Abstract
Background/Objective: This systematic review aims to evaluate the effect of interventions based on the mindfulness and/or acceptance process on ruminative thoughts, in patients with depression. Method: Electronic searches in Medline, Embase, Cochrane Central, PsycInfo, and Cinahl until December 2016, in addition to hand-searches of relevant studies, identified eleven studies that fulfilling inclusion criteria. Results: A meta-analysis of the effect of the intervention compared to usual care showed a significant and moderate reduction of ruminative thoughts (g = −0.59, 95% CI: −0.77, −0.41; I2 = 0%). Furthermore, findings suggest that mindfulness/acceptance processes might mediate changes in rumination, and that they in turn mediate in the clinical effects of interventions. A meta-analysis of three studies that compared the intervention to other active treatments (medication, behavioral activation and cognitive-behavioral therapy, respectively) showed no significant differences. Conclusions: Mindfulness-based cognitive therapy compared to usual care, produces a significant and moderate reduction in rumination. This effect seems independent of the treatment phase (acute or maintenance) or the number of past depressive episodes, and it was maintained one month after the end of treatment. However, further controlled studies with real patients that compare the most commonly used cognitive-behavioral techniques to treat ruminative thoughts to the acceptance and mindfulness techniques are needed.
Keywords: Depression, Meta-analysis, Mindfulness, Rumination, Systematic review
Resumen
Antecedentes/Objetivo: Revisión sistemática para evaluar el efecto de las intervenciones basadas en la atención plena y/o en el proceso de aceptación de pensamientos rumiativos en la depresión. Método: Búsquedas sistemáticas en Medline, Embase, Cochrane Central, PsycInfo y Cinahl hasta diciembre 2016 y búsquedas manuales identificaron once estudios. Resultados: Un metanálisis que comparó el efecto de la intervención basada en Mindfulness con la atención habitual mostró una reducción significativa y moderada de pensamientos rumiativos. Los hallazgos sugieren que los procesos de atención/aceptación producen cambios en las rumiaciones e influyen en el efecto clínico de las intervenciones. Otro metanálisis con estudios que compararon la intervención basada en Mindfulness con otros tratamientos activos (medicación, activación conductual y terapia cognitivo-conductual, respectivamente) no mostraron diferencias significativas (g = −0,02, 95% CI: −0,39, 0,35; I2 = 0%). Conclusiones: Mindfulness en comparación con la atención habitual, produce una reducción significativa y moderada en la rumia. Este efecto parece independiente de la fase de tratamiento o del número de episodios depresivos pasados, y se mantuvo un mes después del final del tratamiento. Sin embargo, se necesitan más estudios controlados con pacientes reales que comparen las técnicas cognitivo-conductuales más utilizadas para tratar los pensamientos rumiativos con técnicas de aceptación y atención plena.
Palabras clave: Depresión, metaanálisis, mindfulness, rumiaciones, revisión sistemática
The interventions based on the Mindfulness-Based Stress Reduction Program (MBSR; Kabat-Zinn, 1990) and on the Mindfulness-based Cognitive Therapy (MBCT; Segal, Williams, & Teasdale, 2002) can be considered the most widespread treatments among clinical psychologists who promote mindfulness for the treatment of depression and cognitive rumination. Both are very similar in structure, learning format and even in the active principles, although some differences between them have also been pointed out (Crane et al., 2012; Johnson, Mullen, Smith, & Wilson, 2016). These two ways of treating human suffering have also been encompassed in so-called third-wave therapies (Hayes, 2004). According to Hayes (2004), although these therapies do not have a unique theoretic framework and did not emerge at the same time, they shared some common features. These features include the recovery of a functional-contextual interpretation of behavior, incorporating natural language analysis into the therapeutic field with an emphasis on the development of broader and more flexible behavioral repertoires, values and expectations. But what it is more important, contrary to second-wave therapies and cognitive-behavior therapies (CBT), which direct efforts on modifying or eliminating maladaptive thoughts (and actions), third-wave therapies emphasize acceptance of those thoughts, as a strategy to overcome them. Therefore, they have finally generically adopted the label of “mindfulness and acceptance based interventions”, integrating four core process: the interest in acceptance, the defusion process, the relevance of “here and now”, and the “self as context” (Hayes, Luoma, Bond, Masuda, & Lillis, 2006; Hayes, Levin, Plumb-Vilardaga, Villatte, & Pistorello, 2013).
Essentially, the aim of interventions based on mindfulness and acceptance is to adopt a non-combative posture and serene conformity with the onset of physical problems (such as certain chronic pains), or psychological events (e.g. unpleasant memories, feelings of anxiety or depression, fears and threats). The acceptance process consists of individuals having direct and full contact with these experiences, without any psychological defense against them. However, this does not mean maintaining a general resigned attitude, or to abandon any direct effort to change, but to focus on acting on aspects of life more easily changeable, such as overt behavior and the life situations that generate certain emotions (Hayes, Wilson, Gifford, Follette, & Strosahl, 1996). Thus, people move from an attitude where thoughts or feelings are literally believed (and they must act), to one where they are simply warned. As a result, the negative impact of these thoughts, memories or feelings decreases (even if the frequency or intensity of these events is maintained).
Different studies have revealed the effectiveness of these mindfulness and acceptance-based interventions with different scope and pathologies, as systematic reviews and meta-analyses have supported (A-Tjak et al., 2015; Chiesa & Serretti, 2011; Fjorback, Arendt, Ornbol, Fink, & Walach, 2011; Hofmann, Sawyer, Witt, & Oh, 2010; Montgomery, Kim, & Franklin, 2011; Ost, 2008, Ost, 2014; Piet & Hougaard, 2011; Powers, Zum Vörde Sive Vörding, & Emmelkamp, 2009; Ruiz, 2012). According to results, acceptance process is a useful mechanism to regulate negative thoughts and, in general, to decrease their negative impact of symptoms. Most of those reviews are basically centered on affective/depressive disorders, and, to a lesser extent, on anxiety disorders.
Ruminative thoughts are presents in several disorders, but especially in depressive disorders. A meta-analysis by Aldao, Nolen-Hoeksema, & Schweizer (2010) shows that rumination represents the more harmful strategy in emotional regulation, compared to other strategies such as avoidance, problem solving, suppression, reappraisal or acceptance. Rumination is a central mechanism in depressive functioning. It is implicated in the relationship between biased cognitive processing and the dysregulation of emotions that typically characterize mood disorders (Gotlib & Joormann, 2010). In this case, ruminative thoughts are in themselves damaging because patients cannot “avoid” thinking about them and this generates discomfort and suffering. The existence of ruminant thoughts has a maintenance function for depression-related conditions (Martell, Addis, & Jacobson, 2001). Taking into account both the role of ruminative thoughts in depression, and the efficacy of therapies based on acceptance and mindfulness on depressive symptoms, our research question is how these strategies affect to ruminative thoughts. Since these thoughts can be directly or indirectly distressing, an acceptance process can be seen as apparently contradictory. If the presence of rumination interferes with the recovery of mental disorders, an acceptance strategy could be affecting this recovery. In this sense, it can be interesting to know how a mindfulness/acceptance procedure is affecting to ruminative thoughts in depressive patients, how effective the use of the mindfulness/acceptance intervention can be on those thoughts, and whether there is a differential effectiveness with the traditional CBT treatment. Therefore, a systematic review was performed to identify studies that assess the influence of interventions based on the mindfulness/acceptance process on ruminative thoughts, in patients with current or past depression.
Method
The study was performed in accordance with the PRISMA statement, which provides a detailed guideline of preferred reporting style for systematic reviews and meta-analyses (Liberati et al., 2009; Moher, Liberati, Tetzlaff, & Altman, 2009).
Selection criteria
Studies reported in English or Spanish were included according to the following a priori criteria: (1) design: randomized (RCTs) or pseudo-randomized (pRCT) controlled trials; (2) participants: patients with a history of at least one Major Depressive Episode (MDE); (3) intervention: studies had to test the efficacy of a specific Mindfulness-Acceptance-Based Behavioral Therapy or technique (e.g. cognitive defusion, values clarification), which are widely recognized in the literature as acceptance and mindfulness strategies or techniques; (4) comparator: treatment as usual (TAU) or other active intervention for the treatment of depression; (5) outcome measures: studies had to include one or more valid measures of ruminative thoughts: such as the Rumination on Sadness Scale (RSS; Raes, Hermans, & Eelen, 2003), the Rumination Response Style Questionnaire (RRS or RSQ; Nolen-Hoeksema & Morrow, 1991), or the Rumination and Reflection Questionnaire (RRQ; Trapnell & Campbell, 1999).
Excluded studies were reviews, editorials, non-randomized, uncontrolled or observational studies, case series and cases studies. We also excluded studies that presented repeat analyses of data already available in the included studies, as well as those published in a language other than English or Spanish.
Identification and selection of studies
A systematic literature search was performed in the following electronic databases: Embase (Elsevier), Medline and PreMedline (OvidSP), PsycInfo (EbscoHost), Cinahl (EbscoHost), and the Cochrane Controlled Trials Register, from the first available year to December 2016. The search strategy was developed for each electronic database using the combination of the following Medical Subject Heading (MeSH) and free-text terms: ([acceptance and commitment therapy] OR [acceptance-based behavior therapy] OR [acceptance-based strategies] OR [acceptance-based treatments] OR [acceptance-based interventions] OR [acceptance-based therapies] OR [acceptance-based approaches] OR [ACT] OR [mindfulness] OR [mindfulness-based strategies] OR [mindfulness-based treatments] OR [mindfulness-based interventions] OR [mindfulness-based therapies] OR [mindfulness-based approaches] OR [MBCT] OR [MBSR] OR [third wave therapies] OR [third wave of CBT]). The search strategies were developed, tested and refined by an experienced information specialist with input from authors (full details can be made available on request). In addition, reference lists of selected articles and other systematic reviews were inspected, and leading researchers in the field of MBCT were contacted to identify further relevant studies. Initially, duplicates were removed from the total number of identified records. Abstracts from the remaining records were then screened to retrieve full-text articles for assessment of eligibility. Finally, studies fulfilling inclusion criteria were selected for meta-analytic assessment. The retrieval process was verified by the four authors (AR, JB, LP, WP). Study inclusion was performed by the authors and disagreements were resolved by consensus.
Data collection and methodological quality of studies
A data extraction sheet was developed and the data collection included author and year, country of analysis, setting, study design (RCT or pRCT), sample characteristics (including age, sex, type of sample, condition), group characteristics (including intervention, comparison condition, number of group participants, drop-outs and withdrawals, follow-up), primary outcomes, definitions of effectiveness, and main findings. For each eligible study, all relevant data were extracted by one researcher. To ensure the quality and accuracy of the data, a second researcher verified the extracted data with their original sources. Quality assessment of studies was performed by one reviewer and verified for accuracy by a second reviewer using the criteria developed by the NHS Center for Reviews and Dissemination, which include 25 items for assessing the internal and external validity (Centre for Reviews and Dissemination, CRD), 2006). Disagreements between raters were resolved by discussion.
Statistical analysis
A meta-analysis was performed with the RevMan 5.2 software. We used the standardized mean difference (Hedges’ g) between treatment and control/comparison groups in the scores’ change from baseline to post-intervention (a negative value represents an effect favoring the MBCT intervention). Since only one study reported the standard deviations (SD) of change, we used the baseline average value as a proxy of the pooled SD, as recommended by Morris (2008). The cumulative result was then calculated by weighting the effect of each study by the inverse of the variance. We used a random effect model since we assumed different true effects across studies.
Statistical heterogeneity was analyzed by means of the Cochrane's Q and Higgins’ I2 statistics (Deeks, Altman, & Bradburn, 2008) (a conservative value of 0.10 was established for the significance of Q). A sensitivity analysis, excluding one study at a time was performed to assess its effect on results. Risk of publication bias was assessed by means of the visual inspection of the funnel plot and the Egger's test (Egger, Davey Smith, Schneider, & Minder, 1997).
Results
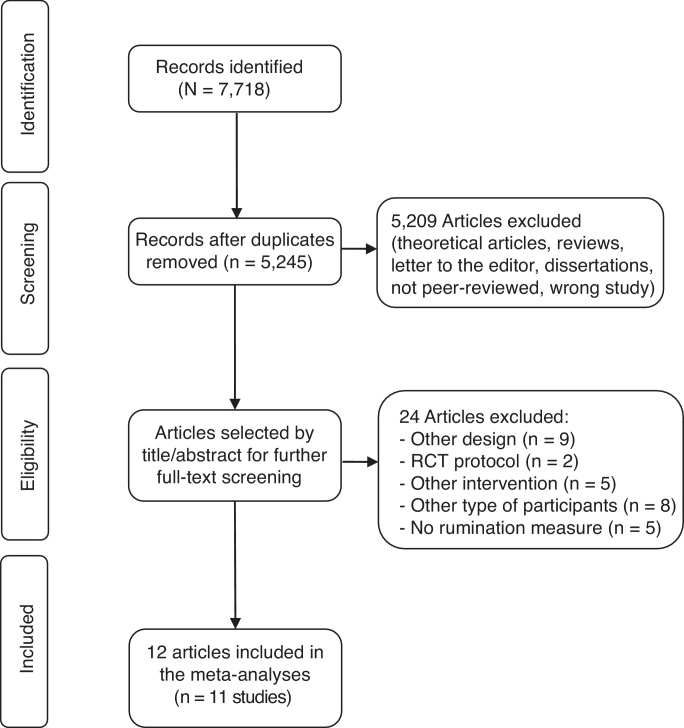
Figure 1 shows the selection process. The electronic search yielded 5,245 references without duplicates. Twelve articles, reporting on 11 studies (9 RCT and 2 pRCT), were included (Table 1). Five studies recruited patients with depression (one of them included a subgroup of non-depressed participants with a history of depression), three studies included patients with residual symptoms, and two included remitted patients. Nine studies compared MBCT to “TAU” or “waiting list” (McIndoo, File, Preddy, Clark, & Hopko, 2016 included a third group that received behavioral activation). Eight of them applied 8 weekly sessions (Batink, Peeters, Geschwind, van Os, & Wichers, 2013; Geschwind, Peeters, Drukker, van Os, & Wichers, 2011; Jermann et al., 2013; Kingston, Dooley, Bates, Lawlor, & Malone, 2007; Schoenberg & Speckens, 2014; Shahar, Britton, Sbarra, Figueredo, & Bootzin, 2010; Van Aalderen et al., 2012; Van Vugt, Hitchcock, Shahar, & Britton, 2012) and one applied 4 sessions (McIndoo et al., 2016). One study compared 12 weekly sessions of mindfulness-based yoga (MBY) to twice-weekly home walking practice with a DVD program (Schuver & Lewis, 2016), other compared 8 sessions of MBCT versus CBT (Manicavasagar, Perich, & Parker, 2012) and other 8 weekly sessions of MBCT to medication and placebo respectively (Bieling et al., 2012). In the nine studies that report the percentage of participants taking antidepressants it was similar between the intervention and control groups (excepting the comparison MBCT vs. medication of Bieling et al., 2012), ranging from 0% to 90% across studies. Five studies used the Rumination on Sadness Scale (RSS; Batink et al., 2013, Geschwind et al., 2011, McIndoo et al., 2016; Schoenberg & Speckens, 2014; Schuver & Lewis, 2016), four the Ruminative Response Scale (RRS) (Kingston et al., 2007, Manicavasagar et al., 2012, Shahar et al., 2010, Van Vugt et al., 2012), one the Rumination/Reflection Questionnaire (RRQ; Jermann et al., 2013) and other used the rumination subscale of the Experience Questionnaire (EQ; Bieling et al., 2012).
Figure 1.
Flow chart of the selection process.
Table 1.
Studies included.
| Author, year, country | Sample | Mean age % women | Taking ADM | On psychotherapy | Intervention | Comparator | Follow up | Rumination measure |
|---|---|---|---|---|---|---|---|---|
| Bieling et al. (2012) Canada | Patients with remitted MDD with at least 2 MDE (N = 84) | 44.1 58% |
0% (MBCT and placebo) 100% (medication) |
n.r. | MBCT (8 weekly group sessions) | 1) Maintenance medication 2) Maintenance placebo |
- | EQ (Rumination subscale) |
|
Geschwind et al. (2011) Batink et al. (2013) The Netherlands |
Patients with current residual depressive symptoms after at least one MDE (N = 130) | 43.9 75% |
34.6% | 12.3% | MBCT (8 weekly group sessions) | TAU | - | RSS |
| Jermann et al. (2013) USA | Remitted patients with ≥3 MDE (N = 36) | 46.8 72% |
0% | n.r. | MBCT (8 weekly group sessions) | TAU | 3 and 9 months | RRQ |
|
Kingston et al. (2007) Ireland |
Patients with ≥3 MDE and residual symptoms (N = 19) | 41.8 90% |
90% | n.r. | MBCT (8 weekly group sessions) | TAU | - | RRS |
|
Manicavasagar et al. (2012) Australia |
Patients with MDD (N = 69) | 45.8 64% |
n.r. | n.r. | MBCT (8 weekly group sessions) | Cognitive behavioural therapy | - | RRS |
| McIndoo et al. (2016) USA | College students with BDI > 14 or MDD (N = 50) | 19.2 62% |
12% | 0% | MBCT (4 weekly individual sessions) |
1) Waiting list 2) Behavioral Activation |
1 month | RRS |
| Schoenberg et al. (2014) The Netherlands |
Patients with MDD and 1-3 past MDE (N = 51) | 49.5 62.8% |
70.6% | n.r. | MBCT (8 weekly group sessions) | Waiting list | - | RSS |
| Schuver et al. (2016) USA | Women with a history of depression and current MDD (N = 40) | 42.8 100% |
52.5% | 2.5% | MBY (12 weekly group sessions) | Home walking program+ TAU | 1 month | RSS |
|
Shahar et al. (2010) USA |
Remitted patients with ≥3 MDE (N = 45) | 46.7 84.4% |
n.r. | 0% | MBCT (8 weekly group sessions) | Waiting list | - | RRS |
|
Van Aalderen et al. (2012) The Netherlands |
Patients with ≥3 MDE (N = 205) | 47.5 71% |
49.3% | n.r. | MBCT (8 weekly group sessions) | TAU | - | RSS |
| Van Vugt et al. (2012) USA | Recurrently depressed patients in partial or full remission (N = 52) | 47.4 73.1% |
50% | 0% | MBCT (8 weekly group sessions) | Waiting list | - | RRS |
Note. ADM: antidepressant medication; EQ: Experience Questionnaire; MBCT: Mindfulness-Based Cognitive Therapy; MBY: Mindfulness-Based Yoga; MDD: major depressive disorder; MDE: major depressive episode; n.r.: non reported; RSS: Rumination on Sadness Scale; RRQ: Rumination/Reflection Questionnaire; RRS: Ruminative Response Scale; TAU: treatment as usual.
Risk of bias of the included studies
Methodological quality of the included studies is shown in Appendix A. The two pRCT were consider of poor quality whereas all the RCT were classified as having a satisfactory quality. Regarding randomization, Schoenberg and Speckens (2014) allocated subjects depending on the date they were accepted for the MBCT course (before or after 8 weeks until onset of the intervention) and Kingston et al. (2007) on the day of referral, and therefore they present a high risk of bias. Only one out of the remaining studies did not report the randomization method. Eight out of the 11 studies adequately concealed the allocation and five assessed outcomes blinded to patients’ allocation. Four studies showed an attrition >20% and four used intention-to-treat analyses. Most studies did not report fidelity of treatment implementation or investigated potential contamination between groups.
Effect on rumination
MBCT vs. TAU
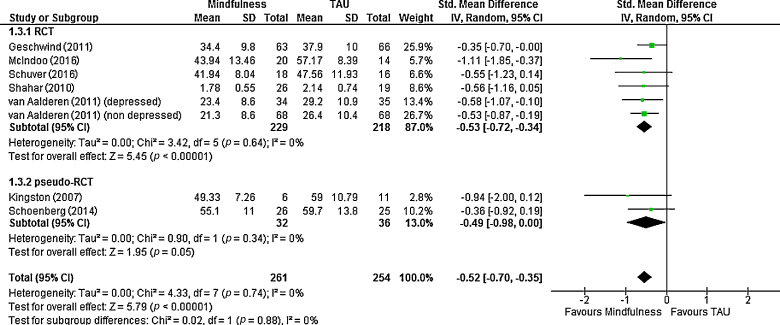
We meta-analyzed post-intervention scores of the six studies that compared MBCT to TAU or waiting list, plus the comparison MBY vs home walking program of Schuver and Lewis (2016) (Figure 2). Jermann et al. (2013) was excluded because their first post-assessment was at 1 month after the end of intervention. For Van Aalderen et al. (2012) we included separately the subgroups of patients with current/no current depression (thus, there were eight estimations). The pooled result was significantly favorable to the mindfulness intervention (n = 516; g = −0.59, 95% CI: 0.77, 0.41; I2 = 0%). Subgroup analysis (Table 2) showed that there were not significant differences between RCTs (k = 6; g = 0.60) and pseudorandomized studies (k = 2; g = −0.52), studies with depressed patients (k = 4, g = −0.63) vs. those with patients in full or partial remission (k = 4, g = −0.56), or between studies including patients with three or more MDE (k = 5; g = −0.54) vs. studies with less stringent criteria (k = 4; g = −0.67). Van Vugt et al. (2012) did not report data that could be meta-analyzed; they also obtained a significant reduction of ruminations favoring MBCT vs TAU (p < .001, R2 = .24).
Figure 2.
Meta-analysis of rumination post-scores, separately by design.
Table 2.
Results of the meta-analyses.
| k (N) | g (95% CI) | Q (p value) | I2 | p* | |
|---|---|---|---|---|---|
| MBCT vs. TAU | 8 (516) | −0.59 (−0.77, −0.41) | 3.07 (p = .88) | 0% | |
| Design | |||||
| RCT | 6 (448) | −0.60 (−0.79, −0.41) | 2.05 (p = .84) | 0% | .76 |
| pRCT | 2 (68) | −0.52 (−1.01, −0.03) | 0.93 (p = .33) | 0% | |
| Patients | |||||
| Depressed | 4 (188) | −0.63 (−0.93, −0.34) | 1.11 (p = .77) | 0% | .71 |
| Full or partial remission | 4 (328) | −0.56 (−0.79, −0.34) | 1.83 (p = .61) | 0% | |
| Major Depression Episodes | |||||
| ≥3 episodes | 5 (326) | −0.54 (−0.76, −0.32) | 2.17 (p = .70) | 0% | .48 |
| Other criteria | 4 (200) | −0.67 (−0.97, −0.38) | 1.44 (p = .70) | 0% | |
| MBCT vs active treatments | 3 (113) | −0.02 (−0.39, 0.35) | 0.48 (p = .79) | 0% | |
Note. * p-value for the between-group difference.
CI: confidence interval; k: number of estimations; MBCT: Mindfulness-Based Cognitive Therapy; pRCT: pseudo-randomized controlled trial: TAU: treatment as usual.
Given the low number of studies included in the MA we did not performed Egger's test to assessed publication bias. Visual inspection of the funnel plot showed that the two studies with higher standard errors obtained the strongest effects, which could suggest a “small-study” bias, although the number of studies is too low to draw firm conclusions.
Follow up data were available for three studies (Jermann et al., 2013, McIndoo et al., 2016; Schuver & Lewis, 2016). We meta-analyzed the change in scores from baseline to one-month follow up and the difference favoring the mindfulness groups was significant, although with a smaller size effect than the observed at post-intervention (g = −0.46, 95% CI: −0.81, −0.10; I2 = 0%).
MBCT vs. active treatments
Three studies included control groups with active treatments for depression (medication, CBT and behavioral activation, respectively). The pooled difference in post-treatment scores compared to MBCT was not significant (n = 113; g = −0.02, 95% CI: −0.39, .35; I2 = 0%).
Rumination as mediator of MBCT effect on depression
Five studies analyzed the mediator role of rumination in the effect of intervention on depressive symptoms, with mixed results. The studies of Shahar et al. (2010) and Van Aalderen et al. (2012) showed an independent significant mediation effect of rumination (bootstrapping point estimates for the individual indirect effect of −1.87 and −0.54 respectively), whereas Batink et al. (2013) and Bieling et al. (2012) did not find significant results (they did not report numerical data). Manicavasagar et al. (2012) only analyzed the association of post rumination scores and depressive symptoms and obtained a significant result both for MBCT (β = −.76, p < .001) and CBT groups (β = −.76, p < .001).
We performed an exploratory subgroup analysis of the change in depression scores comparing the studies that obtained medium/strong (g ≥ .50) vs. weak (g < .50) effects on rumination, including all studies that reported data. For the study of Geschwind et al. (2011), we used the data reported in the article of Batink et al. (2013), since it offers separated results for patients with 2 or less versus 3 or more depressive episodes (and only the former showed a reduction in rumination ≥ .50). For McIndoo et al. (2016) the MBCT sample was split in two equal subgroups, to independently compare them to waiting list and behavioral activation, respectively. Eight studies applied different versions of the Beck Depression Inventory (BDI; Beck, Steer, & Brown, 1996) and two used the Inventory of Depressive Symptoms (IDS; Rush, Gullion, Basco, Jarrett, & Trivedi, 1996). Studies that showed medium/strong effects on rumination obtained a significant reduction in depression scores (k = 6; g = −0.55, 95% CI: −0.95, −0.15; I2 = 55%). Schuver and Lewis (2016) accounted for all the observed heterogeneity; in this study, despite the observed reduction in rumination favoring the mindfulness group, no significant differences in depression were found, and excluding it of the MA yielded a g = −.69. In the subgroup of studies that found weak effects on rumination the reduction in depression scores was at the limit of significance (k = 6; g = −0.29; 95% CI: −0.58, 0.00; I2 = 44%), although there was (non-significant) heterogeneity with two studies showing a medium and strong effect, respectively. The difference between subgroups was not significant (p = .30), although when the mentioned above study of Schuver and Lewis (2016) was excluded it reached the threshold of significance (p = .05).
Discussion
Main findings of the study
In this review we aimed to understand how mindfulness/acceptance therapies affect ruminative thoughts in patients with current or past depressive disorders. Eleven studies were identified in the literature, nine RCT of good methodological quality and two pRCT. There was some heterogeneity among them (e.g. patients in diverse phases of their depressive disorder, number of past episodes, scales used, different attrition rates), but results were statistically consistent. They show that MBCT, compared to usual care, produces a significant and moderate (according to the usual parameters, Cohen, 1988) reduction in rumination. This effect seems independent of the treatment phase (acute or maintenance) or the number of past depressive episodes, and it was maintained one month after the end of treatment. On the other hand, mindfulness/acceptance procedures seems as effective at reducing rumination as other treatments such as medication, CBT and behavioral activation. However, these results must be interpreted with caution given the low number of studies included, but they are in line with the narrative review published by Barraca (2012), who concluded that acceptance and mindfulness strategies are as or more effective than others such as focalized distraction or some forms of restructuring. However, it can not be ruled out that part of the explanation of this outcome has to do with the common factors of the different therapies that are used for the treatment of depression.
A first consideration is whether these results could be considered unexpected, since mindfulness/acceptance process do not try to reduce (or suppress) unpleasant thoughts, but the emotional impact they produce on the individual. Indeed, some laboratory studies with healthy participants have shown that mindfulness/acceptance strategies, compared to suppression techniques, did not reduced intrusive thoughts but the stress associated with them (Marcks & Woods, 2005; Najmi, Riemann, & Wegner, 2009). Unfortunately, the rumination scales used in the included studies assess the occurrence of intrusive thoughts but not their emotional impact. It is possible that the reduction of ruminative thinking is related to the fact of not “feeding” those thoughts, as it has been considered that the most frequent onset and the highest intensity of certain thoughts could be related to trying to avoid or reject them, or make them disappear, in accordance with the theory of the ironic process of mental control (Wegner, 1994). Therefore, although the purpose of acceptance and mindfulness procedures was to allow the ruminative or intrusive thoughts to occur, albeit affecting the patient to a lesser extent, in the end, paradoxically, they would reduce it because of the thoughts not being stimulated by means of attempts to control, restructure or reduce them. This is a desirable clinical outcome, as it would lead to improvement in the patient, but at the current state of research it is not possible to conclude whether improvements in rumination scores are due to the patients’ altered relationship with their ruminative thoughts or to the frequency/intensity of these.
A second consideration refers to whether the effects observed on rumination are actually produced by the proposed psychological mechanisms (mindfulness/acceptance). Although most of the included studies applied measures of the participants’ perception of their own mindfulness/acceptance skills, only four reported the associations of these measures with rumination (using different statistical approaches). At the correlational level, Van Aalderen et al. (2012) found a statistically significant negative correlation (r = −.56, p < .001) among the scores on the subscale “accept without judgment” (from the Kentucky Inventory of Mindfulness Questionnaire, KIMS) and the level of rumination, whereas Bieling et al. (2012) did not observe a significant association using the Toronto Mindfulness Scale. Batink et al. (2013) found that changes produced in rumination by the MBCT intervention were significantly mediated by KIMS scores. Finally, Manicavasagar et al. (2012) observed that post-scores in the Mindful Attention Awareness Scale (MAAS) significantly related to lower rumination in the MBCT group, but not in the CBT condition. This is an interesting result since MBCT did not outperform CBT in the increasing of mindfulness skills or the reduction of rumination; this suggests that MBCT training, rather than increasing mindfulness skills compared to CBT, could enable patients to orientate the application of those skills to their ruminative thinking, whereas CBT would decrease rumination through other psychological mechanisms.
Third, ruminative thoughts have been found as a central mechanism in the onset and maintenance of depressive functioning (Gotlib & Joormann, 2010; Martell et al., 2001), and therefore we analyzed the mediator role of rumination in the effect of interventions on depressive symptoms. The five studies providing data obtained mixed results, and the heterogeneity of the statistical procedures applied precluded a quantitative synthesis of the data reported. Instead, we performed an exploratory subgroup meta-analysis that showed a better antidepressant effect in the studies that obtained a stronger effect on rumination. The only study that compared MBCT to CBT, Manicavasagar et al. (2012), found that rumination significantly predicted symptoms at post-intervention (when treatment were decreasing both depression symptoms and ruminative thoughts), and it could raise the question of whether rumination is a central process to feel depressed or it is part of the core of symptoms of depression. In this last case, the decrement of ruminative thoughts can be understood as part of therapy efficacy.
Clinical implications of the mediating role of rumination
From a clinical perspective, mindfulness/acceptance interventions have shown to be as effective to reduce depressive symptomatology as antidepressant drugs or CBT (Bockting, Hollon, Jarrett, Kuyken, & Dobson, 2015; Clarke, Mayo-Wilson, Kenny, & Pilling, 2015; Khoury et al., 2013), but the evidence on their mechanisms of action is still scarce. In this review we have presented an integrated view of the empirical findings about the effect of mindfulness/acceptance interventions on ruminative thoughts in depression. Results are positive and furthermore suggest that changes in rumination are mediated by mindfulness/acceptance processes, and that they in turn mediate in the clinical effects of interventions.
Limitations of the study and implications for future research
However, these conclusions are constrained by several limitations, such as the few studies identified, the heterogeneity of the measures used, the lacking of reporting about associations between rumination, self-perceived mindfulness skills and depressive symptoms, or the scarcity of follow up data. There is a need of more well controlled studies with real patients, that compare the most commonly used cognitive-behavioral techniques to treat ruminative and intrusive thoughts (e.g. restructuring, cognitive exposure or stopping the thought) to the acceptance and mindfulness techniques. It also should be necessary to carry out a comparison of the psychometric properties of the existing instruments to assess rumination, as well as including measures of the participants’ perception of their mindfulness/acceptance skills, and of the impact of ruminative thoughts on their psychological functioning. Assessments of these variables should be taken at different time-points during therapy, to analyze the temporal evolution of the changes produced by the intervention (i.e. whether the acceptance of ruminative thoughts occurs before their reduction or not). Medium and long-term follow up data are needed, since relapse and recurrence are common in major depression and different therapeutic strategies could lead to different long-term effects. A more sound knowledge of these aspects will enable a more efficient application of psychological therapies to treat depression, as well as a more personalized treatment according to the different patients’ psychological traits and skills. But along with this type of approach, the analysis from a more experiential perspective of the experience of rumination on the part of patients will be another of the challenges for future research.
Funding and acknowledgments
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The authors would like to thank to Leticia Cuellar for her technical assistance with the search strategies and to Carlos Gonzalez for his assistance with the literature retrieval. The authors would also like to thank Jason Willis-Lee for his translation and copyediting support.
Footnotes
References marked with an asterisk indicate studies included in the meta-analyses.
Appendix A. Quality assessment for the randomized controlled trials (RCT) and non-randomized controlled trials (nRCT).
| Geschwind et al. (2011),Batink et al. (2013) | Bieling et al. (2012) | Jermann et al. (2013) | Kingston et al. (2007) | Manicavasagar et al. (2012) | McIndoo et al. (2016) | Schoenberg et al. (2014) | Schuver et al. (2016) | Shahar et al. (2010) | Van Aalderen et al. (2011) | Van Vugt et al. (2012) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Was there a comparison group? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 2. Was the comparison group concurrent? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 3. Were participants enrolled into the groups by the researchers? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 4. Was the study described as an RCT? | Yes | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes | Yes |
| 5. Was allocation of treatment concealed? | Yes | Yes | Yes | No | Yes | Yes | No | Unclear | Yes | Yes | Yes |
| 6. Was the method used to assign participants to treatment groups truly random? | Yes | Yes | Yes | No | Yes | Yes | No | Yes | Unclear | Yes | Yes |
| 7. Was the assessment of outcomes conducted blind to treatment allocation? | No | Yes | No | Unclear | Yes | Unclear | No | Yes | Yes | Unclear | Yes |
| 8. Has there been a systematic attempt to identify and measure potential confounders? | Yes | Yes | Yes | No | No | Yes | Yes | No | Yes | Yes | Yes |
| 9. Were possible confounders controlled for appropriately in the analysis? | Yes | Yes | Yes | No | Yes | Yes | Yes | No | Yes | Yes | Yes |
| 10. Was the intervention (and control) delivered as planned? | Yes | Yes | Yes | Yes | Yes | Yes | Unclear | Unclear | Unclear | Unclear | Unclear |
| 11. Was there an investigation of possible contamination? | No | No | No | No | No | No | No | No | No | No | No |
| 12. Was contamination accounted for in the analysis? | No | No | No | No | No | No | No | No | No | No | No |
| 13. Was the sample size adequate for the analysis of the main outcome variables? | Yes | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes | Yes |
| 14. Were the eligibility criteria for the study adequately specified? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 15. Were participant characteristics described? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 16. Were all participants who began the study accounted for at the end of the study? | Yes | No | No | No | No | Yes | No | No | Yes | Yes | Yes |
| 17. Were at least 80% of participants who began the study assessed at the end of the study? | Yes | No | No | No | No | Yes | Yes | Yes | Yes | Yes | Yes |
| 18. Did analysis include all participants who entered the study and who provided baseline data? | Yes | No | No | No | No | Yes | No | Yes | No | Yes | No |
| 19. Were the methods of analysis appropriate? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 20. Was the main outcome(s) assessed using an appropriate (a validated) measure? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 21. Were data collected at the same time for both groups? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes |
| 22. Was the length of follow-up appropriate? | No | No | Yes | No | No | Yes | No | Yes | No | Yes | No |
| Internal validity | Satisfactory | Satisfactory | Satisfactory | Poor | Satisfactory | Satisfactory | Poor | Satisfactory | Satisfactory | Satisfactory | Satisfactory |
| 23. Was any inappropriate coercion used to encourage attendance or assignment to control/comparison groups? | No | No | No | No | No | No | No | No | No | No | No |
| 24. Were the participants unrepresentative of the populations that would receive these treatments in practice? | No | No | No | No | No | No | No | No | No | No | No |
| 25. Did the intervention group have characteristics that would limit its wider adoption? | No | No | No | No | No | No | No | No | No | No | No |
| External validity | Good | Good | Good | Good | Good | Good | Good | Good | Good | Good | Good |
References1
- Aldao A., Nolen-Hoeksema S., Schweizer S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review. 2010;30:217–237. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- A-Tjak J.G.L., Davis M.L., Morina N., Powers M.B., Smits J.A.J., Emmelkamp P.M.G. A Meta-Analysis of the Efficacy of Acceptance and Commitment Therapy for Clinically Relevant Mental and Physical Health Problems. Psychotherapy and Psychosomatics. 2015;84:30–36. doi: 10.1159/000365764. [DOI] [PubMed] [Google Scholar]
- Barraca J. Mental control from a third-wave behavior therapy perspective. International Journal of Clinical and Health Psychology. 2012;12:109–121. [Google Scholar]
- Batink T., Peeters F., Geschwind N., van Os J., Wichers M. How Does MBCT for Depression Work? Studying Cognitive and Affective Mediation Pathways. PLoS ONE. 2013;8:e72778. doi: 10.1371/journal.pone.0072778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck A., Steer R., Brown G. Psychological Corporation; San Antonio, TX: 1996. Manual for the Beck Depression Inventory–II. [Google Scholar]
- Bieling P.J., Hawley L.L., Bloch R.T., Corcoran K.M., Levitan R.D., Young L.T., Macqueen G.M., Segal Z.V. Treatment-specific changes in decentering following mindfulness-based cognitive therapy versus antidepressant medication or placebo for prevention of depressive relapse. Journal of Consulting and Clinical Psychology. 2012;80:365–372. doi: 10.1037/a0027483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bockting C.L., Hollon S.D., Jarrett R.B., Kuyken W., Dobson K. A lifetime approach to major depressive disorder: The contributions of psychological interventions in preventing relapse and recurrence. Clinical Psychology Review. 2015;41:16–26. doi: 10.1016/j.cpr.2015.02.003. [DOI] [PubMed] [Google Scholar]
- Centre for Reviews and Dissemination, CRD . University of York; York: 2006. Systematic Review of the Clinical Effectiveness of Self Care Support Networks in Health and Social Care. [Google Scholar]
- Chiesa A., Serretti A. Mindfulness based cognitive therapy for psychiatric disorders: A systematic review and meta-analysis. Psychiatry Research. 2011;187:441–453. doi: 10.1016/j.psychres.2010.08.011. [DOI] [PubMed] [Google Scholar]
- Clarke K., Mayo-Wilson E., Kenny J., Pilling S. Can non-pharmacological interventions prevent relapse in adults who have recovered from depression?. A systematic review and meta-analysis of randomised controlled trials. Clinical Psychology Review. 2015;39:58–70. doi: 10.1016/j.cpr.2015.04.002. [DOI] [PubMed] [Google Scholar]
- Cohen J. 2nd ed. Lawrence Erlbaum; New Jersey: 1988. Statistical Power Analysis for the Behavioral Sciences. [Google Scholar]
- Crane R.S., Kuyken W., Williams J.M.G., Hastings R.P., Cooper L., Fennell M.J.V. Competence in Teaching Mindfulness-Based Courses: Concepts. Development and Assessment. Mindfulness. 2012;3:76–84. doi: 10.1007/s12671-011-0073-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deeks J.J., Altman D.G., Bradburn M.J. Statistical Methods for Examining Heterogeneity and Combining Results from Several Studies in Meta-Analysis. In: Egger M., Davey-Smith G., Altman D., editors. Systematic Reviews in Health Care. BMJ Publishing Group; London, UK: 2008. pp. 285–312. [Google Scholar]
- Egger M., Davey Smith G., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. British Medical Journal. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fjorback L.O., Arendt M., Ornbol E., Fink P., Walach H. Mindfulness-Based Stress Reduction and Mindfulness-Based Cognitive Therapy - a systematic review of randomized controlled trials. Acta Psychiatrica Scandinavica. 2011;124:102–119. doi: 10.1111/j.1600-0447.2011.01704.x. [DOI] [PubMed] [Google Scholar]
- *Geschwind N., Peeters F., Drukker M., van Os J., Wichers M. Mindfulness training increases momentary positive emotions and reward experience in adults vulnerable to depression: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2011;79:618–628. doi: 10.1037/a0024595. [DOI] [PubMed] [Google Scholar]
- Gotlib I.H., Joormann J. Cognition and Depression: Current Status and Future Directions. Annual Review of Clinical Psychology. 2010;6:285–312. doi: 10.1146/annurev.clinpsy.121208.131305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes S. Acceptance and Commitment Therapy, Relational Frame Theory, and the Third Wave of Behavioral and Cognitive Therapies. Behavior Therapy Integrative Behavioral Couples Therapy. 2004;35:639–665. doi: 10.1016/j.beth.2016.11.006. [DOI] [PubMed] [Google Scholar]
- Hayes S., Levin M., Plumb-Vilardaga J., Villatte J., Pistorello J. Acceptance and Commitment Therapy and Contextual Behavioral Science: Examining the Progress of a Distinctive Model of Behavioral and Cognitive Therapy. Behavior Therapy. 2013;44:180–198. doi: 10.1016/j.beth.2009.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes S., Wilson K., Gifford E., Follette V., Strosahl K. Experimental avoidance and behavioral disorders: A functional dimensional approach to diagnosis and treatment. Journal of Consulting and Clinical Psychology. 1996;64:1152–1168. doi: 10.1037//0022-006x.64.6.1152. http://www.ncbi.nlm.nih.gov/pubmed/8991302. [DOI] [PubMed] [Google Scholar]
- Hayes S.C., Luoma J.B., Bond F.W., Masuda A., Lillis J. Acceptance and Commitment Therapy: Model, processes and outcomes. Psychology Faculty Publications. Paper, 101. 2006 doi: 10.1016/j.brat.2005.06.006. http://scholarworks.gsu.edu/psych_facpub. [DOI] [PubMed] [Google Scholar]
- Hofmann S.G., Sawyer A.T., Witt A.A., Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2010;78:169–183. doi: 10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jermann F., Van der Linden M., Gex-Fabry M., Guarin A., Kosel M., Bertschy G., Aubry J.M., Bondolfi G. Cognitive Functioning in Patients Remitted from Recurrent Depression: Comparison with Acutely Depressed Patients and Controls and Follow-up of a Mindfulness-Based Cognitive Therapy Trial. Cognitive Therapy and Research. 2013;37:1004–1014. [Google Scholar]
- Johnson D., Mullen D., Smith I.D., Wilson A. Mindfulness in addictions. BJPscyh Advances. 2016;22:412–419. [Google Scholar]
- Kabat-Zinn J. Delta; New York: 1990. Full Catastrophe Living: The program of the Stress Reduction Clinic at the University of Massachusetts Medical Center. [Google Scholar]
- Khoury B., Lecomte T., Fortin G., Masse M., Therien P., Bouchard V., Chapleau M.A., Paquin K., Hofmann S.G. Mindfulness-based therapy: A comprehensive meta-analysis. Clinical Psychology Review. 2013;33:763–771. doi: 10.1016/j.cpr.2013.05.005. [DOI] [PubMed] [Google Scholar]
- Kingston T., Dooley B., Bates A., Lawlor E., Malone K. Mindfulness-based cognitive therapy for residual depressive symptoms. Psychology and Psychotherapy: Theory, Research and Practice. 2007;80:193–203. doi: 10.1348/147608306X116016. [DOI] [PubMed] [Google Scholar]
- Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P.A., Clarke M., Devereaux P.J., Kleijnen J., Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Journal of Clinical Epidemiology. 2009;62:e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- Manicavasagar V., Perich T., Parker G. Cognitive Predictors of Change in Cognitive Behaviour Therapy and Mindfulness-Based Cognitive Therapy for Depression. Behavioural and Cognitive Psychotherapy. 2012;40:227–232. doi: 10.1017/S1352465811000634. [DOI] [PubMed] [Google Scholar]
- Marcks B.a., Woods D.W. A comparison of thought suppression to an acceptance-based technique in the management of personal intrusive thoughts: A controlled evaluation. Behaviour Research and Therapy. 2005;43:433–445. doi: 10.1016/j.brat.2004.03.005. [DOI] [PubMed] [Google Scholar]
- Martell C.R., Addis M.E., Jacobson N.S. W. W. Norton; New York: 2001. Depression in context: Strategies for guided action. [Google Scholar]
- *McIndoo C.C., File A.A., Preddy T., Clark C.G., Hopko D.R. Mindfulness-based therapy and behavioral activation: A randomized controlled trial with depressed college students. Behaviour Research and Therapy. 2016;77:118–128. doi: 10.1016/j.brat.2015.12.012. [DOI] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Journal of Clinical Epidemiology. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- Montgomery K.L., Kim J.S., Franklin C. Acceptance and commitment therapy for psychological and physiological illnesses: A systematic review for social workers. Health & Social Work. 2011;36:169–181. doi: 10.1093/hsw/36.3.169. [DOI] [PubMed] [Google Scholar]
- Morris S.B. Estimating effect sizes from pretest-posttest-control group designs. Organizational Research Methods. 2008;11:364–386. [Google Scholar]
- Najmi S., Riemann B.C., Wegner D.M. Managing unwanted intrusive thoughts in obsessive-compulsive disorder: relative effectiveness of suppression, focused distraction, and acceptance. Behaviour Research and Therapy. 2009;47:494–503. doi: 10.1016/j.brat.2009.02.015. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S., Morrow J. A prospective study of depression and posttraumatic stress symptoms after a natural disaster: The 1989 Loma Prieta earthquake. Journal of Personality and Social Psychology. 1991;61:115–121. doi: 10.1037//0022-3514.61.1.115. [DOI] [PubMed] [Google Scholar]
- Ost L.-G. Efficacy of the third wave of behavioral therapies: A systematic review and meta-analysis. Behaviour Research and Therapy. 2008;46:296–321. doi: 10.1016/j.brat.2007.12.005. [DOI] [PubMed] [Google Scholar]
- Ost L.-G. The efficacy of Acceptance and Commitment Therapy: An updated systematic review and meta-analysis. Behaviour Research and Therapy. 2014;61:105–121. doi: 10.1016/j.brat.2014.07.018. [DOI] [PubMed] [Google Scholar]
- Piet J., Hougaard E. The effect of mindfulness-based cognitive therapy for prevention of relapse in recurrent major depressive disorder: A systematic review and meta-analysis. Clinical Psychology Review. 2011;31:1032–1040. doi: 10.1016/j.cpr.2011.05.002. [DOI] [PubMed] [Google Scholar]
- Powers M.B., Zum Vörde Sive Vörding M.B., Emmelkamp P.M.G. Acceptance and Commitment Therapy: A Meta-Analytic Review. Psychotherapy and Psychosomatics. 2009;78:73–80. doi: 10.1159/000190790. [DOI] [PubMed] [Google Scholar]
- Raes F., Hermans D., Eelen P. De Nederlandstalige versie van de Ruminative Response Scale (RRS-NL) en de Rumination on Sadness Scale (RSS-NL) (The Dutch version of the Ruminative Response Scale (RRS-NL) and the Rumination on Sadness Scale (RSS-NL)) Gedragstherapie. 2003;36:97–104. [Google Scholar]
- Ruiz F.J. Acceptance and Commitment Therapy versus Traditional Cognitive Behavioral Therapy: A Systematic Review and Meta-analysis of Current Empirical Evidence. International Journal of Psychology & Psychological Therapy. 2012;12:333–357. [Google Scholar]
- Rush A.J., Gullion C.M., Basco M.R., Jarrett R.B., Trivedi M.H. The Inventory of Depressive Symptomatology (IDS): psychometric properties. Psychological Medicine. 1996;26:477–486. doi: 10.1017/s0033291700035558. [DOI] [PubMed] [Google Scholar]
- Schoenberg P.L.A., Speckens A.E.M. Modulation of induced frontocentral theta (Fm-θ) event-related (de-)synchronisation dynamics following mindfulness-based cognitive therapy in Major Depressive Disorder. Cognitive Neurodynamics. 2014;8:373–388. doi: 10.1007/s11571-014-9294-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Schuver K.J., Lewis B.A. Mindfulness-based yoga intervention for women with depression. Complementary Therapies in Medicine. 2016;26:85–91. doi: 10.1016/j.ctim.2016.03.003. [DOI] [PubMed] [Google Scholar]
- Segal Z.V., Williams J.M.G., Teasdale J.D. Guilford Press; New York: 2002. Mindfulness-based cognitive therapy for depression. [Google Scholar]
- *Shahar B., Britton W.B., Sbarra D.A., Figueredo A.J., Bootzin R.R. Mechanisms of Change in Mindfulness-Based Cognitive Therapy for Depression: Preliminary Evidence from a Randomized Controlled Trial. International Journal of Cognitive Therapy. 2010;3:402–418. [Google Scholar]
- Trapnell P., Campbell J. Private self-consciousness and the five-factor model of personality: distinguishing rumination from reflection. Journal of Personality and Social Psychology. 1999;76:284–304. doi: 10.1037//0022-3514.76.2.284. [DOI] [PubMed] [Google Scholar]
- *Van Aalderen J.R., Donders a.R.T., Giommi F., Spinhoven P., Barendregt H.P., Speckens a.E.M. The efficacy of mindfulness-based cognitive therapy in recurrent depressed patients with and without a current depressive episode: A randomized controlled trial. Psychological Medicine. 2012;42:989–1001. doi: 10.1017/S0033291711002054. [DOI] [PubMed] [Google Scholar]
- Van Vugt M.K., Hitchcock P., Shahar B., Britton W. The Effects of Mindfulness-Based Cognitive Therapy on Affective Memory Recall Dynamics in Depression: A Mechanistic Model of Rumination. Frontiers in Human Neuroscience. 2012;6 doi: 10.3389/fnhum.2012.00257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wegner D.M. Ironic processes of mental control. Psychological Review. 1994;101:34–52. doi: 10.1037/0033-295x.101.1.34. [DOI] [PubMed] [Google Scholar]