Abstract
Objectives:
This cross-sectional study examined the associations among optimism, psychological resilience, endogenous pain inhibition, and clinical knee pain severity. Two hypotheses were tested. First, we hypothesized that experimentally-tested endogenous pain inhibition would mediate the relationship between optimism and clinical knee pain severity. Secondly, it was also hypothesized that optimism would moderate the relationships of psychological resilience with endogenous pain inhibition and clinical knee pain severity, particularly for individuals with high optimism.
Methods:
A total of 150 individuals with or at risk for symptomatic knee osteoarthritis completed the Life Orientation Test-Revised, the Brief Resilience Scale, and the revised Short Form – McGill Pain Questionnaire-2 to assess optimism, psychological resilience, and clinical knee pain severity, respectively. Endogenous pain inhibition was examined experimentally using a conditioned pain modulation (CPM) protocol with algometry (test stimulus) and a cold pressor task (conditioning stimulus).
Results:
As hypothesized, results demonstrated that increased CPM significantly mediated the association between higher optimism and lower clinical knee pain severity. Further, optimism moderated the association between psychological resilience and CPM. However, contrary to our hypothesis, greater psychological resilience was associated with enhanced CPM in individuals with low optimism only.
Discussion:
This study suggests that an optimistic outlook may beneficially impact clinical pain severity by altering endogenous pain modulatory capacity. Furthermore, individuals with low optimism (i.e., pessimists) may be more adept at engaging resources that promote psychological resilience, which in turn, enhances endogenous pain modulatory capacity. Therefore, this study supports consideration of psychological resilience factors when evaluating experimental and clinical pain outcomes.
Keywords: Optimism, psychological resilience, osteoarthritis, conditioned pain modulation, knee pain
Introduction
Optimism is a personality attribute associated with the tendency to expect positive outcomes for the future, which often results in an increased sense of hopefulness and confidence.1, 2 A growing body of empirical evidence suggests that optimism reliably exerts widespread mental and physical health-promoting effects. 1, 3, 4 Of particular relevance to the current study, literature suggests that a more optimistic outlook positively influences pain experiences in both clinical and experimental settings. For example, optimism has been linked with lower reports of clinical pain severity and less pain-related interference in patients with painful musculoskeletal disorders5-7, various types of cancer8-10, and following surgical procedures.11-13 Likewise, experimental studies of psychophysical pain testing in healthy volunteers have shown that higher levels of optimism are related to decreased pain sensitivity and distress as well as greater placebo analgesia.14-16
Our group has previously shown that greater optimism is associated with enhanced endogenous pain inhibition via a conditioned pain modulation (CPM) paradigm in a non-clinical sample of healthy adults.17 We interpreted these results as suggesting that heightened endogenous pain inhibitory capacity may account, at least in part, for the positive clinical pain outcomes often demonstrated by optimistic individuals. Additionally, our group has also found that greater optimism is associated with decreased endogenous pain facilitation (temporal summation of heat pain) in a clinical sample of older adults with knee OA.18 Despite this initial work, no study to date has directly tested the possibility that adaptive endogenous pain modulatory processes may contribute to the positive pain outcomes often experienced by optimistic individuals with a chronic pain condition. As a logical extension of the work previously completed by our group, we now seek to determine whether optimism beneficially affects clinical pain severity through heightened endogenous pain inhibition (i.e., enhanced CPM).
Furthermore, it also remains unclear whether optimistic individuals might engage other resources that could be beneficially associated with endogenous pain inhibitory capacity (i.e., CPM) and clinical pain severity. Compared to their pessimistic counterparts, optimists are more likely to expect that positive outcomes will occur for them in the future. In an effort to ensure that these positive outcomes do occur, optimists actively engage adaptive coping strategies and behaviors that diminish stress responses and promote psychological resilience.19 As such, optimism and psychological resilience are likely to be indirectly related through shared associations with adaptive coping strategies such as positive thinking and engagement in pleasurable activities, for example. Psychological resilience is characterized by the ability to successfully adapt to stressful events in the face of adverse conditions.20 Evidence has shown that optimism is positively linked with psychological resilience, and that psychological resilience promotes adjustment to chronic pain.21 Specifically, prior literature has demonstrated that psychological resilience predicts adaptive experimental pain responses, such as greater habituation to heat and cold pain and less reported ischemic pain.22, 23 Interestingly, one study found a more pronounced effect of resilience on experimental pain severity in high stress participants, suggesting that psychological resilience may exert a greater protective influence on particular subgroups of individuals experiencing laboratory-induced pain.23 Given that personality characteristics such as optimism have previously been shown to augment the beneficial effects of adaptive psychological functioning on physical health 24, 25, it stands to reason that the positive impact of psychological resilience on experimental and clinical pain will be most pronounced for those individuals with high levels of optimism.
The goal of the present study was to examine associations among optimism, psychological resilience, endogenous pain inhibition via a CPM protocol, and self-reported clinical pain severity in a sample of individuals with or at risk for knee osteoarthritis (OA). Two primary hypotheses were tested. (1) Endogenous pain inhibition will mediate the association between optimism and clinical knee pain severity. Specifically, greater optimism will be associated with enhanced CPM, which in turn will be associated with less clinical knee pain severity. Figure 1 illustrates the putative conceptual model representing the first hypothesis. (2) Optimism will moderate the associations of psychological resilience with endogenous pain inhibition and clinical knee pain severity. Greater psychological resilience will be associated with enhanced CPM and less clinical knee pain severity, but only for those with high optimism. This is because optimists are likely to engage resources that promote psychological resilience. Figure 2 displays the putative conceptual model for the second hypothesis. It was also determined whether these hypothesized relationships held true after accounting for important control variables, particularly pain catastrophizing and negative affect. Given the overlap between measures of catastrophizing, negative affect, and pain, it is now commonplace for data analytic techniques addressing clinical or experimental pain to adjust for catastrophizing or some general negative affective factor.26-30 This was done in the current study in order to establish the unique effects of optimism and psychological resilience. A portion of this study has previously been presented in abstract form at the 36th annual meeting of the American Pain Society.
Figure 1.
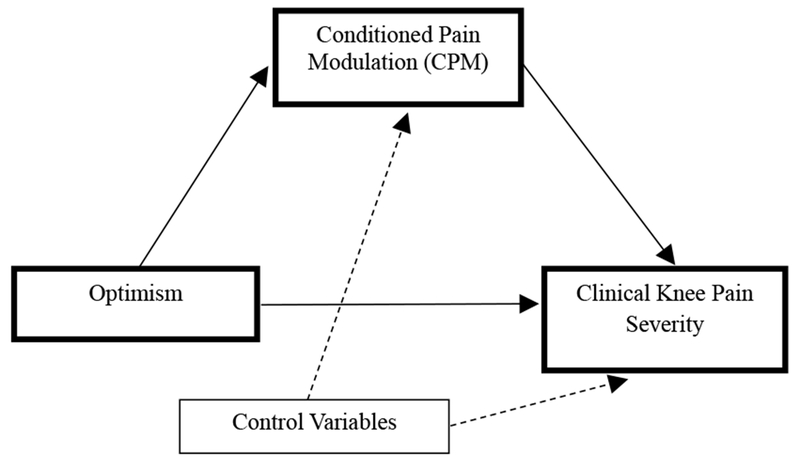
Mediation model representing the indirect association of optimism with clinical knee pain severity through conditioned pain modulation.
Figure 2:
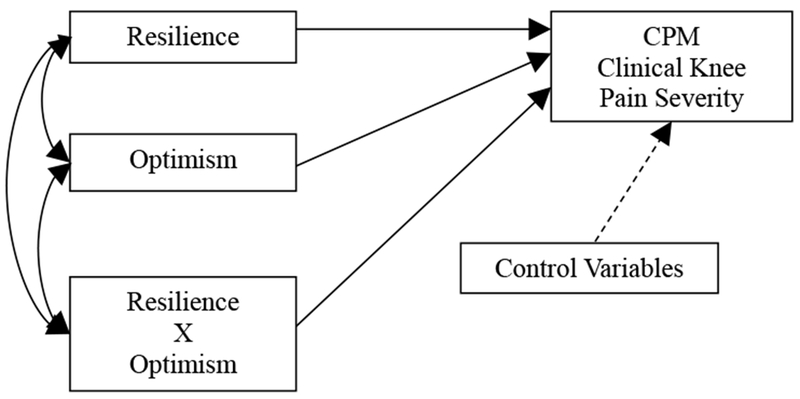
Moderation model representing the interaction between psychological resilience and optimism in relation to conditioned pain modulation (CPM) and clinical knee pain severity.
Methods
Study Overview
The current study is part of a larger ongoing project that aims to enhance the understanding of mechanisms underlying ethnic/racial group differences in knee pain (Understanding Pain and Limitations in Osteoarthritic Disease – Second Cycle, UPLOAD-2). The UPLOAD-2 study addresses these aims by directly and prospectively assessing the nature and evolution of altered central pain processing and its relationship with progression of pain and disability among middle-aged and older non-Hispanic blacks (NHB) and non-Hispanic whites (NHW) The UPLOAD-2 study is a multi-site investigation that recruits participants at the University of Florida and the University of Alabama at Birmingham. The participants described in the current analysis were recruited at both sites between August 2015 and May 2017, and have not previously been included in any published literature. The measures and procedures described below are limited to those involved in the current study. All procedures were reviewed and approved by the Institutional Review Boards at the University of Florida and University of Alabama at Birmingham.
Participants
We enrolled 150 community-dwelling participants aged 45 years and older with or at risk of knee OA, who were consecutively enrolled into the UPLOAD-2 study. Specifically, all individuals were positive upon initial telephone screening using a questionnaire that has previously shown 87% sensitivity and 92% specificity for radiographically confirmed symptomatic knee OA31. In addition, all participants reported current knee pain and were negative for other rheumatologic conditions (e.g. rheumatoid arthritis, fibromyalgia) that could explain knee pain. Given that there is widespread variability in definitions of OA,32 we adopted this approach to be as inclusive as possible in recruitment, as our primary focus is on understanding factors associated with knee pain rather than OA pathophysiology itself. Participants were recruited from the community via posted fliers, radio and print media advertisements, orthopedic clinic recruitment, and word-of-mouth referral. All participants provided informed consent and were compensated for their participation.
Procedures
Initial Screening.
All participants completed initial screening via telephone to determine eligibility for study inclusion. The following sociodemographic and physical health data were obtained as part of the screening: self-reported sex, age, and ethnic/racial identity, as well as a brief health history, including symptoms of knee OA. Individuals who endorsed knee pain and met initial study inclusion criteria presented approximately one to two weeks later for a health assessment session.
Initial criteria for participant inclusion into the study were as follows: 1) between 45 and 85 years of age; 2) having or being at risk for unilateral or bilateral symptomatic knee OA based upon American College of Rheumatology criteria33; and 3) availability to complete the multi-session protocol. Individuals were excluded from participation if they met any of the following criteria: 1) prosthetic knee replacement or other clinically significant surgery to the arthritic knee; 2) heart disease, congestive heart failure, or history of acute myocardial infarction; 3) peripheral neuropathy; 4) systemic rheumatic disorders including rheumatoid arthritis, systemic lupus erythematosus, and fibromyalgia; 5) chronic daily opioid use; 6) excessive anxiety regarding protocol procedures (e.g., refusal to complete controlled noxious stimulation procedures); or 7) hospitalization within the preceding year for psychiatric illness.
Health Assessment Session (HAS).
During the HAS, participants completed physical and mental health assessments to ensure participant safety and confirm ongoing study inclusion. For example, three consecutive blood pressure readings were obtained to assess for uncontrolled hypertension. Individuals with blood pressure readings that were > 150/95 were excluded from further study participation to minimize risk of potential cardiovascular events associated with noxious stimulation during quantitative sensory testing (QST). Furthermore, all individuals underwent a bilateral knee joint evaluation by an experienced examiner (i.e., the study rheumatologists [R.S. and L.B.H.] or nurse practitioner [T.L.G.]). Participants were categorized as either having, or being at risk for, knee OA using the American College of Rheumatology criteria for symptomatic knee OA33.
Quantitative Sensory Testing (QST) Session.
Approximately one week following the HAS, participants completed the QST session. For this study, endogenous pain inhibition was assessed using a “pain-inhibition-by-pain” model where pain in a local area (test stimulus) is inhibited by a second, co-occurring pain (conditioning stimulus), also known as “conditioned pain modulation” (CPM). To begin, baseline pressure pain threshold (PPT) was assessed at the trapezius muscle on participants’ left side using a hand-held, computerized pressure algometer (Medoc, Ltd., AlgoMed, Ramat Yishai) with a circular, rubber-tipped contact surface of 1.0 cm2. Participants indicated when the increasing pressure sensation first became painful. PPTs were measured in kilopascals (kPa). Following baseline PPT determination, participants immersed their right hand up to the wrist for one minute in a cold pressor (conditioning stimulus) maintained at 12°C. Participants were informed that they could remove their hand from the cold pressor at any time. The cold pressor consisted of an ARTIC A25 refrigerated bath with an SC150 immersion circulator (ThermoFisher Scientific, USA). Thirty seconds after initiating the cold pressor, while the hand was still immersed, PPT (test stimulus) was again assessed at the trapezius muscle. Following a ten-minute rest period, this entire protocol was repeated to complete a second CPM trial, with re-assessment of baseline PPT, cold pressor immersion, and concurrent conditioning PPT testing. Though there is ongoing debate regarding whether concurrent CPM trials are preferred to those in which the test stimulus is applied immediately after withdrawal of the conditioning stimulus, we chose to utilize a concurrent protocol given prior research showing that inhibitory effects are maximized during concurrent application of the conditioning stimulus.35 CPM was calculated by computing a percent change from baseline PPT to conditioning PPT. Percent change scores for each of the two CPM trials were calculated according to the following formula [((conditioned PPT – test PPT) / test PPT) *100].
Measures
Ethnicity/Race.
Participants provided self-report regarding ethnicity and racial background using response options consistent with the 2000 United States census survey.34 The primary groups enrolled self-identified as either non-Hispanic Black (NHB) or non-Hispanic White (NHW).
Body Mass Index.
Using the same scale for all participants, weight was measured without shoes to the nearest 0.1 kilogram (kg). Height was measured to the nearest 0.1 centimeter (cm) using a wall-mounted stadiometer which was calibrated daily with a standardized measuring rod. Body mass index (BMI) was calculated using the following algorithm: weight in kg/height in m2.
Revised version of the Short-form McGill Pain Questionnaire (SF-MPQ-2).
Participants completed the SF-MPQ-2 by rating the extent to which they experienced each of 22 pain descriptors in the past week using an 11-point numeric rating scale (0 = “none” to 10 = “worst possible”)35. The SF-MPQ-2 has been shown to have adequate reliability and validity in individuals with chronic pain conditions.36 Furthermore, the SF-MPQ-2 demonstrated excellent internal consistency in the present study (Cronbach’s α = .97). This measure is comprised of four summary scales: (1) continuous descriptors (throbbing pain, cramping pain, gnawing pain, aching pain, heavy pain, and tender), (2) intermittent descriptors (shooting pain, stabbing pain, sharp pain, splitting pain, electric-shock pain, and piercing), (3) neuropathic descriptors (hot-burning pain, cold-freezing pain, pain caused by light touch, itching, tingling or ‘pins and needles’, and numbness), and (4) affective descriptors (tiring-exhausting, sickening, fearful, and punishing-cruel). Instructions on the SF-MPQ-2 were modified to instruct participants that they should limit their descriptions of pain severity to only the pain experience in the knee(s). A total pain score was computed by averaging participant intensity ratings across all 22 pain descriptors. For the purpose of the current study, the total pain score for the SF-MPQ-2 was used as a measure of clinical knee pain severity. The SF-MPQ-2 was chosen over a simple numeric rating scale to capture a more comprehensive, dynamic account of each participant’s pain experience.
Life orientation test-revised (LOT-R).
Participants rated generalized positive outcome expectancies on 6 self-report items (plus 4 filler items) on a 5-point scale ranging from 0 (strongly disagree) to 4 (strongly agree). Dispositional optimism was calculated by averaging together the 3 negatively worded items (e.g., I hardly ever expect things to go my way) that were reverse scored with the 3 positively worded items (e.g., I am always optimistic about my future). Substantial research supports the reliability and validity of the LOT-R instrument.37 Additionally, the LOT-R demonstrated acceptable internal consistency in the present study (Cronbach’s α = .78).
Brief resilience scale (BRS).
The BRS measures an individual’s ability to recover from, and adapt to, stressful situations on 6 self-report items. Each item consists of a 5-point Likert-style scale ranging from 1 (strongly disagree) to 5 (strongly agree). Items 2, 4, and 6 are negatively worded items (e.g., “I have a hard time making it through stressful events”); therefore, they are reverse coded. These items are then averaged with the three positively worded items (e.g., “I tend to bounce back quickly after hard times) for a summary resilience score. The BRS has repeatedly shown both good reliability and validity. 38, 39 The BRS demonstrated good internal consistency in the present study (Cronbach’s α = .80).
Positive and negative affective scale (PANAS).
The PANAS is a 20-item scale that assesses positive and negative affect; however, the present study utilized only the 10 items corresponding to the negative affect subscale. Participants rated affect on a 5-point scale (1 = very slightly or not at all; 5 = extremely). Negative affect was calculated by summing all 10 items, resulting in scores ranging from 10 to 50. The PANAS has shown excellent psychometric reliability and validity across studies40-42, and in the current study the internal consistency of the negative affect subscale was excellent (Cronbach’s α = 90). Consistent with expected standards, this study controlled for negative affect as it is often inversely associated with optimism.
Coping strategies questionnaire-revised (CSQ-R).
The CSQ-R assesses the extent to which individuals use pain coping strategies across 7 possible strategies; however, the present study only used the catastrophizing subscale. Additionally, the CSQ-R was chosen over a larger, more comprehensive scale (e.g. Pain Catastrophizing Scale) to adequately balance assessment needs while minimizing time and burden of participants. Participants rated pain related catastrophic thoughts on a scale from 0 (never do that) to 6 (always do that). The reliability and validity of the CSQ-R subscales have previously been shown to be acceptable.43-45 Furthermore, the CSQ-R was included in analyses given documented relationships amongst optimism and catastrophizing.18 The internal consistency of the CSQ-R catastrophizing subscale was excellent (Cronbach’s α = 93).
Data Analysis
All data were analyzed using SPSS, version 24 (IBM; Chicago, IL). All participants provided complete demographic data (e.g., sex, age, and ethnicity/race); however, a small portion of missing data existed for CPM (< 10%) as well as self-report questionnaires (< 5% for any one questionnaire). Data were deemed to be missing at random; and therefore, a simple data imputation method was completed using the macro for Hot Deck imputation. This data imputation method is well validated and accepted in the statistical community46, 47 and resulted in complete study data for each of the 150 participants. The presence of CPM effects was examined using pairwise t tests. Pearson’s correlations were used to evaluate the associations among continuously measured variables including optimism, psychological resilience, CPM, and clinical knee pain severity. One-way analysis of variance (ANOVA) was used to examine group differences across ethnic/racial background and sex.
To test the first hypothesis, the PROCESS macro created and described by Hayes48 for obtaining a 95% bootstrapped percentile confidence interval with 5,000 resamples was utilized to test whether CPM significantly mediated the association between optimism and clinical knee pain severity. Bootstrapping is a non-parametric resampling procedure that has been shown to be a viable alternative to normal-theory tests of the intervening mediator between the independent and dependent variables49. The percentile confidence interval was incorporated to help minimize the potential of Type I error related to the test of the indirect effect. The bootstrapping technique indicates whether the total effect (path c) of optimism on clinical knee pain severity is comprised of a significant mediated effect (a×b). Path a denotes the effect of optimism on CPM, whereas, path b is the effect of CPM on clinical knee pain severity.
To test the second hypothesis, the PROCESS macro was again used to examine whether the relationship between psychological resilience and CPM was significantly moderated by optimism. The Johnson Neyman Technique with bootstrapped percentile confidence intervals was then applied to probe the interaction between optimism and psychological resilience. This technique tests the significance of the conditional association between psychological resilience and CPM within the observed range of values of the moderator (optimism) until the value of the moderator is identified, for which the conditional association is just statistically significant at a set level (α = .05). Values of the moderator for which the conditional association is significant constitute the region of significance. Determining the region of significance is desirable because it negates the need to choose arbitrary conditional values of the moderator (e.g., +/− 1SD around the mean).
Results
Overall participant characteristics and descriptive information for the entire sample are displayed in Table 1. The mean age of this study’s sample was 57.6 years (SD = 7.98) with a range of 45-78 years. The study sample was mostly comprised of women (64%), and participants’ sex was coded as 1 = men and 2 = women. The racial composition of the study’s sample was relatively equal, 49% self-identified as NHB and the remaining 51% self-identified as NHW. Ethnicity/race was coded as 1 = NHB and 2 = NHW. BMI for this sample was in the obese range (>30 kg/m2).50 The majority of participants in this study were recruited from the University of Florida site (63%) compared to the University of Alabama at Birmingham site (37%). Of the 150 study participants, 64% met criteria for symptomatic knee OA according to American College of Rheumatology, while the remaining 36% were at risk for knee OA. Neither CPM (t148 = 1.10, p = .275) nor clinical knee pain severity reported on the SF-MPQ-2 (t148 = 1.42, p = .159) significantly differed between participants with symptomatic knee OA and participants at risk for knee OA.
Table 1:
Participant characteristics and descriptive data for key study variables.
| Variable | % | Mean (SD) | Range |
|---|---|---|---|
| Age | 57.63 (7.98 | 45 - 78 | |
| Sex | |||
| Men | 64 | ||
| Women | 36 | ||
| Race | |||
| non-Hispanic White | 51 | ||
| non-Hispanic Black | 49 | ||
| BMI | 31.90 (7.43) | 19 - 59 | |
| PANAS Negative Affect | 16.64 (6.46) | 9 - 42 | |
| CSQ Catastrophizing | 1.41 (1.27) | 0 - 6 | |
| LOT-R Optimism | 10.53 (3.18) | 2 - 18 | |
| BRS Resilience | 3.72 (.76) | 1.33 – 5 | |
| CPM | 33.34 (34.50) | −22.47 – 243.50 | |
| SF-MPQ-2 Clinical Knee Pain Severity | 2.55 (2.26) | 0 – 8.55 |
Note: Age measured in years; BMI = Body Mass Index; PANAS = Positive and Negative Affect Scale; CSQ = Coping Strategies Questionnaire; LOT-R = Life Orientation Test-Revised; BRS = Brief Resilience Scale; CPM = conditioned pain modulation measured as percent change from baseline; SF-MPQ-2 = Revised Short Form – McGill Pain Questionnaire-2.
CPM and SF-MPQ-2
Pairwise t-tests revealed significant CPM effects on PPTs assessed at the trapezius for both Trial 1 (t149 = 10.65, p < .001) and Trial 2 (t149 = 7.26, p < .001), such that the PPTs obtained during concurrent application of cold water pain were significantly greater than baseline PPTs. CPM effects, calculated as percent change from baseline, for Trial 1 and Trial 2 were averaged together to obtain an overall CPM value that was used in all subsequent analyses. CPM was non-normally distributed, with skewness of 0.77 (SE = 0.19) and kurtosis of 1.42 (SE = 0.39). Similarly, clinical knee pain severity reported on the SF-MPQ-2 was also non-normally distributed, with skewness of 0.86 (SE = 0.19) and kurtosis of −0.26 (SE = 0.39). Data transformation did not significantly improve the normality of these variables; therefore, each variable was left untransformed and analyzed as such.
Bivariate Associations and Examination of Statistical Covariates
Zero-order correlations are presented in Table 2. Consistent with previous findings from our laboratory and others, greater optimism was significantly correlated with heightened endogenous pain inhibition represented by CPM and lower clinical knee pain severity on the SF-MPQ-2. CPM was also significantly and inversely correlated with clinical knee pain severity. Psychological resilience was significantly correlated with less clinical knee pain severity, but not with CPM. Optimism and psychological resilience were not significantly correlated. Further, greater clinical knee pain severity reported on the SF-MPQ-2 was significantly correlated with age, BMI, pain catastrophizing, and negative affect. NHB participants reported significantly greater clinical knee pain severity than NHW participants (F = 26.62, p < .001); however, CPM was not significantly different across race (F = 0.02, p = .883). There was no significant difference between men and women for clinical knee pain severity (F = 0.22, p = .641) or CPM (F = 0.01, p = .982). Age, BMI, racial background, pain catastrophizing, and negative affect were subsequently included as statistical covariates in multivariable analyses examining the associations among optimism, psychological resilience, CPM, and clinical knee pain severity.
Table 2:
Pearson’s correlations among continuously-measured variables.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| 1. Age | —— | ||||||
| 2. PANAS Negative affect | −.367** | —— | |||||
| 3. CSQ Catastrophizing | −.354** | .493** | —— | ||||
| 4. BMI | −.280** | .102 | .243** | —— | |||
| 5. LOT-R Optimism | .211** | −.137 | −.333** | −.109 | —— | ||
| 6. BRS Resilience | .202* | −.527** | −.329** | −.001 | .094 | —— | |
| 7. CPM | .039 | −.047 | −.123 | −.051 | .190* | .141 | —— |
| 8. SF-MPQ-2 Clinical Knee Pain Severity | −.344** | .402** | .620** | .264** | −.368** | −.181* | −.216** |
= p < .05
= p < .01
Note: PANAS = Positive and Negative Affect Scale; CSQ = Coping Strategies Questionnaire; BMI = Body Mass Index; LOT-R = Life Orientation Test-Revised; BRS = Brief Resilience Scale; CPM = conditioned pain modulation; SF-MPQ-2 = Revised Short Form – McGill Pain Questionnaire-2.
Hypothesis 1
The overall mediation model adjusted for covariates shown in Figure 3 accounted for a significant 47% of the total variance in clinical knee pain severity ratings (R2 = .467, p < .001). The mediation effect (path a×b) of optimism on clinical knee pain severity through CPM had a point estimate of −.019 and a 95% percentile confidence interval of −.048 to −.003. This confidence interval suggests that, even after statistically controlling covariates, the mediated effect represented by a×b is significantly different from zero (i.e., the null effect) at p < .05. The directions of paths a (t = 2.17, p = .032) and b (t = −2.17, p = .031) are consistent with the interpretation that greater optimism is associated with enhanced endogenous pain inhibitory capacity via CPM, which in turn, is associated with less severe clinical knee pain. Thus, CPM was a significant mediator of the association between optimism and clinical knee pain severity. Given the cross-sectional nature of this study, it could be argued that individuals with less clinical knee pain severity experience greater CPM, and subsequently maintain a more optimistic outlook towards the future. To test this possibility, an additional mediation model was analyzed using clinical knee pain severity as the independent variable, CPM as the mediator, and optimism as the dependent variable. When modeled in this direction, results revealed non-significant mediation (point estimate of −.053 and 95% percentile confidence interval of −.137 to .009). This lack of significance lends further credence to the validity of our original hypothesis that greater optimism is associated with enhanced CPM, which in turn, is associated with less clinical knee pain severity.
Figure 3.
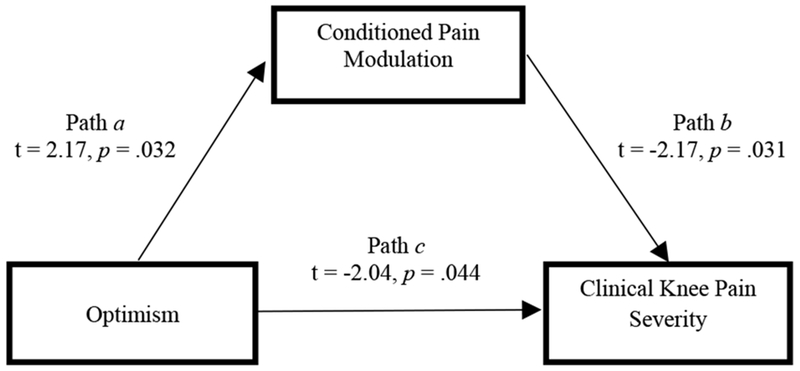
Conditioned pain modulation (CPM) significantly mediates the association between optimism (LOT-R) and clinical knee pain severity (SF-MPQ-2).
Significant mediation: (a x b = −.019; 95% percentile CI of −.048 to −.003)
Hypothesis 2
The overall moderation model adjusted for covariates (Table 3) accounted for a small, yet significant, 10% of the variance in CPM (R2 = .097, p = .048). There was a significant interaction between psychological resilience and optimism in relation to CPM (t = −2.20, p = .031), suggesting that the association of psychological resilience and endogenous pain inhibitory capacity (CPM) is indeed moderated by optimism. However, contrary to our hypothesis, results of the Johnson–Neyman technique (Table 4) show that greater psychological resilience is significantly associated with enhanced CPM, but only for those with low levels of optimism (≤ 9.87). As optimism approaches intermediate and high levels, the association between psychological resilience and CPM weakens and is no longer significant (Figure 4). Lastly, there was no significant interaction between psychological resilience and optimism in relation to clinical knee pain severity (t = −0.03, p = .975).
Table 3:
Moderation analysis testing whether optimism (LOT-R) and psychological resilience (BRS) are interactively related to conditioned pain modulation (CPM) adjusting for covariates.
| Variable | Coeff | SE | t | p | 95% CI LL to UL |
|---|---|---|---|---|---|
| Age | −.026 | .396 | −.066 | .947 | −.809 to .757 |
| Ethnicity/Race | −3.413 | 6.221 | −.549 | .584 | −15.711 to 8.884 |
| BMI | −.094 | .398 | −.236 | .814 | −.881 to .693 |
| PANAS Negative Affect | .332 | .565 | .589 | .557 | −.784 to 1.448 |
| CSQ Catastrophizing | −1.779 | 2.799 | −.636 | .526 | −7.315 to 3.758 |
| BRS Psychological Resilience | 33.150 | 13.059 | 2.538 | .012 | 7.332 to 58.968 |
| LOT-R Optimism | 10.614 | 4.041 | 2.627 | .009 | 2.627 to 18.601 |
| Interaction | −2.433 | 1.116 | −2.180 | .031 | −4.640 to −.227 |
Note: Ethnicity/Race coded 1 = non-Hispanic Black, 2 = non-Hispanic White; BMI = Body Mass Index, Coeff = coefficient, SE = standard error, CI = confidence interval, LL = lower limit, UL = upper limit; Interaction = psychological resilience by optimism.
Table 4:
Johnson-Neyman technique demonstrating the moderated effect of psychological resilience (BRS) on endogenous pain inhibition (CPM) across observed values for optimism (LOT-R).
| LOT-R Values (moderator) | Coeff | SE | t | p | 95% CI LL to UL |
|---|---|---|---|---|---|
| 2.00 | 28.284 | 10.988 | 2.574 | .011 | 6.562 to 50.006 |
| 2.80 | 26.338 | 10.178 | 2.588 | .011 | 6.216 to 46.459 |
| 3.60 | 24.391 | 9.383 | 2.599 | .010 | 5.841 to 42.941 |
| 4.40 | 22.445 | 8.608 | 2.607 | .010 | 5.427 to 39.462 |
| 5.20 | 20.498 | 7.858 | 2.609 | .010 | 4.964 to 36.033 |
| 6.00 | 18.552 | 7.141 | 2.598 | .010 | 4.435 to 32.668 |
| 6.80 | 16.605 | 6.467 | 2.568 | .011 | 3.820 to 29.390 |
| 7.60 | 14.659 | 5.853 | 2.505 | .013 | 3.088 to 26.229 |
| 8.40 | 12.721 | 5.318 | 2.391 | .018 | 2.199 to 23.225 |
| 9.20 | 10.758 | 4.889 | 2.202 | .029 | 1.101 to 20.430 |
| 9.87 | 9.165 | 4.636 | 1.977 | .050 | .000 to 18.331 |
| 10.00 | 8.819 | 4.595 | 1.919 | .057 | −.265 to 17.903 |
| 10.80 | 6.873 | 4.464 | 1.539 | .126 | −1.952 to 15.697 |
| 11.60 | 4.926 | 4.509 | 1.092 | .276 | −3.987 to 13.839 |
| 12.40 | 2.980 | 4.725 | .631 | .529 | −6.362 to 12.321 |
| 13.20 | 1.033 | 5.091 | .203 | .840 | −9.032 to 11.099 |
| 14.00 | −0.913 | 5.578 | −.164 | .870 | −11.940 to 10.114 |
| 14.80 | −2.860 | 6.156 | −.465 | .643 | −15.029 to 9.310 |
| 15.60 | −4.806 | 6.802 | −.707 | .481 | −18.254 to 8.642 |
| 16.40 | −6.753 | 7.500 | −.901 | .370 | −21.579 to 8.074 |
| 17.20 | −8.699 | 8.235 | −1.056 | .293 | −24.979 to 7.581 |
| 18.00 | −10.646 | 8.999 | −1.183 | .239 | −28.435 to 7.114 |
Figure 4.
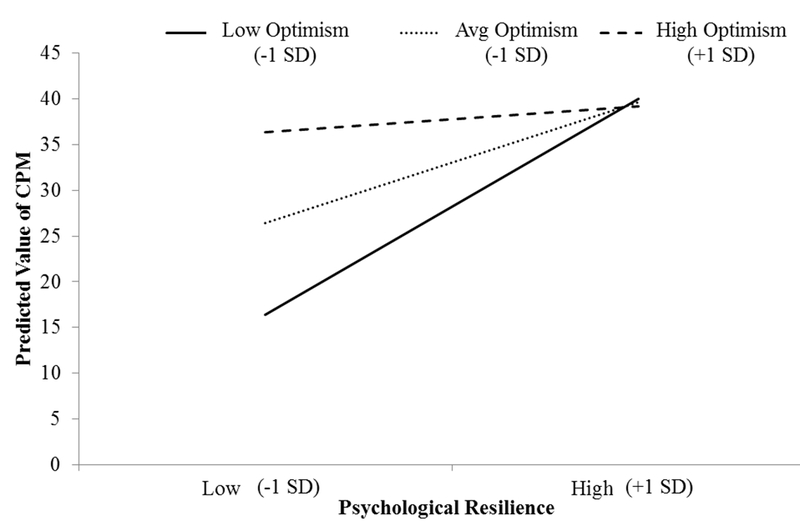
Plot of simple slopes depicting associations of psychological resilience and conditioned pain modulation (CPM) at low, average (intermediate), and high levels of Optimism. Note: SD = standard deviation.
Discussion
Results fully supported our first hypothesis and revealed that greater CPM mediated the relationship between high optimism and less clinical knee pain severity. This suggests that enhanced endogenous pain inhibition may account, at least partly, for the association between optimism and decreased clinical pain severity in individuals with or at risk for symptomatic knee OA. Our second hypothesis, however, was only partially supported. Indeed, results demonstrated that the relationship between psychological resilience and CPM was moderated by optimism. We hypothesized that the relationship between psychological resilience and CPM would only be significant for those with high optimism, yet we found the opposite. Specifically, greater psychological resilience was significantly related to enhanced endogenous pain inhibition (CPM) only for individuals with low optimism.
Regarding this study’s support for our first hypothesis, cognitive and behavioral factors offer insight into the links between optimism and clinical as well as experimental pain outcomes. For example, optimistic individuals have been found to be more likely to engage in approach-oriented coping strategies (e.g., planning, seeking support), and less likely to engage in avoidance coping strategies (e.g., denial, isolating oneself) when confronted with threats or challenges.51-53Approach-oriented coping often beneficially enhances health and pain-specific outcomes because individuals who utilize this coping style are more likely to access healthcare resources appropriately, engage in health-promoting behaviors, and seek social support.54, 55 Individuals with a highly optimistic outlook on life may be well-positioned to engage endogenous pain inhibitory processes that decrease their perception of pain given their propensity for approach-oriented coping styles.
In addition to the cognitive and behavioral factors, biological underpinnings of their relationship between optimism and endogenous pain inhibition is also worthy of discussion. As previously reviewed by our group, optimism is associated with the engagement of many cortical regions involved in the processing of pain signals.56 Prior brain imaging studies have revealed a network of subcortical (e.g., amygdala, periaqueductal gray) and cortical structures (e.g., prefrontal cortex (PFC), anterior cingulate cortex (ACC), insula, somatosensory cortices) that are involved in pain processing and modulation.57, 58 Interestingly, experimental induction of an optimistic bias has been associated with greater activation of regions involved in endogenous pain inhibition, such as the PFC and anterior cingulate, and with reduced activation of key pain processing areas such as the insula and secondary somatosensory cortex.59, 60 Thus, optimism may promote patterns of brain activity that enhance endogenous pain inhibition and ultimately attenuate pain perception in daily life, highlighting the importance of maintaining an optimistic outlook.
Psychological resilience in the face of chronic pain is perhaps best characterized by the ability to maintain positive affect, minimize maladaptive cognitive process such as pain catastrophizing, and remain engaged in highly valued activities of daily living.21 Optimism has been suggested to be a key personality characteristic of individuals with high psychological resilience.21 Therefore, it is not surprising that optimistic individuals routinely engage many of the cognitive and behavioral resources that promote psychological resilience. For individuals with chronically painful conditions such as knee OA, maintaining optimism and psychological resilience synergistically promotes adjustment to chronic pain and less severe pain.61, 62 Accordingly, our second study hypothesis focused on the interplay between psychological resilience and optimism in relation to CPM and clinical knee pain severity. We found that psychological resilience was significantly associated with enhanced CPM for individuals with low optimism, but not intermediate or high optimism. These findings potentially suggest that when optimism is low or absent in the context of chronic knee OA-related pain, behaviors and coping strategies that promote psychological resilience become necessary to engage. As a result, CPM may be promoted and enhanced. Alternatively, when individuals maintain a high degree of optimism, there is less need to engage psychological resilience. In turn, psychological resilience is not associated with CPM. The clinical relevance of these findings in relation to chronic pain is unclear at this time, especially given that optimism did not significantly moderate the association between psychological resilience and clinical knee pain severity in this study.
From a public health perspective, understanding factors related to chronic pain management and improved physical functioning is crucial to providing precise, appropriate interventions for those afflicted. Arthritis-related pain places an immense strain on the economy through health care utilization costs, lost workplace productivity, and medication coverage.63 Because existing surgical and medical approaches to OA treatment are limited in efficacy and can have substantial adverse effects,64 it is imperative that alternative interventions be implemented based on a more comprehensive model of chronic pain management. This research suggests that optimism and psychological resiliency may be two targets for psychotherapeutic intervention that have clear relationships to effective pain modulation in knee OA patients.
While some patients respond well to traditional cognitive-behavioral therapy (CBT) for chronic pain, effect sizes for CBT are modest and this form of treatment is effective for some patients, but not all.65, 66 Thus, it is important to consider creative avenues to enhance and expand the current armamentarium of psychotherapeutic interventions for chronic pain. Given the results of our study and that of others, designing new (or modifying existing) interventions to enhance optimism and/or psychological resilience appears to be a potentially fruitful line of research for the management of chronic pain moving forward. For example, limited but promising prior research suggests that “optimism training” may positively increase the ability to expect favorable outcomes in the future, which in turn decreases sensitivity to experimental pain stimuli.67, 68 Additionally, bolstering other psychological resources, such as resilience, could provide additional pain management benefits particularly for individuals with low optimism. To illustrate, studies have shown that resilience can be enhanced by focusing on psychological attributes, such as positive reappraisal of traumatic events, promotion of meaning-making, and preservation of a sense of purpose in the face of trauma. Addressing additional psychosocial factors including positive affect, the capacity for self-regulation, and increased positive social interactions and bonding may also have a positive impact on building psychological resilience.69
Although this study provides novel information regarding the associations among optimism and psychological resilience with experimental and clinical pain in a sample of adults with or at risk for knee OA, there are several limitations that warrant consideration when interpreting these results. To begin, both CPM and SF-MPQ-2 were significantly skewed and kurtotic in this study. The normality assumption for parametric data analysis was therefore not met. Although most parametric statistics are robust to violations of normality when sample sizes are appropriately large70, our results should still be interpreted with caution. Next, the cross-sectional and correlational nature of this study limits the ability to draw causal inferences from the data; however, we argue that this does not preclude the use of mediation and moderation models to describe patterns of association. For instance, the application of a mediation model to cross-sectional data is currently well accepted in the statistical community given that the model presents a strong theoretical basis and a logical temporal precedence among the variables included in the model.71 That our mediation model was significant when modeled as optimism → CPM → clinical knee pain severity, but non-significant when modeled in reverse, lends credence to the temporal precedence of our mediation model as hypothesized. Further support for our mediation model comes from a substantial theoretical foundation established by previous research conducted by our group.17, 18 Next, we examined CPM using standard procedures involving mechanical pressure and cold water pain,72 and we examined clinical pain responses using the SF-MPQ-2. Whether similar findings of associations with optimism and psychological resilience will be found using other methods of assessing CPM and clinical pain outcomes needs to be examined. Finally, the present study focused specifically on adults with or at risk for symptomatic knee OA. Whether our findings can be replicated and generalized to other chronic pain populations remains unknown. It will be important for future research to explore the relationships among optimism, psychological resilience, and experimental and clinical pain in other chronic pain conditions to confirm the generalizability of our findings.
Despite these limitations, this study supports the value of considering psychological factors such as optimism and resiliency when evaluating pain modulatory processes in individuals with chronic pain. Additionally, results suggest that individuals lacking resources in one protective factor (e.g., optimism) may be able to engage alternate, effective resources to better modulate painful experiences. Additional experimental studies evaluating endogenous pain inhibition in this context are crucial to confirm these conclusions. Future interventional studies evaluating the effectiveness of building optimism and psychological resilience may provide insight into treatment targets for individuals with chronic pain. Given that the number of US adults with arthritis is projected to rise to 67 million by the year 2030, 63, 73 continued research in this area has the potential for a large impact in the coming years.
Acknowledgments
Disclosures
Funding and support provided by NIH/NIA Grants R37AG033906-14 (R.B.F) and R01AG054370 (K.T.S); UF CTSA Grant UL1TR001427 and UAB CTSA Grant UL1TR001417 from the NIH Center for Advancing Translational Sciences; NIH Training Grants TL1TR001418 provided to the University of Alabama at Birmingham (K.A.T.), R25CA090314 provided to the Moffitt Cancer Center (H.W.B.), T32AG049673 provided to the University of Florida (E.L.T.), and NIH/NIA Grant K99AG052642 (E.J.B). All authors declare that there are no conflicts of interest with this study.
References
- 1.Goodin BR, Bulls HW. Optimism and the experience of pain: benefits of seeing the glass as half full. Curr Pain Headache Rep 2013;17:329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wright MA, Wren AA, Somers TJ, et al. Pain acceptance, hope, and optimism: relationships to pain and adjustment in patients with chronic musculoskeletal pain. J Pain 2011;12:1155–1162. [DOI] [PubMed] [Google Scholar]
- 3.Scheier MF, Carver CS. Optimism, coping, and health: assessment and implications of generalized outcome expectancies. Health Psychol 1985;4:219. [DOI] [PubMed] [Google Scholar]
- 4.Scheier MF, Carver CS. Effects of optimism on psychological and physical well-being: Theoretical overview and empirical update. Cognit Ther Res 1992;16:201–228. [Google Scholar]
- 5.Ferreira V, Sherman A. The relationship of optimism, pain and social support to well-being in older adults with osteoarthritis. Aging Ment Health 2007;11:89–98. [DOI] [PubMed] [Google Scholar]
- 6.Treharne GJ, Kitas GD, Lyons AC, et al. Well-being in rheumatoid arthritis: the effects of disease duration and psychosocial factors. J Health Psychol 2005;10:457–474. [DOI] [PubMed] [Google Scholar]
- 7.Sipilä K, Ylöstalo PV, Ek E, et al. Association between optimism and self-reported facial pain. Acta Odontol Scand 2006;64:177–182. [DOI] [PubMed] [Google Scholar]
- 8.Wong WS, Fielding R. Quality of life and pain in Chinese lung cancer patients: Is optimism a moderator or mediator? Qual Life Res 2007;16:53–63. [DOI] [PubMed] [Google Scholar]
- 9.Allison PJ, Guichard C, Gilain L. A prospective investigation of dispositional optimism as a predictor of health-related quality of life in head and neck cancer patients. Qual Life Res 2000;9:951–960. [DOI] [PubMed] [Google Scholar]
- 10.Kurtz ME, Kurtz JC, Given CW, et al. Patient Optimism and Mastery—Do They Play a Role in Cancer Patients’ Management of Pain and Fatigue? J Pain Symptom Mange 2008;36:1–10. [DOI] [PubMed] [Google Scholar]
- 11.Mahler HI, Kulik J. Optimism, pessimism and recovery from coronary bypass surgery: Prediction of affect, pain and functional status. Psychol Health Med 2000;5:347–358. [Google Scholar]
- 12.Peters ML, Sommer M, de Rijke J, et al. Somatic and psychologic predictors of long-term unfavorable outcome after surgical intervention. Ann Surg 2007;245:487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosenberger PH, Kerns R, Jokl P, et al. Mood and attitude predict pain outcomes following arthroscopic knee surgery. Ann Behav Med 2009;37:70–76. [DOI] [PubMed] [Google Scholar]
- 14.Geers AL, Wellman JA, Helfer SG, et al. Dispositional optimism and thoughts of well-being determine sensitivity to an experimental pain task. Ann Behav Med 2008;36:304–313. [DOI] [PubMed] [Google Scholar]
- 15.Geers AL, Wellman JA., Fowler SL, et al. Dispositional optimism predicts placebo analgesia. J Pain 2010;11:1165–1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hanssen MM, Vancleef LMG, Vlaeyen JWS, et al. More optimism, less pain! The influence of generalized and pain-specific expectations on experienced cold-pressor pain. J Behav Med 2014;37:47–58. [DOI] [PubMed] [Google Scholar]
- 17.Goodin BR, Kronfil T, King CD, et al. Testing the relation between dispositional optimism and conditioned pain modulation: does ethnicity matter? J Behav Med 2013;36:165–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goodin BR, Glover TL, Sotolongo A, et al. The association of greater dispositional optimism with less endogenous pain facilitation is indirectly transmitted through lower levels of pain catastrophizing. J Pain 2013;14:126–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wu G, Feder A, Cohen H, et al. Understanding resilience. Frontiers Behav Neurosci 2013;7:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Norman E Resiliency enhancement: Putting the strength perspective into social work practice. New York: Columbia University Press, 2012. [Google Scholar]
- 21.Sturgeon JA, Zautra AJ. Resilience: a new paradigm for adaptation to chronic pain. Curr Pain Headache Rep 2010;14:105–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smith BW, Tooley EM, Montague EQ, et al. The role of resilience and purpose in life in habituation to heat and cold pain. J Pain 2009;10:493–500. [DOI] [PubMed] [Google Scholar]
- 23.Friborg O, Hjemdal O, Rosenvinge JH, et al. Resilience as a moderator of pain and stress. J Psychosom Res 2006;61:213–219. [DOI] [PubMed] [Google Scholar]
- 24.Tusaie K, Puskar K, Sereika SM. A predictive and moderating model of psychosocial resilience in adolescents. J Nurs Scholarsh 2007;39:54–60. [DOI] [PubMed] [Google Scholar]
- 25.Smith TW. Personality as risk and resilience in physical health. Curr Dir Psychol Sci 2006;15:227–231. [Google Scholar]
- 26.Gaskin M, Greene AF, Robinson ME, et al. Negative affect and the experience of chronic pain. J Psychosom Res 1992;36:707–713. [DOI] [PubMed] [Google Scholar]
- 27.Goodin BR, McGuire L, Allshouse M, et al. Associations between catastrophizing and endogenous pain-inhibitory processes: sex differences. J Pain 2009;10:180–190. [DOI] [PubMed] [Google Scholar]
- 28.Huyser BA, Parker JC. Negative affect and pain in arthritis. Rheum Dis Clin North Am 1999;25:105–121. [DOI] [PubMed] [Google Scholar]
- 29.Owens MA, Bulls HW, Trost Z, et al. An Examination of Pain Catastrophizing and Endogenous Pain Modulatory Processes in Adults with Chronic Low Back Pain. Pain Med 2016;17:1452–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sullivan MJ, Thorn B, Haythornwaite JA, et al. Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain 2001;17:52–64. [DOI] [PubMed] [Google Scholar]
- 31.Roux CH, Mazieres B, Purchot J, et al. Screening for hip and knee osteoarthritis in the general population: predictive value of a questionnaire and prevalence estimates. Ann Rheum Dis 2008;67:1406–1411. [DOI] [PubMed] [Google Scholar]
- 32.Kraus VB, Blanco FJ, Englund M, et al. Call for standardized definitions of osteoarthritis and risk stratification for clinical trials and clinical use. Osteoarthritis Cartilage 2015;23:1233–1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Altman R, Asch E, Bloch D, et al. Development of criteria for the classification and reporting of osteoarthritis: classification of osteoarthritis of the knee. Arthritis Rheum 1986;29:1039–1049. [DOI] [PubMed] [Google Scholar]
- 34.Vincent GK, Velkoff VA. The next four decades, the older population in the United States: 2010 to 2050. Washington, DC: US Census Bureau, 2010. [Google Scholar]
- 35.Dworkin RH, Turk DC, Revivki DA, et al. Development and initial validation of an expanded and revised version of the Short-form McGill Pain Questionnaire (SF-MPQ-2). Pain 2009;144:35–42. [DOI] [PubMed] [Google Scholar]
- 36.Hawker GA, Milan S, Kendzerska T, et al. Measures of adult pain: Visual analog scale for pain (vas pain), numeric rating scale for pain (nrs pain), mcgill pain questionnaire (mpq), short-form mcgill pain questionnaire (sf-mpq), chronic pain grade scale (cpgs), short form-36 bodily pain scale (sf-36 bps), and measure of intermittent and constant osteoarthritis pain (icoap). Arthritis Care Res 2011;63. [DOI] [PubMed] [Google Scholar]
- 37.Burke KL, Joyner AB, Czech DR, et al. An investigation of concurrent validity between two optimism/pessimism questionnaires: The life orientation test-revised and the optimism/pessimism scale. Curr Psychol 2000;19:129–136. [Google Scholar]
- 38.Smith BW, Dalen J, Wiggins K, et al. The brief resilience scale: assessing the ability to bounce back. Int J Behavl Med 2008;15:194–200. [DOI] [PubMed] [Google Scholar]
- 39.Windle G, Bennett KM, Noyes J. A methodological review of resilience measurement scales. Health Qual Life Outcomes 2011; 9:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Crawford JR, Henry JD. The Positive and Negative Affect Schedule (PANAS): Construct validity, measurement properties and normative data in a large non-clinical sample. Br J Clin Psychol 2004;43:245–265. [DOI] [PubMed] [Google Scholar]
- 41.Sibille KT, Kindler LL, Glover TL, et al. Affect balance style, experimental pain sensitivity, and pain-related responses. Clin J Pain 2012;28:410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol 1988;54:1063. [DOI] [PubMed] [Google Scholar]
- 43.Jensen MP, Keefe FJ, Lefebvre JC, et al. One-and two-item measures of pain beliefs and coping strategies. Pain 2003;104:453–469. [DOI] [PubMed] [Google Scholar]
- 44.Riley JL III, Robinson ME. CSQ: Five factors or fiction? Clin Journal Pain 1997;13:156–162. [DOI] [PubMed] [Google Scholar]
- 45.Rosenstiel AK, Keefe FJ. The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain 1983;17:33–44. [DOI] [PubMed] [Google Scholar]
- 46.Reilly M Data analysis using hot deck multiple imputation. Stat 1993;307–313. [Google Scholar]
- 47.Kalton G, Kasprzyk D. The treatment of missing survey data. Surv Methodol 1986;12:1–16. [Google Scholar]
- 48.Hayes AF. PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling. 2012.
- 49.Hayes AF. Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Commun Monogr 2009;76:408–420. [Google Scholar]
- 50.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA 2014;311:806–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Edgar L, Remmer J, Rosberger Z, et al. Resource use in women completing treatment for breast cancer. Psychooncology 2000;9:428–438. [DOI] [PubMed] [Google Scholar]
- 52.Epping-Jordan JE, Compas BE, Osowiecki DM, et al. Psychological adjustment in breast cancer: processes of emotional distress. Health Psychol 1999;18:315. [DOI] [PubMed] [Google Scholar]
- 53.King KB, Rowe MA, Kimble LP, et al. Optimism, coping, and long-term recovery from coronary artery surgery in women. Res Nurs Health 1998;21:15–26. [DOI] [PubMed] [Google Scholar]
- 54.Billings AG, Moos RH. Coping, stress, and social resources among adults with unipolar depression. J Pers Soc Psychol 1984;46:877. [DOI] [PubMed] [Google Scholar]
- 55.Scheier MF Carver CS. Optimism, coping, and health: assessment and implications of generalized outcome expectancies. Health Psychol 1985;4:219–47. [DOI] [PubMed] [Google Scholar]
- 56.Piche M, Arsenault M, Rainville P. Cerebral and cerebrospinal processes underlying counterirritation analgesia. J Neurosci 2009;29:14236–1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wilder-Smith CH, Schindler D, Lovblad K, et al. Brain functional magnetic resonance imaging of rectal pain and activation of endogenous inhibitory mechanisms in irritable bowel syndrome patient subgroups and healthy controls. Gut 2004;53:1595–1601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wiech K, Kalisch R, Weiskopf N, et al. Anterolateral prefrontal cortex mediates the analgesic effect of expected and perceived control over pain. J Neurosci 2006;26:11501–11509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wiech K, Ploner M, Tracey I. Neurocognitive aspects of pain perception. Trends Cogn Sci 2008;12:306–313. [DOI] [PubMed] [Google Scholar]
- 60.Smith BW, Zautra AJ. Vulnerability and resilience in women with arthritis: test of a two-factor model. J Consult Clin Psychol 2008;76:799. [DOI] [PubMed] [Google Scholar]
- 61.Cousins LA, Cohen LL, Venable C. Risk and resilience in pediatric chronic pain: Exploring the protective role of optimism. J Pediatr Psychol 2014;40:934–942. [DOI] [PubMed] [Google Scholar]
- 62.Murphy L, Helmick CG. The impact of osteoarthritis in the United States: a population-health perspective: A population-based review of the fourth most common cause of hospitalization in U.S. adults. Orthop Nurs 2012;31:85–91. [DOI] [PubMed] [Google Scholar]
- 63.Wood AM, Brock TM, Heli K, et al. A Review on the Management of Hip and Knee Osteoarthritis. Int J Chronic Dis 2013;2013:845015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Morley S, Williams A, Hussain S. Estimating the clinical effectiveness of cognitive behavioural therapy in the clinic: evaluation of a CBT informed pain management programme. Pain 2008;137:670–680. [DOI] [PubMed] [Google Scholar]
- 65.Hofmann SG, Asnaai A, Vonk IJJ, et al. The Efficacy of Cognitive Behavioral Therapy: A Review of Meta-analyses. Cognit Ther Res 2012;36:427–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Fosnaugh J, Geers AL, Wellman JA. Giving off a rosy glow: the manipulation of an optimistic orientation. J Soc Psychol 2009;149:349–364. [DOI] [PubMed] [Google Scholar]
- 67.Peters ML, Sommer M, de Rijke JM, et al. Predictors of physical and emotional recovery 6 and 12 months after surgery. Br J Surg 2010;97:1518–1527. [DOI] [PubMed] [Google Scholar]
- 68.Sturgeon JA, Zautra AJ. Psychological resilience, pain catastrophizing, and positive emotions: perspectives on comprehensive modeling of individual pain adaptation. Curr Pain Headache Rep 2013;17:317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kitchen CMR. Nonparametric vs parametric tests of location in biomedical research. Am J Ophthalmol 2009;147:571–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York, NY: The Guilford Press, 2013. [Google Scholar]
- 71.Yarnitsky D, Bouhassira D, Drewes AM, et al. Recommendations on practice of conditioned pain modulation (CPM) testing. Eur J Pain 2015;19:805–806. [DOI] [PubMed] [Google Scholar]
- 72.Hootman JM, Helmick CG. Projections of US prevalence of arthritis and associated activity limitations. Arthritis Rheum 2006;54:226–229. [DOI] [PubMed] [Google Scholar]


