Abstract
This paper addresses the major developments in primary care in the Russian Federation under the evolving Semashko model. The overview of the original model and its current version indicates some positive characteristics, including the financial accessibility of care, focus on prevention, patient lists, and gatekeeping by primary-care providers. However, in practice these characteristics do not work according to expectations. The current primary-care system is inefficient and has low quality of care by international standards. The major reasons for the gap between the positive characteristics of the model and the actual developments are discussed, including the excessive specialization of primary care, weak health-workforce policy, the delay in the shift to a general practitioner model, and the dominance of the multispecialty polyclinic, which does not prove advantageous over alternative models. Government attempts to strengthen primary care cover a wide range of activities, but they are not enough to improve the system and cannot do this without more a systematic and consistent approach. The major lesson learnt is that the lack of generalists and coordination cannot be compensated for by the growing number of specialists in the staff of primary-care facilities. Big multispecialty settings (polyclinics in the Russian context) have the potential for more integrated service delivery, but to make it happen, action is needed. Simple decisions, like merging polyclinics, do not help much.
Keywords: health policy, primary health care, general practitioner, Semashko model
Introduction
Primary health care (PHC) is the first point of contact with health care where most preventive and curative health care needs are satisfied. This generalist care is focused on the person as a whole, instead of only one specific organ or health problem.1,2 There is evidence that countries with strong PHC systems have relatively higher indicators of health outcomes.3 Strengthening this sector is an important strategy for improving service delivery, including decreasing avoidable hospital admissions and emergency visits,4 and enhancing patient satisfaction. This is an important element of health policy throughout the world.5
Russia and most other postcommunist countries have inherited the Semashko model of primary care (named after the first Minister of Health in the USSR – Nikolai Semashko), dominated by publicly owned medical facilities, salaried health workers, large providers of PHC, and an exceptionally high degree of governmental administration. This system provides universal access to care, and thus has substantially improved the health status of the population relative to the starting point of its implementation in the late 1920s.6,7 However, in the USSR, health care was heavily underfunded and had a number of noticeable problems with the dominance of inpatient care, inefficient service provision, and weak incentives for providers.8,9 These problems have promoted the search for a new health-finance and -provision model.
After the collapse of the USSR in 1991, Russia introduced a social health-insurance system and started service-delivery restructuring with a focus on downsizing hospital capacity and moving patients to outpatient settings. Strengthening PHC was declared a priority in all the strategic documents of the transition period. However, the actual development of this sector has been slow and inconsistent. Contrary to postcommunist Central and Eastern European (CEE) countries, Russia developed its own system of primary-care development, emphasizing highly consolidated service provision in big multispecialty facilities and the dominance of public ownership. General practice is still in its infancy, while an attempt has been made to compensate for this with a growing number of specialists in primary-care settings. Currently, PHC is a complex mix of inherited and new institutions, which together make a model that is an alternative to the prevailing European model of self-employed GPs or group practices.2
International literature on PHC in Russia is limited. The papers available state that the country has a strategy of incremental reforms.10,11 Some papers have explored the priority of PHC in the overall health care system, and concluded that actual monetary support has lagged behind political declarations. Specialty care still prevails in Russia and other former Soviet countries.12 Most authors conclude that the Semashko model has remained practically untouched,10–12 although this is not entirely true. This model has evolved significantly, but not always positively.
Another body of literature has compared PHC internationally. The Primary Health Care Activity Monitor in Europe (PHAMEU), which includes nine CEE countries, concludes that the traditional division between “East and West” is disappearing. Estonia, Lithuania, and Slovenia are among the countries with the strongest PHC systems in Europe.2 A number of papers address the specific characteristics of PHC transformation, including GP task profiles13–15 and the growing variety of primary-care practices.16
This analysis does not cover Russia or other former Soviet Union countries with similar health systems, such as Belarus, Ukraine, Kazakhstan, and Armenia. This is a serious gap in the literature, since these countries have a specific model of PHC. This paper fills this gap. Our objectives are twofold: first, to highlight the characteristics and developments of the Russian PHC model, and second, to look at the outcomes of this model from an international perspective and discuss their strengths and weaknesses. An overview of key primary-care characteristics is provided, followed by a presentation of the major problems of the sector and recent efforts to ameliorate them, and then a comparison of the efficiency and quality of primary care internationally. We conclude with a discussion of this model and lessons learnt.
The analysis is based on a review of the literature on PHC developments, as well as the materials from the Russian federal and regional ministries of health. Recent plans to strengthen this sector are also evaluated. Statistical analysis is based on national data. World Health Organization and Organization for Economic Cooperation and Development (OECD) databases are used to compare economic conditions, workforce developments, and efficiency. The comparison of the comprehensiveness of PHC is based on the methodology of the PHAMEU2 and a survey of 171 primary-care physicians from 14 Russian regions. A list of questions from the European report was distributed through the Russian social network Vkontakte in May 2016 and then supplemented with face-to-face interviews with 20 physicians in Moscow polyclinics. The sample of respondents was developed with specific selection criteria. As such, a descriptive analysis was supplemented with a survey and interviews.
The authors are deeply involved in developing the national health care strategy in the capacity of independent experts. This paper summarizes the current approaches to strengthen PHC. Our major motivation to produce this paper is to share information on recent developments in Russia with policy makers in countries that have delayed major reforms of primary care and are now looking for the ways to catch up with the European mainstream. Another motivation is to revisit the Semashko model (which is usually criticized in the literature) and to compare its original design with the actual implementation.
Major characteristics of the Russian primary-care system
The major principle of the Semashko model is the financial accessibility of care. This has not been questioned in modern Russia. All citizens are entitled to free health care. However, the health system is heavily underfunded. Public health funding is currently only 3.5% of GDP, while in European countries it is 6%–10%.17,18 Limited financial resources undermine the principle of financial accessibility. People often have to pay formally and informally. The share of private funding is 39% of total health care expenditure against an average 24% for Europe.17,18 The share of outpatient care is much lower than for inpatient care. Most visits to the doctor and diagnostic tests are free.
The governance of PHC is centralized at the level of regional governments. This is seen as a way to consolidate resources and mitigate imbalances across communities in the region (There are 85 regions in the country with the population ranging from 500,000 to 12 million. Each region has 10-20 local communities [municipalities]). The downside is that the role of communities is insignificant: most decisions are made by regional health authorities and territorial social health-insurance funds that act as major purchasers of care. Attempts to decentralize governance in the 1990s were not successful, given serious underfunding and the geographic inequity of economic capacity.19
A major provider of PHC is the multispecialty, publicly owned polyclinic. This is usually much bigger than traditional general practices in Western countries. The capacity of polyclinics varies from 100 to 120,000 people served in big cities to fewer than 15,000 in small towns and rural areas. PHC for adults and children is separated, with separate adult and child polyclinics operating in urban areas. District therapists serve adults and district pediatricians serve children (together they are further referred to as district physicians [DPs]). GPs or family doctors are relatively rare.
Polyclinics provide primary and specialty care for uninfectious diseases and preventive services. The “district service” is a structural unit of polyclinics with a staff of DPs, GPs, and nurses. In the original Semashko model, DPs were the sole providers of primary care, but currently specialists provide a greater volume of care in polyclinics. Depending on the size of the policlinic, there are five to 20 categories of specialists providing most of the polyclinic’s services: 60%–65% of visits.20 Most polyclinics have diagnostic units (eg, laboratories, endoscopy) and units that are responsible for preventive services and health promotion. Patients of polyclinics have access to a wide range of services under the same roof.
People can choose a polyclinic, and most choose the provider closest to their place of residence. Patients enrolled in a polyclinic form the patient list. DPs and GPs have smaller catchment areas, while specialists serve all the enrollees of the polyclinic. The patient list is an important characteristic of the system. It existed in the original Semashko model, and has not been questioned since. Polyclinics are responsible for their enrollees’ health care on a long-term basis, which is usually regarded as the indicator of strong primary care.2,10,15
According to federal regulations, DPs and GPs act as “gatekeepers” and refer patients to specialists and hospitals. This is also a characteristic of a strong PHC system, since it ensures the coordination and continuity of care provided at various levels of service delivery.2,10,15 The gatekeeping function was in the design of the original Semashko model, but currently it is not strictly followed in many regions. As the following section shows, patients can see some specialists directly without a referral from primary-care physicians.
The Semashko model considers prevention, a major area of primary care and the scope of preventive activities, has been increasing. A recent innovation is a large-scale federal program of “dispensarization” (a term from the original Semashko model), which includes a wide range of checkups and screenings and covers around a third of the population. Each polyclinic enrollee is supposed to have them once every 3 years. Program monitoring is based on the number of detected cases of disease, including those at an early stage.21
A special characteristic of the Semashko model is the “method of dynamic dispensary surveillance”. This method presumes that every detected case of a serious disease is subject to a certain set of protocols, including planning curative activities, documenting them, ensuring the required number of contacts with DPs and specialists, a monitoring process, and outcome indicators. The design of these protocols (they were developed in the late 1960s) has some resemblance to the modern programs of chronic-disease management that are common in many Western countries,22,23 although they do not include some elements of these programs, such as multi-specialty groups of providers, distant monitoring of patients’ status, and bundled payment. This method was relatively well developed in the USSR, but in the decades since it has given way to the large-scale detection of new cases under the program of “dispensarization” without clear follow-up targets.
The original Semashko model was based on total public ownership of medical facilities and on medical workers as employees. The situation has changed over the last two decades. The number of private providers has increased substantially, mostly in the area of outpatient specialty care. But their share of the total number of physician visits remains low – 6.4%. Most physicians in private facilities are employees, similarly to public facilities. The bulk of services provided by private facilities is for out-of-pocket payment. The involvement of private providers in the provision of publicly funded care is limited to around 4%.24 The principles of patient lists and gatekeeping do not extend to private settings: they operate without catchment areas, do not have any commitments for the constant management of cases, and most contacts do not require primary-care referrals. GPs are equally uncommon in private settings.
PHC in Russia is much broader than was presumed by the original concept (as mostly generalist care). It is also broader than in most Western countries. The concept of “extended primary-care composition” advocated by some international scholars10 in Russia has reached the form of multispecialty polyclinics. The federal law “On the basics of health protection in the Russian Federation” (2011) conceptualized extended primary care by introducing the concepts of primary physician care and specialized primary medical care. The former is provided by DPs and GPs, the latter by polyclinic specialists.
These concepts mean that the borders of PHC and outpatient care practically coincide, while in Western countries a distinction between outpatient and primary care remains even in extended PHC systems: outpatient care is significantly wider in scope and totally different in function and clinical areas. Specialists do neither act as gatekeepers and coordinators of care, nor do they provide comprehensive care focused on the patient as a whole. Most importantly, specialists are not responsible for the ongoing surveillance of patients; rather, they provide episodic care. Even when specialists are first-contact physicians, all other characteristics of PHC are absent or limited.
The extended composition of PHC is the major distinction of its organization in Russia. The other basic features of the system – financial accessibility, patient list, gatekeeping, preventive-care orientation, ongoing surveillance of serious cases – can be regarded as indicators of a strong PHC system. Contrary to many criticisms of the Semashko model of primary care, it was originally well designed by modern standards. However, Russia currently faces a lot of problems with the implementation of this design.
Current activities to strengthen primary care
The government is attempting to solve PHC problems in the following directions:
overcoming the shortage of DPs and improving their competence;
improving polyclinic performance;
strengthening preventive activities;
closing the gap between urban and rural PHC;
increasing the remuneration of primary-care physicians.
Overcoming the shortage of primary-care physicians and improving their competence
The worldwide tendency of specialization of the health workforce and a decrease in the share of generalists25,26 is particularly strong in Russia. This tendency started in the USSR in the 1970s and continues today. Most clinical functions of DPs have been delegated to specialists, and the number of the latter has increased to a level where specialists outnumber other doctors in such polyclinics as PHC facilities. DPs have turned into the internal medicine specialists dealing with the simplest cases and losing their core position in PHC.27
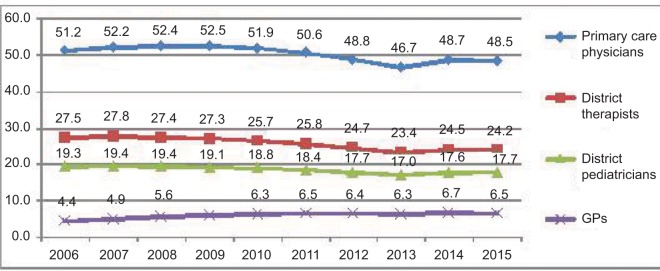
A shift to a GP model was declared in the 1990s, but then gave way to reservations about this model. It is seen as appropriate mostly for rural areas and small urban neighborhoods. The actual implementation of this shift has been very inconsistent, contrary to most CEE countries, which have trained enough GPs to replace DPs during the 8–10 years of transition.13 The number of GPs in Russia in 2014 was only 0.7 per 10,000 residents compared to an average of 8.7 in the pre-2004 EU and 5.7 in the post-2004 EU.17 The total number of primary-care physicians (DPs and GPs) per resident has been decreasing. This decrease over the last 10 years has not been compensated for by the insignificant increase in the number of GPs. The latter still have a marginal role in PHC. They account for only 13% of the total number of primary-care physicians (Figure 1).
Figure 1.
Number of primary-care physicians per 100,000 population between 2006–2015 in Russia.
Notes: Data from The Russian Federation Ministry of Health.39
Regulation of the supply of health workers in Russia is poorly focused on primary care. Medical universities have substantial discretion in setting the structure of undergraduate and postgraduate training. A study of medical university capacity indicated that in 2016, only 20% of universities had general practice as a subject in undergraduate medical training and only 70% had postgraduate positions in general practice, while in European countries all medical schools have this subject for undergraduates and postgraduates.2 The proportion of students that choose to become GPs in Russia is <5%, while the average figure for 31 European countries is 17% and in some countries (eg, France) is 35%–45%.28 Our estimate of the shortage of DPs is 33%, and for district pediatricians 12%. The estimate is based on the standards of the enrolled population – 1,700 for district therapist and 800 for district pediatrician. To meet these standards, the country needs 90,600 DPs, but the current number is only 60,600. The physicians available have to hold more than one position and are thus overburdened. The average number of residents served by district therapists is 2,630 patients, which is about 50% higher than the target (1,700 residents) established by the Russian federal Ministry of Health (MoH).
Apart from the inadequate number of DPs, their task profile is limited by Western standards. To measure the comprehensiveness of care (ie, competence to treat a set of diseases), we rely on the indicators that were used by the PHAMEU in 31 European countries2 and the aforementioned survey of Russian DPs. A major indicator of PHC comprehensiveness is the percentage of total contacts with patients handled solely by primary-care physicians without referral to specialists. Russian DPs were asked to make this estimate for their own practices. The average share for all respondents was 70%. This is a very optimistic estimate. However, it is substantially lower than in most European countries, where 85%–95% of contacts are handled by general practitioners without the involvement of specialists.2 Other indicators of comprehensiveness are also relatively low in Russia.29 This can be interpreted as a result of the excessive specialization of PHC and the inadequate training and professional development of DPs.
The government is looking for ways to overcome the shortage of DPs and strengthen their clinical capacity. The strategy of health-workforce development includes a shift to 2–5 years’ postgraduate training, continuous postgraduate training to replace periodic training, the development of a new system of accreditation, and strengthening the role of medical associations in accreditation.30 These are the activities planned for the medium term. The immediate action (which started in 2017) is loosening the requirements to work as a DP. Most medical graduates are accredited for practicing as DPs without postgraduate training. The new approach may mitigate the shortage of DPs in the short run, but at the expense of the quality of primary care. No other country fills vacancies of primary-care physicians through loosening the requirements for practice. The most important alternative approaches are economic incentives and the regulation of postgraduate training by promoting postgraduate training of general practitioners.25,31
Improving polyclinic performance
As major PHC providers, polyclinics are underfunded. While having a low share of public health expenditure in GDP, Russia spends more on inpatient care than outpatient care: 50.3% and 33.2% respectively.32 The financial priority of this sector is relatively low. Underfunding is the major reason for the inadequate infrastructure of primary care, the lack of diagnostic capacity and modern IT, with the resultant long waiting times, and rationing and underprovision of services. There are problems with inadequate patient-flow logistics, the appointment system, and the division of labor between physicians and nurses and between individual units of polyclinics.
Contrary to expectations, polyclinics do not integrate the coordination or continuity of care. Based on a survey of physicians in 2012,33 there was service-delivery fragmentation:
the joint development of patient management plans by DPs and specialists was very rare, ie, they did not work cooperatively;
the frequency of direct patient visits to specialists bypassing DPs was high, which can be interpreted as the result of lack of coordination of the latter;
the frequency of timely feedback of specialists to a referring physician on the results of treatment was very low, which indicated a low level of teamwork and continuity of care;
the level of awareness of polyclinic physicians of their patients’ hospital admissions and emergency visits was low, which limits the scope for integrative care.
The government is currently dealing with the most obvious areas of polyclinic inefficiency. There are two major directions for these activities. The first is the consolidation of service delivery through merging polyclinics into big local complexes. The reason for this consolidation is to concentrate expensive diagnostic equipment and specialists (that are in short supply) in big facilities, thereby increasing their accessibility. The second direction is to improve the organization of service delivery in the polyclinics themselves.
The first strategy is particularly strong in Moscow. Since 2011, 452 polyclinics have been merged into 46 outpatient centers for adult care, with a catchment area of 250–300,000 enrollees each. A total of 40 child-outpatient centers have been established, with 30,000–50,000 enrollees each.34 The enrollees of these centers now have better access to a wider range of polyclinics, including those where major diagnostic equipment is concentrated. The number of computed tomography tests doubled from 2010 to 2014, while magnetic resonance imaging tests tripled. The waiting time has become much shorter (Table 1).
Table 1.
Number of diagnostic tests and waiting time in 2010 and 2014 in Moscow city outpatient centers34
| Number of tests, thousand
|
Average waiting time, days
|
|||
|---|---|---|---|---|
| 2010 | 2014 | 2010 | 2014 | |
| CT | 278.8 | 570.9 | 60 | 15 |
| MRI | 59.2 | 197.5 | 50 | 16 |
| Ultrasound devices | – | – | 10 | 7 |
Abbreviations: CT, computed tomography; MRI, magnetic resonance imaging.
Access to polyclinic specialists has improved. The waiting time for consultations reduced by 2–3 times in 2010–2014, while their number remained constant. Improved access can be accounted for by organizational changes rather than additional financial input.34 Merging polyclinics in Moscow has allowed three levels of service delivery to be developed: DPs plus some categories of specialists – cardiologists, ophthalmologists, surgeons, and urologists – who are accessible to patients without referral, most other outpatient specialists who work in designated units of outpatient centers, and outpatient departments of hospitals where the best specialists are concentrated. These are linked to each other by a referral system. The Moscow health department regulates the “routes” of patients and establishes referral patterns according to the availability and workload of PHC physicians. When they are too busy, direct access to some specialists is allowed. A new information system has been introduced to support this organizational scheme.
Following the restructuring of the polyclinics, patients have to travel further to reach the outpatient center where diagnostic and specialty services are provided. However, shorter waiting times are probably a more important indicator of better access to these services. In addition to these activities, the following innovations have been introduced:34
Visits to patients’ homes previously made by DPs have been shifted to a special home-visit service, which is a separate unit. This service is staffed with physicians and nurses who specialize in this service. There are two objectives of this innovation: to reduce the burden on DPs and allow them to spend more time with patients in their offices, and to redistribute emergency calls from the centralized city emergency service to the polyclinics, which are closer to the patients and less costly.
Patients can make an appointment with any DP, rather than to a regular doctor. The objective is to encourage patient choice and facilitate access to care.
The position of duty physician has been introduced in polyclinics. This physician is responsible for the provision of care to those who need health care, but do not have an appointment.
Nurses’ posts have been established for concentrating routine activities.
IT has been introduced to facilitate appointments, medical records, prescriptions, and communication among providers within polyclinics. Completion of this process is planned for 2018.
A separate unit for managing chronic multimorbidity cases is being piloted in a few polyclinics.
These innovations have reorganized polyclinics through the specialization of some curative and organizational functions. The positive part of this process is the possibility to increase physicians’ productivity and allow them to spend more time with their patients. This is particularly important for DPs, who are heavily overburdened.
The negative side is the risk of further decreasing the role of DPs as core providers of PHC. With a narrowing area of gatekeeping, they are losing their responsibility for patient lists. Patients increasingly have to deal with physicians who do not know them, which makes health care even more fragmented. Reservations about this process were made public by a group of Moscow district therapists. They urged that the fundamental principle of a patient list and gatekeeping are undermined by delegation of DP functions to other personnel.50
The second direction of PHC reform is represented by “Resource-saving polyclinics”. The objective is to make PHC more patient-oriented and increase the efficiency of internal processes in polyclinics. Currently, the project is being piloted in three regions (Yaroslavl and Kaliningrad oblasts and Sebastopol city), and is planned for the entire country. It includes the following activities:35
delegation of some physicians’ functions to nurses;
improving logistics in polyclinics, including more careful separation of patient flows across individual providers;
improving the appointment system;
introducing electronic communication and reducing the amount of paperwork;
new structural units for preventive activities.
The 2 years of this project (2015–2016) gave promising results. According to the MoH, the average time of physicians’ contact with patients doubled in these regions, appointments with physicians were easier to make, and patient waiting time reduced by a factor of 12.35
Strengthening prevention and health promotion
Although prevention has traditionally been an important characteristic of primary care, a new wave of preventive activities started in the current decade, focusing on the detection of new cases under the “dispensarization” program. The substantial coverage of the program increased the number of detected new cases more than sevenfold in 2015 relative to the start of the program in 2012. Identification of the first and second stages of cancer was 60%–80% of the total number of new cancer cases.36
Substantial results have been achieved in the area of health education. Polyclinics are increasingly involved in promoting healthy lifestyles. Together with some regulatory initiatives (decreasing smoking and alcohol abuse, encouraging healthy diets, and building new sport grounds in residential areas), the new policy reduced the sales of alcohol from 10.7 L per capita in 2011 to 8.7 in 2015. The share of smokers reduced from 35% of the adult population in 2014 to 31% in 2016. Over the last 15 years, the share of people who are regularly involved in physical exercise has tripled, and is now close to 30%.37
The unsolved problem is the lack of consistency in the implementation of the principle of dynamic dispensary surveillance of detected cases. No more than half the cases with indication of a serious disease detected under the program are covered by constant management by primary-care providers,21 ie, follow-up activities are still limited. Moreover, these activities are not even planned or monitored by the program. In spite of large-scale preventive measures, a substantial number of acute cases become chronic without appropriate management. Chronic-disease management covers only 10.6% of myocardial infarctions, 23% of unstable cardiac angina, and 43.6% of ischemic heart disease. The target outcomes of these measures are not specified, and there is a lack of teamwork among specialists.38 Therefore, the program’s positive effect is partly devalued.
Improving primary care in rural and remote areas
An attempt has been made to mitigate the gap between the supply of health workers in urban and rural areas. Physicians are encouraged to work in rural areas through lump-sum compensation for housing costs under the “Rural physicians” program. The number of rural physicians increased from 44,758 in 2011 to 55,812 in 2016.35 However, these attempts have so far had limited effect. The number of physicians willing to participate in the program decreased from 7,413 to 4,922 in 2016. A substantial gap in physician-population ratio in urban and rural areas still remains: 45.2 vs 14.5 per 10,000 residents.39 It is clear that the economic incentives are not strong enough to compensate for the low basic salary of rural physicians and lack of possibilities for professional development.
PHC in remote areas where a substantial number of people live is also to be strengthened. The MoH has issued a regulatory act on requirements for the location of medical facilities with specific targets of PHC accessibility in terms of the maximum distance between residential areas and medical facilities. Each region of the country has developed a road map to reach these targets in the next 3–4 years. Mobile health units are being organized. Each residential area will be equipped with emergency communication. The first steps have been made to establish health telecommunication.40,41
New policy of health-worker remuneration
Russia inherited the low Soviet remuneration of health workers. Until recently, the salary of physicians was only 25% higher than the national average (compared to two to five times higher in Western countries).18 Nurses’ salaries are 27% lower, and medical assistants 52% lower. The average salary of primary care physicians is traditionally much lower than their counterparts in hospitals. A deeply rooted perception of physicians as a “cheap” health care resource has traditionally limited the motivation to work in primary care.42
In 2012, a presidential decree initiated an ambitious project to increase the average salaries of physicians to 200% of the average wage in the economy of the region where they work by 2018, and salaries of nurses and medical assistants to 100%. Targets were successfully reached in the first years of this project (2012–2015), but then progress slowed, due to the economic crisis. The original targets are most likely to be reached in 2018, a presidential election year.
Another innovation is the “effective contract”, a Russian version of pay for performance. Health authorities and polyclinic managers developed a set of performance indicators for each category of health workers and pay them for reaching these indicators. The major indicators for primary care include the number of physician visits, rate of hospital admissions and emergency calls across polyclinic catchment areas, and number of cancer and TB cases detected at early stages. The results of patient surveys are also taken into account. The range of these indicators varies across regions and individual polyclinics. According to the MoH, 83% of employees are currently covered by an effective contract.35
The actual outcome of this policy remains unclear. Many polyclinics use pay-for-performance schemes that are designed to create collective incentives for better performance, rather than incentives for individual employees. In the first years of the program (2012–2015), additional funding for increasing salaries was poorly linked to performance, and thus most of the increase in average salary was not related to the target indicators. Currently, there is a search for new incentives.37
In contrast to Western countries, where the basic salary makes up the bulk of remuneration, with concerns about too much focus on pay for performance in some countries,43 in Russia the basic salary is low. For example, polyclinic physicians in small cities often have an average basic salary of US$200–300 per month. Bonuses added to a low basic salary will not radically change the motivation of physicians. A national survey of physicians in 2013 indicated that only 20% of them were ready to work more effectively with the available bonuses and that most were seeking a higher level of basic salary.44 This perception has been taken into account in the recent recommendations of the MoH to increase the share of basic salary to 85%–90% (including payment for special conditions). Even with all these inconsistencies and contradictions, the effective contract is viewed positively by most health workers. This innovation, together with the centralized policy of remuneration, may encourage better performance by primary-care providers.
Efficiency and quality of primary care
The OECD report4 uses the following indicators of PHC efficiency: hospital-admission rates, volumes of inpatient care, and frequency of emergency care because of the unavailability of primary care. The presumption is that stronger PHC systems are more likely to reduce demand for inpatient and emergency care. The major indicator of quality is patient satisfaction with regular primary-care physicians. We use a similar approach to evaluate the performance of primary care in Russia.
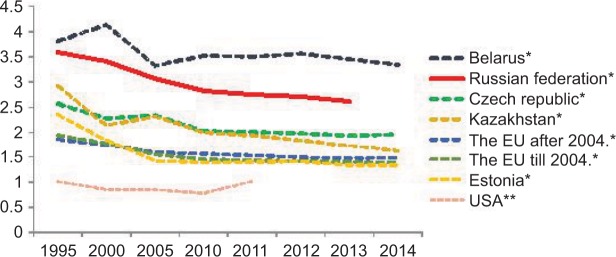
The major long-term positive outcome is a decrease in inpatient care. This trend is even stronger than it is internationally (Figure 2). However, the dominance of hospitals in the Russian health care system remains. There is a strong public perception that quality care is provided only in inpatient facilities. The competence of primary-care physicians is often questioned by patients. The capacity of polyclinics is not always enough to take on cases that are no longer treated in hospitals after their capacity was reduced. Therefore, in spite of the hospital restructuring, the number of bed-days per capita remains 70%–75% higher than in the EU and nearly three times higher than in the US. Russia uses more inpatient care relative to most CEE countries, which had similar indicators at the start of transition to a new model of service delivery. Only Belarus has even higher indicators. Both Russia and Belarus used a very conservative strategy of primary-care development during the transition period.11,12
Figure 2.
Number of bed days per capita in all inpatient-care facilities in Russia and selected countries in 1995–2014.
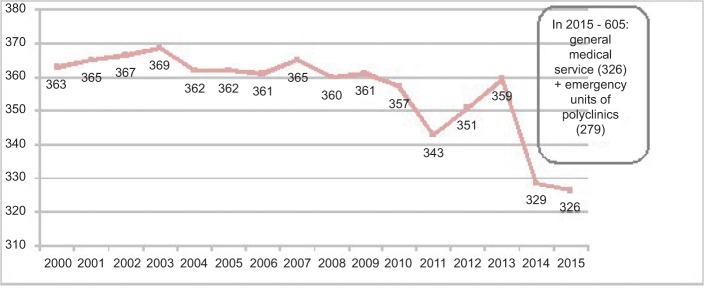
The number of emergency visits per 1,000 residents in Russia was stable during 2000–2013 and then went down sharply (Figure 3). This decrease was the result of shifting a substantial portion of emergency visits from the general medical emergency service (a separate institution) to polyclinics where special emergency units had been established. In 2015, these units provided 279 emergency visits per 1,000 residents, in addition to 326 emergency visits made by the general emergency service. This makes a total of 605 emergency visits per 1,000 residents. Therefore, the total frequency of emergency visits has increased.
Figure 3.
Emergency care visits rate per 1,000 population of Russia in 2000–2015.
Notes: Data from The Russian Federation Ministry of Health.40
This indicator can be approximately compared with the “proportion of residents who visited an emergency department because primary care was not available” from the OECD report for Europe as an indicator of primary-care strength. The average of this proportion is 23% for 26 EU countries, with most countries ranging between 8% and 30%.18 We tentatively conclude that in Russia, the frequency of emergency visits is nearly three times higher than the average for OECD countries.
The Levada Center (one of the biggest sociological organizations in Russia) survey indicated that in mid-2016, 44% of respondents were dissatisfied with the length of visits to polyclinics and 63% with the qualifications and number of polyclinic physicians.45 Similar estimates for European countries indicate that 80%–90% of respondents are satisfied with their GPs.2 Over the last decade, Russia has achieved substantial improvements in health indicators – total and specific disease mortality – and life expectancy. This is the result of the economic growth in the early 2010s and additional health funding; however, these indicators are still substantially lower than in Western countries.37
Discussion
Primary care in Russia was originally well designed under the Semashko model. Financial accessibility, a focus on prevention, including the dynamic dispensary surveillance method, patient lists, and gatekeeping made the system potentially strong. However, in practice, this potential is not fulfilled. The gap between expectations regarding the prevailing model of service delivery and its actual implementation has increased over the last few decades. The model does not ensure the efficiency or quality of care. There is substantial evidence of the low priority of PHC, a shortage of DPs, low economic incentives for medical workers, and a gap between urban and rural areas. The detection of new cases under a large-scale prevention program is not followed by their management, contrary to the original design of the system. The gatekeeping function of primary-care providers is weakening.
The current problems of PHC have nothing to do with the original design of the Semashko model; rather, they are deeply rooted in the long-term developments that started in the USSR and continued in modern Russia. First, specialization in PHC, common in many countries, has gone too far in Russia. Specialists have replaced a substantial number of DPs, rather than supplementing them. This process has resulted in a decline in DPs’ clinical areas and their coordination function. They are no longer in the driver’s seat10 in big multispecialty polyclinics. Importantly, the new division of labor in primary care does not compensate for the shortage of DPs, because specialists usually deal with episodic demand and have limited commitment to the constant surveillance of patients’ health needs and comorbidity cases. The need for strong generalists has not diminished.
Second, the government has lost the leverage to regulate the supply of physicians. Postgraduate training is skewed toward specialists, particularly those who provide private services (eg, dentists, urologists), while the number of generalists in training is falling. The structural imbalances in supply have become a characteristic of the current health system,42 which reflects the lack of strategic vision in the governance of the system.
Third, the country has missed the shift to the GP model, which has allowed CEE countries to extend the comprehensiveness of primary care.29 In Russia, the presumption was that generalists can be strengthened by a growing number of specialists in the model of multispecialty polyclinics. But this has not happened. The narrow clinical area of DPs, together with their shortage, generates demand for the growing number of specialists and eventually leads to a shortage of specialists as well, creating the vicious circle of shortages. The current attempt to fill the vacancies of DPs with graduates of medical universities without postgraduate training is a manifestation of this process. The alternative to this approach is to train the required number of qualified GPs with an extended clinical area and make them major providers of primary care. This will take a few years, but cannot be avoided.
Finally, the model of the multispecialty polyclinic as the major provider of PHC has not changed in the transition period and is not questioned now. Although this model is promising for the integration of care, its potential is dependent on the coordination of care, its continuity, and the joint work of individual providers. There is a substantial body of international evidence on this point.46–48 Recent attempts to consolidate polyclinics into bigger entities is not a panacea for inefficient service delivery. The first evidence of its impact is contradictory: better access to expensive diagnostic resources is coupled with a growing demand for specialty care and a loosening of the coordination of primary-care providers. The same holds true for organizational restructuring. The positive part of this process is the possibility to increase physicians’ productivity and the amount of time spent with their patients. The negative side is the risk of further dismantling the role of DPs as core providers of primary care. They are losing their patients, who are increasingly having to deal with physicians who do not know them well, which fragments health care even more. This is a corollary of the excessive specialization of primary care.
The comparison of primary care models in Russia and CEE countries29 does not demonstrate the strength of polyclinics relative to the smaller settings of solo- and group-GP practices, which dominate most CEE countries. Apart from the lack of evidence of higher integration, there is the problem of weak economic incentives in polyclinics. The recent innovations of pay for performance are not related to the comprehensiveness of care, and thus do not provide incentives for professional development. The salary of GPs is only 10%–15% higher than that of DPs. The economic “signal” for an entire facility does not reach individual physicians and nurses in a big setting.49
The polyclinic model has created a new category of specialists that provide only outpatient care and thus have limited professional competence (eg, nonoperating urologists in polyclinics). In the absence of GPs with a wide clinical area, specialists work with simple cases and most specialists are not affiliated with hospitals; therefore, their incentives for professional development are limited. A polyclinic is an administrative body, rather than a voluntary cooperative of physicians in group practices. They are headed by administrators who make decisions on patient lists for individual DPs, determine the scope of preventive services, ration diagnostic resources for each physician, and set salaries. This administrative pressure does not fit with the work of PHC providers: the sole responsibility for the health of patients on the list, a wide variety of activities that are not easy to predict (eg, interaction with families, community, specialists), and the high level of creativity that is needed to ensure the successful management of cases. Not surprisingly, newly trained GPs usually feel uncomfortable in polyclinics. Some of them prefer the position of DP.
Conclusion
Russian primary care has evolved from the Semashko model to a model that has lost some of the positive characteristics of the original and does not ensure efficient and quality care. This can be attributed to the excessive specialization of primary care, weak health-workforce policy, delays in the shift to a GP model, and the dominance of the multispecialty polyclinic, which has not proved better than alternative models. Some of the attempts to strengthen PHC are promising, but they are not enough to compensate for the lack of strategic vision in previous decades. More systematic and consistent reforms are needed. Major lessons learnt are:
The low priority of primary care generates demand for specialty care and eventually results in structural imbalances in the entire health system.
The lack of generalists and coordination cannot be compensated for by the growing number of specialists on the staff of primary-care facilities.
Big multispecialty settings (polyclinics in the Russian context) have the potential for better service-delivery integration, but to make this happen, action is needed. Simple decisions, like merging polyclinics, do not help much.
Delegating some functions of primary-care physicians to other categories of medical personnel may or may not contribute to higher performance of primary-care facilities, depending on how this delegation is managed.
Acknowledgments
This paper is an output of a research project implemented as part of the Basic Research Program at the National Research University Higher School of Economics (HSE) in Moscow, Russia.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Starfield B. Primary care: concept, evaluation, and policy. New York: Oxford University Press; 1992. [Google Scholar]
- 2.Kringos D, Boerma W, Hutchinson A, Saltman R. The European Observatory on Health Systems and Health Policies. Vol. 1. WHO; 2015. Building primary care in a changing Europe. [PubMed] [Google Scholar]
- 3.Macinko J, Starfield B, Shi L. The contribution of primary care systems to health outcomes within Organization for Economic Cooperation and Development (OECD) countries, 1970-1998//Health Services Research. 2003;38:831–865. doi: 10.1111/1475-6773.00149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.OECD (2016) Health at a Glance: Europe. 2016. [Accessed September 26, 2018]. http://www.oecd-ilibrary.org/social-issues-migration-health/health-at-a-glance-europe_23056088.
- 5.World Health Organization . World Health Report 2008: Primary Care Now More than Ever. Geneva: 2008. [Google Scholar]
- 6.Davis C. The organization and performance of the contemporary Soviet health system. In: Lapidus G, Swanson G, editors. State and Welfare, USA/USSR: Contemporary Policy and Practice. Berkeley: University of California; 1988. [Google Scholar]
- 7.Twigg J. Balancing the state and the market: Russia’s adoption of obligatory medical insurance//Europe-Asia Studies. 1998;50:583–602. [Google Scholar]
- 8.Sheiman I. New methods of financing and managing health care in the Russian Federation//Health Policy. 1995;32:167–180. doi: 10.1016/0168-8510(95)00734-a. [DOI] [PubMed] [Google Scholar]
- 9.Telyukov A. A concept of health-financing reform in the Soviet Union. International Journal of Health Services. 1991;21:493–504. doi: 10.2190/XH2D-D6U7-A81K-TQW4. [DOI] [PubMed] [Google Scholar]
- 10.Boerma W. Coordination and integration in European primary care. Primary Care in the Driver’s Seat? In: Saltman R, Rico A, Boerma W, editors. European Observatory on health systems and health policy. Berkshire, UK: Open University Press; 2006. pp. 3–21. [Google Scholar]
- 11.Kuhlbrandt Ch, Boerma W. Primary care reforms in countries of the former Soviet Union: success and challenges. Eurohealth. 2015;21(2) [Google Scholar]
- 12.Kuhbrandt C, Boerma W. Primary care reforms in countries of the former Soviet Union: success and challenges. Eurohealth. 2015;21(2):3–6. [Google Scholar]
- 13.Atun R. Introducing a complex health innovation – primary health care reforms in Estonia (multimethods evaluation) Health Policy. 2006;79:79–91. doi: 10.1016/j.healthpol.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 14.Grielen S, Boerma W, Groenewegen P. Unity or diversity? Task profiles of general practitioners in Central and Eastern Europe. European Journal of Public Health. 2000;10(4):249–254. [Google Scholar]
- 15.Groenewegen P, Dourgnon P, Greb S, Jurgutis A, Willems S. Strengthening weak primary care system: Step towards stronger primary care in selected Western and Eastern European countries. Health Policy. 2013;113:170–179. doi: 10.1016/j.healthpol.2013.05.024. [DOI] [PubMed] [Google Scholar]
- 16.Groenewegen P, Heinemann S, Greb S, Scharfer W. Primary care practice composition in 34 countries. Health Policy. 2015;119:1576–1583. doi: 10.1016/j.healthpol.2015.08.005. [DOI] [PubMed] [Google Scholar]
- 17.Rosstat Federal statistical service of the Russian Federation. In Russian. 2016. [Accessed September 26, 2018]. Available from: http://www.gks.ru/wps/wcm/connect/rosstat_main/rosstat/ru/statistics/population/healthcare/
- 18.World Health Organization European Health for All Database. 2017. [Accessed September 26, 2018]. Available from: https://gateway.euro.who.int/en/hfa-explorer/
- 19.Popovich L, Potapchik E, Shishkin S, Richardson E, Vacroux A, Mathivet B. Russian Federation: Health system review. Health Syst Transit. 2011;13(7):1–190. [PubMed] [Google Scholar]
- 20.Federal State Statistics Service [homepage on the Internet] Statistical form № 30 of the Russian Federation Statistical Agency. The order № 866 of December 27. 2016. [Accessed October 08, 2018]. Available from: http://www.gks.ru/wps/wcm/connect/rosstat_main/rosstat/en/main/
- 21.Yakovleva T. Objazatelnoe meditsinskoe strahovanie. 1. Moscow: Russian Federation; 2017. [Accessed October 16, 2018]. Presentation at the IX Russian conference “Medicine and quality – 2016”; p. 23. Russian. Available from: http://www.ffoms.ru/system-oms/journal/archive-journal/45/4527003/ [Google Scholar]
- 22.Nolte E, McKee M. Caring for people with chronic conditions: a health system perspective. Berkshire, UK: Open University Press; 2008. [Google Scholar]
- 23.Nolte E, Frølich A, Hildebrandt H, Pimperl A, Schulpen GJ, Vrijhoef HJ. Implemented integrated care: a synthesis of experiences in three European countries. Intl J Care Coordination. 2016;19(1–2):5–19. [Google Scholar]
- 24.Stadchenko NN. Rost platnykh uslug malo svyazan s problemami besplatnoy medpomoshchi. [The growth of paid medical services has little to do with the problems of free medical care] Kommersant. Jun 22, 2016. [Accessed May 2, 2017]. Available from: https://www.kommersant.ru/doc/3019197. Russian.
- 25.Lafortune G, Moreira L. Trends in supply of doctors and nurses in EU and OECD countries; OECD Health Division, Expert Group Meeting on European Health Workforce; 16 November 2015; Brussels. 2015. [Accessed September 18, 2016]. Available from: https://www.oecd.org/health/health-systems/OECD-Trends-in-education-and-training-November2015.pdf. [Google Scholar]
- 26.Pearson M. Using Evidence in HRH Policy Making in OECD countries. OECD Health Division. Health Workforce Australia 2013. Nov 18, 2013. [Accessed July 15, 2017]. Available from: https://www.oecd.org/els/health-systems/Health-workforce_Evidence-in-HRH-policy-making.pdf.
- 27.Denisov I. Family medicine development in Russi//Glavvrach № 5. 2007 Russian. [Google Scholar]
- 28.Lember M, Cartier T, Bourgueil Y, Dedeu T, Kringos D. Structure and organization of primary care. In: Kringos D, Boerma W, Hutchinson A, Saltman R, editors. Building primary care in a changing Europe. Copenhagen: WHO; 2015. pp. 41–65. [Google Scholar]
- 29.Sheiman I, Shevski V. Two models of primary care development: Russia vs Central and Eastern European countries. National Research University - Higher School of Economics. Basic Research Program Working Papers. 2017. (Series: Public and Social Policy WP BRP 06/PSP/2017). [Google Scholar]
- 30.Government of the Russian Federation Rasporjazhenie Pravitelstva, O komplekse mer po obespecheniu sistemi zdravoohranenija Rossijskoj Federacii medicinskimi kadrami do 2018 goda. [The degree of the Government on the complex of activities to ensure the supply of medical workers to the Russian Federation health system until 2018. 2013 Russian. [Google Scholar]
- 31.Ono T, Lafortune G, Schoenstein M. Health Workforce Planning in OECD Countries: A Review of 26 Projection Models from 18 Countries. [Accessed September 26, 2018];OECD Health Working Papers. 2013 62 doi: 10.1787/5k44t787zcwb-en. Available from: [DOI] [Google Scholar]
- 32.Flek V. Russian health finance based on health accounting system. Moscow: Booki Vedi; 2015. Russian. [Google Scholar]
- 33.Sheiman I, Shevski V. Evaluation of health care delivery integration: the case of the Russian Federation. Health Policy. 2014;115(2–3):128–137. doi: 10.1016/j.healthpol.2013.12.011. [DOI] [PubMed] [Google Scholar]
- 34.Moscow City Department of Health Presentation on the implementation of the state program “Capital health care in 2012–2020”. 2015 Russian. [Google Scholar]
- 35.The Russian Federation Ministry of Health Implementation of public declaration of aims and objectives of the Russian Federation Ministry of Health in 2016. 2017 Russian. [Google Scholar]
- 36.The Russian Federation Ministry of Health Presentation of Veronika Skvortsova, Minister of Health at the Gaidar Conress. 2015. [Accessed September 26, 2018]. Available from: http://doctor.59.ru/text/newsline_med/884048.html.
- 37.Shishkin S, Sheiman I, Abdin S, Boyrski S, Sazchina S. Publishing house of HSE. Moscow: 2017. [Accessed September 26, 2018]. fc. Available from: https://www.hse.ru/data/2017/01/12/1115337576/Дoклад_итoг.pdf. Russian. [Google Scholar]
- 38.Bokeria L, Stupakov I, Gudkova R, Analysis of cardio-vascular diseases indicators Zdravoohranenie No 6 2015. 2015 Russian. [Google Scholar]
- 39.The Russian Federation Ministry of Health . Resources and health facilities activity. Statistical Handbook; Moscow: 2016. [Accessed September 26, 2018]. Available from: https://www.fedstat.ru/indicator/31557.do. Russian. [Google Scholar]
- 40.The Russian Federation Ministry of Health Report “The results of the Ministry of Health work in 2015 and objectives for 2016”. Accessed September 26, 2018 Russian. [Google Scholar]
- 41.The Russian Federation Ministry of Health Prikaz #132 n of 27.02.2016. 2016 Russian. [Google Scholar]
- 42.Gerry C, Sheiman I. Too many and too few: the paradoxical case of physicians in the Russian Federation. International Journal of Health Planning and Management. 2017 doi: 10.1002/hpm.2471. [DOI] [PubMed] [Google Scholar]
- 43.Busse R, Mays N. Paying for chronic disease care. In: Nolte E, McKee M, editors. Caring for People with Chronic Conditions A Health System Perspective. Berkshire, UK: Open University Press; 2008. pp. 195–221. [Google Scholar]
- 44.Shishkin, et al. National Research University – High School of Economics. Report “Transformation of the health workforce structure and motivation under the influence of economic, technological factors and state workforce policy”. Russian: 2016. [Google Scholar]
- 45.Levada Center . Report “Physician, patient and the power in the process of health reform”. Moscow: 2016. Russian. [Google Scholar]
- 46.Hwang W, Chang J, Laclair M, Paz H. Effects of integrated delivery system on cost and quality. Am J Manag Care. 2013;19:e175–e184. [PubMed] [Google Scholar]
- 47.Rittenhouse DR, Grumbach K, O’Neil EH, Dower C, Bindman A. Physician organization and care management in California: from cottage to Kaiser. Health Affairs. 2004;23:51–62. doi: 10.1377/hlthaff.23.6.51. [DOI] [PubMed] [Google Scholar]
- 48.Weeks W. Higher Health Care Quality And Bigger Savings Found At Large Multispecialty Medical Groups. Health Affairs. 2010;29:991–997. doi: 10.1377/hlthaff.2009.0388. [DOI] [PubMed] [Google Scholar]
- 49.Sheiman I. Payment Methods for Integration: Typology, Evidence and Pre-conditions of Implementation. [AccessedSeptember 26, 2018];Journal of Pharmaceutical Care and Health Systems. 2016 3(2) doi: 10.4172/2376/0419/1000154. Available from: [DOI] [Google Scholar]
- 50.The report of eighteen district therapists (2016) On the failure of the project of “Moscow standard of a polyclinic”. Deistvia profsouz. 2016 Mar 26; Russian. [Google Scholar]