LIPC single nucleotide polymorphisms (SNPs).
Results
The LIPC SNPs rs2043085 and rs1532085 were significantly associated with body mass index (BMI), waist circumference (WC), lipid accumulation product, visceral adiposity index, and TyG index-related parameters [including the TyG index, TyG with adiposity status (TyG-BMI), and TyG-WC index], whereas the rs1800588 SNP was only significantly associated with the TyG index. The associations became nonsignificant after further adjustment for serum TG levels. No significant association was observed between any the studied LIPC SNPs and IR status.
Conclusion
Our data revealed a pleiotropic association between the LIPC variants and visceral adiposity indicators and TyG index-related parameters, which are mediated by serum TG levels.
Electronic supplementary material
The online version of this article (10.1186/s13098-018-0383-9) contains supplementary material, which is available to authorized users.
Keywords: Hepatic lipase, Single-nucleotide polymorphism, Triglyceride level, High-density lipoprotein cholesterol level, Adiposity status, Visceral adiposity indicators, TyG index-related parameters
Background
Insulin resistance (IR) is an insensitivity state of the peripheral tissue to the effects of insulin. IR and the consequence of compensatory hyperinsulinemia are fundamental pathogenic factors for various metabolic abnormalities [1] that contribute to the development of diabetes mellitus and cardiovascular disease [2, 3]. Hyperinsulinemic euglycemic pump remains the gold standard for measuring IR, whereas homeostatic model assessment for insulin resistance (HOMA-IR) index is more practically used for determining IR in clinical application. Recently, multiple predictors for IR have also been proposed. For example, the visceral adiposity index (VAI) is an indicator of adipose tissue dysfunction and a surrogate marker for IR, which is calculated on the basis of anthropometric body mass index (BMI), waist circumference (WC), and lipid traits [4, 5]. The lipid accumulation product (LAP), a mathematical model based on a combination of serum triglyceride (TG) levels and WC, is a sensitive marker for visceral obesity that has the potential to estimate IR [6, 7]. The product of TG and fasting plasma glucose (FPG) levels (the TyG index) and the TyG index-related parameters, including the TyG with adiposity status (TyG-BMI index) and the TyG-WC index (particularly the TyG-BMI), have been proposed as simple, efficient, and clinically useful surrogate markers for early identification of IR, which may further predict the occurrence of metabolic syndromes and diabetes mellitus [8–11].
Hepatic lipase (HL, encoded by LIPC) is a glycoprotein primarily synthesized and secreted by hepatocytes, and to a lesser extent, by macrophages and other tissues [12]. HL is a member of the triacylglycerol lipase family and is a key enzyme responsible for the hydrolysis of TGs and phospholipids in nearly all lipoprotein subclasses, resulting in the generation of small and dense particles [13]. HL also plays a role in the metabolism of high density lipoprotein (HDL) by converting large, TG-rich HDL2 into small, dense HDL3; moreover, it is a negative regulator of plasma HDL cholesterol (HDL-C) levels [12]. In humans, HL overexpression considerably reduces HDL-C levels because of the increased catabolic rate, whereas HL deficiency increases the levels of large HDL2 particles, enriches HDL with TG, and causes hyperalphalipoproteinemia because of slow apolipoprotein AI catabolism [13]. Andrés-Blasco et al. [14] also showed that HL-inactivation in mice fed with a high-fat, high cholesterol diet, exhibited augmented glucose levels for HL−/− mice in feed state with similar serum insulin levels compared to wild type mice, suggesting glucose intolerance. In addition to its enzymatic functions, HL facilitates the uptake of chylomicron remnant-like particles by acting as a ligand for glycosaminoglycans on the surface of rat hepatocytes [13]. Overall, HL is crucial for reverse cholesterol transport, and it affects the lipoprotein and possibly glucose metabolism [14–16].
Recent studies have shown pleiotropic associations of LIPC single nucleotide polymorphisms (SNPs), which included lipid profiles, hepatic lipase activity, serum insulin levels, insulin sensitivity, markers for oxidative stress, metabolic syndrome and atherosclerotic cardiovascular diseases [17–26]. By contrast, controversial results have been reported on the association between LIPC SNPs and obesity [27–29]. The visceral adiposity indicators and TyG index-related parameters represent complex phenotypes with the combinations of adiposity status and metabolic traits. Therefore, in the present study, we aimed to investigate the association between LIPC SNPs and adiposity status, visceral adiposity indicators and TyG index-related parameters and IR in term of HOMA-IR in the Taiwanese population.
Methods
Participants
This study was approved by the Institutional Review Board of the Taipei Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation (IRB No. 02-XD39-090). After obtaining informed consent from the study participants, they were recruited consecutively during cardiovascular health examinations between October 2003 and September 2005 at Chang Gung Memorial Hospital. Exclusion criteria included a history of myocardial infarction, stroke, or transient ischemic attack; a history of cancer; and current renal or liver disease. Initially, 617 individuals were recruited. Participants who were younger than 18 years or who took medications for dyslipidemia and diabetes mellitus were further excluded. Finally, 592 Han Chinese participants (310 men with a mean age of 45.0 ± 9.6 years, and 282 women with a mean age of 46.7 ± 9.7 years) were enrolled for analysis. Current smokers were defined as those who regularly smoked cigarettes at the time of the survey. BMI was calculated by dividing the participants’ weight (in kilograms) by their height squared (in meters). WC was measured using an inelastic tape at the midpoint of the bottom of the rib cage and the top of the iliac crest. Obesity was defined as a BMI of 25 kg/m2 or more [30], and central obesity was defined as a WC greater than 90 cm for men and greater than 80 cm for women.
Genomic DNA extraction and genotyping
Three LIPC SNPs (rs2043085, rs1532085, and rs1800588), that have previously been found consistently associated with various metabolic phenotypes [17, 18, 22, 31, 32], were selected according to the NCBI SNP database (http://www.ncbi.nlm.nih.gov/SNP). Genotyping was then performed using TaqMan SNP Genotyping Assays from Applied Biosystems (ABI; Foster City, CA, USA). For quality control purposes, approximately 10% of the samples were regenotyped in a blinded manner, revealing identical results.
Laboratory examinations and assays
Laboratory examinations and assays were performed as previously reported [10]. In brief, serum insulin levels were measured using an immunoradiometric assay (Biosource, Nivelles, Belgium). Glucose levels were determined enzymatically using the hexokinase method, and triglyceride levels were measured by automatic enzymatic colorimetry. High-density lipoprotein cholesterol (HDLC) levels were measured enzymatically after phosphotungsten/magnesium precipitation. The HOMA-IR index was calculated as follows: HOMA-IR = fasting insulin (μU/mL) × FPG (mmol/L)/22.5 [33]. According to the previous studies [34, 35], the determination of cut-off values were made on the percentile criterion (66th to 90th according to studies) of values in the general population and the cut-off values ranged from 1.55 to 3.8, with no age or gender differences in HOMA-IR levels under 50 years old. In our study, IR was identified when the HOMA-IR index reached the upper quartile. VAI and LAP were calculated using the following formulas: VAI for men, [WC (cm)/39.68 + (1.88 × BMI)] × (TG/1.03) × (1.31/HDL-C); VAI for women, [WC (cm)/36.58 + (1.89 × BMI)] × (TG/0.81) × (1.52/HDL-C) [4]; LAP for men (WC [cm] − 65) × TG); and LAP for women, (WC [cm] − 58) × TG) [22]. Notably, both the TG and HDL-C levels were expressed in mmol/L. Finally, the TyG-related parameters were calculated as follows: TyG index, Ln [TG (mg/dL) × FPG (mg/dL)/2] [36, 37]; TyG-BMI index, TyG index × BMI; and TyG-WC index, TyG index × WC. Overall, the intra- and inter-assay variability of coefficients was within the range of 1.2–8.2% (Additional file 1: Table S1).
Statistical analysis
A Chi squared test was used to examine the differences in the categorical variables and to compare allele and genotype frequencies. The clinical characteristics of continuous variables are expressed as mean ± SD and were tested using a two-sample t test or analysis of variance. A general linear model was applied to capture the major effect of each polymorphism on clinical phenotype variables, with age, sex, smoking, use of antihypertensive medication, and HDL cholesterol levels with or without serum TG levels as confounding covariates. All biomarker levels were logarithmically transformed prior to statistical analysis to adhere to a normality assumption, and the Bonferroni method was used to correct multiple comparisons where applicable. Values of P < 0.05 obtained using two-sided tests were considered statistically significant. Missing data were approached with listwise deletion.
Results
Baseline data
The demographic data, clinical biochemical data, lipid profiles, adiposity status, visceral adiposity indicators, and TyG index-related parameters of the participants, stratified by sex, are summarized in Table 1. A significantly higher percentage of men were current smokers (P < 0.001) than were women. In addition, men had significantly higher BMIs (P < 0.001), WCs (P < 0.001), TG (P < 0.001), circulating levels of FPG (P < 0.001), serum insulin (P = 0.01), HOMA-IR (P < 0.001), LAP (P < 0.001), VAI (P < 0.001), TyG index (P < 0.001), TyG-BMI index (P < 0.001), and TyG-WC index (P < 0.001), than did women. By contrast, circulating HDL-C (P < 0.001) was lower in men than in women. For the status of glucose metabolism, the proportion of individuals are presented below: fasting glucose levels of 464 subjects are under 100 mg/dL, 108 subjects show fasting glucose levels ranging from 100 to 125 mg/dL and another 20 subjects have greater than 126 mg/dL respectively.
Table 1.
Clinical and biochemical characteristics of the study population
| Total | Men | Women | P value | |
|---|---|---|---|---|
| Number | 592 | 310 | 282 | |
| Age (years) | 45.8 ± 9.7 | 45.0 ± 9.6 | 46.7 ± 9.7 | 0.035 |
| BMI (kg/m2) | 24.3 ± 3.5 | 24.9 ± 3.2 | 23.6 ± 3.7 | 2.97 × 10−7 |
| Waist circumference (cm) | 85.0 ± 9.6 | 87.9 ± 7.8 | 81.8 ± 10.5 | 1.05 × 10−16 |
| Current smokers (number; %) | 115; 19.4 | 104; 33.5 | 11; 3.9 | 4.02 × 10−21 |
| Systolic blood pressurea (mmHg) | 113.1 ± 16.1 | 114.0 ± 14.3 | 112.1 ± 17.8 | 0.076 |
| Diastolic blood pressurea (mmHg) | 75.0 ± 9.9 | 76.8 ± 9.7 | 73.1 ± 9.9 | 6.9 × 10−6 |
| HDL-C (mg/dL) | 55.4 ± 14.3 | 49.9 ± 12.0 | 61.5 ± 14.2 | 2.16 × 10−25 |
| TG (mg/dL) | 142.5 ± 119.1 | 172.9 ± 148.0 | 109.2 ± 60.1 | 2.26 × 10−15 |
| Fasting plasma glucose (mg/dL) | 96.2 ± 22.6 | 99.0 ± 26.0 | 93.2 ± 17.8 | 5.40 × 10−5 |
| Fasting serum insulin (µU/mL) | 9.2 ± 4.9 | 9.8 ± 5.6 | 8.6 ± 3.9 | 0.005 |
| HOMA-IR | 2.2 ± 1.4 | 2.4 ± 1.6 | 2.0 ± 1.1 | 1.09 × 10−4 |
| LAP | 3560.2 ± 3902.0 | 4240.1 ± 4780.9 | 2812.8 ± 2412.0 | 1.30 × 10−7 |
| VAI | 196.1 ± 245.0 | 265.9 ± 308.9 | 119.4 ± 100.4 | 8.78 × 10−29 |
| TyG index | 8.6 ± 0.6 | 8.8 ± 0.7 | 8.4 ± 0.5 | 2.26 × 10−15 |
| TyG-BMI | 210.3 ± 38.3 | 220.5 ± 35.4 | 199.0 ± 38.2 | 1.24 × 10−13 |
| TyG-WC | 735.7 ± 116.8 | 777.3 ± 102.8 | 690.0 ± 114.3 | 6.27 × 10−23 |
Continuous variables are presented as mean ± SD. HDL-C, TG, LAP, VAI, TyG, TyG-BMI and TyG-WC values were logarithmically transformed before statistical testing to meet the assumption of normal distributions; however, the untransformed data are shown
BMI body mass index, HDL-C high-density lipoprotein cholesterol, TG triglycerides, HOMA-IR homeostasis model assessment of insulin resistance, LAP lipid accumulation product, VAI visceral adiposity index, TyG index the product of triglycerides and fasting glucose, WC waist circumference
aOnly those participants not using antihypertensive drugs were analyzed
Relationship between LIPC SNPs and adiposity status
To determine the effects of LIPC genotypes on adiposity status, we created an additive model by using HDL-C, TG, BMI and WC as variables of interest (Table 2). After adjustment for age, sex, smoking status, and use of antihypertensive medications, all three SNPs were more significantly associated with TG or HDL-C levels after additional adjustment for HDL-C or TG levels (all P = 0.012 for HDL-C and P = 3.4 × 10−5, 2.6 × 10−5 and 0.012 for TG, respectively, after the Bonferroni correction).
Table 2.
Association of LIPC SNPs with adiposity status
| SNPs | Genotypes | P* | Adjusted P | ||
|---|---|---|---|---|---|
| MM | Mm | mm | |||
| rs2043085 | CC | CT | TT | ||
| BMI (kg/m2) | 23.7 ± 3.3 | 24.4 ± 3.6 | 24.8 ± 3.4 | 0.002 | 0.024 |
| WC (cm) | 83.6 ± 9.2 | 85.1 ± 9.7 | 87.2 ± 9.8 | 2.8 × 10−4 | 3.4 × 10−3 |
| HDL-C (mg/dL) | 54.5 ± 14.1 | 55.9 ± 14.6 | 55.2 ± 14.2 | 0.001# | 0.012 |
| TG (mg/dL) | 119.6 ± 65.4 | 144.8 ± 112.1 | 169.2 ± 175.7 | 2.8 × 10−6 | 3.4 × 10−5 |
| rs1532085 | GG | GA | AA | ||
| BMI (kg/m2) | 23.8 ± 3.3 | 24.5 ± 3.6 | 24.7 ± 3.4 | 0.006 | 0.072 |
| WC (cm) | 83.6 ± 9.3 | 85.2 ± 9.6 | 86.9 ± 9.9 | 0.001 | 0.012 |
| HDL-C (mg/dL) | 54.5 ± 14.0 | 55.8 ± 14.5 | 55.3 ± 14.5 | 0.001# | 0.012 |
| TG (mg/dL) | 119.6 ± 65.5 | 144.6 ± 111.5 | 171.0 ± 179.8 | 2.2 × 10−6 | 2.6 × 10−5 |
| rs1800588 | CC | CT | TT | ||
| BMI (kg/m2) | 24.4 ± 3.5 | 24.4 ± 3.5 | 23.6 ± 3.4 | 0.432 | 1.0 |
| WC (cm) | 85.5 ± 9.8 | 85.2 ± 9.4 | 83.4 ± 9.8 | 0.631 | 1.0 |
| HDL-C (mg/dL) | 53.9 ± 13.1 | 55.7 ± 14.7 | 58.3 ± 16.1 | 0.001# | 0.012 |
| TG (mg/dL) | 135.1 ± 96.1 | 147.9 ± 139.7 | 146.8 ± 105.8 | 0.001 | 0.012 |
Abbreviations as in Table 1
MM homozygosity of major allele, Mm heterozygosity, mm homozygosity of minor allele
Adjusted P: the P value were shown with Bonferroni corrections, n = 12
P*: adjusted for age, sex, current smoke, hypertension medicine, HDL-C
#Adjusted for age, sex, current smoke, hypertension medicine, TG
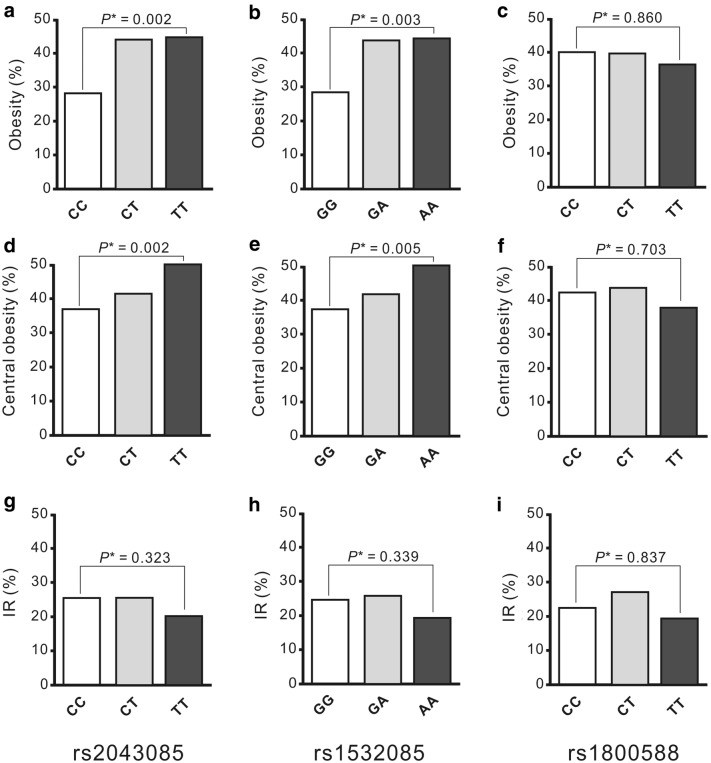
Moreover, after adjustment for age, sex, smoking status, use of antihypertensive medications, and HDL-C levels, the participants carrying the minor alleles of the studied SNPs exhibited a trend of higher BMIs (P = 0.024 and 0.072 for rs2043085 and rs1532085, respectively, after the Bonferroni correction), higher WCs (P = 3.4 × 10−3, and 0.012 for rs2043085 and rs1532085, respectively, after the Bonferroni correction), and significantly higher frequencies of obesity and central obesity statuses, compared with those carrying the major alleles (Fig. 1). By contrast, no significant association was observed between the rs1800588 genotype and adiposity status.
Fig. 1.
Adiposity status and insulin resistance (IR) according to LIPC SNP genotypes. a–f Significant associations were found between LIPC SNPs rs2043085 and rs1532085, but not rs1800588, genotypes and adiposity status, including obesity and central obesity (All P < 0.01). g–i No significant association of LIPC genotypes and IR were noted
Associations between LIPC SNPs and visceral adiposity indicators
To determine whether the LIPC genotypes influenced visceral adiposity indicators, we analyzed the LAP and VAI (Table 3). After adjustment for age, sex, smoking status, use of antihypertensive medications, and HDL-C levels with the Bonferroni correction, participants carrying the minor alleles of the rs2043085 and rs1532085 genotypes exhibited a significant trend of higher LAP (P = 3.2 × 10−6 and 8.1 × 10−6 for rs2043085 and rs1532085, respectively) and VAI (P = 4.3 × 10−6 and 5.2 × 10−6 for rs2043085 and rs1532085, respectively). However, the associations became nonsignificant after further adjustment for serum TG levels. By contrast, no significant association between the rs1800588 genotype and visceral adiposity indicators was observed.
Table 3.
Association of LIPC SNPs with visceral adiposity indicators, TyG index related parameters and insulin resistance
| SNPs | Genotypes | P* (adjusted P) | P** (adjusted P) | ||
|---|---|---|---|---|---|
| MM | Mm | mm | |||
| rs2043085 | CC | CT | TT | ||
| LAP | 2863.0 ± 2180.5 | 3609.6 ± 3537.8 | 4451.0 ± 5943.0 | 1.8 × 10−7 (3.2 × 10−6) | 0.016 (0.288) |
| VAI | 183.8 ± 132.6 | 219.0 ± 203.6 | 266.4 ± 381.5 | 2.4 × 10−7 (4.3 × 10−6) | 0.011 (0.198) |
| TyG | 8.5 ± 0.6 | 8.6 ± 0.7 | 8.8 ± 0.7 | 1.7 × 10−5 (3.1 × 10−4) | 0.542 |
| TyG-BMI | 202.5 ± 35.0 | 211.7 ± 39.7 | 217.9 ± 38.1 | 2.0 × 10−5 (3.6 × 10−4) | 0.026 (0.468) |
| TyG-WC | 713.2 ± 109.5 | 736.9 ± 118.3 | 765.7 ± 117.6 | 1.4 × 10−6 (2.5 × 10−5) | 0.013 (0.234) |
| HOMA-IR | 2.2 ± 1.3 | 2.2 ± 1.4 | 2.3 ± 1.5 | 0.422 | 0.818 |
| rs1532085 | GG | GA | AA | ||
| LAP | 2876.5 ± 2181.0 | 3613.7 ± 3519.0 | 4470.7 ± 6085.4 | 4.5 × 10−7 (8.1 × 10−6) | 0.040 (0.720) |
| VAI | 184.1 ± 132.1 | 218.5 ± 202.5 | 270.1 ± 390.5 | 2.9 × 10−7 (5.2 × 10−6) | 0.029 (0.522) |
| TyG | 8.5 ± 0.6 | 8.6 ± 0.7 | 8.8 ± 0.7 | 1.0 × 10−5 (1.8 × 10−4) | 0.701 |
| TyG-BMI | 202.8 ± 35.1 | 211.9 ± 39.5 | 217.3 ± 38.8 | 5.1 × 10−5 (9.2 × 10−4) | 0.051 (0.918) |
| TyG-WC | 713.4 ± 110.4 | 738.4 ± 117.3 | 763.2 ± 119.7 | 4.7 × 10−6 (8.5 × 10−5) | 0.034 (0.612) |
| HOMA-IR | 2.2 ± 1.3 | 2.2 ± 1.4 | 2.3 ± 1.5 | 0.449 | 0.766 |
| rs1800588 | CC | CT | TT | ||
| LAP | 3385.6 ± 3198.8 | 3746.4 ± 4593.1 | 3514.7 ± 3246.5 | 0.026 (0.468) | 0.288 |
| VAI | 208.8 ± 184.7 | 230.6 ± 290.1 | 207.7 ± 176.1 | 0.003 (0.054) | 0.163 |
| TyG | 8.6 ± 0.6 | 8.6 ± 0.7 | 8.8 ± 0.7 | 4.6 × 10−4 (0.008) | 0.521 |
| TyG-BMI | 210.2 ± 37.4 | 211.9 ± 39.0 | 205.6 ± 39.2 | 0.455 | 0.242 |
| TyG-WC | 735.2 ± 116.2 | 739.7 ± 115.5 | 726.4 ± 125.0 | 0.182 | 0.303 |
| HOMA-IR | 2.2 ± 1.4 | 2.2 ± 1.4 | 2.2 ± 1.5 | 0.219 | 0.632 |
Abbreviations as in Table 1
MM homozygosity of major allele, Mm heterozygosity, mm homozygosity of minor allele
Adjusted P: the P value were shown with Bonferroni corrections, n = 18
P*: adjusted for age, sex, current smoke, hypertension medicine, HDL-C; P**: Further adjusted for TG
Associations between LIPC SNPs and TyG-related parameters and IR status
To determine whether the LIPC genotypes influenced TyG-related parameters, we analyzed the TyG, TyG-BMI, and TyG-WC indices (Table 3). After adjustment for age, sex, smoking status, use of antihypertensive medications, and HDL-C levels with the Bonferroni correction, the participants carrying the minor alleles of the rs2043085 and rs1532085 genotypes tended to have a significantly higher TyG index (P = 3.1 × 10−4 and 1.8 × 10−4 for rs2043085 and rs1532085, respectively), TyG-BMI index (P = 3.6 × 10−4 and 9.2 × 10−4 for rs2043085 and rs1532085, respectively), and TyG-WC index (P = 2.5 × 10−5 and 8.5 × 10−5 for rs2043085 and rs1532085, respectively). In addition, significant associations were observed between the rs1800588 genotype and TyG index (P = 0.008 after the Bonferroni correction); however, these associations became nonsignificant after further adjustment for serum TG levels. By contrast, no significant association between the rs1800588 genotype and the TyG-BMI and TyG-WC indices was observed. Furthermore, no significant association between LIPC SNPs and the HOMA-IR and IR statuses was noted (Table 3 and Fig. 1).
Associations between LIPC SNPs and each quartile of the visceral adiposity indicators and TyG index-related parameters
To confirm the effect of LIPC genotypes on the visceral adiposity indicators and TyG index-related parameters, we further analyzed the frequencies of the additive model of LIPC genotypes in each quartile of the studied parameters (Additional file 1: Table S2). After adjustment for age, sex, smoking status, use of antihypertensive medications and HDL-C levels with the Bonferroni correction, significant P values were obtained for the rs2043085 and rs1532085 SNPs (all P < 0.01). The participants carrying the minor alleles exhibited a trend of higher frequencies in the upper quartiles of the studied parameters. By contrast, no significant difference in the rs1800588 genotype frequencies was observed between the quartiles of the studied parameters.
Discussion
This study investigated the association between LIPC SNPs and adiposity status, visceral adiposity indicators, and TyG index-related parameters, and HOMA-IR in the Taiwanese population. Our data revealed at least a trend of significant association between two LIPC SNPs, rs2043085 and rs1532085, and BMI, WC, and adiposity status. In addition, these LIPC SNPs were associated with visceral adiposity indicators and TyG index-related parameters, either in continuous variables or in quartiles which were mediated by serum TG levels. The pleiotropic associations further support a complex interaction between LIPC SNPs and the risk of metabolic syndromes, diabetes mellitus and future atherosclerotic cardiovascular disease.
Previous studies have reported controversial results on the association between HL and obesity. For example, mice lacking HL were reported to be lean and protected against diet-induced obesity and hepatic steatosis in one study [38]. The influence of LIPC alleles on obesity was investigated through a reciprocal hemizygosity analysis [39]. Additionally, several studies have revealed that LIPC SNPs, mostly promoter SNPs, are not associated with BMI. However, one previous study [29] demonstrated the association between LIPC promoter SNPs and BMI. Mägi et al. [40] reported that the rs2043085 SNP was the most significant SNP in the LIPC locus associated with lipid traits and BMI through a reverse regression approach by using software for correlated phenotype analysis (SCOPA) and META-SCOPA software. Our data revealed that SNPs rs2043085 and rs1532085 were significantly associated with adiposity status. Differential associations between the studied SNPs in adiposity status are interesting. SNP rs1800588 is the promoter LIPC SNP that has been most widely reported to be associated with various phenotypes [17–21]. LIPC is expressed only in the liver, and both rs1532085 and rs1800588 were associated with the expression of LIPC [41]. LIPC SNP rs2043085 exhibited high linkage disequilibrium with rs1532085 and either of them has been shown to be the most significant SNP in the LIPC locus associated with various phenotypes in several genome-wide association studies (GWASs) [26, 42, 43]. Using a bivariate genome-wide approach for seven studies of the STAMPEED consortium, comprising 22,161 participants of European ancestry, Kraja et al. [26] also showed variants in the LIPC gene as one of the loci associated with metabolic syndrome. Our data suggested that the haplotype block, combining all the three studied SNPs, may be more crucial for future studies as a marker for atherosclerotic cardiovascular disease.
The combined associations of LIPC SNPs with insulin surrogate markers that based on both metabolic and adiposity status are noteworthy. Shared common variants have similarly been reported between lipid genes and glucose metabolism, inflammation, BMI, cardiometabolic traits, and coronary artery disease [20, 40, 44–46]. Pickrell et al. [21] developed a method of detecting pairs of traits that exhibited an asymmetry in the effect sizes of associated variants, which is more consistent with a causal relationship between the traits and the authors indicated that an elevated BMI causally increases TG levels, but the reverse is not true. By contrast, we have previously demonstrated that LIPC SNPs were associated with serum TG and HDL cholesterol levels independently of the BMI [17]. These results suggest the independence of association between LIPC SNPs and metabolic and adiposity status.
The genetic determinants of the visceral adiposity indicators and TyG index-related parameters have not been previously reported. These parameters are complex traits derived from simple phenotypes, including metabolic phenotypes with or without adiposity status, with the serum TG level as the most common component of all indices. Thus, a polymorphism associated with both adiposity status and serum TG levels may be associated with these parameters. Furthermore, the associations became nonsignificant after adjustment for serum TG levels. Because of the involvement of serum TG levels in each parameter, other genetic determinants of serum TG levels may also be the genetic determinants of these parameters; however, further research is required to confirm this phenomenon.
The term pleiotropy is used to describe the phenomenon by which genetic variation at a single locus exerts an effect on more than one phenotype. Pleiotropy observed in genetic association studies can provide insight into the shared biology underlying a spectrum of phenotypes. Pleiotropy may be caused by the third variable with mediational, interactive, reverse causal, or suppressive effect [47–49]. By using the National Human Genome Research Institute’s catalog of a published GWAS, Sivakumaran et al. [50] reported that 4.6% of the SNPs and 16.9% of the genes exhibited the cross-phenotype effect. However, with the growing number of GWASs, this effect is likely to be underestimated. Some chromosomal regions, including the gene loci near LIPC, appear to be particular foci for association with multiple phenotypes [20, 21]. Moreover, different LIPC SNPs have been associated with levels of circulating malondialdehyde-modified low-density lipoprotein [22]; phospholipids and sphingolipids [51]; folate and vitamin E [52]; BMI [29, 39]; metabolic syndrome [26]; and diseases such as advanced age-related macular degeneration [43, 53, 54], coronary artery disease [18], and myocardial infarction [19]. Our data further revealed that the LIPC SNPs are associated with adiposity status, visceral adiposity indicators, and TyG index-related parameters in the Taiwanese population. Visceral obesity has been shown to be associated with IR and a high risk of developing type 2 diabetes after myocardial infarction [55]. Several human studies also indicate that these surrogated markers for IR may identify individuals at a high risk of developing cardiovascular events and mortality [56–62]. Thus, our findings implicated that the genetic determinants of these parameters is crucial in providing a method for identifying high-risk populations of cardiovascular diseases for preventive medicine.
By contrast, IR is influenced by multiple factors, including lipid profiles, obesity and inflammation, in which LIPC SNPs are not associated with circulating inflammatory markers in our study population (data not shown). We also found no significant association between any the studied LIPC SNPs and IR in term of HOMA-IR.
The main limitation of this study is its medium sample size and relatively low number of genotyped participants. This limitation may be more marked because a complex trait was central to this analysis. Nevertheless, such associations may be attributed to the mediational effect of serum TG levels. Furthermore, only three LIPC SNPs were analyzed, which suggests an incomplete coverage of LIPC SNPs; hence, the study did not represent all genetic variations of LIPC.
Conclusions
This study provided the first evidence of genetic determinants of various visceral adiposity indicators and TyG index-related parameters. Previous studies have demonstrated that the genetic determinants of serum TG levels determine the risk of coronary artery disease [21, 63]. Additional studies may be necessary to elucidate whether the genetic determinants of serum TG levels are also crucial in pleiotropic genetic associations for visceral adiposity indicators and TyG index-related parameters through mediational effects.
Additional file
Additional file 1: Table S1. Inter- and intra-assay variability measures of the biochemistry. Table S2. Associations of the LIPC SNPs with each quartile of visceral adiposity indicators and TyG index related parameters.
Authors’ contributions
M-ST and SW prepared the DNA samples, participated in genotyping, performed statistical analysis and drafted the manuscript. L-KE and H-HC assisted in study design and contributed to the discussion. L-AH assisted in study design and performed and corrected statistical analysis. Y-LK designed the study, drafted and revised the manuscript. All authors read and approved the final manuscript.
Acknowledgements
We greatly appreciate technical support from the Core Laboratory of the Taipei Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The data are within the manuscript.
Consent for publication
Not applicable.
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of Taipei Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation. After obtaining informed consent, participants from the general population were consecutively recruited during routine cardiovascular health examinations.
Funding
This study was supported by grants from the Taipei Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation (TCRD-TPE-103-RT-2, TCRD-I103-01-01, TCRD-TPE-MOST-103-01, TCRD-TPE-MOST-104-09, TCRD-TPE-106-C1-1, TCRD-TPE-106-RT-3), grants from the Tzu Chi University, Hualien, Taiwan (TCMMP104-06-03), Grants from the National Science Council (MOST 104-2314-B-303-013-MY3) to Y. L. Ko, and grants from the Taipei Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation (TCRD-TPE-103-22, TCRD-TPE-104-18, TCRD-TPE-106-46, TCRD-TPE-106-46(2/2)) to M. S. Teng.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- SNPs
single nucleotide polymorphisms
- BMI
body mass index
- WC
waist circumference
- IR
insulin resistance
- HDL-C
high-density lipoprotein cholesterol
- LDL-C
low-density lipoprotein cholesterol
- TG
triglycerides
- LAP
lipid accumulation product
- VAI
visceral adiposity index
- TyG index
the product of TG and fasting plasma glucose levels
- TyG-BMI
TyG index with body mass index
- TyG-WC
TyG index with waist circumference
References
- 1.Matthaei S, Stumvoll M, Kellerer M, Häring HU. Pathophysiology and pharmacological treatment of insulin resistance. Endocr Rev. 2000;21:585–618. doi: 10.1210/edrv.21.6.0413. [DOI] [PubMed] [Google Scholar]
- 2.Lillioja S, Mott DM, Spraul M, Ferraro R, Foley JE, Ravussin E, et al. Insulin resistance and insulin secretory dysfunction as precursors of non-insulin-dependent diabetes mellitus: prospective studies of Pima Indians. N Engl J Med. 1993;329:1988–1992. doi: 10.1056/NEJM199312303292703. [DOI] [PubMed] [Google Scholar]
- 3.Rader DJ. Effect of insulin resistance, dyslipidemia, and intra-abdominal adiposity on the development of cardiovascular disease and diabetes mellitus. Am J Med. 2007;120:S12–S18. doi: 10.1016/j.amjmed.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 4.Amato MC, Giordano C, Galia M, Criscimanna A, Vitabile S, Midiri M, et al. Visceral adiposity index: a reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care. 2010;33:920–922. doi: 10.2337/dc09-1825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ciresi A, Amato MC, Pizzolanti G, Giordano Galluzzo C. Visceral adiposity index is associated with insulin sensitivity and adipocytokine levels in newly diagnosed acromegalic patients. J Clin Endocrinol Metab. 2012;97:2907–2915. doi: 10.1210/jc.2012-1518. [DOI] [PubMed] [Google Scholar]
- 6.Kahn HS. The lipid accumulation product is better than BMI for identifying diabetes: a population-based comparison. Diabetes Care. 2006;29:151–153. doi: 10.2337/diacare.29.01.06.dc05-1805. [DOI] [PubMed] [Google Scholar]
- 7.Ioachimescu AG, Brennan DM, Hoar BM, Hoogwerf BJ. The lipid accumulation product and all-cause mortality in patients at high cardiovascular risk: a PreCIS database study. Obesity (Silver Spring) 2010;18:1836–1844. doi: 10.1038/oby.2009.453. [DOI] [PubMed] [Google Scholar]
- 8.Du T, Yuan G, Zhang M, Zhou X, Sun X, Yu X. Clinical usefulness of lipid ratios, visceral adiposity indicators, and the triglycerides and glucose index as risk markers of insulin resistance. Cardiovasc Diabetol. 2014;13:146. doi: 10.1186/s12933-014-0146-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee SH, Han K, Yang HK, Kim MK, Yoon KH, Kwon HS, et al. Identifying subgroups of obesity using the product of triglycerides and glucose: the Korea national health and nutrition examination survey, 2008–2010. Clin Endocrinol (Oxf) 2015;82:213–220. doi: 10.1111/cen.12502. [DOI] [PubMed] [Google Scholar]
- 10.Er LK, Wu S, Chou HH, Hsu LA, Teng MS, Sun YC, et al. Triglyceride glucose-body mass index is a simple and clinically useful surrogate marker for insulin resistance in nondiabetic individuals. PLoS ONE. 2016;11:e0149731. doi: 10.1371/journal.pone.0149731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zheng S, Shi S, Ren X, Han T, Li Y, Chen Y, et al. Triglyceride glucose-waist circumference, a novel and effective predictor of diabetes in first-degree relatives of type 2 diabetes patients: cross-sectional and prospective cohort study. J Transl Med. 2016;14:260. doi: 10.1186/s12967-016-1020-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kobayashi J, Miyashita K, Nakajima K, Mabuchi H. Hepatic lipase: a comprehensive view of its role on plasma lipid and lipoprotein metabolism. J Atheroscler Thromb. 2015;22:1001–1011. doi: 10.5551/jat.31617. [DOI] [PubMed] [Google Scholar]
- 13.Annema W, Tietge UJ. Role of hepatic lipase and endothelial lipase in high-density lipoprotein-mediated reverse cholesterol transport. Curr Atheroscler Rep. 2011;13:257–265. doi: 10.1007/s11883-011-0175-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Andrés-Blasco I, Herrero-Cervera A, Vinué Á, Martínez-Hervás S, Piqueras L, et al. Hepatic lipase deficiency produces glucose intolerance, inflammation and hepatic steatosis. J Endocrinol. 2015;227:179–191. doi: 10.1530/JOE-15-0219. [DOI] [PubMed] [Google Scholar]
- 15.Cohen JC, Vega GL, Grundy SM. Hepatic lipase: new insights from genetic and metabolic studies. Curr Opin Lipidol. 1999;10:259–267. doi: 10.1097/00041433-199906000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Thuren T. Hepatic lipase and HDL metabolism. Curr Opin Lipidol. 2000;2000(11):277–283. doi: 10.1097/00041433-200006000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Ko YL, Hsu LA, Hsu KH, Ko YH, Lee YS. The interactive effects of hepatic lipase gene promoter polymorphisms with sex and obesity on high-density-lipoprotein cholesterol levels in Taiwanese–Chinese. Atherosclerosis. 2004;172:135–142. doi: 10.1016/j.atherosclerosis.2003.09.013. [DOI] [PubMed] [Google Scholar]
- 18.Zhang C, Lopez-Ridaura R, Rimm EB, Li T, Hunter DJ, et al. Genetic variation in the hepatic lipase gene and the risk of coronary heart disease among US diabetic men: potential interaction with obesity. Diabetologia. 2006;49:1552–1559. doi: 10.1007/s00125-006-0235-2. [DOI] [PubMed] [Google Scholar]
- 19.Ahmad T, Chasman DI, Buring JE, Lee IM, Ridker PM, et al. Physical activity modifies the effect of LPL, LIPC, and CETP polymorphisms on HDL-C levels and the risk of myocardial infarction in women of European ancestry. Circ Cardiovasc Genet. 2011;4:74–80. doi: 10.1161/CIRCGENETICS.110.957290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Price AL, Spencer CC, Donnelly P. Progress and promise in understanding the genetic basis of common diseases. Proc Biol Sci. 2015;282:20151684. doi: 10.1098/rspb.2015.1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pickrell JK, Berisa T, Liu JZ, Ségurel L, Tung JY, Hinds DA. Detection and interpretation of shared genetic influences on 42 human traits. Nat Genet. 2016;48:709–717. doi: 10.1038/ng.3570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yamazaki K, Bujo H, Taira K, Itou N, Shibasaki M, Takahashi K, et al. Increased circulating malondialdehyde-modified LDL in the patients with familial combined hyperlipidemia and its relation with the hepatic lipase activity. Atherosclerosis. 2004;172:181–187. doi: 10.1016/j.atherosclerosis.2003.05.001. [DOI] [PubMed] [Google Scholar]
- 23.Pihlajamäki J, Karjalainen L, Karhapää P, Vauhkonen I, Taskinen MR, et al. G-250A substitution in promoter of hepatic lipase gene is associated with dyslipidemia and insulin resistance in healthy control subjects and in members of families with familial combined hyperlipidemia. Arterioscler Thromb Vasc Biol. 2000;20:1789–1795. doi: 10.1161/01.ATV.20.7.1789. [DOI] [PubMed] [Google Scholar]
- 24.Waterworth DM, Jansen H, Nicaud V, Humphries SE, Talmud PJ, EARSII Study Group Interaction between insulin (VNTR) and hepatic lipase (LIPC-514C>T) variants on the response to an oral glucose tolerance test in the EARSII group of young healthy men. Biochim Biophys Acta. 2005;1740:375–381. doi: 10.1016/j.bbadis.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 25.Andrés-Blasco I, Vinué Á, Herrero-Cervera A, Martínez-Hervás S, Nuñez L, et al. Hepatic lipase inactivation decreases atherosclerosis in insulin resistance by reducing LIGHT/lymphotoxin β-receptor pathway. Thromb Haemost. 2016;116:379–393. doi: 10.1160/TH15-10-0773. [DOI] [PubMed] [Google Scholar]
- 26.Kraja AT, Vaidya D, Pankow JS, Goodarzi MO, Assimes TL, Kullo IJ, et al. A bivariate genome-wide approach to metabolic syndrome: STAMPEED consortium. Diabetes. 2011;60:1329–1339. doi: 10.2337/db10-1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Murtomäki S, Tahvanainen E, Antikainen M, Tiret L, Nicaud V, Jansen H, et al. Hepatic lipase gene polymorphisms influence plasma HDL levels: results from Finnish EARS participants. European atherosclerosis research study. Arterioscler Thromb Vasc Biol. 1997;17:1879–1884. doi: 10.1161/01.ATV.17.10.1879. [DOI] [PubMed] [Google Scholar]
- 28.St-Pierre J, Miller-Felix I, Paradis ME, Bergeron J, Lamarche B, Després JP, et al. Visceral obesity attenuates the effect of the hepatic lipase −514C>T polymorphism on plasma HDL-cholesterol levels in French–Canadian men. Mol Genet Metab. 2003;78:31–36. doi: 10.1016/S1096-7192(02)00223-8. [DOI] [PubMed] [Google Scholar]
- 29.Wang H, Zhang D, Ling J, Lu W, Zhang S, Zhu Y, et al. Gender specific effect of LIPC C-514T polymorphism on obesity and relationship with plasma lipid levels in Chinese children. J Cell Mol Med. 2015;19:2296–2306. doi: 10.1111/jcmm.12663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tan CE, Ma S, Wai D, Chew SK, Tai ES. Can we apply the national cholesterol education program adult treatment panel definition of the metabolic syndrome to Asians? Diabetes Care. 2004;27:1182–1186. doi: 10.2337/diacare.27.5.1182. [DOI] [PubMed] [Google Scholar]
- 31.Lu X, Huang J, Mo Z, He J, Wang L, Yang X, et al. Genetic susceptibility to lipid levels and lipid change over time and risk of incident hyperlipidemia in Chinese populations. Circ Cardiovasc Genet. 2016;9:37–44. doi: 10.1161/CIRCGENETICS.115.001096. [DOI] [PubMed] [Google Scholar]
- 32.Shohet RV, Vega GL, Bersot TP, Mahley RW, Grundy SM, Guerra R, et al. Sources of variability in genetic association studies: insights from the analysis of hepatic lipase (LIPC) Hum Mutat. 2002;19:536–542. doi: 10.1002/humu.10079. [DOI] [PubMed] [Google Scholar]
- 33.Bonora E, Targher G, Alberiche M, Bonadonna RC, Saggiani F, Zenere MB, et al. Homeostasis model assessment closely mirrors the glucose clamp technique in the assessment of insulin sensitivity: studies in subjects with various degrees of glucose tolerance and insulin sensitivity. Diabetes Care. 2000;23:57–63. doi: 10.2337/diacare.23.1.57. [DOI] [PubMed] [Google Scholar]
- 34.Gayoso-Diz P, Otero-González A, Rodriguez-Alvarez MX, Gude F, García F, De Francisco A, Quintela AG. Insulin resistance (HOMA-IR) cut-off values and the metabolic syndrome in a general adult population: effect of gender and age: EPIRCE cross-sectional study. BMC Endocr Disord. 2013;13:47. doi: 10.1186/1472-6823-13-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gayoso-Diz P, Otero-Gonzalez A, Rodriguez-Alvarez MX, Gude F, Cadarso-Suarez C, García F, De Francisco A. Insulin resistance index (HOMA-IR) levels in a general adult population: curves percentile by gender and age. The EPIRCE study. Diabetes Res Clin Pract. 2011;94(1):146–155. doi: 10.1016/j.diabres.2011.07.015. [DOI] [PubMed] [Google Scholar]
- 36.Simental-Mendia LE, Rodriguez-Moran M, Guerrero-Romero F. The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects. Metab Syndr Relat Disord. 2008;6:299–304. doi: 10.1089/met.2008.0034. [DOI] [PubMed] [Google Scholar]
- 37.Guerrero-Romero F, Simental-Mendia LE, Gonzalez-Ortiz M, Martinez-Abundis E, Ramos-Zavala MG, Hernandez-Gonzalez SO, et al. The product of triglycerides and glucose, a simple measure of insulin sensitivity. Comparison with the euglycemic hyperinsulinemic clamp. J Clin Endocrinol Metab. 2010;95:3347–3351. doi: 10.1210/jc.2010-0288. [DOI] [PubMed] [Google Scholar]
- 38.Chiu HK, Qian K, Ogimoto K, Morton GJ, Wisse BE, Agrawal N, et al. Mice lacking hepatic lipase are lean and protected against diet-induced obesity and hepatic steatosis. Endocrinology. 2010;151:993–1001. doi: 10.1210/en.2009-1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Farahani P, Fisler JS, Wong H, Diament AL, Yi N, Warden CH. Reciprocal hemizygosity analysis of mouse hepatic lipase reveals influence on obesity. Obes Res. 2004;12:292–305. doi: 10.1038/oby.2004.37. [DOI] [PubMed] [Google Scholar]
- 40.Mägi R, Suleimanov YV, Clarke GM, Kaakinen M, Fischer K, Prokopenko I, et al. SCOPA and META-SCOPA: software for the analysis and aggregation of genome-wide association studies of multiple correlated phenotypes. BMC Bioinform. 2017;11(18):25. doi: 10.1186/s12859-016-1437-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Folkersen L, van’t Hooft F, Chernogubova E, Agardh HE, Hansson GK, Hedin U, et al. Association of genetic risk variants with expression of proximal genes identifies novel susceptibility genes for cardiovascular disease. Circ Cardiovasc Genet. 2010;3:365–373. doi: 10.1161/CIRCGENETICS.110.948935. [DOI] [PubMed] [Google Scholar]
- 42.Benner C, Spencer CC, Havulinna AS, Salomaa V, Ripatti S, Pirinen M. FINEMAP: efficient variable selection using summary data from genome-wide association studies. Bioinformatics. 2016;32:1493–1501. doi: 10.1093/bioinformatics/btw018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fritsche LG, Igl W, Bailey JN, Grassmann F, Sengupta S, Bragg-Gresham JL, et al. A large genome-wide association study of age-related macular degeneration highlights contributions of rare and common variants. Nat Genet. 2016;48:134–143. doi: 10.1038/ng.3448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Li N, van der Sijde MR, LifeLines Cohort Study Group. Bakker SJ, Dullaart RP, van der Harst P, Gansevoort RT, et al. Pleiotropic effects of lipid genes on plasma glucose, HbA1c, and HOMA-IR levels. Diabetes. 2014;63:3149–3158. doi: 10.2337/db13-1800. [DOI] [PubMed] [Google Scholar]
- 45.Ligthart S, Vaez A, Hsu YH, Inflammation Working Group of the CHARGE Consortium. PMI-WG-XCP. LifeLines Cohort Study. Stolk R, Uitterlinden AG, et al. Bivariate genome-wide association study identifies novel pleiotropic loci for lipids and inflammation. BMC Genomics. 2016;10(17):443. doi: 10.1186/s12864-016-2712-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kim YK, Hwang MY, Kim YJ, Moon S, Han S, Kim BJ. Evaluation of pleiotropic effects among common genetic loci identified for cardio-metabolic traits in a Korean population. Cardiovasc Diabetol. 2016;15:20. doi: 10.1186/s12933-016-0337-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.MacKinnon D, Krull JL, Lockwood CM. Equivalence of the mediation, confounding and suppression effect. Prev Sci. 2000;1:173–181. doi: 10.1023/A:1026595011371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Solovieff N, Cotsapas C, Lee PH, Purcell SM, Smoller JW. Pleiotropy in complex traits: challenges and strategies. Nat Rev Genet. 2013;14:483–495. doi: 10.1038/nrg3461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ko YL, Hsu LA, Wu S, Teng MS, Chou HH. CRP and SAA1 haplotypes are associated with both C-reactive protein and serum amyloid A levels: role of suppression effects. Mediat Inflamm. 2016;2016:5830361. doi: 10.1155/2016/5830361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sivakumaran S, Agakov F, Theodoratou E, Prendergast JG, Zgaga L, Manolio T, et al. Abundant pleiotropy in human complex diseases and traits. Am J Hum Genet. 2011;89:607–618. doi: 10.1016/j.ajhg.2011.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Demirkan A, van Duijn CM, Ugocsai P, Isaacs A, Pramstaller PP, Liebisch G, et al. Genome-wide association study identifies novel loci associated with circulating phospho- and sphingolipid concentrations. PLoS Genet. 2012;8:e1002490. doi: 10.1371/journal.pgen.1002490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hall MA, Verma A, Brown-Gentry KD, Goodloe R, Boston J, Wilson S, et al. Detection of pleiotropy through a phenome-wide association study (PheWAS) of epidemiologic data as part of the environmental architecture for genes linked to environment (EAGLE) study. PLoS Genet. 2014;10:e1004678. doi: 10.1371/journal.pgen.1004678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Neale BM, Fagerness J, Reynolds R, Sobrin L, Parker M, Raychaudhuri S, et al. Genome-wide association study of advanced age-related macular degeneration identifies a role of the hepatic lipase gene (LIPC) Proc Natl Acad Sci USA. 2010;107:7395–7400. doi: 10.1073/pnas.0912019107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Seddon JM, Reynolds R, Rosner B. Associations of smoking, body mass index, dietary lutein, and the LIPC gene variant rs10468017 with advanced age-related macular degeneration. Mol Vis. 2010;16:2412–2424. [PMC free article] [PubMed] [Google Scholar]
- 55.Barbarash O, Gruzdeva O, Uchasova E, Dyleva Y, Belik E, Akbasheva O, et al. The role of adipose tissue and adipokines in the manifestation of type 2 diabetes in the long-term period following myocardial infarction. Diabetol Metab Syndr. 2016;8:24. doi: 10.1186/s13098-016-0136-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sánchez-Íñigo L, Navarro-González D, Fernández-Montero A, Pastrana-Delgado J, Martínez JA. The TyG index may predict the development of cardiovascular events. Eur J Clin Invest. 2016;46(2):189–197. doi: 10.1111/eci.12583. [DOI] [PubMed] [Google Scholar]
- 57.Wang Y, He S, He J, Wang S, Liu K, Chen X. Predictive value of visceral adiposity index for type 2 diabetes mellitus: a 15-year prospective cohort study. Herz. 2015;40(Suppl 3):277–281. doi: 10.1007/s00059-014-4175-1. [DOI] [PubMed] [Google Scholar]
- 58.Chen HY, Chiu YL, Chuang YF, Hsu SP, Pai MF, Yang JY, Peng YS. Visceral adiposity index and risks of cardiovascular events and mortality in prevalent hemodialysis patients. Cardiovasc Diabetol. 2014;4(13):136. doi: 10.1186/s12933-014-0136-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lee SH, Kwon HS, Park YM, Ha HS, Jeong SH, Yang HK, Lee JH, Yim HW, Kang MI, Lee WC, Son HY, Yoon KH. Predicting the development of diabetes using the product of triglycerides and glucose: the Chungju metabolic disease cohort (CMC) study. PLoS ONE. 2014;9(2):e90430. doi: 10.1371/journal.pone.0090430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wehr E, Pilz S, Boehm BO, März W, Obermayer-Pietsch B. The lipid accumulation product is associated with increased mortality in normal weight postmenopausal women. Obesity (Silver Spring) 2011;19(9):1873–1880. doi: 10.1038/oby.2011.42. [DOI] [PubMed] [Google Scholar]
- 61.Ioachimescu AG, Brennan DM, Hoar BM, Hoogwerf BJ. The lipid accumulation product and all-cause mortality in patients at high cardiovascular risk: a PreCIS database study. Obesity (Silver Spring) 2010;18(9):1836–1844. doi: 10.1038/oby.2009.453. [DOI] [PubMed] [Google Scholar]
- 62.Bozorgmanesh M, Hadaegh F, Azizi F. Predictive performances of lipid accumulation product vs. adiposity measures for cardiovascular diseases and all-cause mortality, 8.6-year follow-up: Tehran lipid and glucose study. Lipids Health Dis. 2010;9:100. doi: 10.1186/1476-511X-9-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nikpay M, Goel A, Won HH, Hall LM, Willenborg C, Kanoni S, et al. A comprehensive 1,000 Genomes-based genome-wide association meta-analysis of coronary artery disease. Nat Genet. 2015;47:1121–1130. doi: 10.1038/ng.3396. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Inter- and intra-assay variability measures of the biochemistry. Table S2. Associations of the LIPC SNPs with each quartile of visceral adiposity indicators and TyG index related parameters.
Data Availability Statement
The data are within the manuscript.