Sexuality and Aging
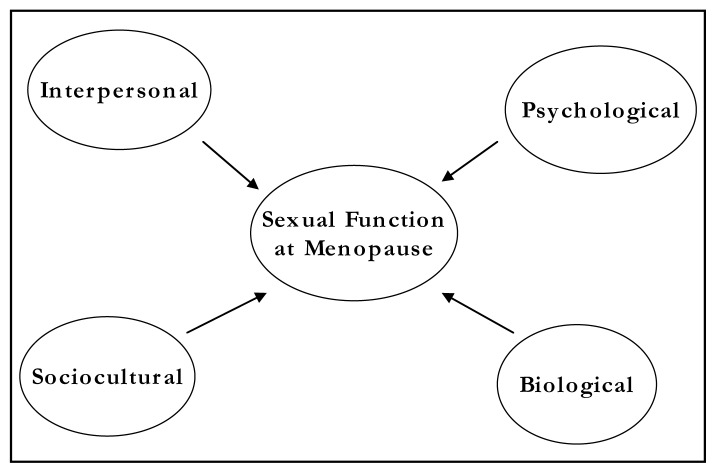
Menopausal and postmenopausal women can experience decreases in both libido, orgasm, and frequency of coitus—most commonly because of physiologic changes due to menopause, less commonly due to depression or marital discord (Figure 1). The differential diagnosis in women who are seen for sexual difficulties during the climacteric is challenging, especially when symptoms such as decline in libido and/ or persistent dyspareunia occur simultaneously with depression and marital discord. Estrogen, with or without androgen, can ameliorate the physiologic changes of menopause affecting sexuality. Depression can be treated with psychotherapy, with or without antidepressant drugs. Marital discord is best treated with couples therapy. The marital difficulties can either be the cause or the consequence of changes in sexual activity. In the latter case the marital discord resolves with the return of regular coital activity.
Figure 1.
Factors impacting changes in sexual function at menopause
The physiologic changes of menopause affecting sexual response are largely mediated by estrogen. The most notable effect is on orgasmic response: Altered nerve function due to the hypoestrogenic state of menopause may delay clitoral reaction time and result in slow or absent orgasmic response. This effect, along with delayed or absent vaginal secretion, diminished orgasmic platform (ie, decreased or absent congestion in the outer third of the vagina), and painful uterine contractions (in some 60- to 70-year-old postmenopausal women) can further affect the sexual experience.1,2 The psychological impact of these sexual changes is varied and can be very disturbing to women and to their partners.
Although the ratio of dysthymia and depression is as high as 2:1 in women versus men, many of these women are not treated for this depression and thus enter the menopausal years with untreated depressive illness.3–5 Depression can itself cause decreased libido as well as marital problems and can complicate any sexual problems arising from menopause. In addition, hot flushes and consequent nonrestorative sleep can complicate all these clinical situations.
Medication and illness in the postmenopausal years can affect sexuality and can complicate existing physiologic changes associated with menopause.6 The newer forms of antidepressant medication, ie, selective serotonin reuptake inhibitors (SSRIs), may cause slowed or absent orgasm and can reduce or eliminate libido in some women. Illness can decrease desire or simply make sexual activity inadvisable, given illness-associated lack of energy or anatomic difficulties.7
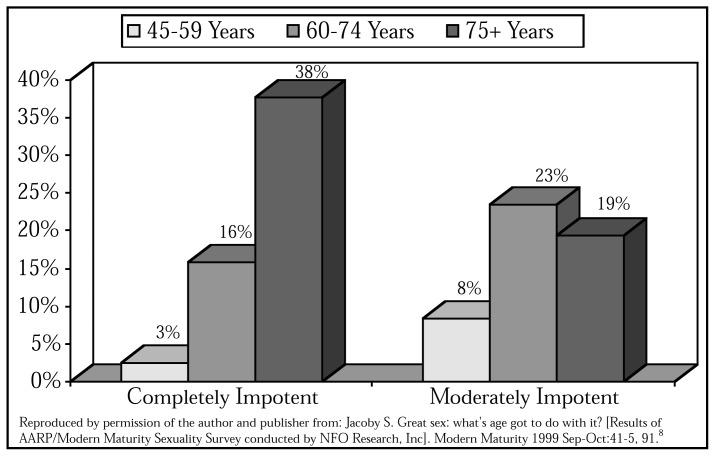
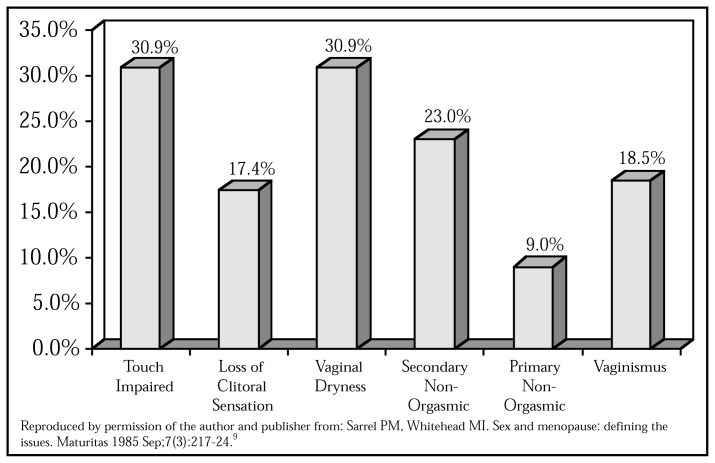
In about one third of couples, male sexual dysfunction contributes to decreased frequency of coitus (Figure 2); the remaining two thirds of couples are affected by physiologic factors of menopause (Figure 3).8 The psychological aspects of aging are less a factor in decreased coital activity than the physiologic effects of aging and the way couples adjust to those changes. Couples may choose to include alternatives to genital-genital contact if the male partner is having erectile problems; increased nonpenile stimulation may be helpful for women who have delayed response; and couples may develop a more flexible attitude toward their sexuality.10
Figure 2.
Importance by age (N=635)
Figure 3.
Specific problems reported by women at a London menopause clinic (N=178)
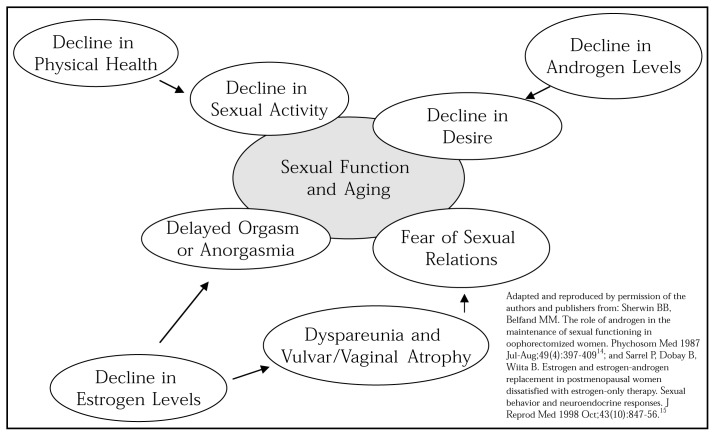
Sexual problems are numerous in the US population and increase with aging. The scientific literature indicates, however, that sexual problems in elderly people are often anatomic or physiologic in nature,11,12 whereas sexual problems in younger people tend to be more psychological and sociocultural.13 Because of the complexity of sexual problems in postmenopausal women, gynecologists and primary care physicians have a central role in expediting the differential diagnosis and treatment (Figure 4).14,15
Figure 4.
Process of aging
Clinical View of Sexual Functioning
Davidson16 divided sexual functioning into behavior and potency, whereas Sarrel and Whitehead8 divided sexual functioning into the desire phase, excitement phase, orgastic phases, and dyspareunia. Both are useful ways to view sexual functioning when evaluating perimenopausal and postmenopausal women. These classifications are shown in Table 1.9,16
Table 1.
Views of Sexual Function from a Clinical Perspective: Comparison of Published Studies
| Davidson16 | Behaviors associated with libido or sexual motivation: sexual desire, sexual fantasies, and satisfaction or pleasure |
| Potency: pelvic vasocongestion, orgasmic contractions, and possible extragenital responses | |
| Sarrel and Whitehead9 | Desire phase: loss of desire or sexual aversion |
| Excitement phase: touch sensation impairment, loss of clitoral sensation, vaginal dryness, and urinary incontinence | |
| Orgasmic phase: primary or secondary | |
| Dyspareunia: vaginal dryness, vaginismus as conditioned response to painful penetration |
Sex and Menopause: Studies on Etiology of Decreased Coitus
Sexual research on sexual functioning during the climacteric has been studied for 30 years. This research has approached the issue from different points of view, including biologic, psychiatric, anthropologic, and sociologic. The two main conclusions are that decreasing sexual activity in a woman results in part from decreasing sexual functioning of her male partner and in part from anatomic and physiologic changes associated with her menopause. The representative studies are summarized in Table 2.17–25 The large majority of these studies found a decrease in coitus and sexual interest of greater than 40% within a few years of the menopause.
Table 2.
Epidemiological Studies of Sexual Complaints in the Menopausal Female
| Kinsey et al, 195317 | 53% decrease in coitus 48% decrease in orgasm |
| Bottiglioni et al, 198218 | University Menopause Clinic in Bologna Five times as many postmenopausal women as premenopausal women had ceased having coitus Postmenopausal women reported coitus less satisfying, decline in orgasmic frequency, 79% decrease in sexual interest |
| McCoy et al, 198519,20 | 85% decrease in sexual interest |
| Sarrel and Whitehead, 19859 | 39% decrease in sexual interest |
| Bajuliye and Sarrel, 198621 | 250 black women in Lagos 40% increase in dyspareunia within one to three years of menopause and 47% loss of sexual desire; by nine years postmenopausal, 70% had ceased sexual activity compared with 10% of their premenopausal partners |
| Hällström et al, 197322 | 800 Swedish women Extensive medical, psychiatric, and psychologic evaluation 181 postmenopausal women had: marked decline in sexual interest, a decline in capacity for orgasm, an increase in dyspareunia, and a decrease in coital activity |
| Keep and Kellerhals et al, 197423 | 448 Swiss women Menopause led to a decrease in the frequency of sexual activity, decrease in the quality of the sexual experience; greatest decline was among the lower social classes |
| Hällström, 197724 | Longitudinal study of menopause in Sweden 52% decrease in sexual interest 20% decrease in orgasm frequency Decrements related to menopause and not to aging |
| Hällström and Samuelsson, 199025 | 33% decrease in sexual interest |
Physiologic Changes at Menopause and Their Effect on Sexuality
Hormones affect sexual arousal through sensory perception, central as well as peripheral nerve transmission and discharge, peripheral blood flow, and capacity to develop muscle tension. Impairment of this mechanism can lead to diminished sexual responsiveness, dyspareunia, decreased sexual activity, decline in sexual desire, and sexual aversion.
Decreasing estrogen affects the integrity of female reproductive tract tissues. Decreased vaginal lubrication and atrophic vaginitis result in dyspareunia. Decreased blood flow to the reproductive organs results in diminished vasocongestion. Progressive ischemia, thinning of the barrier layers of skin and mucous membrane tissue, loss of subcutaneous fat, and a shrinking introitus are among many changes which occur in the genital structures as a result of hypoestrogenemia. Extragenital effects include loss of pelvic muscle tone, decreased intraurethral pressure, a smaller bladder, and thinning of the mucous membrane lining of the bladder and urethra. These effects have been found to be somewhat ameliorated by continuing sexual activity despite no estrogen replacement. Women who were sexually active had less atrophy than those who were not.26 In general, the health of the vaginal tissues decline in the absence of estrogen stimulation, despite sexual activity.
The physiology of the sexual response changes with prolonged hypoestrogenemia. These changes include diminished and slowed clitoral reaction time, diminished or absent secretion by the Bartholin glands, delayed or absent vaginal secretion, decreased vaginal length, and decreased transcervical width as well as possible painful uterine contractions in women aged 60 years to 70 years. Lack of estrogen decreases blood flow to the genitalia, and one study found a 50% increase in vulvar blood flow measured ultrasonographically when estradiol treatment was initiated.27 Ovarian steroids affect nerve cell growth, proliferation, transmission time, and rate of discharge along nerve fibers. A hypoestrogenemic state results in altered nerve function. Possible clinical manifestations of change in peripheral nerve function in postmenopausal women are numbness, itching, clothing intolerance, increased 2-point discrimination threshold, paresthesia, loss of clitoral reaction sensation, and decreased capacity for orgasm.28,29 Ovarian steroids can also affect neurotransmitters centrally, although this topic is beyond the scope of this article.
All these changes affect desire, mainly through aversion. A postmenopausal patient’s experiences of persistent dyspareunia, postcoital bleeding, delayed or absent lubrication, and delayed or absent orgasm affect her motivation for sexual intercourse. Pain can cause vaginismus, a conditioned response to painful coitus. Lack of sexual relations due to physiologic change may then be further complicated by the effect of this condition on the marital relationship. Decline in sexual relations may cause a couple to respond or cope in ways that lead to further decline in coitus and further deterioration of the marital relationship.
Testosterone and Libido
Androgen levels in postmenopausal women decline over time. The impact of this decline on libido depends on the woman’s inherent biologic sensitivity to testosterone, her sexual history, and many other factors. Half of postmenopausal women continue to secrete appreciable amounts of testosterone from their ovaries, whereas the other half of postmenopausal women have negligible ovarian production of testosterone.30 In postmenopausal women who still secrete testosterone, testosterone levels may be approximately 50% lower than in premenopausal, younger women.31 Postmenopausal ovarian stromal tissue secretes testosterone but little to no androstenedione.32
The evidence that testosterone affects libido in women draws from clinical research on women who have lost ovarian testosterone production.33,34 The best known of that research was done by Sherwin35, who examined mood, memory, and libido before and after surgical oophorectomy in the absence of preexisting depressive illness. With regard to testosterone and libido, Sherwin35 found that in surgically menopausal women, women receiving estrogen-testosterone preparations reported higher levels of sexual desire and arousal and higher frequency of sexual fantasies compared with women treated postoperatively with estrogen alone or with placebo. Other research on replacement therapy in postmenopausal women described use of estrogen versus estrogen-testosterone and found that libido improved in the combined treatment group only.36–39 Evidence shows that to the degree loss of testosterone affects libido in postmenopausal women, testosterone replacement can improve libidinal functioning.40,41
Moreover, hormone replacement therapy itself can decrease libido through the effect of different forms of estrogen on sex-hormone-binding globulin (SHBG).42 In this circumstance, estrogen replacement stimulates production of SHBG and thus results in reduced levels of free estradiol and free testosterone. These reductions can cause return of hot flushes and dyspareunia as well as decrease in libido. The increase in SHBG can be ameliorated by prescribing a combined testosterone and estrogen preparation, by changing to an estrogen preparation that does not stimulate SHBG as greatly, or by prescribing testosterone along with the estrogen preparation the patient is already on.
Libido and the Psyche
Physiologic problems must always be treated despite presence of psychiatric illness, because these two factors can have an indistinguishably intertwined impact on libido and coital activity. Dyspareunia-related decrease in frequency of coitus can be the primary cause of marital problems and can present as a marital problem when in fact physiologic problems of menopause are the cause of the change in libido. Lack of libido due to low testosterone levels can induce the same type of marital conflict, a circumstance that can in turn mislead physicians into diagnosing a psychological problem as the cause of the lack of libido.
For depression or anxiety disorders to be the cause of decrease in libido, onset of the psychiatric illness must be established and correlated with the onset of sexual symptoms. Depression and anxiety in women may directly affect libido and sexual response through loss of desire and also may affect the woman’s sexual partner in that he stops initiating sexual relations. Libido can be affected by marital stress as well as by accumulated anger between the couple. Both these factors should be taken into account when evaluating decrease in libido.13 However, the chronicity of the coital problem and of the libidinal problem is a critical aspect of determining the cause of decreasing libido and frequency of coitus.
Many perimenopausal and postmenopausal women have untreated dysthymia, a new episode of depression, or an untreated anxiety disorder. Because of the high prevalence of these untreated psychiatric illnesses, the likelihood of psychiatric comorbidity in postmenopausal women is high.43
Many types of medication used to treat psychiatric illness can lead to a decrease in libido or orgasm. This issue will be reviewed in another article on the newer forms of antidepressant medication. Because prevalence of depression and anxiety disorders is higher in women than in men and often remains untreated, the probability of a comorbid psychiatric disorder developing in midlife patients is high. Consequently, evaluation for problems of libido requires in-depth evaluation for depression and anxiety as well as for marital discord.
Psychological barriers to continued sexual functioning can also exist. Women who did not find sex pleasurable before menopause may look forward to ceasing sexual activity after menopause. Women with problems in their marital relationships may have resentment toward their spouses, and menopause may give these women permission to decline sex. Some women were raised to believe that sexual relations end at a certain age, and altered body image due to atrophic changes can impact libido. Consideration of these factors is necessary for understanding libido and the psyche.44 For marital problems to be the cause of decrease in libido, the marital problems must precede the decrease in libido and must be somewhat long-standing.
Cultural issues
Cultural issues too can affect a woman’s view of herself and thus can affect her psyche as well as her libido. Societal attitudes toward sex in midlife affect behavior.12 A woman’s value as a sexual person increases or decreases postmenopausally according to the society in which she lives.12 In a Nigerian study, most of the older women became sexually abstinent.21 In contrast, older women in almost 25% of primitive societies were seen as less inhibited, became more sexually active, and were more attractive to young men. Thus, societal context can substantially affect women’s libido.21
Previous sexual functioning has also proved to be a predictor of future sexual functioning. Koster and Garde45 examined sexual wellness in Danish women aged 40, 45, and 51 years by in-person interview and by questionnaire and found that current frequency of sexual desire was highly correlated with former sexual activity. An additional finding was that anticipation of declining desire predicted decline in desire.
Sexual scripts may require people to adapt to the challenges of aging. Geriatric problems with health, pulmonary function, cardiovascular function, and mobility may all affect a woman’s ability to have sexual relations.7 Degree of comfort with alternative modes of sexual interaction may also affect her ability to have continued sexual relations.46
Summary
Coital and libidinal change can be singularly caused by anatomic and physiologic change associated with the climacteric—by psychiatric illness, by marital discord, or by a combination of all these factors. The ideal treatment for women in midlife is complete evaluation of the factors affecting sexuality and use of a combined treatment approach to ameliorate these factors. Use of such an individualized approach can enable the women in midlife to continue to have a satisfying sexual life, should they choose to do so.
Our Contemporary World
Everything, absolutely everything in our contemporary world, has been tailed to the measure of men.Eva Peron, 1919–1952, First Lady of Argentina, women’s suffrage and social activist
Eva Peron, 1919–1952, First Lady of Argentina, women’s suffrage and social activist
Footnotes
Presented at the Conjoint Annual Meeting of the American Society for Reproductive Medicine and the Canadian Fertility and Andrology Society 32nd Annual Postgraduate Program, Toronto, Canada, September 25–26, 1999, and published as a course handout to participants.
References
- 1.Goldstein MK, Teng NN. Gynecologic factors in sexual dysfunction of the older woman. Clin Geriatr Med. 1991 Feb;7(1):41–61. [PubMed] [Google Scholar]
- 2.Sarrel PM. Sexuality and menopause. Obstet Gynecol. 1990 Apr;75(4 Suppl):26S–30S. discussion 31S–35S. [PubMed] [Google Scholar]
- 3.Weissman MM, Klerman GL. Sex differences and the epidemiology of depression. Arch Gen Psychiatry. 1977 Jan;34(1):98–111. doi: 10.1001/archpsyc.1977.01770130100011. [DOI] [PubMed] [Google Scholar]
- 4.Weissman MM, Klerman GL. Gender and depression. Trends Neurosci [TINS] 1985 Sep;8(9):416–20. [Google Scholar]
- 5.Nolen-Hoeksema S. Sex differences in unipolar depression: evidence and theory. Psychol Bull. 1987 Mar;101(2):259–82. [PubMed] [Google Scholar]
- 6.Deamer RL, Thompson JF. The role of medications in geriatric sexual function. Clin Geriatr Med. 1991 Feb;7(1):95–111. [PubMed] [Google Scholar]
- 7.Mooradian AD. Geriatric sexuality and chronic diseases. Clin Geriatr Med. 1991 Feb;7(1):113–31. [PubMed] [Google Scholar]
- 8.Great sex: what’s age got to do with it? Modern Maturity. 1999 Sep-Oct;:41–5. 91. [Results of AARP / Modern Maturity Sexuality Survey conducted by NFO Research, Inc] [Google Scholar]
- 9.Sarrel PM, Whitehead MI. Sex and menopause: defining the issues. Maturitas. 1985 Sep;7(3):217–24. doi: 10.1016/0378-5122(85)90043-x. [DOI] [PubMed] [Google Scholar]
- 10.Barber HR. Sexuality and the art of arousal in the geriatric woman. Clin Obstet Gynecol. 1996 Dec;39(4):970–3. doi: 10.1097/00003081-199612000-00025. [DOI] [PubMed] [Google Scholar]
- 11.Pfeiffer E, Verwoerdt A, Davis GC. Sexual behavior in middle life. Am J Psychiatry. 1972 Apr;128(10):1262–7. doi: 10.1176/ajp.128.10.1262. [DOI] [PubMed] [Google Scholar]
- 12.Sarrel PM. Sexuality in the middle years. Obstet Gynecol Clin North Am. 1987 Mar;14(1):49–62. [PubMed] [Google Scholar]
- 13.Frank E, Anderson C, Rubinstein D. Frequency of sexual dysfunction in “normal” couples. N Engl J Med. 1978 Jul 20;299(3):111–5. doi: 10.1056/NEJM197807202990302. [DOI] [PubMed] [Google Scholar]
- 14.Sherwin BB, Gelfand MM. The role of androgen in the maintenance of sexual functioning in oophorectomized women. Psychosom Med. 1987 Jul-Aug;49(4):397–409. doi: 10.1097/00006842-198707000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Sarrel P, Dobay B, Wiita B. Estrogen and estrogen-androgen replacement in postmenopausal women dissatisfied with estrogen-only therapy. Sexual behavior and neuroendocrine responses. J Reprod Med. 1998 Oct;43(10):847–56. [PubMed] [Google Scholar]
- 16.Davidson JM, Gary GD, Smith ER. The sexual psychoendocrinology of aging. In: Meites J, editor. Neuroendocrinology of aging. New York: Plenum Press; 1983. pp. 221–58. [Google Scholar]
- 17.Kinsey Alfred C, et al., editors. Institute for Sex Research. Sexual behavior in the human female. Philadelphia: Saunders; 1953. [Google Scholar]
- 18.Bottiglioni F, De Aloysio D. Female sexual activity as a function of climacteric conditions and age. Maturitas. 1982 Apr;4(1):27–32. doi: 10.1016/0378-5122(82)90016-0. [DOI] [PubMed] [Google Scholar]
- 19.McCoy N, Culter W, Davidson JM. Relationships among sexual behavior, hot flashes, and hormone levels in perimenopausal women. Arch Sex Behav. 1985 Oct;14(5):385–94. doi: 10.1007/BF01542000. [DOI] [PubMed] [Google Scholar]
- 20.McCoy NL, Davidson JM. A longitudinal study of the effects of menopause on sexuality. Maturitas. 1985 Sep;7(3):203–10. doi: 10.1016/0378-5122(85)90041-6. [DOI] [PubMed] [Google Scholar]
- 21.Bajulaiye O, Sarrel PM. A survey of perimenopausal symptoms in Nigeria. In: Notelovitz M, van Keep PA, editors. The climacteric in perspective; Proceedings of the Fourth International Congress on the Menopause; Lake Buena Vista, Florida. October 28–November 2, 1984; Lancaster, Boston: MTP Press Limited; 1986. pp. 161–75. [Google Scholar]
- 22.Hällström T. Mental disorder and sexuality in the climacteric: a study in psychiatric epidemiology. Goteborg: Esselte studium; 1973. [Reports from the Psychiatric Research Centre, St. Jörgen’s Hospital; 6. Scandinavian University Books] [Google Scholar]
- 23.van Keep PA, Kellerhals JM. The impact of socio-cultural factors on symptom formation. Some results of a study on ageing women in Switzerland. Psychother Psychosom. 1974;23(1–6):251–63. doi: 10.1159/000286648. [DOI] [PubMed] [Google Scholar]
- 24.Hällström T. Sexuality in the climacteric. Clin Obstet Gynaecol. 1977 Apr;4(1):227–39. [PubMed] [Google Scholar]
- 25.Hällström T, Samuelsson S. Changes in women’s sexual desire in middle life: the longitudinal study of women in Gothenburg. Arch Sex Behav. 1990 Jun;19(3):259–68. doi: 10.1007/BF01541551. [DOI] [PubMed] [Google Scholar]
- 26.Masters WH, Johnson VE. Human sexual response. Boston: Little, Brown; 1966. [Google Scholar]
- 27.Sarrel PM. Progestogens and blood flow. Int Proc J; Proceedings of the Consensus Development Conference on Progestogens; Naples. 1988; 1989. pp. 226–71. [Google Scholar]
- 28.Rauramo L. In: van Keep PA, Lauritzen C, editors. Estrogens and psychic function; Ageing and estrogens; workshop conference in Geneva; October 5–6, 1972; Sponsored by the International Health Foundation, Geneva Basel. New York: Karger; 1973. [Google Scholar]
- 29.Sarrel L, Sarrel P. Sexual turning points: the seven stages of adult sexuality. New York: MacMillan; 1984. [Google Scholar]
- 30.Lucisano A, Acampora MG, Russo N, Maniccia E, Montemurro A, Dell’Acqua S. Ovarian and peripheral plasma levels of progestogens, androgens and oestrogens in postmenopausal women. Maturitas. 1984 Jul;6(1):45–53. doi: 10.1016/0378-5122(84)90064-1. [DOI] [PubMed] [Google Scholar]
- 31.Botella-Llusia J, Orio-Bosch A, Sanchez-Garrido F, Tresquerres JAF. Testosterone and 17 beta-oestradiol secretion of the human ovary. II. Normal postmenopausal women, postmenopausal women with endometrial hyperplasia and postmenopausal women with adenocarcinoma of the endometrium. Maturitas. 1997 Jan;2(1):7–12. doi: 10.1016/0378-5122(80)90054-7. [DOI] [PubMed] [Google Scholar]
- 32.Longcope C, Hunter R, Franz C. Steroid secretion by the postmenopausal ovary. Am J Obstet Gynecol. 1980;138:564–8. doi: 10.1016/0002-9378(80)90287-2. [DOI] [PubMed] [Google Scholar]
- 33.Plouffe L, Jr, Cohen DP. The role of androgens in menopausal hormone replacement therapy. In: Lorrain J, Plouffe L Jr, Ravnikar V, Speroff L, Watts N, editors. Comprehensive management of menopause. New York: Springer-Verlag; 1994. pp. 297–308. (Clinical perspectives in obstetrics and gynecology). [Google Scholar]
- 34.Sherwin BB. Impact of progestins on mood and cognition in women [abstract]. Presented at the: North American Menopause Society; Chicago, IL. September 26–28, 1996. [Google Scholar]
- 35.Sherwin B. Changes in sexual behavior as a function of plasma sex steroid levels in post-menopausal women. Maturitas. 1985 Sep;7(3):225–33. doi: 10.1016/0378-5122(85)90044-1. [DOI] [PubMed] [Google Scholar]
- 36.Cardozo L, Gibb DM, Tuck SM, Thom MH, Studd JW, Cooper DJ. The effects of subcutaneous hormone implants during climacteric. Maturitas. 1984 Mar;5(3):177–84. doi: 10.1016/0378-5122(84)90050-1. [DOI] [PubMed] [Google Scholar]
- 37.Cardozo L, Gibb DM, Studd JW, Tuck SM, Thorn MH, Cooper DJ. The use of hormone implants for climacteric symptoms. Am J Obstet Gynecol. 1984 Feb 1;148(3):336–7. doi: 10.1016/s0002-9378(84)80080-0. [DOI] [PubMed] [Google Scholar]
- 38.Burger HG, Hailes J, Menelaus M, Nelson J, Hudson B, Balazs N. The management of persistent menopausal symptoms with oestradiol-testosterone implants: clinical, lipid and hormonal results. Maturitas. 1984 Dec;6(4):351–8. doi: 10.1016/0378-5122(84)90008-2. [DOI] [PubMed] [Google Scholar]
- 39.Burger H, Hailes J, Nelson J, Menelaus M. Effect of combined implants of oestradiol and testosterone on libido in postmenopausal women. Br Med J (Clin Res Ed) 1987 Apr 11;294(6577):936–7. doi: 10.1136/bmj.294.6577.936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Graziottin A. Loss of libido in the postmenopause. Menopausal Med. 2000 Spring;8(1):9–12. [Google Scholar]
- 41.Davis SR. Androgen treatment in women. Med J Aust. 1999 Jun 7;170(11):545–9. [PubMed] [Google Scholar]
- 42.Nachtigall LE, Raju U, Banerjee S, Wan L, Levitz M. Serum estradiol-binding profiles in postmenopausal women undergoing three common estrogen replacement therapies: associations with sex hormone-binding globulin, estradiol, and estrone levels. Menopause. 2000 Jul-Aug;7(4):243–50. doi: 10.1097/00042192-200007040-00006. [DOI] [PubMed] [Google Scholar]
- 43.Jensvold MF, Halbreich U, Hamilton JA, editors. Psychopharmacology and women: sex, gender, and hormones. Washington DC: American Psychiatric Press; 1996. [Google Scholar]
- 44.Barbach L. Sexuality through menopause and beyond. Menopause Manage. 1996 Nov-Dec;5(5):18–21. [Originally published in: The pause: positive approaches to menopause by Lonnie Barbach Copyright © Lonnie Barbach, 1993 Dutton Signet/Penguin Books] [Google Scholar]
- 45.Koster A, Garde K. Sexual desire and menopausal development. A prospective study of Danish women born in 1936. Maturitas. 1993 Jan;16(1):49–60. doi: 10.1016/0378-5122(93)90133-3. [DOI] [PubMed] [Google Scholar]
- 46.Bachmann GA. Sexual issues at menopause. Ann N Y Acad Sci. 1990;592:87–94. doi: 10.1111/j.1749-6632.1990.tb30317.x. discussion 123–33. [DOI] [PubMed] [Google Scholar]