Abstract
Objective:
This study aimed to examine whether the Unified Protocol (UP), a transdiagnostic cognitive-behavioral therapy for emotional disorders (i.e., anxiety, mood, and related disorders), is efficacious in the treatment of co-occurring emotional disorders compared to established single disorder protocols (SDPs) that target specific disorders (e.g., panic disorder).
Method:
Participants included 179 adults seeking outpatient psychotherapy. Participant age ranged from 18 to 66 years, with an average of 30.66 years (SD = 10.77). The sample was 55% female and mostly Caucasian (83%). Diagnostic assessments were completed with the Anxiety Disorder Interview Schedule (ADIS), and disorder-specific, clinician-rated measures for the comorbid diagnoses of interest.
Results:
In both treatment conditions, participants’ mean number of diagnoses dropped significantly from baseline to posttreatment, and baseline to 12-month followup. Additionally, large effects were observed for changes in comorbid generalized anxiety (ESSG: UP = −1.72; SDP = −1.98), social anxiety (ESSG: UP = −1.33, −0.86; SDP = −1.60, −1.54), and depression (ESSG: UP = −0.83; SDP = −0.84). Significant differences were not observed in between-group comparisons.
Conclusions:
Results suggest that both the UP and SDPs are efficacious in reducing symptoms of comorbid emotional disorders. The clinical, practical, and cost-effective advantages of transdiagnostic CBT are discussed.
Keywords: Unified Protocol, cognitive-behavioral therapy, transdiagnostic treatment, comorbidity, emotional disorders
Emotional disorders (i.e., anxiety, mood, and related disorders; Barlow, 2000) are characterized by high rates of comorbidity (Barlow et al., 2016); for example, estimates of lifetime comorbidity rates for anxiety and depressive disorders are as high as 75% (Brown & Barlow, 2009). Research suggests that patients with comorbid emotional disorders demonstrate poorer treatment outcomes than patients with a single diagnosis (Rosellini et al., 2015). Specifically, comorbidity has been linked to chronicity and severity of psychopathology, relapse rates, treatment seeking, suicide potential, and overall psychosocial functioning (Brown et al., 2001).
Recent conceptualizations of the prevalent comorbidity amongst emotional disorders have emphasized the presence of shared underlying mechanisms that contribute to their onset (e.g., Wilamowska et al., 2010). Specifically, neuroticism, defined as the tendency for frequent and intense negative emotions accompanied by perceived lack of control over these experiences, has been implicated across a range of conditions (Barlow et al., 2014), and higher levels of this trait are associated with increased rates of comorbidity (Griffith et al., 2010). Beyond the neurotic temperament, individuals with emotional disorders also display shared functional processes that maintain their symptoms; specifically, frequently occurring negative emotions are perceived as aversive, prompting avoidant coping that ultimately increases the frequency and intensity of these experiences (see Sauer-Zavala & Barlow, 2014).
Transdiagnostic interventions that target shared mechanisms may confer both clinical and practical advantages over more traditional protocols focused on a single Diagnostic and Statistical Manual (DSM; e.g., American Psychiatric Association, 2013) disorder (Sauer-Zavala et al., 2017). First, by directly targeting common processes, transdiagnostic treatments can simultaneously address symptoms of co-occurring conditions. Additionally, transdiagnostic approaches may address the time and training burden that has limited successful dissemination of evidence-based psychological treatments as clinicians need only learn the basics of one treatment approach to provide research supported care to a range of common presentations. Several studies have found transdiagnostic treatments to be efficacious in the treatment of emotional conditions (Akbari et al., 2015; Milosevic et al., 2017; Palermo et al., 2016), as well as in the treatment of comorbid emotional disorders compared to other specific interventions or treatment as usual more broadly (Stice et al., 2015; Titcov, et al., 2015).
The Unified Protocol for Transdiagnostic Treatment of Emotional Disorders (UP; Barlow et al., 2011a; Barlow et al., 2011b; Barlow et al., 2018a; Barlow et al., 2018b) is a transdiagnostic, cognitive-behavioral intervention consisting of 5 core modules that target the abovementioned temperamental characteristics underlying all anxiety, depressive, and related disorders. The UP has demonstrated efficacy in reducing general symptoms of anxiety and depression (Ellard et al., 2010; Farchione et al., 2012) and these improvements were maintained 18 months after treatment (Bullis et al., 2014). Further, in a recently conducted larger clinical trial comparing the UP to gold-standard, single-disorder protocols (SDPs) for generalized anxiety disorder (GAD), social anxiety disorder (SAD), Panic Disorder (PD), and obsessive-compulsive disorder (OCD), the transdiagnostic UP approach led to equivalent symptom reduction on patients’ principal diagnosis compared to the SDP associated with that disorder. Notably, the UP condition evidenced lower rates of attrition than the SDP condition (Barlow et al., 2017).
The current study aimed to explore the efficacy of the UP in treating comorbid emotional conditions in a diagnostically heterogeneous sample from this larger clinical trial (Barlow et al., 2017). Specially, this study had three aims: 1) Characterize comorbidity in the current sample, 2) Evaluate whether the UP indeed leads to reductions in symptoms of comorbid disorders, and 3) Compare the UP to established SDPs in the reduction of comorbid psychopathology.
Methods
Participants
Individuals in the present study were a subset of participants from a clinical trial comparing two active treatment conditions (UP and SDPS targeting four principal anxiety disorders) and a waitlist control condition (n = 223; see Barlow et al., 2017). The current study included those participants who received psychological treatment during the trial (n = 179), and excluded individuals that were randomized to the waitlist condition. Additional information regarding inclusion and exclusion criteria can be found in Barlow et al. (2017).
Participants in the current subsample ranged in age from 18 to 66 years old, with an average age of 30.60 years (SD = 10.70). The majority of the sample identified as female (55.30%), non-Hispanic White (76.0%), and college educated or higher (65.40%). All participants met diagnostic criteria for at least one principal (most interfering and severe) anxiety disorder restricted to the following four categories: panic disorder, with or without agoraphobia (PD/A; n = 47 [26.30%]); generalized anxiety disorder (GAD; n = 49 [27.40%]), obsessivecompulsive disorder (OCD; n = 35 [19.60%]), or social anxiety disorder (SAD; n = 48 [26.80%]). Clinical diagnoses were made with the Anxiety Disorder Interview Schedule (ADIS; Di Nardo et al., 1994; Brown & Barlow, 2014).
Procedures
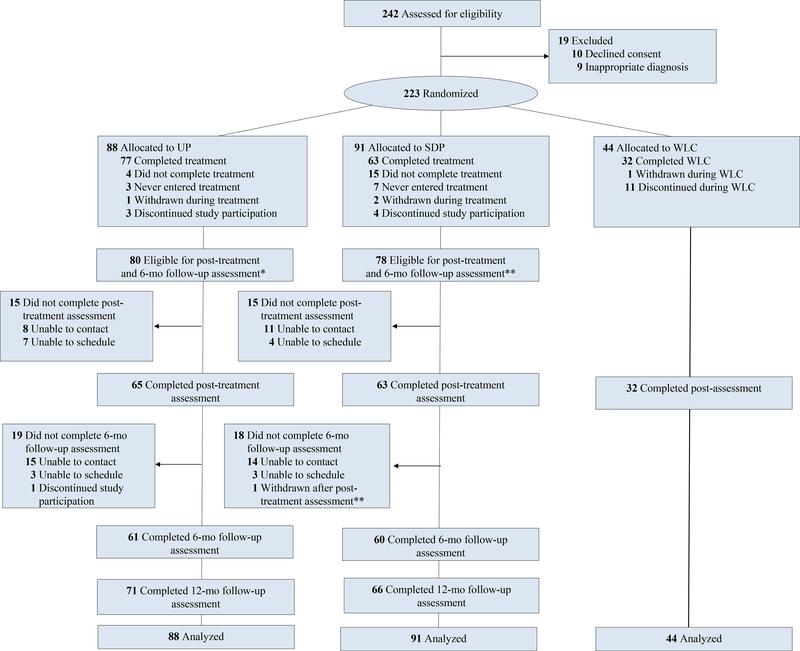
The clinical trial was approved by the study site’s Institutional Review Board, and all participants provided written informed consent prior to enrolling. The current study was carried out in accordance with the latest version of the Declaration of Helsinki. Figure 1 illustrates the study design and patient flow. As noted above, participants were randomized to either a waitlist condition or treatment with the UP or SDPs corresponding to their principal diagnosis (1:2:2 allocation ratio, respectively). All participants were assigned one principal diagnosis after administration of a diagnostic interview (see Measures below); if randomized to the SDP condition, the principal diagnosis determined which SDP the participant received. SDPs included: 1) SAD: Managing Social Anxiety: A Cognitive-Behavioral Therapy Approach – 2nd edition (MSA-II; Hope et al., 2006; Hope et al., 2000); 2) PD/A: Mastery of Your Anxiety and Panic – 4th edition (MAP-IV; Barlow & Craske, 2007; Craske & Barlow, 2007); 3) GAD: Mastery of Your Anxiety and Worry – 2nd edition (MAW-II; Craske & Barlow, 2006; Zinbarg et al., 2006); and 4) OCD: Treating Your OCD with Exposure and Response (Ritual) Prevention Therapy – 2nd edition (Foa et al., 2012; Yadin et al., 2012).
Figure 1.
Recruitment Flow Diagram
The number and duration of sessions was determined via published guidelines associated with each SDP protocol; UP treatment (session number/duration) was provided in accordance with recommendations for the SDP corresponding to the patient’s principal diagnosis. Specifically, patients with GAD, SAD, and OCD received 16 sessions (within a 21-week treatment window) and patients with PD/A received 12 sessions (within a 16-week treatment window). Further, sessions were 50-minutes in duration, with the exception of treatment for participants with a principal diagnosis of OCD, for whom sessions lasted 90 minutes. To ensure treatment fidelity, expert raters associated with the development of each protocol assessed 20% of randomly selected treatment sessions for adherence and competence. Overall scores for treatment fidelity fell in the good to excellent range (M: UP = 4.44/5; SDPs = 4.09/5).
Patients were also required to attend assessment visits while enrolled in the trial. Data were collected at baseline, posttreatment, and 12-month follow-up. All assessments were conducted by independent study evaluators who were blinded to participants’ study condition.
Measures
Anxiety Disorders Interview Schedule
(ADIS; Di Nardo, et al., 1994; Brown & Barlow, 2014). The ADIS is a semi-structured clinical interview based on diagnostic criteria from the Diagnostic and Statistical Manual (DSM; APA, 2013). Study evaluators assessed patients using the ADIS for anxiety, mood, somatic symptom disorders, and substance use disorders, and screened them for other disorders (e.g., ADHD, eating disorders). Due to the publication of DSM-5 (APA, 2013) partway through the clinical trial, 137 patients (76.5%) were assigned diagnoses based on DSM-IV criteria and 42 patients (23.5%) were assigned diagnoses based on DSM-5 criteria. Since panic disorder and agoraphobia are separated in DSM-5, study evaluators rated these diagnoses together as overall PD/A symptoms for those patients diagnosed according to the new diagnostic criteria in DSM-5 (APA, 2013).
Panic Disorder Severity Scale
(PDSS; Shear et al., 1997). The PDSS is a brief, 7-item, clinician-rated measure that was designed to assess panic disorder symptoms and their impact on an individual’s functioning. Each item on the PDSS falls on a 5-point Likert-scale, with higher scores indicating higher symptom severity and impairment. The PDSS displays good concurrent validity and inter-rater reliability, including in treatment outcome research for patients with panic disorder with or without agoraphobia (Shear et al., 1997; Shear et al., 2001a; Wuyek et al., 2011). Study evaluators administered the PDSS to all participants with a clinical PD/A diagnosis at all assessment visits.
Liebowitz Social Anxiety Scale
(LSAS; Liebowitz, 1987). The LSAS is a 24-item, clinician-rated scale that measures both fear and avoidance of social interactions and performances. A total score was obtained by adding the separate fear and avoidance scores for each item, with higher scores indicating higher severity. The LSAS has demonstrated strong internal consistency and convergent validity with other measures of SAD (Fresco et al., 2001; Heimberg, et al., 1999). Study evaluators administered the LSAS to all patients in the trial with a clinical SAD diagnosis at all assessment time-points.
Generalized Anxiety Disorder Severity Scale
(GADSS; Shear et al., 2006). The GADSS is a 6-item, clinician-rated measure that evaluates core symptoms of GAD and their impact on an individual’s functioning. Items are rated on a 5-point scale, ranging from 0 (none) to 4 (very severe). Psychometric studies have shown that the GADSS has high internal consistency, good convergent validity with other measures, and captures changes in symptoms and impairment over the course of treatment (Shear et al., 2006). Study evaluators administered the GADSS to all patients in the trial with a clinical GAD diagnosis at all assessments.
Yale-Brown Obsessive Compulsive Scale Interview-2nd edition
(Y-BOCS-II; Goodman et al., 1989; Storch et al., 2010). The Y-BOCS-II is a 10-item, clinician-rated interview designed to assess severity of OCD symptoms and resulting impairment. Items on the scale are scored on a 0 (none) to 5 (extreme) Likert-scale. The Y-BOCS has demonstrated high internal consistency, one-week test–retest reliability, and interrater reliability as well as good construct validity (Goodman et al., 1989; Storch et al., 2010; Wu et al., 2016). Patients with an OCD diagnosis were given a 64-item checklist at baseline, listing possible obsessions and compulsions. In addition, these patients were administered the Y-BOCS-II at all assessment visits.
Structured Interview Guide for the Hamilton Depression Rating Scale
(SIGH-D; Williams, 1988). The SIGH-D is a 17-item, clinician-rated interview guide that was developed to provide specific instructions for administration and scoring of the Hamilton Rating Scale for Depression (HRSD; Hamilton, 1960; Shear et al., 2001b). The SIGH-D has demonstrated good inter-rater and test-retest reliability (Shear et al., 1988). This interview was completed with all participants at each assessment point.
Results
Aim 1.
A summary of the diagnostic composition of the sample can be viewed in Table 1. Comorbidity was highly prevalent; 150 (83.80%) participants met diagnostic criteria for at least one co-occurring disorder at baseline assessment, with a range of one to seven diagnoses (M = 2.49, SD = 1.44). Chi square analyses indicated no significant differences in the presence of comorbid diagnoses as a function of treatment condition at baseline, χ2 (1, n = 179) =.25, p =.61, phi =.05. Notably, almost half of the GAD sample met diagnostic criteria for co-occurring SAD. Co-occurring PD and GAD were diagnosed most frequently among participants with principal OCD.
Table 1.
Presence of Comorbid Diagnoses by Principal Diagnosis and Treatment Condition (N = 179; UP n = 88; SDP n = 91)
| CO-SAD | CO-PD | CO-AG | CO-GAD | CO-OCD | CO-DEP | |
|---|---|---|---|---|---|---|
| SAD | ||||||
| UP n = 23 (26%) | - | 2 (9%) | 1 (4%) | 0 | 1 (4%) | 5 (22%) |
| SDP n = 25 (28%) | - | 0 | 0 | 7 (28%) | 3 (12%) | 2 (8%) |
| PD/A | ||||||
| UP n = 25 (28%) | 6 (24%) | - | 22 (88%) | 7 (28%) | 1 (4%) | 2 (8%) |
| SDP n = 22 (24%) | 6 (27%) | 2 (10%) | 20 (91%) | 8 (36%) | 0 | 1 (5%) |
| GAD | ||||||
| UP n = 22 (25%) | 10 (45%) | 1 (5%) | 1 (5%) | - | 1 (5%) | 4 (18%) |
| SDP n = 27 (30%) | 10 (37%) | 4 (15%) | 4 (15%) | - | 7 (26%) | 5 (19%) |
| OCD | ||||||
| UP n = 18 (21%) | 7 (39%) | 0 | 0 | 4 (22%) | - | 1 (6%) |
| SDP n = 17 (19%) | 4 (24%) | 1 (6%) | 0 | 5 (29%) | - | 1 (6%) |
Note. Patients were included in the PRIN PD/A category if they met diagnostic criteria for DSM- IV PD/A or DSM-5 diagnostic criteria for PD. As represented above, all patients in the UP condition had principal PD and 22 had co-occurring AG. In the SDP condition, 20 patients had principal PD with co-occurring AG, and 2 patients had principal AG
Aim 2.
The second aim of this study was to explore the extent to which the UP addresses comorbid disorders in a diagnostically heterogeneous sample with a high degree of co-occurring conditions. To address this aim, we first examined the UP’s efficacy in significantly reducing 1) the number of clinically significant diagnoses on the ADIS from baseline to posttreatment and baseline to 12-month follow-up and 2) scores on disorder-specific, clinician-rated measures from baseline to posttreatment and baseline to 12-month follow-up. First, paired-samples t-tests were conducted to evaluate the impact of the UP on participants’ mean number of clinically significant diagnoses. There was a statistically significant decrease in number of diagnoses from baseline (M = 2.56, SD = 1.47) to posttreatment (M = .84, SD = 1.30), t (62) = 8.96, p < .0005, and baseline (M = 2.42, SD = 1.40) to 12-month follow-up (M = .83, SD = 1.20), t (68) = 9.41, p < .0005.
Next, to ensure that our estimates were limited to the UP’s effects on comorbid conditions, we restricted our sample to include individuals with co-occurring PD/A (or PD or AG), SAD, GAD, OCD, major depressive disorder (MDD), and persistent depressive disorder (PDD), which were evaluated at each time point by clinician-rated, disorder-specific measures (see Method). For example, individuals with a principal diagnosis of SAD were removed from our evaluations of change on the LSAS, our measure of SAD severity. Standardized Mean Gain Effect sizes (ESSG) were calculated to determine the magnitude of change from baseline to posttreatment, and baseline to 12-month follow-up. Standardized mean gain was chosen for these analyses due its inclusion of a correction for repeated measures assessments (King et al., 2006). Large effects were seen for change on the GADSS, LSAS, and HAM-D (see Table 2). Due to small number of individuals with comorbid PD/A and OCD, analyses were not completed for the PDSS baseline to posttreatment (n = 2), or the YBOCS for posttreatment (n = 2) or 12-month follow-up (n = 2).
Table 2.
Effect Sizes for Change on Comorbid Disorder-Specific Measures by Treatment Condition
| Unified Protocol | Single Disorder Protocols | |||||
|---|---|---|---|---|---|---|
| ES | SE | 95% CI | ES | SE | 95% CI | |
| Baseline to Posttreatment: | ||||||
| GAD (GADSS) | −1.72 | 0.52 | −2.73: −0.76 | −1.98 | 0.44 | −1.69: −0.03 |
| PD/A (PDSS) SAD | - | - | - | - | - | - |
| (LSAS fear) | −1.33 | 0.33 | −1.98: −0.67 | −1.60 | 0.47 | −2.53: −0.67 |
| (LSAS avoidance) | −0.86 | 0.30 | −1.45: −0.27 | −1.54 | 0.49 | −2.50: −0.59 |
| OCD (YBOCS) | - | - | - | −0.72 | 0.36 | −1.42: −0.01 |
| DEP (HAM-D) | −0.83 | 0.15 | −1.12: −0.54 | −0.84 | 0.18 | −1.19: −0.48 |
| Baseline to 12 mo f/u: | ||||||
| GAD (GADSS) | −0.81 | 0.40 | −1.59: −0.03 | −1.76 | 0.48 | −2.70: −0.82 |
| PD/A (PDSS) | −2.85 | 1.48 | −5.76: 0.05 | - | - | - |
| SAD | ||||||
| (LSAS fear) | −1.63 | 0.39 | −2.39: −0.88 | −1.42 | 0.43 | −2.27: −0.57 |
| (LSAS avoidance) | −1.06 | 0.32 | −1.70: −0.43 | −1.59 | 0.47 | −2.51: −0.66 |
| OCD (YBOCS) | - | - | - | −0.69 | 0.39 | −1.45: 0.08 |
| DEP (HAM-D) | −0.80 | 0.16 | −1.12: −0.48 | −0.95 | 0.19 | −1.32: −0.58 |
Note. ES = Standardized Mean Gain effect size.
Aim 3.
As described above, Aim 3 of the present study was to explore whether the transdiagnostic UP approach was associated with greater decreases in comorbid conditions than single disorder approaches designed to address one primary condition. Consistent with analytic procedures used in our primary outcomes paper (Barlow et al., 2017), we combined the individual SDPs into one variable to represent all of the SDPs used in the trial. Similar to Aim 2, we compared the UP to SDP on 1) number of clinically significant diagnoses on the ADIS at baseline, posttreatment, and 12-month follow-up, and 2) scores on disorder-specific measures from baseline to post-treatment, and baseline to 12-month follow-up. First, independent samples t-tests revealed no significant differences for mean number of diagnoses between the UP and SDPs at baseline (UP M = 2.48, SD = 1.44; SDP M = 2.51, SD = 1.46; t (177) = −.13, p = .90), posttreatment (UP M = .84, SD = 1.30; SDP M = 1.05, SD = 1.27; t (118) = −.90, p = .37), or 12- month follow-up (UP M = .82, SD = 1.20; SDP M = .83, SD = 1.21; t (132) = −.02, p = .98).
To evaluate changes on the disorder-specific measures by treatment condition at each time point, within group and between group effect sizes were examined. Again, individuals with the principal diagnosis associated with each disorder-specific measure were removed, allowing for examination of specific change in comorbid diagnoses. And again, due to small sample sizes, analyses were not completed for the PDSS or the YBOCS. Effect sizes (ESSG) were calculated to determine the magnitude of change from pre- to post-treatment and from pre-treatment to followup for the SDP condition (see Table 2). Similar to the UP condition, large effects were seen for change on the GADSS, LSAS, and HAM-D. Next, between group effect sizes (Hedge’s g, with correction for small sample size) were calculated to determine the magnitude of the difference between conditions at each time point on disorder-specific symptom measures (see Table 3). Very small, nonsignificant effects were observed on the HAM-D (−0.04 to 0.10) at all time points between the UP and SDP, and small to moderate (though still nonsignificant) effects were observed on the GADSS (−0.4 to 0.6) and LSAS (−0.5 to 0.6). In sum, results suggested that there were no significant differences between UP and SDP in decreasing comorbid symptoms at posttreatment and 12-month follow-up for GAD, SAD, or DEP.
Table 3.
Effect Sizes for Between Group Differences on Comorbid Disorder-Specific Measures
| Pooled SD | Hedge ’s g | SE | 95% CI | |
|---|---|---|---|---|
| Baseline: | ||||
| GAD (GADSS) | 3.38 | −0.39 | 0.33 | −1.04: 0.27 |
| SAD | ||||
| (LSAS fear) | 12.39 | −0.46 | 0.30 | −1.06: 0.13 |
| (LSAS avoidance) | 14.10 | −0.51 | 0.30 | −1.11: 0.09 |
| DEP (HAM-D) | 6.80 | −0.04 | 0.16 | −0.35: 0.27 |
| Posttreatment: | ||||
| GAD (GADSS) | 3.31 | −0.29 | 0.42 | −1.12: 0.54 |
| SAD | ||||
| (LSAS fear) | 10.59 | 0.58 | 0.38 | −0.17: 1.32 |
| (LSAS avoidance) | 11.06 | 0.17 | 0.37 | −0.57: 0.90 |
| DEP (HAM-D) | 4.98 | −0.01 | 0.19 | −0.38: 0.37 |
| 12-month follow-up: | ||||
| GAD (GADSS) | 4.80 | 0.58 | 0.41 | −0.21: 1.38 |
| SAD | ||||
| (LSAS fear) | 12.37 | 0.39 | 0.36 | −0.31: 1.10 |
| (LSAS avoidance) | 12.27 | 0.23 | 0.36 | −0.47: 0.93 |
| DEP (HAM-D) | 5.58 | 0.10 | 0.18 | −0.26: 0.45 |
Note. Hedge’s g includes correction for small sample size, n < 20.
Discussion
The ability to elegantly address symptoms of comorbid conditions is often cited as a potential advantage of transdiagnostic interventions. The primary purpose of the present study was to explore whether a leading transdiagnostic treatment, the UP, leads to improvements in cooccurring disorders. Indeed, results suggest that the UP is efficacious in reducing symptoms of comorbid psychopathology; specifically, participants in the UP condition evidenced significant decreases in mean number of clinically significant diagnoses from baseline to posttreatment, and baseline to 12-month follow-up. Similarly, significant changes on clinician-rated, disorderspecific measures were also observed at each time point. A secondary aim of the present study was to compare this change in comorbid disorder symptoms following treatment with the UP to treatment with leading and well established SDPs. Contrary to expectations, significant differences were not found when comparing the UP and SDP in the reduction of comorbid psychopathology; that is, both treatments led to decreases in mean number of diagnoses, and decline in symptoms of co-occurring conditions on disorder-specific measures.
Few studies have investigated the effect of treatment on comorbid disorders. However, in several studies, treatment for a principal anxiety disorder resulted in significant declines in the frequency of comorbid disorders from pretreatment to posttreatment (e.g., Allen et al., 2007; Craske et al., 2007). Davis et al. (2010) reported similar findings in a naturalistic sample taken from our clinical center; specifically, treatment for principal anxiety and depressive disorders led to decreases in the number of patients with comorbid disorders.s.
Consistent with these findings, the lack of significant differences observed by treatment condition in this study suggests that both the UP and SDPs are efficacious treatments for cooccurring emotional disorders. The lingering question is, why? One potential explanation for these findings lies in the similarities of the treatments; skills presented in both the UP and SDPs were similar and often overlapped (e.g., cognitive interventions, exposures), although these skills, and other aspects of treatment, are very specifically targeted in SDPs and require somewhat different application procedures. Nevertheless, the fact that participants were able to generalize these skills is quite encouraging from a clinical standpoint, and speaks to the broadbased and transdiagnostic utility of cognitive-behavioral treatment elements. Another possibility, consistent with a more mechanism-based perspective of psychopathology, is that both treatments resulted in changes to underlying, core processes common to the range of emotional disorders, such as neuroticism. Although SDPs did not directly target shared mechanisms, at least in the way that the UP was designed to do, many of the procedures were similar and it is possible that changes occurred at that level. Further investigation in this area is needed.
Current findings support the practical and cost-effective nature of incorporating transdiagnostic treatments into both clinical training programs and routine clinical practice. As outpatient psychotherapy continues to shift away from the standard 50-minute session (Olfson & Marcus, 2010), dissemination of effective science-based treatment is becoming even more critical in our field. Training clinicians to use one set of research supported modules for patients presenting with heterogeneous, co-occurring psychological disorders reduces the time and effort it takes to learn multiple SDPs, the cost of training, supervising, and implementing different manualized treatments for different diagnoses, and provides the potential for more efficient and more broad-based dissemination of effective treatment (McHugh & Barlow, 2010). Thus, transdiagnostic treatments offer a promising avenue for treating co-occurring emotional disorders to address the comorbid, complex presentations regularly seen in routine clinical practice.
Despite promising early findings, study limitations warrant mention. As published previously, participants reported generally high levels of education and lower depression than comparable participant samples. Additionally, the UP and three of the four SDPs included were developed at the data collection/treatment site, potentially limiting generalizability (Barlow et al., 2017). Specific to the current study’s focus on comorbid conditions, sample sizes were small after removing principal diagnoses, limiting between-group comparisons across time points in some instances. Specifically, sample sizes were small for comparisons on diagnosis-specific measures after principal diagnoses were removed. A power analysis in G*Power (Faul, Erdfelder, Lang, & Buchnear, 2007) indicated that a minimum of 52 patients (26 per group) would be necessary to explore changes on diagnosis-specific measures (e.g., using t-tests) to be adequately powered to find a large effect. Of note, the current study was adequately powered for the between-group analyses examining changes in number of diagnoses between conditions.
In sum, both treatments were effective in reducing comorbid symptoms. This study offers preliminary evidence for the UP’s efficacy in treating co-occurring emotional disorders. Current results require further study through replication and in different clinical settings. Future work is needed to more specifically understand how these outcomes are achieved (i.e., which underlying mechanisms might be involved) and whether there are differences in mechanisms across treatments.
Highlights.
The Unified Protocol for Transdiagnostic Treatment of Emotional Disorders (UP) reduces symptoms of comorbid psychological disorders
Compared to established treatments targeting single disorders, both the UP and single disorder protocols were efficacious in reducing symptoms of comorbid emotional disorders at posttreatment and 12-month follow-up
The UP is a practical and cost-effective transdiagnostic treatment for comorbid psychopathology commonly seen in the treatment of emotional disorders
Footnotes
Conflict of Interest
Please note the following financial disclosures/conflicts of interest: Dr. Barlow reported receiving royalties from Oxford University Press (which includes royalties for the treatment manuals included in this study), Guilford Publications Inc., Cengage Learning, and Pearson Publishing; receiving grants from the National Institute of Mental Health, the National Institute of Alcohol and Alcohol Abuse, and Colciencias (Government of Columbia Initiative for Science, Technology, and Health Innovation); serving as a consultant for and receiving honoraria from the Agency for Healthcare Research and Quality, the Foundation for Informed Medical Decision Making, the Department of Defense, the Renfrew Center, the Chinese University of Hong Kong, Universidad Catolica de Santa Maria (Arequipa, Peru), New Zealand Psychological Association, Hebrew University of Jerusalem, Mayo Clinic, and various American universities.
Drs. Farchione and Sauer-Zavala reported receiving royalties from Oxford University Press (for one of the treatment manuals included in this study). No other disclosures were reported.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Akbari M, Roshan R, Shabani A, Fata L, Shairi MR, Zarghami F, 2015. Transdiagnostic treatment of co-occurrence of anxiety and depressive disorders based on repetitive negative thinking: A case series. Iran. J. Psych 10, 200–211. [PMC free article] [PubMed] [Google Scholar]
- 2.Allen LB, White KS, Barlow DH, Shear MK, Gorman JM, Woods SW, 2010. Cognitive-behavior therapy (CBT) for panic disorder: Relationship of anxiety and depression comorbidity with treatment outcome. J. Psychopathol. Behav. Assess 32, 185–192. doi: 10.1007/s10862-009-9151-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Psychiatric Association., 2013. Diagnostic and Statistical Manual of MentalDisorders (DSM-5), fifth ed. American Psychiatric Associations Publishing, Washington, D.C. [Google Scholar]
- 4.Barlow DH, 2000. Unraveling the mysteries of anxiety and its disorders from the perspectiveof emotion theory. Am. Psychol 55, 1247–1263. doi: 10.1037//0003-066X.55.11.1247 [DOI] [PubMed] [Google Scholar]
- 5.Barlow DH, Allen LB, Choate ML, 2016. Toward a unified treatment for emotional disorders–Republished article. Behav. Ther 47, 838–853. doi: 10.1016/j.beth.2016.11.005 [DOI] [PubMed] [Google Scholar]
- 6.Barlow DH, Craske MG, 2007. Mastery of Your Anxiety and Panic: Workbook. Oxford; , New York. [Google Scholar]
- 7.Barlow DH, Ellard KK, Fairholme CP, Farchione TJ, Boisseau CL, Allen LB,Ehrenreich-May J, 2011a. Unified Protocol for Transdiagnostic Treatment of Emotional Disorders: Workbook, first ed. Oxford, New York. [Google Scholar]
- 8.Barlow DH, Farchione TJ, Bullis JR, Gallagher MW, Murray-Latin H, Sauer-Zavala S, … & Cassiello-Robbins C, 2017. The Unified Protocol for Transdiagnostic Treatment of Emotional Disorders compared with diagnosis-specific protocols for anxiety disorders: A randomized clinical trial. JAMA Psychiatry. 74, 875–884. doi: 10.1001/jamapsychiatry.2017.2164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barlow DH, Fairholme CP, Ellard KK, Boisseau CL, Allen LB, Ehrenreich-May J,2011b. Unified Protocol for Transdiagnostic Treatment of Emotional Disorders: Therapist Guide, first ed. Oxford, New York. [Google Scholar]
- 10.Barlow DH, Farchione TJ, Sauer-Zavala S, Latin HM, Ellard KK, Bullis JR, . .Cassiello-Robbins C, 2018a. Unified Protocol for Transdiagnostic Treatment of Emotional Disorders: Therapist Guide, second ed. Oxford, New York. [Google Scholar]
- 11.Barlow DH, Sauer-Zavala S, Farchione TJ, Murray-Latin H, Ellard KK, Bullis JR,… Cassiello-Robbins C, 2018b. Unified Protocol for Transdiagnostic Treatment of Emotional Disorders: Workbook, second ed. Oxford, New York. [Google Scholar]
- 12.Barlow DH, Sauer-Zavala S, Carl JR, Bullis JR, Ellard KK, 2014. The nature,diagnosis, and treatment of neuroticism: Back to the future. Clin. Psychol. Sci 2, 344–365. doi: 10.1177/2167702613505532 [DOI] [Google Scholar]
- 13.Brown TA, Barlow DH, 2014. Anxiety and Related Disorders Interview Schedule forDSM-5 (ADIS-5L): Lifetime Version-Client Interview Schedule. Oxford, New York. [Google Scholar]
- 14.Brown TA, Barlow DH, 2009. A proposal for a dimensional classification system basedon the shared features of the DSM-IV anxiety and mood disorders: Implications for assessment and treatment. Psychol. Assess. 21, 256–271. doi: 10.1037/a0016608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brown TA, Campbell LA, Lehman CL, Grisham JR, Mancill RB, 2001. Currentand lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. J. Abnorm. Psychol 110, 585–599. doi: 10.1037//0021-843x.110.4.585 [DOI] [PubMed] [Google Scholar]
- 16.Bullis JR, Fortune MR, Farchione TJ, Barlow DH, 2014. A preliminary investigationof the long-term outcome of the Unified Protocol for Transdiagnostic Treatment of Emotional Disorders. Compr. Psychiatry 55, 1920–1927. doi: 10.1016/j.comppsych.2014.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Craske MG, Barlow DH, 2006. Mastery of Your Anxiety and Worry: Workbook.Oxford, New York. [Google Scholar]
- 18.Craske MG, Barlow DH, 2007. Mastery of Your Anxiety and Panic: Therapist Guide. Oxford, New York. [Google Scholar]
- 19.Craske MG, Farchione TJ, Allen LB, Barrios V, Stoyanova M, Rose R, 2007. Cognitive behavioral therapy for panic disorder and comorbidity: More of the same or less of more? Behav. Res. Ther 45, 1095–1109. doi: 10.1016/j.brat.2006.09.006 [DOI] [PubMed] [Google Scholar]
- 20.Davis L, Barlow DH, Smith L, 2010. Comorbidity and the treatment of principal anxietydisorders in a naturalistic sample. Behav. Ther 41, 296–305. doi: 10.1016/j.beth.2009.09.002 [DOI] [PubMed] [Google Scholar]
- 21.Di Nardo PA, Brown TA, Barlow DH, 1994. Anxiety Disorders Interview Schedule for DSM-IV: Lifetime Version (ADIS-IV-L). Oxford, UK. [Google Scholar]
- 22.Ellard KK, Fairholme CP, Boisseau CL, Farchione TJ, Barlow DH, 2010. UnifiedProtocol for the Transdiagnostic Treatment of Emotional Disorders: Protocol development and initial outcome data. Cogn. Behav. Pract 17, 88–101. doi: 10.1016/j.cbpra.2009.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Thompson-Hollands J, Carl JR, … Barlow DH, 2012. Unified Protocol for Transdiagnostic Treatment of Emotional Disorders: A randomized controlled trial. Behav. Ther 43, 666–678. doi: 10.1016/j.beth.2012.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Faul F, Erdfelder E, Lang A-G, Buchner A, 2007. G*Power 3: A flexible statisticalpower analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 39, 175–191. [DOI] [PubMed] [Google Scholar]
- 25.Foa EB, Yadin E, Lichner TK, 2012. Exposure and Response (Ritual) Prevention forObsessive-Compulsive Disorder: Therapist Guide. Oxford, New York. [Google Scholar]
- 26.Fresco DM, Coles ME, Heimberg RG, Liebowitz MR, Hami S, Stein MB, Goetz D, 2001. The Liebowitz Social Anxiety Scale: A comparison of the psychometric properties of self-report and clinician-administered formats. Psychol. Med 31, 1025–1035. doi: 10.1017/S0033291701004056 [DOI] [PubMed] [Google Scholar]
- 27.Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado P, Heninger GR,Charney DS, 1989. The Yale-Brown Obsessive Compulsive Scale II. Validity. Arch. Gen. Psychiatry 46, 1012–1016. doi: 10.1001/archpsyc.1989.01810110054008 [DOI] [PubMed] [Google Scholar]
- 28.Griffith JW, Zinbarg RE, Craske MG, Mineka S, Rose RD, Waters AM, Sutton JM, 2010. Neuroticism as a common dimension in the internalizing disorders. Psychol. Med 40, 1125–1136. doi: 10.1017/s0033291709991449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hamilton M, 1960. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 23, 56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Heimberg RG, Horner KJ, Juster HR, Safren SA, Brown EJ, Schneier FR,Liebowitz MR, 1999. Psychometric properties of the Liebowitz Social Anxiety Scale. Psychol. Med 29, 199–212. doi: 10.1016/j.janxdis.2011.03.009 [DOI] [PubMed] [Google Scholar]
- 31.Hope DA, Heimberg RG, Juster HR, Turk CL, 2000. Managing Social Anxiety: ACognitive-Behavioral Therapy Approach. The Psychological Corporation, New York. [Google Scholar]
- 32.Hope DA, Heimberg RG, Turk CL, 2006. Managing Social Anxiety: A Cognitive-Behavioral Therapy Approach Therapist Guide. Oxford, UK. [Google Scholar]
- 33.King LA, King DK, McArdle J, Saxe G, Doran-Lamarca S, Orazem R, 2006. Latentdifference score approach to longitudinal trauma research. J. Trauma. Stress 19, 771–785. doi: 10.1002/jts.20188 [DOI] [PubMed] [Google Scholar]
- 34.Liebowitz MR, 1987. Social phobia. Mod. Probl. Pharmacopsychiatry. 22, 141–173. doi: 10.1159/000414022 [DOI] [PubMed] [Google Scholar]
- 35.McHugh RK, Barlow DH, 2010. The dissemination and implementation of evidencebased psychological treatments. A review of current efforts. Am. Psychol 65, 73–84. doi: 10.1037/a0018121 [DOI] [PubMed] [Google Scholar]
- 36.Milosevic I, Chudzik SM, Boyd S, McCabe RE, 2017. Evaluation of an integratedgroup cognitive-behavioral treatment for comorbid mood, anxiety, and substance use disorders: A pilot study. J. Anxiety Disord 46, 85–100. doi: 10.1016/j.janxdis.2016.08.002 [DOI] [PubMed] [Google Scholar]
- 37.Olfson M, Marcus SC, 2010. National trends in outpatient psychotherapy. Am. J.Psychiatry 167, 1456–1463. doi: 10.1176/appi.ajp.2010.10040570 [DOI] [PubMed] [Google Scholar]
- 38.Palermo TM, Bromberg MH, Beals-Erickson S, Law EF, Durkin L, Noel M, Chen M, 2016. Development and initial feasibility testing of brief cognitive-behavioral therapy for insomnia in adolescents with comorbid conditions. Clin. Pract. Pediatr. Psychol 4, 214–226. doi: 10.1037/cpp0000140 [DOI] [Google Scholar]
- 39.Rosellini AJ, Boettcher H, Brown TA, Barlow DH, 2015. A transdiagnostictemperament-phenotype profile approach to emotional disorder classification: An update. Psychopathol. Rev 2, 110–128. doi: 10.5127/pr.036014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sauer-Zavala S, Barlow DH, 2014. The case for borderline personality disorder as an emotional disorder: Implications for treatment. Clin. Psychol. Sci. Pract 21, 118–138. doi: 10.1111/cpsp.12063 [DOI] [Google Scholar]
- 41.Sauer-Zavala S, Wilner JG, Barlow DH, 2017. Addressing neuroticism in psychological treatment. Personal. Disord 8, 191–198. doi: 10.1037/per0000224 [DOI] [PubMed] [Google Scholar]
- 42.Shear K, Belnap BH, Mazumdar S, Houck P, Rollman BL, 2006. Generalized Anxiety Disorder Severity Scale (GADSS): A preliminary validation study. Depress. Anxiety 23, 77–82. doi: 10.1002/da.20149 [DOI] [PubMed] [Google Scholar]
- 43.Shear MK, Brown TA, Barlow DH, Money R, Sholomskas DE, Woods SW, … Papp LA, 1997. Multicenter collaborative Panic Disorder Severity Scale. Am. J. Psychiatry 154, 1571–1575. doi: 10.1176/ajp.154.11.1571 [DOI] [PubMed] [Google Scholar]
- 44.Shear MK, Rucci P, Williams J, Frank E, Grochocinski V, Vander Bilt J, … Wang T, 2001a. Reliability and validity of the Panic Disorder Severity Scale: Replication and extension. J. Psychiat. Res 35, 293–296. doi: 10.1016/S0022-3956(01)00028-0 [DOI] [PubMed] [Google Scholar]
- 45.Shear MK, Vander Bilt J, Rucci P, Endicott J, Lydiard B, Otto MW, … Frank DM, 2001b. Reliability and validity of a structured interview guide for the Hamilton Anxiety Rating Scale (SIGH‐A). Depress. Anxiety 13, 166–178. doi: 10.1002/da.1033.abs [DOI] [PubMed] [Google Scholar]
- 46.Stice E, Rohde P, Butryn M, Menke KS, Marti CN, 2015. Randomized controlled pilot trial of a novel dissonance-based group treatment for eating disorders. Behav. Res. Ther 65, 67–75. doi: 10.1016/j.brat.2014.12.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Storch EA, Rasmussen SA, Price LH, Larson MJ, Murphy TK, Goodman WK, 2010. Development and psychometric evaluation of the Yale–Brown Obsessive-Compulsive Scale—Second Edition. Psychol. Assess 22, 223–232. doi: 10.1037/a0018492 [DOI] [PubMed] [Google Scholar]
- 48.Titov N, Dear BF, Staples LG, Terides MD, Karin E, Sheehan J,...McEvoy PM, 2015. Disorder-specific versus transdiagnostic and clinician-guided versus self-guided treatment for major depressive disorder and comorbid anxiety disorders: A randomized controlled trial. J. Anxiety Disord 35, 88–102. doi: 10.1016/j.janxdis.2015.08.002 [DOI] [PubMed] [Google Scholar]
- 49.Wilamowska ZA, Thompson-Hollands J, Fairholme CP, Ellard KK, Farchione TJ, Barlow DH, 2010. Conceptual background, development, and preliminary data from the Unified Protocol for Transdiagnostic Treatment of Emotional Disorders. Depress. Anxiety 27, 882–890. doi: 10.1002/da.20735 [DOI] [PubMed] [Google Scholar]
- 50.Williams JB, 1988. A structured interview guide for the Hamilton Depression Rating Scale. Arch. Gen. Psychiatry 45, 742–747. doi: 10.1001/archpsyc.1988.01800320058007 [DOI] [PubMed] [Google Scholar]
- 51.Wu MS, McGuire JF, Horng B, Storch EA, 2016. Further psychometric properties of the Yale–Brown Obsessive Compulsive Scale—Second Edition. Compr. Psychiatry 66, 96–103. doi: 10.1016/j.comppsych.2016.01.007 [DOI] [PubMed] [Google Scholar]
- 52.Wuyek LA, Antony MM, McCabe RE, 2011. Psychometric properties of the Panic Disorder Severity Scale: Clinician‐administered and self‐report versions. Clin. Psychol. Psychother 18, 234–243. doi: 10.1002/ccp.703 [DOI] [PubMed] [Google Scholar]
- 53.Yadin E, Foa EB, Lichner TK, 2012. Treating Your OCD with Exposure and Response (Ritual) Prevention: Workbook. Oxford, New York. [Google Scholar]
- 54.Zinbarg RE, Craske MG, Barlow DH, 2006. Mastery of Your Anxiety and Worry: Therapist Guide. Oxford, New York. [Google Scholar]