Abstract
Background and purpose
Fatigue is a major consequence of subarachnoid hemorrhage (SAH), but the specific characteristics are unclear. Our objective was to investigate the nature of post‐SAH fatigue (mental or physical) and to determine the relationship with functional outcome in the chronic stage. Also, the possible influence of mood disorders and acute SAH‐related factors [SAH type and external cerebrospinal fluid (CSF) drainage] on the presence of fatigue was investigated.
Methods
Patients with an aneurysmal SAH (aSAH) or angiographically negative SAH (anSAH) were assessed 3–10 years post‐SAH (N = 221). Questionnaires were used to investigate mental and physical fatigue and mood. Functional outcome was examined with the Glasgow Outcome Scale Extended. Between‐group comparisons and binary logistic regression analysis were performed.
Results
Frequencies of mental and physical fatigue were 48.4% and 38.5%, respectively, with prevalence of mental fatigue being significantly higher. A two‐way anova with SAH type and external CSF drainage as independent variables and mental fatigue as dependent variable showed a significant main effect of CSF drainage only (P < 0.001). Only mental fatigue explained a significant part of the variance in long‐term functional outcome (model χ 2 = 52.99, P < 0.001; Nagelkerke R² = 0.32).
Conclusions
Mental fatigue after SAH is a serious burden to the patient and is associated with impaired long‐term functional outcome. Distinguishing different aspects of fatigue is relevant as mental post‐SAH fatigue might be a target for treatment aimed to improve long‐term outcome.
Keywords: functional outcome, mental fatigue, physical fatigue, return to work, subarachnoid hemorrhage
Introduction
Fatigue is one of the major consequences after subarachnoid hemorrhage (SAH) 1, 2; however, relatively little is known about the specific characteristics of post‐SAH fatigue. Moreover, it is unknown whether fatigue is associated with long‐term functional outcome, including return to work (RTW), following SAH.
After SAH, reported frequencies of fatigue vary from 31% to 90% 3, 4, 5, 6, depending on the instrument used, timing post‐SAH and type of SAH 1. Post‐SAH fatigue is often investigated as a unitary construct, despite the fact that fatigue after brain injury is a multidimensional phenomenon, with physical and mental components 7, 8. Physical and mental fatigue are notably different in nature and manifestation, with mental fatigue being most typical for patients with brain injury 9, 10. Mental fatigue is described as a sustained feeling of exhaustion, lack of energy and reduced initiative resulting from performing mentally demanding activities and accompanied by other symptoms such as stress sensitivity and irritability. In contrast, physical fatigue is generally characterized as physically felt exhaustion, with coexisting symptoms such as bodily pain 9, 11, 12. Knowledge about the precise nature and characteristics of post‐SAH fatigue is lacking, but may be paramount as different types of fatigue might require different treatments.
To understand the different aspects of post‐SAH fatigue, it is also important to investigate possible comorbid variables. Anxiety and depression have been associated with post‐SAH fatigue in general 4, 6; however, relationships between mood disorders and mental and physical fatigue separately have not been investigated until now. Furthermore, several acute SAH‐related mechanisms could possibly be associated with long‐term consequences. SAH most often results from rupture of an intracranial aneurysm [aneurysmal SAH (aSAH)], but in around 15% of cases no structural cause for the hemorrhage can be found [angiographically negative SAH (anSAH)]. Generally, anSAH is regarded as a benign pathology, but only one study compared levels of fatigue between aSAH and anSAH patients and found no differences in percentages of overall fatigue 13. Also, external cerebrospinal fluid (CSF) drainage (for acute hydrocephalus and in cases with raised intracranial pressure) is common after SAH and has been related to unfavorable long‐term outcome 14, 15. However, the relation between CSF drainage and fatigue post‐SAH is unknown.
Moreover, the possible relationship between specific aspects of post‐SAH fatigue and functional outcome, including RTW, has barely been investigated. A few studies found associations between fatigue and quality of life 5, 16 and leisure resumption after SAH 17. In other subtypes of stroke, it is well established that fatigue affects RTW 18 and functional independence 19, 20.
The aim of the present study was twofold: first, to investigate whether mental and physical fatigue can be distinguished after SAH and to what extent both types are related to mood disorders and SAH‐related variables; secondly, to investigate the predictive value of mental and physical fatigue for long‐term functional outcome.
Methods
Patients and procedure
Survivors after SAH treated at the University Medical Center Groningen (UMCG) between 2005 and 2012 were eligible for inclusion in the present study. SAH was diagnosed by computed tomography (CT). CT angiography and digital subtraction angiography were performed to determine the presence of a symptomatic intracranial aneurysm (aSAH) or to prove its absence (anSAH). Exclusion criteria were age under 18 years at the time of SAH or severe comorbidity that could interfere with the outcome of the study. Demographical data (age, sex), date of the SAH, clinical condition on admission (World Federation of Neurological Surgeons score) and presence of motor impairment (total or partial loss of a body function) were obtained from patients’ medical reports. In aSAH patients, location of the symptomatic aneurysm as well as treatment (coiling/clipping) were recorded. External CSF drainage (external ventricular or external lumbar drainage) was initiated for suspected increased intracranial pressure based on somnolence and/or the presence of severe headache, with or without enlarged ventricles on CT scan. Persisting CSF resorption disturbances (based on enlarged ventricular system on follow‐up CT scan and clinical signs/symptoms) were treated with ventriculoperitoneal shunting.
All included patients had also participated in one of our two previous cohort studies: a retrospective study of long‐term resumption of daily activities 17 and a prospective study of cognitive functioning post‐SAH 21. Questionnaires on fatigue and mood were sent to all patients between 3 and 10 years post‐SAH followed by a structured telephone interview about functional outcome, including RTW. The study was approved by the Medical Ethical Committee of the UMCG. All participants gave written informed consent and were treated in accordance with the Declaration of Helsinki.
Questionnaires
Fatigue
The Dutch Multifactor Fatigue Scale (DMFS 9) is designed to measure fatigue in the chronic phase after acquired brain injury and consists of 38 items (scoring: 1 totally disagree to 5 totally agree). Higher scores indicate higher levels of fatigue. The DMFS is subdivided into five scales, and the following two subscales were used in this study: (i) Mental‐f, addressing consequences and precursors of mental fatigue (range 7–35); (ii) Physical‐f, addressing consequences and precursors of physical fatigue and physical fitness (range 6–30).
Scores on both subscales were examined in contrast to a norm group of 129 healthy control participants (without neurological conditions, psychiatric disorders, other medical problems influencing fatigue, or chronic fatigue syndrome). Scores above the 89th percentile were considered to be high.
Mood
The Hospital Anxiety and Depression Scale (HADS 22) was used to investigate anxiety (HADS‐A) and depression (HADS‐D), higher scores indicating higher symptom frequency.
Outcome measures
Functional outcome was examined with the Glasgow Outcome Scale Extended (GOSE) 23, 24, and scores were dichotomized into good outcome (7–8) and poor outcome (3–6). RTW was only assessed in patients who were employed or were actively seeking work before the SAH. Questions about work resumption of the GOSE were used, and answers were dichotomized into complete RTW (able to work to previous capacity) and incomplete RTW (reduced work capacity or unable to work).
Statistical analyses
Statistical analyses were conducted using SPSS software (version 23.0, SPSS Inc., Armonk, NY, USA). Z‐tests for difference of proportions were used to investigate if the proportions of mental and physical fatigue were significantly different. Correlations were calculated to examine associations of fatigue with outcome (Spearman) and mood (Pearson), and between the two DMFS subscales (Pearson). Differences in fatigue levels between groups were investigated using independent t tests, Mann–Whitney U tests and two‐way analysis of variance (anova). Effect sizes (Cohen's d) were calculated. Binary logistic regression analysis (Enter method) was performed to determine the influence of Mental‐f, Physical‐f, HADS‐A and HADS‐D on the GOSE scores. Overall alpha level was set at 0.05, with Bonferroni–Holm corrections in the case of multiple comparisons.
Results
Participants
In total, 221 patients were included in this study (Fig. 1). No significant differences were found between the patients who declined to participate and those who responded with respect to age, sex or World Federation of Neurological Surgeons grade.
Figure 1.
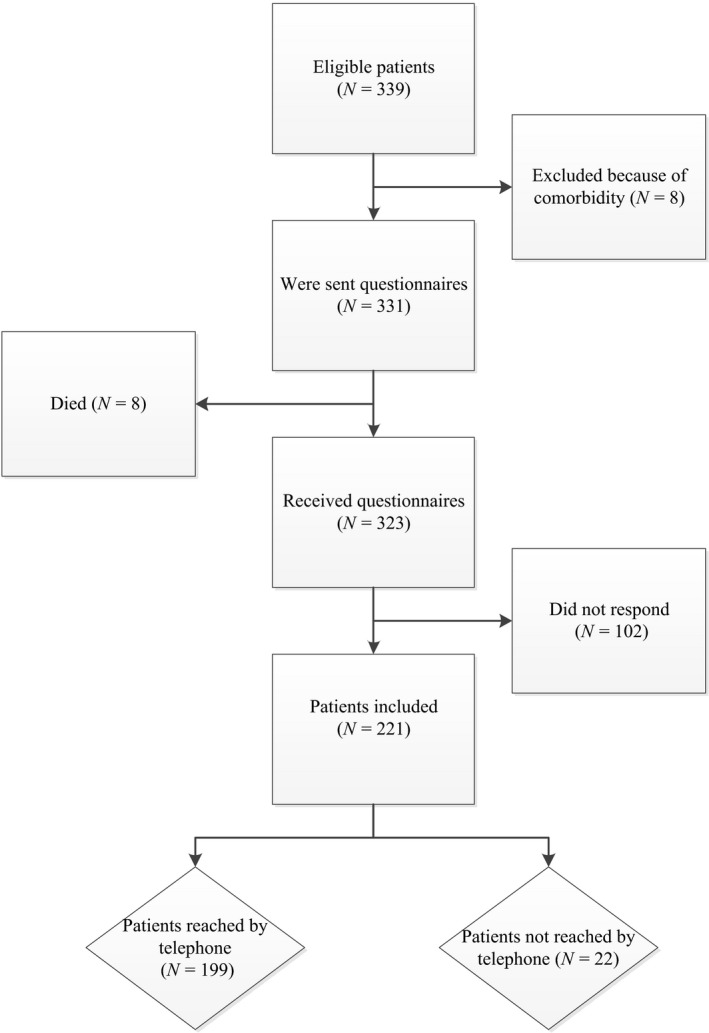
Flow diagram of included and excluded patients.
Table 1 shows the demographic and SAH characteristics of all patients.
Table 1.
Characteristics of included SAH patients
| aSAH (N = 166) | anSAH (N = 55) | |
|---|---|---|
| Number of women | 114 (68.7%) | 23 (41.8%) |
| Age at time of the SAH in years, mean (SD) | 54.0 (10.0) | 55.4 (10.2) |
| Time since SAH in years, mean (range) | 6.8 (3‐10) | 6.9 (3‐10) |
| WFNS | ||
| Low (1–3) | 131 (78.9%) | 50 (90.9%) |
| High (4–5) | 35 (21.1%) | 5 (9.1%) |
| External CSF drainage (ventricular or lumbar) | 84 (50.6%) | 16 (29.1%) |
| VP shunt for chronic hydrocephalus (after external drainage) | 17 (10.2%) | 1 (1.8%) |
| Treatment aSAH | ||
| Clipping | 57 (34.3%) | N/A |
| Coiling | 107 (64.5%) | N/A |
| None | 2 (1.2%) | N/A |
| Aneurysm circulationa | ||
| Anterior | 140 (84.3%) | N/A |
| Posterior | 26 (15.7%) | N/A |
| Motor impairment | ||
| Yes | 4 (2.4%) | 0 (0%) |
| No | 162 (97.6%) | 55 (100%) |
anSAH, angiographically negative subarachnoid hemorrhage; aSAH, aneurysmal subarachnoid hemorrhage; CSF, cerebrospinal fluid; N/A, not applicable; SAH, subarachnoid hemorrhage; VP shunt, ventriculoperitoneal shunt; WFNS, World Federation of Neurological Surgeons. aAnterior: aneurysms of the anterior cerebral or communicating artery, middle cerebral artery, posterior communicating artery, internal carotid artery, ophthalmic artery and anterior choroidal artery. Posterior: aneurysms of the basilar artery, posterior cerebral artery, superior cerebellar artery and vertebral artery.
Characteristics of fatigue and associations with mood
Compared to the norm group, 48.4% of all SAH patients reported high scores on Mental‐f and 38.5% on Physical‐f. The prevalence of mental fatigue was significantly higher than the prevalence of physical fatigue (Z‐statistic for difference of proportions 3, > critical value of 1.96, P < 0.05). The overlap between the presence or absence of mental and physical fatigue was 71.0%. The correlation between Mental‐f and Physical‐f was strong and positive (0.60). Significant and moderate correlations were found: Mental‐f with HADS‐A (0.54) and HADS‐D (0.55) and Physical‐f with HADS‐A (0.47) and HADS‐D (0.58), with all P < 0.05.
Fatigue and SAH‐related variables
Mental‐f scores were significantly higher in patients with aSAH compared to patients with anSAH. Patients with CSF drainage had significantly higher scores on Physical‐f and Mental‐f than patients without drainage. Effect sizes for the significant differences were medium to high. No significant differences were found on the DMFS regarding other SAH‐related variables (Table 2). The results of a two‐way anova with both SAH type and external CSF drainage as independent variables and Mental‐f as dependent variable showed only a significant main effect of external CSF drainage, F(1, 217) = 14.70, P < 0.001. For Physical‐f, no significant main and interaction effects (of either SAH type or CSF drainage) were found.
Table 2.
Scores on DMFS subscales and SAH‐related variables
| Characteristics | N | DMFS subscales | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mental‐f | Physical‐f | ||||||||
| M (SD) | t | P | d | M (SD) | t | P | d | ||
| SAH type | |||||||||
| aSAH | 166 | 22.4 (7.1) | 2.39 | 0.018* | 0.36 | 17.0 (5.8) | 1.50 | 0.14 | 0.24 |
| anSAH | 55 | 19.8 (7.5) | 15.6 (6.0) | ||||||
| WFNS | |||||||||
| Low (1–3) | 181 | 21.3 (7.2) | −2.09 | 0.04 | 0.36 | 16.4 (5.7) | −1.47 | 0.14 | 0.26 |
| High (4–5) | 40 | 23.9 (7.3) | 17.9 (6.3) | ||||||
| External CSF drainage | |||||||||
| Yes | 100 | 24.3 (6.6) | 5.01 | <0.001* | 0.68 | 17.6 (5.9) | 2.34 | 0.02* | 0.32 |
| No | 121 | 19.6 (7.2) | 15.8 (5.7) | ||||||
| VP shunt | |||||||||
| Yes | 18 | 24.0 (6.4) | 1.36 | 0.18 | 0.33 | 18.5 (5.9) | 1.43 | 0.16 | 0.35 |
| No | 203 | 21.6 (7.4) | 16.5 (5.8) | ||||||
| Treatment aSAH | |||||||||
| Clipping | 57 | 21.6 (7.0) | −1.06 | 0.29 | 0.17 | 17.2 (6.1) | 0.46 | 0.65 | 0.07 |
| Coiling | 107 | 22.8 (7.2) | 16.8 (5.7) | ||||||
| Aneurysm circulation aSAHa | |||||||||
| Anterior | 140 | 22.3 (6.9) | −0.54 | 0.59 | 0.11 | 16.8 (5.8) | −0.78 | 0.44 | 0.17 |
| Posterior | 26 | 23.1 (8.1) | 17.8 (5.7) | ||||||
aAnterior: aneurysms of the anterior cerebral or communicating artery, middle cerebral artery, posterior communicating artery, internal carotid artery, ophthalmic artery and anterior choroidal artery. Posterior: aneurysms of the basilar artery, posterior cerebral artery, superior cerebellar artery and vertebral artery. anSAH, angiographically negative subarachnoid hemorrhage; aSAH, aneurysmal subarachnoid hemorrhage; CSF, cerebrospinal fluid; DMFS, Dutch Multifactor Fatigue Scale; Mental‐f, DMFS Mental fatigue; Physical‐f, DMFS Physical fatigue; SAH, subarachnoid hemorrhage; VP shunt, ventriculoperitoneal shunt; WFNS, World Federation of Neurological Surgeons. *Significant differences after Bonferroni–Holm correction.
Fatigue and functional outcome
Poor outcome according to the GOSE (3–6) was found in 42.7% of all patients. RTW was determined in 130 patients, with incomplete RTW in 56.9%. Moderate negative correlations were found between DMFS and GOSE, indicating that higher levels of mental and physical fatigue were related to poor outcome (Table 3). Effect sizes for significant differences of Mental‐f and Physical‐f between patients with poor and good outcome, as well as between complete and incomplete RTW, were large. Two‐way anovas revealed no significant interactions between external CSF drainage and GOSE and RTW on Mental‐f and Physical‐f, all P > 0.05.
Table 3.
Associations between DMFS subscales, GOSE and RTW
| Spearman correlations between DMFS subscales and GOSE | Mean scores on the DMFS subscales M (SD) | Good outcome versus poor outcome | Complete versus incomplete RTW | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GOSE SAH | GOSE aSAH | GOSE anSAH | GOSE good outcome (7–8) N = 114 | GOSE poor outcome (3–6) N = 85 | Complete RTW N = 56 | Incomplete RTW N = 74 | t | P | d | t | P | d | |
| Mental‐f | −0.52* | −0.53* | −0.42* | 18.6 (6.4) | 25.4 (6.4) | 17.8 (5.4) | 24.8 (6 .9) | −7.41 | <0.001* | 1.06 | −6.36 | <0.001* | 1.13 |
| Physical‐f | −0.43* | −0.42* | −0.49* | 14.4 (5.1) | 19.0 (5.7) | 13.6 (4.8) | 18.3 (5.4) | −5.89 | <0.001* | 0.86 | −5.13 | <0.001* | 0.94 |
anSAH, angiographically negative subarachnoid hemorrhage; aSAH, aneurysmal subarachnoid hemorrhage; DMFS, Dutch Multifactor Fatigue Scale; GOSE, Glasgow Outcome Scale Extended; Mental‐f, DMFS Mental fatigue; Physical‐f, DMFS Physical fatigue; RTW, return to work; SAH, subarachnoid hemorrhage. *Significant differences (P < 0.05).
A binary logistic regression analysis with the dichotomized GOSE score as dependent variable showed that outcome could be significantly predicted by a model including Mental‐f, Physical‐f, HADS‐D and HADS‐A (χ² = 52.99, P < 0.001, Nagelkerke R² = 0.32). This model correctly classified 75.8% of patients. Table 4 shows that in this model only Mental‐f was a significant predictor of functional outcome; the odds of a patient with mental fatigue having unfavorable functional outcome were slightly higher than those of a patient without mental fatigue.
Table 4.
Results of binary logistic regression on GOSE
| B (SE) | 95% CI for odds ratio | |||
|---|---|---|---|---|
| Lower | Odds ratio | Upper | ||
| Included | ||||
| Constant | −3.98 (0.72)* | 0.02 | ||
| DMFS Mental‐f | 0.12 (0.03)* | 1.05 | 1.12 | 1.19 |
| DMFS Physical‐f | 0.05 (0.04) | 0.98 | 1.05 | 1.14 |
| HADS‐D | 0.08 (0.06) | 0.97 | 1.08 | 1.21 |
| HADS‐A | −0.01 (0.05) | 0.89 | 0.99 | 1.10 |
CI, confidence interval; DMFS, Dutch Multifactor Fatigue Scale; GOSE, Glasgow Outcome Scale Extended; HADS‐A, Hospital Anxiety and Depression Scale Anxiety; HADS‐D, Hospital Anxiety and Depression Scale Depression; Mental‐f, DMFS Mental fatigue; Physical‐f, DMFS Physical fatigue. *P < 0.05.
Discussion
This is the first study that investigated two major aspects of fatigue separately, namely mental and physical fatigue, and aimed to determine their mutual relationship with functional outcome in the chronic stage post‐SAH. High frequencies of both mental and physical fatigue were found, with significantly more mental fatigue. Moreover, only mental fatigue was significantly related to unfavorable long‐term functional outcome after SAH, compared to physical fatigue and mood problems.
In this study, mental fatigue was identified as an important factor post‐SAH, in line with previous studies defining mental fatigue as most distinctive for brain injury 9, 10. Despite some overlap, our data support a distinction between mental and physical fatigue. Approximately one‐third of all SAH patients was differently affected, either with mental or with physical fatigue. This corroborates the view that post‐SAH fatigue is a multisymptom construct, with mental and physical aspects. In previous studies, post‐SAH fatigue was described as a unitary construct 3, 4, 5, 25, addressed in questionnaires by just one single item or scored on scales designed for a non‐neurological population 1, 26. This has caused a large variation in reported frequencies 1, 2, 6 and has led to an insufficient understanding of post‐SAH fatigue. The current study also revealed that both mental and physical fatigue and mood are related phenomena after SAH. However, mental fatigue and physical fatigue were more prevalent than mood disorders; ergo, a significant proportion of SAH patients with mental or physical fatigue were not depressed or anxious. This is all in line with findings in other subtypes of stroke, in which the theoretical distinction between fatigue on the one side and depression or anxiety on the other side is supported 27. Furthermore, higher levels of mental, not physical, fatigue were found in aSAH patients in the present study. However, the differences in mental fatigue were at least partly explained by a higher rate of external CSF drainage after aSAH. In the literature, external drainage for hydrocephalus has been related to post‐SAH cognitive dysfunction and unfavorable functional outcome 28. Nevertheless, the association between mental and physical fatigue and functional outcome could not be explained by the need for external drainage for suspected increased intracranial pressure [in the case of somnolence, or hydrocephalus on (acute) CT scan] in the present study. In addition, other SAH‐related variables (i.e. treatment method, clinical condition on admission, shunting for persistent CSF resorption disturbances) were not significantly related to mental or physical fatigue.
Our study is the first to demonstrate that both mental and physical fatigue, although separately, are related to unfavorable long‐term functional outcome after SAH. Around 60% of all included SAH patients did not return to work completely after SAH, consistent with previous studies 2, 29. SAH patients with poor functional outcome, including incomplete RTW, experienced significantly more mental and physical fatigue. The finding that only mental fatigue was significantly related to unfavorable functional outcome after SAH, in comparison with physical fatigue and mood disorders, shows the relevance of differentiating between the two types of fatigue. A proper distinction may be very relevant for tailoring counseling of patients and their spouses. Previous studies only reported that greater fatigue was associated with poorer quality of life 16, 30 and impaired leisure resumption 17, but the influence of specific aspects of fatigue on RTW was unclear until now.
One of the limitations of our study is selection bias, due to patients who declined to participate. However, responders and non‐responders did not differ significantly regarding demographic and SAH‐related factors. Therefore, it is believed that our sample is fairly representative. Furthermore, the questionnaire used in our study (DMFS) has not been used before; therefore comparison with previous studies is difficult. However, the DMFS was specifically designed to measure fatigue in the chronic phase after brain injury and has been shown to have good psychometric properties 9. There is growing evidence that the characteristics of fatigue after brain injury are different than in other patient groups, such as patients with chronic fatigue syndrome or cancer 7, 8. Thus, the use of a brain‐injury‐specific scale as a way to measure different aspects of post‐SAH fatigue can even be considered as a strength of the current study. Lastly, compared to previous studies 31, a relatively high percentage of patients were treated with external CSF drainage, possibly related to the indication used in our hospital; all cases with a decreased level of consciousness and suspected increased intracranial pressure, irrespective of a CT scan showing enlarged ventricles or not, received either external ventricular or external lumbar drainage.
In conclusion, high frequencies of both mental and physical fatigue were found up to 10 years after SAH. Both types of fatigue were present, also in the absence of mood problems. Differences in fatigue levels between aSAH and anSAH patients could be explained, at least partly, by the need for early external CSF drainage. Moreover, mental fatigue was most prevalent after SAH and was the best predictor of functional outcome in the chronic stage, compared to physical fatigue and mood disorders. Considering the multidimensional nature of post‐SAH fatigue, mental and physical fatigue should be assessed separately. Moreover, distinguishing different aspects of post‐SAH fatigue plausibly supports clinicians and researchers in improving treatment methods and may improve long‐term functional outcome of SAH patients.
Disclosure of conflicts of interest
The authors declare no financial or other conflicts of interest.
Acknowledgements
This study was supported by the charitable foundation Stichting Catharina Heerdt, with no involvement other than financial support.
References
- 1. Kutlubaev MA, Barugh AJ, Mead GE. Fatigue after subarachnoid haemorrhage: a systematic review. J Psychosom Res 2012; 72: 305–310. [DOI] [PubMed] [Google Scholar]
- 2. Al‐Khindi T, Macdonald RL, Schweizer TA. Cognitive and functional outcome after aneurysmal subarachnoid hemorrhage. Stroke 2010; 41: e519–e536. [DOI] [PubMed] [Google Scholar]
- 3. Eskesen V, Sorensen EB, Rosenorn J, Schmidt K. The prognosis in subarachnoid hemorrhage of unknown etiology. J Neurosurg 1984; 61: 1029–1031. [DOI] [PubMed] [Google Scholar]
- 4. Passier PE, Post MW, van Zandvoort MJ, Rinkel GJ, Lindeman E, Visser‐Meily JM. Predicting fatigue 1 year after aneurysmal subarachnoid hemorrhage. J Neurol 2011; 258: 1091–1097. [DOI] [PubMed] [Google Scholar]
- 5. Powell J, Kitchen N, Heslin J, Greenwood R. Psychosocial outcomes at 18 months after good neurological recovery from aneurysmal subarachnoid haemorrhage. J Neurol Neurosurg Psychiatry 2004; 75: 1119–1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Boerboom W, van Zandvoort MJ, van Kooten F, Khajeh L, Visser‐Meily JM, Ribbers GM, et al Long‐term fatigue after perimesencephalic subarachnoid haemorrhage in relation to cognitive functioning, mood and comorbidity. Disabil Rehabil 2017; 39: 928–933. [DOI] [PubMed] [Google Scholar]
- 7. Kluger BM, Krupp LB, Enoka RM. Fatigue and fatigability in neurologic illnesses: proposal for a unified taxonomy. Neurology 2013; 80: 409–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kutlubaev MA, Duncan FH, Mead GE. Biological correlates of post‐stroke fatigue: a systematic review. Acta Neurol Scand 2012; 125: 219–227. [DOI] [PubMed] [Google Scholar]
- 9. Visser‐Keizer AC, Hogenkamp A, Westerhof‐Evers HJ, Egberink IJ, Spikman JM. Dutch multifactor fatigue scale: a new scale to measure the different aspects of fatigue after acquired brain injury. Arch Phys Med Rehabil 2015; 96: 1056–1063. [DOI] [PubMed] [Google Scholar]
- 10. Palm S, Ronnback L, Johansson B. Long‐term mental fatigue after traumatic brain injury and impact on employment status. J Rehabil Med 2017; 49: 228–233. [DOI] [PubMed] [Google Scholar]
- 11. Chaudhuri A, Behan PO. Fatigue in neurological disorders. Lancet 2004; 363: 978–988. [DOI] [PubMed] [Google Scholar]
- 12. Staub F, Bogousslavsky J. Fatigue after stroke: a major but neglected issue. Cerebrovasc Dis 2001; 12: 75–81. [DOI] [PubMed] [Google Scholar]
- 13. Boerboom W, Heijenbrok‐Kal MH, Khajeh L, van Kooten F, Ribbers GM. Differences in cognitive and emotional outcomes between patients with perimesencephalic and aneurysmal subarachnoid haemorrhage. J Rehabil Med 2014; 46: 28–32. [DOI] [PubMed] [Google Scholar]
- 14. Degos V, Gourraud PA, Tursis VT, Whelan R, Colonne C, Korinek AM, et al Elderly age as a prognostic marker of 1‐year poor outcome for subarachnoid hemorrhage patients through its interaction with admission hydrocephalus. Anesthesiology 2012; 117: 1289–1299. [DOI] [PubMed] [Google Scholar]
- 15. Dupont S, Rabinstein AA. Extent of acute hydrocephalus after subarachnoid hemorrhage as a risk factor for poor functional outcome. Neurol Res 2013; 35: 107–110. [DOI] [PubMed] [Google Scholar]
- 16. Visser‐Meily JM, Rhebergen ML, Rinkel GJ, van Zandvoort MJ, Post MW. Long‐term health‐related quality of life after aneurysmal subarachnoid hemorrhage: relationship with psychological symptoms and personality characteristics. Stroke 2009; 40: 1526–1529. [DOI] [PubMed] [Google Scholar]
- 17. Buunk AM, Groen RJ, Veenstra WS, Spikman JM. Leisure and social participation in patients 4–10 years after aneurysmal subarachnoid haemorrhage. Brain Inj 2015; 29: 1589–1596. [DOI] [PubMed] [Google Scholar]
- 18. Andersen G, Christensen D, Kirkevold M, Johnsen SP. Post‐stroke fatigue and return to work: a 2‐year follow‐up. Acta Neurol Scand 2012; 125: 248–253. [DOI] [PubMed] [Google Scholar]
- 19. Glader EL, Stegmayr B, Asplund K. Poststroke fatigue: a 2‐year follow‐up study of stroke patients in Sweden. Stroke 2002; 33: 1327–1333. [DOI] [PubMed] [Google Scholar]
- 20. van de Port IG, Kwakkel G, Schepers VP, Heinemans CT, Lindeman E. Is fatigue an independent factor associated with activities of daily living, instrumental activities of daily living and health‐related quality of life in chronic stroke? Cerebrovasc Dis 2007; 23: 40–45. [DOI] [PubMed] [Google Scholar]
- 21. Buunk AM, Groen RJ, Veenstra WS, Metzemaekers JD, van der Hoeven JH, van Dijk JM, et al Cognitive deficits after aneurysmal and angiographically negative subarachnoid hemorrhage: memory, attention, executive functioning, and emotion recognition. Neuropsychology 2016; 30: 961–969. [DOI] [PubMed] [Google Scholar]
- 22. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983; 67: 361–370. [DOI] [PubMed] [Google Scholar]
- 23. Teasdale GM, Pettigrew LE, Wilson JT, Murray G, Jennett B. Analyzing outcome of treatment of severe head injury: a review and update on advancing the use of the Glasgow Outcome Scale. J Neurotrauma 1998; 15: 587–597. [DOI] [PubMed] [Google Scholar]
- 24. Wilson JT, Pettigrew LE, Teasdale GM. Structured interviews for the Glasgow Outcome Scale and the extended Glasgow Outcome Scale: guidelines for their use. J Neurotrauma 1998; 15: 573–585. [DOI] [PubMed] [Google Scholar]
- 25. Khajeh L, Ribbers GM, Heijenbrok‐Kal MH, Blijdorp K, Dippel DWJ, Sneekes EM, et al The effect of hypopituitarism on fatigue after subarachnoid hemorrhage. Eur J Neurol 2016; 23: 1269–1274. [DOI] [PubMed] [Google Scholar]
- 26. Ogden JA, Utley T, Mee EW. Neurological and psychosocial outcome 4 to 7 years after subarachnoid hemorrhage. Neurosurgery 1997; 41: 25–34. [DOI] [PubMed] [Google Scholar]
- 27. Hinkle JL, Becker KJ, Kim JS, Choi‐Kwon S, Saban KL, McNair N, et al Poststroke fatigue: emerging evidence and approaches to management: a Scientific Statement for Healthcare Professionals from the American Heart Association. Stroke 2017; 48: e159–e170. [DOI] [PubMed] [Google Scholar]
- 28. Hutter BO, Gilsbach JM. Short‐ and long‐term neurobehavioral effects of lumbar puncture and shunting in patients with malabsorptive hydrocephalus after subarachnoid haemorrhage: an explorative case study. J Clin Neurosci 2017; 36: 88–93. [DOI] [PubMed] [Google Scholar]
- 29. Hop JW, Rinkel GJ, Algra A, van Gijn J. Changes in functional outcome and quality of life in patients and caregivers after aneurysmal subarachnoid hemorrhage. J Neurosurg 2001; 95: 957–963. [DOI] [PubMed] [Google Scholar]
- 30. Fertl E, Killer M, Eder H, Linzmayer L, Richling B, Auff E. Long‐term functional effects of aneurysmal subarachnoid haemorrhage with special emphasis on the patient's view. Acta Neurochir (Wien) 1999; 141: 571–577. [DOI] [PubMed] [Google Scholar]
- 31. Germanwala AV, Huang J, Tamargo RJ. Hydrocephalus after aneurysmal subarachnoid hemorrhage. Neurosurg Clin N Am 2010; 21: 263–270. [DOI] [PubMed] [Google Scholar]


