Abstract
Outbreaks of arbovirus infections vectored by invasive Aedes albopictus have already occurred and are predicted to become increasingly frequent in Southern Europe. We present a probabilistic model to assess risk of arbovirus outbreaks based on incident cases worldwide, on the probability of arrival of infected travelers, and on the abundance of the vector species. Our results show a significant risk of Chikungunya outbreak in Rome from mid June to October in simulations with high human biting rates (i.e. when ≥50% of the population is bitten every day). The outbreak risk is predicted to be highest for Chikungunya and null for Zika. Simulated increase of incident cases in selected endemic countries has no major impact on the outbreak risk. The model correctly estimated the number of imported cases and can be easily adapted to other urban areas where Ae. albopictus is the only potential vector present.
Introduction
Arboviruses (arthropod-borne viruses) are neglected human pathogens responsible of a large burden of morbidity especially in tropical and subtropical regions where mosquito species are abundant1. In the last years, arboviruses such Dengue (DENV), Chikungunya (CHIKV) and Zika (ZIKV) extended their geographical range allowing autochthonous transmission and causing major outbreaks at temperate latitudes in almost all continents2. In Europe, recent DENV outbreaks were recorded in France3,4 and Croatia5 while outbreaks of CHIKV were recorded in France6 and Italy7,8. Not surprisingly, all these events took place in Southern Europe (Euro-Mediterranean region), where a stable and extensive colonization by the Asian tiger mosquito Aedes albopictus creates permissive conditions for transmission. Aedes albopictus is less efficient in DENV and ZIKV transmission compared to Ae. aegypti9,10 while in many locations worldwide both Ae. aegypti and Ae. albopictus are generally highly susceptible to infection, dissemination and transmission of CHIKV11. Alarmingly, Ae. albopictus may reach high densities in urban areas of many Mediterranean countries12, reaching values up to 40 mosquito females per person13.
The establishment of a competent vector and suitable conditions for secondary transmission are both necessary to cause an outbreak in case of introduction of the virus from an external source. Hence, an increase of incident cases in tropical/subtropical areas coupled with increased traveller flow are critical factors in order to catalyze local outbreaks in Euro-Mediterranean cities. Unfortunately, the risk of outbreak cannot be easily predicted. In this context, mathematical and statistical models are powerful tools to elucidate the role played by each factor in determining the likelihood of local transmission14 and are often the only choice left to health authorities when facing the problem of calculating the outbreak risk.
Local-scale models are availble to assess the risk of outbreak probability for DENV, CHIKV and ZIKV in temperate regions following the importation of a single infectious case15,16. However, model predictions are based on data of Ae. albopictus abundance in Northern Italy without estimates of the probability of imported cases from abroad. On the other hand, the large-scale model developed by17 assesses the seasonal risks of the introduction and spread of ZIKV in Europe without vector abundance data.
Here we present a probabilistic model to assess the risk of CHIKV, DENV and ZIKV outbreaks in Rome based on actual data on the abundance of the vector species, Ae. albopictus, as well as on estimates of risk of virus introduction via the large flow of travelers through the international airport of Rome Fiumicino (FCO).
Materials and Methods
Model
Following the approach of Johansson and colleagues18–20, a probabilistic model was developed to compute the probability of observing an mosquito-borne arbovirus outbreak (P) in Rome generated by the importation of infected human cases. This probability is the result of two main processes, i.e. the arrivals of infected travelers to Rome and the autochthonous transmission of a specific arbovirus within the city. The explicit formula is the following:
| 1 |
The probability of outbreak in Rome (Eq. 1) could be interpreted as one minus the probability that no outbreak would take place. The latter is the product, for each country j, week i and type of traveler t (resident or visitor, see below for details), of the sum of probability of not arriving in Rome and the probability that one arrives without generating any autochthonous transmission , to the power of the number of infected host (see details in Technical Appendixes, section 1).
The model was run over an ensemble of 100,000 parameter sets, each one obtained by resampling their specific distribution (Table 1), in order to take into account the uncertainty. The results are reported as mean probability and credible interval per week. Additionally, we computed the year cumulative probability of outbreak, the expected cumulative number of incoming infected hosts in Rome and the frequency of infected host among travelers from different WHO regions.
Table 1.
Distributions and mathematical equations used to estimate parameters in the calculation of the basic reproductive number (R0) for DENV, CHIKV and ZIKV.
| Parameter | Description | Virus | Specification | Value | Reference |
|---|---|---|---|---|---|
| m | Mosquito mortality rate (1 /m = average mosquito life-span in days) | Dengue | Function | 2(0.031 + 95820e(T - 50.4)) | Manica et al. 2017 |
| Chikungunya | Function | 2(0.031 + 95820e(T - 50.4)) | Manica et al. 2017 | ||
| Zika | Function | 2(0.031 + 95820e(T - 50.4)) | Manica et al. 2017 | ||
| χ H | Susceptibility to infection of humans, transmission efficiency from an infected mosquito to human | Dengue | Uniform | Min = 0.56; Max = 0.67 | Vega-Rua et al. 2013 |
| Chikungunya | Uniform | Min = 0.14; Max = 0.84 | Vega-Rua et al. 2013 | ||
| Zika | Uniform | Min = 0.19; Max = 0.39 | Di Luca et al. 2016 | ||
| χ H | Susceptibility to infection of mosquito, transmission efficiency from an infected human to mosquito | Dengue | Uniform | Min = 0.14; Max = 0.39 | Talbalaghi et al. 2010 |
| Chikungunya | Uniform | Min = 0.75; Max = 0.90 | Talbalaghi et al. 2010 | ||
| Zika | Uniform | Min = 0.03; Max = 0.17 | Di Luca et al. 2016 | ||
| 1/ωV | Length of extrinsic incubation period (days) | Dengue | LogNormal | Mean = 2.9–0.08 T, SD = sqrt(1/4.9) | Chan & Johansson 2012 |
| Chikungunya | Uniform | Min = 2; Max = 3) | Dubrulle et al. 2009 | ||
| Zika | Uniform | Min = 7; Max = 14) | Guzzetta 2016 et al. 2016 | ||
| 1/γ | Infectious period in human hosts (days) | Dengue | Uniform | Min = 2; Max = 7 [Accessed 2017/02/27] | http://www.who.int/denguecontrol/human/en/ |
| Chikungunya | Uniform | Min = 2; Max = 6 [Accessed 2017/02/27] | https://wwwnc.cdc.gov/travel/yellowbook/2016/infectious-diseases-related-to-travel/chikungunya | ||
| Zika | Uniform | Min = 4; Max = 7 | Guzzetta et al. 2016 | ||
| k | Biting rate | 0.09 | Uniform | Min = 0.08; Max = 0.1 | Manica et al. 2017 |
| Reporting rate | Dengue | 22% | Shepard et al. 2014 | ||
| Chikungunya | 54% | Moro et al. 2010 | |||
| Zika | 10% | Zhang et al. 2017 | |||
| Symptomatic rate | Dengue | 24% | Shepard et al. 2014 | ||
| Chikungunya | 84% | Moro et al. 2010 | |||
| Zika | 20% | Zhang et al. 2017 | |||
| T | Mean Temperature | — | Mean and SD from air temperature in Rome 2003–2014 (°C) | Meteorological weather station “Roma sud” Hydrographic Service of Regione Lazio (http://www.idrografico.roma.it/annali). | |
| V/H | Vector to host ratio | — | Set according to different scenario | This work |
Model parametrization of the mosquito-borne arbovirus autochthonous transmission and the probability of arrival of infected travelers are described below and detailed in Table 1 as well as in Technical Appendixes (sections 3 and 4).
Autochthonous transmission
Autochthonous transmission is described on the basis of the basic reproduction number (R0) that in the case of mosquito-borne pathogen is computed as the product between the number of infectious mosquitoes generated from an infectious human (R0HV) and the number of infectious humans generated by the infectious mosquitoes surviving the extrinsic incubation period (R0VH), as follows (see21,22):
| 2 |
When R0 < 1 (epidemic threshold), the probability of observing sustained autochthonous transmission after importation of a single case is negligible. On the other hand, when R0 > 1 the probability of observing sustained autochthonous arbovirus transmission after importation of a single case is
| 3 |
as demonstrated by23.
R0 in (2) depends on several eco-epidemiological parameters related to the mosquito-borne arbovirus transmission and the mosquito life cycle that were defined following recent literature on Italian Ae. albopictus (Table 1). For every simulation run, every parameter value was sampled from its specific distribution, unless otherwise specified (Table 1). Temperature-dependence of some parameters (such as mosquito mortality) was incorporated using weekly temperatures recorded in Rome form meteorological stations (for details see Technical Appendixes, section 2).
Precise and reliable estimates of mosquito abundance through time over a large metropolitan area like Rome are challenging to obtain. However, we relied on previous field experiments24,25 and to recent model results13,26 to get an estimate of peaking mosquito abundance. Additionally, the temporal dynamic vector abundance was described as a function of time using previously collected empirical data25 (see Fig. S1 in Technical Appendixes).
On this basis, under the hypothesis of homogeneous mixing, we derived R0 for DENV, CHIKV and ZIKV for three scenarios of human biting rate (HBR = 0.1; 0.5; 1) corresponding respectively to 10%, 50% and 100% of human hosts bitten every day (Technical Appendixes, section 3).
Probability of arrival of infected travelers
The expected number of CHIKV, DENV and ZIKV infected travelers arriving in Rome can be derived from the weekly probability of traveling to Rome, for each selected country, and the weekly number of incident cases recorded in the same country. The number of infected travelers to Rome is assumed to follow a binomial distribution of parameter ρ (probability of traveling to Rome) and size I (number of infected hosts) and, by extension, is the probability of traveling to Rome from country j during week i while Iij is the number of infected human hosts recorded in country j at week i. Therefore, the expected number of infected travelers to Rome from country j during week i (Nij) and its credible intervals can be estimated by simulating draws from a binomial distribution (details available in Technical Appendixes, section 4).
Weekly traveler counts by country of origin at Rome Fiumicino international airport were obtained from Banca d’Italia27 for two categories: visitors and residents. Visitors are travelers arriving directly from their resident country to Rome and staying at least one night in Rome. Residents are (returning) travelers whose resident address is in Rome municipality. In case of travelers returning from multiple destinations, we considered the last country visited as country of origin. For visitors, we estimated the weekly probability of traveling to Rome by dividing the weekly number of visitors from each country by their country population size. A portion of infected host may be not infectious at the moment of traveling, so the probability of travel was corrected by multiplying it by the length of infectious period (in days) to seven (days) fraction. For residents, we set the weekly probability of returning to Rome (their home residence) equal to 1.
Annual incident cases for DENV, CHIKV, ZIKV for 2013, 2014 and 2015 were obtained from available WHO reports (Table S1) and corrected for under-reporting rates for each virus: DENV28, CHIKV29, ZIKV30 (See Technical Appendixes, section 4).
The temporal pattern (by epidemiological week) of infected cases in endemic countries were extracted from the 2013–2015 annual series of DENV for a subset of countries (herein after “reference countries”) from which this information was publicly available either from national websites reporting official data (e.g. the Health Ministry), from the regional offices of WHO or from scientific publications (see Table S2 in Technical Appendixes for consulted websites). The temporal pattern of DENV cases was taken as reference also for CHIKV and ZIKV. The temporal pattern of DENV in reference countries was also used to distribute proportionally the yearly number of cases in similar endemic countries where no temporal pattern were available (See Technical Appendixes, section 4).
Finally, to assess the impact of future potential outbreak, we performed a scenario analysis by increasing either two- or ten fold the number of incident cases in those countries with both a highest air travelers flow with Rome and largest number of incident cases in 2012–2015 (i.e. Brazil, Dominique Republic, India, Mexico, French Polynesia, Thailand).
The model and all statistical analysis were carried out with the R software31.
Results
In order to assess the risk of exotic arbovirus outbreak in Rome under different scenarios of human biting rates (HBR), we first predicted the weekly risk of autochthonous transmission and the probability of introduction of an infected traveler from endemic countries. We then used these estimates to calculate the overall probability of outbreak under different scenarios of incident cases reported worldwide.
Autochthonous transmission (R0)
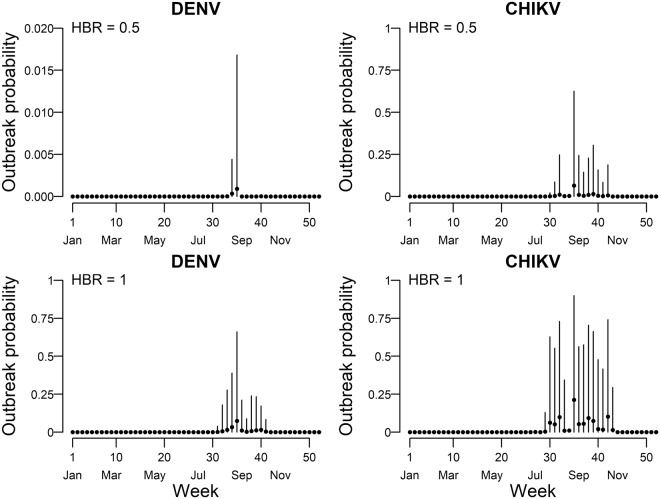
We estimated the risk of arbovirus autochthonous transmission under three scenarios corresponding to 10% (HBR = 0.1), 50% (HBR = 0.5) and 100% (HBR = 1) of human hosts bitten daily, under the hypothesis of homogeneous mixing (Technical Appendixes, section 3) and described the temporal dynamics of the risk based on the actual Ae. albopictus seasonal dynamics in Rome (Fig. S1). Our model predicted the possibility of secondary transmission for DENV and CHIKV (i.e. upper limit of the credible interval of the estimated mean of R0 > 1) when HBR ≥ 1 or ≥0.5, respectively (Fig. 1). No secondary transmission was predicted for ZIKV (Fig. 1). Secondary transmission was estimated to be possible from August to first half of October (weeks 31–42) for DENV at HBR = 1 and CHIKV at HBR = 0.5, and from second half of June to second half of October (weeks 26–44) for CHIKV at HBR = 1.
Figure 1.
Estimated temporal patterns of R0 for Dengue (DENV), Chikungunya (CHIKV) and Zika (ZIKV) viruses under three different scenarios of daily human biting rates (HBR = 0.1 green lines; HBR = 0.5 red lines; HBR = 1 blue lines). On the x-axis the week of the year, on the y-axis the R0 value. Solid lines represent the mean values, shaded area represent the 95% credible interval. The horizontal dashed line indicates the threshold R0 = 1.
Probability of arrival of infected travellers
We estimated the weekly proportion of infected travelers arriving through the international airport of Rome Fiumicino from arbovirus endemic countries and sojourning for at least one night in Rome based on the annual means of visitors (7,256,831/year) and returning residents (2,214,806/year) in the period 2013–2015 (Fig. 2; Fig. S3) and on annual incident cases worldwide (Table S1 and S4). Arrivals of DENV infected travelers were predicted throughout the year (mean: 6.1; CI: 4.9–7.4/100,000 travelers) with higher proportions (>10/100,000 travelers/week) from the first half of February to end of May (weeks 7–21) and a peak of 16.9/100,000 travelers in the first half of April (week 16). The temporal pattern of CHIKV infected travelers (mean: 1, CI: 0.5–1.6/100,000 travelers) was less regular and with lower peaks (>3/100,000 travelers/week) predicted at weeks 3, 30, 42 and the highest peak (6 infected travelers/100,000 travelers/week) in second half of January (week 3). Lower proportions of ZIKV infected travelers (>2 per 100,000 travelers/week) were estimated from January to early May (weeks 1–18), while afterwards the proportion was estimated to be negligible with the exception of week 38 (second half of September), when the estimated proportion of infected reached 5.8/100,000 travelers. Resident returning travelers were the main introduction pathway for CHIKV, while visitor travelers were estimated in similar proportion for DENV and ZIKV (Fig. 2).
Figure 2.
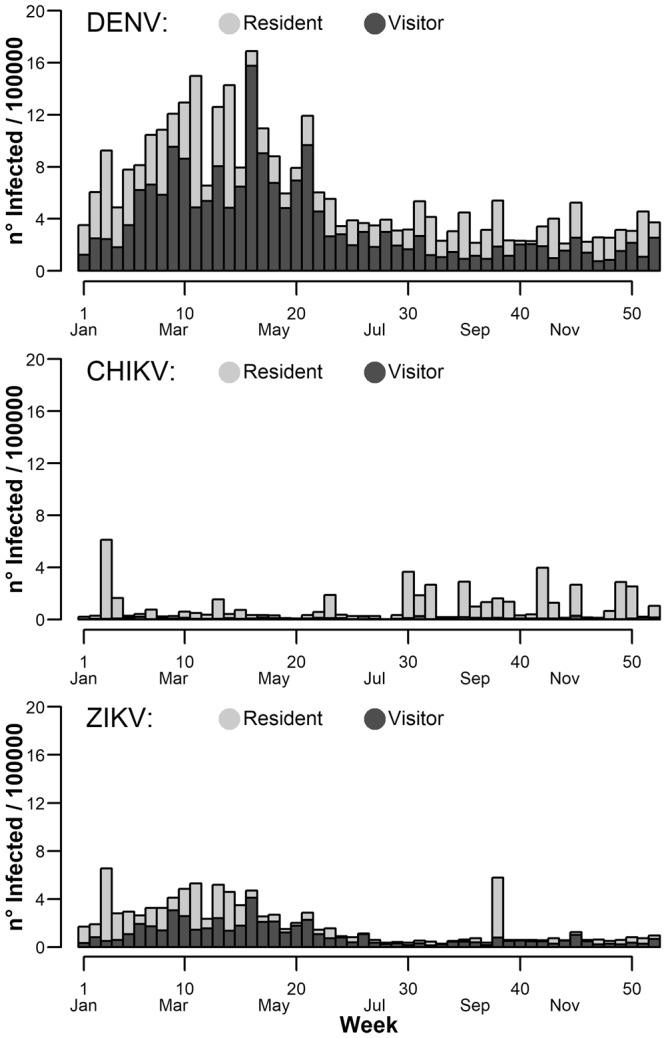
Estimated temporal pattern of worldwide incident cases for Dengue (DENV), Chikungunya (CHIKV) and Zika (ZIKV) viruses in travelers landing at Rome international airport. On the x-axis the week of the year, on the y-axis the number of infected per 100,000 travellers. Light grey bars represent the average number of resident travelers, dark grey bars represent the average number of foreign visitor travellers.
Regarding the different WHO regions, PAHO (Pan American Health Organization) was estimated to be the main source of infected travelers during the whole year for all viruses, while SEARO (South-East Asia), EMRO (Eastern Mediterranean) and WPRO (Western Pacific) regions had a smaller and scattered risk of infection (Fig. S3) and a lower traveler flow (Fig. S4).
The mode of the expected number of yearly cumulative infected travelers to Rome was 98 for DENV (95% Credible Interval 79–118), 14 for CHIKV (95% Credible Interval 8–22) and 26 for ZIKV (95% Credible Interval 16–36) (Fig. 3). The number of notified cases in Lazio region falls within distributions of expected cases (Fig. 3).
Figure 3.
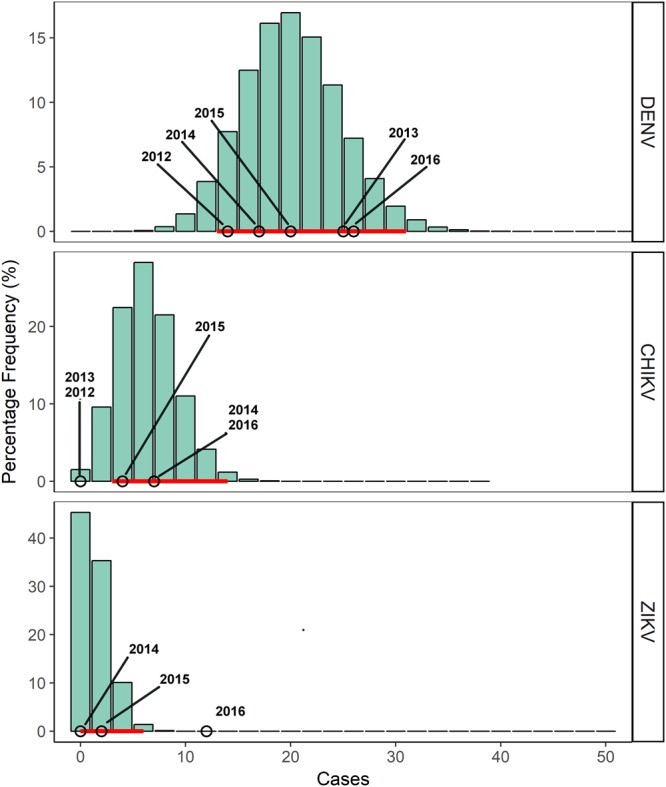
Frequency distributions (%) of predicted cumulative numbers of reported incoming travelers infected by Dengue (DENV), Chikungunya (CHIKV) and Zika (ZIKV) viruses. The histograms are the frequencies (%) of reported incoming infected travelers obtained from model runs while the horizontal red line is the 95% credible interval of predicted cases. Circles are the officially notified cases in Lazio region33,34.
Probability of outbreak in Rome
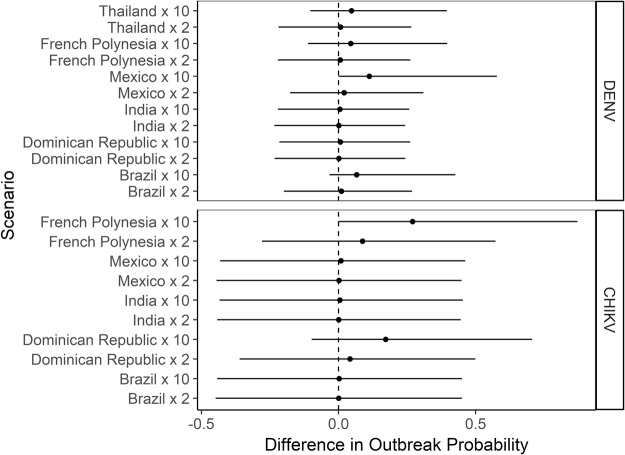
We estimated the mean probability of outbreak in Rome adopting measured flow of resident and visitor travelers to Rome and global number of incident cases in the 2013–2015 period (Fig. 4).
Figure 4.
Weekly mean estimates and 95% credible interval of predicted probability of Dengue (DENV) and Chikungunya (CHIKV) virus outbreaks under two different scenarios of daily human biting rates (HBR = 0.5 upper panels; HBR = 1 lower panels). Dots represent the mean outbreak probability, the vertical lines represent their 95% credible intervals.
The yearly mean probability of outbreak was null for ZIKV at all levels of HBR and for DENV and CHIKV at HBR < 0.5 (data not shown) and negligible for DENV at HBR = 0.5 (Fig. 4). The mean outbreak probability was <0.1 at HBR = 1 for DENV (Fig. 4) and at HBR = 0.5 for CHIKV (Fig. 4), and increased up to 0.21 at HBR = 1 for CHIKV (week 35) (Fig. 4). The resulting annual cumulative probability of outbreak at HBR = 0.5 was 0.001 for DENV and 0.11 for CHIKV while it was 0.13 for DENV and 0.46 for CHIKV at HBR = 1.
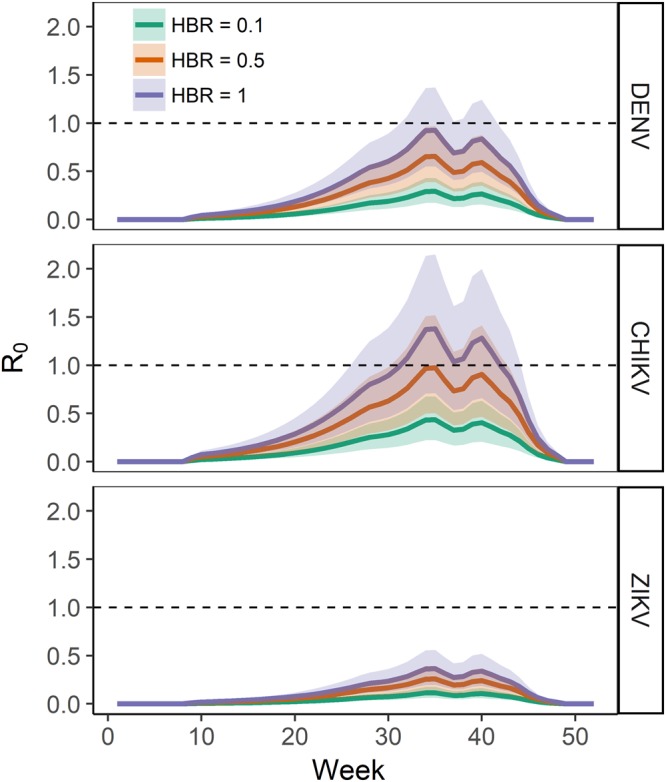
Keeping the baseline flow of travelers from selected countries to Rome stable at HBR = 1, the model predicted that the cumulative yearly probability does not significantly increase with increasing incident cases (Fig. 5), with the exceptions of major DENV epidemics (x10 increase of incident cases) in Mexico and CHIKV in French Polynesia (Fig. 5).
Figure 5.
Yearly cumulative outbreak probability for Dengue (DENV) and Chikungunya (CHIKV) viruses in Rome in the case of HBR = 1. Differences in outbreak probability are shown considering 2012–2015 incident cases worldwide as baseline and comparing them with increasing epidemics (x2, x10) in selected countries. Dots represent the mean difference between baseline and scenario; solid horizontal lines represent the 95% credible interval of the difference distributions. The dashed vertical line indicates no difference.
Discussion
Our modeling exercise based on available data on air passenger flow, incident cases worldwide and on actual entomological field data showed that the outbreak risk in Rome is higher for CHIKV than for DENV and null for ZIKV. The probability of CHIKV-outbreak was estimated to be very low and restricted in time at the HBR = 0.5 scenario, and much higher and extended from mid-June to October at HBR = 1. During the 2017-CHIKV outbreak in Rome, the estimated vector to host ratio at the time of the earliest notified case was 0.4–2.626, which corresponds to a daily HBR between 0.02 and 0.23 (see Technical Appendixes 3). However, Ae. albopictus abundance estimates in Rome25 suggest that it is likely that the majority of the population experiences even lower daily HBR for most of the summer season. It is important to note that values of HBR > 1 may be expected during the peak of the mosquito reproductive season in specific hot-spots areas within the city (e.g. in small urban green areas25 or in the cemetery32), as shown by the very high number of landing Ae. albopictus females (up to 40) collected through human land catch (HLC) by a single volunteer in 15′13.
Overall, the model estimates a very low proportion of infected travelers arriving in Rome each year, i.e. 6.1 (CI = 4.9 −7.4) every 100,000 travelers for DENV, 1.9 (1.2–2.7) for ZIKV and 1 (0.5–1.6) for CHIKV. These estimates match the number of notified cases33–35 and improves an early attempt to estimate the flux of infected travelers based on airline tickets and modeled DENV global incident cases36. Notably, the estimated figure of infected travelers is mostly made up of returning residents, in agreement with data of the National Surveillance System according to which nearly 80% of CHIKV and DENV imported cases are returning travelers residing in Italy37.
Importantly, the period of August is predicted to be conductive for DENV and CHIKV transmission, but this time window can be extended from June to October in hot-spots of Ae. albopictus abundance. Since our model predicts for this period the arrival of a maximum of 9 infected visitors, it is unlikely - although possible - that an Ae. albopictus female bites one of those infected individuals (out of a total of approximately 3,000,000 of inhabitants) and initiates the outbreak. It should be noted that the model assumes homogeneity in the spatial distribution of mosquitoes and hosts while both have (possibly different) aggregate distributions. For example, it is likely that most visitors distribute in the central area of the city where most touristic attractions are located (e.g. Vatican City State). On the other hand, vector abundance is higher in residential areas where small houses with garden are located and where the vector to host ratio is critically high. This is consistent with the higher proportion of as CHIKV autochthonous cases registered in Anzio (a small town about 60 km South of Rome) as opposed to Rome during the 2017 CHIKV outbreak26. The higher outbreak risk for CHIKV compared to DENV is also the result of the higher competence of Ae. albopictus for the former virus38. Notably, the outbreak probability of DENV and CHIKV slightly changed when we simulated epidemics of increased intensity in 5 countries that have a large exchange of travellers with Rome. This is due to a combination of relatively low incidence proportion of CHIKV and DENV in the endemic countries, a short viremic period and the low fractions of travellers to Rome compared to the total population.
As in all modelling exercises, our model has some limitations. First, WHO estimates of country specific annual arbovirus cases are known to be prone to errors (see39). We assessed the temporal pattern of incident 2012–2015 DENV cases from reports available on official websites of national public health organisations (e.g. the national health ministry) or WHO regional offices. Therefore, the reliability of the data may differ according to the country specific technical sophistication of case assessment and reporting procedure. Second, we used DENV incident case temporal pattern to infer seasonal transmission dynamics and applied the same temporal pattern to CHIKV and ZIKV simulations and to all countries in the same WHO sub-region. Third, estimates for key epidemiological parameters, such as Ae. albopictus competence for ZIKV, are based on a limited number of experiments. This implies that model parametrization ought to be updated when more recent and reliable estimates will be available. Fourth, outbreak probability is computed without considering possible reactive interventions carried out by public health authorities after the detection of each case in order to reduce the transmission risk.
Finally, although a formal sensitivity analysis of model parameters was not attempted, we inferred the uncertainty of model output by simulation. Each parameter was resampled 100,000 times from parameter-specific sampling distributions as done by others40,41, resulting in an ensemble of possible scenarios rather than a parameter dependent one. Therefore, by calculating the most reliable interval of outbreak probability over the 100,000 simulations we implicitly included the uncertainty in the model output generated by model parameters.
Conclusion
Our study provides the first quantitative estimation of DENV, CHIKV and ZIKV outbreak risk in south European metropolitan area and allows to predict several patterns of the potential outbreak: (i) which arbovirus is most likely to cause and outbreak, (ii) in which period of the year the probability of secondary transmission is highest, (iii) which type of travelers and origin of flights are more likely to cause virus importation, and (iv) the relative importance of an increase in vector density or in the global number of incident cases. The approach proposed can be easily adapted to other cities for which data on the temporal dynamics of travelers and seasonal dynamic of Ae. albopictus are available and serve as guide for public health officers in charge of preventing arbovirus outbreaks.
Given the latest 2017 CHIKV outbreak in the town of Anzio nearby Rome with limited propagation of the outbreak to Rome iteself1, next research should focus on factors influencing local transmission at the spatial scale relevant for the host-vector contact. Since both the vectors and the human population exhibit an aggregate spatial distribution, a more precise risk model should tackle the relevant spatial scale where those distributions do overlap with the probability of arrival of an infected traveler.
Electronic supplementary material
Acknowledgements
We thank Luca Delucchi for technical assistance with cluster computing and Stefano Merler for useful suggestions on methodological issues. The study was partially supported by an internal Sapienza Grant (Ateneo 2016). R.R. and M.M. were partly supported by the European Union’s Horizon 2020 Research and Innovation Programme under ZIKAlliance Grant Agreement no. 734548.
Author Contributions
A.G.S. Conceptualization, data curation, writing original draft, review & editing. M.M. Conceptualization, formal analysis, writing original draft, review & editing. R.R. Supervision, original draft review & editings. A.d.T. Supervision, original draft review & editing. B.C. Conceptualization, data curation, original draft review & editing
Data Availability
The data used as model inputs are third party data freely available.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-018-34664-5.
References
- 1.Liang G, Gao X, Gould EA. Factors responsible for the emergence of arboviruses; strategies, challenges and limitations for their control. Emerg. Microbes Infect. 2015;4:e18. doi: 10.1038/emi.2015.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weaver SC, Reisen WK. Present and future arboviral threats. Antiviral Res. 2010;85:328–345. doi: 10.1016/j.antiviral.2009.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.La Ruche G, et al. First two autochthonous dengue virus infections in metropolitan France, September 2010. Euro Surveill. 2010;15:19676. [PubMed] [Google Scholar]
- 4.Marchand E, et al. TAutochthonous case of dengue in France, October 2013. Euro Surveill. 2013;18:20661. doi: 10.2807/1560-7917.ES2013.18.50.20661. [DOI] [PubMed] [Google Scholar]
- 5.Gjenero-Margan I, et al. Autochthonous dengue fever in Croatia, August-September 2010. Euro Surveill. 2011;16:1–4. [PubMed] [Google Scholar]
- 6.Grandadam M, et al. Chikungunya virus, Southeastern France. Emerg. Infect. Dis. 2011;17:910–913. doi: 10.3201/eid1705.101873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rezza G, et al. Infection with chikungunya virus in Italy: an outbreak in a temperate region. Lancet. 2007;370:1840–1846. doi: 10.1016/S0140-6736(07)61779-6. [DOI] [PubMed] [Google Scholar]
- 8.Venturi G, et al. Detection of a chikungunya outbreak in Central Italy, August to September 2017. Euro Surveill. 2017;22:1–4. doi: 10.2807/1560-7917.ES.2017.22.39.17-00646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lambrechts L, Scott TW, Gubler DJ. Consequences of the expanding global distribution of Aedes albopictus for dengue virus transmission. PLoS Negl. Trop. Dis. 2010;4:e646. doi: 10.1371/journal.pntd.0000646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ciota AT, et al. Effects of Zika Virus Strain and Aedes Mosquito Species on Vector Competence. Emerg. Infect. Dis. 2017;23:1110–1117. doi: 10.3201/eid2307.161633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weaver SC. Arrival of chikungunya virus in the new world: prospects for spread and impact on public health. PLoS Negl. Trop. Dis. 2014;8:e2921. doi: 10.1371/journal.pntd.0002921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cunze S, Koch LK, Kochmann J, Klimpel S. Aedes albopictus and Aedes japonicus - two invasive mosquito species with different temperature niches inEurope. Parasit. Vectors. 2016;9:573. doi: 10.1186/s13071-016-1853-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Manica M, Rosà R, Della Torre A, Caputo B. From eggs to bites: do ovitrap data provide reliable estimates of Aedes albopictus biting females? PeerJ. 2017;5:e2998. doi: 10.7717/peerj.2998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wearing HJ, Robert MA, Christofferson RC. Dengue and chikungunya: modelling the expansion of mosquito-borne viruses into naïve populations. Parasitology. 2016;143:1–14. doi: 10.1017/S0031182016000421. [DOI] [PubMed] [Google Scholar]
- 15.Guzzetta G, et al. Assessing the potential risk of Zika virus epidemics in temperate areas with established Aedes albopictus populations. Eurosurveillance. 2016;21:1–6. doi: 10.2807/1560-7917.ES.2016.21.15.30199. [DOI] [PubMed] [Google Scholar]
- 16.Guzzetta G, et al. Potential Risk of Dengue and Chikungunya Outbreaks in Northern Italy Based on a Population Model of Aedes albopictus (Diptera: Culicidae) PLoS Negl. Trop. Dis. 2016;10:e0004762. doi: 10.1371/journal.pntd.0004762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rocklöv J, et al. Assessing Seasonal Risks for the Introduction and Mosquito-borne Spread of Zika Virus in Europe. EBioMedicine. 2016;9:250–256. doi: 10.1016/j.ebiom.2016.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Johansson MA, et al. On the treatment of Airline travelers in mathematical models. PLoS One. 2011;6:1–7. doi: 10.1371/journal.pone.0022151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johansson MA, et al. Assessing the Risk of International Spread of Yellow Fever Virus: A Mathematical Analysis of an Urban Outbreak in Asunción, 2008. Am. J. Trop. Med. Hyg. 2012;86:349–358. doi: 10.4269/ajtmh.2012.11-0432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Johansson MA, Powers AM, Pesik N, Cohen NJ, Staples JE. Nowcasting the spread of chikungunya virus in the Americas. PLoS One. 2014;9:e104915. doi: 10.1371/journal.pone.0104915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith DL, et al. Ross, macdonald, and a theory for the dynamics and control of mosquito-transmitted pathogens. PLoS Pathog. 2012;8:e1002588. doi: 10.1371/journal.ppat.1002588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Poletti P, et al. Transmission potential of chikungunya virus and control measures: the case of Italy. PLoS One. 2011;6:e18860. doi: 10.1371/journal.pone.0018860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lloyd AL, Zhang J, Root AM. Stochasticity and heterogeneity in host-vector models. J. R. Soc. Interface. 2007;4:851–863. doi: 10.1098/rsif.2007.1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cianci D, et al. Estimating mosquito population size from mark-release-recapture data. J. Med. Entomol. 2013;50:533–542. doi: 10.1603/ME12126. [DOI] [PubMed] [Google Scholar]
- 25.Manica M, et al. Spatial and Temporal Hot Spots of Aedes albopictus Abundance inside and outside a South European Metropolitan Area. PLoS Negl. Trop. Dis. 2016;10:e0004758. doi: 10.1371/journal.pntd.0004758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Manica M, et al. Transmission dynamics of the ongoing chikungunya outbreak in Central Italy: from coastal areas to the metropolitan city of Rome, summer 2017. Eurosurveillance Bull. Eur. sur les Mal. Transm. =Eur. Commun. Dis. Bull. 2017;22:17–00685. doi: 10.2807/1560-7917.ES.2017.22.44.17-00685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Banca d’Italia. Indagine sul turismo internazionale at www.bancaditalia.it/statistiche (2016).
- 28.Shepard DS, et al. Approaches to refining estimates of global burden and economics of dengue. PLoS Negl. Trop. Dis. 2014;8:e3306. doi: 10.1371/journal.pntd.0003306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moro ML, et al. Chikungunya virus in North-Eastern Italy: a seroprevalence survey. Am. J. Trop. Med. Hyg. 2010;82:508–11. doi: 10.4269/ajtmh.2010.09-0322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kucharski AJ, et al. Transmission Dynamics of Zika Virus in Island Populations: A Modelling Analysis of the 2013-14 French Polynesia Outbreak. PLoS Negl. Trop. Dis. 2016;10:e0004726. doi: 10.1371/journal.pntd.0004726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.R Core Development Team. R: a language and environment for statistical computing, 3.2.1, http://www.r-project.orgISBN 3-900, (2015).
- 32.Caputo B, et al. The ‘auto-dissemination’ approach: a novel concept to fight Aedes albopictus in urban areas. PLoS Negl. Trop. Dis. 2012;6:e1793. doi: 10.1371/journal.pntd.0001793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ministero della Salute. Sorveglianza dei casi umani di Chikungunya, Dengue, West Nile Disease ed altre arbovirosi e valutazione del rischio di trasmissione in Italia– 2015 (2015).
- 34.Ministero della Salute. Sorveglianza dei casi umani di Chikungunya, Dengue, West Nile Disease ed altre arbovirosi e valutazione del rischio di trasmissione in Italia– 2017. Piano Nazionale di sorveglianza e risposta alle arbovirosi trasmesse da zanzare (Aedes sp.) con particolare riferimento ai virus Chikungunya, Dengue e Zika - 2017 (2017).
- 35.Vairo F, et al. Regional surveillance for arbovirus in Lazio Region, Italy during the ZIKV epidemic in Latin America. Int. J. Infect. Dis. 2016;53:16. doi: 10.1016/j.ijid.2016.11.044. [DOI] [Google Scholar]
- 36.Quam MB, et al. Estimating air travel-associated importations of dengue virus into Italy. J. Travel Med. 2015;22:186–93. doi: 10.1111/jtm.12192. [DOI] [PubMed] [Google Scholar]
- 37.Napoli C, Salcuni P, Pompa MG, Declich S, Rizzo C. Estimated imported infections of chikungunya and dengue in Italy, 2008 to 2011. J. Travel Med. 2012;19:294–297. doi: 10.1111/j.1708-8305.2012.00640.x. [DOI] [PubMed] [Google Scholar]
- 38.Talbalaghi A, Moutailler S, Vazeille M, Failloux AB. Are Aedes albopictus or other mosquito species from northern Italy competent to sustain new arboviral outbreaks? Med. Vet. Entomol. 2010;24:83–87. doi: 10.1111/j.1365-2915.2009.00853.x. [DOI] [PubMed] [Google Scholar]
- 39.Bhatt S, et al. The global distribution and burden of dengue. Nature. 2013;496:504–507. doi: 10.1038/nature12060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ng V, et al. Assessment of the probability of autochthonous transmission of chikungunya virus in Canada under recent and projected climate change. Environ. Health Perspect. 2017;125:1–12. doi: 10.1289/EHP168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Manica M, et al. Transmission dynamics of the ongoing chikungunya outbreak in Central Italy: from coastal areas to the metropolitan city of Rome, summer 2017. Eurosurveillance. 2017;22:18–41. doi: 10.2807/1560-7917.ES.2017.22.44.17-00685. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used as model inputs are third party data freely available.