Abstract
Introduction:
Rates of alternative tobacco product use (ATPs; eg, cigars, cigarillos, pipes) among cigarette smokers are on the rise but little is known about the subgroups at highest risk. This study explored interactions between demographic, tobacco, and psychosocial factors to identify cigarette smokers at highest risk for ATP use from a racially/ethnically and socioeconomically diverse sample of adult smokers across the full smoking spectrum (nondaily, daily light, daily heavy).
Methods:
Two-thousand three-hundred seventy-six adult cigarette smokers participated in an online cross-sectional survey. Quotas ensured equal recruitment of African American (AA), white (W), Hispanic/Latino (H) as well as daily and nondaily smokers. Classification and Regression Tree modeling was used to identify subgroups of cigarette smokers at highest risk for ATP use.
Results:
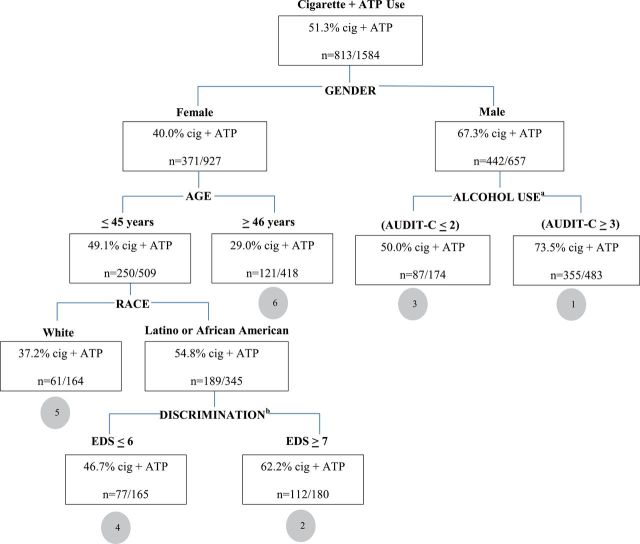
51.3% were Cig+ATP smokers. Alcohol for men and age, race/ethnicity, and discrimination for women increased the probability of ATP use. Strikingly, 73.5% of men screening positive for moderate to heavy drinking and 62.2% of younger (≤45 years) African American/Hispanic/Latino women who experienced regular discrimination were Cig+ATP smokers.
Conclusions:
Screening for concurrent ATP use is necessary for the continued success of tobacco cessation efforts especially among male alcohol users and racial/ethnic minority women who are at greatest risk for ATP use.
Introduction
Between 8%–38% of US daily smokers and as much as 44% of nondaily smokers use one or more alternative tobacco product (ATPs; eg, cigarillos) in combination with cigarettes.1–4 These numbers are expected to grow as tax increases on cigarettes prompt more smokers to begin using ATPs.5 Increased use of ATPs may also be due to perceptions that they are a safer alternative to cigarettes,6,7 despite data suggesting that they can be just as harmful.8 The average nicotine yield in commercially available cigarettes ranges from 0.09 to 1.4mg/cigarette,9 compared with nicotine yields of 1.5–1.8mg/unit for hand-rolled cigarettes,10 1.5, 1.4, and 3.4mg/unit for little, large, and premium cigars,8 and 2.9mg for a hookah session.11 More concerning is that exposure to carbon monoxide and select carcinogens (eg, NNN, PAH) is higher in many combustible ATPs compared with cigarettes.8 Unfortunately, health risks from ATPs are often overlooked by ATP users and health care practitioners. In clinical practice, individuals are identified as cigarette smokers but use of cigarettes in conjunction with ATPs is rarely assessed.3,12 In research, cigarette smokers who report use of ATPs are frequently excluded from clinical trials,13–16 perpetuating an almost complete lack of knowledge about patterns of use, risk of use, and effective treatments.
Literature has begun to describe the profile of cigarette smokers who also use ATPs (Cig+ATP). Compared to smokers who use cigarettes exclusively, Cig+ATP smokers are younger, male, nondaily smokers, heavier users of alcohol and/or marijuana, and of lower socioeconomic status.1,2,17–20 Although they appear to have the same level of nicotine dependence and to smoke the same number of cigarettes per day, ATP users are more likely than cigarette smokers to have made a recent quit attempt.20 ATP users may also be more likely to be racial/ethnic minorities, although this finding is inconsistent across studies.4,19,20
Existing studies have used regression analyses, or similar approaches, to identify factors associated with ATP use. These statistical approaches have limitations.21 Most notably, the inclusion and interpretation of interaction effects in regression models is difficult. A priori interactions may be tested, but unspecified interaction effects are not explored. Our resulting knowledge-base, then, is limited to “main effect” predictors of ATP use while controlling for all other factors, which does not capture the complexities of “real world” ATP users—for example, cigarette smokers who use ATPs are more likely to be men, controlling for race/ethnicity, age, smoking level and alcohol use. In actuality, these characteristics likely co-occur to produce synergistic patterns of risk. It is more likely, for example, that ATP users are racial/ethnic minority men who are younger, nondaily smokers, and heavy/problem drinker, but the nature of these interrelationships has not been examined.
Another limitation of regression analyses is that they determine the average effect for a sample, but the resulting models only weakly predict outcome for many individuals.21 Because risk is not equally distributed, knowing the subgroups of cigarette smokers at highest risk for ATP use, and the factors placing individuals at highest risk, has important implications for tobacco control interventions. Classification and regression trees (CART) address these limitations by simultaneously considering all variables and their potential interactions to arrive at a model that powerfully predicts outcome for the most relevant subgroup(s).21 CART models reveal factors that would otherwise be masked by other variables, the output makes it easy to visualize the hierarchical interaction of variables, and the resulting observed probabilities are easier to interpret than odds ratios. In addition, cut-points are made based on the true nature of the relationship of predictor to outcome and not on arbitrary or predefined values.
CART analyses are increasingly being used in the medical field for developing screening and/or treatment algorithms to aid in clinical decision making.22 Broadly, CART are used to identify patient subgroups for whom prognoses differ or for whom early identification and treatment could improve disease outcomes.23–25 Examples of CART applications include developing a brief cognitive screening battery for dementia,26 identifying patients who are most likely to experience new onset or least likely to experience improvements of depressive symptoms during outpatient mental health treatment,27 and understanding who benefits at each stage of a web-based diabetes self-management program.28
CART analyses have been used to a much lesser extent in tobacco, but they have utility in targeting interventions to smokers who are overlooked or less likely to benefit from conventional treatments. Recent tobacco-related CART applications have included identification of subgroups of smokers at highest risk of relapse following standard smoking cessation treatment29 and subgroups of smokers for whom more intensive treatments may be needed in order to optimize cessation outcomes.30,31 CART analyses have not been applied to ATP users.
Given our lack of knowledge of how demographic, tobacco, and psychosocial factors interact in their association with ATP use, this study used CART modeling to identify subgroups of cigarette smokers at highest risk for ATP use from a sample of racially/ethnically and socioeconomically diverse adult smokers across the full smoking spectrum (nondaily, daily light, daily heavy). Variables included in the CART model were demographic (eg, gender, age, socioeconomic status), tobacco (eg, number of cigarettes smoked per day [CPD], dependence, quit attempts), and alcohol use factors significantly associated with ATP use in previous regression-based studies.1,17–20 Other variables were selected to address gaps in the literature. Specifically, we included variables related to price and harm reduction because lower cost, increased marketing, and differences in tobacco regulation of ATPs versus cigarettes (eg, some ATP products can be sold individually) may motivate cigarette smokers to use other forms of tobacco,32,33 and the threat of tax increases may prompt more cigarette smokers, especially price-sensitive low-income and racial/ethnic minority smokers, to begin using these products.5 ATPs have been marketed as more natural and less harmful than cigarettes and many ATP smokers may use these products to reduce their perceived harm from smoking.6,7 Therefore, we included harm reduction strategies in our model. Discrimination was included in the CART because it has been consistently linked to smoking patterns (eg, prevalence, dependence) among racial/ethnic minorities, women, and individuals of low socioeconomic status.34–37 Previous research also suggests that high levels of racial discrimination in combination with increased availability and targeted marketing of ATPs in low income and racial/ethnic minority communities may contribute to increased use of these products.5,38 The resulting CART model provides the first comprehensive picture of the interrelationship between previously and newly examined demographic, tobacco, and psychosocial factors and has important implications for improving the identification and treatment of ATP users in research and practice.
Methods
Participants were current adult (≥25 years) cigarette smokers who completed a cross-sectional survey administered through an online panel survey service, Survey Sampling International, between July 5 and August 15, 2012. Survey Sampling International maintains an online panel of 1.5 million people in the United States who have indicated willingness to participate in online surveys and uses nonprobability sampling to recruit participants into the panel and recruits potential panelists through a variety of websites, online communities, and social networks.39 Eligible cigarette smokers self-identified as non-Hispanic African American (AA), non-Hispanic white (W), or Hispanic/Latino (H), and English speaking. Women who were currently pregnant or breast-feeding were excluded because pregnant women are likely to at least temporarily modify their smoking behavior.40 Individuals who smoked on fewer than 4 days in the past 30 days were also ineligible.41 Finally, age criteria were established because much of the existing research has been in college age students, while less is known about ATP use among cigarette smokers across the lifespan.17,20,42,43
Because race/ethnicity and smoking level are understudied risk factors for ATP use,3,4,19,20 the sample was stratified and quotas were established to obtain equal samples of AA, W, H across nondaily and daily smoking levels. Of the 42 715 participants who began the screener, 35 698 were ineligible because of full quotas or they did not meet the study criteria, 4581 discontinued before completing the survey (90% of whom discontinued during the screener, prior to starting the survey), and 60 participants were removed for completing the survey more than once. This resulted in a study sample size of 2376 participants—1201 nondaily smokers (401 AA, 400W, 400 H) and 1175 daily smokers (393 AA, 396W, 386 H). All procedures were approved by the University of Minnesota Institutional Review Board.
Measures
Use of ATPs
Using standard questions, participants reported (yes/no) whether they used cigars, cigarillos, little cigars, smokeless tobacco, pipes, hand-rolled cigarettes, and hookahs in the past 30 days.2 For each form of tobacco used, participants were asked to provide the number of days used in the past 30 and average amount on the days used. Participants who reported using any ATP in the past 30 days were categorized as Cig+ATP smokers. Participants reporting no ATP use were categorized as cigarette only smokers (Cig Only).
Demographics
Participants’ reported their age, gender, highest level of education, monthly household income, and race/ethnicity. Race/ethnicity was assessed using standard items from the US Department of Health and Human Services.44 Only participants identifying as non-Hispanic white, non-Hispanic black, or Hispanic of any race were included in the study.
Tobacco and Alcohol Use Characteristics
Participants reported the average CPD on the days smoked in the past 7 days, whether they typically smoke menthol or nonmenthol, and the number of 24-hour quit attempts in the last year. Nondaily, daily light, and daily heavy smoking level was computed from combination of how many days smoked and the average CPD. Nondaily smokers smoked at least one cigarette on 4–24 days in the past 30 days.41,45–47 Daily smokers smoked 25–30 days in the past 30 days and were further stratified into light daily smokers (≤10 CPD)14,15 and moderate to heavy daily smokers (>10 CPD).13,48
Nicotine dependence was assessed using the “time to first cigarette of the day” item from the Fagerström Test for Nicotine Dependence.49 This single item has been found to be a strong measure of nicotine dependence and predictor of nicotine exposure across a range of smoking levels.50 To assess price sensitivity, participants were asked how often the buy versus borrow cigarettes from other people and whether the price of cigarettes has influenced them to smoke less (yes/no), the brand they buy (yes/no), and where they buy cigarettes (yes/no).51 To assess harm reduction, participants were asked (yes/no) if they were currently trying to cut down on the number of cigarettes that they smoked.52 Efforts to reduce harm were further assessed by asking participants (yes/no) if they were currently setting a limit for how many cigarettes they smoked a day to decrease their health risks from smoking and how often they had tried to limit their smoking in the last year to decrease their health risks (five-point scale from “Never” to “Always”).53
The Alcohol Use Disorders Identification Test-Consumption (AUDIT-C) was used to assess alcohol use. This screening measure is effective for detecting alcohol misuse in AA, H, and W adults.54 Scores range from 0 to 12 with scores of ≥4 in men and ≥3 in women indicating possible alcohol misuse.
Psychosocial Factors
The two-item Patient Health Questionnaire was used to assess depressive symptoms.55 This validated screening tool has been used extensively and is effective for detecting depressive symptoms in AA, H, and W adults.55,56 Scores range from 0 to 6 with scores of ≥3 indicating possible depressive symptoms. The short version of the Everyday Discrimination Scale was used to assess experiences of discrimination in five situations (eg, received poorer service at stores/restaurants) and the primary reason for these experiences (eg, gender, race, age, socioeconomic status).57 The Everyday Discrimination Scale is one of the most widely used scales for measuring perceived discrimination, and it has been found to measure discrimination equivalently among AA, H, and W adults, regardless of the perceived reason for discrimination.58 Scores range from 0 to 25 with higher scores indicating greater frequency of discrimination in daily life.
Statistical Analyses
Univariate differences between Cig+ATP versus Cig Only smokers were compared using the chi-square test for categorical variables and the two sample t tests for continuous variables. To control for multiple testing a Bonferroni correction was applied to the Type I error rate to determine univariate significance. CART methodology was used to identify subgroups at highest risk for Cig+ATP use. This methodology derives hidden patterns in data by constructing a series of binary splits on the outcome of interest. The most discriminating predictor is selected to form the first partition/split based on the variables ability to minimize the within-group variance of the dependent variable. This step is applied recursively to each partition/split until the sample size within each subgroup (terminal node) is at or below a prespecified level which, for this study, was specified as 10% of the total sample size. Using the methods described by Therneau et al.,59 the data were randomly partitioned into a training and validation data set. The training data set contained 1584 participants (2/3 of the sample; Figure 1) and was used to derive a decision tree using Gini splitting rules in SAS Enterprise Miner version 12.3.60 A maximum tree was constructed and standard pruning strategies were then applied to arrive at a parsimonious tree with a low misclassification rate and high discriminatory capacity.61 The validation data set contained the remaining 792 participants (1/3 of sample) and was used to evaluate the acceptability and predictive ability of the training data set model and is included as Supplementary Figure 1.
Figure 1.
Classification and regression tree derived from the training dataset (n = 1584) identifying the highest risk subgroups for use of alternative tobacco products in combination with cigarettes (Cig+ATP) (misclassification rate = 0.34, receiver operating characteristic = 0.70). The tree derived from the validation data set (n = 792) identified the same outcome discriminators, terminal nodes, and ordered subgroups (Supplementary Figure 1). aAUDIT-C = Alcohol Use Disorders Identification Test-Consumption; bEDS = Everyday Discrimination Scale. This figure is adapted from Lei et al.62 The original figure was published by BioMed Central.
Results
Of the 2376 participants, 1220 (51.3%) were Cig+ATP smokers and 1156 (48.7%) were Cig Only smokers. Cig+ATP smokers used a median of 2.0 (range 1.0–7.0) other tobacco products, with 41.6% using one other tobacco product, 28.7% using two, 17.4% using three, 6.9% using four, 2.5% using five, 1.1% using six, and 1.8% using seven other tobacco products in the past 30 days. The frequency of ATP use is displayed in Table 1.
Table 1.
Frequency and Amount of Use by Tobacco Product for Smokers Who Use Cigarettes in Combination With Alternative Tobacco Product (Cig+ATP) Compared With Those Who Use Cigarettes Only
| Cigarette+ATP smokers (n = 1220) | Cigarette only smokers (n = 1156) | |||||
|---|---|---|---|---|---|---|
| % Yes | Median (range) | % Yes | Median (range) | |||
| Product endorsement | Days used in past 30 | Amount used on days smoked | Product endorsement | Days used in past 30 | Amount used on days smoked | |
| Cigarettes | 100.0% | 20.0 (4–30) | 6.0 (1–80) | 100.0% | 29.0 (4–30) | 9.0 (1–60) |
| Cigarsa | 58.4% | 4.0 (1–30) | 1.0 (1–16) | — | — | — |
| Cigarillosb | 42.2% | 5.0 (1–30) | 2.0 (1–60) | — | — | — |
| Hand-rolled cigarettes | 38.4% | 4.0 (1–30) | 4.0 (1–50) | — | — | — |
| Little cigarsc | 28.0% | 3.0 (1–30) | 2.0 (1–50) | — | — | — |
| Hookah or water pipe | 16.6% | 2.0 (1–30) | 1.0 (1–10)d | — | — | — |
| Snuff/smokeless tobacco | 14.8% | 5.0 (1–30) | 2.0 (1–15) | — | — | — |
| Pipes | 12.5% | 4.0 (1–30) | 1.0 (1–20) | — | — | — |
| Median (range) | Median (range) | P | |
|---|---|---|---|
| Cigarettes per monthe | 136.5 (4–2400) | 180.0 (5–1800) | <.0001 |
| Tobacco products per monthf | 193.0 (5–3030) | 180.0 (5–1800) | <.0001 |
aDefined as weighing >3 pounds/1000 cigars.
bDefined as weighing ≤3 pounds/1000.
cIntermediate in size between large and little cigars; containing about 3 grams of tobacco.
dThe median hookah/water pipe session lasted 15 minutes (range = 1–160 minutes).
eCalculated as days used in past 30 × amount used on days smoked.
fCalculated as the sum of days used in past 30 × amount used on days smoked for cigarettes, cigars, cigarillos, hand-rolled cigarettes, little cigars, hookah/water pipe, snuff/smokeless tobacco, and pipes combined.
Univariate differences between Cig+ATP versus Cig Only smokers are displayed in Table 2. Compared to Cig Only smokers, Cig+ATP users were younger, more likely to be male, racial/ethnic minorities, nondaily, menthol, and price-sensitive smokers (ie, less likely to buy all of the cigarettes they smoked, more likely to choose their cigarette brand based on price). In addition, ATP users had higher rates of depressive symptoms, alcohol use, and experienced greater frequency of discrimination. The primary reason for discrimination was race, reported by 24.9% of the sample, overall, followed by “other” (13.9%), another aspect of physical appearance (12.4%), age (10.1%), gender (9.1%), weight (9.0%), ancestry/national origin (6.8%), education/income (6.1%), height (3.1%), sexual orientation (2.5%), and religion (2.0%) (data not shown).
Table 2.
Univariate Differences Between Smokers Who Use Cigarettes in Combination With Alternative Tobacco Product (Cig+ATP) Compared With Those Who Use Cigarettes Only
| Cigarette+ATP (n = 1220) | Cigarette only (n = 1156) | P a | |
|---|---|---|---|
| Demographics | |||
| Gender, % male | 54.3% | 28.7% | <.0001 |
| Age, mean (SD) | 40.2 (11.6) | 45.9 (12.6) | <.0001 |
| Race, % | |||
| Non-Hispanic white | 27.0% | 40.4% | <.0001 |
| Non-Hispanic African American | 35.7% | 31.0% | |
| Hispanic | 37.3% | 28.6% | |
| Education, % college graduate or higher | 38.9% | 31.5% | ns |
| Income, % <$1800/mo | 39.3% | 40.1% | ns |
| Tobacco and alcohol use characteristics | |||
| Smoking status, % | |||
| Nondaily | 55.2% | 45.7% | <.0001 |
| Daily light (1–10 CPD) | 21.2% | 27.6% | |
| Daily heavy (≥11 CPD) | 23.6% | 26.7% | |
| Menthol smoker | 60.4% | 53.9% | .001 |
| Cigarettes per day, mean (SD) | 9.3 (8.7) | 10.1 (8.5) | ns |
| Time to first cigarette, % within 30 minutes of waking | 59.0% | 54.4% | ns |
| 24-hour quit attempts in last 12 months, mean (SD) | 5.5 (9.5) | 5.9 (11.8) | ns |
| Price sensitivity | |||
| Price of cigs influenced them to smoke less, % yes | 59.5% | 55.7% | ns |
| Price of cigs influenced where they buy cigs, % yes | 68.9% | 71.5% | ns |
| Price of cigs influenced the brand they buy, % yes | 48.4% | 39.4% | <.0001 |
| Buy vs. borrow cigs, % buy all cigs they smoke | 56.0% | 71.3% | <.0001 |
| Harm reduction | |||
| Trying to cut down on cigs smoke, % yes | 70.7% | 70.8% | ns |
| Limit CPD to decrease health risk, % yes | 48.9% | 43.7% | ns |
| Limit smoking in last year to decrease health risks, % always or often | 29.5% | 30.8% | ns |
| Alcohol | |||
| Alcohol, mean (SD)b | 4.6 (3.1) | 3.3 (3.0) | <.0001 |
| Alcohol, % alcohol misuse | 66.6% | 48.8% | <.001 |
| Psychosocial | |||
| Depression, mean (SD)c | 2.1 (1.8) | 1.8 (1.8) | <.0001 |
| Depression, % depressive symptoms | 38.0% | 29.8% | <.0001 |
| Discrimination frequency, mean (SD)d | 8.3 (6.7) | 5.9 (5.7) | <.0001 |
CPD = number of cigarettes smoked per day; ns = nonsignificant. A modified version of this table appears in Lei et al.62 The original table was published by BioMed Central.
a P values represent those that are significant after Bonferroni correction, which was applied because of the large sample size and to minimize the likelihood of a Type I error due to multiple testing. Variables with a P value below the corrected Type I error rate of 0.0023 (0.05/22) are considered significant.
bAlcohol Use Disorders Identification Test-Consumption scores range from 0 to 12 with scores of ≥4 for men and ≥3 for women indicating possible alcohol misuse.
cTwo-item Patient Health Questionnaire scores range from 0 to 6 with scores of 3 or higher indicating possible depressive symptoms.
dScores range from 0 to 25 with higher scores indicating greater frequency of discrimination in daily life.
When CART methodology was applied to examine the variables jointly related to ATP use only gender, age, alcohol, race/ethnicity, and experiences of discrimination emerged as outcome discriminators, resulting in a tree with six terminal nodes (Figure 1, training data-set, n = 1584). The tree can be interpreted in multiple ways. Three interpretations are provided for illustrative purposes. Using the percentages, which represent observed probabilities of ATP use, CART identified six subgroups: 73.5% of men with AUDIT-C alcohol scores of ≥3 (n = 355) were ATP users, followed by 62.2% of younger (≤45 years) Latina and African American women with greater experiences of discrimination (EOD ≥ 7, n = 112), 50.0% of men with AUDIT-C scores ≤2 (n = 87), 46.7% of younger Latina and African American women with fewer experiences of discrimination (n = 77), 37.2% of younger white women (n = 61), and 29.0% of older women (n = 121).
It is also informative to interpret the tree in terms of the factors that increase and decrease the probability of ATP use. To do this, one compares the rates of ATP use among the six subgroups to the average rate of ATP use for the sample (51.3%); factors placing subgroups above and below the sample average are interpreted as increasing and decreasing the probability of Cig+ATP use, respectively. The combination of male gender and moderate to high alcohol use scores increased the probability of ATP use (probability = 73.5%) as did the combination of female gender, younger age, racial/ethnic minority status, and greater experiences of discrimination (probability = 62.2%). Conversely, the combination of female gender and older age decreased the probability of ATP use (probability = 29.0%) as did the combination of female gender, younger age, and nonracial/ethnic minority status (probability = 37.2%).
Risk ratios can also be computed for reference and comparison groups of interest by comparing observed probabilities from the terminal nodes. Men with an AUDIT-C score ≥3 had a 1.47 or 47% (0.735/0.500) higher risk of ATP use compared with men with an AUDIT-C score of ≤2, younger racial/ethnic minority women with more experiences of discrimination had a 33% (0.622/0.467) higher risk of ATP use compared to those with less experiences of discrimination, younger racial/ethnic minority women with more experiences of discrimination had a 114% (0.622/0.290) higher risk of ATP use compared with older women, while younger racial/ethnic minority women with fewer experiences of discrimination and younger white women had a 61% (0.467/0.290) and 28% (0.372/0.290) higher risk of ATP use, respectively, compared with older women.
The tree derived from the validation data set identified the same outcome discriminators, terminal nodes, and ordered subgroups (Supplementary Figure 1; n = 792). The misclassification rate (0.34 and 0.35, respectively) and discriminatory capacity (receiver operating characteristic index = 0.70 and 0.69, respectively) of both the training- and validation-derived trees were very good.
Discussion
This is the first known study to identify cigarette smokers at highest risk for ATP use by examining the complex interrelationships between demographic, tobacco, and psychosocial factors. Several important findings emerged. The first important finding is the high rate of ATP use among the sample overall (51.3%), which is notably higher than previous studies (8%–38%),1–4 possibly reflecting the changing pattern of tobacco use among US adults. A recent study, however, corroborates our results, findings that almost half of African American adult cigarette smokers had used an ATP in the past 30 days.38 While Cig+ATP users smoked fewer cigarettes per month, they supplemented their cigarettes with a notable number of ATPs and were exposed to significantly more total tobacco products per month. The prevalence and frequency at which ATPs were used is concerning. Cigars contain higher levels of cancer-causing nitrosamines, more tar and tobacco, and greater exposure to carbon monoxide, hydrocarbons, and ammonia than cigarettes.63 And, while some hand-rolled cigarettes, little cigars, and cigarillos have a nicotine and carcinogen profiles similar to cigarettes, others more closely resembling full-size cigars,8,64 suggesting that use of these products in conjunction with cigarettes may lead to increased nicotine and carcinogen exposure.
The second important, and concerning, finding is the high the rates of ATP use among female cigarette smokers. To our knowledge, no previous studies have documented high rates of ATP use in women, possibly because the association has been masked by male gender in traditional regression-based analyses.1,2,17–20 Yet our study suggests that younger, AA and H women with regular experiences of discrimination—for example, two or more events a few times a month—have rates of ATP use (62%) that are only slightly lower than the highest risk men (73%). While the probability of Cig+ATP use for the other subgroups of women was at or below the sample average, their probability of being Cig+ATP smokers was still high, ranging from 30% for older women to 50% for younger racial/ethnic minority women with less frequent experiences of discrimination.
The third important finding is the influence of alcohol use in men. Notably, nearly three-fourths (73%) of men with an AUDIT-C score of ≥3 were Cig+ATP smokers. While lower levels of drinking (ie, AUDIT-C ≤ 2) decreased men’s risk of being Cig+ATP smokers, men with low alcohol use scores still had a 50% probability of ATP use.
Findings of this study extend the literature in key ways. Previous studies have commonly identified male gender, alcohol use, racial/ethnic minority status, younger age, lower socioeconomic status, and lower levels of smoking as factors associated with ATP use.1–4,17–20,65 In a complementary statistical methodology paper published by our group, we found that logistic regression modeling identified nine factors that were associated with ATP use: gender, age, race, nicotine dependence, buying cigarettes or borrowing, whether the price of cigarettes influenced the brand purchased, whether the participants set limits on cigarettes per day, alcohol use scores, and discrimination frequencies.62 Many of these factors were not identified here; however, the advantage of the current study is that CART considered all possible interactions among variables, while previous studies have only identified main effect predictors. Within a broader context, the findings are useful in informing research and clinical practice. Guided by the current literature, providers might not consider female cigarette smokers a high risk group due to the perceived low rate of ATP use among women. To the contrary, our findings suggest that identification and treatment of female Cig+ATP smokers is paramount given that the prevalence rates for women, especially younger racial/ethnic minority women, are comparable to that of the highest risk men. Similarly, findings suggest that tobacco control resources for ATP users should also be allocated toward men who are moderate to heavy drinkers.
Limitations
Our oversampling of AA, H, and nondaily smokers was a strength of the study because these groups have a high probability of ATP use,4,6,19,20,42,43,66,67 but our sample is not representative of US adults and rates of use cannot be generalized to the US population. In addition, the survey was self-administered in English and therefore our H sample is limited to more acculturated Hs. However, our sample was comprised of socioeconomically diverse adult smokers from across the United States who represented the full spectrum of smoking levels and is similar in age, gender, education, and nicotine dependence (ie, factors influencing ATP use) to individuals in the Tobacco Use Supplements to the Current Population Surveys, a nationally representative data set of smoking behaviors among US adults,68,69 thus enhancing the generalizability of our findings. Finally, use of both a training and validation data set supports the CART derived in the current sample; however we are unable to make inferences beyond the current sample. Future studies are needed to determine if the model derived in the current study would be valid in other sample of ATP users.
In conclusion, ATP use is overlooked in research and clinical practice. Given the growing prevalence of ATP use, screening and treatment of Cig+ATP smokers is critically important to the continued success of tobacco control efforts. While achieving abstinence from all tobacco products should be the recommendation and the focus of treatment for all smokers,12 data from this study suggest that initial efforts may be particularly warranted for male moderate to heavy alcohol users and for younger AA and H women who are at greatest risk for ATP use.
Supplementary Material
Supplementary Figure 1 can be found online at http://www.ntr.oxfordjournals.org
Funding
This work was funded by Pfizer’s Global Research Awards for Nicotine Dependence (PI: JSA). JSA is also supported in part by the National Institute for Minority Health Disparities (NCMHD/NIH—1P60MD003422). Pfizer had no role in the design and conduct of the study; in the collection, analysis, and interpretation of the data; or in the preparation, review, or approval of the manuscript.
Declaration of Interests
None declared.
Supplementary Material
References
- 1. Backinger CL, Fagan P, O’Connell ME, et al. Use of other tobacco products among U.S. adult cigarette smokers: prevalence, trends and correlates. Addict Behav. 2008;33(3):472–489. doi:10.1016/j.addbeh.2007.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kasza KA, Bansal-Travers M, O’Connor RJ, et al. Cigarette smokers’ use of unconventional tobacco products and associations with quitting activity: findings from the ITC-4U.S. cohort. Nicotine Tob Res. 2014;16(6):672–681. doi:10.1093/ntr/ntt212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. McGrath DS, Temporale KL, Bozec LJ, Barrett SP. Polytobacco use in non-daily smokers: an issue requiring greater attention. Prev Med. 2011;53(4–5):353–354. doi:10.1016/j.ypmed.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 4. Popova L, Ling PM. Alternative tobacco product use and smoking cessation: a national study. Am J Public Health. 2013;103(5):923–930. doi:10.2105/AJPH.2012.301070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cantrell J, Kreslake JM, Ganz O, et al. Marketing little cigars and cigarillos: advertising, price, and associations with neighborhood demographics. Am J Public Health. 2013;103(10):1902–1909. doi:10.2105/AJPH.2013.301362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jolly DH. Exploring the use of little cigars by students at a historically black university. Prev Chronic Dis. 2008;5(3):1–9. www.ncbi.nlm.nih.gov/pmc/articles/PMC2483573/ Accessed May 11, 2015. [PMC free article] [PubMed] [Google Scholar]
- 7. Page JB, Evans S. Cigars, cigarillos, and youth: emergent patterns in subcultural complexes. J Ethn Subst Abuse. 2004;2(4):63–76. doi:10.1300/J233v02n04_04. [Google Scholar]
- 8.Djordjevic M, Doran KA. Nicotine content and delivery across tobacco products. In: Henningfield J, London E, Pogun S, eds. Nicotine Psychopharmacology. Vol. 192: Berlin Heidelberg: Springer;2009:61–82. doi:10.1007/978-3-540-69248-5_3. [DOI] [PubMed] [Google Scholar]
- 9. Federal Trade Commission. Tar, Nicotine, and Carbon Monoxide of the Smoke of 1294 Varieties of Domestic Cigarettes for the Year 1998. Washington, DC: Federal Trade Commission Report; 2000. www.ftc.gov/sites/default/files/documents/reports/2000-report-tar-nicotine-and-carbon-monoxide-covering-1998/1998tarnicotinereport_0.pdf Accessed May 11, 2015. [Google Scholar]
- 10. Kaiserman MJ, Rickert WS. Carcinogens in tobacco smoke: benzo[a]pyrene from Canadian cigarettes and cigarette tobacco. Am J Public Health. 1992;82(7):1023–1026. www.ncbi.nlm.nih.gov/pmc/articles/PMC1694072/ Accessed May 11, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Shihadeh A, Saleh R. Polycyclic aromatic hydrocarbons, carbon monoxide, “tar”, and nicotine in the mainstream smoke aerosol of the narghile water pipe. Food Chem Toxicol. 2005;43(5):655–661. doi:10.1016/j.fct.2004.12.013. [DOI] [PubMed] [Google Scholar]
- 12. Fiore M, Jaen C, Baker T, et al. Treating Tobacco Use and Dependence Clinical Practice Guideline: 2008 Update. Washington, DC: U.S. Department of Health and Human Services; 2008. [Google Scholar]
- 13. Ahluwalia JS, Harris KJ, Catley D, Okuyemi KS, Mayo MS. Sustained-release bupropion for smoking cessation in African Americans: a randomized controlled trial. JAMA. 2002;288(4):468–474. doi:10.1001/jama.288.4.468. [DOI] [PubMed] [Google Scholar]
- 14. Ahluwalia JS, Okuyemi K, Nollen N, et al. The effects of nicotine gum and counseling among African American light smokers: a 2×2 factorial design. Addiction. 2006;101(6):883–891. doi:10.1111/j.1360-0443.2006.01461.x. [DOI] [PubMed] [Google Scholar]
- 15. Cox LS, Nollen NL, Mayo MS, et al. Bupropion for smoking cessation in African American light smokers: a randomized controlled trial. J Natl Cancer Inst. 2012;104(4):290–298. doi:10.1093/jnci/djr513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Okuyemi KS, James AS, Mayo MS, et al. Pathways to health: a cluster randomized trial of nicotine gum and motivational interviewing for smoking cessation in low-income housing. Health Educ Behav. 2007;34(1):43–54. doi:10.1177/1090198106288046. [DOI] [PubMed] [Google Scholar]
- 17. Bombard JM, Pederson LL, Koval JJ, O’Hegarty M. How are lifetime polytobacco users different than current cigarette-only users? Results from a Canadian young adult population. Addict Behav. 2009;34(12):1069–1072. doi:10.1016/j.addbeh.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 18. Bombard JM, Pederson LL, Nelson DE, Malarcher AM. Are smokers only using cigarettes? Exploring current polytobacco use among an adult population. Addict Behav. 2007;32(10):2411–2419. doi:10.1016/j.addbeh.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 19. CDC. Any tobacco use in 13 states—Behavioral Risk Factor Surveillance System. MMWR Morb Mortal Wkly Rep. 2010;59(30):946–950. www.cdc.gov/mmwr/preview/mmwrhtml/mm5930a3.htm Accessed May 11, 2015. [PubMed] [Google Scholar]
- 20. Richardson A, Xiao H, Vallone DM. Primary and dual users of cigars and cigarettes: profiles, tobacco use patterns and relevance to policy. Nicotine Tob Res. 2012;14(8):927–932. doi:10.1093/ntr/ntr306. [DOI] [PubMed] [Google Scholar]
- 21. Brieman L, Friendman J, Oshen R, Stone C. Classification and Regression Trees. Pacific Grove, CA: Wedsworth; 1984. [Google Scholar]
- 22. Ebell M. AHRQ White Paper: use of clinical decision rules for point-of-care decision support. Med Decis Making. 2010;30(6):712–721. doi:10.1177/0272989X10386232. [DOI] [PubMed] [Google Scholar]
- 23. Doering S, Muller E, Kopcke W, et al. Predictors of relapse and rehospitalization in schizophrenia and schizoaffective disorder. Schizophr Bull. 1998;24(1):87–98. http://schizophreniabulletin.oxfordjournals.org/content/24/1/87.long Accessed May 11, 2015. [DOI] [PubMed] [Google Scholar]
- 24. Janni W, Gastroph S, Hepp F, et al. Prognostic significance of an increased number of micrometastatic tumor cells in the bone marrow of patients with first recurrence of breast carcinoma. Cancer. 2000;88(10):2252–2259. www.ncbi.nlm.nih.gov/pubmed/10820346 Accessed May 11, 2015. [DOI] [PubMed] [Google Scholar]
- 25. Kiely M, El-Mohandes AA, Gantz MG, Chowdhury D, Thornberry JS, El-Khorazaty MN. Understanding the association of biomedical, psychosocial and behavioral risks with adverse pregnancy outcomes among African-Americans in Washington, DC. Matern Child Health J. 2011;15(suppl 1):S85–95. doi:10.1007/s10995-011-0856-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Belle SH, Mendelsohn AB, Seaberg EC, Ratcliff G. A brief cognitive screening battery for dementia in the community. Neuroepidemiology. 2000;19(1):43–50. www.ncbi.nlm.nih.gov/pubmed/10654287 Accessed May 11, 2015. [DOI] [PubMed] [Google Scholar]
- 27. Berman MI, Hegel MT. Predicting depression outcome in mental health treatment: a recursive partitioning analysis. Psychother Res. 2014;24(6):675–686. doi:10.1080/10503307.2013.874053. [DOI] [PubMed] [Google Scholar]
- 28. Glasgow RE, Strycker LA, King DK, Toobert DJ. Understanding who benefits at each step in an internet-based diabetes self-management program: application of a recursive partitioning approach. Med Decis Making. 2014;34(2):180–191. doi:10.1177/0272989X13498156. [DOI] [PubMed] [Google Scholar]
- 29. Piper ME, Loh WY, Smith SS, Japuntich SJ, Baker TB. Using decision tree analysis to identify risk factors for relapse to smoking. Subst Use Misuse. 2011;46(4):492–510. doi:10.3109/10826081003682222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Swan GE, Jack LM, Javitz HS, McAfee T, McClure JB. Predictors of 12-month outcome in smokers who received bupropion sustained-release for smoking cessation. CNS Drugs. 2008;22(3):239–256. doi:1172.7047/08/0003-0239. [DOI] [PubMed] [Google Scholar]
- 31. Swan GE, Javitz HS, Jack LM, Curry SJ, McAfee T. Heterogeneity in 12-month outcome among female and male smokers. Addiction. 2004;99(2):237–250. doi:10.1111/j.1360-0443.2003.00629.x. [DOI] [PubMed] [Google Scholar]
- 32. Centers for Disease Control and Prevention. Consumption of cigarettes and combustible tobacco—United States, 2000–2011. MMWR Morb Mortal Wkly Rep. 2012;61(30):565–569. doi:mm6130a1 [pii]. [PubMed] [Google Scholar]
- 33. Government Accountability Office. Tobacco taxes: large disparities in rates for smoking products trigger significant market shifts to avoid higher taxes (pp. 1–57) 2012. www.gao.gov/products/GAO-12–475 Accessed May 11, 2015.
- 34. Kendzor DE, Businelle MS, Reitzel LR, et al. Everyday discrimination is associated with nicotine dependence among African American, Latino, and White smokers. Nicotine Tob Res. 2014;16(6):633–640. doi:10.1093/ntr/ntt198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Schulz AJ, Gravlee CC, Williams DR, Israel BA, Mentz G, Rowe Z. Discrimination, symptoms of depression, and self-rated health among african american women in detroit: results from a longitudinal analysis. Am J Public Health. 2006;96(7):1265–1270. doi:10.2105/AJPH.2005.064543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Williams DR. Race, socioeconomic status, and health. The added effects of racism and discrimination. Ann N Y Acad Sci. 1999;896:173–188. doi:10.1111/j.1749–6632.1999.tb08114.x. [DOI] [PubMed] [Google Scholar]
- 37. Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: socioeconomic status, stress, and discrimination. J Health Psychol. 1997;2(3):335–351. doi:10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- 38. Corral I, Landrine H, Simms DA, Bess JJ. Polytobacco use and multiple-product smoking among a random community sample of African-American adults. BMJ Open. 2013;3(12):e003606. doi:10.1136/bmjopen-2013–003606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Survey Sampling International. ESOMAR 28. Fact Sheets 2014. www.surveysampling.com/ssi-media/Corporate/Fact-Sheets-2013/ESOMAR-28 Accessed April 6, 2015.
- 40. Floyd RL, Rimer BK, Giovino GA, Mullen PD, Sullivan SE. A review of smoking in pregnancy: effects on pregnancy outcomes and cessation efforts. Annu Rev Public Health. 1993;14:379–411. doi:10.1146/annurev.pu.14.050193.002115. [DOI] [PubMed] [Google Scholar]
- 41. Shiffman S, Tindle H, Li X, Scholl S, Dunbar M, Mitchell-Miland C. Characteristics and smoking patterns of intermittent smokers. Exp Clin Psychopharmacol. 2012;20(4):264–277. doi:10.1037/a0027546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Cullen J, Mowery P, Delnevo C, et al. Seven-year patterns in US cigar use epidemiology among young adults aged 18–25 years: a focus on race/ethnicity and brand. Am J Public Health. 2011;101(10):1955–1962. doi:10.2105/AJPH.2011.300209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Sterling K, Berg CJ, Thomas AN, Glantz SA, Ahluwalia JS. Factors associated with small cigar use among college students. Am J Health Behav. 2013;37(3):325–333. doi:10.5993/AJHB.37.3.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Dorsey R, Graham G. New HHS data standards for race, ethnicity, sex, primary language, and disability status. JAMA. 2011;306(21):2378–2379. doi:10.1001/jama.2011.1789. [DOI] [PubMed] [Google Scholar]
- 45. Schauer GL, Malarcher AM, Berg CJ. Differences in smoking and cessation characteristics among adult nondaily smokers in the United States: findings from the 2009–2010 National Adult Tobacco Survey. Nicotine Tob Res. 2014;16(1):58–68. doi:10.1093/ntr/ntt113. [DOI] [PubMed] [Google Scholar]
- 46. Shiffman S, Dunbar MS, Scholl SM, Tindle HA. Smoking motives of daily and non-daily smokers: a profile analysis. Drug Alcohol Depend. 2012;126(3):362–368. doi:10.1016/j.drugalcdep.2012.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Shiffman S, Ferguson SG, Dunbar MS, Scholl SM. Tobacco dependence among intermittent smokers. Nicotine Tob Res. 2012;14(11):1372–1381. doi:10.1093/ntr/nts097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Okuyemi KS, Harris KJ, Scheibmeir M, Choi WS, Powell J, Ahluwalia JS. Light smokers: issues and recommendations. Nicotine Tob Res. 2002;4(suppl 2):S103–112. doi:10.1080/1462220021000032726. [DOI] [PubMed] [Google Scholar]
- 49. Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. Br J Addict. 1991;86(9):1119–1127. www.ncbi.nlm.nih.gov/pubmed/1932883 Accessed May 11, 2015. [DOI] [PubMed] [Google Scholar]
- 50. Muscat JE, Stellman SD, Caraballo RS, Richie JP., Jr Time to first cigarette after waking predicts cotinine levels. Cancer Epidemiol Biomarkers Prev. 2009;18(12):3415–3420. doi:10.1158/1055–9965.EPI-09-0737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Al-Delaimy WK, Edland S, Pierce JP, Mills AL, White MM. Technical Report on Analytic Methods and Approaches Used in the 2008 California Tobacco Survey Analysis. Vol 1: Data Collection Methodology. La Jolla, CA: University of California, San Diego; 2009. [Google Scholar]
- 52. Al-Delaimy WK, Edland S, Pierce JP, Mills AL, White MM. Technical Report on Analytic Methods and Approaches Used in the 2005 California Tobacco Survey Analysis. Vol 1: Data Collection Methodology. La Jolla, CA: University of California, San Diego; 2007. [Google Scholar]
- 53. Okuyemi KS, Richter KP, Ahluwalia JS, Mosier MC, Nazir N, Resnicow K. Smoking reduction practices among African American smokers. Nicotine Tob Res. 2002;4(suppl 2):S167–173. doi:10.1080/1462220021000032744. [DOI] [PubMed] [Google Scholar]
- 54. Frank D, DeBenedetti AF, Volk RJ, Williams EC, Kivlahan DR, Bradley KA. Effectiveness of the AUDIT-C as a screening test for alcohol misuse in three race/ethnic groups. J Gen Intern Med. 2008;23(6):781–787. doi:10.1007/s11606-008-0594-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41(11):1284–1292. doi:10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 56. Lowe B, Kroenke K, Grafe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2). J Psychosom Res. 2005;58(2):163–171. doi:10.1016/j.jpsychores.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 57. Sternthal MJ, Slopen N, Williams DR. Racial Disparities in Health. Du Bois Review: Social Science Research on Race. 2011;8(1):95–113. doi:10.1017/s1742058x11000087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Kim G, Sellbom M, Ford KL. Race/ethnicity and measurement equivalence of the Everyday Discrimination Scale. Psychol Assess. 2014;26(3):892–900. doi:10.1037/a0036431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Therneau TM, Atkinson EJ. An introduction to recursive partitioning using the RPART routines http://cran.r-project.org/web/packages/rpart/vignettes/longintro.pdf Accessed May 11, 2015.
- 60. Gordon L. Using Classification and Regression Trees (CART) in SAS Enterprise Miner for Applications in Public Health, Paper 089-2013. SAS Global Forum: Data Mining and Text Analytics 2013. http://support.sas.com/resources/papers/proceedings13/089-2013.pdf Accessed May 11, 2015.
- 61. Breiman L, Friedman J, Olshen R, Stone C. Classification and Regression Trees. Monterey, CA: Wadsworth and Brooks/Cole Advanced Books and Software; 1986. [Google Scholar]
- 62. Lei Y, Nollen N, Ahluwalia JS, Yu Q, Mayo MS. An application in identifying high-risk populations in alternative tobacco product use utilizing logistic regression and CART: a heuristic comparison. BMC Public Health. 2015;15(1):341. doi:10.1186/s12889-015-1582-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. National Cancer Institute. Smoking and Tobacco Control Monograph 9: Cigars: Health Effects and Trends. Bethesda, MD: National Cancer Institute; 1998. http://cancercontrol.cancer.gov/Brp/tcrb/monographs/9/index.html Accessed May 11, 2015. [Google Scholar]
- 64. Henningfield JE, Fant RV, Radzius A, Frost S. Nicotine concentration, smoke pH and whole tobacco aqueous pH of some cigar brands and types popular in the United States. Nicotine Tob Res. 1999;1(2):163–168. doi:10.1080/14622299050011271. [DOI] [PubMed] [Google Scholar]
- 65. Campbell ML, Bozec LJ, McGrath D, Barrett SP. Alcohol and tobacco co-use in nondaily smokers: an inevitable phenomenon? Drug Alcohol Rev. 2012;31(4):447–450. doi:10.1111/j.1465-3362.2011.00328.x. [DOI] [PubMed] [Google Scholar]
- 66. King BA, Dube SR, Tynan MA. Current tobacco use among adults in the United States: findings from the National Adult Tobacco Survey. Am J Public Health. 2012;102(11):e93–e100. doi:10.2105/AJPH.2012.301002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Rath JM, Villanti AC, Abrams DB, Vallone DM. Patterns of tobacco use and dual use in US young adults: the missing link between youth prevention and adult cessation. J Environ Public Health. 2012;2012:679134. doi:10.1155/2012/679134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Trinidad DR, Perez-Stable EJ, Emery SL, White MM, Grana RA, Messer KS. Intermittent and light daily smoking across racial/ethnic groups in the United States. Nicotine Tob Res. 2009;11(2):203–210. doi:10.1093/ntr/ntn018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Trinidad DR, Perez-Stable EJ, White MM, Emery SL, Messer K. A nationwide analysis of US racial/ethnic disparities in smoking behaviors, smoking cessation, and cessation-related factors. Am J Public Health. 2011;101(4):699–706. doi:10.2105/AJPH.2010.191668. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.