Abstract
Background
The inverse association between physical activity and cardiovascular disease (CVD) is well‐ established and has previously been shown in people with and without single CVD risk factors. We examined whether level of global cardiovascular risk, on the basis of the pooled cohort equation or Reynolds risk score, which include multiple risk factors, modified the physical activity–CVD association.
Methods and Results
Participants in the prospective WHS (Women's Health Study; n=27 536) reported their leisure‐time physical activity at study entry (1992–1995) and during follow‐up through 2013. Participants were divided into 10‐year cardiovascular risk groups on the basis of the pooled cohort equation and Reynolds risk score. The primary outcome was incident total CVD. The CVD hazard ratio for active (≥500 kcal/wk of physical activity) compared with inactive (<500 kcal/wk) individuals was 0.73 (95% confidence interval, 0.66–0.80) in multivariable models. This association was not modified by level of cardiovascular risk; physical activity was inversely associated with CVD within all pooled cohort equation and Reynolds risk score groups (P=0.17 and P=0.66 for interaction, respectively). When the joint association of physical activity and level of cardiovascular risk was examined, women with higher risk on the basis of either the pooled cohort equation or Reynolds risk score had higher CVD rates compared with those at low risk, regardless of physical activity. However, among women at both high and low risk, being physically active was associated with lower risk of CVD events.
Conclusions
In this large prospective cohort of women, level of global cardiovascular risk did not modify the inverse association between leisure‐time physical activity and incident CVD. Thus, promoting physical activity is important in women at both low and high cardiovascular risk.
Keywords: coronary heart disease, exercise, primary prevention, risk assessment, stroke
Subject Categories: Epidemiology, Exercise, Cardiovascular Disease, Primary Prevention, Women
Clinical Perspective
What Is New?
This study examined whether physical activity is equally beneficial for prevention of incident cardiovascular disease in individuals at high cardiovascular risk compared with those at low cardiovascular risk, as assessed by the pooled cohort equation.
Leisure‐time physical activity was significantly associated with lower risk of incident coronary heart disease, stroke, and total cardiovascular disease, independent of the pooled cohort equation risk score.
In addition, leisure‐time physical activity was inversely associated with risk of cardiovascular disease, with risk reductions of similar magnitude, across groups of women, according to pooled cohort equation risk.
What Are the Clinical Implications?
The key finding from this study is that women with low as well as high cardiovascular risk can benefit from regular exercise.
It is particularly important for clinicians to promote physical activity in women with high cardiovascular risk because their absolute rate of disease is high.
This information is important not only for clinicians but also for informing future physical activity guidelines.
The inverse association between physical activity and cardiovascular disease (CVD) is well established, with both moderate‐ to vigorous‐intensity exercise as well as brisk walking having cardiovascular benefits.1, 2, 3, 4 Furthermore, this inverse association has been shown in various high‐risk subgroups, including older adults, current smokers, and adults with diabetes mellitus (DM), hypercholesterolemia, or hypertension.2, 3, 5, 6, 7, 8, 9, 10 Although physical activity reduces CVD risk in people with and without single CVD risk factors, it is unclear if physical activity is equally beneficial for prevention of CVD among women with varying levels of global cardiovascular risk.
A recent study in Australian adults showed that recreational physical activity was significantly associated with reduced risk of CVD mortality after adjustment for the Framingham risk score and obesity.11 Another study conducted in the WHI‐OS (Women's Health Initiative Observational Study) recently found that recreational physical activity was the only lifestyle factor independently associated with incident CVD when added to traditional risk factor models (variables from the pooled cohort equation [PCE] and Reynolds risk score [RRS]).12 Although these studies provide evidence that physical activity is inversely associated with CVD independent of traditional cardiovascular risk factors, neither study examined whether the association differs according to level of risk. It is important to determine if the physical activity–CVD association differs by level of cardiovascular risk because if those at highest risk do not benefit from exercise, it is necessary to focus on other lifestyle factors or medications to decrease their risk of experiencing a cardiovascular event.
The purpose of this study was to determine whether level of global cardiovascular risk, as assessed by the PCE or the RRS, modifies the association between leisure‐time physical activity and incident CVD. In other words, we examined whether physical activity is equally beneficial for prevention of total CVD in individuals at high cardiovascular risk compared with those at low cardiovascular risk. In addition, we investigated coronary heart disease (CHD) and stroke separately as well as associations for walking specifically.
Methods
Study Population
The WHS (Women's Health Study) is a completed randomized trial (1992–2004) testing aspirin and vitamin E for preventing CVD and cancer among 39 876 initially healthy, US female health professionals aged ≥45 years at study entry (1992–1995).13 After trial completion, 33 682 participants (88.6% of those alive) consented to be followed up in an observational study.14 At baseline, women reported on questionnaires their medical history and lifestyle characteristics, including physical activity, age, race/ethnicity, DM, blood pressure, blood pressure treatment, smoking status, and cholesterol‐lowering medications. Information on medical conditions and risk factors was updated yearly. Women provided written consent to participate, and the study was approved by the institutional review board of Brigham and Women's Hospital (Boston, MA). The data, analytical methods, and study materials will not be made available to other researchers for purposes of reproducing the results or replicating the procedure.
Women eligible for the current analysis were those who had complete ascertainment of plasma lipids as well as information on physical activity and other risk factors (n=27 536). Plasma samples were measured for total, low‐density, and high‐density lipoprotein cholesterol, high‐sensitivity C‐reactive protein, and hemoglobin A1c (among diabetic people) in a core laboratory certified by the National Heart, Lung, and Blood Institute–Centers for Disease Control and Prevention Lipid Standardization Program.
Assessment of Leisure‐Time Physical Activity
Each participant reported average time per week during the previous year spent on 8 recreational activities: walking/hiking, jogging, running, bicycling, aerobic exercise/dance, lap swimming, tennis/squash/racquetball, and lower‐intensity exercise/yoga/stretching/toning.3 Number of flights of stairs climbed daily was also reported. A metabolic equivalent task (MET) score was assigned to each activity on the basis of its energy cost. One MET corresponds to an energy expenditure of ≈1 kcal/kg of body weight per hour; thus, energy expenditure in kilocalories per week was estimated by multiplying the MET score by body weight and hours per week. This assessment of physical activity has been shown to be valid and reliable15; for example, the correlation between 4 1‐week activity diaries kept over 1 year and questionnaire estimates of physical activity was 0.62.
Physical activity was assessed at baseline and updated at months 36, 72, and 96 during the trial, at trial conclusion (120 months), and year 2 (144 months), year 4 (168 months), year 7 (204 months), and year 9 (228 months) of observational follow‐up.
Assessment of Level of Global Cardiovascular Risk
Global cardiovascular risk was estimated on the basis of the recently developed PCE and the RRS. The PCE includes the following risk factors: age, total cholesterol, high‐density lipoprotein cholesterol, systolic blood pressure (including treated or untreated status), DM, and current smoking status.16 Participants were then categorized into 4 groups on the basis of their 10‐year risk of atherosclerotic CVD, as predicted by the PCE, as previously described16: <5%, 5% to <7.5%, 7.5% to <10%, and ≥10%. The RRS additionally includes high‐sensitivity C‐reactive protein, family history of premature myocardial infarction (MI; before 60 years of age), and hemoglobin A1c among diabetic people only.17 Similarly, participants were also categorized into 4 groups on the basis of their predicted 10‐year risk of atherosclerotic CVD, according to the RRS17: <5%, 5% to <10%, 10% to <20%, and ≥20%.
Ascertainment of CVD
The primary end point for this analysis was incident CVD, which included MI, stroke, CVD death, coronary artery bypass graft surgery, or percutaneous coronary intervention. In addition, MI and stroke were examined separately. Women reported events on follow‐up questionnaires every 6 months during the first year or 12 months thereafter, and medical records were obtained to confirm self‐reports, as previously described.13 MI was confirmed according to World Health Organization criteria, diagnostic ECG changes, or elevated cardiac enzymes. Stroke was confirmed by diagnosis of a new neurological deficit of sudden or rapid onset lasting ≥24 hours that was attributable to a cerebrovascular event. Death was confirmed to be from cardiovascular causes on the basis of an examination of autopsy reports, death certificates, medical records, and information obtained from family members. The use of coronary artery bypass graft surgery or percutaneous transluminal coronary angioplasty was confirmed by a review of the medical records. This analysis included end points ascertained as of February 2013.
Statistical Analysis
All analyses were conducted using SAS, version 9.4 (SAS Institute Inc, Cary, NC) software. Eligible participants contributed person‐time from return of baseline questionnaires to the first diagnosis of CVD, death from any cause, unavailability for follow‐up, or February 2013.
We first examined the independent associations of PCE or RRS and leisure‐time physical activity with risk of incident CVD by including the risk score and physical activity simultaneously in the same model. Simple updated levels of physical activity, in which outcomes were predicted from the most recent questionnaire, were used. For example, events that occurred between baseline and 36 months were examined in relation to physical activity level reported on the baseline questionnaire; events from 36 to 72 months were examined in relation to the physical activity reported on the 36‐month questionnaire; and so forth. Physical activity data were carried forward for cycles where data were missing. We categorized women according to amount of energy expended: <200, 200 to 599, 600 to 1499, and ≥1500 kcal/wk. Cox proportional hazards models were used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for incident CHD, stroke, and total CVD as a function of PCE, RRS, or physical activity, adjusted for age (in years) and randomized treatment assignment (aspirin or vitamin E). In multivariable models, we additionally adjusted for smoking status (never, past, or current smoker); alcohol consumption (4 categories); saturated fat, fiber, and fruit and vegetable intake (quintiles); menopausal status (premenopausal or postmenopausal); postmenopausal hormone use (never, past, or current); and parent history of MI <60 years of age (PCE and physical activity models only). Tests for linear trend were performed by modeling the median level of PCE, RRS, or physical activity in each category as a continuous variable. In a sensitivity analysis, we also examined the association between physical activity and total CVD after excluding coronary artery bypass graft surgery and percutaneous coronary intervention as end points.
To assess whether level of global cardiovascular risk modified the association between leisure‐time physical activity and incident CVD, we created a dichotomous variable for physical activity where women reporting ≥500 kcal/wk were categorized as active and women reporting <500 kcal/wk were categorized as inactive. This cut point was chosen because, given the average weight of the women in this study, 500 kcal/wk is equivalent to meeting the current physical activity guidelines.1, 18 We then modeled risk of incident CVD as a function of physical activity within PCE categories and RRS categories. To test for interaction, participants were cross classified into 8 groups according to physical activity and PCE or RRS. The interaction was assessed by the difference in −2 log likelihood between the model containing the cross‐classified physical activity–CVD risk variables and the main effects model.
In addition to total leisure‐time activity, we also examined the association between walking and risk of incident CVD as well as whether this association was modified by level of global cardiovascular risk. We categorized women into approximate quartiles of time spent walking per week: 0 minutes, 1 to 59 minutes, 1 to 2.5 hours, and ≥2.5 hours. We also created a dichotomous walking variable (<1 versus ≥1 h/wk) to examine effect modification by PCE or RRS, and the interaction was examined as previously described.
Results
During a median follow‐up of 19.1 years (interquartile range, 17.5–19.7 years), 1860 incident cases of total CVD, 458 incident cases of CHD, and 650 incident strokes were documented. The mean (SD) age of the study population at baseline was 54.7 (7.0) years. We examined PCE risk in relation to other potential risk factors for CVD at baseline (Table 1). In addition to higher levels of the risk factors that are included in the PCE model, women with higher PCE risk had higher body mass index, were less likely to drink alcohol, and reported less physical activity. Women with PCE risk <5% reported a mean (SD) 976 (1245) kcal/wk of physical activity at baseline, whereas women with PCE risk ≥10% reported 855 (1216) kcal/wk.
Table 1.
Baseline Characteristics According to the PCE Among 27 536 Participants in the WHS
| Characteristics | PCE Category | |||
|---|---|---|---|---|
| <5% (n=21 634) | 5%–<7.5% (n=2478) | 7.5%–<10% (n=1400) | ≥10% (n=2024) | |
| PCE | 1.9 (1.2) | 6.1 (0.7) | 8.6 (0.7) | 15.6 (5.9) |
| RRS | 1.5 (1.1) | 4.8 (2.1) | 7.0 (3.5) | 13.3 (8.9) |
| Physical activity, kcal/wk | 976 (1245) | 882 (1151) | 901 (1174) | 855 (1216) |
| Age at randomization, y | 52.3 (4.8) | 60.2 (6.2) | 63.1 (6.4) | 66.8 (7.2) |
| Body mass index, kg/m2 | 25.6 (4.9) | 27.0 (5.2) | 27.0 (5.0) | 27.1 (5.3) |
| Current smoker, % | 7.0 | 27.0 | 28.9 | 30.7 |
| Parental history of MI, % | 14.9 | 13.5 | 13.1 | 11.5 |
| Hypertension, % | 18.7 | 42.3 | 50.5 | 72.3 |
| Hypercholesterolemia, % | 25.8 | 46.0 | 47.7 | 54.6 |
| Diabetes mellitus, % | 0.9 | 5.4 | 6.7 | 15.7 |
| Postmenopausal, % | 45.1 | 80.7 | 88.6 | 92.3 |
| Hormone therapy, % | 45.4 | 43.1 | 37.7 | 31.2 |
| Drink alcohol, % | 57.6 | 51.2 | 49.1 | 46.7 |
| Saturated fat, g/d | 19.6 (7.9) | 20.3 (8.4) | 19.7 (8.5) | 19.5 (8.2) |
| Fruit, servings/d | 2.2 (1.5) | 2.3 (1.9) | 2.2 (1.5) | 2.4 (1.7) |
| Vegetables, servings/d | 3.9 (2.6) | 4.0 (2.8) | 4.0 (2.6) | 4.1 (2.6) |
| Fiber, g/d | 19.0 (8.2) | 19.1 (8.2) | 19.1 (8.6) | 19.7 (8.5) |
All values are mean (SD) for continuous variables or frequencies for categorical variables. MI indicates myocardial infarction; PCE, pooled cohort equation; RRS, Reynolds risk score; WHS, Women's Health Study.
The association between PCE and incident CHD, stroke, and total CVD in these data is shown in Table 2. In multivariable‐adjusted models, women with PCE risk ≥10% had an HR of 7.06 (95% CI, 4.96–10.06) for CHD, 3.33 (95% CI, 2.43–4.57) for stroke, and 5.09 (95% CI, 4.24–6.12) for total CVD compared with women with PCE risk <5%. Similarly, women with RRS ≥20% had an HR of 9.91 (95% CI, 6.52–15.08) for CHD, 3.22 (95% CI, 2.17–4.80) for stroke, and 7.66 (95% CI, 6.16–9.53) for total CVD compared with women with RRS <5% (Table S1). In addition, independent of PCE or RRS, there was a significant inverse association between leisure‐time physical activity and risk of CHD, stroke, and total CVD (Table 2). In multivariable‐adjusted models that included PCE, women who reported ≥1500 kcal/wk of physical activity compared with women reporting <200 kcal/wk had an HR of 0.66 (95% CI, 0.51–0.86) for CHD, 0.72 (95% CI, 0.57–0.90) for stroke, and 0.71 (95% CI, 0.63–0.81) for total CVD. Results were similar for physical activity when multivariable models included RRS instead of PCE (HR for total CVD, 0.73; 95% CI, 0.64–0.83 comparing extreme categories). When treated as a dichotomous variable, the HR for ≥500 kcal/wk of physical activity (ie, meeting physical activity recommendations) was 0.64 (95% CI, 0.53–0.77) for CHD, 0.78 (95% CI, 0.66–0.91) for stroke, and 0.73 (95% CI, 0.66–0.80) for total CVD (Table 3). In sensitivity analyses, results were similar for PCE, RRS, and physical activity when coronary artery bypass graft surgery and percutaneous coronary intervention were not included in the total CVD end point (HRs comparing extreme categories were 4.83 [95% CI, 3.86–6.05] for PCE, 5.88 [95% CI, 4.52–7.66] for RRS, and 0.73 [95% CI, 0.62–0.86] for physical activity).
Table 2.
HRs (95% CIs) of CHD, Stroke, and Total CVD, According to PCE or Physical Activity Category
| Variable | No. of Person‐Years (No. of Events) | Age‐ and Treatment‐Adjusted HR (95% CI) | Multivariable‐Adjusted HR (95% CI)a |
|---|---|---|---|
| CHD | |||
| PCE | |||
| <5% | 387 838 (189) | 1.00 | 1.00 |
| 5%–<7.5% | 41 470 (75) | 3.98 (2.97–5.33) | 2.92 (2.13–3.98) |
| 7.5%–<10% | 22 345 (60) | 6.04 (4.33–8.43) | 4.28 (2.99–6.12) |
| ≥10% | 29 336 (134) | 10.57 (7.79–14.36) | 7.06 (4.96–10.06) |
| P value for trend | … | <0.0001 | <0.0001 |
| Physical activity, kcal/wk | |||
| 0–199 | 121 156 (178) | 1.00 | 1.00 |
| 200–599 | 87 310 (87) | 0.61 (0.47–0.79) | 0.72 (0.55–0.93) |
| 600–1499 | 129 465 (100) | 0.51 (0.40–0.65) | 0.64 (0.50–0.83) |
| ≥1500 | 143 058 (93) | 0.51 (0.40–0.66) | 0.66 (0.51–0.86) |
| P value for trend | … | 0.0001 | 0.06 |
| Stroke | |||
| PCE | |||
| <5% | 387 544 (301) | 1.00 | 1.00 |
| 5%–<7.5% | 41 452 (94) | 2.01 (1.55–2.60) | 1.81 (1.38–2.37) |
| 7.5%–<10% | 22 351 (86) | 2.98 (2.24–3.98) | 2.65 (1.95–3.60) |
| ≥10% | 29 432 (169) | 3.87 (2.92, 5.13) | 3.33 (2.43, 4.57) |
| P value for trend | … | <0.0001 | <0.0001 |
| Physical activity, kcal/wk | |||
| 0–199 | 120 712 (211) | 1.00 | 1.00 |
| 200–599 | 87 234 (141) | 0.85 (0.69–1.05) | 0.93 (0.75–1.15) |
| 600–1499 | 129 707 (165) | 0.72 (0.59–0.88) | 0.81 (0.66–1.00) |
| ≥1500 | 143 125 (133) | 0.62 (0.50–0.78) | 0.72 (0.57–0.90) |
| P value for trend | … | <0.0001 | 0.003 |
| Total CVD | |||
| PCE | |||
| <5% | 391 108 (865) | 1.00 | 1.00 |
| 5%–<7.5% | 41 159 (296) | 2.92 (2.53–3.39) | 2.48 (2.12–2.90) |
| 7.5%–<10% | 22 119 (223) | 3.94 (3.32–4.68) | 3.31 (2.76–3.98) |
| ≥10% | 28 820 (476) | 6.21 (5.29–7.30) | 5.09 (4.24–6.12) |
| P value for trend | … | <0.0001 | <0.0001 |
| Physical activity, kcal/wk | |||
| 0–199 | 121 364 (647) | 1.00 | 1.00 |
| 200–599 | 87 903 (393) | 0.77 (0.68–0.88) | 0.87 (0.76–0.99) |
| 600–1499 | 130 047 (434) | 0.62 (0.55–0.70) | 0.73 (0.65–0.83) |
| ≥1500 | 143 891 (386) | 0.59 (0.52–0.67) | 0.71 (0.63–0.81) |
| P value for trend | … | <0.0001 | <0.0001 |
CHD indicates coronary heart disease; CI, confidence interval; CVD, cardiovascular disease; HR, hazard ratio; and PCE, pooled cohort equation.
Adjusted for age; randomized treatment assignment; smoking status; consumption of alcohol, saturated fat, fiber, fruits, and vegetables; menopausal status; postmenopausal hormone use, parental history of myocardial infarction <60 years of age; physical activity (PCE model); PCE (physical activity model).
Table 3.
HRs (95% CIs) of CHD, Stroke, and Total CVD for Being Physically Active (≥500 kcal/wk) Within Categories of PCE
| Variable | No. of Events | Age‐ and Treatment‐Adjusted HR (95% CI) | Multivariable HR (95% CI)a |
|---|---|---|---|
| CHD | |||
| All women | 458 | 0.57 (0.47–0.68) | 0.64 (0.53–0.77) |
| PCE | |||
| <5% | 189 | 0.75 (0.57–1.01) | 0.78 (0.58–1.05) |
| 5%–<7.5% | 75 | 0.78 (0.49–1.23) | 0.77 (0.48–1.24) |
| 7.5%–<10% | 60 | 0.58 (0.34–0.98) | 0.57 (0.33–0.98) |
| ≥10% | 134 | 0.47 (0.32–0.68) | 0.51 (0.35–0.74) |
| P value for interaction | … | 0.06 | 0.10 |
| Stroke | |||
| All women | 650 | 0.70 (0.60–0.82) | 0.78 (0.66–0.91) |
| PCE | |||
| <5% | 301 | 0.82 (0.65–1.04) | 0.89 (0.70–1.13) |
| 5%–<7.5% | 94 | 0.73 (0.48–1.10) | 0.71 (0.47–1.08) |
| 7.5%–<10% | 86 | 0.91 (0.59–1.39) | 0.91 (0.59–1.41) |
| ≥10% | 169 | 0.60 (0.44–0.82) | 0.59 (0.43–0.82) |
| P value for interaction | … | 0.31 | 0.36 |
| Total CVD | |||
| All women | 1860 | 0.67 (0.61–0.73) | 0.73 (0.66–0.80) |
| PCE | |||
| <5% | 865 | 0.78 (0.68–0.89) | 0.84 (0.73–0.97) |
| 5%–<7.5% | 296 | 0.79 (0.63–1.00) | 0.78 (0.61–0.98) |
| 7.5%–<10% | 223 | 0.68 (0.52–0.89) | 0.68 (0.52–0.90) |
| ≥10% | 476 | 0.64 (0.53–0.77) | 0.64 (0.53–0.78) |
| P value for interaction | … | 0.13 | 0.17 |
CHD indicates coronary heart disease; CI, confidence interval; CVD, cardiovascular disease; HR, hazard ratio; PCE, pooled cohort equation.
Adjusted for age; randomized treatment assignment; smoking status; consumption of alcohol, saturated fat, fiber, fruits, and vegetables; menopausal status; postmenopausal hormone use; and parental history of myocardial infarction <60 years of age.
We found little evidence that the association between physical activity and CHD, stroke, or total CVD was different among women, according to their global cardiovascular risk (Table 3 and Table S2). Leisure‐time physical activity was associated with lower CVD risk across categories of PCE and RRS. For total CVD, the HR for physically active compared with inactive women was 0.84 (95% CI, 0.73–0.97) among women with PCE <5%, 0.78 (95% CI, 0.61–0.98) among women with PCE 5% to <7.5%, 0.68 (95% CI, 0.52–0.90) among women with PCE 7.5% to <10%, and 0.64 (95% CI, 0.53–0.78) among women with PCE ≥10% (P=0.17 for interaction). Similar results were seen for cardiovascular risk, as determined by the RRS as well. Although the association between physical activity and CVD appeared stronger in some strata compared with others, none of the interactions between PCE or RRS and physical activity were statistically significant.
The joint associations of leisure‐time physical activity and PCE on risk of incident CVD is shown in the Figure. Although risk of incident CVD increases substantially as PCE increases, within each category, women who were active had lower CVD risk than women who were inactive. Overall, inactive women with PCE ≥10% had 7.98 (95% CI, 6.65–9.59) times the rate of CVD compared with active women with PC risk <5%. Likewise, for RRS, inactive women with RRS ≥20% had 11.99 (95% CI, 9.37–15.34) times the rate of CVD compared with active women with RRS <5% (Figure S1).
Figure 1.
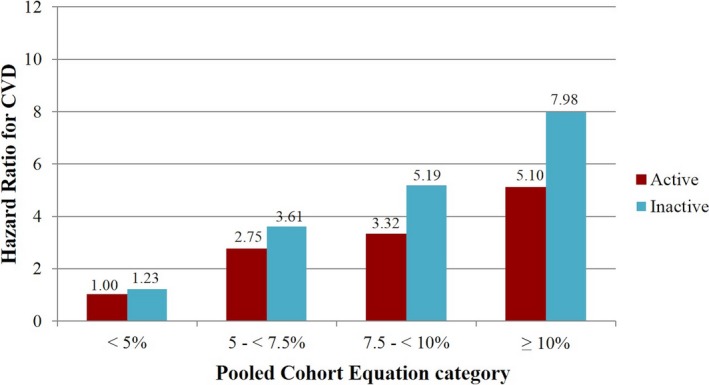
Age‐ and treatment‐adjusted hazard ratios (HRs) for total cardiovascular disease (CVD) for the joint association between physical activity and pooled cohort equation. The models included age and randomized treatment assignment. All HRs were significant at P=0.01. P=0.13 for interaction.
Time spent walking per week was also associated with significantly lower CVD risk (Table S3). Women who reported walking ≥2.5 h/wk had an HR for CVD of 0.64 (95% CI, 0.56–0.73) compared with women who did not walk. In general, the inverse association between walking and incident CVD held across various categories of cardiovascular risk (Table S4).
Discussion
In this large prospective cohort of women from the WHS, leisure‐time physical activity was significantly inversely associated with incident CHD, stroke, and total CVD, independent of traditional cardiovascular risk factors. Level of global cardiovascular risk, as estimated by the PCE and RRS models, did not modify the inverse association between physical activity and CVD. That is, habitual leisure‐time physical activity was inversely associated with risk of CVD, with risk reductions of similar magnitude, across groups of women according to the PCE and RRS. Furthermore, results were similar for MI and stroke when examined separately.
Similar to prior studies, we found that physical activity was independently associated with risk of incident CVD after adjusting for risk scores that included traditional cardiovascular risk factors as well as inflammation, family history, and hemoglobin A1c. Among middle‐aged men and women in Australia, Dhaliwal and colleagues found that, after adjusting for both the Framingham Risk Score and waist/hip ratio, individuals reporting the highest amount of recreational physical activity had an odds ratio of 0.35 (95% CI, 0.13–0.98) for CVD mortality compared with individuals reporting the lowest amount of physical activity.11 Likewise, based on data from the WHI‐OS, Paynter et al found that women reporting ≥21.1 MET‐h/wk of physical activity, compared with 0 to 1.4 MET‐h/wk, had HRs of 0.67 (95% CI, 0.51–0.87) and 0.65 (95% CI, 0.50–0.85) for incident CVD after adjusting for other lifestyle factors and components of the PCE and RRS, respectively.12 These estimates are similar to that from the current study (HR, 0.72; 95% CI, 0.63–0.82), whereas the estimate from the study by Dhaliwal et al11 is a bit stronger. A possible explanation for the difference is that all individuals in the high category of physical activity in the study by Dhaliwal et al,11 which included younger men and women, may have exercised at a higher level than the older women in our study and the WHI‐OS. In addition, the study by Dhaliwal et al11 only adjusted for components of the Framingham risk score and waist/hip ratio, so there may be residual confounding by other lifestyle factors.
Previous studies have shown that physical activity is beneficial for prevention of CVD in subgroups of individuals at high CVD risk. Among diabetic women in the NHS (Nurses’ Health Study), Hu and colleagues found that those who reported ≥7 h/wk of moderate to vigorous physical activity had a 45% lower risk of incident CVD compared with women reporting <1 h/wk.5 In addition, they found that walking alone was also inversely associated with CVD in women with DM.5 In a study among individuals with hypercholesterolemia, Williams and Franklin found that ≥3.6 MET‐h/d of running or walking compared with ≤1.07 MET‐h/d was associated with a 37% lower risk of fatal CVD and a 26% lower risk of nonfatal CVD after adjusting for other risk factors.8 In a study of 470 163 Taiwanese adults, Li et al reported that, among hypertensive individuals, risk of mortality was 37% higher for those who were inactive compared with those who were active.6 Among participants in the Harvard Alumni Health Study, Paffenbarger et al found that men with a high level of physical activity (≥2000 kcal/wk) had lower rates of heart attack than those with a low level of physical activity (<2000 kcal/wk), even in the presence of various cardiovascular risk factors, including older age, smoking, and obesity.9 In a follow‐up to this analysis, Sesso and colleagues found that, among men with multiple (≥4) CVD risk factors, those who were more active had reduced CHD risk compared with those who were less active.10 It is not surprising that physical activity is associated with lower risk of CVD in these high‐risk subgroups because many of the mechanisms for the benefits of exercise include improvements in several of these cardiovascular risk factors, including blood pressure, lipoprotein levels, and glucose tolerance.19, 20, 21
Prior studies have investigated whether physical activity attenuates CVD risk among individuals with a cluster of metabolic abnormalities, but the data are limited. Hamer and Stamatakis examined physical activity among the metabolically healthy and unhealthy, as determined by blood pressure, high‐density lipoprotein cholesterol, DM, waist circumference, and C‐reactive protein.22 Among participants with ≥2 metabolic risk factors at baseline, those who reported engaging in moderate‐to‐vigorous physical activity ≥3 times per week had an HR for CVD mortality of 0.63 (95% CI, 0.40–0.99) compared with those who reported none. Similar findings have been reported in a few other cohort studies for physical activity23, 24, 25 as well as for physical fitness.26 In a meta‐analysis examining cardiorespiratory fitness as a predictor of all‐cause mortality and CHD/CVD, results from 8 cohort studies indicated that each MET higher level of maximal aerobic capacity correlated with an 11% (95% CI, 7%–15%) lower risk of CHD/CVD among individuals with >3 metabolic factors.26
This study is a significant contribution to the literature because we used both the PCE and the RRS to estimate level of global cardiovascular risk and showed that recreational physical activity was associated with a lower rate of incident CVD, even among adults at highest CVD risk. The US Preventive Services Task Force recommends diet and physical activity counseling in adults at high risk for CVD.27 They found that intensive diet and physical activity behavioral counseling in adults with CVD risk factors resulted in consistent improvements in several intermediate outcomes (total cholesterol, low‐density lipoprotein, systolic blood pressure, diastolic blood pressure, fasting glucose, DM incidence, and weight outcomes). However, the US Preventive Services Task Force found that limited evidence was available for decreases in CVD rates.
Strengths of our study include its prospective design, the large sample size, detailed assessment of physical activity collected multiple times during the study, and long duration of follow‐up. However, limitations include the fact that physical activity was self‐reported, so measurement is less precise. Nonetheless, this questionnaire has been previously validated in a similar study population.15 Another limitation is that our study only included predominantly white women of higher socioeconomic status and may not be generalizable to other groups. Future work should seek to replicate these findings in more diverse nationally representative samples. In addition, we could only estimate level of cardiovascular risk on the basis of the PCE and RRS at baseline because that was the only time blood was collected from study participants. Finally, although results from this study support physical activity for CVD prevention in women at high cardiovascular risk, we are unable to make inferences specifically about initiation of physical activity in high‐risk women based on the current analysis.
In conclusion, in this large prospective cohort of women, level of global cardiovascular risk did not modify the inverse association between leisure‐time physical activity and risk of incident CVD. The present findings suggest that women with low as well as high cardiovascular risk can benefit from regular exercise. Thus, promoting physical activity is particularly important in women with high cardiovascular risk, because their absolute rate of disease is high. This information is important not only for clinicians, but also for informing the 2018 update to the present federal physical activity guidelines (https://health.gov/paguidelines/second-edition).
Sources of Funding
The WHS (Women's Health Study) was supported by grants CA‐047988, HL‐043851, HL‐080467, and HL‐099355 from the National Institutes of Health (Bethesda, MD). Biomarkers were funded through The Reynolds Risk Score Project, which was supported by investigator‐initiated research grants from the Donald W. Reynolds Foundation (Las Vegas, NV) with additional support from the Doris Duke Charitable Foundation (New York, NY) and the Leducq Foundation (Paris, France).
Disclosures
Ridker has received investigator‐initiated research grant support from the National Heart, Lung, and Blood Institute, Novartis, Pfizer, AstraZeneca, and Kowa. He is also listed as a coinventor on patents held by the Brigham and Women's Hospital, which relate to the use of inflammatory biomarkers in cardiovascular disease and diabetes mellitus that have been licensed to AstraZeneca and Siemens. The remaining authors have no disclosures to report.
Supporting information
Table S1. Hazard Ratios (95% CI) of Coronary Heart Disease (CHD), Stroke, and Total Cardiovascular Disease (CVD) According to Categories of the Reynolds Risk Score
Table S2. Hazard Ratios (95% CI) of Coronary Heart Disease (CHD), Stroke, and Total Cardiovascular (CVD) for Being Physically Active (≥500 kcal/week) Within Categories of the Reynolds Risk Score
Table S3. Hazard Ratios (95% CI) of Total CVD According to Time Spent Walking Per Week
Table S4. Hazard Ratios (95% CI) of Total CVD for Walking (≥1 h/week Versus <1 h/week) Within Categories of Pooled Cohort Risk or Reynolds Risk Score
Figure S1. Age‐ and treatment‐adjusted hazard ratios (HR) for total CVD for the joint association between physical activity and Reynolds Risk Score.
(J Am Heart Assoc. 2018;7:e008234 DOI: 10.1161/JAHA.117.008234.)
References
- 1. Physical Activity Guidelines Advisory Committee . Physical Activity Guidelines Committee Report, 2008. Washington, DC: US Department of Health and Human Services; 2008:683. [Google Scholar]
- 2. Manson JE, Greenland P, LaCroix AZ, Stefanick ML, Mouton CP, Oberman A, Perri MG, Sheps DS, Pettinger MB, Siscovick DS. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. 2002;347:716–725. [DOI] [PubMed] [Google Scholar]
- 3. Lee IM, Rexrode KM, Cook NR, Manson JE, Buring JE. Physical activity and coronary heart disease in women: is “no pain, no gain” passe? JAMA. 2001;285:1447–1454. [DOI] [PubMed] [Google Scholar]
- 4. Chomistek AK, Henschel B, Eliassen AH, Mukamal KJ, Rimm EB. Frequency, type, and volume of leisure‐time physical activity and risk of coronary heart disease in young women. Circulation. 2016;134:290–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hu FB, Stampfer MJ, Solomon C, Liu S, Colditz GA, Speizer FE, Willett WC, Manson JE. Physical activity and risk for cardiovascular events in diabetic women. Ann Intern Med. 2001;134:96–105. [DOI] [PubMed] [Google Scholar]
- 6. Li CS, Liu CC, Tsai MK, Tai YP, Wai JP, Tsao CK, Wen CP. Motivating patients to exercise: translating high blood pressure into equivalent risk of inactivity. J Hypertens. 2015;33:287–293. [DOI] [PubMed] [Google Scholar]
- 7. Manson JE, Hu FB, Rich‐Edwards JW, Colditz GA, Stampfer MJ, Willett WC, Speizer FE, Hennekens CH. A prospective study of walking as compared with vigorous exercise in the prevention of coronary heart disease in women. N Engl J Med. 1999;341:650–658. [DOI] [PubMed] [Google Scholar]
- 8. Williams PT, Franklin BA. Incident diabetes mellitus, hypertension, and cardiovascular disease risk in exercising hypercholesterolemic patients. Am J Cardiol. 2015;116:1516–1520. [DOI] [PubMed] [Google Scholar]
- 9. Paffenbarger RS Jr, Wing AL, Hyde RT. Physical activity as an index of heart attack risk in college alumni. Am J Epidemiol. 1978;108:161–175. [DOI] [PubMed] [Google Scholar]
- 10. Sesso HD, Paffenbarger RS Jr, Lee IM. Physical activity and coronary heart disease in men: the Harvard Alumni Health Study. Circulation. 2000;102:975–980. [DOI] [PubMed] [Google Scholar]
- 11. Dhaliwal SS, Welborn TA, Howat PA. Recreational physical activity as an independent predictor of multivariable cardiovascular disease risk. PLoS One. 2013;8:e83435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Paynter NP, LaMonte MJ, Manson JE, Martin LW, Phillips LS, Ridker PM, Robinson JG, Cook NR. Comparison of lifestyle‐based and traditional cardiovascular disease prediction in a multiethnic cohort of nonsmoking women. Circulation. 2014;130:1466–1473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ridker PM, Cook NR, Lee IM, Gordon D, Gaziano JM, Manson JE, Hennekens CH, Buring JE. A randomized trial of low‐dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med. 2005;352:1293–1304. [DOI] [PubMed] [Google Scholar]
- 14. Shiroma EJ, Cook NR, Manson JE, Buring JE, Rimm EB, Lee IM. Comparison of self‐reported and accelerometer‐assessed physical activity in older women. PLoS One. 2015;10:e0145950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wolf AM, Hunter DJ, Colditz GA, Manson JE, Stampfer MJ, Corsano KA, Rosner B, Kriska A, Willett WC. Reproducibility and validity of a self‐administered physical activity questionnaire. Int J Epidemiol. 1994;23:991–999. [DOI] [PubMed] [Google Scholar]
- 16. Goff DC Jr, Lloyd‐Jones DM, Bennett G, Coady S, D'Agostino RB, Gibbons R, Greenland P, Lackland DT, Levy D, O'Donnell CJ, Robinson JG, Schwartz JS, Shero ST, Smith SC Jr, Sorlie P, Stone NJ, Wilson PW, Jordan HS, Nevo L, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Smith SC Jr, Tomaselli GF; American College of Cardiology/American Heart Association Task Force on Practice Guidelines . 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:S49–S73. [DOI] [PubMed] [Google Scholar]
- 17. Ridker PM, Buring JE, Rifai N, Cook NR. Development and validation of improved algorithms for the assessment of global cardiovascular risk in women: the Reynolds Risk Score. JAMA. 2007;297:611–619. [DOI] [PubMed] [Google Scholar]
- 18. Sattelmair J, Pertman J, Ding EL, Kohl HW III, Haskell W, Lee IM. Dose response between physical activity and risk of coronary heart disease: a meta‐analysis. Circulation. 2011;124:789–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ahmed HM, Blaha MJ, Nasir K, Rivera JJ, Blumenthal RS. Effects of physical activity on cardiovascular disease. Am J Cardiol. 2012;109:288–295. [DOI] [PubMed] [Google Scholar]
- 20. Kraus WE, Houmard JA, Duscha BD, Knetzger KJ, Wharton MB, McCartney JS, Bales CW, Henes S, Samsa GP, Otvos JD, Kulkarni KR, Slentz CA. Effects of the amount and intensity of exercise on plasma lipoproteins. N Engl J Med. 2002;347:1483–1492. [DOI] [PubMed] [Google Scholar]
- 21. Thompson PD, Crouse SF, Goodpaster B, Kelley D, Moyna N, Pescatello L. The acute versus the chronic response to exercise. Med Sci Sports Exerc. 2001;33:S438–S445; discussion S452‐S453. [DOI] [PubMed] [Google Scholar]
- 22. Hamer M, Stamatakis E. Low‐dose physical activity attenuates cardiovascular disease mortality in men and women with clustered metabolic risk factors. Circ Cardiovasc Qual Outcomes. 2012;5:494–499. [DOI] [PubMed] [Google Scholar]
- 23. Broekhuizen LN, Boekholdt SM, Arsenault BJ, Despres JP, Stroes ES, Kastelein JJ, Khaw KT, Wareham NJ. Physical activity, metabolic syndrome, and coronary risk: the EPIC‐Norfolk prospective population study. Eur J Cardiovasc Prev Rehabil. 2011;18:209–217. [DOI] [PubMed] [Google Scholar]
- 24. Reddigan JI, Ardern CI, Riddell MC, Kuk JL. Relation of physical activity to cardiovascular disease mortality and the influence of cardiometabolic risk factors. Am J Cardiol. 2011;108:1426–1431. [DOI] [PubMed] [Google Scholar]
- 25. Tjonna AE, Lund Nilsen TI, Slordahl SA, Vatten L, Wisloff U. The association of metabolic clustering and physical activity with cardiovascular mortality: the HUNT study in Norway. J Epidemiol Community Health. 2010;64:690–695. [DOI] [PubMed] [Google Scholar]
- 26. Kodama S, Saito K, Tanaka S, Maki M, Yachi Y, Asumi M, Sugawara A, Totsuka K, Shimano H, Ohashi Y, Yamada N, Sone H. Cardiorespiratory fitness as a quantitative predictor of all‐cause mortality and cardiovascular events in healthy men and women: a meta‐analysis. JAMA. 2009;301:2024–2035. [DOI] [PubMed] [Google Scholar]
- 27. LeFevre ML; US Preventive Services Task Force . Behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease prevention in adults with cardiovascular risk factors: US Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2014;161:587–593. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Hazard Ratios (95% CI) of Coronary Heart Disease (CHD), Stroke, and Total Cardiovascular Disease (CVD) According to Categories of the Reynolds Risk Score
Table S2. Hazard Ratios (95% CI) of Coronary Heart Disease (CHD), Stroke, and Total Cardiovascular (CVD) for Being Physically Active (≥500 kcal/week) Within Categories of the Reynolds Risk Score
Table S3. Hazard Ratios (95% CI) of Total CVD According to Time Spent Walking Per Week
Table S4. Hazard Ratios (95% CI) of Total CVD for Walking (≥1 h/week Versus <1 h/week) Within Categories of Pooled Cohort Risk or Reynolds Risk Score
Figure S1. Age‐ and treatment‐adjusted hazard ratios (HR) for total CVD for the joint association between physical activity and Reynolds Risk Score.


