Abstract
A quantitative survey was completed by 103 primary care physicians (PCPs) and 59 cardiologists who regularly prescribed β‐blockers to assess knowledge and use of this heterogeneous drug class for hypertension. More cardiologists than PCPs chose β‐blockers as initial antihypertensive therapy (30% vs 17%, P < 0.01). Metoprolol and carvedilol were the most commonly prescribed β‐blockers. Cardiologists rated “impact on energy” and “arterial vasodilation” as more important than PCPs (P < 0.05/<0.01, respectively). Awareness of vasodilation was greater for carvedilol (52%) than nebivolol (31%). Association between β‐blockers and clinical variables included nebivolol with β1‐selectivity, nebivolol and carvedilol with vasodilation and efficacy in older patients and African Americans, metoprolol with heart rate reduction, and atenolol and metoprolol with weight gain and hyperglycemia. Physicians preferred prescribing β‐blockers with lower risk of incident diabetes. Clinical practice guidelines influenced physician prescribing more than formularies or performance metrics. This survey captures physicians’ perceptions/use of various β‐blockers and clinically relevant knowledge gaps.
1. INTRODUCTION
Affecting >85 million Americans, hypertension is a major risk factor for heart disease, stroke, renal disease, and poor cardiovascular (CV) outcomes.1, 2, 3, 4 In 2014, approximately 73 000 deaths in the United States were attributed to hypertension, an increase of 34.1% since 2004.5 While many efficacious options for pharmacologically lowering blood pressure (BP) are available—including angiotensin‐converting enzyme inhibitors (ACEI), angiotensin II receptors blockers (ARBs), calcium channel blockers (CCBs), diuretics, aldosterone antagonists, and β‐blockers6—hypertension remains uncontrolled in nearly 50% of hypertensive adults,7 and the prevalence of resistant hypertension is rising.8
β‐blockers are a diverse class of drugs once considered a core treatment option for achieving BP control; however, current US practice guidelines no longer recommend β‐blockers as first‐line therapy.6 The current recommendations are based on long‐term outcome studies and meta‐analyses in which treatment with nonvasodilatory β‐blockers was associated with undesirable CV and stroke outcomes.9, 10, 11, 12, 13 An acknowledged limitation of those studies was that the β‐blockers investigated may not fully represent this heterogeneous drug class.12, 14 Newer vasodilatory β‐blockers, namely carvedilol and nebivolol, have distinct mechanisms of action from previous generations of β‐blockers and from each other.15, 16 Unlike atenolol and metoprolol, which are non‐vasodilatory β1‐selective adrenergic receptor antagonists, carvedilol is a nonselective β‐adrenergic antagonist with vasodilation occurring via α1‐adrenergic antagonism.14, 17 Nebivolol is also vasodilatory, but is a highly β1‐selective antagonist with β3‐agonistic and nitric oxide‐mediated vasodilatory properties.18, 19 Such distinct mechanisms of action may contribute to improved CV event risk and may reduce side effects over non‐vasodilatory β‐blockers, with potential implications for adherence and persistence.20, 21, 22, 23 Indeed, a large retrospective cohort study examining CV event risk leading to hospitalization in hypertensive patients receiving one of three β1‐selective blockers (nebivolol, metoprolol, or atenolol) as monotherapy revealed that nebivolol treatment was associated with lower risk of CV‐related hospitalization than either atenolol or metoprolol.24
Hypertension clinical practice guidelines now recommend a target systolic blood pressure (SBP)/diastolic blood pressure (DBP) <130/80 mm Hg for adults with confirmed cardiovascular disease (CVD), 10‐year atherosclerotic CVD event risk ≥10%, or for patients with diabetes mellitus, chronic kidney disease, or who are >65 years old.6 In order to achieve target blood pressure, most patients will require ≥2 antihypertensives.25 By combining treatments with different but complementary mechanisms of action (eg, ACEIs or β‐blockers with diuretics and CCBs), additive effects on BP reduction may be achieved, allowing for lower dosages of both drugs.25, 26 Given the current hypertension guidelines and the need for multiple antihypertensives to achieve BP control, β‐blockers will continue to play an important role as add‐on therapy in hypertension management.
To assess the importance of factors that may influence physicians when prescribing antihypertensives, particularly β‐blockers, a 20‐minute quantitative online survey was conducted to identify physician perceptions, knowledge, and prescribing of currently available treatments among cardiologists and primary care physicians (PCPs).
2. METHODS
The 20‐minute web‐based survey was designed and conducted to meet the following objectives: (a) measure physicians’ use of currently available classes of antihypertensive drugs, including in specific populations; (b) evaluate β‐blocker use, as well as perceptions of and reasons for prescribing β‐blockers; (c) evaluate awareness of key differentiating properties of vasodilatory β‐blockers; (d) identify future needs for hypertension treatment; and (e) identify the current use of and preferences for educational resources.
PCPs and cardiologists were selected from a database (SERMO) of US physicians who elected to participate in primary research surveys. To ensure that physicians included in the survey were experienced prescribers of β‐blockers and familiar with the β‐blocker drug class, included survey participants: (a) had treated >30 hypertensive patients (new and existing) in the past 3 months, (b) were personally responsible for prescribing β‐blockers, and (c) had written >50 β‐blocker prescriptions in the last 3 months. Informed consent was obtained prior to initiation of the survey, which was conducted according to Market Research Society guidelines.27 The identities of the participants were kept confidential and were not disclosed to the sponsor company.
The survey covered the following topics: the proportion of patients using each type of antihypertensive; identification of treatments as first‐, second‐, third‐line therapy, etc; the proportion of patients in special populations (eg, African American patients with uncomplicated hypertension and diabetic patients) receiving therapy and from which drug class; the importance of antihypertensive features (eg, efficacy in patients >60 years old, effect on weight or fatigue, etc); a ranking of unmet medical needs in hypertensive patients; concomitant medications in patients receiving β‐blockers and the presence of comorbid conditions; the importance of drug features when choosing a β‐blocker; reasons for not prescribing β‐blockers; the association of a particular β‐blocker with clinical features; awareness of the vasodilatory properties of β‐blockers; the perceived value of a single‐pill combination (SPC) of a β‐blocker and renin‐angiotensin aldosterone system (RAAS) inhibitor; and how frequently hypertension educational materials were accessed and preferentially used.
The survey was designed and conducted by McCann Health (formerly Double Helix); survey programming and invitation management were handled by SERMO (https://www.sermo.com), and data processing was conducted by Digitab, Inc (https://www.digitab.uk.com). The survey questionnaire is available in the supplement. Analyses were performed using QPS statistical software (QPSMR CL, version 2016.1). All physicians provided complete responses, as programming ensured that all respondents answered all required questions; there were no missing or incomplete data. Results were aggregated and not specifically linked to individual participants. Differences between PCPs and cardiologists were examined by t tests to determine significance between means and by z tests to determine significance between percentages.
3. RESULTS
3.1. Participating physicians
During August and September 2016, invitations were sent to US physicians (cardiologists, 704; PCPs, 869); of those who responded (n = 130 [18.5%] and n = 302 [34.8%], respectively), 45% of cardiologists and 34% of PCPs met the inclusion criteria, resulting in 162 physicians surveyed (59 cardiologists, 103 PCPs). Most cardiologists (71%) and PCPs (78%) were from private offices or clinics. In the 3 months prior to the survey, cardiologists and PCPs self‐reported seeing an average (±standard deviation) of 499 ± 226 and 399 ± 195 hypertensive patients, respectively, with 29% and 20% being new patients.
3.2. Antihypertensive use
Compared with PCPs, a significantly higher proportion of cardiologists’ caseloads were prescribed β‐blockers (cardiologists, 46%; PCPs, 28%; P < 0.01) and aldosterone antagonists (12% vs 7%, P < 0.01) for hypertension. Though the treatment of choice among all physicians for first‐line therapy was an ACEI, a significantly greater proportion of patients were prescribed β‐blockers as a first‐line therapy by cardiologists than by PCPs (30% vs 17%, P < 0.01; Figure 1A). For second‐line therapy, a similar proportion of patients were prescribed ACEIs (25%), diuretics (26%), ARBs (23%), β‐blockers (25%), or CCBs (23%), while only 5% received aldosterone antagonists; differences were not significant between cardiologists and PCPs (data not shown).
Figure 1.
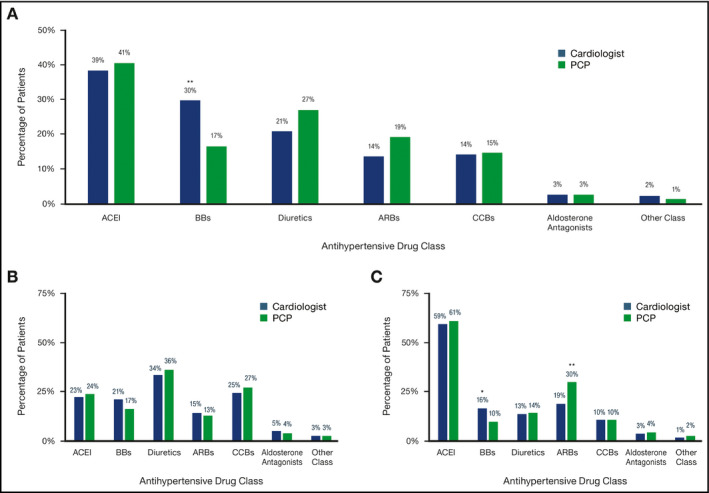
First‐line Hypertension Treatments in a General Patient Population (A), African American Patients (B), or Diabetic Patients (C). N = 162: A, All patients; QB1: Thinking about your hypertensive patients, what proportion of patients typically receive each of the following classes of treatment at each line of therapy? B, African American patients; QB2: Now, thinking about your uncomplicated hypertensive African American patients, what proportion of patients typically receive each of the following classes of treatment at first‐line therapy? C, Diabetic patients; QB3: Now, thinking about your uncomplicated hypertensive diabetic patients, what proportion of patients typically receive each of the following classes of treatment at first‐line therapy? *P < 0.05, **P < 0.01. ACEI, angiotensin‐converting enzyme inhibitors; ARBs, angiotensin II receptors blockers; BB, β‐blockers; CCBs, calcium channel blockers; PCP, primary care physician
3.3. β‐blocker use
In the previous 3 months, metoprolol was the most commonly prescribed β‐blocker (cardiologists, 40%; PCPs, 42%), followed by carvedilol (33% vs 26%, P < 0.05), atenolol (13% vs 18%), nebivolol (8% vs 7%), bisoprolol (5% vs 8%, P < 0.05), or other β‐blockers (2% vs 1%). For both cardiologists and PCPs, nearly three‐quarters of patients taking β‐blockers were either prediabetic and/or obese (74%, each). A similar percentage of diabetic patients were treated with β‐blockers by cardiologists (23%) and PCPs (25%).
Fatigue was the leading reason for not prescribing β‐blockers, ranking in the top three reasons most of the time for both cardiologists (78%) and PCPs (82%; Figure 2). Most physicians did not consider formulary/payer considerations, a reason for not prescribing β‐blockers.
Figure 2.
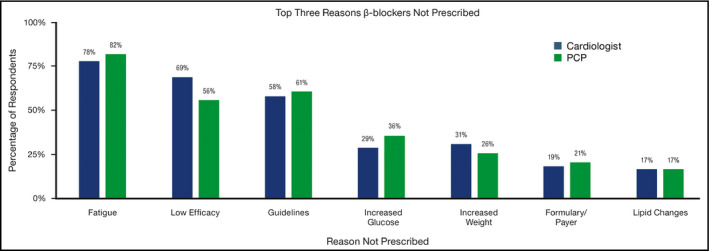
Use and Association of β‐blockers. A, QB11. To start, what are the main reasons for not prescribing β‐blockers for uncomplicated hypertension patients? Physicians selected the variables above among their top 3 reasons for not prescribing β‐blockers. PCP, primary care physician
3.4. β‐blocker attributes
The key drug features considered by physicians when choosing a particular β‐blocker included the ability to reduce heart rate, efficacy in patients aged >60 years, side effects other than fatigue, β1‐selectivity, impact on fatigue/energy, and impact on arterial vasodilation (Table 1). Among physicians surveyed, 52% of physicians (68% cardiologists, 43% PCPs) closely associated carvedilol with vasodilation. In contrast, only 31% of physicians (36% cardiologists, 29% PCPs) associated nebivolol with vasodilation. More PCPs than cardiologists associated all queried β‐blockers with vasodilation (17% vs 5%, P < 0.05). A significantly greater number of cardiologists than PCPs were aware of the specific mechanisms by which either carvedilol or nebivolol achieve vasodilation (carvedilol: 86% cardiologists, 58% PCPs, P < 0.01; nebivolol: 51% vs 30%, P < 0.01).
Table 1.
Mean ratings (±SD) of importance of features when choosing an agent
| Feature | Any antihypertensive agent | β‐blockers | ||
|---|---|---|---|---|
| Cardiologist | PCP | Cardiologist | PCP | |
| Reduction in heart rate | 11.4 ± 11.9 | 9.9 ± 8.7 | 14.4 ± 13.4 | 18.3 ± 17.8 |
| Efficacy in patients aged >60 y | 10.6 ± 10.6 | 12.5 ± 10.8 | 10.1 ± 11.0 | 11.6 ± 10.5 |
| Other side effects[Link] | 10.0 ± 10.8 | 10.3 ± 8.1 | 9.5 ± 9.6 | 11.7 ± 8.1 |
| β1‐selectivity | NA | NA | 10.2 ± 8.3 | 10.3 ± 9.2 |
| Impact on fatigue/energy | 10.3 ± 8.5 | 8.8 ± 6.5 | 11.6 ± 9.8a | 8.9 ± 6.6 |
| Impact on arterial vasodilation | 11.0 ± 10.0 | 9.8 ± 9.3 | 12.0 ± 13.8b | 6.0 ± 5.1 |
| Efficacy in African American patients | 8.8 ± 6.9 | 10.2 ± 8.3 | 6.5 ± 6.1 | 7.6 ± 7.2 |
| Impact on diuresis | 9.2 ± 9.5 | 7.8 ± 5.4 | NA | NA |
| Impact on sleep or mood[Link] | 5.4 ± 4.9 | 5.6 ± 4.9 | 7.7 ± 6.4 | 6.0 ± 6.5 |
| Impact on glucose | 5.7 ± 5.7 | 7.5 ± 7.1 | 4.9 ± 4.7 | 6.1 ± 6.8 |
| Impact on weight | 4.9 ± 4.7 | 5.6 ± 5.0 | 5.1 ± 6.9 | 5.1 ± 5.2 |
| Impact on lipids | 5.6 ± 4.8 | 5.6 ± 4.4 | 4.4 ± 4.7 | 5.2 ± 4.8 |
| Impact on reducing/blocking aldosterone | 7.1 ± 7.0 | 6.5 ± 6.2 | 3.6 ± 4.2 | 3.2 ± 4.1 |
COPD, chronic obstructive pulmonary disease; NA, not applicable; PCP, primary care physician; SD, standard deviation.
QB4/10. Thinking about all the treatment classes/β‐blockers you currently use to treat hypertension, from the list of features below, please rate how important each is on your decision to use a particular agent/β‐blocker for hypertensive patients, allocating 100 points across the features. The higher the number of points you allocate to a feature, the greater importance it has.
Examples include COPD exacerbation, dyspnea, or erectile dysfunction.
Example includes depression.
P < 0.05.
P < 0.01 vs PCP.
When asked about features physicians associated with a particular β‐blocker (0 = not at all associated; 10 = very closely associated; mean scores, Table 2), β1‐selectivity was most highly associated with nebivolol (6.3) vs carvedilol (which is nonselective28; 5.1), atenolol (5.0), or metoprolol (5.8). Significant between‐group differences were identified for the association of β1‐selectivity with either carvedilol (PCPs, 5.7; cardiologists, 4.1; P < 0.01) or atenolol (cardiologists, 6.1; PCPs, 4.2; P < 0.01). Nebivolol and carvedilol were more highly associated with arterial vasodilation (nebivolol, 5.8; carvedilol, 5.5) than either atenolol (3.9) or metoprolol (4.0), neither of which has primary vasodilating properties.28 Metoprolol and atenolol were strongly associated with reducing heart rate (metoprolol, 7.6; atenolol, 7.5). Nebivolol and carvedilol were least associated with fatigue (Table 2).
Table 2.
Association of Features with β‐blockers Used (All Physicians)
| Feature | β‐blockers | |||
|---|---|---|---|---|
| Nebivolol | Carvedilol | Atenolol | Metoprolol | |
| Reduction in heart rate | 6.2 ± 2.3 | 6.9 ± 2.1 | 7.5 ± 1.9 | 7.6 ± 1.9 |
| Efficacy in patients aged >60 y | 6.2 ± 2.2 | 6.3 ± 2.1 | 5.7 ± 2.2 | 6.0 ± 2.1c |
| β1‐selectivity | 6.3 ± 2.6 | 5.1 ± 2.9d | 5.0 ± 2.8b | 5.8 ± 2.7 |
| Fatigue | 4.7 ± 2.6 | 5.4 ± 2.2 | 6.7 ± 1.8 | 5.8 ± 2.4 |
| Arterial vasodilation | 5.8 ± 2.6 | 5.5 ± 2.4a | 3.9 ± 2.5 | 4.0 ± 2.5c |
| Efficacy in African American patients | 5.5 ± 2.2 | 5.3 ± 2.2 | 4.8 ± 2.3 | 4.9 ± 2.3 |
| Impact on diuresis | 3.4 ± 2.6 | 3.3 ± 2.7 | 3.5 ± 2.6 | 3.1 ± 2.5 |
| Impact on mood | 4.4 ± 2.7 | 4.8 ± 2.4 | 5.8 ± 2.1 | 5.1 ± 2.3 |
| Impact on sleep | 4.2 ± 2.3 | 4.1 ± 2.4 | 4.7 ± 2.4 | 4.5 ± 2.5 |
| Increase in glucose | 4.1 ± 2.5 | 4.3 ± 2.5 | 4.9 ± 2.3 | 4.5 ± 2.4 |
| Weight gain | 3.8 ± 2.5 | 4.1 ± 2.2 | 4.8 ± 2.3 | 4.4 ± 2.3 |
| Lipid changes | 3.9 ± 2.4 | 4.0 ± 2.3 | 4.8 ± 2.2 | 4.1 ± 2.3 |
| Reducing/blocking aldosterone | 4.0 ± 2.7 | 3.5 ± 2.6 | 3.4 ± 2.5 | 3.4 ± 2.5 |
| COPD exacerbation | 4.1 ± 2.5 | 4.7 ± 2.4 | 5.7 ± 2.5 | 5.0 ± 2.3 |
| Dyspnea | 3.7 ± 2.7 | 4.4 ± 2.3 | 5.1 ± 2.5 | 4.3 ± 2.5 |
| Erectile dysfunction | 4.3 ± 2.4 | 5.3 ± 2.3 | 6.4 ± 2.1 | 5.7 ± 2.4 |
COPD, chronic obstructive pulmonary disorder; PCP, primary care physician; SD, standard deviation.
QB12. Thinking about each of the β‐blockers in turn, please indicate how closely you associate each with the following features on a scale of 0‐10 where 0 = not at all associated and 10 = very closely associated.
Rated on a scale from 0 (not at all associated) to 10 (very closely associated); mean scores are presented ± SD.
The four β‐blockers queried in this survey question were included based on the expectation of frequency of use and clinical utility.
P < 0.05.
P < 0.01 in favor of cardiologists vs PCPs.
P < 0.05.
P < 0.01 in favor of PCPs vs cardiologists.
Physicians reported varied associations between specific β‐blockers and changes in weight or glucose levels (Figure 3A,B). Approximately one‐third of cardiologists and PCPs were unaware that β‐blockers are associated with weight gain (34% vs 39%),29 while 42% of surveyed physicians were unaware that any β‐blockers are associated with a clinically relevant increase in glucose.30 Atenolol and metoprolol were most associated with weight gain and clinically relevant changes in glucose, while nebivolol was least associated with either outcome. Only 10% of cardiologists and 2% of PCPs associated carvedilol with weight gain (P < 0.05).
Figure 3.
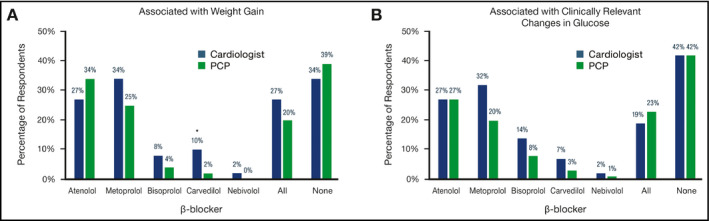
Use and Association of β‐blockers With Clinically Relevant Outcomesa. A, QB16. Which of the following β‐blockers do you consider to be associated with weight gain? B, QB17. Which of the following β‐blockers do you consider to be associated with clinically relevant changes in glucose? aAll possible answers to this survey question are shown. *P < 0.05. PCP, primary care physician
3.5. Importance of β‐blocker attributes
When physicians were asked about the importance of particular drug attributes when choosing treatments, cardiologists rated “arterial vasodilation” and “impact on fatigue/energy” as more important features for β‐blocker selection than PCPs (Table 1).
On a scale of 0 to 10 (0 = no value; 10 = very valuable), cardiologists and PCPs responded similarly to the value of an FDA‐approved SPC of a β‐blocker/RAAS inhibitor for hypertension (mean score = cardiologists, 5.5; PCPs, 5.8), with a net 24% of cardiologists and 27% of PCPs rating the value in the top three levels of importance (ie, 8, 9, or 10).
3.6. Special populations
An analysis of the first‐line therapy used in special populations revealed that African American patients were frequently treated with diuretics (35%) and CCBs (26%; Figure 1B), diabetic patients were frequently prescribed ACEI (60%) or ARBs (26%; Figure 1C), and cardiologists prescribed β‐blockers to greater percentages of African Americans (21% vs 17%) and diabetic patients (16% vs 10%, P < 0.05) than PCPs (Figure 1B,C).
On a scale of 0 to 10 (0 = no chance; 10 = certain), physicians showed a positive response to using a drug other than atenolol or metoprolol for lowering the risk of new‐onset diabetes in prediabetic or obese patients (mean score = cardiologists, 6.7; PCPs, 6.9; a net 36% of cardiologists and 50% of PCPs responded in the top three levels of certainty [ie, 8, 9, or 10]).
3.7. Educational preferences
Continuing medical education (CME) was a major source of education for physicians, both in terms of frequency used and preference for material (ranked in the top 3, Figure S1). Publications and sales representatives were also among the most frequently utilized resources, and publications and medical conferences were other top preferred sources of educational material (ranked in the top 3, Figure S1). However, cardiologists used publications more frequently (ranked first, 46% vs 30%, P < 0.05) and indicated a greater preference for publications as a method for obtaining hypertension information than PCPs (ranked first, 37% vs 26%). On a scale of 0 to 10 (0 = not at all impactful; 10 = very impactful), clinical practice guidelines (mean score = 8.0) influenced prescribing behaviors more than either formulary (mean score = 6.7) or performance metrics (mean score = 6.1), with no differences between cardiologists and PCPs.
3.8. Unmet needs
Both cardiologists and PCPs ranked “better efficacy” as the highest unmet need in hypertension (cardiologists, 47%; PCPs, 39%), followed by “resistant hypertension” (22% vs 36%), “fewer adverse events” (25% vs 18%), and “new fixed‐dose combinations” (5% vs 7%). These top unmet needs did not significantly differ between cardiologists and PCPs.
4. DISCUSSION
While the percentage of patients achieving BP control with treatment over the last 20 years has increased, hypertension remains a major public health concern and the aim of national programming efforts.7, 31 Consistent with these goals, surveyed physicians identified improvement in efficacy, better BP control with fewer side effects, and treatment of resistant hypertension as major areas of unmet needs. Additionally, physicians reported using β‐blockers primarily as a second‐line or later therapy for hypertension consistent with current hypertension management guidelines,6 which recommend diuretics, CCBs, ACEIs, or ARBs as first‐line therapy, and β‐blockers as add‐on medication absent compelling indications.
The goal of this study was to identify physician perceptions of β‐blockers and educational opportunities when perceptions did not align with known pharmacology or clinical evidence. Several such areas were identified in this study. First, physicians cited fatigue as the main reason for not using β‐blockers, a common reason for study discontinuation in clinical trials of early‐generation β‐blockers such as propranolol, atenolol, or timolol.6, 21 However, recent clinical evidence suggests that fatigue and other β‐blocker side effects are drug‐specific rather than a class‐wide effect.12, 14, 32 Second, physicians were split on their awareness of β‐blockers’ impact on weight gain: Surveyed physicians either associated all queried β‐blockers with weight gain, were unaware that β‐blockers affect weight gain, or associated only certain β‐blockers—atenolol and metoprolol in particular—with these effects. Clinical data support the latter.29, 33, 34 Third, while most physicians did not associate β‐blockers with reducing/blocking aldosterone compared with other antihypertensive agents, evidence shows that β‐blockers reduce aldosterone levels.35, 36 Fourth, physicians associated metoprolol and atenolol more highly with reductions in heart rate than nebivolol and carvedilol. Heart rate reductions with early‐generation β‐blocker treatment for primary cardiovascular disease prevention in hypertensive patients, such as atenolol or metoprolol, have been associated with increased risk of CV events.37, 38 Smaller reductions in heart rate have been noted for nebivolol,39 which may be linked to improvements in risk of primary CV events.24 Finally, physicians in this study associated efficacy in African American patients with all four β‐blockers; however, the efficacy of individual β‐blockers in this patient population has been variable. In previous studies, atenolol treatment was less effective in African American versus white patients with hypertension,40 and compared with either CCB or ACEI treatment, atenolol treatment resulted in fewer African American patients achieving BP reduction goals.41 Nebivolol effectively reduced BP versus placebo in a recent trial in African American patients with hypertension,42 although no head‐to‐head trials comparing β‐blockers have been conducted in this patient population. Overall, future educational efforts for physicians should aim to dispel misperceptions by emphasizing current clinical data.
In this survey, carvedilol and nebivolol were considered more vasodilatory compared with other β‐blockers, but the overall awareness among physicians of the vasodilatory properties of either drug was incomplete; this gap in knowledge was more pronounced for nebivolol than for carvedilol, with less than one‐third of physicians associating nebivolol with vasodilation vs >50% for carvedilol. Further, some physicians incorrectly associated metoprolol and atenolol (or all β‐blockers listed) with vasodilation, indicating another gap in knowledge among antihypertensive prescribers. Increasing physician understanding of the vasodilatory effects of nebivolol and carvedilol, specifically, is potentially important for specific groups of patients. For example, previous reports have linked non‐vasodilatory β‐blockers with increases in body weight,29 blood glucose, and lipids,18, 20 while the vasodilating β‐blockers have neutral or beneficial effects on weight gain,29, 34, 43 insulin sensitivity, and lipid levels.20, 44 Because many of the patients treated by surveyed physicians were prediabetic, diabetic, or obese, and given the relative metabolic benefit of vasodilatory versus non‐vasodilatory β‐blockers, these survey findings suggest a substantial opportunity for educating physicians on β‐blockers that do not affect weight or blood glucose levels.43
There were several instances in which cardiologists diverged significantly from PCPs in their perception or use of β‐blockers. For example, cardiologists prescribed β‐blockers to a greater proportion of patients, were more likely to use β‐blockers as first‐line treatment for hypertension, and prescribed different types of β‐blockers than PCPs. One likely explanation for these differences is that cardiologists saw more patients with complicated hypertension who presented with additional conditions including systolic heart failure, previous myocardial infarction, or ischemic heart disease, for which β‐blockers are indicated and effective.6, 45, 46 On β‐blocker features, PCPs more highly associated atenolol and metoprolol (incorrectly) with vasodilation; as noted above, only carvedilol and nebivolol are vasodilatory. Knowledge of this drug property has important clinical implications: BP lowering by non‐vasodilatory β‐blockers occurs primarily via reduced cardiac output, whereas vasodilatory β‐blockers primarily decrease peripheral vascular resistance.47 Additionally, while surveyed physicians highly associated nebivolol with β1‐selectivity, cardiologists and PCPs diverged significantly on their association of carvedilol with β1‐selectivity. Some PCPs significantly and incorrectly associated carvedilol with β1‐selectivity. While nebivolol is highly β1‐selective, carvedilol is nonselective, acting on both β1 ‐and β2‐ (as well as α1‐) adrenergic receptors.14 Taken together, these results indicate gaps of knowledge and opportunities for educating PCPs on specific properties of drugs within the β‐blocker class; such improvements in physician understanding could positively impact clinical outcomes.24, 48
The findings from this survey indicate that long‐term studies on the differential and possibly beneficial effects of newer generation β‐blockers on various clinical outcomes are warranted, particularly in prediabetic, obese, and other special populations. In particular, studies aimed at clarifying the effects of carvedilol and nebivolol would be valuable given that recent meta‐analyses suggested that BP lowering by combined β/α‐receptor blockers (ie, carvedilol) was less effective than by β1‐selective blockers (ie, nebivolol).49, 50 As the most frequently used and preferred source of education by physicians in this study, CME modules and peer‐reviewed publications may provide greater benefit than other initiatives for accessible and consistent educational efforts.
The results of this survey should be considered with the following limitations in mind. First, self‐reported findings may differ from clinical practice; however, during this study, the identities of surveyed physicians remained confidential, so that physicians may have been more comfortable sharing their true perceptions. Second, with an overall physician response rate of 27.5%, nonresponder bias may have impacted the survey results. Finally, this survey only included physicians who were frequent prescribers of β‐blockers for hypertension; their perceptions may not extend to health care providers who prescribe β‐blockers more sparingly or not at all. Surveying additional physicians, such as infrequent prescribers of β‐blockers or health care providers from specialties other than primary care and cardiology, could help extend the generalizability of these findings.
5. CONCLUSIONS
This survey highlights several educational gaps in and between PCPs and cardiologists, on their knowledge and prescribing of β‐blockers for hypertension treatment. Future educational and research efforts should highlight how differences between β‐blockers impact side effects, hypertension control, and patient outcomes and how this information is most effectively conveyed to prescribing physicians.
CONFLICT OF INTEREST
The research reported herein was funded by Allergan plc, Madison, NJ. Brent Egan has received royalties from UpToDate, research support from Medtronic and Quintiles, and honoraria for consulting with AstraZeneca and Medtronic and for lecturing with Merck Serono. John Flack is a consultant with Vascular Dynamics, Quantum Genomics, Recor Medical, Idorsia, Bayer, and Forest Laboratories, Inc (Allergan), and does research for GlaxoSmithKline, Valencia Technologies Corp, and Bayer. Mehul Patel is an employee of Allergan plc. Sofia Lombera is an employee of McCann Health and regularly works with pharmaceutical clients. The authors have no additional conflict of interests to disclose. Editorial assistance was provided by Gina Daniel, PhD, and Lynn M. Anderson, PhD, of Prescott Medical Communications Group, Chicago, IL; editorial assistance was funded by Allergan plc, Madison, NJ.
AUTHOR CONTRIBUTIONS
All authors contributed extensively and equally to the material presented in this manuscript. All authors had equal opportunity to review and edit the manuscript and give approval prior to submission.
Supporting information
ACKNOWLEDGEMENTS
The authors would like to acknowledge Hannah Robinson and Rebecca Kingston for their project management and data analysis support, as well as SERMO and Digitab, Inc., for their assistance with data collection and analysis.
Egan B, Flack J, Patel M, Lombera S. Insights on β‐blockers for the treatment of hypertension: A survey of health care practitioners. J Clin Hypertens. 2018;20:1464–1472. 10.1111/jch.13375
Sofia Lombera was formerly Double Helix.
REFERENCES
- 1. Hsu CY, McCulloch CE, Darbinian J, Go AS, Iribarren C. Elevated blood pressure and risk of end‐stage renal disease in subjects without baseline kidney disease. Arch Intern Med. 2005;165(8):923‐928. [DOI] [PubMed] [Google Scholar]
- 2. Levy D, Larson MG, Vasan RS, Kannel WB, Ho KK. The progression from hypertension to congestive heart failure. JAMA. 1996;275(20):1557‐1562. [PubMed] [Google Scholar]
- 3. Franco OH, Peeters A, Bonneux L, de Laet C. Blood pressure in adulthood and life expectancy with cardiovascular disease in men and women: life course analysis. Hypertension. 2005;46(2):280‐286. [DOI] [PubMed] [Google Scholar]
- 4. Ford ES. Trends in predicted 10‐year risk of coronary heart disease and cardiovascular disease among U.S. adults from 1999 to 2010. J Am Coll Cardiol. 2013; 61(22):2249‐2252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics‐2017 update: a report from the American Heart Association. Circulation. 2017;135(10):e146–e603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Hypertension. 2018;71:1269–1324. [DOI] [PubMed] [Google Scholar]
- 7. Fryar C, Ostchega Y, Hales C, Zhang G, Kruszon‐Moran D. Hypertension Prevalence and Control Among Adults: United States, 2015–2016. NCHS data brief, no 289. Hyattsville, MD: National Center for Health Statistics; 2017. [PubMed] [Google Scholar]
- 8. Prosser HC, Gregory C, Hering D, et al. Preferred fourth‐line pharmacotherapy for resistant hypertension: are we there yet? Curr Hypertens Rep. 2017;19(4):30. [DOI] [PubMed] [Google Scholar]
- 9. Dahlof B, Sever PS, Poulter NR, et al. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo‐Scandinavian Cardiac Outcomes Trial‐Blood Pressure Lowering Arm (ASCOT‐BPLA): a multicentre randomised controlled trial. Lancet. 2005;366(9489):895‐906. [DOI] [PubMed] [Google Scholar]
- 10. Dahlof B, Devereux RB, Kjeldsen SE, et al. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002;359(9311):995‐1003. [DOI] [PubMed] [Google Scholar]
- 11. Lindholm LH, Carlberg B, Samuelsson O. Should beta blockers remain first choice in the treatment of primary hypertension? A meta‐analysis. Lancet. 2005;366(9496):1545‐1553. [DOI] [PubMed] [Google Scholar]
- 12. Wiysonge CS, Bradley HA, Volmink J, Mayosi BM, Opie LH Beta‐blockers for hypertension. Cochrane Database Syst Rev. 2017;1:Cd002003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Warmack TS, Estes MA, Heldenbrand S, Franks AM. Beta‐adrenergic antagonists in hypertension: a review of the evidence. Ann Pharmacother. 2009;43(12):2031‐2043. [DOI] [PubMed] [Google Scholar]
- 14. Poirier L, Tobe SW. Contemporary use of beta‐blockers: clinical relevance of subclassification. Can J Cardiol. 2014;30(5 Suppl):S9‐S15. [DOI] [PubMed] [Google Scholar]
- 15. Fisker FY, Grimm D, Wehland M. Third‐generation beta‐adrenoceptor antagonists in the treatment of hypertension and heart failure. Basic Clin Pharmacol Toxicol. 2015;117(1):5‐14. [DOI] [PubMed] [Google Scholar]
- 16. Mann SJ. Redefining beta‐blocker use in hypertension: selecting the right beta‐blocker and the right patient. J Am Soc Hypertens. 2017;11(1):54‐65. [DOI] [PubMed] [Google Scholar]
- 17. Leonetti G, Egan CG. Use of carvedilol in hypertension: an update. Vasc Health Risk Manag. 2012;8:307‐322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Marketou M, Gupta Y, Jain S, Vardas P. Differential metabolic effects of beta‐blockers: an updated systematic review of nebivolol. Curr Hypertens Rep. 2017;19(3):22. [DOI] [PubMed] [Google Scholar]
- 19. Fongemie J, Felix‐Getzik E. A review of nebivolol pharmacology and clinical evidence. Drugs. 2015;75(12):1349‐1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bakris GL, Fonseca V, Katholi RE, et al. Metabolic effects of carvedilol vs metoprolol in patients with type 2 diabetes mellitus and hypertension: a randomized controlled trial. JAMA. 2004;292(18):2227‐2236. [DOI] [PubMed] [Google Scholar]
- 21. Kountz DS. Are tolerability concerns a class effect of beta‐blockers in treating patients with hypertension? Postgrad Med. 2009;121(1):14‐24. [DOI] [PubMed] [Google Scholar]
- 22. Signorovitch JE, Samuelson TM, Ramakrishnan K, et al. Persistence with nebivolol in the treatment of hypertension: a retrospective claims analysis. Curr Med Res Opin. 2012;28(4):591‐599. [DOI] [PubMed] [Google Scholar]
- 23. Choi YJ, Ah YM, Kong J, et al. Implication of different initial beta blockers on treatment persistence: atenolol vs new‐generation beta blocker, a population‐based study. Cardiovasc Ther. 2016;34(4):268‐275. [DOI] [PubMed] [Google Scholar]
- 24. Egan B, Gradman A, Ali S, Li Q, Patel M, Basile J. Cardiovascular outcomes with nebivolol, atenolol, and metoprolol in patients with hypertension: a large, retrospective, propensity score‐matched cohort study. JACC. 2017;69(11, Suppl):1691. [Google Scholar]
- 25. Gradman AH, Basile JN, Carter BL, Bakris GL. Combination therapy in hypertension. J Am Soc Hypertens. 2010;4(1):42‐50. [DOI] [PubMed] [Google Scholar]
- 26. Wald DS, Law M, Morris JK, Bestwick JP, Wald NJ. Combination therapy versus monotherapy in reducing blood pressure: meta‐analysis on 11,000 participants from 42 trials. Am J Med. 2009;122(3):290‐300. [DOI] [PubMed] [Google Scholar]
- 27. Market Research Society: Code of Conduct . [website]. 2014. https://www.mrs.org.uk/pdf/mrs%20code%20of%20conduct%202014.pdf. Accessed August 21, 2017.
- 28. Fares H, Lavie CJ, Ventura HO. Vasodilating versus first‐generation beta‐blockers for cardiovascular protection. Postgrad Med. 2012;124(2):7‐15. [DOI] [PubMed] [Google Scholar]
- 29. Messerli FH, Bell DS, Fonseca V, et al. Body weight changes with beta‐blocker use: results from GEMINI. Am J Med. 2007;120(7):610‐615. [DOI] [PubMed] [Google Scholar]
- 30. Fonseca VA. Effects of beta‐blockers on glucose and lipid metabolism. Curr Med Res Opin. 2010;26(3):615‐629. [DOI] [PubMed] [Google Scholar]
- 31. Office of Disease Prevention and Health Promotion . 2020 Topics & Objectives‐ Heart Disease and Stroke. 2014; https://www.healthypeople.gov/2020/topics-objectives/topic/Heart-Disease-and-Stroke/objectives#4547. Accessed October 18, 2017.
- 32. Ko DT, Hebert PR, Coffey CS, Sedrakyan A, Curtis JP, Krumholz HM. Beta‐blocker therapy and symptoms of depression, fatigue, and sexual dysfunction. JAMA. 2002;288(3):351‐357. [DOI] [PubMed] [Google Scholar]
- 33. Sharma AM, Pischon T, Hardt S, Kunz I, Luft FC. Beta‐adrenergic receptor blockers and weight gain: a systematic analysis. Hypertension. 2001;37(2):250‐254. [DOI] [PubMed] [Google Scholar]
- 34. Flack J, Mallick M, Patel P. The effects of nebivolol on weight in individuals with hypertension. Poster #61. American Society of Consultant Pharmacists. Kissimmee, FL: 2017.
- 35. Ayers K, Byrne LM, DeMatteo A, Brown NJ. Differential effects of nebivolol and metoprolol on insulin sensitivity and plasminogen activator inhibitor in the metabolic syndrome. Hypertension. 2012;59(4):893‐898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Blumenfeld JD, Sealey JE, Mann SJ, et al. Beta‐adrenergic receptor blockade as a therapeutic approach for suppressing the renin‐angiotensin‐aldosterone system in normotensive and hypertensive subjects. Am J Hypertens. 1999;12(5):451‐459. [DOI] [PubMed] [Google Scholar]
- 37. Bangalore S, Sawhney S, Messerli FH. Relation of beta‐blocker‐induced heart rate lowering and cardioprotection in hypertension. J Am Coll Cardiol. 2008;52(18):1482‐1489. [DOI] [PubMed] [Google Scholar]
- 38. Messerli FH, Rimoldi SF, Bangalore S, Bavishi C, Laurent S. When an increase in central systolic pressure overrides the benefits of heart rate lowering. J Am Coll Cardiol. 2016;68(7):754‐762. [DOI] [PubMed] [Google Scholar]
- 39. Van Nueten L, Taylor FR, Robertson JI. Nebivolol vs atenolol and placebo in essential hypertension: a double‐blind randomised trial. J Hum Hypertens. 1998;12(2):135‐140. [DOI] [PubMed] [Google Scholar]
- 40. Cushman WC, Reda DJ, Perry HM, Williams D, Abdellatif M, Materson BJ. Regional and racial differences in response to antihypertensive medication use in a randomized controlled trial of men with hypertension in the United States. Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents. Arch Intern Med. 2000;160(6):825‐831. [DOI] [PubMed] [Google Scholar]
- 41. Saunders E, Weir MR, Kong BW, et al. A comparison of the efficacy and safety of a beta‐blocker, a calcium channel blocker, and a converting enzyme inhibitor in hypertensive blacks. Arch Intern Med. 1990;150(8):1707‐1713. [PubMed] [Google Scholar]
- 42. Saunders E, Smith WB, DeSalvo KB, Sullivan WA. The efficacy and tolerability of nebivolol in hypertensive African American patients. J Clin Hypertens (Greenwich). 2007;9(11):866‐875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Manrique C, Whaley‐Connell A, Sowers JR. Nebivolol in obese and non‐obese hypertensive patients. J Clin Hypertens (Greenwich). 2009;11(6):309‐315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Taylor AA, Bakris GL. The role of vasodilating beta‐blockers in patients with hypertension and the cardiometabolic syndrome. Am J Med. 2010;123(7 Suppl 1):S21‐S26. [DOI] [PubMed] [Google Scholar]
- 45. Fihn SD, Gardin JM, Abrams J, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2012;126(25):e354–e471. [DOI] [PubMed] [Google Scholar]
- 46. Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62(16):e147–e239. [DOI] [PubMed] [Google Scholar]
- 47. Bakris G. An in‐depth analysis of vasodilation in the management of hypertension: focus on adrenergic blockade. J Cardiovasc Pharmacol. 2009;53(5):379‐387. [DOI] [PubMed] [Google Scholar]
- 48. Webb AJ, Fischer U, Rothwell PM. Effects of beta‐blocker selectivity on blood pressure variability and stroke: a systematic review. Neurology. 2011;77(8):731‐737. [DOI] [PubMed] [Google Scholar]
- 49. Wong GW, Laugerotte A, Wright JM. Blood pressure lowering efficacy of dual alpha and beta blockers for primary hypertension. Cochrane Database Syst Rev. 2015;8:Cd007449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Wong GW, Boyda HN, Wright JM Blood pressure lowering efficacy of beta‐1 selective beta blockers for primary hypertension. Cochrane Database Syst Rev. 2016;3:Cd007451. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


