Abstract
[Purpose] This study aimed to examine the effect of core stabilization exercise (CSE) on joint position sense, pain intensity, and functional disability in patients with subacute non-specific low back pain (NSLBP). [Participants and Methods] Thirty-eight participants with subacute nonspecific low back pain of 6–12 weeks duration, aged 18–60 years, were included in this study. Participants were randomly divided into two groups: a core stabilization exercise group (n=19) or a control group (n=19). Outcomes measures included lumbar joint repositioning error (LJRE), numeric pain rating scale (11-NRS), and the Roland-Morris disability questionnaires (RMDQ). Measures were taken at baseline, 4 weeks, 7 weeks of intervention, and at 4 weeks after the last intervention. [Results] All outcomes measures were significantly improved in the core stabilization exercise group, compared with the control group. [Conclusion] Core stabilization exercise can improve acuity of joint position sense, reduce pain, and functional disability compared with thermal therapy. The finding demonstrated that core stabilization exercises are more suitable for patients with subacute NSLBP than thermal therapy and this should be useful to clinicians.
Keywords: Low back pain, Exercise, Joint sense
INTRODUCTION
Low back pain (LBP) is the most common musculoskeletal disorder and is a costly problem1). More than 90% of LBP cases are classified as non-specific low back pain (NSLBP) because the precise cause is unclear2, 3). Impaired local trunk muscle activation and reduced proprioceptive acuity in patients with LBP may alter muscle recruitment patterns which may cause motor control dysfunction and more compressive load to the spine, resulting in recurrent LBP4). A possible hypothesis is that changes in motor planning, via the direct influence of pain on the motor centers, compromise feedback control and lead to poor lumbar joint position sense4,5,6).
In subacute NSLBP, disrupted afferent information may alter local trunk muscle activation and cause poor joint position sense7,8,9) which in turn leads to repeated microtrauma and recurrent pain. Systematic reviews of randomized controlled trials in patients with subacute LBP conclude that active exercise is effective in managing this disorder10). Extension and flexion exercises are the most widely used to reduce pain and disability11,12,13). However, these exercises may not address lumbar joint position sense, which is a key problem in subacute NSLBP. Research guidelines recommend core stabilization exercise (CSE) as a commonly used treatment strategy for chronic LBP14,15,16,17,18,19). CSE involves the activation and training of deep core muscles transversus abdominis (TrA) and lumbar multifidus (LM), with minimal activity of the superficial muscles19,20,21,22,23). Low-threshold recruitment of local and global muscle systems is important to provide modulation of the CNS for efficient motor integration of the muscles and may enhance joint position sense24,25,26). However, to our knowledge, the effect of CSE as an active treatment on lumbar joint position sense in patients with subacute NSLBP has never been explored.
The purpose of this study was to investigate the effect of CSE on lumbar joint position sense, pain intensity, and functional disability in patients with subacute NSLBP. We hypothesized that CSE might be an appropriate therapeutic exercise to provide clinical benefits in patients with subacute NSLBP.
PARTICIPANTS AND METHODS
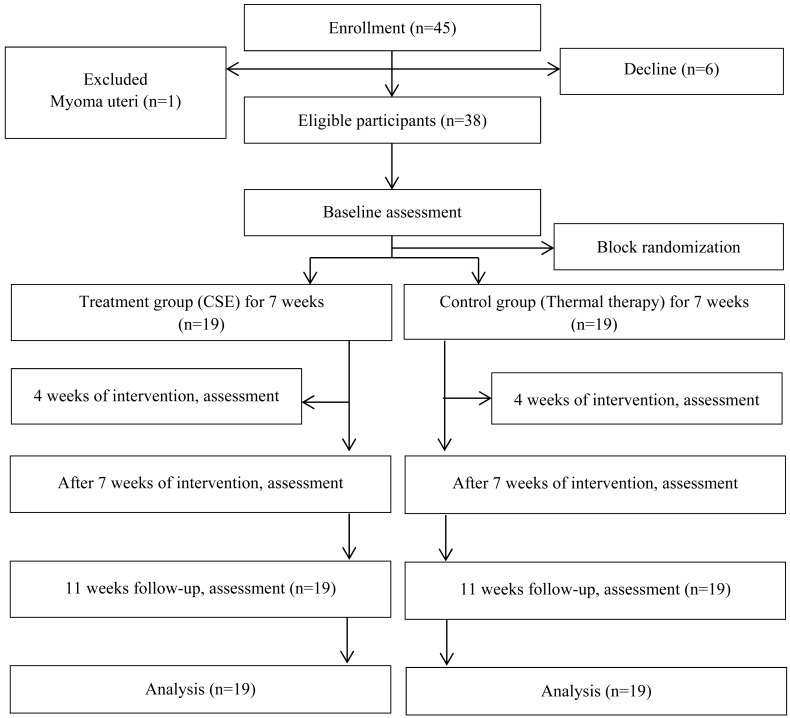
This study was an assessor-blinded, randomized controlled trial. Participants were recruited from the physical therapy clinic, Khon Kaen University, through advertisements on social networks. The study protocol was approved by the Ethics Committee for Human Research at Khon Kaen University, Thailand (Reference number: HE572309) and registered at clinicaltrials.gov (Registration number: NCT02645760).
Participants with subacute NSLBP of between 6 to 12 weeks duration, aged between 18 and 60 years; mean age 38.76 ± 10.3 years, weight 60.71 ± 10.5 kg and height 157.42 ± 8.1 cm, and had a pain intensity of at least 3 out of 10 on an 11-point numeric rating scale (11-NRS) were included. Exclusion criteria were spinal surgery, suspected serious spinal abnormality, or pregnancy. A prior sample size was estimated based on the joint reposition sense at 1-month follow-up, and assuming 80% power and 5% significance. A total of 38 participants was required to detect a clinically meaningful difference of 0.4 cm on the joint reposition sense between the groups from our pilot study.
Participants were initially screened using an interview. Written informed consent was obtained from all participants before they enrolled in the study and received a physical examination. Lumbar joint position sense, pain intensity, and functional disability were measured by an assessor who was blinded to group allocation and treatment, at baseline, after 4 and 7 weeks of intervention, and at 11 weeks follow-up.
After performing pre-test assessments, participants were randomly allocated to either the CSE group or control group and stratified by age group to achieve an approximate balance between groups. Random numbers were computer generated and kept in sealed envelopes with consecutive numbering. The randomization process was performed by an assistant researcher.
All participants were treated by physiotherapists for 20 minutes a session, twice per week for 7 weeks in the Physical Therapy Laboratory, Khon Kaen University, Thailand. They were requested not to participate in any other physical programs, and to record drugs and any side effects of the intervention in a diary log book during the study.
Participants in the CSE group were supervised to perform exercises based on criteria recommended by Puntumetakul and coworkers19). CSE activates transversus abdominis (TrA) and lumbar multifidus (LM) muscles. In week 1–2, the researcher trained the participants how to contract TrA and LM muscles simultaneously with an abdominal drawing-in maneuver (ADIM) technique in low load positions of the spine (lying). Exercises in week 3–7 focused on increasing the precision and duration of co-contraction of the 2 muscles with controlled movements of upper and lower extremities and progressed to high load positions (sitting, standing). The program consisted of 10 repetitions with 10-second holds in each repetition. All participants were asked to perform home exercises for 15 minutes every day and record them in their diary. Exercise performance was re-assessed at each session to determine whether the participants could successfully perform the exercises.
Thermal therapy, hydrocollator and therapeutic ultrasound are the standard treatment widely used for LBP management in Thailand27). These are effective in alleviating the pain and disability in patients with LBP and were used in the second intervention group in this study. Participants in the control group received 5 minutes of therapeutic ultrasound using a 1-MHz ultrasound frequency with an intensity of 0.8–1.0 W/cm2 on continuous mode (Enraf Nonius Sonoplus 434, ENRAF, Netherlands). After that, each of the participants received 15 minutes of heat via a hydrocollator pack (60°C) (Enraf-Nonius Medical Equipment Company Ltd., Bangkok, Thailand), which was placed over the painful area of the lower back in a prone lying position (Fig. 1).
Fig. 1.
Flow of participants through the study.
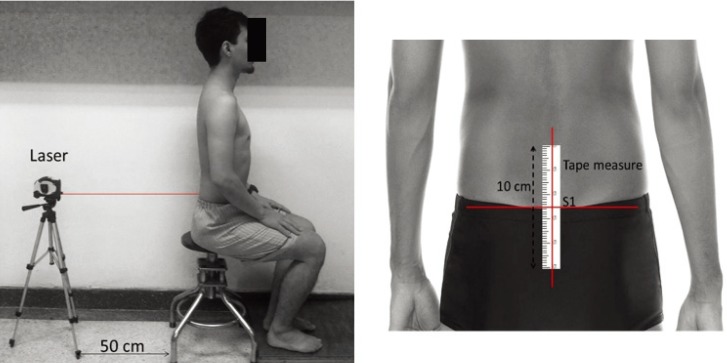
Joint repositioning sense was used to assess the lumbar joint repositioning error. All participants sat with feet supported, hips and knees flexed 90 degrees. A 10-cm tape measure was placed on the lower lumbar area with the 0 cm of tape measure marking on the sacral segment 1 (S1), as the start point of measure and marked by a stable based (tripot) laser pointer Fig. 2. Each participant was asked to remember the starting position (neutral position) and maintain it for 5 seconds, then to move their pelvis from the maximum anterior to the maximum posterior tilt, maintain each position for 5 seconds, and return to the starting position. With the laser point on the tape-measure, the distance from the starting point (repositioning error) was measured in centimeters. Participants were allowed to practice twice before the examination started. The test was performed 3 times using rest intervals of 1 minute, and the average values were used for the analysis.
Fig. 2.
Measurement positioning for joint repositioning error.
The 11-NRS was used to assess the current, minimum, and maximum levels of pain intensity at rest28, 29) and the Thai version of the Roland-Morris disability questionnaire (RMDQ) was used to assess LBP-related functional disability30, 31).
SPSS version 21.0 for Windows (IBM Corp., Armonk, NY, USA) was used to analyze data. Normality of the data was calculated with the Shapiro-Wilk test. Nonparametric statistics were used to analyze outcome variables as the data were not normally distributed. The Mann–Whitney test was used to analyze differences between groups separately at each time point and the change in scores for each outcome variable. Friedman’s analysis of variance (ANOVA) was used to compare continuous outcome variables between baseline and at each time point in both groups. In this study, the significant level was set at p<0.05.
RESULTS
All demographic data and baseline clinical characteristics were equally balanced between the groups (p>0.05); (Table 1).
Table 1. Baseline demographic and clinical characteristics of the participants.
| Characteristics | Total (n=38) |
Treatment group (CSE) (n=19) |
Control group (n=19) |
p-value |
|---|---|---|---|---|
| Female gender, n (%) | 34 (89.5) | 16 (84.2) | 18 (94.7) | |
| Age (years) | 38.8 ± 10.3 | 39.6 ± 10.3 | 37.9 ± 10.6 | 0.661 |
| Height (cm) | 157.4 ± 8.1 | 157.9 ± 9.4 | 156.9 ± 6.8 | 0.696 |
| Weight (kg) | 60.7 ± 10.5 | 62.3 ± 9.9 | 59.1 ± 11.0 | 0.353 |
| Body mass index (kg/m2) | 24.5 ± 3.7 | 24.9 ± 3.1 | 24.0 ± 4.3 | 0.443 |
| Low back pain duration (weeks) | 8.4 ± 2.5 | 8.3 ± 2.4 | 8.4 ± 2.5 | 0.943 |
Values are presented as the mean ± SD; Age, Height, Weight, BMI, Body mass index and Low back pain duration.
The CSE group had significantly reduced joint repositioning error, compared with the control group at 7 weeks of intervention (p=0.048) and at 4-week follow-up periods (p<0.001) with the effect size 0.628 and 1.421, respectively.
In addition, at 4 weeks of the intervention, 7 weeks of the intervention, and at 4-week follow-up, CSE group more significantly reduced pain intensity at rest than the control group (p<0.001) with the effect size 1.465, 1.755 and 2.269, respectively and functional disability (p<0.001) with the effect size 1.171, 0.997 and 1.157, respectively.
These results illustrated that the treatment group had a significant decrease in lumbar joint repositioning error, pain intensity at rest, and functional disability from baseline to each follow-up period, respectively. However, the control group recorded no significant changes of lumbar joint repositioning error from baseline at each follow-up period. For other outcome variables, pain intensity at rest and functional disability, a significant reduction occurred in both treatment and control groups from baseline to each follow-up (p<0.001). The mean and standard deviation (SD) of comparisons between the treatment group and the control group for all outcome variables are shown in Table 2.
Table 2. Comparison of treatment group (n=19) and control group (n=19) on lumbar joint repositioning error, pain intensity at rest and functional disability.
| Variables | Mean ± Standard deviation | Mean differences between groups | p-value (between group) | ||
|---|---|---|---|---|---|
| Treatment group (CSE) | Control group | ||||
| Lumbar joint repositioning error (LRPE) (cm) | |||||
| Baseline | 0.8 ± 0.4 | 0.6 ± 0.4 | 0.2 | 0.109 | |
| 4 weeks of intervention | 0.6 ± 0.3† | 0.7 ± 0.4 | −0.1 | 0.659 | |
| 7 weeks of intervention | 0.4± 0.3† | 0.7 ± 0.4 | −0.2 | 0.048* | |
| 4-week follow-up | 0.4 ± 0.2† | 0.7 ± 0.3 | −0.4 | <0.001** | |
| Pain intensity at rest (0–10 NRS) (scores) | |||||
| Baseline | 5.1 ± 0.9 | 5.4 ± 1.4 | −0.3 | 0.560 | |
| 4 weeks of intervention | 2.1 ± 1.8† | 4.6 ± 1.6† | −2.5 | <0.001** | |
| 7 weeks of intervention | 1.3 ± 1.8†† | 3.6 ± 1.6† | −2.3 | 0.001* | |
| 4-week follow-up | 0.7 ± 0.9†† | 3.9 ± 1.8† | −3.2 | <0.001** | |
| Functional disability (RMDQ) (scores) | |||||
| Baseline | 6.8 ± 4.3 | 8.8 ± 5.3 | −2.0 | 0.246 | |
| 4 weeks of intervention | 2.4 ± 2.9†† | 6.8 ± 4.5† | −4.4 | 0.001* | |
| 7 weeks of intervention | 1.5 ± 2.3†† | 4.9 ± 4.2†† | −3.4 | 0.001* | |
| 4-week follow-up | 0.8 ± 1.6†† | 4.0 ± 3.5† | −3.2 | 0.001* | |
For between group *Significant different at p<0.05, **Significant different at p<0.001. For within group †Significant different at p<0.05, ††Significant different at p<0.001.
DISCUSSION
The results of the study showed that the CSE group had significant improvements in lumbar repositioning sense, reduced pain intensity at rest, and functional disability compared with the control group at all measurement time points. Lumbar joint repositioning error significantly reduced after intervention and at 11 weeks follow-up in the CSE group, whereas, it increased in the control group in post training assessment. This suggests that lumbar joint reposition sense deteriorates in patients with subacute NSLBP who do not exercise their core muscles. CSE may also have a retaining effect on improving lumbar joint position sense. As increases in muscle activity stimulate muscle spindles and joint receptors; the accuracy of the sensory integration procedure is enhanced empowering precise joint repositioning26).
In the present study, the CSE program decreased resting pain intensity and functional disability in patients with subacute NSLBP. Improved function increases patients’ ability to complete activities of daily living. Although physical modalities (Ultrasound and thermal therapy) given to the control group also reduced their pain and functional disability, CSE has more clinical advantages to improve subacute NSLBP. CSE may enhance activation of local trunk muscles and improve coordination of the trunk muscles, which is important for improving the stability of the lumbar segment and reducing spinal overload. Based on our findings, we recommend that patients with subacute NSLBP should receive CSE rather than passive treatment (US and thermal therapy) to reduce pain intensity. There were no adverse effects found in either groups during the study.
The findings of the study also concluded that a moderate correlation was observed between disability and pain in patients with subacute NSLBP in CSE group at 4 weeks of intervention (r=0.506) (p=0.027), and at 7 weeks of intervention (r=0.647) (p=0.003), but no correlation was found at 4-week follow-up. In the control group, no correlation was found in every time point of assessment.” This result is similar to data reported by Roland and Morris31) and Hides and colleagues32) who examined the relationship between pain and back disability in patients with acute LBP. Enhancing back movement performance and improvement in joint reposition sense may also improve functional disability. The ability to hold a co-contraction pattern between TrA and LM muscles may develop specific motor control and help to restore kinesthetic awareness and lumbo-pelvic position sense. Our study confirms that the CSE program, especially the first stage of the program, could improve lumbar joint reposition sense impairment in patients with subacute NSLBP.
Although NSLBP has unknown causes, previous studies suggested that motor control deficits may reduce lumbar joint reposition sense and this may cause repeated micro-trauma and recurrence of LBP. Alternatively, pain may lead to changes in motor control. Possible mechanisms have been proposed that pain may affect motor control and change motor planning via the direct influence of pain on the motor centers. It can be surmised that all of these problems lead to poor lumbar joint position sense4, 5).
The effect size of the present study between treatment and control groups is 1.421, and this effect size demonstrates that statistically significant effects between groups. The sample size (n=19) per group in this study was sufficient to address the existing knowledge gap. Although the between-group mean difference on the joint reposition sense was 0.35 cm and less than clinically meaningful difference (0.4 cm) set from our pilot study, it had high statistically significant difference and effects size. Thus, we believe that these changes are likely to reach clinical significance. In addition, the minimal detectable change on the joint reposition sense in the previous study was 0.24 cm (Enoch et al.)33). Therefore, the mean different found from our study may be useful for clinical relevance. A limitation of this study was that muscle activity was not assessed directly, such as with electromyography (EMG), further studies are required to measure the effect of CSE on trunk muscles activity.
CSE is effective in patients with subacute NSLBP in improving acuity of lumbar joint position sense, improving functional ability and decreasing pain, and provides clinicians with a useful treatment intervention.
Conflict of interest
None.
Acknowledgments
The authors thank the participants for their willingness to partake in this study and BNOJPH, Research Center in Back, Neck, Other Joint Pain and Human Performance, Khon Kaen University, Khon Kaen, Thailand.
REFERENCES
- 1.Woolf AD, Pfleger B: Burden of major musculoskeletal conditions. Bull World Health Organ, 2003, 81: 646–656. [PMC free article] [PubMed] [Google Scholar]
- 2.Deyo RA, Mirza SK, Martin BI: Back pain prevalence and visit rates: estimates from U.S. national surveys, 2002. Spine, 2006, 31: 2724–2727. [DOI] [PubMed] [Google Scholar]
- 3.Ehrlich GE: Low back pain. Bull World Health Organ, 2003, 81: 671–676. [PMC free article] [PubMed] [Google Scholar]
- 4.O’Sullivan PB, Burnett A, Floyd AN, et al. : Lumbar repositioning deficit in a specific low back pain population. Spine, 2003, 28: 1074–1079. [DOI] [PubMed] [Google Scholar]
- 5.Brumagne S, Cordo P, Lysens R, et al. : The role of paraspinal muscle spindles in lumbosacral position sense in individuals with and without low back pain. Spine, 2000, 25: 989–994. [DOI] [PubMed] [Google Scholar]
- 6.Luoto S, Taimela S, Alaranta H, et al. : Psychomotor speed in chronic low-back pain patients and healthy controls: construct validity and clinical significance of the measure. Percept Mot Skills, 1998, 87: 1283–1296. [DOI] [PubMed] [Google Scholar]
- 7.Solomonow M: Sensory-motor control of ligaments and associated neuromuscular disorders. J Electromyogr Kinesiol, 2006, 16: 549–567. [DOI] [PubMed] [Google Scholar]
- 8.Hodges PW, Richardson CA: Inefficient muscular stabilization of the lumbar spine associated with low back pain. A motor control evaluation of transversus abdominis. Spine, 1996, 21: 2640–2650. [DOI] [PubMed] [Google Scholar]
- 9.Leinonen V, Kankaanpää M, Luukkonen M, et al. : Lumbar paraspinal muscle function, perception of lumbar position, and postural control in disc herniation-related back pain. Spine, 2003, 28: 842–848. [PubMed] [Google Scholar]
- 10.Hayden JA, van Tulder MW, Malmivaara AV, et al. : Meta-analysis: exercise therapy for nonspecific low back pain. Ann Intern Med, 2005, 142: 765–775. [DOI] [PubMed] [Google Scholar]
- 11.Cherkin DC, Deyo RA, Battié M, et al. : A comparison of physical therapy, chiropractic manipulation, and provision of an educational booklet for the treatment of patients with low back pain. N Engl J Med, 1998, 339: 1021–1029. [DOI] [PubMed] [Google Scholar]
- 12.Miller ER, Schenk RJ, Karnes JL, et al. : A comparison of the McKenzie approach to a specific spine stabilization program for chronic low back pain. J Manual Manip Ther, 2005, 13: 103–112. [Google Scholar]
- 13.Davies JE, Gibson T, Tester L: The value of exercises in the treatment of low back pain. Rheumatol Rehabil, 1979, 18: 243–247. [DOI] [PubMed] [Google Scholar]
- 14.Costa LO, Maher CG, Latimer J, et al. : Motor control exercise for chronic low back pain: a randomized placebo-controlled trial. Phys Ther, 2009, 89: 1275–1286. [DOI] [PubMed] [Google Scholar]
- 15.França FR, Burke TN, Caffaro RR, et al. : Effects of muscular stretching and segmental stabilization on functional disability and pain in patients with chronic low back pain: a randomized, controlled trial. J Manipulative Physiol Ther, 2012, 35: 279–285. [DOI] [PubMed] [Google Scholar]
- 16.França FR, Burke TN, Hanada ES, et al. : Segmental stabilization and muscular strengthening in chronic low back pain: a comparative study. Clinics (Sao Paulo), 2010, 65: 1013–1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Javadian Y, Behtash H, Akbari M, et al. : The effects of stabilizing exercises on pain and disability of patients with lumbar segmental instability. J Back Musculoskeletal Rehabil, 2012, 25: 149–155. [DOI] [PubMed] [Google Scholar]
- 18.Koumantakis GA, Watson PJ, Oldham JA: Trunk muscle stabilization training plus general exercise versus general exercise only: randomized controlled trial of patients with recurrent low back pain. Phys Ther, 2005, 85: 209–225. [PubMed] [Google Scholar]
- 19.Puntumetakul R, Areeudomwong P, Emasithi A, et al. : Effect of 10-week core stabilization exercise training and detraining on pain-related outcomes in patients with clinical lumbar instability. Patient Prefer Adherence, 2013, 7: 1189–1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Panjabi MM: The stabilizing system of the spine. Part I. Function, dysfunction, adaptation, and enhancement. J Spinal Disord, 1992a, 5: 383–389, discussion 397. [DOI] [PubMed] [Google Scholar]
- 21.Panjabi MM: The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis. J Spinal Disord, 1992b, 5: 390–396, discussion 397. [DOI] [PubMed] [Google Scholar]
- 22.O’Sullivan PB, Twomey L, Allison GT: Altered abdominal muscle recruitment in patients with chronic back pain following a specific exercise intervention. J Orthop Sports Phys Ther, 1998, 27: 114–124. [DOI] [PubMed] [Google Scholar]
- 23.Cresswell AG, Oddsson L, Thorstensson A: The influence of sudden perturbations on trunk muscle activity and intra-abdominal pressure while standing. Exp Brain Res, 1994, 98: 336–341. [DOI] [PubMed] [Google Scholar]
- 24.Boucher JA, Preuss R, Henry SM, et al. : The effects of an 8-week stabilization exercise program on lumbar movement sense in patients with low back pain. BMC Musculoskelet Disord, 2016, 17: 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kong YS, Cho YH, Park JW: Changes in the activities of the trunk muscles in different kinds of bridging exercises. J Phys Ther Sci, 2013, 25: 1609–1612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kong YS, Jang GU, Park S: The effects of prone bridge exercise on the Oswestry disability index and proprioception of patients with chronic low back pain. J Phys Ther Sci, 2015, 27: 2749–2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pensri P, Foster NE, Srisuk S, et al. : Physiotherapy management of low back pain in Thailand: a study of practice. Physiother Res Int, 2005, 10: 201–212. [DOI] [PubMed] [Google Scholar]
- 28.Mannion AF, Balagué F, Pellisé F, et al. : Pain measurement in patients with low back pain. Nat Clin Pract Rheumatol, 2007, 3: 610–618. [DOI] [PubMed] [Google Scholar]
- 29.Williamson A, Hoggart B: Pain: a review of three commonly used pain rating scales. J Clin Nurs, 2005, 14: 798–804. [DOI] [PubMed] [Google Scholar]
- 30.Jirarattanaphochai K, Jung S, Sumananont C, et al. : Reliability of the Roland-Morris Disability Questionnaire (Thai version) for the evaluation of low back pain patients. J Med Assoc Thai, 2005, 88: 407–411. [PubMed] [Google Scholar]
- 31.Roland M, Morris R: A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine, 1983, 8: 141–144. [DOI] [PubMed] [Google Scholar]
- 32.Hides JA, Richardson CA, Jull GA: Multifidus muscle recovery is not automatic after resolution of acute, first-episode low back pain. Spine, 1996, 21: 2763–2769. [DOI] [PubMed] [Google Scholar]
- 33.Enoch F, Kjaer P, Elkjaer A, et al. : Inter-examiner reproducibility of tests for lumbar motor control. BMC Musculoskelet Disord, 2011, 12: 114–125. [DOI] [PMC free article] [PubMed] [Google Scholar]