Abstract
BACKGROUND:
All-cause readmission rates in patients undergoing ileostomy formation are as high as 20–30%. Dehydration is a leading cause. No predictive model for dehydration readmission has been described.
OBJECTIVE:
To develop and validate the Dehydration Readmission after Ileostomy Prediction (DRIP) scoring system to predict risk of readmission for dehydration after ileostomy formation.
DESIGN:
Patients who underwent ileostomy formation were identified using the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) dataset (2012–2015). Predictors for dehydration were identified using multivariable logistic regression analysis and translated into point scoring system based on corresponding β coefficients using 2012–2014 data (derivation). Model discrimination was assessed with receiver operating characteristic curves using 2015 data (validation).
SETTINGS:
This study used the ACS-NSQIP.
PATIENTS:
A total of 8064 patients (derivation) and 3467 patients (validation) were included from the ACS-NSQIP.
MAIN OUTCOME MEASURES:
Dehydration readmission within 30 days of operation
RESULTS:
A total of 8064 patients were in the derivation sample, with 2.9% (20.1% overall) readmitted for dehydration. Twenty-five variables were queried, and seven predictors were identified with points assigned: ASA Class III (4 points), female gender (5 points), ileal pouch anal anastomosis (4 points), age ≥65 years (5 points), shortened length of stay (5 points), ASA Class I-II with inflammatory bowel disease (7 points), and hypertension (9 points). A 39-point, 5-tier risk category scoring system was developed. The model performed well in derivation (AUC=0.71) and validation (AUC=0.74) samples and passed the Hosmer-Lemeshow goodness-of-fit test.
LIMITATIONS:
Limitations of this study pertained to those of the ACS-NSQIP including: lack of generalizability, lack of ileostomy-specific variables, and inability to capture multiple readmission ICD-9/10 codes.
CONCLUSIONS:
The DRIP score is a validated scoring system that identifies patients at risk for dehydration readmission after ileostomy formation. It is a specific approach to optimize patient factors, implement interventions, and prevent readmissions. See Video Abstract at http://links.lww.com/DCR/Axxx.
Keywords: Dehydration, Hospital readmission, Ileostomy, Risk scoring system
Readmission within 30-days of hospital discharge has received widespread attention as a potential healthcare quality indicator. In 2013, the Center for Medicare and Medicaid Services established the Hospital Readmission Reduction Program (HRRP), a cost-containment strategy that financially penalizes hospitals with higher than expected 30-day readmission. Though conditions targeted by the HRRP have been predominately medical, it is anticipated that readmission after surgical procedures will be used to structure financial incentives and hospital compensation in the near future.1
All-cause readmission rates after colorectal surgery are as high as 30%.2,3 Previous studies have identified ileostomy creation as one of the driving risk factors.3–5 According to the Agency for Healthcare Research and Quality (AHRQ), ileostomies had a nationwide, 30-day hospital readmission rate of 30% in 2013 and contributed to $94 million in healthcare expenditures.6 Dehydration is the most common cause of 30-day readmission following ileostomy creation, accounting for approximately 20–40% of ileostomy-related readmissions and having reported readmission rates of 7–20% alone.7–10
Current literature examining readmission after ileostomy creation is scarce, with most existing reports utilizing single-institution databases.7–10 To our knowledge, no studies to date have attempted to both risk-stratify patients and generate predictive models or scoring systems to assess the risk of readmission due to dehydration. Using the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) 2012–2015 dataset, we developed the Dehydration Readmission after Ileostomy Prediction (DRIP) scoring system—a novel, validated scoring system of patient and clinical factors that could be used to identify patients at risk for being readmitted for dehydration after ileostomy creation. This proposed scoring system may enable earlier identification of high-risk patients and implementation of preventative measures, thereby potentially reducing unplanned readmissions after colorectal surgery.
METHODS
Data Source
A retrospective analysis was conducted using the 2012–2015 ACS-NSQIP Participant User File (PUF) database.11,12 This national database contains risk-adjusted data on patients undergoing surgery at participant hospitals. Certified Surgical Clinical Reviewers prospectively collect data on up to 273 perioperative variables.13 This study was reviewed and approved by the Institutional Review Board of the Johns Hopkins University School of Medicine.
Study Population
Patients undergoing proctectomy, colectomy, enterectomy with ileostomy formation, or ileostomy formation procedures alone were included (Current Procedural Terminology [CPT] codes 44211, 44212, 45113, 45119, 44155, 44157, 44158, 44125, 44187, and 44310). CPT codes 44150 and 44210 were not considered, as these codes do not specify whether ileostomy or ileoproctostomy was performed. Other procedures performed in addition to ileostomy formation, such as ileal conduit (50688, 50690, 50820, 50830, 51590, 51595, and 51596), colostomy (44141, 44143, 44206, 44340, 45110, and 45126), and ileostomy takedown (44620, and 44320) were also excluded. Patients were also excluded if they met any of the following exclusion criteria: a) missing information for readmission and admission type; b) were discharged to another acute care facility; c) died prior to discharge; d) were not discharged before the 30-day post-operative follow-up; and e) their operation was performed in an outpatient setting or if they had a length of hospital stay (LOS) of 0 days. Because NSQIP captures 30-day post-operative readmission, which may undercount the true 30-day post-discharge readmission, patients with LOS >15 days were excluded to mitigate the possibility of bias due to immortal person-time (patients are “immortal” for 30-day readmission until they are discharged from the hospital, so patients with long LOS would have artificially low readmission risk).14
Baseline characteristics of patients
Demographic and clinical characteristics were compared between patients with readmissions for dehydration and patients with no readmissions. Demographic characteristics included age (<40, 40–49, 50–64, and ≥65 years), sex, and race (white, black, other [American Indian/Alaskan Native, Native Hawaiian/Pacific Islander, Asian], unknown, not reported)). Clinical characteristics included the American Society of Anesthesiologists (ASA) Physical Status Classification (“I-II”, no or mild disturbance; “III”, severe disturbance; and “IV-V”, life-threatening and moribund), body mass index (BMI; <18.5, underweight; 18.5–24.9, normal; 25–29.9, overweight; and ≥30 kg/m2, obese), partial/full dependence, and preoperative comorbidities: diabetes mellitus (oral agents or insulin), current smoker, dyspnea, disseminated cancer, COPD, hypertension requiring medication, chronic steroid use, weight loss (>10% decrease in body weight in the past six months), bleeding disorder, and blood transfusion. Other variables evaluated include operative approach (laparoscopic or open), procedure type (proctectomy±colectomy, colectomy, enterectomy, or ileostomy), prolonged or shortened length of hospital stay (LOS) defined using the 75th and 25th percentiles, respectively, based on LOS and procedure type. Hospital LOS was calculated as days from procedure to discharge. Prolonged operative time was defined as values >75th percentile by procedure type. International Classification of Diseases, 9th edition, (ICD-9) codes were used to define rectal cancer (154, 154.0, 154.1, 154.2, and 154.3), colon cancer (153, 153.0–153.7, 153.9), inflammatory bowel disease (IBD, 555, 555.0–555.2, and 555.9), and diverticulitis (562.11 and 562.13).
Outcomes
The primary outcome was unplanned readmission from dehydration, defined by NSQIP as “return to the same or another hospital for any reason, within 30 days of principle surgical procedure”. Dehydration ICD-9 and ICD-10 codes of 276.51 and E86.0, respectively, were used to determine readmission for dehydration.
Statistical analysis
Patients were classified into two groups based on the occurrence of readmission from dehydration. Patients readmitted for reasons other than dehydration were omitted from analysis. Factors were assessed for association with primary outcomes using Pearson’s Chi-square test. Fisher’s exact test was used when appropriate. The entire dataset was partitioned into years 2012–2014 and year 2015 samples—the former (derivation cohort) to derive a prediction model and generate a risk score, and the latter (validation cohort) to validate the proposed scoring system. Multivariable logistic regression analysis was used to identify predictors of readmission. Overall, twenty-five factors were considered in the development of the prediction model. Statistically significant factors associated with readmission from dehydration in the univariate analysis, as well as clinically relevant factors regardless of statistical significance, were included in the model. Because prior reports have demonstrated IPAA as a significant predictor for post-ileostomy formation readmission, we included IPAA as a potential predictor a priori.9 Shortened and prolonged LOS were also included a priori into the prediction model due to reported literature on the association between LOS and readmission.15–18 All variables were examined for interaction. Discrimination of the prediction model was assessed using the area under the receiver operating characteristic curve (ROC). Goodness-of-fit was assessed using the Hosmer-Lemeshow test. Validity of the prediction model and scoring tool was tested on the 2015 sample of the study population. Furthermore, the predicted risk for readmission for dehydration was computed for each risk category.
A simple scoring technique was applied to allow for easy use in a clinical setting. Coefficients (β) for all significant risk factors were multiplied by 10 and rounded to the nearest integer to create a score for each risk factor, a method previously described.19 The final risk score ranging from 0 (no risk) to 39 (very high risk) was obtained by summing all the points from each component. The final risk score was then stratified into five risk categories: very low (0–2 points), low (3–8 points), medium (9–14 points), high (15–23 points), and very high (24–39 points). A five-tier risk category system was generated as an attempt to create normally distributed risk scores and to allow for higher predictability. All statistical analysis was performed using Stata, version 14.0 (StataCorp, College Station, Texas, USA).
RESULTS
Study population for derivation cohort
A total of 11,531 patients were identified for inclusion. Of these, 8,064 patients who underwent ileostomy formation between January 1, 2012 and December 31, 2014 comprised the derivation subset, with 237 (2.9%) readmitted for known dehydration. The overall readmission rate was 20.1%. The median age was 55 years (IQR 43–65 years); a slight majority were male (n=4,418 [54.8%]), and most were white (n=6,601 [81.9%]). Approximately one-third were diagnosed with rectal cancer (n=2690 [33.2%]) as the primary indication for surgery. Proctectomy with or without colectomy was the most frequently performed procedure (n=6227 [77.2%]), and more than half of all procedures were performed using an open approach (n=5143 [63.8%]).
Demographic, clinical, and operative characteristics between patients who were readmitted for dehydration were compared to those who were not readmitted. (Table 1). Readmitted patients demonstrated statistically significantly higher rates of females, ASA class III, diabetes, dyspnea, colon cancer, IBD, hypertension, and IPAA.
TABLE 1.
Demographic, Clinical, and Operative Characteristics of Patients Undergoing Ileostomy Formation
| Characteristic, n (%)> | No readmission 7827 (97.06) |
Readmission for dehydration 237 (2.94) |
p |
|---|---|---|---|
| Age group, years | 0.48 | ||
| <40 | 1603 (97.48) | 41 (2.49) | |
| 40–49 | 1229 (97.08) | 37 (2.92) | |
| 50–64 | 2890 (97.11) | 86 (2.89) | |
| ≥65 | 2105 (96.65) | 73 (3.35) | |
| Female | 3524 (96.65) | 122 (3.35) | 0.05 |
| Race | 0.40 | ||
| White | 6405 (97.03) | 196 (2.97) | |
| Black | 482 (96.40) | 18 (3.60) | |
| Other1/Unknown | 940 (97.61) | 23 (2.39) | |
| ASA classification | 0.01 | ||
| I-II | 3985 (97.43) | 105 (2.57) | |
| III | 3548 (96.52) | 128 (3.48) | |
| IV-V | 285 (98.62) | 4 (1.38) | |
| BMI group, kg/m2 | 0.10 | ||
| Underweight (<18.5) | 293 (97.67) | 7 (2.33) | |
| Normal (18.5–24.9) | 2617 (97.32) | 72 (2.68) | 0.10 |
| Overweight (25–29.9) | 2201 (96.32) | 84 (3.68) | |
| Obese (≥30) | 2201 (96.32) | 84 (3.68) | |
| Partially/fully dependent | 105 (99.06) | 1 (0.94) | 0.38 |
| Diabetes | 796 (95.46) | 38 (4.56) | <0.01 |
| Current smoker | 1297 (97.08) | 39 (2.92) | 0.96 |
| Dyspnea | 325 (95.03) | 17 (4.97) | 0.02 |
| Disseminated cancer | 554 (97.19) | 16 (2.81) | 0.85 |
| Indication | <0.01 | ||
| Rectal cancer | 2619 (97.72) | 61 (2.28) | |
| Colon cancer | 470 (96.91) | 15 (3.09) | |
| IBD | 2177 (95.99) | 91 (4.01) | |
| IBD | 2177 (95.99) | 91 (4.01) | |
| Diverticulitis | 509 (98.26) | 9 (1.74) | |
| Other | 2052 (97.11) | 61 (2.89) | |
| History of COPD | 211 (96.79) | 7 (3.21) | 0.80 |
| Hypertension | 2600 (95.91) | 111 (4.09) | <0.01 |
| Steroid use | 1392 (96.73) | 47 (3.27) | 0.42 |
| Weight loss | 473 (97.33) | 13 (2.67) | 0.72 |
| Bleeding disorder | 255 (98.08) | 5 (1.92) | 0.32 |
| Blood transfusion | 127 (89.22) | 1 (10.78) | 0.19 |
| Emergency case | 518 (98.48) | 8 (1.52) | 0.05 |
| Transfer (not from home) | 319 (98.46) | 5 (1.54) | 0.13 |
| Operative approach | 0.57 | ||
| Open | 4996 (97.14) | 147 (2.86) | |
| Lap | 2831 (96.92) | 90 (3.08) | |
| Procedure type | 0.19 | ||
| Proctectomy±Colectomy | 6034 (96.90) | 193 (3.10) | |
| Colectomy | 794 (96.95) | 25 (3.05) | |
| Enterectomy | 306 (98.39) | 5 (1.61) | |
| Ileostomy | 693 (98.02) | 14 (1.98) | |
| IPAA | 1460 (95.80) | 64 (4.20) | <0.01 |
| Prolonged length of stay2 | 2124 (96.63) | 74 (3.37) | 0.16 |
| Shortened length of stay2 | 2306 (97.22) | 66 (2.78) | 0.59 |
| Prolonged operative time3 | 2124 (96.63) | 74 (3.37) | 0.16 |
Abbreviations: ASA, American Society of Anesthesiology; BMI, Body Mass Index; COPD, Chronic Obstructive Pulmonary Disease; IBD, Inflammatory Bowel Disease; LOS, Length of Stay; SD, Standard Deviation; IPAA, Ileal Pouch Anal Anastomosis.
ASA: I-II (No/Mild Disturb), III (Severe Disturb), IV-V (Life Threat/Moribund)
Asian, Native Hawaiian/Pacific Islander, or American Indian/Alaska Native.
Defined as length of stay greater than or equal to the 75th percentile for prolonged length of stay and less than or equal to the 25th percentile for shortened length of stay.
Defined as operative time greater than or equal to the 75th percentile.
Missing data: ASA, n=9; Functional status, n=16.
Predictors of readmission for dehydration and scoring system
The final model identified seven predictors (including one interaction term included due to its statistical significance) and passed the goodness-of-fit test (p=0.66) (Table 2). Hypertension was most strongly associated with dehydration readmission (OR 2.49, 95% CI 1.23–5.03, p<0.001), followed by ASA I-II with IBD (OR 2.06, 95% CI 1.15–3.68, p=0.015), age ≥65 (OR 1.68, 95% CI 1.03–2.74, p=0.037), female gender (OR 1.59, 95% CI 1.16–2.19, p=0.004), shortened LOS (OR 1.59, 95% CI 1.01–2.52, p=0.042), ASA III (OR 1.51, 95% CI 1.04–2.21, p=0.032), and IPAA (OR 1.51, 95% CI 1.07–2.1, p=0.019). A simple point scoring system was created with points assignment as follows: 9 points for hypertension, 7 points for ASA class I-II with IBD diagnoses, 5 points each for female gender, age ≥65, and shortened LOS; and 4 points each for ASA class III and IPAA. A 39 point, 5-tier risk category scoring system was developed: lowest risk category (0–2 points) with 0.73% risk rate, low risk category (3–8 points) with 1.71%, medium risk category (9–14 points) with 2.60%, high risk category (15–23 points) with 4.62%, and highest risk (24–39 points) with 5.45% (Table 3). Overall, the predicted risk was similar between derivation and validation samples; rates were slightly higher in the derivation sample for the highest risk category (7.01% derivation and 5.53% validation samples).
TABLE 2.
Predictors for Readmission for Dehydration after Ileostomy Formation
| Factors | OR (95% CI) | β (95% CI) | p | Score |
|---|---|---|---|---|
| Hypertension | 2.49 (1.23−5.03) | 0.91 (0.20−1.62) | 0.01 | +9 |
| ASA I-II and IBD | 2.06 (1.15−3.68) | 0.72 (0.14−1.30) | 0.02 | +7 |
| Age | ||||
| <65 | Reference | |||
| ≥65 | 1.68 (1.03−2.74) | 0.52 (0.03−1.00) | 0.04 | +5 |
| Gender | ||||
| Male | Reference | |||
| Female | 1.59 (1.16−2.19) | 0.46 (0.15−0.78) | <0.01 | +5 |
| Shortened LOS1 | 1.59 (1.01−2.52) | 0.48 (0.02−0.94) | 0.04 | +5 |
| ASA category | ||||
| ASA I-II | Reference | |||
| ASA III | 1.51 (1.04−2.21) | 0.41 (0.03−0.79) | 0.03 | +4 |
| IPAA | 1.51 (1.07−2.13) | 0.41 (0.07−0.76) | 0.01 | +4 |
| TOTAL | - | - | - | 39 |
Abbreviations: OR, Odds Ratio; CI, Confidence Interval; ASA, American Society of Anesthesiology; IBD, Inflammatory Bowel Disease; LOS, Length of Stay; IPAA, Ileal Pouch Anal Anastomosis.
The above model was adjusted for most of the factors from Table 1 (statistical significant or clinically relevant) and few interaction terms.
1LOS < 4 days for proctectomy+colectomy, LOS<5 days for colectomy or enterectomy, LOS<3 days for ileostomy.
TABLE 3.
Risk Categories for Readmission for Dehydration after Ileostomy Formation
| Predicted risk | |||||||
|---|---|---|---|---|---|---|---|
| Derivation sample |
Validation sample | Derivation sample |
Validation sample | ||||
| Risk category | Points assignment | Risk (%) | Risk (%) | Risk % (95% CI) | Risk % (95% CI) | ||
| Lowest risk | 0–2 points | 4/545 (0.73) | 1/217 (0.46) | 1.12 (0.69–1.54) | 0.76 (0.03–1.27) | ||
| Low risk | 3–8 points | 29/1692 (1.71) | 10/727 (1.38) | 1.93 (1.50–2.36) | 1.35 (0.08–1.91) | ||
| Medium risk | 9–14 points | 86/3313 (2.60) | 33/1435 (2.30) | 2.67 (2.28–3.04) | 2.20 (1.65–2.74) | ||
| High risk | 15–23 points | 106/2294 (4.62) | 34/990 (3.43) | 4.20 (3.54–4.86) | 4.11 (3.10–5.13) | ||
| Highest risk | 24–39 points | 12/220 (5.45) | 7/98 (7.14) | 7.01 (4.92–9.11) | 5.53 (2.63–8.43) | ||
Study population for validation cohort
A total of 3,467 patients undergoing ileostomy formation between January 1, 2015 and December 31, 2015 comprised the validation subset, with 2.5% readmitted for dehydration. Demographic, clinical, and operative characteristics were similar to those in the derivation sample. Median age of patients was 55 years. 54.1% were male, and 78.9% were Caucasian. 37.6% of patients were diagnosed with rectal cancer. Proctectomy±colectomy was the most frequently performed procedure (76.5%), and more than half of all procedures were open (56.4%).
Validation
ROC analysis in the derivation sample demonstrated good predictive abilities of the model with area under curve (AUC) of 0.71 (95% CI, 0.68–0.74). This predictive ability was maintained in the validation sample (AUC of 0.74, 95% CI, 0.69–0.79) (Figure 1). The model passed the Hosmer-Lemeshow goodness-of-fit test (p=0.35), and the AUC for the scoring system provided acceptable and consistent results for both derivation and validation samples (AUC of 0.62 for both, with 95% CI 0.59–0.65 for derivation sample, and 0.56–0.67 for validation sample). Similar results were obtained for the total risk score (median of 12 [IQR 7–17] in the derivation sample vs. median of 12 [IQR 7–18] in the validation sample) and distribution of risk categories, with an even greater rate for the highest risk category (7.14% from validation sample vs. 5.45% from derivation sample). A proposed pre-discharge quality improvement form was created for use in the clinical setting (Figure 2).
FIGURE 1a.
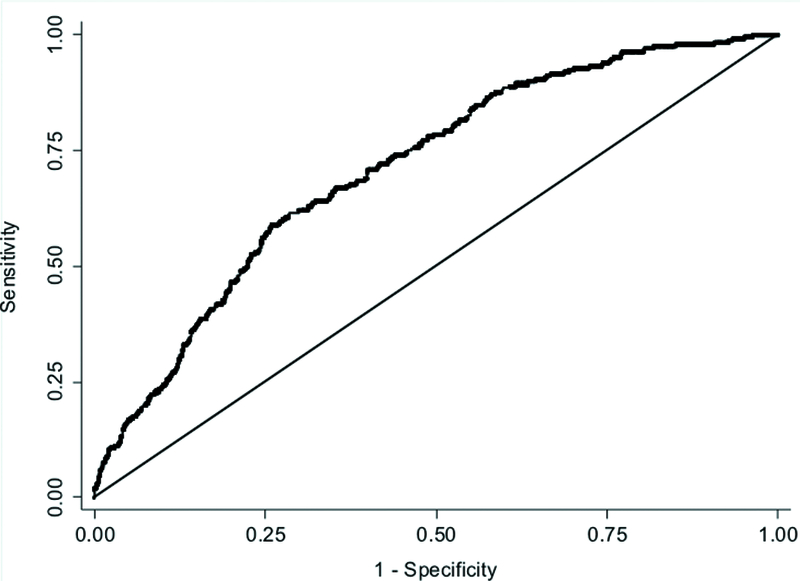
Receiver operating characteristic (ROC) curve for the prediction model (0.71) (derivation sample).
FIGURE 2.
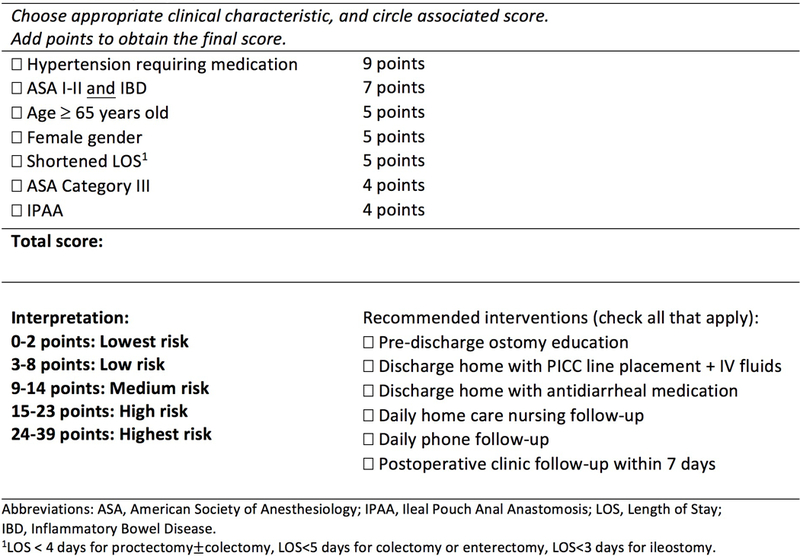
Quality Improvement Form.
DISCUSSION
Dehydration is one of the most common reasons for readmission for patients who undergo ileostomy formation. The DRIP score is the first known risk-stratification tool to predict the risk of readmission due to dehydration in patients undergoing ileostomy formation. Six independent variables and one interaction term were predictive of readmission, from which we derived a 39-point scoring system. Readmission risk was stratified into five categories, demonstrating the ability of this scoring system to distinguish differences in patient risk profiles. Utilization of this validated scoring system may provide the impetus for preventive interventions for identified high-risk patients and could potentially reduce readmissions after colorectal surgery.
The data from which our predictive scoring system was derived is comparable to that reported in prior studies. Our overall 30-day readmission rate after ileostomy creation was 20.1%, consistent with prior studies with reported rates of 18–26%.20–22 Similar to other studies, our study showed that dehydration was the most common reason for readmission, accounting for 14.4% of readmissions after ileostomy formation.
Independent predictors included in the DRIP score are consistent with those reported in the literature. Several studies have identified IPAA as an independent predictor of readmission for dehydration.9,23 IPAA may be a risk factor for dehydration readmission due to the creation of a more proximal ileostomy, which has higher susceptibility to fluid losses than a more distal ileostomy. Older age has also been demonstrated as a factor for high ileostomy output, dehydration, and readmission after ileostomy formation, as it may be associated with diminished fluid absorption capability in the small bowel and decreased tolerance for fluid shifts that occur following ileostomy creation.24,25 Though hypertension was a somewhat surprising factor, a single-institution study has reported similar findings.24 Hypertension may serve as an indirect proxy for diuretic use. The NSQIP definition of hypertension comprises of patients on anti-hypertensive medications. As such, patients diagnosed with hypertension may be treated with diuretics that may contribute to additional fluid losses and raise the dehydration risk. This would be consistent with studies demonstrating postoperative diuretic use as a risk factor for dehydration readmission in ileostomy patients; in fact, several studies have demonstrated perioperative diuretic use as being the sole risk factor for readmission for dehydration.7,9
Our findings also suggest that a LOS <25th percentile by procedure type is marginally significantly associated with increased odds of readmission, a conclusion supported by one recent study.25 The relationship between hospital LOS and readmission has been subject to debate. Nationwide, overall readmission rates for colorectal surgery have increased, while LOS has decreased, an observation that may potentially be attributed to the implementation of Enhanced Recovery After Surgery (ERAS) programs.16 Some studies have supported findings that longer LOS instead is associated with increased odds of readmission, owing to a more complicated postoperative hospital course.3,15,22 However, broadly comprehensive studies of mixed patient populations have estimated a tradeoff between LOS and readmission rate at the hospital level (with a 6% increase in readmission risk per each day reduction in mean LOS).26 More specifically, LOS <4 days has also been associated with increased risk of readmission among some colorectal surgery patients.27 We suspect that physiological alterations (ex. fluid balance shifts) patients experience following ileostomy formation may not be assessed adequately within a short time frame, and therefore shorter LOS may be associated with greater likelihood of readmission. Implementation of the DRIP score into ERAS programs could therefore offer potential benefit in determining which patients may be appropriate candidates for ERAS pathways and when patients may be appropriately discharged from the hospital.
Previous studies have assessed the effectiveness of postoperative ileostomy pathways, which combine multidisciplinary care before and after discharge (ex. ileostomy education, use of stoma output diaries, and nursing visits), and medical interventions (ex. restriction of oral hypotonic fluids, use of isotonic solutions, antidiarrheal/antisecretory medications, caloric nutritional support, and IV fluid therapy via central catheter inserted prior to discharge).20,28 Our study is the first to operationalize its findings with a scoring system to identify patients at higher risk for readmission. The DRIP score allows for patient risk stratification at the time of hospital discharge to enable more targeted interventions and improved hospital resource allocation. For example, patients identified as being at highest risk for dehydration readmission may receive multiple interventions such as outpatient IV fluids, prescription for antidiarrheal medications, daily home care nursing visits, more extensive ostomy education, and earlier postoperative clinic follow-up within a week of discharge. In contrast, patients at lowest risk for dehydration readmission may simply receive basic ileostomy care education. The AHRQ reports a mean cost of $15,434 per readmission for ileostomy procedures. We anticipate that the DRIP score has the potential to deliver higher value care.6 Further studies, however, are needed to assess which specific intervention(s) are appropriate at each risk stratification level and whether such interventions are effective in reducing dehydration readmissions and healthcare costs. Cost analyses comparing the costs needed to provide additional care/services for patients in the highest risk category with the costs accrued by the hospital when an ileostomy patient is readmitted for dehydration should also be considered.
This study is the first to use the NSQIP dataset to examine readmission for dehydration after ileostomy creation and to create a predictive model and risk scoring system. Prior single-institution studies investigating this topic have reported wide variation in readmission rates. The ACS-NSQIP provides a large sample size that not only increases statistical power but also reduces the effect of such single-institution variation. That our study uses aggregate data collected from hundreds of hospitals reduces the possibility of our dehydration readmission rate being largely due to single-institution factors. In this sense, NSQIP is more generalizable than single-institution databases or databases that target specific age groups such as Medicare for patients ≥65 years. Furthermore, NSQIP captures readmission-specific variables and standardized patient and clinical variables that may be lacking or less accurate in claims databases.
Despite rigorous statistical methodology and thorough study design, our study is subject to limitations pertaining to the NSQIP database. Several variables we had desired to assess for inclusion into the scoring system (ex. preoperative labs, ostomy output, pre-discharge medications) demonstrated substantial missingness or were not captured by NSQIP; we therefore did not include these variables in our analysis. Further modification and optimization of the DRIP score to include additional ileostomy-related variables such as ostomy output, antidiarrheal/diuretic use, and preoperative labs including hematocrit and electrolytes would enhance the predictive power of this scoring system. This can be accomplished through future external validation studies that apply the DRIP score to more specific institutional data. Our study, however, was able to demonstrate success with internal validation by partitioning the NSQIP database into derivation and validation samples.
Our dehydration readmission rate was slightly lower than in prior studies (2.9%).7–9,22,24,28–30 We suspect this may be due to differences in study population extraction. Whereas ileostomates may be easily identified in single-institution databases, the use of national databases like NSQIP requires extracting our study population based on ileostomy-related CPT code selection and identification of dehydration readmissions by ICD-9/10 codes. Our true incidence of dehydration may be underreported, as NSQIP only captures a single ICD-9/10 readmission for diagnosis. In other words, patients with a secondary diagnosis of dehydration would not be identified in our cohort. Patients who received intravenous fluid infusions in an ambulatory setting would also not be captured. However, this underreporting would bias our estimates towards the null to form more conservative conclusions. All prior studies citing higher dehydration readmission rates have been single institution studies with considerably smaller sample sizes and wide variation of reported rates. As such, any dehydration readmissions reported at their institutions make up a larger proportion of their dehydration readmission rates and may be affected by institution-specific factors.
Lastly, NSQIP reports 30-day postoperative readmissions rather than 30-day post-discharge readmissions. This discrepancy introduces immortal person-time bias, as patients are “immortal” for 30-day readmission until they are discharged from the hospital. To address this issue of immortal person-time bias and still enable adequate follow-up time, we excluded patients with LOS >15 days, a cutoff consistent with previous methods utilized to address this particular issue.14,31
The DRIP score is a novel, validated scoring system that identifies patients at high-risk for readmission from dehydration after ileostomy formation. It represents a proposed and specific strategy to identify high-risk patients, optimize known and modifiable risk factors, implement targeted interventions, prevent avoidable readmissions, and enhance hospital resource allocation.
FIGURE 1b.
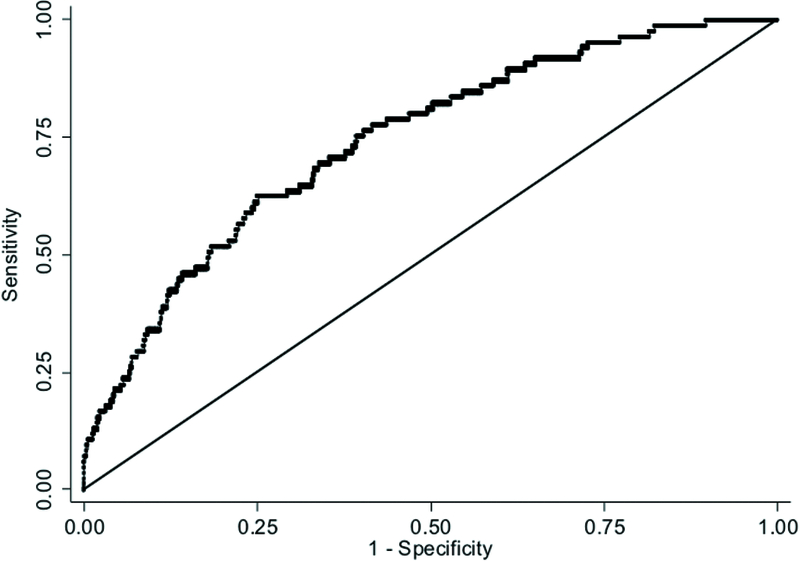
Receiver operating characteristic (ROC) curve for the prediction model (0.74) (validation sample).
ACKNOWLEDGMENTS
Sophia Y. Chen received financial support from the Johns Hopkins Institute for Clinical and Translational Research (ICTR), funded partly by Grant TL1 TR001078 from the National Center for Advancing Translational Sciences (NCATS)—a component of the NIH.
Support/Funding: This study was made possible by the Johns Hopkins Institute for Clinical and Translational Research (ICTR), which is funded in part by Grant Number TL1 TR001078 from the National Center for Advancing Translational Sciences (NCATS) a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the Johns Hopkins ICTR, NCATS or NIH.
Financial Disclosure: Conflicts of Interest and Source of Funding: All authors report no conflicts of interest in association with this manuscript. The American College of Surgeons National Surgical Quality Improvement Program and the hospitals participating in the ACS-NSQIP are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
REFERENCES
- 1.Centers for Medicare & Medicaid Services. Readmissions Reduction Program (HRRP). https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html. Published 2016. Accessed November 10, 2016.
- 2.Damle RN, Alavi K. Risk factors for 30-d readmission after colorectal surgery: a systematic review. J Surg Res. 2016;200:200–207. [DOI] [PubMed] [Google Scholar]
- 3.Damle RN, Cherng NB, Flahive JM, et al. Clinical and financial impact of hospital readmissions after colorectal resection: predictors, outcomes, and costs. Dis Colon Rectum. 2014;57:1421–1429. [DOI] [PubMed] [Google Scholar]
- 4.Kulaylat AN, Dillon PW, Hollenbeak CS, Stewart DB. Determinants of 30-d readmission after colectomy. J Surg Res. 2015;193:528–535. [DOI] [PubMed] [Google Scholar]
- 5.Orcutt ST, Li LT, Balentine CJ, et al. Ninety-day readmission after colorectal cancer surgery in a Veterans Affairs cohort. J Surg Res. 2016;201:370–377. [DOI] [PubMed] [Google Scholar]
- 6.HCUP. All patient readmissions within 30 days National statistics, 2013 Index stay 101 Coronary atherosclerosis and other heart disease. Healthc Cost Util Proj. 2016:8–9. [Google Scholar]
- 7.Messaris E, Sehgal R, Deiling S, et al. Dehydration is the most common indication for readmission after diverting ileostomy creation. Dis Colon Rectum. 2012;55:175–180. [DOI] [PubMed] [Google Scholar]
- 8.Hayden DM, Pinzon MCM, Francescatti AB, et al. Hospital readmission for fluid and electrolyte abnormalities following ileostomy construction: preventable or unpredictable? J Gastrointest Surg. 2013;17:298–303. [DOI] [PubMed] [Google Scholar]
- 9.Paquette IM, Solan P, Rafferty JF, Ferguson MA, Davis BR. Readmission for dehydration or renal failure after ileostomy creation. Dis Colon Rectum. 2013;56:974–979. [DOI] [PubMed] [Google Scholar]
- 10.Nagle D, Pare T, Keenan E, Marcet K, Tizio S, Poylin V. Ileostomy pathway virtually eliminates readmissions for dehydration in new ostomates. Dis Colon Rectum. 2012;55:1266–1272. [DOI] [PubMed] [Google Scholar]
- 11.Henderson WG, Daley J. Design and statistical methodology of the National Surgical Quality Improvement Program: why is it what it is? Am J Surg. 2009;198(suppl):S19–S27. [DOI] [PubMed] [Google Scholar]
- 12.ACS-NSQIP. ACS-NSQIP data collection, analysis, and reporting. https://www.facs.org/quality-programs/acs-nsqip/program-specifics/data. Accessed November 10, 2016.
- 13.American College of Surgeons National Surgical Quality Improvement Program. User Guide for the ACS NSQIP Participant User Data File (PUF). https://www.facs.org/~/media/files/quality_programs/nsqip/nsqip_puf_user_guide_2015.ashx. Published 2015. Accessed October 11, 2016.
- 14.Lucas DJ, Haut ER, Hechenbleikner EM, Wick EC, Pawlik TM. Avoiding immortal time bias in the American College of Surgeons National Surgical Quality Improvement Program readmission measure. JAMA Surg. 2014;149:875–877. [DOI] [PubMed] [Google Scholar]
- 15.Kelly KN, Iannuzzi JC, Aquina CT, et al. Timing of discharge: a key to understanding the reason for readmission after colorectal surgery. J Gastrointest Surg. 2015;19:418–427. [DOI] [PubMed] [Google Scholar]
- 16.Schneider EB, Hyder O, Brooke BS, et al. Patient readmission and mortality after colorectal surgery for colon cancer: impact of length of stay relative to other clinical factors. J Am Coll Surg. 2012;214:390–398. [DOI] [PubMed] [Google Scholar]
- 17.Kelly M, Sharp L, Dwane F, Kelleher T, Comber H. Factors predicting hospital length-of-stay and readmission after colorectal resection: a population-based study of elective and emergency admissions. BMC Health Serv Res. 2012;12:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shah PM, Johnston L, Sarosiek B, et al. Reducing readmissions while shortening length of stay: the positive impact of an enhanced recovery protocol in colorectal surgery. Dis Colon Rectum. 2017;60:219–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baltodano PA, Webb-Vargas Y, Soares KC, et al. A validated, risk assessment tool for predicting readmission after open ventral hernia repair. Hernia. 2016;20:119–129. [DOI] [PubMed] [Google Scholar]
- 20.Hardiman KM, Reames CD, McLeod MC, Regenbogen SE. Patient autonomy-centered self-care checklist reduces hospital readmissions after ileostomy creation. Surgery. 2016;160:1302–1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wick EC, Shore AD, Hirose K, et al. Readmission rates and cost following colorectal surgery. Dis Colon Rectum. 2011;54:1475–1479. [DOI] [PubMed] [Google Scholar]
- 22.Kiran RP, Delaney CP, Senagore AJ, Steel M, Garafalo T, Fazio VW. Outcomes and prediction of hospital readmission after intestinal surgery. J Am Coll Surg. 2004;198:877–883. [DOI] [PubMed] [Google Scholar]
- 23.Datta I, Buie WD, Maclean AR, Heine JA. Hospital readmission rates after ileal pouch-anal anastomosis. Dis Colon Rectum. 2009;52:55–58. [DOI] [PubMed] [Google Scholar]
- 24.Chun LJ, Haigh PI, Tam MS, Abbas MA. Defunctioning loop ileostomy for pelvic anastomoses: predictors of morbidity and nonclosure. Dis Colon Rectum. 2012;55:167–174. [DOI] [PubMed] [Google Scholar]
- 25.Fish DR, Mancuso CA, Garcia-Aguilar JE, et al. Readmission after ileostomy creation: retrospective review of a common and significant event. Ann Surg. 2017;265:379–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kaboli PJ, Go JT, Hockenberry J, et al. Associations between reduced hospital length of stay and 30-day readmission rate and mortality: 14-year experience in 129 Veterans Affairs hospitals. Ann Intern Med. 2012;157:837–845. [DOI] [PubMed] [Google Scholar]
- 27.Hendren S, Morris AM, Zhang W, Dimick J. Early discharge and hospital readmission after colectomy for cancer. Dis Colon Rectum. 2011;54:1362–1367. [DOI] [PubMed] [Google Scholar]
- 28.Nagle DA. Toward better understanding of readmissions for physiologic complications of ileostomy. Dis Colon Rectum. 2013;56:933–934. [DOI] [PubMed] [Google Scholar]
- 29.Phatak UR, Kao LS, You YN, et al. Impact of ileostomy-related complications on the multidisciplinary treatment of rectal cancer. Ann Surg Oncol. 2014;21:507–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bax TW, McNevin MS. The value of diverting loop ileostomy on the high-risk colon and rectal anastomosis. Am J Surg. 2007;193:585–587. [DOI] [PubMed] [Google Scholar]
- 31.Lucas DJ, Haider A, Haut E, et al. Assessing readmission after general, vascular, and thoracic surgery using ACS-NSQIP. Ann Surg. 2013;258:430–439. [DOI] [PMC free article] [PubMed] [Google Scholar]


