Abstract
Background
Aura symptoms have been reported in up to 23% of cluster headache patients, but it is not known whether clinical characteristics are different in participants with and without aura.
Methods
Using validated web‐based questionnaires we assessed the presence and characteristics of attack‐related aura and other clinical features in 629 subjects available for analysis from an initial cohort of 756 cluster headache subjects. Participants who screened positive for aura were contacted by telephone for confirmation of the ICHD‐III criteria for aura.
Results
Typical aura symptoms before or during cluster headache attacks were found in 44/629 participants (7.0%) mainly involving visual symptoms (61.4%). Except for lower alcohol consumption and higher prevalence of frontal pain in participants with aura, no differences in clinical characteristics were found compared with participants without aura.
Conclusion
At least 7.0% of the participants with cluster headache in our large cohort reported typical aura symptoms, which most often involved visual symptoms. No major clinical differences were found between participants with and without aura.
Keywords: cluster headache, aura, epidemiology, headache characteristics, LUCA study
INTRODUCTION
Cluster headache is a rare headache disorder typically characterized by attacks of excruciating, unilateral temporal or (peri‐)orbital pain lasting 15–180 minutes and associated with facial autonomic symptoms and/or restlessness.1 Migraine‐like aura symptoms have been reported in up to 23% of cluster headache patients.2, 3, 4, 5 For many clinicians, this seems much higher than to their clinical impression. The auras reported are most often visual and sometimes very short‐lasting. Diagnostic criteria differ between migraine and cluster headache in the International Classification of Headache Disorders‐III (ICHD‐III beta).1 In migraine with and without aura are the major subtypes.1 Aura is not mentioned in the cluster headache criteria. Therefore, for a patient with cluster headache and typical aura, the criteria formulated for “typical aura with headache” seem closest.1
In migraine, attacks with aura are in general associated with a shorter and less severe headache phase.6 This has led to the hypothesis that different mechanisms are involved in migraine with and without aura.6, 7, 8, 9 Here, we set out to investigate whether attacks of cluster headache with and without aura differ with respect to the other clinical characteristics.
MATERIAL AND METHODS
Study Setting and Participants Selection
This explorative cross‐sectional study was conducted as part of the ongoing, nation wide, Leiden University Cluster Headache neuroanalysis program (LUCA).10 There have been earlier reports based on the LUCA program including the results of studies on allodynia.11, 12, 13, 14 In one smaller study, the results of an interview by phone regarding aura symptoms were reported (in Dutch).13 Although the results did not differ substantially with this study, the 2 studies cannot be compared completely as the previous study was smaller and did not use this aura questionnaire.
The LUCA website is heavily promoted throughout the Netherlands through professional contacts and various local lay and medical media to attract as many potential participants as possible. In addition, participants attending the LUMC and other headache clinics are invited as well to participate in the LUCA study.
For the LUCA study, persons of 18 years or older who are living in the Netherlands and who believe they have cluster headache, either confirmed or not by a physician, were invited to fill in a validated, web‐based, screening questionnaire for cluster headache. The questionnaire is based on the ICHD‐II criteria15 and has a diagnostic specificity of 0.89 for cluster headache.10 More details about the validation of this screening methods can be found in the report of Wilbrink et al.10 In the Netherlands, the Dutch General Practitioners Guidelines recommend referral to a neurologist when one is suspecting cluster headache, for diagnosis and start of cluster headache treatment.16 Therefore virtually all participants received a diagnosis by a neurologist. All people who screened positive received a second, more extensive web‐based questionnaire, which is based on the ICHD‐II. As known, all participants fulfilling the ICHD‐II criteria fulfill also to the ICHD‐III beta version for cluster headache.1, 11
For this aura study, subjects diagnosed with cluster headache as described above received an email asking them to fill in an additional validated questionnaire about aura symptoms, which was previously found to have a positive predictive value of 88% and a negative predictive value of 70%.17 The questionnaire contains questions regarding the presence, duration and clinical characteristics of visual, sensory, aphasic, and dysarthric aura symptoms preceding or during cluster headache attacks. In addition, it contains questions about (comorbid) migraine. Those who did not respond to the initial email were reminded twice per email and when still not responding, they were contacted 2 more times (once by regular mail and finally once by telephone). All participants who screened positive for aura like symptoms were contacted by telephone for confirmation of the ICHD‐III criteria for typical aura with headache for their cluster headache attacks, which took about 30 minutes per participant. In addition, they were asked about having migraine (with or without aura) according to the ICHD‐III criteria.
Only participants who had filled in all items and were available for a telephone interview (when screened positive for aura like symptom) were included.
The study was approved by the local medical ethical committee of Leiden University Medical Centre and all participants provided written informed consent.
Statistics
No power analysis was performed for this cross‐sectional study. Comparisons between attack characteristics was made using a Mann Whitney test for ordinal data, a chi‐square test for nominal data, and an independent T test for interval data (2‐tailed). No adjustments were made for multiple comparisons. Analyses were performed using SPSS 20.0 (SPSS Inc., IBM, Armonk, NY, USA). Statistical significance was set at P < .05.
RESULTS
By August 2014, there were 756 subjects with a questionnaire‐based diagnosis of cluster headache in the LUCA database. In 720/756 (95.2%) of these the diagnosis had been separately confirmed by a physician. Six hundred and forty‐one of 756 (84.8%) agreed to also fill in the aura questionnaire.
In the aura questionnaire, 88/641 (13.7%) indicated to have aura like symptoms. To be accurate, we contacted these 88 participants by phone to assess the ICHD‐III beta criteria for typical aura with headache. By means of the telephone interview, typical aura according the ICHD‐III criteria beta was diagnosed in 44/88 participants and no aura in 32/88 (the remaining 12 did not participate in the telephone interview and were defined as unknown). Therefore, a total of 44 participants with cluster headache with aura and 585 participants with cluster headache without typical aura were available for further analysis (Fig. 1).
Figure 1.
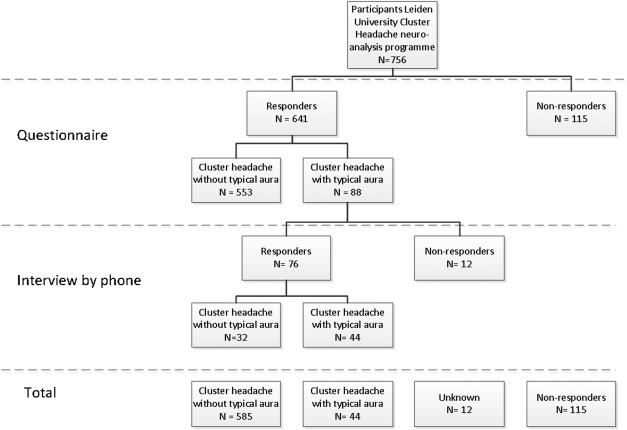
—Flowchart study flow.
Nonresponder analysis revealed no significant differences in baseline characteristics between responders and nonresponders of the questionnaire and if indicated telephone interview (Supporting Information Table S1).
Aura Characteristics in Cluster Headache with Typical Aura
Visual symptoms were most frequently reported to be part of the aura (27/44; 61.4%), followed by sensory symptoms (17/44; 38.6%), dysarthria (12/44; 27.3%), and dysphasia (10/44; 22.7%; Table 1). There was much overlap, but interestingly, isolated dysarthric, aphasic, and sensory symptoms without visual symptoms were also reported.
Table 1.
Typical Aura Symptoms †
| N = 44 | N (%) | Onset, N |
|---|---|---|
| Before – During Attack | ||
| Isolated visual | 14 (31.8) | 10 – 4 |
| Isolated sensory | 5 (11.4) | 1 – 4 |
| Isolated dysphasia | 4 (9.1) | 1 – 3 |
| Isolated dysarthria | 6 (13.6) | 2 – 4 |
| Visual and sensory | 4 (9.1) | 4 – 1 |
| Visual and dysphasia | 1 (2.3) | 1 – 0 |
| Visual and dysarthria | 2 (4.5) | 1 – 1 |
| Sensory and dysphasia | 2 (4.5) | 0 – 2 |
| Visual, sensory, and dysphasia | 2 (4.5) | 2 – 0 |
| Visual, sensory, and dysarthria | 3 (6.8) | 2 – 1 |
| Visual, sensory, dysphasia, and dysarthria | 1 (2.3) | 0 – 1 |
†According to ICHD‐III beta version criteria.
Visual symptoms most often (70.4%) started before the cluster headache attack whereas sensory, dysarthric, and aphasic aura symptoms started most often during the headache phase (Table 1).
The median duration was 15 minutes for dysarthric symptoms, 20 minutes for visual symptoms and 25 minutes for both sensory and aphasic symptoms. Aura symptoms were not present during all cluster headache attacks. In participants with aura symptoms, roughly half of the attacks were accompanied or preceded by visual, sensory, and dysarthric symptoms. Aphasic symptoms were reported in a smaller proportion of attacks (Table 2).
Table 2.
Duration and Frequency of Aura Symptoms During/Before Cluster Headache Attack †
| Visual aura N = 27 | Sensory aura N = 17 | Dysphasia aura N = 10 | Dysarthria N = 12 | |
|---|---|---|---|---|
| Duration aura symptoms (minutes); median (min‐max) | 20 (5–60) | 25 (5–60) | 25 (3–120) | 15 (7–75) |
| Cluster headache attacks with aura (%); median (min‐max) | 50 (5–100) | 50 (1–100) | 20 (1–100) | 65 (15–100) |
†Some participants reported more than one kind of aura as shown in Table 1.
Six out of these 44 participants reported also typical aura symptoms without headache, which occurred strictly with visual aura symptoms and fulfilled to the criteria of “typical aura without headache.” None of these 6 participants reported to also have migraine.
Three case reports to illustrate the reported aura symptoms:
This man suffered from episodic cluster headache since he was 30 years old. He experienced a cluster headache bout every 2 years lasting 6–8 weeks. He had very severe pain right above the left eye together with ipsilateral conjunctival injection, lacrimation, ptosis, and rhinorrhea, with a sense of restlessness and agitation. An attack lasted about 3 hours without intervention and about 30 minutes with the use of oxygen only. About 30 minutes before the cluster headache attacks, he experienced zig‐zag figures in his left eye, which spreads gradually over 10 minutes and then stopped. Twenty minutes later the headache started. He reports these visual symptoms in 10% of his cluster headache attacks.
A 57‐year‐old woman had chronic cluster headache attacks, with about 3 attacks a week since the age of 51. The very severe left orbital attacks lasted about 60 minutes without intervention. They were accompanied with restlessness and agitation and ipsilateral conjunctival injection, lacrimation, ptosis, miosis, and nasal congestion or rhinorrhoea. Before every attack, she saw unilateral (left eye) blurry zig‐zag figures and after several minutes she also developed a heavy and slurred speech. Both symptoms start 5 minutes before the headache and both disappear after about 20 minutes. We have classified this as both a visual and dysarthric aura.
A 58‐year‐old male was diagnosed with episodic cluster headache and he experienced twice a year a bout of 8–10 weeks. The very severe pain is located periorbitally and above the left eye and is accompanied by restlessness and ipsilateral conjunctival injection, lacrimation, ptosis, eyelid edema, miosis, and nasal congestion or rhinorrhea. Without intervention the attacks last between 1.5 and 3 hours. Before about 80% of his attacks he experienced a slurred speech like being drunk for about 15–20 minutes. About 5 minutes after start of the slurred speech the headache starts. We classified this as dysarthria. His partner has noticed this difference in speech as well.
Comparison Between Participants With Typical Aura and No Aura
In each group 2/3 had episodic and 1/3 chronic cluster headache. The 2 groups did not differ in demographic and clinical characteristics except for lower alcohol consumption and higher prevalence of frontal pain in participants with cluster headache with typical aura (Table 3). Comorbid migraine was reported in 13.6% (N = 6) of the participants with typical aura, of whom 2 females (33.3%) and 10.4% (N = 61) of participants without typical aura of whom 34 females (55.7%). Those who experienced aura associated with cluster headache attacks experienced (mainly visual) aura associated with migraine in 4 participants and no aura associated with their migraine in 2 participants.
Table 3.
Characteristics Cluster Headache Participants: With Versus Without Aura
| Cluster headache with aura (N = 44) | Cluster headache without aura (N = 585) | P‐value | |
|---|---|---|---|
| Demographic characteristics | |||
| Age at onset (years) mean ± SD | 30.2 ± 11.9 | 30.3 ± 12.8 | .954 |
| Years of education mean ± SD | 13.0 ± 2.7 | 12.8 ± 3.3 | .631 |
| Male, n (%) | 27 (61.8) | 437 (74.7) | .052 |
| BMI mean ± SD | 25.3 ± 4.6 | 25.4 ± 3.7 | .855 |
| Migraine, n (%) | 6 (13.6) | 61 (10.4) | .506 |
| Drugs use, n (%) | 1 (2.3) | 63 (10.8) | .074 |
| Smoking (pack years) mean ± SD | 15.9 ± 15.1 | 17.9 ± 16.0 | .429 |
| Alcohol (glasses per week) mean ± SD | 4.1 ± 4.9 | 7.2 ± 9.2 | .030 |
| HADS † mean ± SD | 11.7 ± 9.2 | 10.9 ± 7.6 | .551 |
| Episodic cluster headache, n (%) | 29 (65.9) | 453 (77.4) | .096 |
| Cluster headache characteristics | |||
| Severity of attack, n (%) | .500 | ||
| Severe | 44 (100.0) | 579 (99.0) | |
| Moderate | 0 (0.0) | 6 (1.0) | |
| Mild | 0 (0.0) | 0 (0.0) | |
| Location of the pain, n (%) ‡ | |||
| Periorbital | 34 (77.3) | 429 (73.3) | .567 |
| Retro‐orbital | 38 (86.4) | 504 (86.2) | .969 |
| Frontal | 34 (77.3) | 337 (57.6) | .011 |
| Supraorbital | 26 (59.1) | 293 (50.1) | .249 |
| Jaw to temple | 28 (63.6) | 306 (52.3) | .150 |
| Temporal | 34 (77.3) | 476 (81.4) | .504 |
| Nature of headache, n (%) ‡ | |||
| Throbbing | 21 (47.7) | 295 (50.4) | .730 |
| Stabbing | 43 (97.7) | 524 (89.6) | .088 |
| Pressing | 37 (84.1) | 449 (76.8) | .270 |
| Autonomic symptoms | |||
| Lacrimation | 42 (95.5) | 520 (88.9) | .173 |
| Conjunctival injection | 32 (72.7) | 406 (69.4) | .667 |
| Nasal congestion | 35 (79.5) | 411 (70.3) | .191 |
| Rhinorrhea | 30 (68.2) | 425 (72.6) | .523 |
| Ptosis | 32 (72.7) | 361 (61.7) | .149 |
| Miosis | 23 (52.3) | 289 (49.4) | .730 |
| Forehead sweating | 23 (52.3) | 265 (45.3) | .371 |
| Eyelid edema | 20 (45.5) | 213 (36.4) | .231 |
| Restlessness | 35 (79.5) | 483 (82.6) | .595 |
P < .05 (Mann‐Whitney test for ordinal data, independent T‐test for interval data and chi‐square test for nominal data).
†HADS = Hospital Anxiety and Depression Scale.
‡More than one answer was possible.
DISCUSSION
We assessed the presence of aura in 629 participants with cluster headache and compared the clinical attack characteristics of cluster headache participants with typical aura with those without aura. Typical aura was found in 7.0% of participants, which lies within the range of other studies, in which aura prevalence varied from 0 to 23%.2, 13, 18, 19, 20, 21, 22
Consistent with the findings from previous studies,3, 4, 13 the most frequent aura symptoms were visual, which in our study started in most cases prior to the headache. Dysarthria and dysphasia, most often during the headache phase, was reported by 27.3% and 22.7% participants, respectively, which seems much higher than the 4.5%–8% reported in previous studies.2, 4, 5, 13
We and others5 found no significant gender differences between participants with cluster headache with or those without aura. This is in contrast with migraine, as males proportionally have more often migraine with aura than females.6, 23 We found no difference in migraine comorbidity between cluster headache participants with and without typical aura.
In migraine with aura, the headache often lasts shorter and is less severe compared with those without aura.6 We failed to find similar differences in attack characteristics between cluster headache with and without aura, except for more frontal pain and lower alcohol consumption in the former. The finding of a lower alcohol consumption in patients with aura is comparable with the situation in migraine, in which also a lower alcohol consumption was found in patients with aura.24 Whether this implies that attacks with aura are more readily provoked by alcohol than attacks without aura remains a matter of speculation.
In participants with cluster headache with aura, we found a lower proportion of visual aura symptoms compared with aura studies in migraine. In migraine, visual symptom, sometimes combined with other aura symptoms, are reported in up to 99% of the migraine with aura patients.25, 26 A lower proportion of visual symptoms compared to migraine was reported in cluster headache in earlier studies.3, 27 Moreover, those who experienced aura associated with their cluster headache attack, and were known with migraine as well, did not always experience an aura during their migraine attack. Bahra reported that as well: those with aura symptoms associated with their cluster headache did not have aura with their migraine headache in 60% of their cases.3
The strength of this study is the large sample size, a well‐defined cohort, an overall high response rate of 83.2%, and detailed information on cluster headache characteristics. Limitations include the retrospectively collected aura data. The major limitation is that we expect that we have missed patients with aura symptoms by using this questionnaire17 and are uncertain about the amount of missed patients. We may have missed differences in population characteristics. It is a challenge to attempt to answer questions regarding aura via a questionnaire. Our interviews by phone confirmed that diagnosing typical versus atypical aura by only using a questionnaire is insufficient and has a low predictive value. Therefore, we would strongly advise for future researchers to diagnose aura by face‐to‐face or telephone interview (or a sample).
Further research should focus on several questions: (i) whether there are regional differences in aura prevalence related to cluster headache around the world, (ii) whether those with aura respond differently to standard treatment, (iii) if there are pathophysiological differences between those with and without aura, and (iv) whether there is a cortical spreading depression in cluster headache as underlying mechanism of the aura symptoms.
Physicians should be aware that cluster headache seldomly can be preceded or accompanied by aura symptoms. In our opinion, there is no need to add a separate diagnosis of cluster headache with aura to the ICHD‐III criteria or include aura in the list of cluster headache symptoms according to the ICHD‐III criteria. When occurring, typical aura symptoms related to cluster headache can be classified as typical aura with headache as before.1
CONCLUSION
Seldomly, cluster headache can be preceded or accompanied by aura symptoms, most often involving visual symptoms, but remarkably often also speech related symptoms occur. Except for frontal pain and intake of alcohol, no differences were found between participants with and without aura.
STATEMENT OF AUTHORSHIP
Category 1
(a) Conception and Design
I.F. de Coo, L.A. Wilbrink
(b) Acquisition of Data
I.F. de Coo, G.D. Ie
(c) Analysis and Interpretation of Data
I.F. de Coo, L.A. Wilbrink, G.D. Ie, J. Haan, M.D. Ferrari
Category 2
(a) Drafting the Manuscript
I.F. de Coo
(b) Revising it for Intellectual Content
L.A. Wilbrink, G.D. Ie, J. Haan, M.D. Ferrari
Category 3
(a) Final Approval of the Completed Manuscript
I.F. de Coo, L.A. Wilbrink, G.D. Ie, J. Haan, M.D. Ferrari
Supporting information
Supporting Information 1
Conflict of Interest: M.D. Ferrari reports grants and consultancy or industry support from Medtronic, Amgen, Lilly, and Electrocore, and independent support from NWO, ZonMW, NIH, European Community, Dutch Heart Foundation, and Fonds Nuts Ohra (to M.D. Ferrari and L.A. Wilbrink). This study was supported by grants from the Netherlands Organisation for Scientific Research (NWO) and the European Union's Seventh Framework programme (2007–2013) under grant agreement no. 602633 to MDF. I.F. de Coo reports support for conference visits from Electrocore. L.A. Wilbrink and J. Haan report no conflict of interest.
REFERENCES
- 1. Headache Classification Committee of the International Headache Society . The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia. 2013;33:629‐808. [DOI] [PubMed] [Google Scholar]
- 2. Schurks M, Kurth T, de Jesus J, et al. Cluster headache: Clinical presentation, lifestyle features, and medical treatment. Headache. 2006;46:1246‐1254. [DOI] [PubMed] [Google Scholar]
- 3. Bahra A, May A, Goadsby PJ. Cluster headache. A prospective clinical study with diagnostic implications. Neurology. 2002;58:354‐361. [DOI] [PubMed] [Google Scholar]
- 4. Donnet A, Lanteri‐Minet M, Guegan‐Massardier E, et al. Chronic cluster headache: A French clinical descriptive study. J Neurol Neurosurg Psychiatry. 2007;78:1354‐1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rozen TD, Fishman RS. Female cluster headache in the United States of America: What are the gender differences? Results from the United States Cluster Headache Survey. J Neurol Sci. 2012;317:17‐28. [DOI] [PubMed] [Google Scholar]
- 6. Rasmussen BK, Olesen J. Migraine with aura and migraine without aura: An epidemiological study. Cephalalgia. 1992;12:221‐228. [DOI] [PubMed] [Google Scholar]
- 7. Russell MB, Rasmussen BK, Fenger K, et al. Migraine without aura and migraine with aura are distinct clinical entities: A study of four hundred and eighty‐four male and female migraineurs from the general population. Cephalalgia. 1996;16:239‐245. [DOI] [PubMed] [Google Scholar]
- 8. Olesen J, Tfelt‐Hansen P, Henriksen L, et al. The common migraine attack may not be initiated by cerebral ischaemia. Lancet. 1981;2:438‐440. [DOI] [PubMed] [Google Scholar]
- 9. Olesen J, Larsen B, Lauritzen M. Focal hyperemia followed by spreading oligemia and impaired activation of rCBF in classic migraine. Ann Neurol. 1981;9:344‐352. [DOI] [PubMed] [Google Scholar]
- 10. Wilbrink LA, Weller CM, Cheung C, et al. Stepwise web‐based questionnaires for diagnosing cluster headache: LUCA and QATCH. Cephalalgia. 2013;33:924‐931. [DOI] [PubMed] [Google Scholar]
- 11. de Coo IF, Wilbrink LA, Haan J, et al. Evaluation of the new ICHD‐III beta cluster headache criteria. Cephalalgia. 2016;36:547‐551. [DOI] [PubMed] [Google Scholar]
- 12. Louter MA, Wilbrink LA, Haan J, et al. Cluster headache and depression. Neurology. 2016;87:1899‐1906. [DOI] [PubMed] [Google Scholar]
- 13. Wilbrink LA, Cheung C, Weller C, et al. [Aura‐related symptoms associated with cluster headache: Outcomes of a LUCA substudy]. Ned Tijdschr Geneeskd. 2013;157:A5306. [PubMed] [Google Scholar]
- 14. Wilbrink LA, Louter MA, Teernstra OPM, et al. Allodynia in cluster headache. Pain. 2017;158:1113‐1117. [DOI] [PubMed] [Google Scholar]
- 15. Headache Classification Committee of the International Headache Society . The International Classification of Headache Disorders, 2nd edition. Cephalalgia. 2004;24:9‐160. [DOI] [PubMed] [Google Scholar]
- 16. Dekker F, Van Duijn NP, Ongering JEP, et al. NHG‐Standaard Hoofdpijn. Huisarts Wet. 2014;57:20‐31. [Google Scholar]
- 17. van Oosterhout WP, Weller CM, Stam AH, et al. Validation of the web‐based LUMINA questionnaire for recruiting large cohorts of migraineurs. Cephalalgia. 2011;31:1359‐1367. [DOI] [PubMed] [Google Scholar]
- 18. Rozen TD. Cluster headache with aura. Curr Pain Headache Rep. 2011;15:98‐100. [DOI] [PubMed] [Google Scholar]
- 19. Ekbom K, Svensson DA, Traff H, et al. Age at onset and sex ratio in cluster headache: Observations over three decades. Cephalalgia. 2002;22:94‐100. [DOI] [PubMed] [Google Scholar]
- 20. Silberstein SD, Niknam R, Rozen T, et al. Cluster headache with aura. Neurology. 2000;54:219‐221. [DOI] [PubMed] [Google Scholar]
- 21. Dong Z, Di H, Dai W, et al. Clinical profile of cluster headaches in China: A clinic‐based study. J Headache Pain. 2013;14:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ekbom K, Waldenlind E, Tfelt‐Hansen P. Cluster headache and aura. Headache. 2009;49:786‐787. [DOI] [PubMed] [Google Scholar]
- 23. Buse DC, Loder EW, Gorman JA, et al. Sex differences in the prevalence, symptoms, and associated features of migraine, probable migraine and other severe headache: Results of the American Migraine Prevalence and Prevention (AMPP) Study. Headache. 2013;53:1278‐1299. [DOI] [PubMed] [Google Scholar]
- 24. Le H, Tfelt‐Hansen P, Skytthe A, et al. Association between migraine, lifestyle and socioeconomic factors: A population‐based cross‐sectional study. J Headache Pain. 2011;12:157‐172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Viana M, Linde M, Sances G, et al. Migraine aura symptoms: Duration, succession and temporal relationship to headache. Cephalalgia. 2016;36:413‐421. [DOI] [PubMed] [Google Scholar]
- 26. Russell MB, Olesen J. A nosographic analysis of the migraine aura in a general population. Brain. 1996;119: 355‐361. [DOI] [PubMed] [Google Scholar]
- 27. Martinez‐Fernandez EAR, Mir P, Franco E, et al. Cluster headache with aura. J Headache Pain. 2002;3:105‐110. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information 1


