Abstract
Objective
This study aimed to assess the heterogeneity and stability of cognition in patients with a non‐affective psychotic disorder and their unaffected siblings. In addition, we aimed to predict the cognitive subtypes of siblings by their probands.
Method
Assessments were conducted at baseline, 3 and 6 years in 1119 patients, 1059 siblings and 586 controls from the Genetic Risk and Outcome of Psychosis (GROUP) study. Group‐based trajectory modeling was applied to identify trajectories and clustered multinomial logistic regression analysis was used for prediction modeling. A composite score of eight neurocognitive tests was used to measure cognitive performance.
Results
Five stable cognitive trajectories ranging from severely altered to high cognitive performance were identified in patients. Likewise, four stable trajectories ranging from moderately altered to high performance were found in siblings. Siblings had a higher risk of cognitive alteration when patients’ alteration was mild (OR = 2.21), moderate (OR = 5.70), and severe (OR = 10.07) compared with patients with intact cognitive function. The familial correlation coefficient between pairs of index patients and their siblings was 0.27 (P = 0.003).
Conclusions
The cognitive profiles identified in the current study might be suitable as endophenotypes and could be used in future genetic studies and predicting functional and clinical outcomes.
Keywords: schizophrenia, psychosis, cognition, cognitive impairment
Significant outcomes.
To our knowledge, this is the first large‐scale study to report cognitive trajectories in patients with psychosis (probands) and their unaffected siblings.
We identified five stable cognitive trajectories in probands: ‘severely altered’, ‘moderately altered’, ‘mildly altered’, ‘normal’, and ‘high performer’. Similarly, four stable cognitive trajectories were identified in healthy siblings: ‘moderately altered’, ‘mildly altered’, ‘normal’, and ‘high performer’.
The cognitive trajectory of probands significantly predicted the cognitive trajectory of siblings. The intraclass correlation (ICC) between pairs of siblings and probands was 0.27.
Limitations.
Selection and attrition bias may be evident as controls were selected by random mailing and study participants dropped out of the study respectively.
The prediction of a moderately altered group of siblings by high cognitive performer group of patients was ambiguous and unstable due to low frequency.
Eight cognitive tests were used in this study; therefore, including other tests may lead to different trajectories with different predictions.
Introduction
Schizophrenia spectrum disorders consist of multiple symptom dimensions, caused by the interaction of genetic, environmental, and internal factors 1. One of these dimensions is cognitive alteration which is present in 75–80% of the patients 2 and which has been demonstrated to be a predictor of symptomatic and functional outcome (e.g., working activity, daily living activity) 3, 4, 5, 6, 7. Evidence on whether cognitive alteration precedes schizophrenia or cognitive function deteriorated after the occurrence of schizophrenia is mixed 8, 9, 10. The most affected cognitive functions are episodic and working memory, attention, verbal fluency, executive function, problem‐solving, processing speed, and social cognition 11.
Cognitive function can be measured based on the actual change in patient's cognitive performance over time or deviation from the familial cognitive performance 12. Although cognitive alteration in patients with schizophrenia is heterogeneous, the majority of the studies shows that cognitive alteration within an individual with schizophrenia is stable and persistent over time 13, 14, 15. On the other hand, in patients with first‐episode psychosis, studies investigating the trajectories of different cognitive performance suggested an improvement over time 16, 17. Given the substantial difference across patients, clustering methods using latent class analysis, hierarchical mixture model and group‐based trajectory modeling have been used to identify cognitive trajectories in a different group of population 18. To date, two to five cognitive trajectories have been identified in patients with psychosis who differ in terms of demographic and clinical characteristics 19, 20, 21, 22, 23. Cognitive alteration is also common in unaffected siblings, but to a lesser extent, and subtyping is relevant to identify meaningful homogeneous trajectories 13, 24, 25, 26, 27, 28. In our previous cross‐sectional study, we demonstrated three subtypes of cognitive alteration (i.e., normal, mixed, and impaired) in siblings 23.
Cognitive alteration in patients with schizophrenia can be associated with cannabis use 29, negative and schizotypy symptoms 30, 31 and medical comorbidities such as diabetes mellitus, hypertension, dyslipidemia, and obesity 32. Other influencing factors include decreased gray matter density in the cerebellum 33, reduced blood omega‐3 fatty acids 34, N‐methyl‐d‐Aspartate receptor (NMDAR) hypofunction 35 and inflammation 36. In siblings, cognitive alteration can be attributed to shared genetic 37, 38, 39 and socio‐environmental risk factors with the patients 13. Cognitive alteration can be considered an inheritable trait of schizophrenia, which itself has a heritability (h 2) 31–62% 40, 41, 42. Some family‐based studies have also found a higher rate of cognitive alteration in unaffected relatives of individuals with schizophrenia than in the general population 43. These findings support the assertion that cognitive dysfunction can be designated an important endophenotype of schizophrenia. This is important for future large‐scale twin/family‐based and SNP‐based heritability studies.
Schizophrenia is invariably acknowledged to be an extremely heterogeneous disorder. Yet, efforts to find meaningful subtypes (cognitive, clinical, or neurobiological) have been manifold but they remain of questionable success. Possible explanations for the unsuccessful subtyping are use of single cognitive test or domain (e.g., intelligence quotient (IQ)) based on mean values that do not take into account heterogeneity, uncertainty on whether cognitive alteration is general or specific, limited number of longitudinal studies with short follow‐up period, small sample size, and limited use of data from healthy siblings and controls 13, 44, 45. Therefore, to our knowledge, this is the first large‐scale long‐term study which included cognitive trajectory modeling for both patients and their unaffected siblings.
The aim of this study was twofold. First, we examined ways to unravel the heterogeneity of neurocognition, by classifying patients and siblings respectively into different subgroups based on the course of composite overall cognition scores over time, separately from each other, based on eight neurocognitive test parameters. After determining meaningful subgroups of patients and siblings, we aimed to predict the cognitive subtypes of siblings by subtypes of patients within a family using sibling‐patient analyses. Given the advancement of clustering technique and increasing trend of identified subgroups of patients with schizophrenia 19, 20, 21, 22, 23, we hypothesized that more meaningful trajectories can be discovered. There has been a substantial controversy regarding the course of cognitive alliteration in patients with schizophrenia and their unaffected siblings 13. The accumulated body of evidence 13 shows that the course of cognitive function in schizophrenia is inconsistent while some studies show stability or improvement, others support deterioration of cognitive function. In this study, we hypothesized that the cognitive trajectory over time is stable. In addition, we hypothesized the probands cognitive trajectory predict siblings cognitive alteration trajectory.
Methods
Study setting and population
The current study was performed within the framework of the Genetic Risk and Outcome of Psychosis (GROUP) project, a longitudinal multi‐center cohort study in the Netherlands and Belgium. Patients with non‐affective psychotic disorder based on DSM‐IV 46, age between 16 and 50 years and good command of the Dutch language were included. Siblings were included if they (i) were between 16 and 50 years, (ii) had a good command of the Dutch language, and (iii) had no lifetime psychotic disorder. Controls were included if they did not have a lifetime diagnosis of psychotic, bipolar or current depressive disorder. In addition, controls were included if they did not have a first or second degree relative with psychotic disorder 47. The procedure of recruitment, informed consent, ethical approval, and population characteristics at baseline have been described in detail elsewhere 48.
Sample size calculation
There was no formal sample size calculation for trajectory modeling analysis. However, Formann estimated that the minimum sample size for latent class analysis is 2k subjects, where k is the number of variables 49. Therefore, we need at least 2k = 28 = 256 subjects in our study, which we satisfy by large. To establish a power of 93% (α = 0.05) in a case–control and a case‐sibling longitudinal study design (standard deviation = 0.15) on cognitive function, at least 1000 patients, 1000 siblings, and 350 controls are needed. In the current study, 1119 patients, 1059 siblings, and 586 healthy controls were participated at baseline, 3 years, and 6 years follow‐up 48.
Assessment of neurocognition
Task selection was based on cognitive domains that have been shown to be altered in schizophrenia 50. The cognitive battery has been described in detail elsewhere 28. This study assessed neurocognitive performance using eight assessment tools. Table 1 shows the list of cognitive domains, their corresponding tests, and outcome measures.
Table 1.
Measures of neurocognition
| Cognitive domains | Group tests | Outcome measure |
|---|---|---|
| Sustained attention and vigilance | Continuous performance test (CPT‐HQ) (CPT performance and CPT variance) | An efficiency score [(accuracy/reaction time) ×1000] was created, in which accuracy was measured as the total number of hits (range 0–28) minus the total number of errors (range 0–28), divided by 28. If this calculation of accuracy was non‐positive (i.e., the number of errors equaled or exceeded the number of hits), then the accuracy was set equal to 0.005. This score was referred to as ‘CPT performance’. Intra‐individual variability in reaction time on the CPT was also evaluated (CPT variance), using the standard deviation score of the subject's mean response time on the hit trials 23, 51. |
| Verbal learning and memory | Word Learning Task (WLT) (Immediate and delayed recall) | Immediate recall (total score of three consecutive trials of 15 words learning) and ‘Delayed recall’ was assessed after 20 min delay |
| Global cognitive functioning | ||
| Processing speed | Digit symbol substitution | Total raw score (0–133) |
| Verbal comprehension | Information | Total raw score (0–28) |
| Working memory | Arithmetic | Total raw score (0–22) |
| Problem‐solving and Visuospatial abilities | Block design | Total raw score (0–68) |
We calculated a composite neurocognitive score based on the following eight neurocognitive measures: CPT performance, CPT variance, immediate recall, delayed recall, digit symbol substitution, information, arithmetic, and block design. Subsequently, linear regression analyses were conducted for each time point. The control subjects score was used to obtain age‐ and gender‐stratified neurocognitive tests z‐score for both patients and siblings. Finally, the composite score for patients and siblings was computed by averaging z‐score of all eight tests.
Assessments of sociodemographic and clinical variables
The sociodemographic variables were age of participants, age of onset of psychosis educational status, gender, and ethnicity. According to Verhage 52, educational status was evaluated as a continuous variable. Psychotic disorder was assessed by the Comprehensive Assessment of Symptoms and History (CASH) 53 or Schedules for Clinical Assessment in Neuropsychiatry (SCAN) questionnaire 54, 55. Level of premorbid functioning was assessed using the Premorbid Adjustment Scale (PAS) 56. Positive and negative symptoms of schizotypy were measured using the Structured Inventory for Schizotypy‐Revised (SIS‐R) 57. The SIS‐R is a reliable and valid semistructured interview for rating schizotypal sign and symptoms administered in unaffected siblings and healthy controls 57. Frequency and distress of psychotic experiences were measured with the Community Assessment of Psychic Experiences (CAPE) questionnaire 58. The CAPE is a 42‐item reliable and valid self‐report questionnaire to assess psychotic‐like experiences in the community and in individuals at an increased risk for developing psychosis (i.e., siblings in our study) and in healthy controls 58. Symptom severity in patients was assessed with the positive and negative syndrome scale (PANSS) 59, 60.
Data analysis and statistical modeling
Descriptive statistics
Patients, siblings, and controls difference in sociodemographic characteristics at baseline were tested using univariate analyses. For gender and ethnicity, Pearson's chi‐squared test was used. Due to the family structure data, linear mixed effects models using family as a random effect were applied to all continuous variables (e.g., sociodemographic, clinical, and cognitive tests) to test for differences between the groups. Maximum likelihood (ML) method was used to estimate the model parameters and Type‐III (overall) tests of fixed effects were used to test for differences between groups. Significant differences were followed by pair‐wise post hoc comparisons between groups. Additionally, Pearson's correlation coefficients between cognitive performances were computed for patients and siblings to explore the possible predictive relationship.
Subtyping and trajectory modeling
Subtyping is the level of overall cognitive functioning across time whereas trajectory is the pattern (e.g., stable, fluctuating, decline, or improvement) of overall cognitive functioning or the specific cognitive domain/test. Group‐based trajectory modeling (GBTM) 61, 62, 63, 64 was conducted to identify clusters of patients and siblings with a similar pattern of neurocognitive function over time. The neurocognitive composite score was used as a dependent variable and follow‐up time (baseline, 3 and 6 years) as an independent variable. First order linear and second order quadratic polynomial models were fitted assuming that individual differences in trajectories could be summarized by a finite set of polynomial functions of time. To determine the number of clusters and the best‐fitting model, a sequential approach was applied where the number of clusters is increased by one. The less complex model (i.e., less trajectory groups) was compared with the complex model (i.e., more groups) using the Bayesian information criterion (BIC) 65 and logged Bayes factor (2*ΔBIC), where ΔBIC = BIC (complex) – BIC (less complex) 66, 67 and where the logged Bayes factor (2*ΔBIC) would indicate trivial (0–2), positive (2–6), strong (6–10) or very strong (>10) evidence for the null hypothesis that the less complex model is the best fit.
First, a single quadratic polynomial trajectory model was examined. If the quadratic term was not significant, the model was repeated with a linear trajectory to determine the BIC value. If the quadratic component in one trajectory model was significant, the quadratic two‐trajectory model was performed. Next, the BIC value of the appropriate two‐trajectory model was compared to the BIC value of the appropriate one‐trajectory model. The process was repeated by increasing the number of trajectories until the best‐fit model was found 68. The trajectory modeling was stopped when the ΔBIC became a negative value. GBTM can handle missing data in the cognition score using ML estimation method to create asymptomatically unbiased parameter estimates under the assumption of data missingness at random 69, 70. We also checked the drop‐out model which includes a logistic model of drop‐out probability per period to interrogate whether the attrition rates significantly affected/biased the cognitive trajectory group membership probabilities 71. For each group, 0 = constant attrition rate, 1 = depends on the previous response (i.e., baseline) and 2 = depends on the two previous responses (i.e., baseline and 3 years).
Comparison among cognitive subtypes
Differences between the subgroups of patients and siblings in all continuous variables were investigated using linear mixed effect models taking familial relationship into account. Type‐III (overall) tests of fixed effects were used to test group differences. If these were significant, pair‐wise comparison was done using Dunnett's method (taking the most normal cognitive profile as a reference group). For gender and ethnicity, the Pearson's chi‐squared test was used to test the difference between subgroups of patients and siblings.
Predicting cognitive subtypes of siblings using subtypes of probands
We considered sibling subtype (multi‐category) as a dependent variable and patient subtype (multi‐category) as an independent variable. The probability of concordance, probability of discordance and Somers’ D statistic 72 were computed on the pairs of subtypes of patients and siblings. A pair of patients‐siblings subtype was reported concordant if the larger value of subtypes of patients was paired with the larger value of subtypes of siblings, and discordant if the larger value of subtypes of patients was paired with the smaller value of subtypes of siblings. Somers’ D of subtypes of siblings, with respect to subtypes of patients, was defined as the difference between the two conditional probabilities of concordance and discordance.
Clustered multinomial logistic regression analysis was conducted taking into account family as a random effect given that siblings and patients belong within the same family. PROC NLMIXED in SAS (Statistical Analysis System) was applied to determine the predictive relationship between subtypes of patients and siblings. An adaptive Gaussian quadrature with ten quadrature points was specified to integrate out the random effect of the likelihood function 73, 74 and to estimate the parameters (i.e., subtypes of patients) and their standard errors. The intra‐cluster correlation coefficient (ICC) was calculated to estimate the familial correlation between pairs of unaffected siblings and probands in the same family. The ICC was calculated as ICCFamily = var(family)/(var(family) + π2/3), where var(family) is the variance of random effect and π is 3.14159. A two‐tailed test at P < 0.05 was considered as statistical significant throughout the analyses. For pair‐wise comparisons, Bonferroni correction for multiple testing was done and statistical significance was determined at P < 0.05/20. All analyses were performed using SAS version 9.4. In this study, GROUP data version 4.00 was used.
Results
Descriptive of the study population
At baseline, patients, siblings, and controls significantly (P < 0.001) differed by sociodemographic, cognitive, and clinical variables. Pair‐wise comparisons revealed that the differences were significant between patients and controls as well as siblings and controls. Patients and siblings cognitive performance was low compared to controls. Additionally, cognitive performances of patients were found to be significantly lower than the performances of their unaffected siblings (Table 2).
Table 2.
Comparison of control, sibling, and patient baseline profiles*
| Variable/Group | Group | Overall group differenceϮ | Pair‐wise group comparison | ||
|---|---|---|---|---|---|
| Controls (n = 586) | Siblings (n = 1059) | Patients (n = 1119) | |||
| Age | 30.42 (10.58) | 27.84 (8.28) | 27.58 (7.94) | F = 22.8, P < 0.001 | Sibs<Ctrs,Pts<Ctrs |
| Age of onset | … | … | 23.69 (7.59) | … | … |
| Gender, male | 45.90 | 45.51 | 76.14 | χ² = 254.1, P < 0.001 | Sibs<Ctrs<Pts |
| Education (Verhage)a | 5.41 (1.78) | 5.07 (2.11) | 4.04 (2.05) | F = 128.5, P < 0.001 | Pts<Sbs<Ctrs |
| Ethnicity, Dutch | 92.12 | 83.24 | 79.22 | χ² = 45.2, P < 0.001 | Pts<Sbs<Ctrs |
| Estimated IQb | 109.75 (15.08) | 102.76 (15.60) | 94.99 (16.12) | F = 185.6, P < 0.001 | Pts<Sbs<Ctrs |
| Overall score PASc | 1.13 (0.59) | 1.13 (0.66) | 1.98 (0.88) | F = 439.0, P < 0.001 | Sbs<Pts, Pts<Ctrs |
| SIS‐Rd | |||||
| Positive | 0.31 (0.35) | 0.38 (0.42) | … | F = 15.4, P < 0.001 | Ctrs<Sbs |
| Negative | 0.24 (0.22) | 0.27 (0.26) | … | F = 9.0, P = 0.002 | Ctrs<Sbs |
| PANSS 5‐factor | |||||
| Positive | … | … | 13.90 (6.55) | … | … |
| Negative | … | … | 15.00 (6.64) | … | … |
| Disorganization | … | … | 16.77 (6.27) | … | … |
| Excitement | … | … | 12.05 (4.05) | … | … |
| Emotional distress | … | … | 15.82 (5.73) | … | … |
| CAPE (Positive dimension)e | |||||
| PE Frequency | 0.19 (0.17) | 0.21 (0.20) | 0.67 (0.49) | F = 566.5, P < 0.001 | Sbs<Pts, Pts<Ctrs |
| PE Distress | 0.43 (0.45) | 0.46 (0.48) | 1.26 (0.69) | F = 531.0, P < 0.001 | Sbs<Pts, Pts<Ctrs |
| Cognitive Performance | |||||
| CPT performancef | 246.36 (54.78) | 243.70 (57.86) | 220.82 (62.14) | F = 52.0, P < 0.001 | Pts<Sbs, Ctrs<Pts |
| CPT variance (ms)g | 72.76 (28.28) | 75.80 (28.44) | 92.99 (36.51) | F = 108.4, P < 0.001 | Sbs<Pts, Pts<Ctrs |
| Block designh | 46.55 (14.16) | 44.87 (15.07) | 40.42 (16.99) | F = 39.2, P < 0.001 | Pts<Sbs<Ctrs |
| Digit symboli | 84.01 (14.58) | 79.21 (15.39) | 65.41 (16.27) | F = 379.9, P < 0.001 | Pts<Sbs<Ctrs |
| Arithmeticj | 15.32 (4.16) | 13.86 (4.43) | 12.27 (4.79) | F = 93.1, P < 0.001 | Pts<Sbs<Ctrs |
| Informationk | 18.84 (4.67) | 16.83 (5.22) | 16.77 (5.47) | F = 31.5, P < 0.001 | Sbs<Ctrs, Pts<Ctrs |
| Immediate recalll | 28.47 (5.37) | 26.89 (5.77) | 22.94 (6.09) | F = 224.5, P < 0.001 | Pts<Sbs<Ctrs |
| Delayed recallm | 9.74 (2.70) | 9.33 (2.64) | 7.53 (2.87) | F = 181.6, P < 0.001 | Pts<Sbs<Ctrs |
*Table presents means (SD) or %; Empty (…) row or column means no measurements in the respective group or variable; aEducation (Verhage): range 0 (no education), 3–5 (school diploma) to 8 (university degree); bIQ: Wechsler Adult Intelligence Scale‐III (WAIS‐III), short form; cPAS: Premorbid Adjustment Scale; dSIS‐R: Structured Inventory for Schizotypy – Revised; eCAPE: Community Assessment for Psychic Experiences; PE frequency and distress: Frequency of positive psychotic experiences and amount of distress of these PE; fCPT performance: Continuous performance test HQ, performance index, gCPT variance (ms): CPT‐HQ variance in reaction time (ms); hBlock design: WAIS‐III Block design; iDigit symbol: WAIS‐III Digit symbol substitution test; jArithmetic: WAIS‐III Arithmetic; kInformation: WAIS‐III Information; lImmediate recall: Word Learning Task (WLT) immediate recall; mDelayed recall: WLT Delayed recall. For the PAS, higher scores reflect poorer premorbid adjustment; Ctrs: Controls; Sibs: Siblings; Pts: Patients; Pair‐wise group comparison explains which group has significantly different values on the measurements; Ϯ P < 0.05/20 was considered as statistically significant.
Correlation between all cognitive tests was significant in patients and siblings except the correlation between CPT performance and block design, arithmetic and information in siblings (Table S1–S2).
Cognitive subtypes and trajectories
A five‐group cognitive trajectory model for patients and four‐group trajectory model for siblings were very strongly favoured for overall cognitive scores (z‐scores) according to the smallest BIC and the logged Bayes factor (Table S3). In patients, the value of logged Bayes factor was 17.34 (>10), thus favouring the five‐cluster model over a six‐cluster model. In siblings, the value of logged Bayes factor was 94.62 (>10), favouring the four‐trajectory model over a five‐cluster model (Table S3). Parameter estimates of linear and quadratic polynomial time functions of trajectory modeling and drop‐out model presented in Tables S4 and S5. The drop‐out of patients and unaffected siblings did not significantly affect/biased their cognitive trajectory group membership probabilities.
Figures 1a and b displays cognitive trajectories of patients and their siblings over 6 years respectively. The cognitive trajectories in patients were labeled as ‘severely altered’, ‘moderately altered’, ‘mildly altered’, ‘normal’, and ‘high performer’. Similarly, the trajectories in siblings were labeled as ‘moderately altered’, ‘mildly altered’, ‘normal’, and ‘high performer’. All initial neurocognitive profiles for patients and siblings were stable over time. Severe and moderate groups were identified based on a broad‐based cognitive alteration of, on average, about 1 SD below the normal cognitive trajectory across a range of cognition composite score. We showed 26.7% of patients had a normal cognitive function, 30.4% mild, 28.4% moderate, and 10.7% severe cognitive alterations. Likewise, 37.6% of siblings showed a normal cognitive functioning, 25.1% mild and 13.0% moderate cognitive alteration. Three point eight percent of patients and 24.2% of siblings had higher cognitive functioning compared with the mean level of the normal cognitive subtype. Patients in this cluster showed a subtle significant decline over time (Fig. 1a), whereas the pattern was stable for siblings (Fig. 1b).
Figure 1.
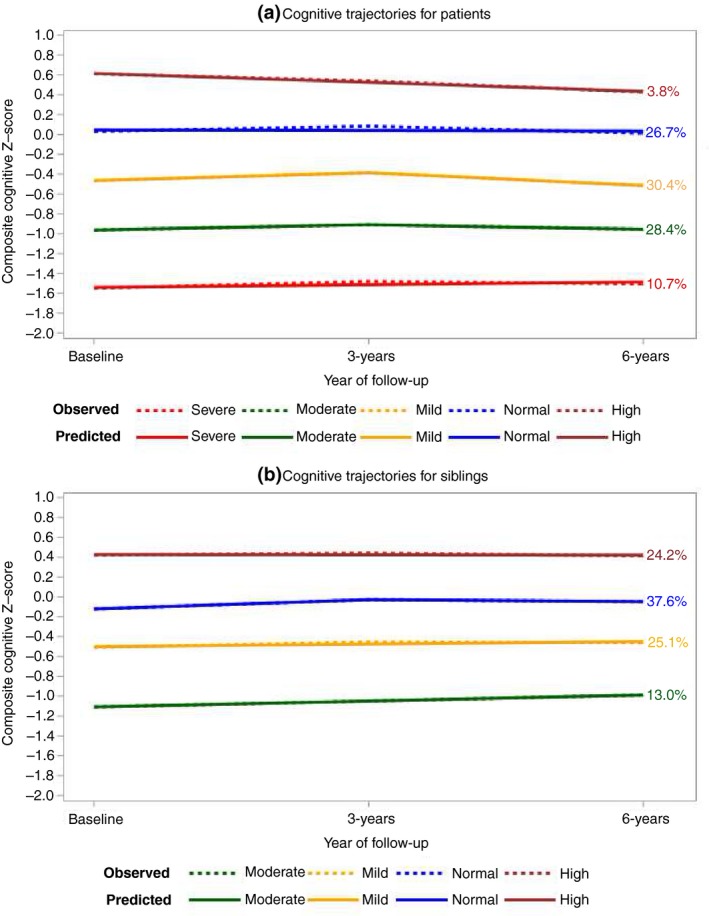
(a) Cognitive trajectories for patients (n = 1119), (b) Cognitive trajectories for siblings (n = 1059). [Colour figure can be viewed at http://www.wileyonlinelibrary.com]
Comparison of cognitive subtypes on all baseline characteristics
Cognitive subtypes of patients were compared based on cognitive measures, demographic characteristics, and clinical variables. Patients with normal cognitive profile differed significantly from other patient subgroups in education, IQ, premorbid functioning, and psychotic symptoms. The detailed pair‐wise comparisons on cognitive subtypes of patients have been shown in Table 3.
Table 3.
Patients cognitive trajectory group profiles (n = 1119)*
| Profiles | Cognitive trajectory group | Overall trajectory group differenceϮ | Pair‐wise comparison** | ||||
|---|---|---|---|---|---|---|---|
| 1. High (n = 31) | 2. Normal (n = 290) | 3. Mild (n = 377) | 4. Moderate (n = 312) | 5. Severe (n = 109) | |||
| Age | 31.4 (8.3) | 27.3 (7.2) | 28.0 (8.0) | 27.3 (8.4) | 26.8 (8.0) | F = 2.5, P = 0.051 | 2 < 1 |
| Age of Onset | 26.2 (8.1) | 23.0 (6.5) | 23.2 (7.9) | 22.9 (7.9) | 23.0 (7.3) | F = 1.4, P = 0.253 | |
| Gender, % male | 74.2 | 77.9 | 74.3 | 77.2 | 75.2 | χ²=1.6, P = 0.816 | |
| Education (Verhage)a | 5.8 (1.9) | 4.9 (1.8) | 4.3 (2.0) | 3.3 (1.9) | 2.6 (1.8) | F = 49.0, P < 0.001 | 2 < 1; 2 > 3,4,5 |
| Ethnicity, % Dutch | 90.3 | 87.2 | 79.9 | 75.1 | 64.5 | χ²=30.6, P < 0.001 | 2 < 1; 2 > 3,4,5 |
| IQ, Estimatedb | 127.8 (10.7) | 110.5 (10.4) | 95.7 (8.6) | 83.3 (7.7) | 72.9 (6.7) | F = 615.6, P < 0.001 | 2 < 1;2 > 3,4,5 |
| PAS, overall scorec | 1.8 (1.0) | 1.8 (0.8) | 1.9 (0.8) | 2.1 (1.0) | 2.3 (0.8) | F = 9.7, P < 0.001 | 2 < 4,5 |
| PANSS 5‐factord | |||||||
| Positive | 14.0 (8.2) | 13.4 (5.9) | 13.1 (5.9) | 15.0 (7.1) | 14.8 (7.7) | F = 4.0, P = 0.003 | 2 < 4 |
| Negative | 15.1 (6.4) | 13.6 (5.9) | 14.3 (6.4) | 16.1 (7.0) | 18.0 (7.1) | F = 11.1, P < 0.001 | 2 < 4,5 |
| Disorganization | 16.0 (6.8) | 14.8 (4.9) | 15.7 (5.6) | 18.3 (6.6) | 21.3 (7.1) | F = 30.5, P < 0.001 | 2 < 4,5 |
| Excitement | 12.8 (5.2) | 11.5 (3.5) | 11.5 (3.7) | 12.7 (4.4) | 13.2 (4.5) | F = 7.0, P = 0.001 | 2 < 4,5 |
| Emotional distress | 16.0 (5.7) | 15.4 (5.4) | 15.2 (5.5) | 16.7 (5.8) | 16.4 (6.8) | F = 3.3, P = 0.024 | 2 < 4 |
| Cognitive performance | |||||||
| CPT performancee | 256.1 (45.7) | 240.9 (52.2) | 225.8 (59.6) | 210.7 (56.5) | 170.0 (78.8) | F = 30.1, P < 0.001 | 2 > 3,4,5 |
| CPT variance (ms)f | 84.2 (35.3) | 83.1 (31.9) | 90.1 (36.0) | 101.8 (37.2) | 106.3 (38.9) | F = 13.4, P < 0.001 | 2 < 4,5 |
| Block designg | 60.4 (8.8) | 53.5 (10.9) | 42.2 (14.3) | 30.7 (13.8) | 20.6 (11.0) | F = 197.6, P < 0.001 | 2 < 1; 2 > 3,4,5 |
| Digit symbolh | 85.2 (14.6) | 76.2 (14.6) | 66.5 (12.5) | 57.8 (12.9) | 47.5 (11.7) | F = 138.7, P < 0.001 | 2 < 1; 2 > 3,4,5 |
| Arithmetici | 18.8 (2.5) | 16.2 (3.2) | 13.0 (3.8) | 9.1 (3.3) | 6.7 (2.7) | F = 264.22, P < 0.001 | 2 < 1; 2 > 3,4,5 |
| Informationj | 24.6 (2.3) | 21.1 (3.4) | 17.4 (4.3) | 13.6 (4.3) | 9.9 (3.5) | F = 243.9, P < 0.001 | 2 < 1; 2 > 3,4,5 |
| Immediate recallk | 32.4 (3.8) | 27.1 (4.7) | 23.4 (4.7) | 19.9 (4.8) | 15.9 (5.0) | F = 173.2, P < 0.001 | 2 < 1; 2 > 3,4,5 |
| Delayed recalll | 12.1 (1.8) | 9.4 (2.4) | 7.6 (2.4) | 6.2 (2.2) | 4.6 (2.0) | F = 142.7, P < 0.001 | 2 < 1 2 > 3,4,5 |
*Table presents mean (SD standard deviation) or %; **Only significantly different trajectory groups are reported based on Dunnett's adjustment. The reference group is normal trajectory group; aEducation (Verhage): range 0 (no education), 3–5 (school diploma) to 8 (university degree); bIQ: Wechsler Adult Intelligence Scale‐III (WAIS‐III), short form; cPAS: Premorbid Adjustment Scale; dPANSS: Positive and negative syndrome scale (higher scores in PAS and PANSS reflect poorer outcomes); eCPT performance: Continuous performance test HQ, performance index, fCPT variance (ms): CPT‐HQ variance in reaction time (ms); gBlock design: WAIS‐III Block design; hDigit symbol: WAIS‐III Digit symbol substitution test; iArithmetic: WAIS‐III Arithmetic; jInformation: WAIS‐III Information; kImmediate recall: Word Learning Task (WLT) immediate recall; lDelayed recall: WLT Delayed recall; Cognitive trajectory: high performance (1) to severely altered (5); Ϯp < 0.05/20 was considered as statistically significant.
Differences between normal cognitive subtype and other subtypes of siblings were statistically significant with regard to age, gender, education, ethnicity, IQ, premorbid functioning, positive symptoms, frequency of psychotic experiences, and all cognitive performances except CPT variance. The detailed pair‐wise comparisons on cognitive subtypes of siblings have been shown in Table 4.
Table 4.
Siblings cognitive trajectory group profiles (n = 1059)*
| Profiles | Cognitive trajectory group | Overall trajectory group differenceϮ | Pair‐wise comparison** | |||
|---|---|---|---|---|---|---|
| 1. High (n = 254) | 2. Normal (n = 413) | 3. Mild (n = 260) | 4. Moderate (n = 132) | |||
| Age | 28.6 (7.7) | 27.9 (8.0) | 27.8 (8.9) | 26.3 (8.9) | F = 5.6, P = 0.001 | 2 < 1 |
| Gender, % male | 55.5 | 43.6 | 41.5 | 40.2 | χ² = 14.1, P = 0.003 | 2 < 1; 2 > 4 |
| Education (Verhage)a | 6.1 (1.8) | 5.3 (2.0) | 4.5 (2.0) | 3.5 (2.1) | F = 62.2, P < 0.001 | 2 < 1; 2 > 3,4 |
| Ethnicity, % Dutch | 87.4 | 85.7 | 79.5 | 74.8 | χ² = 14.1, P = 0.003 | 2 < 1; 2 > 3,4 |
| IQ, Estimatedb | 120.7 (9.9) | 104.9 (9.5) | 92.1 (7.9) | 81.9 (6.7) | F = 684.7, P < 0.001 | 2 < 1; 2 > 3,4 |
| PAS, overall scorec | 0.9 (0.6) | 1.1 (0.7) | 1.2 (0.6) | 1.3 (0.7) | F = 13.6, P < 0.001 | 2 < 4, 2 > 1 |
| SIS‐Rd | ||||||
| Positive | 0.3 (0.4) | 0.4 (0.4) | 0.4 (0.4) | 0.5 (0.5) | F = 4.2, P = 0.006 | 2 < 4 |
| Negative | 0.3 (0.3) | 0.3 (0.2) | 0.3 (0.3) | 0.3 (0.3) | F = 2.5, P = 0.108 | |
| CAPE (Positive dimension)e | ||||||
| PE Frequency | 0.2 (0.2) | 0.2 (0.2) | 0.2 (0.2) | 0.3 (0.3) | F = 4.3, P = 0.006 | 2 < 4 |
| PE Distress | 0.4 (0.4) | 0.5 (0.5) | 0.5 (0.5) | 0.6 (0.5) | F = 2.4, P = 0.074 | |
| Cognitive performance | ||||||
| CPT performancef | 254.9 (58.9) | 245.3 (49.8) | 242.4 (59.7) | 220.9 (68.3) | F = 9.3, P < 0.001 | 2 > 4 |
| CPT variance (ms)g | 70.9 (26.0) | 74.6 (26.7) | 80.0 (30.3) | 80.2 (32.3) | F = 4.8, P = 0.003 | 2 > 1; 2 < 3,4 |
| Block designh | 56.3 (8.4) | 48.2 (12.4) | 37.1 (13.8) | 28.1 (11.9) | F = 208.3, P < 0.001 | 2 < 1;2 > 3,4 |
| Digit symboli | 89.7 (11.9) | 81.4 (13.0) | 72.7 (14.4) | 65.5 (13.8) | F = 121.7, P < 0.001 | 2 < 1;2 > 3,4 |
| Arithmeticj | 17.7 (2.6) | 14.9 (3.2) | 11.5 (3.6) | 8.2 (3.1) | F = 318.5, P < 0.001 | 2 < 1; 2 > 3,4 |
| Informationk | 21.8 (3.5) | 17.5 (4.0) | 14.1 (3.8) | 10.6 (3.6) | F = 299.9, P < 0.001 | 2 < 1; 2 > 3,4 |
| Immediate recalll | 31.4 (4.4) | 27.3 (4.9) | 25.0 (5.0) | 20.7 (4.8) | F = 159.0, P < 0.001 | 2 < 1; 2 > 3,4 |
| Delayed recallm | 11.3 (2.1) | 9.5 (2.4) | 8.5 (2.3) | 6.6 (1.8) | F = 113.2, P < 0.001 | 2 < 1; 2 > 3,4 |
*Table presents mean (standard deviation) or %; **Only significantly different trajectory groups are reported based on Dunnett's adjustment. The reference group is normal trajectory group; aEducation (Verhage): range 0 (no education), 3–5 (school diploma) to 8 (university degree); bIQ: Wechsler Adult Intelligence Scale‐III (WAIS‐III), short form; cPAS: Premorbid Adjustment Scale; dSIS‐R: Structured Inventory for Schizotypy—Revised (higher scores in PAS and SIS‐R reflect poorer outcomes); eCAPE: Community Assessment for Psychic Experiences; PE frequency and distress: Frequency of positive psychotic experiences and amount of distress of these PE; fCPT performance: Continuous performance test HQ, performance index, gCPT variance (ms): CPT‐HQ variance in reaction time (ms); hBlock design: WAIS‐III Block design; iDigit symbol: WAIS‐III Digit symbol substitution test; jArithmetic: WAIS‐III Arithmetic; kInformation: WAIS‐III Information; lImmediate recall: Word Learning Task (WLT) immediate recall; mDelayed recall: WLT Delayed recall; Cognitive trajectory: high performance (1) to moderately altered (4); Ϯ P < 0.05/20 was considered as statistically significant.
Association of cognitive subtypes of patients and siblings
In the sibling‐patient pair analysis, we generated 1070 pairs of affected and unaffected siblings. The number of pairs was more than 1059 because we paired multiple unaffected siblings with their single affected sibling or multiple affected siblings with their single unaffected sibling within a family. The contingency table of the subtypes of patients and siblings is presented in the Table S6. Somers’ D value for the association between cognitive subtypes of patients and subtypes of siblings amongst the 1070 sib‐pairs was 0.29. A positive value of Somers’ D indicates that the siblings have better cognitive scores than their probands.
Since the cell frequency of moderately altered subtype in the sibling coupled with high cognitive performance in the patient was zero (Table S6), we combined the high cognitive performer group of patients with the normal cognitive group. The combined normal and high performer group of patients was considered as the reference group.
Table S7 presents the association between cognitive subtypes of patients and siblings. Overall, cognitive subtypes of patients significantly predicted the siblings’ subtypes. Here, we present a risk of an unaffected sibling to be grouped in any of mildly altered, moderately altered, and severely altered groups given the cognitive trajectory of their corresponding affected sibling. The familial correlation was 0.27 at a significance level of P = 0.003.
We observed that unaffected sibling with a severely and moderately altered patients was at risk of having mild alterations with an odds ratio (OR) of 2.56 (95% CI 1.26–5.18) and 1.83 (95% CI 1.12–2.98) respectively. However, mild cognitive alterations in patients did not predict mild alterations in their unaffected siblings (OR = 0.86, P = 0.54). Compared with siblings of patients with intact cognitive function, siblings were at risk of moderate alteration if their probands cognitive alteration was mild (OR = 2.21, 95% CI 1.05–4.64), moderate (OR = 5.70, 95% CI 2.77–11.70), or severe (OR = 10.07, 95% CI 4.15–24.44). Subsequently, siblings had a low likelihood of having high cognitive performance if patients were severely (OR = 0.26, 95% CI 0.09–0.63) or moderately (OR = 0.39, 95% CI 0.24–0.64) altered and a low likelihood of mild cognitive alteration (OR = 0.37, 95% CI 0.24–0.59) when the probands performance was normal or high. In general, unaffected siblings of patients with severe alteration were likely to develop moderate to mild cognitive alterations.
Discussion
To our knowledge, this is the first large‐scale study to report cognitive trajectories in patients with non‐affective psychosis (probands) and their unaffected siblings. We identified five stable and persistent cognitive trajectories within the proband group: ‘severely altered’, ‘moderately altered’, ‘mildly altered’, ‘normal’, and ‘high performer’. Similarly, we identified four stable and persistent trajectories among unaffected siblings: ‘moderately altered’, ‘mildly altered’, ‘normal’, and ‘high performer’. The normal subgroup differed significantly from the other subgroups in sociodemographic, symptomatic, and cognitive profiles. Furthermore, the cognitive trajectory of probands significantly predicted the cognitive trajectory of siblings, the intraclass correlation (ICC) between pairs of siblings and probands was 0.27.
In this study, the trajectory modeling demonstrated five cognitive subgroups for patients and four cognitive subgroups for siblings, which confirms the presence of distinct subgroups defined by cognitive functioning and provides further support for cognitive heterogeneity within psychosis patients and healthy siblings. Similarly, previous cluster analysis studies have reported two to five distinct subgroups in patients 19, 20, 21, 22, 23 and three subgroups in healthy siblings 23. In agreement with previous studies 75, 76, 77, approximately 69.5% of patients had poor cognitive performance (i.e., severe, moderate, and mild alteration level). On the other hand, 30.5% of patients had an intact cognitive function. This finding is higher than previous studies that reported 19–28% of patients with psychosis found to have an intact cognitive function 20, 78, 79, 80, 81. This discrepancy may be due to the difference in duration of follow‐up, cognitive assessment tools, use of composite score, and level of cognitive function at baseline.
Similar to our earlier cross‐sectional study 23, a total of 38% siblings exhibited a stable lower cognitive performance (i.e., both moderate and mild level) over the 6 years. Siblings in the moderate altered group were more often an ethnic minority, young, less intelligent, and with high psychotic experiences as supported by the previous review 13. In line with the previous study 82, we depicted that patients and siblings with mild to severe cognitive alteration performed at least 1 SD below normal cognition. In accordance with our hypothesis and previous studies report 13, 83, 84, we also found cognitive trajectories in patients and their unaffected siblings were stable over the 6 years follow‐up period. This is different from other previous literature 13, 16, 17, which may be related to the use of a composite score that obliterated the change occurred in individual cognitive domain.
Negative and positive symptoms in patients with moderately and severely altered cognition were significantly higher than in the mildly altered and intact subgroups. This finding was consistent with previous studies and supports the notion that psychotic symptoms have been strongly associated with cognitive alteration 19, 20, 30, 31, 85. In line with previous findings 19, 20, 86, IQ was significantly lower in patients with mild to severe cognitive alteration compared with patients with intact cognitive function.
The positive Somers’ D value from the sib‐pair analysis showed that the proband is more likely to show low cognitive performance than the sibling, which implies the illness itself, medication and motivation may have an impact on cognitive performance. Congruent with our hypothesis, the cognitive subtypes of the patients significantly predicted the cognitive subtypes of siblings within the family. The poorer the cognitive profile of the patient, the better it predicted the profile of a more cognitively altered sibling. Moreover, siblings with a high‐performance profile are less predicted when their probands are severely altered.
We found a familial correlation of 27% for cognitive function, which is high compared with other complex diseases such as depression or bipolar disorder and can be used in clinical practice. Of note, this correlation represents the familial risk (which involves genetic and shared familial environment), as sibling designs do not allow to estimate the extent of the genetic and shared environmental contribution separately. As is evident from the literature, the neurocognitive alteration is heritable and genetically correlated with schizophrenia 42, 87, 88. Indeed, Husted et al. showed that neurocognitive traits are highly heritable in patients with known familial schizophrenia (h 2 = 31–62%) 42.
Using a large patient sample data, we uncovered five cognition trajectories after 10 years, which signifies a high degree of heterogeneity is still evident within non‐affective psychosis patients and warrants further investigation. In line with previous studies 23, 41, 89, we demonstrated that cognitive performance of siblings was between those of patients and controls indicating a parallel between cognitive performance and familial liability. Subtyping cognitive profile of unaffected siblings may also provide insight to identify familial groups with high‐risk for developing psychosis and initiate preventive strategies targeting healthy siblings. Although not investigated in the present study, adding genetic markers may unravel additional cognitive subtypes given that cognitive traits are heritable. Neurocognitive measures have been proposed as one of the reliable endophenotypic markers of liability for schizophrenia, as cognitive deficits are transmitted within families of a patient with schizophrenia 40, 41. Therefore, the subtyping of cognitive trajectories in our study may provide insight for determining possible endophenotypic markers associated with schizophrenia and future genetic analyses. Identifying distinctive cognition subtypes may also be helpful to predict variation in clinical and functional outcomes. In addition, identifying meaningful subtypes lends support to develop group‐based diagnostic criteria for cognitive alteration. Moreover, given that not all patients or siblings develop cognitive alteration (30.5% patients vs. 61.8% siblings), identifying subgroups of individuals is helpful for personalized medicine to provide individualized evidence‐based interventions rather than ‘one‐size‐fits‐all’ approach, such as cognitive remediation therapy, cognitive adaption training, and medication therapy to improve cognitive performance 19. In this study, we proved that about one‐third of siblings cognitive trajectory predicted by patients cognitive trajectory which can be applied in clinical utility on an individual dyad level though further investigation is required on genetic, sociodemographic, and environmental factors that affect cognitive performance. Furthermore, the present study showed that clinical characteristics (i.e., subclinical psychotic experiences in siblings, and psychotic symptoms in patients) and premorbid functioning were poor in moderately to severely altered subgroups, which shades light to understand the pathophysiologic mechanisms of cognitive alteration in schizophrenia.
Cognitive performance of a large number of patients with non‐affective psychosis, their unaffected siblings, and healthy controls was followed for 6 years using a comprehensive neurocognitive battery, which can be useful to ensure the clinical and cognitive validity of trajectories. We included patients and more than one siblings within the same family to investigate the joint cognitive trajectory of patients and siblings. Moreover, the study provided considerable evidence that siblings’ cognitive alteration may be predicted by the different cognitive profiles of their probands. A methodological strength of the current study was that we used drop‐out modeling within the same model as the group‐based trajectory modeling 70 to identify the long‐term cognitive trajectories. Other studies did not take into account the drop‐out modeling of the dependency of cognitive functioning with the function of several time points 75, 83, 84.
Some limitations of this study should also be mentioned. First, even though the drop‐out modeling analysis showed the absence of dependency of cognitive functioning at previous assessments both in patients and unaffected siblings, attrition bias may still be evident. Second, we found that the prediction of the high cognitive performer group of patients on a moderate group of siblings was ambiguous and unstable due to low frequency. Third, strong associations between the patient's cognitive performance and their siblings’ cognitive performance may not be claimed based on the sib‐pair analysis. Fourth, generating cognition composite score instead of using multivariate cognitive tests may have an impact on finding meaningful trajectory. Fifth, this study used eight neurocognitive tests; therefore, including other tests may lead to different trajectories with different predictions. Finally, the effect of cognitive trajectories on clinical and functional outcomes was not investigated.
In conclusion, our findings confirmed that cognitive functioning in patients with psychotic disorder and their unaffected siblings is heterogeneous. We demonstrated that the cognitive performance of unaffected siblings is situated between that of the patients and the healthy controls. We identified five distinct cognitive trajectories in patients and four trajectories in siblings, which remained stable during 6‐year follow‐up. These trajectories are validated by observing the associations with external factors, such as sociodemographic, (subclinical) psychotic experiences, and premorbid functioning. Moreover, patients cognitive subtypes significantly predicted the sibling subtypes highlighting the heritability of cognition. The study also supports neurocognitive trajectories as a valuable endophenotypic marker. This profiling approach warrants further evaluation in future molecular studies as well as in studies predicting functional and clinical outcomes.
Funding
TD is funded by a scholarship from Graduates School of Medical Science, University Medical Center Groningen, The Netherlands. This work was supported by Geestkracht programme of the Dutch Health Research Council (Zon‐Mw) (10‐000‐1001), and matching funds from participating pharmaceutical companies (Lundbeck; AstraZeneca; Eli Lilly and Janssen Cilag) and, universities and mental health care organizations (Amsterdam: Academic Psychiatric Centre of the Academic Medical Center and the mental health institutions: GGZ Ingeest; Arkin, Dijk en Duin; GGZ Rivierduinen; Erasmus Medical Centre and GGZ Noord Holland Noord. Groningen: University Medical Center Groningen and the mental health institutions: Lentis, GGZ Friesland; GGZ Drenthe; Dimence; Mediant; GGNet Warnsveld; Yulius Dordrecht and Parnassia psycho‐medical center The Hague. Maastricht: Maastricht University Medical Centre and the mental health institutions: GGZ Eindhoven en De Kempen; GGZ Breburg; GGZ Oost‐Brabant; Vincent van Gogh voor Geestelijke Gezondheid; Mondriaan; Virenze riagg; Zuyderland GGZ; MET ggz; Universitair Centrum Sint‐Jozef Kortenberg; CAPRI University of Antwerp; PC Ziekeren Sint‐Truiden; PZ Sancta Maria Sint‐Truiden; GGZ Overpelt and OPZ Rekem. Utrecht: University Medical Center Utrecht and the mental health institutions: Altrecht; GGZ Centraal and Delta). The sponsors have no role in designing the study, in the collection, analysis, and interpretation of data, in the writing of the report and in the decision to submit the paper for publication.
Declaration of interests
None.
Supporting information
Table S1. Pearson's correlation coefficients of cognitive tests at baseline for patients (n = 1119).
Table S2. Pearson's correlation coefficients of cognitive tests at baseline for siblings (n = 1059).
Table S3. Bayesian Information Criterion (BIC) and logged Bayes factor (2*ΔBIC) in patients and siblings.
Table S4. Parameter estimates of trajectory model for patients.
Table S5. Parameter estimates of trajectory model for Siblings.
Table S6. Contingency table of subtypes for the pair of patients with their corresponding siblings*.
Table S7. Parameter estimates of subtypes of patients on the subtype of sibling (n = 1070 pairs)*.
Acknowledgement
We are grateful for the generosity of time and effort by the patients, their families, and healthy subjects. Furthermore, we would like to thank all research personnel involved in the GROUP project, in particular: Joyce van Baaren, Erwin Veermans, Ger Driessen, Truda Driesen, Karin Pos, Erna van ‘t Hag, Jessica de Nijs, Wendy Beuken, and Debora Op ‘t Eijnde.
Appendix 1.
Genetic Risk and Outcome of Psychosis (GROUP) investigators are: Agna A. Bartels‐Velthuis (University of Groningen, University Medical Center Groningen, University Center for Psychiatry, Rob Giel Research Center, Groningen, the Netherlands), Nico J. van Beveren (Antes Center for Mental Health Care, Rotterdam, the Netherlands; Erasmus MC, Department of Psychiatry, Rotterdam, the Netherlands; Erasmus MC, Department of Neuroscience, Rotterdam, the Netherlands), Wiepke Cahn (University Medical Center Utrecht, Department of Psychiatry, Brain Centre Rudolf Magnus, Utrecht, the Netherlands), Lieuwe de Haan (Academic Medical Center, University of Amsterdam, Department of Psychiatry, Amsterdam, the Netherlands), Philippe Delespaul (Maastricht University Medical Center, Department of Psychiatry and Psychology, School for Mental Health and Neuroscience, Maastricht, the Netherlands), Carin J. Meijer (Academic Medical Center, University of Amsterdam, Department of Psychiatry, Amsterdam, the Netherlands), Inez Myin‐Germeys (KU Leuven, Department of Neuroscience, Research Group Psychiatry, Center for Contextual Psychiatry, Leuven, Belgium), Rene S. Kahn (University Medical Center Utrecht, Department of Psychiatry, Brain Centre Rudolf Magnus, Utrecht, the Netherlands), Frederike Schirmbeck (Academic Medical Center, University of Amsterdam, Department of Psychiatry, Amsterdam, the Netherlands), Claudia J.P. Simons (Maastricht University Medical Center, Department of Psychiatry and Psychology, School for Mental Health and Neuroscience, Maastricht, the Netherlands; GGzE, Institute for Mental Health Care Eindhoven and De Kempen, Eindhoven, the Netherlands), Therese van Amelsvoort (Maastricht University Medical Center, Department of Psychiatry and Psychology, School for Mental Health and Neuroscience, Maastricht, the Netherlands), Neeltje E. van Haren (University Medical Center Utrecht, Department of Psychiatry, Brain Centre Rudolf Magnus, Utrecht, the Netherlands), Jim van Os (Maastricht University Medical Center, Department of Psychiatry and Psychology, School for Mental Health and Neuroscience, Maastricht, the Netherlands; King's College London, King's Health Partners, Department of Psychosis Studies, Institute of Psychiatry, London, United Kingdom), Ruud van Winkel (Maastricht University Medical Center, Department of Psychiatry and Psychology, School for Mental Health and Neuroscience, Maastricht, the Netherlands; KU Leuven, Department of Neuroscience, Research Group Psychiatry, Center for Contextual Psychiatry, Leuven, Belgium).
Islam MdA, Habtewold TD, van Es FD, Quee PJ, van den Heuvel ER, Alizadeh BZ, Bruggeman R. Long‐term cognitive trajectories and heterogeneity in patients with schizophrenia and their unaffected siblings.
Contributor Information
B. Z. Alizadeh, Email: b.z.alizadeh@umcg.nl.
GROUP Investigators:
Agna A. Bartels‐Velthuis, Nico J. van Beveren, Wiepke Cahn, Lieuwe de Haan, Philippe Delespaul, Carin J. Meijer, Inez Myin‐Germeys, Rene S. Kahn, Frederike Schirmbeck, Claudia J.P. Simons, Therese van Amelsvoort, Neeltje E. van Haren, Jim van Os, and Ruud van Winkel
References
- 1. van Os J, Kenis G, Rutten BP. The environment and schizophrenia. Nature 2010;468:203–212. [DOI] [PubMed] [Google Scholar]
- 2. Palmer BW, Dawes SE, Heaton RK. What do we know about neuropsychological aspects of schizophrenia? Neuropsychol Rev 2009;19:365–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Heinrichs RW, Zakzanis KK. Neurocognitive deficit in schizophrenia: a quantitative review of the evidence. Neuropsychology 1998;12:426–445. [DOI] [PubMed] [Google Scholar]
- 4. Green MF, Kern RS, Braff DL, Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the” right stuff”? Schizophr Bull 2000;26:119–139. [DOI] [PubMed] [Google Scholar]
- 5. Faber G, Smid HG, Van Gool AR et al. Neurocognition and recovery in first episode psychosis. Psychiatry Res 2011;188:1–6. [DOI] [PubMed] [Google Scholar]
- 6. Nuechterlein KH, Ventura J, Subotnik KL, Hayata JN, Medalia A, Bell MD. Developing a cognitive training strategy for first‐episode schizophrenia: integrating bottom‐up and top‐down approaches. Am J Psychiatr Rehabil 2014;17:225–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Harvey PD. What is the evidence for changes in cognition and functioning over the lifespan in patients with schizophrenia? J Clin Psychiatry 2014;75(Suppl 2):34–38. [DOI] [PubMed] [Google Scholar]
- 8. Bora E. Neurodevelopmental origin of cognitive impairment in schizophrenia. Psychol Med 2015;45:1–9. [DOI] [PubMed] [Google Scholar]
- 9. Bowie CR, Harvey PD. Cognitive deficits and functional outcome in schizophrenia. Neuropsychiatr Dis Treat 2006;2:531–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Peuskens J, Demily C, Thibaut F. Treatment of cognitive dysfunction in schizophrenia. Clin Ther 2005;27:S25–S37. [DOI] [PubMed] [Google Scholar]
- 11. Walker AE, Spring JD, Travis MJ. Addressing cognitive deficits in Schizophrenia: toward a neurobiologically informed approach. Biol Psychiatry 2017;81:e1–e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kendler KS, Ohlsson H, Mezuk B, Sundquist JO, Sundquist K. Observed cognitive performance and deviation from familial cognitive aptitude at age 16 years and ages 18 to 20 years and risk for schizophrenia and bipolar illness in a Swedish national sample. JAMA Psychiatry 2016;73:465–471. [DOI] [PubMed] [Google Scholar]
- 13. Shmukler AB, Gurovich IY, Agius M, Zaytseva Y. Long‐term trajectories of cognitive deficits in schizophrenia: a critical overview. Eur Psychiatry 2015;30:1002–1010. [DOI] [PubMed] [Google Scholar]
- 14. Hoff AL, Svetina C, Shields G, Stewart J, DeLisi LE. Ten year longitudinal study of neuropsychological functioning subsequent to a first episode of schizophrenia. Schizophr Res 2005;78:27–34. [DOI] [PubMed] [Google Scholar]
- 15. Sánchez‐Torres A, Moreno‐Izco L, Lorente‐Omeñaca R et al. Individual trajectories of cognitive performance in first episode psychosis: a 2‐year follow‐up study. Eur Arch Psychiatry Clin Neurosci 2017;1–13. 10.1007/s00406-017-0857-z [DOI] [PubMed] [Google Scholar]
- 16. Anda L, Brønnick KS, Johnsen E, Kroken RA, Jørgensen H, Løberg E. The course of neurocognitive changes in acute psychosis: relation to symptomatic improvement. PLoS ONE 2016;11:e0167390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Heilbronner U, Samara M, Leucht S, Falkai P, Schulze TG. The longitudinal course of Schizophrenia across the lifespan: clinical, cognitive, and neurobiological aspects. Harv Rev Psychiatry 2016;24:118–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Strauss JS, Bartko JJ, Carpenter WT Jr. The use of clustering techniques for the classification of psychiatric patients. Br J Psychiatry 1973;122:531–540. [DOI] [PubMed] [Google Scholar]
- 19. Reser MP, Allott KA, Killackey E, Farhall J, Cotton SM. Exploring cognitive heterogeneity in first‐episode psychosis: what cluster analysis can reveal. Psychiatry Res 2015;229:819–827. [DOI] [PubMed] [Google Scholar]
- 20. Uren J, Cotton SM, Killackey E, Saling MM, Allott K. Cognitive clusters in first‐episode psychosis: overlap with healthy controls and relationship to concurrent and prospective symptoms and functioning. Neuropsychology 2017;31:787. [DOI] [PubMed] [Google Scholar]
- 21. Heinrichs RW, Awad AG. Neurocognitive subtypes of chronic schizophrenia. Schizophr Res 1993;9:49–58. [DOI] [PubMed] [Google Scholar]
- 22. Gilbert E, Mérette C, Jomphe V et al. Cluster analysis of cognitive deficits may mark heterogeneity in schizophrenia in terms of outcome and response to treatment. Eur Arch Psychiatry Clin Neurosci 2014;264:333–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Quee PJ, Alizadeh BZ, Aleman A, van den Heuvel E; GROUP Investigators . Cognitive subtypes in non‐affected siblings of schizophrenia patients: characteristics and profile congruency with affected family members. Psychol Med 2014;44:395–405. [DOI] [PubMed] [Google Scholar]
- 24. Petrova N, Dorofeikova M. Cognition in schizophrenia: selective impairment and factors that influence it. Eur Psychiat 2017;41:S193. [Google Scholar]
- 25. Trandafir A, Méary A, Schürhoff F, Leboyer M, Szöke A. Memory tests in first‐degree adult relatives of schizophrenic patients: a meta‐analysis. Schizophr Res 2006;81:217–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Krukow P, Karakuła‐Juchnowicz H, Juchnowicz D, Morylowska‐Topolska J, Flis M, Jonak K. Processing speed is associated with differences in IQ and cognitive profiles between patients with schizophrenia and their healthy siblings. Nord J Psychiatry 2017;71:33–41. [DOI] [PubMed] [Google Scholar]
- 27. Kéri S, Janka Z. Critical evaluation of cognitive dysfunctions as endophenotypes of schizophrenia. Acta Psychiatr Scand 2004;110:83–91. [DOI] [PubMed] [Google Scholar]
- 28. Meijer J, Simons CJ, Quee PJ, Verweij K. Cognitive alterations in patients with non‐affective psychotic disorder and their unaffected siblings and parents. Acta Psychiatr Scand 2012;125:66–76. [DOI] [PubMed] [Google Scholar]
- 29. Sánchez‐Torres AM, Basterra V, Rosa A et al. Lifetime cannabis use and cognition in patients with schizophrenia spectrum disorders and their unaffected siblings. Eur Arch Psychiatry Clin Neurosci 2013;263:643–653. [DOI] [PubMed] [Google Scholar]
- 30. Sahakyan L, Kwapil TR. Positive schizotypy and negative schizotypy are associated with differential patterns of episodic memory impairment. Schizophr Res Cogn 2016;5:35–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Harvey PD, Koren D, Reichenberg A, Bowie CR. Negative symptoms and cognitive deficits: what is the nature of their relationship? Schizophr Bull 2005;32:250–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bora E, Akdede B, Alptekin K. The relationship between cognitive impairment in schizophrenia and metabolic syndrome: a systematic review and meta‐analysis. Psychol Med 2017;47:1030–1040. [DOI] [PubMed] [Google Scholar]
- 33. Wang J, Zhou L, Cui C, Liu Z, Lu J. Gray matter morphological anomalies in the cerebellar vermis in first‐episode schizophrenia patients with cognitive deficits. BMC Psychiatry 2017;17:374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Satogami K, Takahashi S, Yamada S, Ukai S, Shinosaki K. Omega‐3 fatty acids related to cognitive impairment in patients with schizophrenia. Schizophr Res Cogn 2017;9:8–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Alherz F, Alherz M, Almusawi H. NMDAR hypofunction and somatostatin‐expressing GABAergic interneurons and receptors: a newly identified correlation and its effects in schizophrenia. Schizophr Res Cogn 2017;8:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Penadés R, García‐Rizo C, Bioque M et al. The search for new biomarkers for cognition in schizophrenia. Schizophr Res Cogn 2015;2:172–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Athanasiu L, Giddaluru S, Fernandes C et al. A genetic association study of CSMD1 and CSMD2 with cognitive function. Brain Behav Immun 2017;61:209–216. [DOI] [PubMed] [Google Scholar]
- 38. Lencz T, Knowles E, Davies G et al. Molecular genetic evidence for overlap between general cognitive ability and risk for schizophrenia: a report from the Cognitive Genomics consorTium (COGENT). Mol Psychiatry 2014;19:168–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Van Den Bossche MJ, Docx L, Morrens M et al. Less cognitive and neurological deficits in schizophrenia patients carrying risk variant in ZNF804A. Neuropsychobiology 2012;66:158–166. [DOI] [PubMed] [Google Scholar]
- 40. Gur RE, Nimgaonkar VL, Almasy L et al. Neurocognitive endophenotypes in a multiplex multigenerational family study of schizophrenia. Am J Psychiatry 2007;164:813–819. [DOI] [PubMed] [Google Scholar]
- 41. Krabbendam L, Marcelis M, Delespaul P, Jolles J, van Os J. Single or multiple familial cognitive risk factors in schizophrenia? Am J Med Genet 2001;105:183–188. [DOI] [PubMed] [Google Scholar]
- 42. Husted JA, Lim S, Chow EW, Greenwood C, Bassett AS. Heritability of neurocognitive traits in familial schizophrenia. Am J Med Genet B Neuropsychiatr Genet 2009;150:845–853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Snitz BE, MacDonald AW III, Carter CS. Cognitive deficits in unaffected first‐degree relatives of schizophrenia patients: a meta‐analytic review of putative endophenotypes. Schizophr Bull 2005;32:179–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Joyce EM, Roiser JP. Cognitive heterogeneity in schizophrenia. Curr Opin Psychiatry 2007;20:268–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Weinberg D, Lenroot R, Jacomb I et al. Cognitive subtypes of schizophrenia characterized by differential brain volumetric reductions and cognitive decline. JAMA Psychiatry 2016;73:1251–1259. [DOI] [PubMed] [Google Scholar]
- 46. American Psychiatric Association . Diagnostic and statistical manual of mental disorders (DSM‐IV‐TR). 4th ed Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 47. Maxwell ME. Family Interview for Genetic Studies (FIGS): a manual for FIGS; 1992.
- 48. Korver N, Quee PJ, Boos HB, Simons CJ, de Haan L; GROUP investigators . Genetic Risk and Outcome of Psychosis (GROUP), a multi‐site longitudinal cohort study focused on gene‐environment interaction: objectives, sample characteristics, recruitment and assessment methods. Int J Methods Psychiatr Res 2012;21:205–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Formann AK. Die latent‐class‐analyse: Einführung in Theorie und Anwendung [latent class analysis: Introduction to theory and application]. Weinheim, Germany: Beltz; 1984. [Google Scholar]
- 50. Nuechterlein KH, Barch DM, Gold JM, Goldberg TE, Green MF, Heaton RK. Identification of separable cognitive factors in schizophrenia. Schizophr Res 2004;72:29–39. [DOI] [PubMed] [Google Scholar]
- 51. Hilti CC, Hilti LM, Heinemann D, Robbins T, Seifritz E, Cattapan‐Ludewig K. Impaired performance on the Rapid Visual Information Processing task (RVIP) could be an endophenotype of schizophrenia. Psychiatry Res 2010;177:60–64. [DOI] [PubMed] [Google Scholar]
- 52. Verhage F. Intelligentie en leeftijd: Onderzoek bij Nederlanders van twaalf tot zevenenzeventig jaar [Intelligence and age: Research among Dutch people aged twelve to seventy‐seven years]. Assen, Netherlands: Van Gorcum; 1964. [Google Scholar]
- 53. Andreasen NC, Flaum M, Arndt S. The Comprehensive Assessment of Symptoms and History (CASH): an instrument for assessing diagnosis and psychopathology. Arch Gen Psychiatry 1992;49:615–623. [DOI] [PubMed] [Google Scholar]
- 54. Aboraya A, Tien A, Stevenson J, Crosby K. Schedules for Clinical Assessment in Neuropsychiatry (SCAN): introduction to WV's mental health community. W V Med J 1998;94:326–328. [PubMed] [Google Scholar]
- 55. Rijnders CT, Van den Berg J, Hodiamont P et al. Psychometric properties of the schedules for clinical assessment in neuropsychiatry (SCAN‐2.1). Soc Psychiatry Psychiatr Epidemiol 2000;35:348–352. [DOI] [PubMed] [Google Scholar]
- 56. Cannon‐Spoor HE, Potkin SG, Wyatt RJ. Measurement of premorbid adjustment in chronic schizophrenia. Schizophr Bull 1982;8:470–484. [DOI] [PubMed] [Google Scholar]
- 57. Vollema MG, Ormel J. The reliability of the Structured Interview for Schizotypy‐Revised. Schizophr Bull 2000;26:619–629. [DOI] [PubMed] [Google Scholar]
- 58. Brenner K, Schmitz N, Pawliuk N et al. Validation of the English and French versions of the community assessment of psychic experiences (CAPE) with a Montreal community sample. Schizophr Res 2007;95:86–95. [DOI] [PubMed] [Google Scholar]
- 59. Kay SR, Fiszbein A, Opfer LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 1987;13:261–276. [DOI] [PubMed] [Google Scholar]
- 60. Lancon C, Auquier P, Nayt G, Reine G. Stability of the five‐factor structure of the Positive and Negative Syndrome Scale (PANSS). Schizophr Res 2000;42:231–239. [DOI] [PubMed] [Google Scholar]
- 61. Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociol Methods Res 2001;29:374–393. [Google Scholar]
- 62. Nagin DS. Analyzing developmental trajectories: a semiparametric, group‐based approach. Psychol Methods 1999;4:139–157. [DOI] [PubMed] [Google Scholar]
- 63. Nagin DS, Odgers CL. Group‐based trajectory modeling in clinical research. Annu Rev Clin Psychol 2010;6:109–138. [DOI] [PubMed] [Google Scholar]
- 64. Niyonkuru C, Wagner AK, Ozawa H, Amin K, Goyal A, Fabio A. Group‐based trajectory analysis applications for prognostic biomarker model development in severe TBI: a practical example. J Neurotrauma 2013;30:938–945. [DOI] [PubMed] [Google Scholar]
- 65. Schwarz G. Estimating the dimension of a model. Ann Stat 1978;6:461–464. [Google Scholar]
- 66. Wit E, van den Heuvel E. ‘All models are wrong..’: an introduction to model uncertainty. Stat Neerl 2012;66:217–236. [Google Scholar]
- 67. Kass RE, Raftery AE. Bayes factors. J Am Stat Assoc 1995;90:773–795. [Google Scholar]
- 68. Andruff H, Carraro N, Thompson A, Gaudreau P, Louvet B. Latent class growth modelling: a tutorial. Tutor Quant Methods Psychol 2009;5:11–24. [Google Scholar]
- 69. Little RJ, Rubin DB. Statistical analysis with missing data. New York: John Wiley & Sons; 2014. [Google Scholar]
- 70. Nagin DS. Group‐based trajectory modeling: an overview. Ann Nutr Metab 2010;65:205–210. [DOI] [PubMed] [Google Scholar]
- 71. Haviland AM, Jones BL, Nagin DS. Group‐based trajectory modeling extended to account for nonrandom participant attrition. Sociol Meth Res 2011;40:367–390. [Google Scholar]
- 72. Somers RH. A new asymmetric measure of association for ordinal variables. Am Sociol Rev 1962;27:799–811. [Google Scholar]
- 73. Kuss O, McLerran D. A note on the estimation of the multinomial logistic model with correlated responses in SAS. Comput Methods Programs Biomed 2007;87:262–269. [DOI] [PubMed] [Google Scholar]
- 74. De Rooij M, Worku HM. A warning concerning the estimation of multinomial logistic models with correlated responses in SAS. Comput Methods Programs Biomed 2012;107:341–346. [DOI] [PubMed] [Google Scholar]
- 75. Thompson WK, Savla GN, Vahia IV et al. Characterizing trajectories of cognitive functioning in older adults with schizophrenia: does method matter? Schizophr Res 2013;143:90–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Irani F, Kalkstein S, Moberg EA, Moberg PJ. Neuropsychological performance in older patients with schizophrenia: a meta‐analysis of cross‐sectional and longitudinal studies. Schizophr Bull 2010;37:1318–1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Szoke A, Trandafir A, Dupont ME, Meary A, Schurhoff F, Leboyer M. Longitudinal studies of cognition in schizophrenia: meta‐analysis. Br J Psychiatry 2008;192:248–257. [DOI] [PubMed] [Google Scholar]
- 78. Ammari N, Heinrichs RW, Pinnock F, Miles AA, Muharib E, McDermid Vaz S. Preserved, deteriorated, and premorbidly impaired patterns of intellectual ability in schizophrenia. Neuropsychology 2014;28:353. [DOI] [PubMed] [Google Scholar]
- 79. Holthausen EA, Wiersma D, Sitskoorn MM et al. Schizophrenic patients without neuropsychological deficits: subgroup, disease severity or cognitive compensation? Psychiatry Res 2002;112:1–11. [DOI] [PubMed] [Google Scholar]
- 80. Kremen WS, Seidman LJ, Faraone SV, Toomey R, Tsuang MT. The paradox of normal neuropsychological function in schizophrenia. J Abnorm Psychol 2000;109:743. [DOI] [PubMed] [Google Scholar]
- 81. Weickert TW, Goldberg TE, Gold JM, Bigelow LB, Egan MF, Weinberger DR. Cognitive impairments in patients with schizophrenia displaying preserved and compromised intellect. Arch Gen Psychiatry 2000;57:907–913. [DOI] [PubMed] [Google Scholar]
- 82. Lewandowski K, Sperry S, Cohen B, Öngür D. Cognitive variability in psychotic disorders: a cross‐diagnostic cluster analysis. Psychol Med 2014;44:3239–3248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Barder HE, Sundet K, Rund BR et al. Neurocognitive development in first episode psychosis 5 years follow‐up: associations between illness severity and cognitive course. Schizophr Res 2013;149:63–69. [DOI] [PubMed] [Google Scholar]
- 84. Barder HE, Sundet K, Rund BR et al. Ten year neurocognitive trajectories in first‐episode psychosis. Front Hum Neurosci 2013;7:643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Potter AI, Nestor PG. IQ subtypes in schizophrenia: distinct symptom and neuropsychological profiles. J Nerv Ment Dis 2010;198:580–585. [DOI] [PubMed] [Google Scholar]
- 86. Joyce EM, Hutton SB, Mutsatsa SH, Barnes TR. Cognitive heterogeneity in first‐episode schizophrenia. Br J Psychiatry 2005;187:516–522. [DOI] [PubMed] [Google Scholar]
- 87. Brzustowicz LM, Simone J, Mohseni P et al. Linkage disequilibrium mapping of schizophrenia susceptibility to the CAPON region of chromosome 1q22. Am J Hum Genet 2004;74:1057–1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Brzustowicz LM, Hodgkinson KA, Chow EW, Honer WG, Bassett AS. Location of a major susceptibility locus for familial schizophrenia on chromosome 1q21‐q22. Science 2000;288:678–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Braff DL, Freedman R, Schork NJ, Gottesman II. Deconstructing schizophrenia: an overview of the use of endophenotypes in order to understand a complex disorder. Schizophr Bull 2006;33:21–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Pearson's correlation coefficients of cognitive tests at baseline for patients (n = 1119).
Table S2. Pearson's correlation coefficients of cognitive tests at baseline for siblings (n = 1059).
Table S3. Bayesian Information Criterion (BIC) and logged Bayes factor (2*ΔBIC) in patients and siblings.
Table S4. Parameter estimates of trajectory model for patients.
Table S5. Parameter estimates of trajectory model for Siblings.
Table S6. Contingency table of subtypes for the pair of patients with their corresponding siblings*.
Table S7. Parameter estimates of subtypes of patients on the subtype of sibling (n = 1070 pairs)*.


