Abstract
Objectives
High crown‐to‐implant ratios may lead to complications due to unfavorable occlusal forces, including nonaxial forces, on the bone surrounding the neck of the implant and within the connection of the crown and implant itself. The aim of this study was to perform a systematic review on the influence of crown‐to‐implant ratio of single‐tooth, nonsplinted, implants on biological and technical complications.
Materials and Methods
MEDLINE (1950–January 2018), EMBASE (1966–January 2018), and Cochrane Central Register of Controlled Trials database (1800–January 2018) were searched to identify eligible studies. Inclusion criteria were as follows: crown‐to‐implant ratio of single‐tooth, nonsplinted, implant‐supported restorations in the posterior maxilla or mandible and follow‐up of at least 1 year. Main outcome measures were as follows: implant survival rate, marginal bone level changes, biological complications, and technical complications. Two reviewers independently assessed the articles. A meta‐analysis was carried out for implant survival rate and peri‐implant bone changes.
Results
Of 154 primarily selected articles, eight studies fulfilled the inclusion criteria. Study groups presented a mean crown‐to‐implant ratio varying from 0.86 (with 10‐mm implants) to 2.14 (with 6‐mm implants). The meta‐analysis showed an implant survival of more than 99% per year and mean peri‐implant bone changes of <0.1 mm per year. Limited biological and technical complications were reported.
Conclusion
Data reviewed in the current manuscript on crown‐to‐implant ratio, ranging from 0.86 to 2.14, of single‐tooth, nonsplinted, implants did not demonstrate a high occurrence of biological or technical complications.
Keywords: biological complications, crown‐to‐implant ratio, dental implants, technical complications
1. INTRODUCTION
High crown‐to‐implant ratios may lead to biological and technical complications due to unfavorable occlusal forces, including nonaxial forces, on the bone surrounding the neck of the implant and within the connection of the crown and implant itself (Lai et al., 2013; Malchiodi, Cucchi, Ghensi, Consonni, & Nocini, 2014). Systematic reviews of Blanes (2009), Quaranta, Piemontese, Rappelli, Sammartino, and Procaccini (2014), and Esfahrood, Ahmadi, Karami, and Asghari (2017) revealed that high crown‐to‐implant ratios did not have an impact on peri‐implant bone loss; however, Garaicoa‐Pazmiño et al. (2014) reported as a result of their systematic review that the higher the crown‐to‐implant ratio the less the peri‐implant bone loss. In the systematic review of Blanes (2009), it was mentioned that there was no association between crown‐to‐implant ratio and technical complications, but, contrary, Quaranta et al. (2014) reported that high crown‐to‐implant ratios could lead to technical failures. All authors of these systematic reviews stated, however, that the included studies were reporting on various restoration designs, with no distinction between splinted and nonsplinted crowns, making interpretation and solid conclusions difficult. Moreover, short implants (≤8 mm) were not very well represented in their studies, making that high crown‐to‐implant ratios were hardly accounted for. In a prospective cohort study, however, Malchiodi et al. (2014) reported a significant correlation between implant success rate and crown‐to‐implant ratio and between peri‐implant bone loss and crown‐to‐implant ratio. They stated that the critical threshold value of crown‐to‐implant ratio for avoiding biological complications was 3.40. These ratios were found in clinical situations with very short implants. However, also in this study, no distinction was made between splinted and nonsplinted crowns. Nonsplinted crowns are a prerequisite to determine a possible effect of high crown‐to‐implant ratios. An overview is missing on the influence of crown‐to‐implant ratios of single‐tooth implants on biological and technical complications to determine at what magnitude there is a possible negative effect.
Frequently, the crown‐to‐implant ratio increases not only for the greater interocclusal space but also for the reduced vertical dimension of the available bone and subsequent need for a short implant. Short endosseous implants from different implant brands have been reported in several reviews with high survival rates, as well in the maxilla as in the mandible (Annibali et al., 2012; Atieh, Zadeh, Stanford, & Cooper, 2012; Esfahrood et al., 2017; Fan, Li, Deng, Wu, & Zhang, 2017; Gonçalves et al., 2015; Kotsovilis, Fourmousis, Karoussis, & Bamia, 2009; Lemos, Ferro‐Alves, Okamoto, Mendonça, & Pellizzer, 2016; Mezzomo, Miller, Trichet, Alonso, & Shinkai, 2014; Monje et al., 2013; Nisand, Picard, & Rocchietta, 2015; Pommer et al., 2011; Renouard, & Nisand, 2006; Srinivasan et al., 2014; Sun, Huang, Wu, & Shi, 2011; Telleman et al., 2011; Thoma, Cha, & Jung, 2017; Thoma, Zeltner, Hüsler, Hämmerle, & Jung, 2015). In the past years, implant lengths have continuously decreased. This shift was possible by the development of more favorable implant surfaces and supported by reporting successful studies on short implants. Implants of <10 mm in length have been considered as short implants (Pommer et al., 2011; Telleman et al., 2011). However, short implants have also been defined as equal or <8 mm in length (Renouard, & Nisand, 2006). Promising results have been recently showed in systematic reviews looking only at implants 6 mm or less in length (Srinivasan et al., 2014). Inserting short implants can avoid the need of bone augmentation in the resorbed posterior region (Guljé, Raghoebar, Vissink, & Meijer, 2014), but may lead consequently to high crown‐to‐implant ratios (Blanes, Bernard, Blanes, & Belser, 2007).
The aim of this study was to perform a systematic review on the influence of crown‐to‐implant ratio of single‐tooth, nonsplinted, implants on biological and technical complications.
2. MATERIALS AND METHODS
A PICO question was developed as follows: Population included study groups with single‐tooth implant restorations, the Intervention was restoration with reported high crown‐to‐implant ratio, Control would be similar restorations with a normal ratio, Outcome looked at biological and technical complications.
2.1. Information sources and search strategy
A thorough search of the literature was conducted with help of a biomedical specialist and was completed on January 1, 2018. The primary database used was MEDLINE (via PubMed). Additional databases used were EMBASE and The Cochrane Central Register of Controlled Trials. The search was supplemented by hand‐searching (checking references of the relevant review articles and eligible studies for additional useful publications). The search strategy was a combination of MesH terms and free text words. The strategy is depicted in Table 1.
Table 1.
Search strategy
| Implant | “Dental Implants, Single‐Tooth”[Mesh] OR “Dental Implantation”[Mesh] OR “Dental Implants”[Mesh] OR Implant[all fields] |
| Crown | (Tooth[all fields] AND Crown[all fields]) OR “tooth crown”[all fields] OR crown[all fields] OR “Crowns”[Mesh] OR crowns[all fields] |
| Ratio | Ratio[tiab] |
| Outcome | “Alveolar Bone Loss”[Mesh] OR “Dental Prosthesis Design”[Mesh] OR “Treatment Outcome”[MeSH Terms] OR “Bone loss”[tiab] OR “marginal” OR peri‐implant* |
| Limitation | “Humans”[MeSH Terms] AND English[lang] |
2.2. Eligibility criteria
The studies had to meet the following requirements:
detailed information is reported with respect to crown‐to‐implant ratio of single‐tooth implant‐supported restorations in the posterior maxilla or mandible; in case of combined data for single‐tooth restorations and splinted restorations, extraction of data for the single‐tooth restoration must be eligible;
retrospective or prospective studies (cohort studies, comparative studies, randomized controlled studies);
the follow‐up period should be at least 1 year;
outcome measures should at least include implant survival and marginal bone level changes;
publications must be reporting in the English peer‐reviewed dental literature.
2.3. Outcome measures
The following outcome measures were assessed:
type of crown‐to‐implant ratio (anatomical or clinical);
crown‐to‐implant ratio;
survival rate of implants during function;
marginal bone level changes;
survival rate of restorations;
screw fracture;
screw loosening;
abutment fracture;
restoration fracture (including chipping);
restoration loosening (of cemented restoration).
2.4. Validity assessment and data extraction
Initial screening of the abstracts was performed by one reviewer (H.J.A.M.), based on the criteria above. Full‐text documents were obtained for all articles meeting the inclusion criteria. Full‐text analysis was performed by two reviewers (H.J.A.M., G.C.B.) independently.
Agreement was reached by a consensus discussion and if necessary, a third reviewer (G.M.R.) was consulted. Methodological quality was assessed using a quality appraisal tool for case series studies, which was developed by Moga, Guo, Schopflocher, and Harstall (2012) and validated by Guo, Moga, Harstall, and Schopflocher (2016). This systematic review and meta‐analysis was performed in compliance with the PRISMA guidelines.
2.5. Statistical analysis
Data from all studies investigating the loss of bone and loss rate of single‐tooth, nonsplinted, implants with different crown‐to‐implant ratio were pooled and analyzed using the software Comprehensive Meta‐Analysis, Version 3 (CMA; Biostat, Englewood, NJ, USA). A random‐effects model was used to calculate the weighted means and corresponding 95% confidence intervals (CI) as well as weighted event rates among the studies. Statistical heterogeneity among studies was assessed with I 2. To analyze sources of heterogeneity between studies, a meta‐regression analysis (random‐effects model) was performed with crown‐to‐implant ratio (Comprehensive Meta‐Analysis, Version 3).
3. RESULTS
The results of the primary search for the period till January 1, 2018, were 99 hits for the MEDLINE search, 44 hits for the EMBASE search, and nine hits for the Cochrane search (Figure 1). Using this strategy, 152 papers were initially identified, of which 34 articles appeared to be double. Reference checking of relevant reviews (hand search) revealed two additional articles that met the criteria. After removing duplicates 120 papers remained. After scanning of titles and abstracts, a further 79 papers were excluded because they did not meet the inclusion criteria. This approach resulted in 41 papers to be evaluated by full‐text analysis. Two articles were describing the same study group but with different evaluation periods; the article with the shortest follow‐up was excluded. Two articles were excluded because the full manuscript appeared to be written in the Chinese language. One article was excluded because this article did not describe a clinical trial with humans. And finally, 29 articles were excluded because there was no information on crown‐to‐implant ratio of nonsplinted implant‐supported single‐tooth restorations or detailed information could not be extracted. A total of eight articles fulfilled the inclusion criteria. Quality assessment, using the quality appraisal tool for case series studies, was carried out by a single, masked examiner (H.J.A.M.). All eight selected articles were rated as having an acceptable level of evidence of crown‐to‐implant ratio influence.
Figure 1.
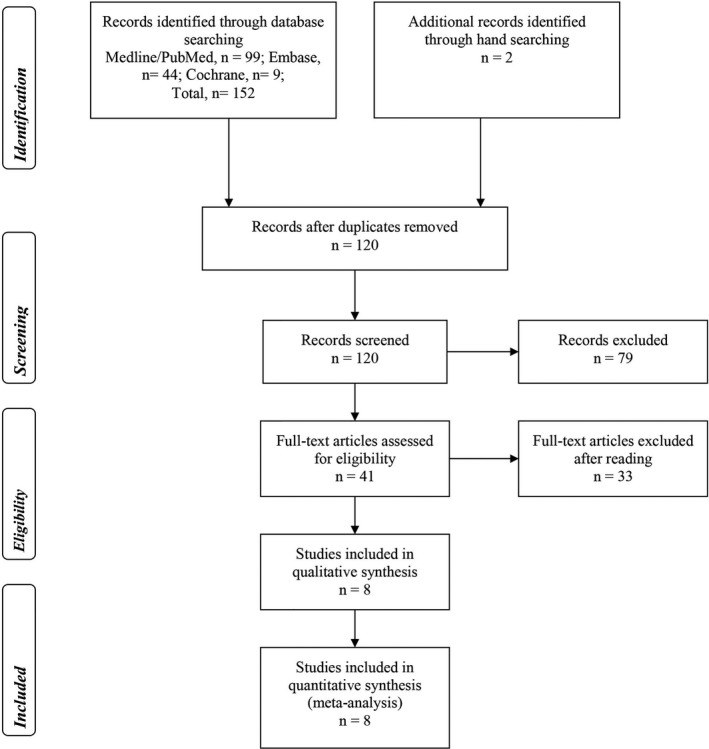
Algorithm of study selection procedure
Characteristics of these studies are depicted in Table 2. Five articles described a prospective study (two articles with two study groups) with a follow‐up varying from 12 to 60 months and with five study groups using implants of 6 mm in length and two study groups with 10‐mm implants. Three articles described a retrospective study with a mean follow‐up varying from 44.5 months to 74 months.
Table 2.
Characteristics of included studies
| Author | Year of publication | Study design | Follow‐up in months | Number of implant‐supported crowns | Location of implant‐supported crown | Implant system | Implant length + category | Implant diameter | Material of restoration | Connection of restoration | Presence of antagonist |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Krennmair et al. | 2007 | Retrospective | 44.5 ± 22.7 | 54 | Maxilla | Frialit‐2 and Camlog | Mean 15.4 ± 0.5 mm | 3.3–5.5 mm | Porcelain fused to metal | Cemented | # |
| Urdaneta et al. | 2010 | Retrospective | 71 ± 23 | 326 | Maxilla and mandible | Bicon | Mean 9.2 mm (from 6 to 14 mm) | 3.5–6 mm | # | Locking taper | Yes |
| Schneider et al. | 2012 | Retrospective | 74 (min 57–max 140) | 100 | Maxilla and mandible | Straumann Standard, Strauman Standard Plus and Brånemark | Mean 11.5 mm (from 7 to 15 mm) | 3.75–5 mm | # | # | Yes |
| Rossi et al. | 2015 | Prospective | 60 | 40 | Maxilla and mandible | Straumann Standard Plus | 6 mm | 4.1 mm | Porcelain fused to metal | Cemented | # |
| Sahrmann et al. | 2016 | Prospective | 36 | 47 | Maxilla and mandible | Straumann Standard Plus | 6 mm | 4.1 mm | Porcelain fused to metal | Screw‐retained | Yes |
| Sahrmann et al. | 2016 | Prospective | 36 | 47 | Maxilla and mandible | Straumann Standard Plus | 10 mm | 4.1 mm | Porcelain fused to metal | Screw‐retained | Yes |
| Rossi et al. | 2016 | Prospective | 60 | 30 | Maxilla and mandible | Straumann Standard | 6 mm | 4.1 mm | Porcelain fused to metal | Cemented | Yes |
| Rossi et al. | 2016 | Prospective | 60 | 30 | Maxilla and mandible | Straumann Standard | 10 mm | 4.1 mm | Porcelain fused to metal | Cemented | Yes |
| Guljé et al. | 2016 | Prospective | 12 | 47 | Maxilla and mandible | Astra Tech Osseospeed | 6 mm | 4.0 mm | Porcelain fused to zirconia | Cemented | Yes |
| Villarinho et al. | 2017 | Prospective | 45 | 46 | Maxilla and mandible | Straumann Standard Plus | 6 mm | 4.1 mm | # | Screw‐retained | # |
#, no (detailed) information provided.
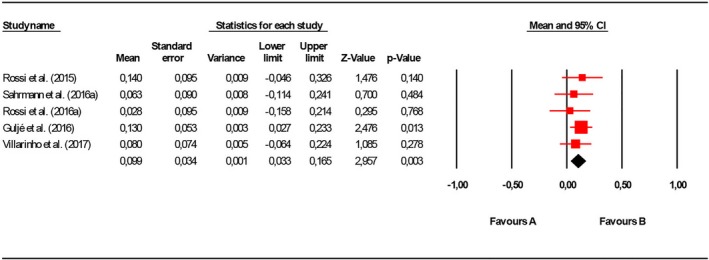
Outcomes of the included studies are depicted in Table 3. The five prospective study groups with 6‐mm implants presented a mean crown‐to‐implant ratio varying from 1.48 to 2.14. The weighted implant loss rate was 0.487 (95% CI: 0.410–0.563; I 2 = 99.51, p = 0.00). The weighted mean bone loss was 0.076 (95% CI: 0.017–0.134; I 2 = 13.79, p = 0.31). To answer the question whether there was an effect of crown‐to‐implant ratio on implant treatment outcomes, a meta‐analysis was performed (Table 4; Figures 2 and 3). Furthermore, the mean crown‐to‐implant ratios of the studies were arranged into the following groups to eventually compare different outcomes with different ratios: <1.00, 1.00–1.49, 1.50–1.99, 2.00–2.49, 2.50–2.99, and ≥3.00, according to the method of Blanes (2009). The meta‐regression analysis did not detect any significant differences regarding implant loss rate and peri‐implant bone loss between the different crown‐to‐implant ratio groups (p = 0.085 and 0.964, respectively). An extra analysis has been carried out for the data of the groups with only 6‐mm implants. Results of this extra analysis are depicted in Table 5 and Figures 4 and 5. For reasons of heterogeneity, only the outcome measures implant survival rate and peri‐implant bone loss could be meaningfully combined. The meta‐analysis is presented per year, assuming a linear distribution of complications. Few papers described technical complications, showing a limited number of adverse events.
Table 3.
Outcomes in included studies
| Author | Year of publication | Type of calculation crown/implant ratio | Mean crown‐to‐implant ratio ± SD | Survival rate of implants during function | Survival rate of restorations | Marginal bone level changes ± SD | Screw fracture | Screw loosening | Abutment fracture | Crown fracture (including chipping) | Crown loosening (of cemented crown) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Krennmair et al. | 2007 | Anatomical | 1.31 ± 0.12 | 100% | # | −2.2 ± 1.4 mm | # | 5.5% | # | 3.7% | 7.4% |
| Urdaneta et al. | 2010 | Clinical | 1.6 (min 0.79–max 4.95) | 98.1% | 94.8% | −0.33 mm | Na | Na | 1% | 5.2% | 5.8% |
| Schneider et al. | 2012 | Clinical | 1.48 ± 0.42 | 95.8% | 100% | −0.01 ± 0.74 mm | 0% | 8% | 0% | 4% | # |
| Rossi et al. | 2015 | Clinical | 1.6 ± 0.4 | 100% | 100% | −0.7 ± 0.6 mm | 0% | 0% | 0% | 0% | 0% |
| Sahrmann et al.a | 2016 | Clinical | 1.48 ± 0.33 | 98% | 98% | −0.19 ± 0.62 mm | 0% | # | # | 0% | Na |
| Sahrmann et al.b | 2016 | Clinical | 0.86 ± 0.18 | 100% | 100% | −0.33 ± 0.71 mm | 0% | # | # | 0% | Na |
| Rossi et al.a | 2016 | Clinical | 1.49 ± 0.36 | 90% | 90% | −0.14 mm | 0% | 0% | 0% | 0% | Na |
| Rossi et al.b | 2016 | Clinical | 0.95 ± 0.21 | 96.7% | 96.7% | −0.18 mm | 0% | 0% | 0% | 0% | 0% |
| Guljé et al. | 2016 | Clinical | 2.14 ± 0.42 | 100% | 100% | −0.13 ± 0.36 mm | 0% | 0% | 0% | 0% | 0% |
| Villarinho et al. | 2017 | Clinical | 1.6 ± 0.3 | 91.3% | 91.3% | −0.3 ± 0.5 mm | 0% | 28.3% | 0% | 0% | Na |
#, no (detailed) information provided; Na, not applicable.
aStudy group with 6‐mm implants; bStudy group with 10‐mm implants.
Table 4.
Meta‐analysis of implant loss rate per year and of mean peri‐implant bone changes per year (confidence interval) for each crown‐to‐implant ratio group
| Crown‐to‐implant ratio | Studies | Sample size (number of implants) | Implant loss rate (%) | Mean peri‐implant bone change (mm) |
|---|---|---|---|---|
| <1.00 |
Sahrmann et al. (2016)b and Rossi et al. (2016)b |
77 | 0.33 | −0.08 (−0.08–0.24) |
| 100–1.49 |
Krennmair et al. (2007), Schneider, Witt, & Hämmerle (2012), Sahrmann et al. (2016)a and Rossi et al. (2016)a |
231 | 0.84 | −0.11 (−0.07–0.30) |
| 1.50–1.99 |
Urdaneta, Rodriguez, McNeil, Weed, and Chuang (2010), Rossi et al. (2015) and Villarinho et al. (2017) |
412 | 0.80 | −0.07 (0.01–0.14) |
| 2.00–2.49 | Guljé et al. (2016) | 47 | 0.01 | −0.13 (0.03–0.23) |
| 2.50–2.99 | – | – | – | – |
| ≥3.00 | – | – | – | – |
aStudy group with 6‐mm implants; bStudy group with 10‐mm implants.
Figure 2.
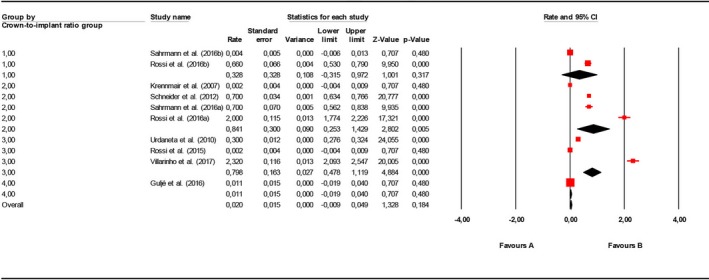
Forest plot for implant loss rate (per year) meta‐analysis for different crown‐to‐implant ratio groups (group 1 = crown‐to‐implant ratio <1.00; group 2 = crown‐to‐implant ratio 1.00–1.49; group 3 = crown‐to‐implant ratio 1.50–1.99; group 4 = crown‐to‐implant ratio 2.00–2.49)
Figure 3.
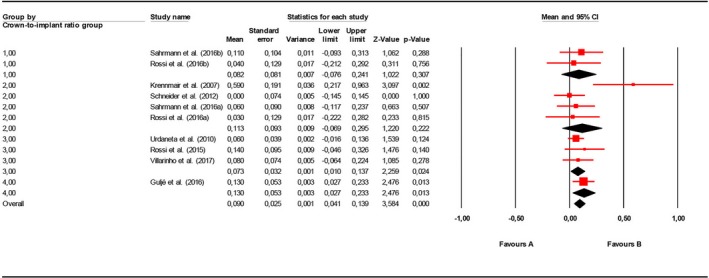
Forest plot for peri‐implant bone loss (millimeter per year) meta‐analysis for different crown‐to‐implant ratio groups (group 1 = crown‐to‐implant ratio <1.00; group 2 = crown‐to‐implant ratio 1.00–1.49; group 3 = crown‐to‐implant ratio 1.50–1.99; group 4 = crown‐to‐implant ratio 2.00–2.49)
Table 5.
Meta‐analysis of studies with 6‐mm implants with implant loss rate per year and of mean peri‐implant bone changes per year (confidence interval)
Figure 4.
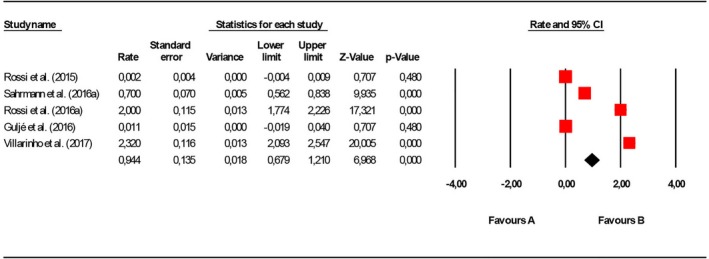
Forest plot for implant loss rate (per year) meta‐analysis for studies with 6‐mm implants
Figure 5.
Forest plot for peri‐implant bone loss rate (millimeter per year) meta‐analysis for studies with 6‐mm implants
4. DISCUSSION
An influence of crown‐to‐implant ratio of single‐tooth, nonsplinted, implants on biological and technical complications could not be demonstrated. A meta‐analysis of implant survival and peri‐implant bone changes showed high survival rates and limited bone loss for different crown‐to‐implant ratio groups.
However, it must be noted that only eight studies (with ten study groups) could be included in the systematic review and meta‐analysis. This makes that firm conclusion could not be drawn on basis of the available material. The main reason for exclusion of articles was the fact that reporting of crown‐to‐implant ratio was not dealing with single‐tooth restorations (short implants were splinted to other short implants or splinted to longer implants) or data of single‐tooth restorations could not be extracted. Earlier systematic reviews on influence of crown‐to‐implant ratio (Blanes, 2009; Esfahrood et al., 2017; Garaicoa‐Pazmiño et al., 2014; Quaranta et al., 2014) included higher numbers of articles, but admitted that various restoration designs were present, with no distinction between splinted and nonsplinted crowns, making interpretation difficult. The authors of the present systematic review have the opinion that analyzing influence of crown‐to‐implant ratio should be done with single, nonsplinted, implant‐supported restorations. Splinted restorations may act differently on connection between crown and implant and, most likely, splinted restorations transmit forces on peri‐implant bone in another magnitude than nonsplinted restorations.
Follow‐up is limited to 74 months in the retrospective studies and 60 months in the prospective studies. Although no influence of crown‐to‐implant ratio is known from long‐term follow studies (≥10 years), most of them are (close to) medium‐term and should be long enough to present some sort of biological or technical complication related to crown‐to‐implant ratio. Total number of implant‐supported restorations is 480 of the retrospective studies and 287 of the prospective studies. These numbers can be called rather low to investigate a possible influence of crown‐to‐implant ratio.
Crown‐to‐implant ratio can be calculated measuring the length of the implant in relation to the crown including the abutment (anatomical ratio) or the length of the supporting bone in relation to the supported suprastructure (clinical ratio). In seven of the eight study groups was a clinical crown‐to‐implant ratio calculated, which is seen as more realistic than an anatomical crown‐to‐implant ratio (Meijer et al., 2012). Mean clinical crown‐to‐implant ratio varied from 0.86 to 1.74, except for the study of Guljé, Raghoebar, Erkens, and Meijer (2016) which reports 2.14. The lather study calculated a ratio deviating significantly from other studies in which also 6‐mm implants were used. This means that in the study of Guljé et al. (2016) the length of the crowns was larger than in the other studies, probably caused by the reason that in this study the 6‐mm implants were placed in cases showing more extreme alveolar bone resorption.
Studies reported high implant survival and crown survival rates, except for the study of Villarinho et al. (2017) which mentioned a survival rate of 91.3% for implants as well as crowns after a follow‐up of 45 months. This percentage is rather low compared to an expected implant survival rate of more than 97% after 5 years as stated in the systematic review of Doornewaard et al. (2017). Also minimal bone loss was reported in the studies, except for the study of Krennmair, Krainhöfner, Schmid‐Schwap, and Piehslinger (2007) in which a mean bone loss of 2.2 mm was mentioned after a mean follow‐up of 45 months. Doornewaard et al. (2017) mentioned a mean bone loss of 1.0 mm to be expected after 5 years. Only in one study (Guljé et al., 2014, 2016) an attempt was made to differentiate between upper and lower jaws. In the former study, no differences were detected regarding implant survival and marginal bone loss.
A minimum amount of technical complications was found in the studies. One exception is again the study of Villarinho et al. (2017) which mentioned screw loosening being 28.3% after a follow‐up of 45 months. This is in strong contrast to other studies and can best be compared with the study of Rossi et al. (2015) in which the same implant system was used. These authors mentioned 0% screw loosening. However, it must be said that in the study of Villarinho et al. (2017) a two‐screw system was used in which the prosthetic screw received a lower initial preload (15 Ncm) than the abutment screw (35 Ncm). In the study of Rossi et al. (2015), only abutment screws (tightened with 35 Ncm) were used, and the crowns were cemented. Possibly, these low torque values are at risk for screw loosening, whether or not extra influenced by a high crown‐to‐implant ratio. No information was given on the occlusal table of the restorations.
To get an overview on influence of crown‐to‐implant ratio on biological and technical complications to determine at what magnitude, there is a possible negative effect, mean crown‐to‐implant ratios of the studies were arranged into groups, following the suggestion of Blanes (2009). In Table 4, a meta‐analysis of implant survival per year and of mean peri‐implant bone changes per year are presented for each crown‐to‐implant ratio group. For reasons of heterogeneity, other outcomes could not be meaningfully combined. The meta‐analysis is presented per year, assuming a linear distribution of complications. This assumption is probably a limitation, because it is questionable if complications follow timelines. There are only limited studies per group, making a meta‐analysis not very worthwhile at this stage. Moreover, there are no studies present to fit into the groups with a mean crown‐to‐implant of 2.50 and higher. The meta‐analysis showed an implant survival of more than 99% per year and mean peri‐implant bone changes of <0.2 mm per year. Given these low numbers of complications in the included studies, it is likely that a possible effect must be found in groups with 2.50 and higher if there is an association between height of crown‐to‐implant ratio and complications. However, more studies are needed, especially in the higher crown‐to‐implant groups, to determine at what magnitude there is a possible negative effect.
It is concluded that data reviewed in the current manuscript on crown‐to‐implant ratio ranging from 0.9 to 2.2 did not demonstrate a high occurrence of biological or technical complications.
CONFLICT OF INTEREST
The authors have stated explicitly that there are no conflict of interests in connection with this article.
Meijer HJA, Boven C, Delli K, Raghoebar GM. Is there an effect of crown‐to‐implant ratio on implant treatment outcomes? A systematic review. Clin Oral Impl Res. 2018;29(Suppl. 18):243–252. 10.1111/clr.13338
REFERENCES
- Annibali, S. , Cristalli, M. P. , Dell'Aquila, D. , Bignozzi, I. , La Monaca, G. , & Pilloni, A. (2012). Short dental implants: A systematic review. Journal of Dental Research, 91, 25–32. 10.1177/0022034511425675 [DOI] [PubMed] [Google Scholar]
- Atieh, M. A. , Zadeh, H. , Stanford, C. M. , & Cooper, L. F. (2012). Survival of short dental implants for treatment of posterior partial edentulism: A systematic review. International Journal of Oral & Maxillofacial Implants, 27, 1323–1331. [PubMed] [Google Scholar]
- Blanes, R. J. (2009). To what extent does the crown–implant ratio affect survival and complications of implant‐supported reconstructions? A systematic review. Clinical Oral Implants Research, 20(Suppl. 4), 67–72. 10.1111/j.1600-0501.2009.01762.x [DOI] [PubMed] [Google Scholar]
- Blanes, R. J. , Bernard, J. P. , Blanes, Z. M. , & Belser, U. C. (2007). A 10‐year prospective study of ITI dental implants placed in the posterior region. II: Influence of the crown‐to‐implant ratio and different prosthetic treatment modalities on crestal bone loss. Clinical Oral Implants Research, 18, 707–714. [DOI] [PubMed] [Google Scholar]
- Doornewaard, R. , Christiaens, V. , De Bruyn, H. , Jacobsson, M. , Cosyn, J. , Vervaeke, S. , & Jacquet, W. (2017). Long‐term effect of surface roughness and patients’ factors on crestal bone loss at dental implants. A systematic review and meta‐analysis. Clinical Implant Dentistry and Related Research, 19, 372–399. 10.1111/cid.12457 [DOI] [PubMed] [Google Scholar]
- Esfahrood, Z. R. , Ahmadi, L. , Karami, E. , & Asghari, S. (2017). Short dental implants in the posterior maxilla: A review of the literature. Journal of the Korean Association of Oral and Maxillofacial Surgeons, 43, 70–76. 10.5125/jkaoms.2017.43.2.70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan, T. , Li, Y. , Deng, W. W. , Wu, T. , & Zhang, W. (2017). Short Implants (5 to 8 mm) Versus Longer Implants (>8 mm) with Sinus Lifting in Atrophic Posterior Maxilla: A Meta‐Analysis of RCTs. Clinical Implant Dentistry and Related Research, 19, 207–215. 10.1111/cid.12432 [DOI] [PubMed] [Google Scholar]
- Garaicoa‐Pazmiño, C. , Suárez‐López del Amo, F. , Monje, A. , Catena, A. , Ortega‐Oller, I. , Galindo‐Moreno, P. , & Wang, H. L. (2014). Influence of crown/implant ratio on marginal bone loss: A systematic review. Journal of Periodontology, 85, 1214–1221. 10.1902/jop.2014.130615 [DOI] [PubMed] [Google Scholar]
- Gonçalves, T. M. , Bortolini, S. , Martinolli, M. , Alfenas, B. F. , Peruzzo, D. C. , Natali, A. , … Garcia, R. C. (2015). Long‐term short implants performance: Systematic review and meta‐analysis of the essential assessment parameters. Brazilian Dental Journal, 26, 325–336. 10.1590/0103-6440201300265 [DOI] [PubMed] [Google Scholar]
- Guljé, F. L. , Raghoebar, G. M. , Erkens, W. A. , & Meijer, H. J. (2016). Impact of Crown‐Implant Ratio of Single Restorations Supported by 6‐mm Implants: A Short‐Term Case Series Study. International Journal of Oral & Maxillofacial Implants, 31, 672–675. https://doi.org/10.11607/jomi.4092 [DOI] [PubMed] [Google Scholar]
- Guljé, F. L. , Raghoebar, G. M. , Vissink, A. , & Meijer, H. J. (2014). Single crowns in the resorbed posterior maxilla supported by either 6‐mm implants or by 11‐mm implants combined with sinus floor elevation surgery: A 1‐year randomised controlled trial. European Journal of Oral Implantology, 7, 247–255. [PubMed] [Google Scholar]
- Guo, B. , Moga, C. , Harstall, C. , & Schopflocher, D. (2016). A principal component analysis is conducted for case series quality appraisal checklist. Journal of Clinical Epidemiology, 69, 199–207. 10.1016/j.jclinepi.2015.07.010 [DOI] [PubMed] [Google Scholar]
- Kotsovilis, S. , Fourmousis, I. , Karoussis, I. K. , & Bamia, C. (2009). A systematic review and meta‐analysis on the effect of implant length on the survival of rough‐surface dental implants. Journal of Periodontology, 80, 1700–1718. 10.1902/jop.2009.090107 [DOI] [PubMed] [Google Scholar]
- Krennmair, G. , Krainhöfner, M. , Schmid‐Schwap, M. , & Piehslinger, E. (2007). Maxillary sinus lift for single implant‐supported restorations: A clinical study. International Journal of Oral & Maxillofacial Implants, 22, 351–358. [PubMed] [Google Scholar]
- Lai, H. C. , Si, M. S. , Zhuang, L. F. , Shen, H. , Liu, Y. L. , & Wismeijer, D. (2013). Long‐term outcomes of short dental implants supporting single crowns in posterior region: A clinical retrospective study of 5‐10 years. Clinical Oral Implants Research, 24, 230–237. 10.1111/j.1600-0501.2012.02452.x [DOI] [PubMed] [Google Scholar]
- Lemos, C. A. , Ferro‐Alves, M. L. , Okamoto, R. , Mendonça, M. R. , & Pellizzer, E. P. (2016). Short dental implants versus standard dental implants placed in the posterior jaws: A systematic review and meta‐analysis. Journal of Dentistry, 47, 8–17. 10.1016/j.jdent.2016.01.005 [DOI] [PubMed] [Google Scholar]
- Malchiodi, L. , Cucchi, A. , Ghensi, P. , Consonni, D. , & Nocini, P. F. (2014). Influence of crown–implant ratio on implant success rates and crestal bone levels: A 36‐month follow‐up prospective study. Clinical Oral Implants Research, 25, 240–251. 10.1111/clr.12105 [DOI] [PubMed] [Google Scholar]
- Meijer, H. J. A. , Telleman, G. , Gareb, C. , Den Hartog, L. , Vissink, A. , & Raghoebar, G. M. (2012). A comparison of implant‐supported crown length measured on digitized casts and intraoral radiographs. International Journal of Prosthodontics, 25, 357–359. [PubMed] [Google Scholar]
- Mezzomo, L. A. , Miller, R. , Trichet, D. , Alonso, F. , & Shinkai, R. S. A. (2014). Meta‐analysis of single crowns supported by short (<10 mm) implants in the posterior region. Journal of Clinical Periodontology, 41, 191–213. 10.1111/jcpe.12180 [DOI] [PubMed] [Google Scholar]
- Moga, C. , Guo, B. , Schopflocher, D. , & Harstall, C. (2012). Development of a quality appraisal tool for case series studies using a modified Delphi technique. Edmonton, AB: Institute of Health Economics; Available at http://www.ihe.ca/advanced-search/development-of-a-quality-appraisal-tool-for-case-series-studies-using-a-modified-delphi-technique. [Google Scholar]
- Monje, A. , Chan, H. L. , Fu, J. H. , Suarez, F. , Galindo‐Moreno, P. , & Wang, H. L. (2013). Are short dental implants (<10 mm) effective? a meta‐analysis on prospective clinical trials. Journal of Periodontology, 84, 895–904. 10.1902/jop.2012.120328 [DOI] [PubMed] [Google Scholar]
- Nisand, D. , Picard, N. , & Rocchietta, I. (2015). Short implants compared to implants in vertically augmented bone: A systematic review. Clinical Oral Implants Research, 26(Suppl 11), 170–179. 10.1111/clr.12632 [DOI] [PubMed] [Google Scholar]
- Pommer, B. , Frantal, S. , Willer, J. , Posch, M. , Watzek, G. , & Tepper, G. (2011). Impact of dental implant length on early failure rates: A meta‐analysis of observational studies. Journal of Clinical Periodontology, 38, 856–863. 10.1111/j.1600-051X.2011.01750.x [DOI] [PubMed] [Google Scholar]
- Quaranta, A. , Piemontese, M. , Rappelli, G. , Sammartino, G. , & Procaccini, M. (2014). Technical and biological complications related to crown to implant ratio: A systematic review. Implant Dentistry, 23, 180–187. 10.1097/ID.0000000000000026 [DOI] [PubMed] [Google Scholar]
- Renouard, F. , & Nisand, D. (2006). Impact of implant length and diameter on survival rates. Clinical Oral Implants Research, 17(Suppl 2), 35–51. [DOI] [PubMed] [Google Scholar]
- Rossi, F. , Botticelli, D. , Cesaretti, G. , De Santis, E. , Storelli, S. , & Lang, N. P. (2016). Use of short implants (6 mm) in a single‐tooth replacement: A 5‐year follow‐up prospective randomized controlled multicenter clinical study. Clinical Oral Implants Research, 27, 458–464. 10.1111/clr.12564 [DOI] [PubMed] [Google Scholar]
- Rossi, F. , Lang, N. P. , Ricci, E. , Ferraioli, L. , Marchetti, C. , & Botticelli, D. (2015). Early loading of 6‐mm‐short implants with a moderately rough surface supporting single crowns ‐ a prospective 5‐year cohort study. Clinical Oral Implants Research, 26, 471–477. 10.1111/clr.12409 [DOI] [PubMed] [Google Scholar]
- Sahrmann, P. , Naenni, N. , Jung, R. E. , Held, U. , Truninger, T. , Hämmerle, C. H. , … Schmidlin, P. R. (2016). Success of 6‐mm implants with single‐tooth restorations: A 3‐year randomized controlled clinical trial. Journal of Dental Research, 95, 623–628. 10.1177/0022034516633432 [DOI] [PubMed] [Google Scholar]
- Schneider, D. , Witt, L. , & Hämmerle, C. H. (2012). Influence of the crown‐to‐implant length ratio on the clinical performance of implants supporting single crown restorations: A cross‐sectional retrospective 5‐year investigation. Clinical Oral Implants Research, 23, 169–174. 10.1111/j.1600-0501.2011.02230.x [DOI] [PubMed] [Google Scholar]
- Srinivasan, M. , Vazquez, L. , Rieder, P. , Moraguez, O. , Bernard, J. P. , & Belser, U. C. (2014). Survival rates of short (6 mm) micro‐rough surface implants: A review of literature and meta‐analysis. Clinical Oral Implants Research, 25, 539–545. 10.1111/clr.12125 [DOI] [PubMed] [Google Scholar]
- Sun, H. L. , Huang, C. , Wu, Y. R. , & Shi, B. (2011). Failure rates of short (≤ 10 mm) dental implants and factors influencing their failure: A systematic review. International Journal of Oral & Maxillofacial Implants, 26, 816–825. [PubMed] [Google Scholar]
- Telleman, G. , Raghoebar, G. M. , Vissink, A. , den Hartog, L. , Huddleston Slater, J. J. , & Meijer, H. J. (2011). A systematic review of the prognosis of short (<10 mm) dental implants placed in the partially edentulous patient. Journal of Clinical Periodontology, 38, 667–676. 10.1111/j.1600-051X.2011.01736.x [DOI] [PubMed] [Google Scholar]
- Thoma, D. S. , Cha, J. K. , & Jung, U. W. (2017). Treatment concepts for the posterior maxilla and mandible: Short implants versus long implants in augmented bone. Journal of Periodontal & Implant Science, 47, 2–12. 10.5051/jpis.2017.47.1.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoma, D. S. , Zeltner, M. , Hüsler, J. , Hämmerle, C. H. , & Jung, R. E. (2015). EAO Supplement Working Group 4 ‐ EAO CC 2015 Short implants versus sinus lifting with longer implants to restore the posterior maxilla: A systematic review. Clinical Oral Implants Research, 26(Suppl 11), 154–169. 10.1111/clr.12615 [DOI] [PubMed] [Google Scholar]
- Urdaneta, R. A. , Rodriguez, S. , McNeil, D. C. , Weed, M. , & Chuang, S. K. (2010). The effect of increased crown‐to‐implant ratio on single‐tooth locking‐taper implants. International Journal of Oral & Maxillofacial Implants, 25, 729–743. [PubMed] [Google Scholar]
- Villarinho, E. A. , Triches, D. F. , Alonso, F. R. , Mezzomo, L. A. M. , Teixeira, E. R. , & Shinkai, R. S. A. (2017). Risk factors for single crowns supported by short (6‐mm) implants in the posterior region: A prospective clinical and radiographic study. Clinical Implant Dentistry and Related Research, 19, 671–680. 10.1111/cid.12494 [DOI] [PubMed] [Google Scholar]


