Abstract
Background:
Validation studies in digital pathology addressed so far diverse aspects of the routine work. We aimed to establish a complete remote digital pathology service.
Methods:
Altogether 2295 routine cases (8640 slides) were reported in our studies on digital versus microscopic diagnostics, remote reporting, diagnostic time, fine-needle aspiration cytology (FNAC) clinics, frozen sections, and diagnostic sessions with residents. The same senior pathologist was involved in all studies. Slides were scanned by ScanScope AT Turbo (Aperio). Digital images were accessed through the laboratory system (LS) on either 14” laptops or desktop computers with double 23” displays for the remote and on-site digital reporting. Larger displays were used when available for remote reporting. First diagnosis was either microscopic, digital, or remote digital only (6 months washout period). Both diagnoses were recorded separately and compared. Turnaround was measured from the registration to sign off or scanning to diagnosis. A diagnostic time was measured from the point slides were made available to the point of diagnosis or additional investigations were necessary, recorded independently in minutes/session, and compared. Jabber Video (Cisco) and Lync (Microsoft) were interchangeably used for the secure, video supervision of activities. Mobile phone, broadband, broadband over Wi-Fi, and mobile broadband were tested for internet connections. Nine autopsies were performed remotely involving three staff pathologists, one autopsy technician, and one resident over the secure video link. Remote and on-site pathologists independently interpreted and compared gross findings. Diverse benefits and technical aspects were studied using logs or information recorded in LS. Satisfaction surveys on diverse technical and professional aspects of the studies were conducted.
Results:
The full concordance between digital and light microscopic diagnosis was 99% (594/600 cases). A minor discordance, without clinical implications, was 1% (6/600 cases). The instant upload of digital images was achieved at 20 Mbps. Deference to microscopic slides and rescanning were under 1%. Average turnaround was shorter and percentage of cases reported up to 3 days higher for remote digital reporting. Larger displays improved the most user experience at magnifications over ×20. A digital diagnostic time was shorter than microscopic in 13 sessions. Four sessions with shorter microscopic diagnostic time included more cases requiring extensive use of magnifications over ×20. Independent interpretations of gross findings between remote and on-site pathologists yielded full agreement in the remote autopsies. Delays in reporting of frozen sections and FNAC due to scanning were clinically insignificant. Satisfaction levels with diverse technical and/or professional aspects of all studies were high.
Conclusions:
Complete routine remote digital pathology services are found feasible in hands of experienced staff. The introduction of digital pathology has improved provisions and organizations of our pathology services in histology, cytology, and autopsy including teaching and interdepartmental collaboration.
Keywords: Autopsy, conference, digital pathology, fine-needle aspiration cytology, frozen sections
INTRODUCTION
Digital pathology has been increasingly seen as a powerful tool for further development of pathology.[1,2,3] Numerous validation studies in digital pathology so far addressed diverse aspects of the routine workload. Evans et al. evaluated frozen section services using a robotic microscopy system, followed by evaluation of digital pathology in routine reporting. The result of this study showed advantages of digital microscopy against robotic microscopy, especially in turnaround.[4,5] In studies from Sweden, the goal was to reduce the time spent on microscopes and improve ergonomics at pathology departments. Increasing number of aging pathologists, complexity of workload, and financial constraints were discussed as main driving factors in search for more efficient organization of pathology services.[6] Pathology departments around the world are therefore implementing digital pathology in routine diagnostics, second opinion, research, and education.[2,5,7,8,9] Apart from better ergonomics, instant access to slides, and remote reporting, the advantages of digital pathology include improved diagnostic quality assurance, shorter turnaround on complex and difficult cases through external consultation services, faster image analysis, streamlining of teaching, and improving working flexibility of pathologists.[6,10,11,12,13,14,15] Smaller pathology departments like ours are especially vulnerable in terms of slower recruitment of pathologists. Our business plan of digitalization has focused on more efficient pathology services with existing resources in securing their continuity. We have expected ergonomics and remote reporting to benefit productivity and execution of overtime, addressing our acute needs. This could be achieved by studying all aspects of the routine workload and activities in our digital pathology project. Our aim was therefore to establish a complete remote routine digital pathology service. Technical issues were seen as main obstacles and improved turnaround and continuity of services as desired benefits.
METHODS
All aspects of our workload at the Department of Pathology, Førde Central Hospital, were studied in our digital pathology project. Altogether 2295 cases (8640 slides) were reported by the same senior pathologist. All slides were prepared by standard techniques and scanned by ScanScope AT Turbo (Aperio) at ×20 in the main laboratory. Digital images were accessed through SymPathy (Tieto), our fully integrated laboratory system (LS), and viewed in ImageScope (Aperio) image viewer in all studies. Study-specific methods are discussed below.
Digital versus microscopic diagnosis
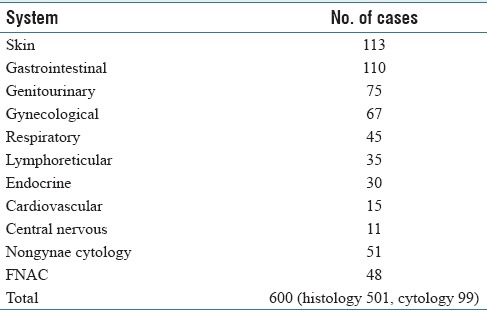
Six hundred consecutive cases (2587 slides) in histology and cytology (nongynae and fine-needle aspiration cytology [FNAC]), previously signed off on the microscope, were scanned and reported digitally on-site by the same senior staff pathologist over the period of 2 months [Table 1]. The pathologist used an OptiPlex desktop computer with double 23” displays (1920 × 1200, Dell). Only request forms were made available for both digital and microscopic reporting. Digital diagnosis was compared with microscopic one as full concordance, minor discordance (without clinical implications), and major discordance (with clinical implications). A washout period between microscopic and digital diagnosis was 6 months. This study was fully compliant to the College of American Pathologists recommendation.[3]
Table 1.
Case workload in study on digital vs. microscopic diagnosis
Remote reporting in digital pathology
This study has been previously published.[12] The same senior staff pathologist reported 950 routine cases (3650 slides) in histology and cytology (nongynae and FNAC), remotely from home, over the period of 19 weeks. The pathologist used an E6340, 14” laptop (1600 × 900 display, Dell) for reporting. An Ultra HD 4K LED TV was used (3840 × 2160, LG) when available. Digital slides were accessed through the same LS. Mobile phone, mobile broadband, broadband over Wi-Fi, and broadband were used for internet connections along with a virtual private network (VPN) technology. Effects of ergonomics and working flexibility on the user experience were observed and recorded as a structured weekly log. Details on network speed, frequency of technical issues, data usage, scanning, and turnaround were collected and evaluated. Turnaround was compared to that of on-site, microscopic reporting, measured from the registration to sign-off.
Diagnostic time in digital pathology
This study has been previously published.[14] The same senior staff pathologist reported 400 consecutive, routine cases (1396 slides) in histology and cytology (nongynae and FNAC) as 20 sessions, 20 cases/session, over 4 weeks. Complex, difficult, and rare cases were excluded from the study to reduce the bias. Digital diagnosis was first, followed by microscopy 6 months later, with only request forms available for both. Digital images were accessed through the same LS. The pathologist used an OptiPlex 7010 desktop computer with double 23” displays (1920 × 1200, Dell) for digital reporting. A microscopic diagnosis was made on an Eclipse 80i light microscope (Nikon). Turnaround referred to diagnostic (slide evaluation) and nondiagnostic time (dictation or typing in reports, disease coding, accessing clinical information, previous history, etc.). An unstructured sessional log was recorded to identify factors contributing to improved diagnostic time. A diagnostic time was measured from the point slides were made available to the point diagnosis was made or additional investigations were deemed necessary, recorded independently in minutes/session, and compared. Broadband speeds were automatically recorded every 30 min into digital reporting sessions and analyzed.
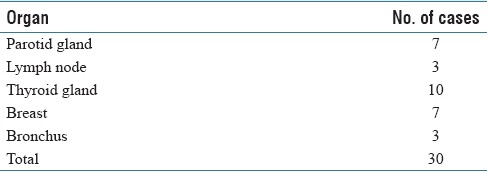
One-stop fine-needle aspiration cytology clinics
We provide rapid on-site consultations for radiologists, surgeons, and physicians on the quality of diagnostic material and where applicable, final diagnosis. During the course of our digital pathology project, the same senior staff pathologist reported remotely 30 cases (57 slides) for one-stop Breast, Head and Neck, Lung, and Ultrasound clinics [Table 2a]. Slides were prepared by standard techniques, stained by rapid Romanowsky in the FNAC clinics, by our laboratory staff or residents, and scanned. Digital images were accessed through the same LS. Turnaround time was recorded for all cases and compared with that of historic, similar cases from our LS, reported microscopically on-site by the same pathologist. It was measured from the point slides were made available for scanning to the point quality of material was confirmed and/or preliminary diagnosis made. The results were phoned to clinicians. Clinicians and patients participated in a brief verbal survey following the each FNAC session (satisfied with remote digital FNAC service – yes/no). Answers were recorded and evaluated.
Table 2a.
Case workload in study on remote digital diagnostics from one-stop FNAC clinics
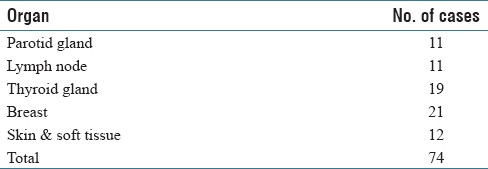
In the previous studies, the same senior staff pathologist already reported additional 74 (197 slides) cases from our regular FNAC clinics [Table 2b]. Digital diagnosis was first in 17 cases (study on diagnostic time in digital pathology) and microscopic first in 48 cases (study on digital vs. microscopic diagnosis). A washout period between diagnoses was 6 months. Nine cases were reported by means of digital pathology only (study on remote reporting in digital pathology). Altogether, 104 cases were reported in all of our FNAC studies.
Table 2b.
Case workload in validation study on remote and on-site digital diagnostics from regular FNAC clinics
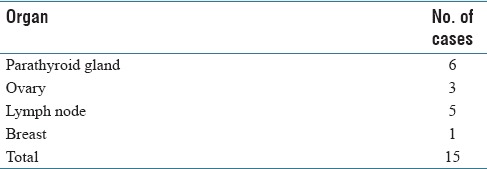
Frozen sections
During the course of our digital pathology project, the same senior staff pathologist reported 15 frozen section cases (57 slides), as shown in Table 3. Frozen sections were prepared by standard techniques, involving laboratory staff or residents, scanned, and reported remotely by means of digital pathology only. The pathologist used an EliteBook, 14” laptop (1920 × 1200, Hewlett-Packard). Digital slides were accessed through the same LS. Turnaround time was recorded for all cases and compared with that of historic, similar cases from our LS, reported microscopically on-site by the same pathologist. It was measured from the point slides were made available for scanning to the point the diagnosis was made. The results were phoned to clinicians. Clinicians participated in a brief verbal survey following the each case (satisfied with remote digital frozen section service – yes/no). Answers were recorded and evaluated.
Table 3.
Case workload in study on digital diagnostics of frozen sections
Internal teaching
We practice regular internal teaching sessions, on average 2 h per week. During the course of our digital pathology project, the same senior staff pathologist provided 15 hourly remote internal teaching sessions to pathologists and residents, over Lync (Microsoft). These included article reviews, case discussions, and presentations from attended conferences. The remote pathologist used an EliteBook 14” laptop (1920 × 1080, Hewlett-Packard). The participants on-site used an OptiPlex 7010 desktop computer connected to the external high-definition 55” display (Samsung). Departmental colleagues participated in a brief verbal survey following the each session (satisfied with remote internal teaching – yes/no). Answers were recorded and evaluated.
Multidisciplinary team meetings and clinical pathological conferences
During the course of our digital pathology project, five multidisciplinary team meetings and clinical pathological conferences (MDT/CPC) were conducted in oncology, urology, and dermatology, over Jabber Video (Cisco), by the same senior staff pathologist working remotely. The pathologist used an EliteBook 14” laptop (1920 × 1080, Hewlett-Packard). The participants on-site used an OptiPlex 7010 desktop computer connected to the external 55” display (Samsung). Clinicians participated in a brief verbal survey following the each meeting (satisfied with remote MDT/CPC service – yes/no). Answers were recorded and evaluated.
Grossing supervision of residents
During the course of our digital pathology project (separately from other studies), the same senior staff pathologist supervised ten remote grossing sessions with residents over Lync (Microsoft). The pathologist was made available for ad hoc consultations when in need by residents. Altogether 97 gross specimens were consulted, including skin, gastrointestinal, gynecological, urological, breast, lymphoid, and thyroid. The pathologist used an EliteBook 14” laptop (1920 × 1080, Hewlett-Packard). The residents on-site used an OptiPlex 7010 desktop computer with a 23” display (1920 × 1200, Dell) and portable high-definition web camera (Cisco). Following the each session, residents participated in a brief verbal survey on satisfaction levels with technical aspects (sound, video; minimal score 1, maximal score 5). Answers were recorded and evaluated.
Diagnostic supervision of residents
During the course of our digital pathology project, 30 remote digital consultations (sign-off sessions), involving 300 cases (950 slides), in routine histology, cytology (FNAC), and autopsy were performed between the same senior staff pathologist and residents over Jabber Video (Cisco). The pathologist used an EliteBook 14” laptop (1920 × 1080 display, Hewlett-Packard). The residents used a desktop computer with double 23” displays (1920 × 1200, Dell). Following the each diagnostic session, residents participated in a brief verbal survey on satisfaction levels with technical aspects (sound, images, LS; minimal score 1, maximal score 5) and personal preferences (digital vs. microscopic sign-off). Answers were recorded and evaluated.
Remote autopsy services
This study has been previously published.[15] To complete our routine, remote digital pathology services, and increase flexibility of the autopsy services, nine autopsies were performed remotely involving three senior staff pathologists, one senior autopsy technician, and one junior resident. The autopsies were performed on site by the autopsy technician or resident, supervised by the same, remote pathologist, over Jabber Video (Cisco) on a high-speed broadband connection. The remote pathologist and autopsy room each connected to the secure virtual meeting room using EliteBook 840, 14” laptops with inbuilt cameras (1920 × 1080, Hewlett-Packard). A portable high-definition web camera (Cisco) was used in the autopsy room. Primary (remote) and secondary (on-site) pathologists independently interpreted and later compared gross findings for the purpose of quality assurance. The video was streamed live only during consultations and interpretation. A satisfaction survey on technical (sound, video, broadband) and professional (external examination, evisceration, dissection, interpretation, consultation, discussion) aspects of the study was conducted (minimum score 1, maximum score 5 per activity).
RESULTS
Digital versus microscopic diagnosis
The full concordance between primary and secondary diagnoses was 99% (594/600 cases). A minor discordance was noted in the remaining cases [Table 4]. There was no major discordance between the diagnoses. Deference to microscopic slides (insufficient material on slide) and rescanning (focusing errors) was 0.2% and 0.5%, respectively. Digital and microscopic workflows were compared in Figure 1. The digital diagnostics was regarded as reliable and introduced into routine practice.
Table 4.
Cases with minor discordance in study on digital vs. microscopic diagnosis
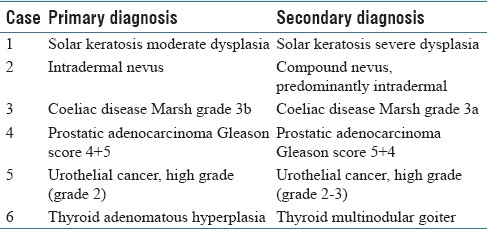
Figure 1.
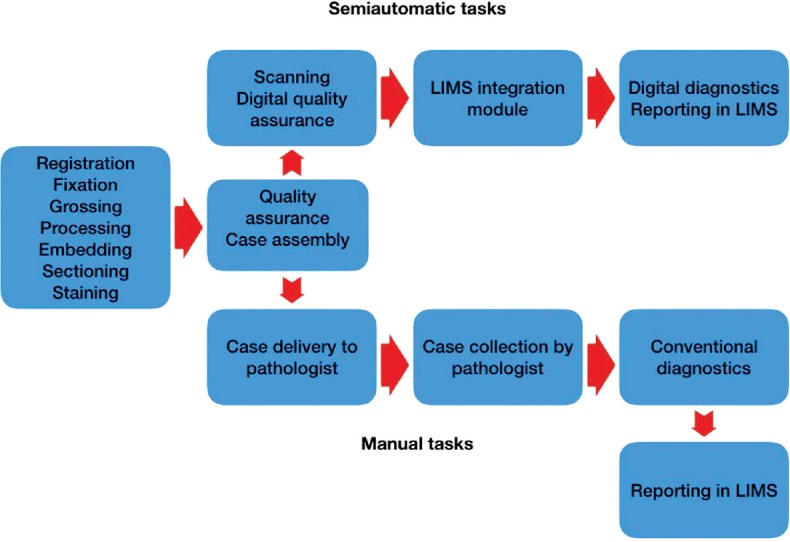
Comparison of workflows in digital and microscopic diagnostics
Remote reporting in digital pathology
Network speeds varied 1–80 Mbps (median download speed 8–65 Mbps). Twenty Mbps were satisfactory for the instant upload of digital images. VPN, image viewer, and laptop failed on two occasions each. An estimated data usage per digital image was 10 MB (1–50 MB). Two cases were deferred to microscopic slides (0.21%) due to scanty material and suboptimal slide quality. Additional nine cases needed to be rescanned for various reasons (0.95%). Average turnaround was shorter, and the percentage of cases reported up to 3 days higher (72.25%) comparing with on-site microscopic reporting (40.56%). Contributing factors to improved turnaround in remote digital reporting were better ergonomics, more working flexibility with a time shift, less disruption, typing in, and canned reports. Larger displays improved the most user experience at magnifications over ×20.
Diagnostic time in digital pathology
A total digital diagnostic time was 1841 and microscopic 1956 min; digital being shorter than microscopic in 13 out of 20 sessions. Four sessions with shorter microscopic diagnostic time included more cases requiring extensive use of magnifications over ×20 (low bacterial and tumor load, nuclear features). Diagnostic time was similar in three sessions. A median broadband speed was 299 Mbps. A diagnostic time in digital pathology can be shorter than microscopy in the routine diagnostic setting, with adequate and stable network speeds, fully integrated LS, and double displays as default parameters. This also related to better ergonomics, larger viewing field, and absence of physical slide handling, with effects on both diagnostic and nondiagnostic time. Differences with previous studies included a design, image size, number of cases, specimen type, network speed, and participant's level of confidence and experience in digital reporting.
One-stop fine-needle aspiration cytology clinics
Due to scanning, the turnaround time was longer by 5 min on average (varying from 1 to 7). Our clinicians and patients reported a full satisfaction with the service.
Frozen sections
Due to scanning, the turnaround time was longer by 3 min on average (varying from 1 to 5). Our clinicians reported a full satisfaction with the service.
Internal teaching
Participants reported a full satisfaction with the service. The departmental agreement was to introduce routine remote internal teaching sessions. Altogether 30 hourly sessions were provided by the same remote staff pathologist since.
Multidisciplinary team meetings and clinical pathological conferences
Clinicians reported a full satisfaction with the service. They also appreciated its potential to secure the continuity in cases of on-site absences on both sides.
Grossing supervision of residents
Occasional minor issues with a sound quality were observed, relating to transient network instabilities. Satisfaction levels with technical aspects of the study were 95%.
Diagnostic supervision of residents
Occasional minor issues with a sound quality were observed, relating to transient network instabilities. Satisfaction levels with technical aspects of the study were 95%. Residents preferred digital diagnostic supervision (90%) over microscopic. Residents also confirmed improved turnaround and administrative time, which mirrored that already reported in the study on remote reporting in digital pathology, for the same senior staff pathologist (better ergonomics, larger viewing field, absence of physical slide handling, and fully integrated LS). Residents’ occasional preference for microscopic sign-off sessions instead of digital ones related to their seniority and case complexity. Our residents are now routinely offered both digital and microscopic sign-off sessions.
Remote autopsy services
Independent interpretations of gross findings between primary and secondary pathologists yielded full agreement. A definite cause of death in one complex autopsy was determined following discussions between pathologists and reviews of the clinical notes. Our satisfaction level with the technical and professional aspects of the study was 87% and 97%, respectively.
Remote autopsy services were found to be feasible in the hands of experienced staff, with increased flexibility and interest of autopsy technicians in the service as a result.
DISCUSSION
Pathology departments worldwide are looking into implementation of digital pathology and building up digital pathology networks due to an increasing and more complex workload, aging pathologists, and health funding growing at a significantly lesser pace, aiming to the better organization and more effective execution of pathology services.[4,6,11]
We have focused on productivity, execution of overtime, and distribution of departmental activities as main targets for digitalization with a complete, remote routine digital pathology services as our goal. Local IT solutions allowed effective and reliable remote digital reporting of histology, cytology, and autopsy. Stable network speeds, fully integrated LS, technical reliability, working flexibility, larger displays, increased productivity, and shorter turnaround time contributed to overall satisfaction with remote digital reporting. A diagnostic time in digital pathology was found to be shorter than traditional microscopy in our routine diagnostic setting. This was also related to the better ergonomics, larger viewing field, and absence of physical slide handling. We have also shown that remote autopsy services are feasible in the hands of experienced staff, with increased flexibility and interest in autopsy technicians in the service as a result.[12,14,15]
Validation studies so far addressed diverse aspects of digital pathology separately, largely within an on-site reporting setup.[1,4,6,7,11] As our focus was on the remote routine digital pathology services, we designed our studies accordingly. A sample size in our studies varied but was deemed satisfactory. The study on digital diagnostics of frozen sections was affected by the sharp fall in frozen section requests, largely due to switch to formalin-fixed examination of sentinel node biopsies, coinciding with our digital pathology project. However, our primary concerns in that study were technical aspects and feasibility of remote frozen section services in the local setup, rather than professional aspects as diagnostic comparison with microscopy. The pathologist involved in this evaluation has also had extended experience in digital reporting of frozen sections from the previous professional appointments. Although limited, provisions of frozen section services are still important to our clinicians, and remote routine digital pathology services secure their continuity.
All aspects of our routine workload were deemed feasible from the remote office but active grossing and FNAC services. However, residents in many departments stand for the grossing service, under supervision by pathologists. A remote pathologist, responsible for the weekly grossing, was made available on demand by residents performing specimen grossing on site, through secure video links. Resident's satisfaction with existing technical solutions was excellent. We have actively supported our clinicians for years to organise and run FNAC services including one-stop Breast, Head and Neck, Lung, and Ultrasound clinics. During that time, we have actively involved both our residents and laboratory personnel in the service, providing an additional practical and theoretical training. Through these activities, their skills in providing high-quality smears and proper, consistent handling of diverse types of specimens provided by clinicians were greatly improved. Residents and laboratory technicians are now regularly involved in FNAC services, even when on-site pathologist is available. On request, a remote pathologist provides video consultations to clinicians responsible for one-stop FNAC clinics. Benefits of the same day provisions on the quality of material and/or diagnosis overweighed recorded, clinically deemed insignificant, delays in reporting. This surrogate solution for grossing and FNAC services in the remote setup has worked as good as the on-site one, in our validation studies and beyond. The additional advantage was our ability to provide continuous service in cases of ad hoc absences of on-site pathologists.
We currently provide complete routine remote digital pathology services in histology, cytology, and autopsy. This has led to increased productivity and improved turnaround for remote pathologists. Our department is becoming more resilient to unforeseen staffing shortages with savings in lodging and transportation of pathologists on temporary contracts (on average 30%). In addition, potential backlogs in the departmental histology workload are now easily accessible to the departmental pathologists for voluntary additional digital diagnostic sessions from home, providing savings in overtime versus temporary staffing. Digital pathology has been fully implemented into our MDT/CPC and partially to our consultation services. Pathologists are now able to, for example, mark and comment on cases for the meetings at the time of reporting. Improved preparations and executions of these service, for both remote and on-site pathologists, have been observed as a result. Dedicated time for supporting staff (secretaries and laboratory staff) has been cut down with savings in time and transportation of slides sent out for consultation. Our residents have also appreciated improved turnaround time, ergonomics, and administrative time using digital diagnostic supervision, similar to findings from our study on remote reporting in digital pathology. Both digital and microscopic sign-off sessions are now routinely offered to and interchangeably used by our residents. Our current resident prefers digital sign-off. Remote internal teaching sessions have become our routine practice. Professional, financial, and health benefits of our digitalization process, discussed in this article, are summarized in Figure 2.
Figure 2.
Contributing factors to professional, financial, and health benefits of digitalization in pathology from our experience
Milestones in our digital pathology project are shown in Tables 5a and 5b. The project was financed from the regional IT budget at $295,000. The costs included one scanner with desktop computer, three 14” laptops, five 23” HD displays, seven optical 2D bar code reader, IT services, and LIMS integration module. The latter two items amounted to 50% of the total. We received support of both laboratory staff, departmental and hospital management. The project group was led by a senior staff pathologist ( first author of this article) with a senior staff pathologist/head of department, senior biomedical scientist, senior engineer, and senior IT consultant as members. The steering group was led by a senior staff pathologist/head of department, head of IT department, hospital medical director, and hospital director of development. All studies were conducted by the same, senior staff pathologist.
Table 5a.
Milestones in our digital pathology project
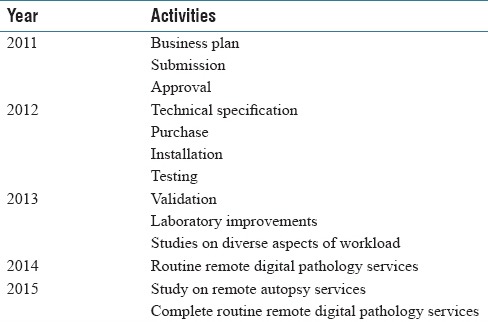
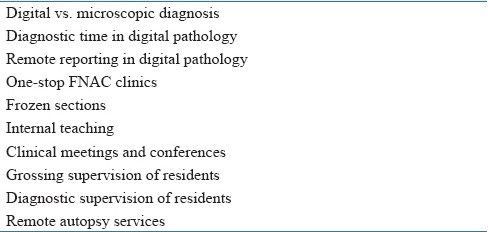
Table 5b.
Studies conducted in our digital pathology project, covering all aspects of workload
Following the conclusion of our digital pathology project, altogether 14,387 cases (47,572 slides) were reported remotely as a routine workload over the period of 4 years (histology, cytology, and autopsy), as shown in Tables 6 and 7. Benefits of digitalization with better use of available resources in mind have led to adjusted distribution of departmental workload and activities. One senior staff pathologist works remotely from home 90% of the time (10% on-site, in the hospital) mainly on histology, autopsy, and internal teaching. Two remaining senior staff pathologists use digital images exclusively for MDT/CPC, sharing mainly grossing, frozen sections, MDT/CPC, and cytology. Diagnostic supervision of residents and remaining departmental activities are being shared between staff pathologists, digital and microscopic. We appreciate that benefits of implemented digital pathology overweigh now our initial investment, excluding annual service costs.
Table 6.
Digital vs. microscopic reporting in histology after departmental digitalization
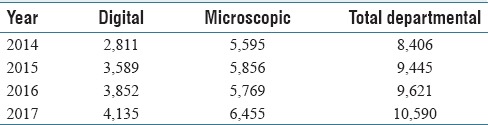
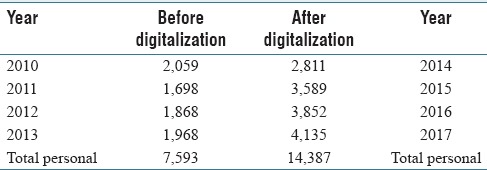
Table 7.
Workload in histology for remote digital pathologist before and after digitalization
Conclusion
A successful implementation of digital pathology relied on both our dedicated staff and continued, throughout support of our departmental and hospital management. This had also initiated closer collaboration and development of the regional digital pathology network, aiming to the establishment of the national one. Financing digital pathology projects through the regional IT budget may be a way to counteract financial constraints most hospitals face today.
The organization of pathology services may therefore benefit from adjustments following the implementation of digital pathology. In our opinion, the expected changes would include their consolidation to the fewer sites, centralization of grossing, rotational presence of pathologists at hospital sites and home offices, and streamlining of consultation services and teaching.
Broadening of applications and closer interdepartmental collaborations with building up digital pathology networks are expected to further advance its worldwide appeal and implementation.
Financial support and sponsorship
Health Authority West grant 795421 (some studies from our digital pathology project).
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We are grateful to our laboratory staff for their valuable contributions.
Footnotes
Available FREE in open access from: http://www.jpathinformatics.org/text.asp?2018/9/1/36/244435
REFERENCES
- 1.Romero Lauro G, Cable W, Lesniak A, Tseytlin E, McHugh J, Parwani A, et al. Digital pathology consultations-a new era in digital imaging, challenges and practical applications. J Digit Imaging. 2013;26:668–77. doi: 10.1007/s10278-013-9572-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Têtu B, Evans A. Canadian licensure for the use of digital pathology for routine diagnoses: One more step toward a new era of pathology practice without borders. Arch Pathol Lab Med. 2014;138:302–4. doi: 10.5858/arpa.2013-0289-ED. [DOI] [PubMed] [Google Scholar]
- 3.Pantanowitz L, Sinard JH, Henricks WH, Fatheree LA, Carter AB, Contis L, et al. Validating whole slide imaging for diagnostic purposes in pathology: Guideline from the College of American Pathologists Pathology and Laboratory Quality Center. Arch Pathol Lab Med. 2013;137:1710–22. doi: 10.5858/arpa.2013-0093-CP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Evans AJ, Chetty R, Clarke BA, Croul S, Ghazarian DM, Kiehl TR, et al. Primary frozen section diagnosis by robotic microscopy and virtual slide telepathology: The University Health Network Experience. Hum Pathol. 2009;40:1070–81. doi: 10.1016/j.humpath.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 5.Bellis M, Metias S, Naugler C, Pollett A, Jothy S, Yousef GM, et al. Digital pathology: Attitudes and practices in the Canadian pathology community. J Pathol Inform. 2013;4:3. doi: 10.4103/2153-3539.108540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thorstenson S, Molin J, Lundström C. Implementation of large-scale routine diagnostics using whole slide imaging in Sweden: Digital pathology experiences 2006-2013. J Pathol Inform. 2014;5:14. doi: 10.4103/2153-3539.129452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bauer TW, Slaw RJ. Validating whole-slide imaging for consultation diagnoses in surgical pathology. Arch Pathol Lab Med. 2014;138:1459–65. doi: 10.5858/arpa.2013-0541-OA. [DOI] [PubMed] [Google Scholar]
- 8.Ribback S, Flessa S, Gromoll-Bergmann K, Evert M, Dombrowski F. Virtual slide telepathology with scanner systems for intraoperative frozen-section consultation. Pathol Res Pract. 2014;210:377–82. doi: 10.1016/j.prp.2014.02.007. [DOI] [PubMed] [Google Scholar]
- 9.Horbinski C, Wiley CA. Comparison of telepathology systems in neuropathological intraoperative consultations. Neuropathology. 2009;29:655–63. doi: 10.1111/j.1440-1789.2009.01022.x. [DOI] [PubMed] [Google Scholar]
- 10.Bauer TW, Schoenfield L, Slaw RJ, Yerian L, Sun Z, Henricks WH, et al. Validation of whole slide imaging for primary diagnosis in surgical pathology. Arch Pathol Lab Med. 2013;137:518–24. doi: 10.5858/arpa.2011-0678-OA. [DOI] [PubMed] [Google Scholar]
- 11.Stathonikos N, Veta M, Huisman A, van Diest PJ. Going fully digital: Perspective of a dutch academic pathology lab. J Pathol Inform. 2013;4:15. doi: 10.4103/2153-3539.114206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vodovnik A. Distance reporting in digital pathology: A study on 950 cases. J Pathol Inform. 2015;6:18. doi: 10.4103/2153-3539.156168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Collins BT. Telepathology in cytopathology: Challenges and opportunities. Acta Cytol. 2013;57:221–32. doi: 10.1159/000350718. [DOI] [PubMed] [Google Scholar]
- 14.Vodovnik A. Diagnostic time in digital pathology: A comparative study on 400 cases. J Pathol Inform. 2016;7:4. doi: 10.4103/2153-3539.175377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vodovnik A, Aghdam MR, Espedal DG. Remote autopsy services: A feasibility study on nine cases. J Telemed Telecare. 2018;24:460–4. doi: 10.1177/1357633X17708947. [DOI] [PubMed] [Google Scholar]



