Abstract
Objective:
This was a retrospective study designed to examine the relationship between inpatient neuropsychological status and future utilization costs.
Methods:
We completed a retrospective chart review of 280 patients admitted to a large academic medical center who were referred for bedside neuropsychological evaluation. Patients were grouped based on neuropsychological recommendation regarding level of supportive needs post discharge (low, moderate, high). Level of support was used as a gross surrogate indicator of cognitive status in this heterogeneous sample. We also included patients who refused assessment. Outcome variables included time to readmission, number of emergency department visits, inpatient admissions, length of hospitalization, and total costs of hospitalizations, 30 days and 1 year following discharge.
Results:
Multivariate analysis indicated patients who refused assessment had higher inpatient service utilization (number of ED visits, number of admissions, and total cost of hospitalization) compared to those with moderate needs. Also, high needs patients had higher total cost of hospitalization at 1 year, and those with low needs used the ED more, compared to those with moderate needs.
Conclusions:
Our findings replicate prior studies linking refusal of neuropsychological evaluation to higher service utilization costs, and suggests a non-linear relationship between cognitive impairment severity and future costs for medical inpatients (different groups incur different types of costs). Results preliminarily highlight the potential utility of inpatient neuropsychological assessment in identifying patients at risk for greater hospital utilization, which may allow for the development of appropriate interventions for these patients.
Keywords: health care utilization, neuropsychological assessment, clinical neuropsychology, hospital utilization
Introduction
Since the Affordable Care Act (ACA) of 2010, the APA and its leadership have encouraged empirical studies supporting inclusion of psychologists in healthcare teams (Goodheart, 2010). Within the field of neuropsychology, even earlier in the era of healthcare reform, Prigatano and Pliskin (2003) argued for the incorporation of healthcare economics models into research demonstrating the efficacy and utility of neuropsychological services. There continues to be strong support and calls for documenting the utility of neuropsychological services in order to advance and adapt neuropsychological practice to the modern healthcare environment (Chelune, 2010; Goldstein, 2010; Kubu, Ready, Festa, Roper, & Pliskin, 2016; Prigatano & Morrone-Strupinsky, 2010; VanKirk, Horner, Turner, Dismuke, & Muzzy, 2013).
One study, VanKirk, Horner, Turner, Dismuke, and Muzzy (2013), sought to evaluate the objective value of outpatient neuropsychological evaluation through reduction in Emergency Room (ER) visits and hospitalizations in a sample of 440 US Veterans. Within-subject comparisons showed significant decreases in incidence of hospitalization and length of hospitalization in the year after outpatient neuropsychological evaluation compared to the year prior that was not attributable to age or time. Incidence of ER visits also decreased from pre to post-evaluation, though it was not significant. These findings provide preliminary evidence of the clinical and potential economic value of outpatient neuropsychological services within a medical setting (VanKirk, Horner, Turner, Dismuke, & Muzzy, 2013).
Another study completed a year later by Horner, VanKirk, Dismuke, Turner, and Muzzy (2014) on the same sample of veterans, examined whether inadequate effort was associated with increased health-care utilization. Only the subset of patients who had been administered standard validity measures were included. Of the 355 patients identified for inclusion, 283 (79.7%) showed adequate effort, and 72 (20.3%) showed inadequate effort. Analyses found inadequate effort and lack of cooperation with outpatient neuropsychological evaluation to be associated with increased health care utilization in the form of more ED visits, hospitalizations, and more days of hospitalization within the year after evaluation, compared with cooperative patients. In sum, this study showed patients who exerted inadequate effort showed greater health-care utilization in the year following evaluations (Horner, VanKirk, Dismuke, Turner, & Muzzy, 2014).
On a related note, recent studies exploring high service utilization and hospital re-admission rates (in both national and international arenas) reported cognitive impairment as an associated risk factor for higher readmission in conditions such as recently diagnosed myocardial infarction (MCI), heart failure, hepatic encephalopathy, and in ED admitted older adults (Ball, Carrington, & Stewart, 2013; Callahan et al., 2015; Saab, 2015; Deschodt et al., 2015; Sperry, Ruiz, & Najjar, 2015). Other studies directly link health status (such as cardiac status and obesity) with cognitive impairment (Stanek, et al., 2011; Gunstad, et al., 2007).
This prior research suggest greater cognitive impairment is significantly associated with greater hospital utilization, and patients who are non-compliant with neuropsychological assessment may have significantly greater hospital utilization than those who were compliant. Neuropsychologists practicing within inpatient hospital settings are well positioned to contribute to the literature regarding cognitive impairment as an associated risk factor for higher hospital readmission rates and service utilization costs (Kubu, Ready, Festa, Roper, & Pliskin, 2016). However, to date, no studies considering the utility of inpatient neuropsychological consultation have been completed.
This was a retrospective study designed to examine the relationship between inpatient neuropsychological status and future utilization costs. The present literature suggests two specific hypotheses: (1) greater cognitive impairment is significantly associated with greater hospital utilization, and (2) patients who were non-compliant with neuropsychological assessment will have significantly greater hospital utilization than those who were compliant. Of note, while all inpatient subjects selected did complete a neuropsychological evaluation of cognitive status, a surrogate indicator of cognitive status (recommended level of support upon discharge) was used to execute this research for a variety of reasons detailed below.
Methods
Research Design
This research was approved by Northwestern University Institutional Review Board. The study utilized a cross-sectional retrospective design to systematically examine electronic medical records (EMR) of 280 patients admitted to a large Midwestern academic medical center, who had suspected cognitive impairment, and were referred for inpatient neuropsychological assessment for determination of dispositional decision-making capacity and post-hospitalization needs as part of discharge planning.
Patients were ultimately grouped primarily using recommended level of post-discharge support for multiple reasons, (1) this was assumed to be a gross surrogate indicator of level of cognitive functioning for this initial exploratory report (the clinicians made recommendations regarding level of support based on cognitive status), (2) this was an easily and consistently identifiable element of most archival consultation reports, (3) grouping based on cognitive scores alone presented multiple challenges as different groups of patients were typically able to tolerate different measures (i.e. patient with severely impaired cognitive functions often could not tolerate the entire battery), and (4) archival test scores taken in isolation (outside of all highly relevant clinical and situational context considered during bedside inpatient neuropsychological evaluation) may not accurately reflect the clinical decisions made at the time of the evaluation.
Outcome analyses examined group differences in readmission rates, service utilization, and cost (emergency room visits and inpatient stays), within an initial 30-day post-hospitalization period, and a longer 1-year period.
Participants
Cases for inclusion were considered by archival record selection and identified via a combination of the Neuropsychology Service database and the EMR. Neuropsychological reports for the selected cases were reviewed to code the independent variables. Outcome variables were harvested from the EMR by the independent Electronic Data Warehouse service. Records of adult patients referred to the Neuropsychology Service for determination of decision-making capacity and dispositional recommendations between September of 2011 and April of 2015 were initially harvested for further examination (N = 329). This time frame was based on the most complete departmental record availability, and the need to allow for a full 1 year time-elapse for outcome measures at the onset of research (research began in the summer of 2016). Table 1 outlines the cases identified for exclusion.
Table 1.
Description of excluded cases
| Number Excluded | Rationale |
|---|---|
| N=15 | Primary mental illness; case referred to Psychiatry Consultation Liaison Team |
| N=15 | Repeat evaluation time <1 year |
| N=7 | No discharge recommendation provided |
| N=3 | Patient transferred to another medical facility |
| N=3 | Death prior to discharge |
| N=2 | 24/7 Palliative care upon discharge (unrelated to cognitive status) |
| N=1 (each) | Leaving against medical advice
(AMA) 24/7 Care upon discharge due to sensory limitation Erroneous medical record Unclear discharge/transfer to another country |
Of note, if subsequent evaluations were completed on the same individual greater than one year apart (for example, the same person was seen once in 2010, then again in 2014), each instance greater than one year apart was deemed a distinct consultation-outcome point in our analyses. This was a small sub-set of individuals, N=13, but as noted above (repeat consultations within 1 year), repetitive consultations are not infrequent in an inpatient medical setting. The final study sample included 280 cases.
The evaluation procedures (conducted for clinical purposes, well before this research was conceived) included a medical record review, clinical interview, bedside neuropsychological evaluation, and review of relevant diagnostic data (e.g. neuroimaging, labs). The typical battery included the Test of Premorbid Functioning (TOPF); Wechsler Adult Intelligence Scale-4th Edition (WAIS-IV) Digit Span, and Similarities subtests; the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS); Trail Making Test; Stroop Test; Verbal Fluency tests; and selected subtests of the Independent Living Scales (ILS), typically the Health and Safety Subtest. Capacity determination and estimation of post-hospitalization support needs were based on the degree of cognitive impairment and the patient’s ability to independently grasp the discharge plan as outlined by the primary team, outline a reasonable and safe discharge plan, and appreciate the risks and benefits of independent versus supported living.
Table 2 outlines the demographic characteristics of the study sample. Overall, the sample was primarily female (59.7%), Caucasian (63.5 %), and elderly (mean age = 73.4, range = 19 – 97). Table 3 details the type and percentages of medical comorbidities present across the total sample and each group. The number of medical comorbidities was coded to emulate the “number of dysfunctional bodily systems” categories used by VanKirk, Horner, Turner, Dismuke & Muzzy, 2013. Each bodily system/medical comorbidity category received a binary score of 1 or 0. The total score is the sum across all categories, and represents the number of dysfunctional bodily systems rather than a “count” of all present comorbidities. Patients had an average of four medical comorbidity categories (range = 0 – 9). One-way ANOVA and post hoc multiple comparisons revealed the low needs group to be significantly younger than the high needs (p = .002) and refusal (p = .006) group. All other demographic comparisons including chi-square for sex and race, and one-way ANOVA for total number of medical comorbidities across groups were non-significant (p>.05).
Table 2.
Descriptive statistics of the study sample
| Low Needs | Moderate Needs | High Needs | Refusal | |
|---|---|---|---|---|
| Number of patients | 40 | 39 | 125 | 76 |
| Sex [N (%)] | ||||
| Male | 16 (40%) | 15 (38.5%) | 57 (45.6%) | 28 (36.8%) |
| Female | 24 (60%) | 24 (61.5%) | 68 (54.4%) | 48 (63.2%) |
| Race [N (%)] | ||||
| Caucasian | 31 (77.5%) | 23 (59.0%) | 68 (54.4%) | 48 (63.2%) |
| African American | 8 (20%) | 12 (30.8%) | 42 (33.6%) | 25 (32.9%) |
| Other | 1 (2.5%) | 4 (10.2%) | 15 (12.0%) | 3 (3.9%) |
| Age [Median (Range)] | 63.5 (19 – 95)* | 77 (22 – 93) | 77 (22 – 97)* | 76 (29 – 93)* |
| Number of Medical Comorbidities [Median (Range)] | 4 (1 – 8) | 4 (0 – 9) | 4 (1– 9) | 5 (2– 8) |
Note. *p<.05
Table 3.
Descriptive statistics of medical comorbidities
| Total Sample [N (%)] |
Low Needs [N (%)] |
Moderate Needs [N (%)] |
High Needs [N (%)] |
Refusal [N (%)] |
|
|---|---|---|---|---|---|
| Neurological | 133 (48%) | 19 (48%) | 15 (38%) | 62 (50%) | 37 (30%) |
| Cardiovascular | 217 (78%) | 26 (65%) | 20 (74%) | 97 (78%) | 64 (52%) |
| Endocrine | 102 (36%) | 12 (30%) | 15 (38%) | 46 (37%) | 29 (23%) |
| Gastrointestinal | 49 (18%) | 5 (13%) | 7 (18%) | 16 (13%) | 21 (17%) |
| Infectious Disease/Autoimmune | 68 (24%) | 10 (25%) | 6 (15%) | 29 (23%) | 23 (18%) |
| Musculoskeletal | 76 (27%) | 5 (13%) | 6 (15%) | 36 (29%) | 29 (23%) |
| Pain | 33 (12%) | 4 (10%) | 5 (13%) | 11 (9%) | 13 (10%) |
| Pulmonary | 88 (31%) | 10 (25%) | 13 (33%) | 37 (30%) | 28 (22%) |
| Cancer | 56 (20%) | 9 (25%) | 12 (31%) | 23 (18%) | 12 (10%) |
| Sensory-Perceptual | 39 (14%) | 8 (20%) | 4 (10%) | 19 (15%) | 8 (6%) |
| Liver | 17 (6%) | 2 (5%) | 6 (15%) | 4 (3%) | 5 (4%) |
| Cognition | 66 (24%) | 10 (25%) | 10 (26%) | 37 (30%) | 9 (7%) |
| Psychiatric | 126 (45%) | 20 (50%) | 18 (46%) | 51 (41%) | 37 (30%) |
| Substance Use | 97 (35%) | 13 (33%) | 13 (33%) | 49 (39%) | 22 (18%) |
| Renal/Urogenital | 123 (44%) | 15 (38%) | 19 (49%) | 52 (42%) | 24 (19%) |
Note. Percentages rounded to nearest whole number
Table 4 outlines the guiding criteria used to make patient group assignments. Group assignment was coded by two independent raters (ES and CM). An intraclass correlation coefficient (ICC) estimate and 95% confidence interval was calculated using SPSS statistical package version 23 (SPSS Inc, Chicago, IL) based on a mean rating (k=2), consistency-agreement, 2-way random effects model. ICC = .970 with 95% confidence interval = .960-.977, indicating excellent interrater reliability. Due to a high level of interrater reliability, the first examiner’s ratings (ES) were used to complete the analysis.
Table 4.
Group criteria guidelines
| Low Needs | Moderate Needs | High Needs | Refusal | |
|---|---|---|---|---|
| Cognitive Functioning | Normal to mildly impaired cognitive function | Moderately impaired cognitive functioning | Severely impaired cognitive functioning | Unknown cognitive
functioning Only completing an interview prior to refusal; only completed 1 test, then refusing all else Failed validity testing; testing results not believed accurate due to lack of cooperation and inconsistent and intermittently insufficient test taking effort Cooperation clearly limited accurate evaluation of cognitive status |
| Cognitive Functioning Descriptor Examples | Normal cognitive status, isolated mild retrieval based memory dysfunction, slowed processing speed, mild working memory impairment | Moderate attentional, executive, memory, language impairment | Severe attentional, executive, memory, or
language impairment Global cognitive impairment |
|
| Knowledge of general health & safety concepts | Intact knowledge of general health and safety concepts | Questionable knowledge of general health and safety concepts | Poor knowledge of general health and safety concepts | |
| Ability to Manage Medical Conditions | Deficits not expected to significantly interfere with ability to manage own medical conditions | Deficits expected to interfere with ability to manage medical conditions upon discharge | Deficits expected to interfere with ability to manage medical conditions and general safety upon discharge | |
| Example of Diagnosis | No diagnosis/normal cognitive status for age, MCI (e.g MCI due to cerebrovascular disease) | Resolving encephalopathy, suspected early dementia, major neurocognitive disorder of mild or moderate severity | Likely severe major neurocognitive disorder, likely advanced dementia | |
| Capacity Determination | Retained capacity for dispositional decisions | With or without capacity for dispositional decisions | Without capacity for dispositional decisions | Capacity deferred to medical ethics/legal |
| Level of Support Recommendation | No to minimal oversight
recommended Able to care for self independently from a cognitive standpoint, or only brief weekly check-ins with family/nurse Commonly recommend independent compensatory aids such as use of an appointment book, pill box, etc. |
Significant daily assistance required for
medical management Assisted living facility, daily family help, paid help 3–4hrs/day 5 days week, Daily assistance with meals, medications |
24/7 supervisory care required for medical
management as well as general health and safety 24/7 family assistance, skilled nursing facility, locked dementia unit |
No recommendation provided |
| Additional Information | Driving restrictions, or minor assistance needed due to physical limitations were not contraindications to low needs group membership | Could not go home and live
independently Did not require full time 24/7 supervisory care |
In rare cases, gross behavioral disturbance or obscenity with examiner; unwilling/unable to engage in meaningful exchange rendering accurate assessment of cognitive status impossible |
Note. These criteria and examples are based on results as stated in archival neuropsychological reports. The examiners did not retrospectively re-analyze or re-interpret individual aspects of archival clinical data.
Outcome Variables
Time to readmission, number of emergency room visits, number of hospitalizations, aggregate length of hospitalization, and total cost of inpatient hospitalizations, served as outcome variables for this study. Total cost of inpatient hospitalizations was provided by the Electronic Data Warehouse and is the total sum of each emergency department (ED) visit and inpatient hospitalization cost incurred during the designated follow up period (eg. ED1 Cost + ED2 Cost +….Hospitalization1 cost + Hospitalization2 cost + …). The cost for each ED visit and inpatient hospitalization included all charges billed from admission to discharge. Follow up outpatient visits were not included in inpatient hospitalization cost. Analyses examined two follow-up periods (initial and extended). Because Medicare penalizes institutions for readmission within 30 days of discharge, the initial follow-up period was set at 30 days following the index hospitalization (Callahan et al., 2015). The extended follow-up period was set at one year following the index hospitalization, based on prior outpatient neuropsychological outcome studies (Horner, VanKirk, Kismuke, Turner, & Muzzy, 2014; VanKirk, Horner, Turner, Dismuke, & Muzzy, 2013). The one-year cost was the total annual cost (the above formula applied for the duration of the year).
Statistical Methods
Ten multivariate models were used to examine the association of group with time to readmission, number of ED visits, number of readmissions, length of stay, and total cost at 30 days and 1 year after the index hospitalization. Each of the models also controlled for other theoretically related variables based on literature (age, sex, race, and baseline medical comorbidity score), if found to be associated with service utilization. Time to readmission across groups was analysed using Cox Proportional Hazards Models, with separate analysis for 30 day and 1 year outcomes. Mean number of ED visits and readmissions within 30 days of discharge across groups was compared using Poisson Regression Analysis. Mean number of ED visits and readmissions within one year of discharge across groups was compared using Negative Binomial Models to accommodate for overdispersion bias. Length of stay and total cost of inpatient hospitalizations across groups for 30 day and one year outcomes were first log transformed and then analysed using General Linear Regression analysis. Statistical significance was set at alpha level of 0.05. Data were analysed using R version 3.3.2.
Results
Group statistics comparing the unadjusted means of the healthcare utilization variables are shown in Table 5, and statistically significant findings are graphically represented in Figures 1–4. Multivariate analysis indicated the moderate needs group had the lowest overall inpatient service utilization, and this group was therefore used as a reference group for subsequent analyses.
Table 5.
Unadjusted mean (SD) healthcare utilization as a function of group
| Low Needs | Moderate Needs | High Needs | Refusal | |
|---|---|---|---|---|
| Time to Readmission asrc | ||||
| 30 Days | 7.14 (6.64) | 13.29(6.24) | 11.65(8.44) | 13.25(10.32) |
| 1 year | 86.58 (93.26) | 104.41 (94.39) | 76.95 (101.52) | 83.33 (99.49) |
| Number of ED Visits asrc | ||||
| 30 Days | 0.45 (1.57)* | 0.10(0.38) | 0.04(0.20) | 0.32(0.10)* |
| 1 year | 2.63(10.44)** | 0.49(1.00) | 0.47(1.65) | 2.66(6.30)*** |
| Number of Inpatient Admissions asrc | ||||
| 30 Days | 0.38(1.10) | 0.18(0.39) | 0.30(0.54) | 0.26(0.62) |
| 1 year | 1.15(1.96) | 1.33(2.02) | 1.02(1.46) | 2.11(3.59)* |
| Length of Inpatient Stay src | ||||
| 30 Days | 6.83(5.12) | 3.38(2.67) | 7.53(5.16) | 7.00(5.21) |
| 1 year | 11.43(8.95) | 10.82(10.44) | 11.85(8.7) | 17.4(17.13) |
| Total Cost of Hospitalization src | ||||
| 30 Days | 9,170(8,071) | 5,227(3,990) | 14,008(12,836) | 13.404(16,387) |
| 1 year | 18,401 (19,715) | 19,448(23,026) | 24,050(16,939)** | 39,466(48,303)*** |
Note. *p≤.05, **p≤.01, ***p≤.001
aage, ssex, rrace, ccomorbidities (number) were included in the multivariate models as indicated by superscripts
Figure 1.
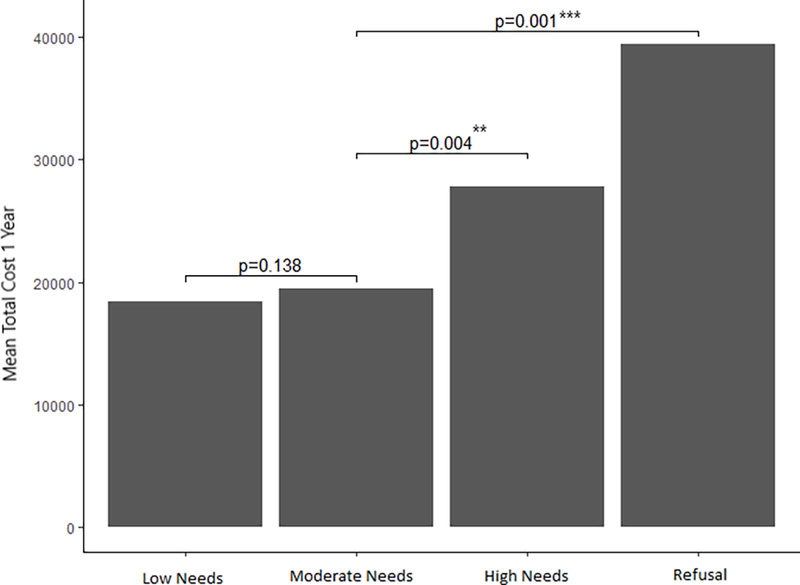
Mean Total Cost in 1 Year by Group and Their Significance
Figure 4.
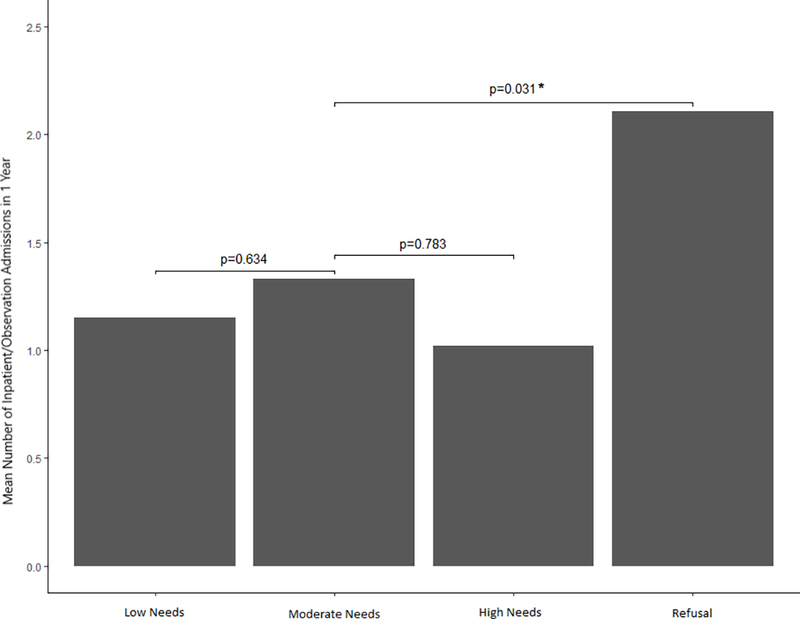
Mean Number of Inpatient/Observation Admission in 1 Year by Group and Their Significance
Compared to the moderate needs group, patients who refused assessment and the high needs group (i.e. the most cognitively impaired group), demonstrated significantly higher inpatient hospitalization costs over the extended (i.e. 1-year) follow-up period (Adjusted R2=0.176; p = .0002). Translated into dollar amounts, the average patient who refused neuropsychological evaluation incurred $39,466 in service utilization costs (p = .001), compared to $27,844 for the average high needs patient (p = .004), and $18,401 and $19,448 for the low and moderate needs patients, respectively.
Patients who refused assessment and the low needs group (i.e. those with least degree of cognitive impairment) demonstrated a higher number of ED visits across the initial and extended follow-up periods compared to the moderate needs group (Wald Test p < 0.001). Specifically, 30 days after discharge, the low needs group was on average 3.5 times more likely to visit the ED (RR = 3.69 (1.29–12.97), p = .024), and those who refused evaluation were nearly three times more likely to visit the ED (RR = 2.9 (1.11–10.06), p = .051), compared to the moderate needs group.
One year after discharge, the low needs group was on average 6.5 times more likely to visit the ED (RR = 6.46 (1.59–26.39), p = .006), and those who refused evaluation were nearly eight times more likely to visit the ED (RR = 7.80 (2.13–26.77), p = .0007), compared to the moderate needs group.
Only the refusal group demonstrated a higher number of readmissions over one year (Wald Test p<0.001), specifically being nearly twice as likely as those with moderate needs to be readmitted (RR = 1.98 (1.06–3.68), p = .031).
Time to readmission, length of inpatient stay, and the inpatient hospitalization cost over the initial 30-day post-hospitalization period did not differ significantly between patient groups.
While true level of care after discharge is not known in our sample, as a post-hoc exploration we considered the level of care as stated in the discharge notes compared to the level of care we recommended: Low Needs Group (N = 40; Discharge: Low 27, Moderate 10, High 3), Moderate Needs Group (N = 39; Discharge: Low 8, Moderate 17, High 14), High Needs (N = 125; Discharge: Low 4, Moderate 11, High 110), Refusal (N = 76; Discharge: Low 29, Moderate 4, High 43).
Discussion
Explanation of Findings
Results suggest those who refuse inpatient neuropsychological assessment have greater hospital utilization and incur higher inpatient healthcare utilization costs, compared to patients identified as moderate needs by neuropsychological evaluation. This finding replicates prior research associating poor effort on outpatient neuropsychological evaluation with higher hospital utilization (Horner, VanKirk, Dismuke, Turner, & Muzzy, 2014). This finding was consistent with our second hypothesis.
The authors agree with prior explanations for this finding put forth in the literature: (1) inadequate effort on examination may serve as a “marker” for these patient’s more general lack of full cooperation in their own healthcare, (2) due to a lack of cooperation there is reduced diagnosis clarity and therefore lack of appropriate treatment, and (3) intentional production or embellishment of symptoms leading to greater healthcare usage (Horner, VanKirk, Dismuke, Turner, & Muzzy, 2014). Also, there may be differences between inpatient and outpatients with respect to motivations to participate in neuropsychological assessment. For example, overt obstinance in the setting of relative inpatient medical stability, versus severe medical illness and feeling too ill for participation, versus refusal due to low health literacy.
Our results also suggest there is not a linear relationship between cognitive impairment severity and future costs for inpatients, and those with high needs and those with low needs incur greater costs on different variables relative to those who fall in the middle. More specifically, those with low needs incur higher ED costs, and those with high needs incur higher inpatient hospitalization costs, relative to those whose needs fall in the middle. This finding was contradictory to our first hypothesis.
One possible explanation for the moderate needs group having the lowest readmission and service utilization rates is they may be more likely to be discharged to a higher level of care than recommended, thereby facilitating medical stability (40% of our moderate needs sample was actually discharged to a high level of care per post-hoc analysis). Low needs patients may be able to recognize the need for medical attention, prior to their conditions becoming destabilized to a point that necessitates admission and more intensive treatment, but resulting in higher ED utilization. We suspect patients with high needs (and severely impaired cognitive status) may tend to undergo extensive neurologic work up at each admission (e.g. MRI, neurology consultation, psychiatry consultation) contributing to mounting costs.
Future Studies
For those who refuse inpatient assessment, future studies may wish to further clarify the nature and type of inpatient refusal (e.g. feeling too ill, obstinance, low health literacy), and consider other aspects of their hospitalization or medical history to find targets of intervention and prevention of high service utilization in this population. For the low needs patients, future studies might further clarify the nature and type of ED usage. It may be possible to develop a metric to describe “false-alarm” versus “accurate” ED use (patients who receive necessary brief treatment and are sent home) to further understand this higher relative cost. For all groups (but of most interest for the moderate and high needs groups), the examiners plan to conduct a future study examining if there is any effect of whether our recommendations were followed on later hospital utilization.
Potential Interventions
Specifically given our findings, post-discharge interventions for the more cognitively intact patients may be aimed at reducing the number of ED visits via closer primary care physician (PCP) follow-up immediately after discharge and throughout the following year. Similarly, early identification and intervention for individuals with poor medication compliance and resistance to treatment may possibly reduce the development of more profuse maladaptive refusal behaviors in the future. Extrapolations may be considered from the psychological literature regarding ways to therapeutically handle resistance or symptom exaggeration. However, caution and possible ethical consideration is imperative given the acute health needs and risks to health/life at the time of medical admission.
Generally, the known potential impact of neurologic, cardiac, psychiatric, and renal comorbidities on cognitive function (and the high prevalence of these comorbidities in our sample) may suggest individuals with these comorbidities should be screened for cognitive impairment at regular intervals. A simple screening measure such as the Montreal Cognitive Assessment (MoCA; Nasreddine et al., 2005) could be used.
The primary care behavioral health model of collaboration may be a helpful model to emulate, offering in-office screenings and consultations and more extensive outpatient evaluations and services as needed. A primary care behavioral health model has shown effectiveness in improving patient outcomes and reducing healthcare costs in comorbidities of depression, obesity, and diabetes among others (Conejo-Ceron et al., 2017; Trickett, Matiaco, Jones, Howlett, & Early, 2016). Integration of neuropsychological services in primary care settings may foster greater medical stability, reduce hospital utilization, and reduce overall healthcare costs for patients with multiple medical comorbidities.
Limitations
Specifically regarding this study, our ability to detect significant group differences may have been limited by insufficient power. Future large-scale studies or meta-analyses may be able to detect finer differences in hospital utilization. Also, the generalizability of our findings may have been negatively affected by several factors. Firstly, our group classification strategy was based on case-by-case clinical decision-making as opposed to a standardized scheme. Secondly, we only examined inpatient service utilization costs and did not consider cost of outpatient medical follow up and medication usage. Thirdly, we were not able to capture ED visits and hospitalizations outside our health system. Fourthly, we did not directly consider the impact of education on our results. While education is corrected for, and taken into account in the archival clinical process we considered, we did not directly control for this variable in our outcomes.
More generally, the study of the inpatient neuropsychological population is presently limited by the characterization of medical comorbidities. The present neuropsychological literature to-date (including this study) utilizes a crude “number of dysfunctional systems” proxy. More elegant models of medical comorbidities such as the Charlson index, Elixhauser comborbidity measure, or comorbidity-polypharmacy score may be helpful to consider with regards to relevance in neuropsychological research (Charlson, Pompei, Ales, & MacKenzie, 1987; Elixhauser Steiner, Harris, Coffey, 1998; Justiniano, et al., 2013). Also, there is presently no precedent, or consensus regarding inclusion/exclusion of repeat cases who belong to a notorious “revolving door” group of inpatients seen multiple times within a year, or at regular intervals for consecutive years. This high-repeat group may likely have its own unique needs but this has not been explored or validated from a neuropsychological standpoint.
Conclusions
Overall, our findings replicate prior research linking lack of cooperation with neuropsychological evaluation with higher service utilization costs, suggests a non-linear relationship between cognitive impairment severity and future costs for medical inpatients (different groups incur different types of costs, indicating a multivariate nature), extend prior findings to include acute medical inpatient settings, and offer more direct examination of post-hospitalization fiscal impact by analyzing the actual accrued costs as opposed to a national average estimate. Our findings demonstrate the potential utility of neuropsychological evaluation in identifying groups of patients at increased risk for greater hospital utilization. We hope these results, along with the growing body of literature highlighting the importance of neuropsychological services within healthcare systems, emphasize the need for further integration of neuropsychological services within both inpatient and outpatient medical care settings.
Figure 2.
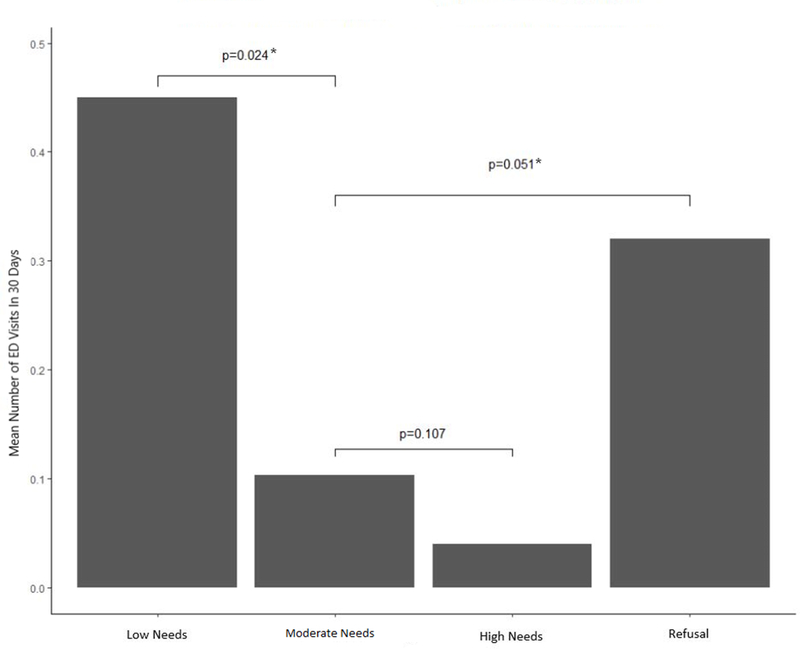
Mean Number of ED Visits in 30 Days by Group and Their Significance
Figure 3.
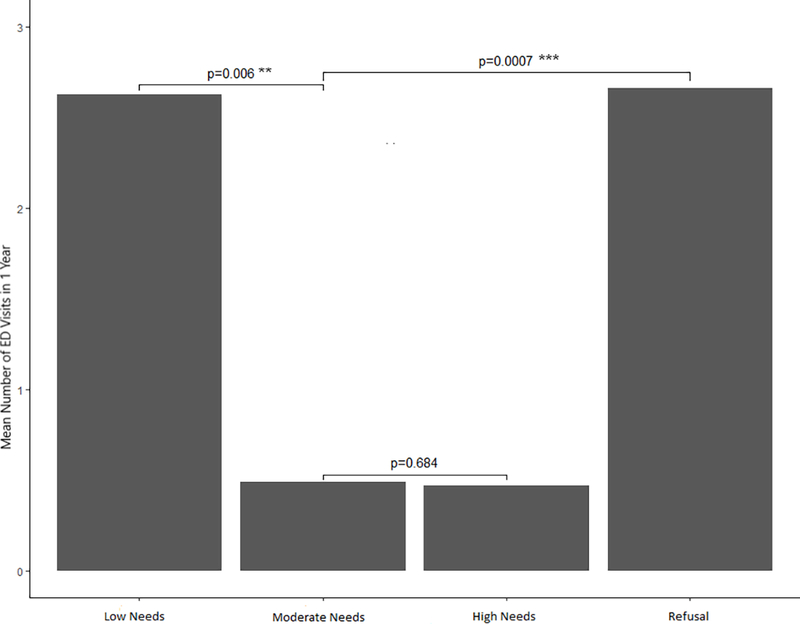
Mean Number of ED Visits in 1 Year by Group and Their Significance
Acknowledgments
The authors would like to acknowledge the work of Allison Hechtman, a volunteer undergraduate student who assisted greatly with records review and data coding during a brief summer internship.
Funding
Research reported in this publication was supported, in part, by the National Institutes of Health’s National Center for Advancing Translational Sciences (Grant Number UL1TR001422) and the Northwestern Medicine Enterprise Data Warehouse (NMEDW). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest
The authors have nothing to disclose and report no conflicts of interest.
References
- Ball J, Carrington MJ, & Stewart S (2013). Mild cognitive impairment in high-risk patients with chronic atrial fibrillation: a forgotten component of clinical management. Heart, 99, 542–547. [DOI] [PubMed] [Google Scholar]
- Callahan KE, Lovato JF, Miller ME, Easterling D, Snitz B, & Williamson JD (2015). Associations of Mild Cognitive Impairment with Hospitalization and Readmission. J Am Geriatric Soc., 63(9), 1880–1885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlson ME, Pompei P, Ales KL, & MacKenzie CR (1987). A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis, 40(5), 373–83. [DOI] [PubMed] [Google Scholar]
- Chelune GJ (2010). Evidence-based research and practice in clinical neuropsychology. The Clinical Neuropsychologist, 24, 454–467. [DOI] [PubMed] [Google Scholar]
- Conejo-Cerón S, Moreno-Peral P, Rodriguez-Morejón A, Motrio E, Navas-Campaña D,…Bellón JA (2017). Effectiveness of Psychological and Educational Interventions to Prevent Depression in Primary Care: A Systematic Review and Meta Analysis. Ann Fam Med, 15(3), 262–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deschodt M, Devriendt E, Sabbe M, Knockaert D, Deboutte P, Boonen S, Flamaing J, & Milisen K (2015). Characteristics of older adults admitted to the emergency department (ED) and their risk factors for ED readmission based on comprehensive geriatric assessment: a prospective cohort study. BMC Geriatrics, 15(54). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elixhauser A, Steiner C, Harris DR, & Coffey RM (1998). Comorbidity measures for use with administrative data. Med Care, 36, 8–27. [DOI] [PubMed] [Google Scholar]
- Garland A, Ramsey CD, Fransoo R, Olafson K, Chateau D, Yogendran M, & Kraut A (2013). Rates of readmission and death associated with leaving hospital against medical advice: a population-based study. Canadian Medical Association, 185(14), 1207–1214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein G (2010). Advocacy for neuropsychology in the public sector: the VA experience. The Clinical Neuropsychologist, 24, 401–416. [DOI] [PubMed] [Google Scholar]
- Goodheart CD (2010). Economics and Psychology Practice: What We Need To Know and Why. Professional Psychology: Research & Practice, 41(3), 189–195. [Google Scholar]
- Gunstad J, Paul RH, Cohen RA, Tate DF, Spitznagel MB, & Gordon E (2007). Elevated body mass index is associated with executive dysfunction in otherwise healthy adults. Comprehensive Psychiatry, 48, 57–61. [DOI] [PubMed] [Google Scholar]
- Horner MD, VanKirk KK, Dismuke CE, Turner TH, & Muzzy W (2014). Inadequate Effort on Neuropsychological Evaluation is Associated With Increased Healthcare Utilization. The Clinical Neuropsychologist, 28(5), 703–713. [DOI] [PubMed] [Google Scholar]
- Justiniano CF, Evans DC, Cook CH, Eiferman DS, Gerlach AT, Beery PR,…Stawicki SPA (2013). Comorbidity-Polypharmacy Score: A Novel Adjunct In Post-Emergency Department Trauma Triage. J Surg Res, 181(1), 16–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubu CS, Ready RE, Festa JR, Roper BL, Pliskin NH (2016). The Times They Are a Changin’: Neuropsychology and Integrated Care Teams. The Clinical Neuropsychologist, 30(1), 51–65. [DOI] [PubMed] [Google Scholar]
- Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S, Whitehead V, Collin I,Cherthkow H (2005). The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc, 53(4), 695–9. [DOI] [PubMed] [Google Scholar]
- Prigatano GP (2003). Health-care economics and clinical neuropsychology In Prigatano GP & Pliskin NH (Eds.), Clinical neuropsychology and cost outcomes research (pp. 1–14). New York, NY: Psychology Press. [Google Scholar]
- Prigatano GP, & Morrone-Strupinksy J (2010). Advancing the profession of clinical neuropsychology with appropriate outcome studies and demonstrated clinical skills. The Clinical Neuropsychologist, 24, 468–480. [DOI] [PubMed] [Google Scholar]
- R Core Team (2014). R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria, URL http://www.R-project.org/.
- Saab S (2015). Evaluation of the impact of rehospitalization in the management of hepatic encephalopathy. International Journal of General Medicine, 8, 165–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southern WN, Nahvi S, & Arnsten JH (2012). Increased Risk of Mortality and Readmission Among Patients Discharged Against Medical Advice. Am J Med, 125(6), 594–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sperry BW, Ruiz G, Najjar SS (2015). Hospital readmission in heart failure, a novel analysis of a long standing problem. Heart Failure Review, 20, 251–258. [DOI] [PubMed] [Google Scholar]
- Stanek KM, Gunstad J, Spitznagel MB, Waechter D, Hughes JW, Luyster F, Rosneck J (2011). Improvements in cognitive functioning following cardiac rehabilitation for older adults with cardiovascular disease. Int J Neurosi., 121(2), 86–93. [DOI] [PubMed] [Google Scholar]
- Sullivan K (2004). Neuropsychological Assessment of Mental Capacity. Neuropsychology Review, 14(3), 131–142. [DOI] [PubMed] [Google Scholar]
- Trickett KH, Matiaco PM, Jones K, Howlett B, & Early KB (2016). Effectiveness of Shared Medical Appointments Targeting the Triple Aim Among Patients With Overwieght, Obesity, or Diabetes. J Am Osteopath Assoc, 116(12), 780–787. [DOI] [PubMed] [Google Scholar]
- VanKirk K, Horner MD, Turner TH, Dismuke CE, & Muzzy W (2013). Hospital Service Utilization is Reduced Following Neuropsychological Evaluation in a Sample of U.S. Veterans. The Clinical Neuropsychologist, 27(5), 750–761. [DOI] [PubMed] [Google Scholar]


