Abstract
Introduction
Acne is a chronic disorder of the pilosebaceous unit affecting all ethnic groups. It remains in the top 5 skin conditions seen worldwide. The paucity of data characterizing acne in South African Blacks led us to the documentation of types and sequelae of acne.
Methods
This is a cross- sectional study describing the spectrum and variants of acne in 5 tertiary hospitals in the second most populous province in South Africa over 3 months (January 1 – March 31, 2015).
Results
Out of 3,814 patients seen in tertiary dermatology clinics, 382 (10%) had a primary diagnosis of acne or rosacea, forming the fourth most common condition seen. Acne accounted for 361 (94.5%); acne vulgaris was the commonest subtype at 273 (75.6%), followed by steroid-induced acne 46 (12.7%), middle-age acne 6 (1.7%), acne excoriée 2 (0.6%), and “undefined” 34 (9.4%).
Conclusion
The observation of steroid-induced acne as the second most common variant in Black patients underlines the need to enquire about steroid use and education about the complications of using steroid-containing skin-lightening creams. Treatment of postinflammatory hyperpigmentation should be part of the armamentarium for holistic acne treatment in Blacks, as it remains a major concern even after active acne has resolved.
Keywords: Acne vulgaris, Steroid-induced acne, Blacks, African, South Africa, Spectrum, Epidemiology, Sequelae
Introduction
Acne is a chronic disorder of the pilosebaceous unit affecting all ethnicities [1, 2]. As people with skin of color make up a growing segment of the global population, with acne as one of the commonest skin conditions, dermatology care should evolve to address the distinct concerns and unique presentations of this population [1]. The paucity and the need for African data on acne, one of the most common skin conditions seen locally and globally, led us to conduct the current study, the aim of which was to describe the different types and unique complications of acne in Black skin. To our knowledge, there is no study describing the subtypes of acne in Black patients in South Africa (S.A.), a country of 50.6 million, of whom 80% are Black and 85% of the population are dependent on the public health sector. For the purpose of the study, “Black” refers to all patients of African ancestry.
Methods
We have conducted a cross-sectional study describing the spectrum and variants of acne in 5 tertiary hospitals in the second most populous province in S.A. over 3 months (January 1 – March 31, 2015). Ethical approval for this study was obtained by the Biomedical Research Ethics committee (BREC) of the University of KwaZulu-Natal. Written informed consent was obtained following which data related to age, ethnic group (based on patient's self-identification), gender, family history, history of topical or systemic corticosteroid use, and skin diagnosis were collected and analyzed. Acneiform disorders were categorized into acne vulgaris, steroid-induced acne, middle-age acne, acne excoriée, and rosacea and were captured using a Microsoft Excel spreadsheet. The data were subsequently analyzed using SAS (v 9.1.3; SAS institute Inc, Cary, NC, USA).
Results
Of 3,814 patients seen in tertiary dermatology clinics during the study period, 382 (10%) had a primary diagnosis of acne or rosacea, which formed the fourth most common category. Acne and rosacea accounted for 361 (94.5%) and 21 (5.5%), respectively. Acne vulgaris was the commonest subtype at 273 (75.6%), followed by steroid-induced acne 46 (12.7%), middle-age acne 6 (1.7%), acne excoriée 2 (0.6%), and the rest were “undefined” 34 (9.4%) (Table 1).
Table 1.
Demographics and acne variants of the studied patients
| Variable | Number | Percentage |
|---|---|---|
| Subtype (n = 361) | ||
| Acne vulgaris | 273 | 75.6 |
| Steroid-induced acne | 46 | 12.7 |
| Middle-age acne | 6 | 1.7 |
| Acne excoriée | 2 | 0.6 |
| Other | 34 | 9.4 |
| Population (n = 355) | ||
| Adult (≥18 years) | 317 | 89.3 |
| Pediatric (<18 years) | 38 | 10.7 |
| Gender (n = 367) | ||
| Females | 269 | 73.5 |
| Males | 97 | 26.5 |
| Ethnicity (n = 367; includes rosacea data) | ||
| African | 284 | 77.4 |
| Indian | 71 | 19.3 |
| White | 4 | 1.1 |
| Mixed | 8 | 2.2 |
Discussion
Acne is consistently reported to be the one of the top 5 most prevalent skin conditions in the general population, as found in large studies in the USA, UK, and France [3], and is therefore one of the most commonly diagnosed skin diseases, particularly in adolescence, with an overall prevalence of about 9.5% worldwide [4]. The prevalence of acne in a recent cross-sectional study of 1,617 patients in the UK in 2016 was 3.8% (42), 7.6% (16), and 9.7% (44) in Whites, Africans, and Asians, respectively [5].
As we have previously reported, it is the most common skin condition seen in Black patients seeking skin care, both in the private and public health sector, in S.A. [6]. Postinflammatory hyperpigmentation (Fig. 1) and keloidal scarring (Fig. 2) remain a major challenge, resulting in an impaired quality of life. In a South African private sector study in 2014, out of 6,664 patients, 44.3% had acne followed by eczema (15.9%) and dyschromia (11.6%). A higher prevalence of dyspigmentation (65%) and scarring was found in an American study of 2,895 patients, as these are distinguishing characteristics in black patients [7]. Similar to other studies, our data documents acne vulgaris as the commonest type of acne followed by corticosteroid-induced acne (Fig. 3). The widespread use of corticosteroids as skin-lightening agents for treating acne-related pigmentation or disorders of pigmentation explains the high prevalence of drug-induced acne, also observed by others [3]. The observation of steroid-induced acne as the second most common variant in Black patients underlines the need to enquire about steroid use as well as education about the complications of using steroid-containing skin-lightening creams. Having said that, treatment of postinflammatory hyperpigmentation and scarring should be part of the armamentarium for holistic acne treatment in Black patients, as it remains a major concern even after active acne has resolved.
Fig. 1.

Skin-colored papules on the cheeks with postinflammatory hyperpigmentation as a complication of acne in Black patients.
Fig. 2.
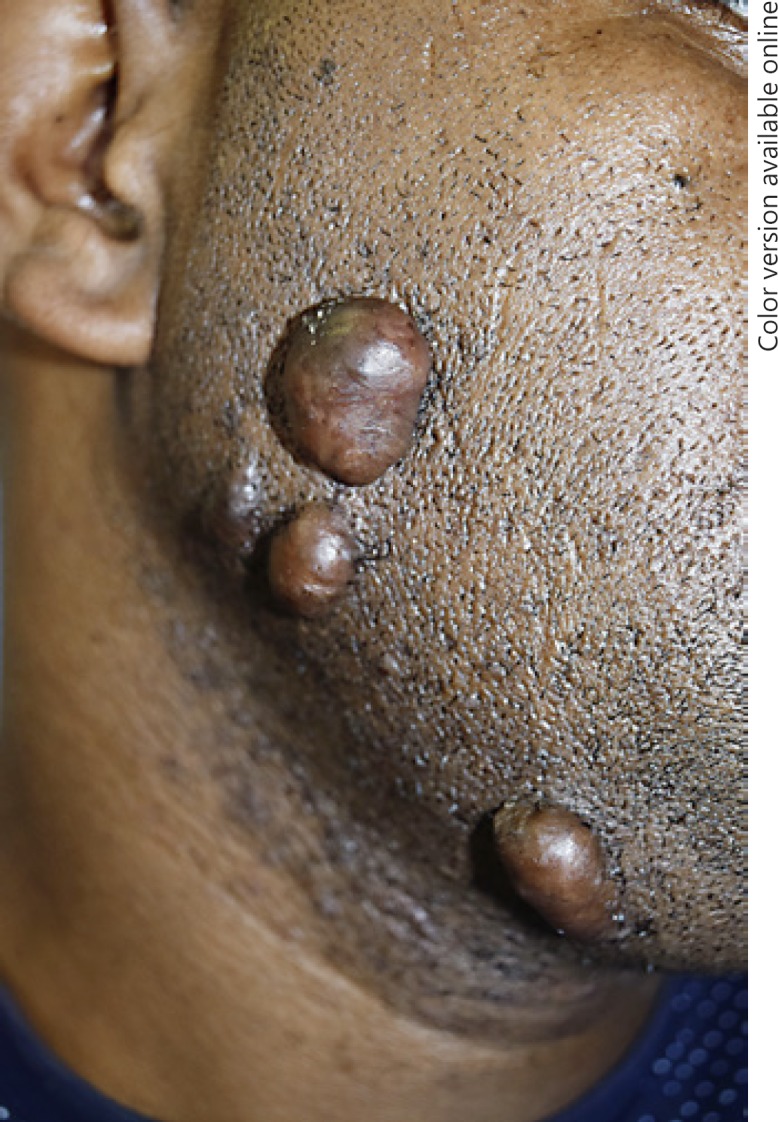
Acne healing with keloidal scarring on the cheeks of a Black male.
Fig. 3.

Typical monomorphic and closed comedones in a Black male patient with steroid-induced acne due to clobetasol diproprionate, a not so uncommon presentation.
Recognition of the various acne phenotypes, causes, and sequalae will assist in better patient care and potentially reduce the need to treat postinflammatory hyperpigmentation, which is a common occurrence and of great concern in Black patients.
Statement of Ethics
Ethical approval for this study was obtained by the Biomedical Research Ethics Committee (BREC) of the University of KwaZulu-Natal. Written informed consent was obtained.
Disclosure Statement
There are no conflicts of interest to disclose.
Acknowledgements
We would like to thank Prof. Robin Graham Brown for his invaluable input to the paper.
References
- 1.Yin NC, McMichael AJ. Acne in patients with skin of color: practical management. Am J Clin Dermatol. 2014;15:7–16. doi: 10.1007/s40257-013-0049-1. [DOI] [PubMed] [Google Scholar]
- 2.Fabbrocini G, Annunziata M, D'arco V, De Vita V, Lodi G, Mauriello M, Pastore F, Monfrecola G. Acne scars: pathogenesis, classification and treatment. Dermatol Res Pract. 2010;2010:893080. doi: 10.1155/2010/893080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhate K, Williams H. Epidemiology of acne vulgaris. Br J Dermatol. 2013;168:474–485. doi: 10.1111/bjd.12149. [DOI] [PubMed] [Google Scholar]
- 4.Dréno B. Recent data on epidemiology of acne (in French) Ann Dermatol Venereol. 2010;137((suppl 2)):S49–S51. doi: 10.1016/S0151-9638(10)70024-7. [DOI] [PubMed] [Google Scholar]
- 5.Banner A, Dinsey M, Ezzedine K, Dadzie O. The spectrum of skin diseases occurring in a multi-ethnic population in Northwest London, UK; findings of a cross-sectional descriptive study. Br J Dermatol. 2016;175:9–10. doi: 10.1111/bjd.14824. [DOI] [PubMed] [Google Scholar]
- 6.Dlova NC, Chateau A, Khoza N, Skenjane A, Mkhize M, Katibi OS, Grobler A, Gweweni JT, Mosam A. Prevalence of skin diseases treated at public referral hospitals in KwaZulu-Natal, South Africa. Br J Dermatol. 2018;178:e1–e2. doi: 10.1111/bjd.15534. [DOI] [PubMed] [Google Scholar]
- 7.Perkins AC, Cheng CE, Hillebrand GG, Miyamoto K, Kimball AB. Comparison of the epidemiology of acne vulgaris among Caucasian, Asian, Continental Indian and African American women. J Eur Acad Dermatol Venereol. 2011;25:1054–1060. doi: 10.1111/j.1468-3083.2010.03919.x. [DOI] [PubMed] [Google Scholar]


