Abstract.
Different health-care management guidelines by the World Health Organization exist to help health workers in resource-limited settings treat patients. However, for children with unclassified fever and no danger signs, management guidelines are less clear and follow-up recommendations differ. Both a “universal follow-up” for all children, irrespective of health status, and a “conditional follow-up” only for children whose fever persists are recommended in different guidelines. It is unclear how feasible and acceptable these two different follow-up guidelines are among community health workers and caregivers of the sick child. This qualitative study was conducted in Ethiopia and was nested within a cluster-randomized controlled trial (cRCT). It aimed to determine health extension workers’ (HEWs’) and caregivers’ experiences of the management of febrile children and their perceptions of universal versus conditional follow-up recommendations. Seventeen HEWs and 20 caregivers were interviewed. The interviews revealed that HEWs’ understanding of how to handle an unclassified fever diagnosis increased with the implementation of the cRCT in both study arms (universal versus conditional follow-up). This enabled HEWs to withhold medicines from children with this condition and avoid referral to health centers. Both follow-up recommendations had perceived advantages, while the universal follow-up provided an opportunity to see the child’s health progress, the conditional follow-up advice allowed saving time and costs. The findings suggest that improved awareness of the unclassified fever condition can make HEWs feel more comfortable in managing these febrile children themselves and omitting unnecessary medication. Future community-level management guidelines should provide clearer instructions on managing fever where no malaria, pneumonia, diarrhea, or danger signs are present.
INTRODUCTION
Globally, a large number of different healthcare management guidelines exist that help health workers in managing patients. Particularly, in resource-limited settings, where diagnostic capabilities are restricted, simple management guidelines can help to treat patients and potentially save lives. Integrated management of childhood illnesses (IMCI), at the health facility level, and integrated community case management (iCCM), at the community level, are examples of existing guidelines. Both are simple and integrated approaches for classifying and managing symptoms of common childhood infections, such as pneumonia, diarrhea, and malaria, as well as for referring severely ill children.1–3 Their instructions on treating these common childhood infections are relatively straight forward, following a stepwise approach, and treatment options for these infections should exist in rural settings. However, when it comes to cases where febrile children cannot be diagnosed with any of these diseases, management guidelines are less clear and follow-up recommendations between IMCI and iCCM differ.
Fever in children is common around the world. It is a symptom of diseases such as malaria or pneumonia, the leading causes of child mortality. However, fever is in most cases self-limiting and commonly resolves quickly, typically in fewer than 3 days.4–6 The steady global decrease in malaria incidence leads to an increased proportion of febrile children seen by health workers who have an unclassifiable diagnosis.7 The commonness of “simple” fever necessitates clear management guidelines for febrile illnesses that cannot be diagnosed using iCCM (i.e. unclassified fever).
Today, according to iCCM guidelines, children with unclassified fever and without danger signs (e.g., cough for 14 days or more, diarrhea for 14 days or more, and blood in stool) should not receive treatment.1 Nevertheless, this recommendation is implemented in different ways in different countries. By contrast, IMCI guidelines recommend that paracetamol be given to children with high fever (38.5°C). Both guidelines also formulate follow-up recommendations differently. According to iCCM, all caregivers of children with unclassified fever should be advised to return to the community health worker (CHW) for a follow-up visit for a reassessment of the child (i.e., universal follow-up).8 On the contrary, IMCI guidelines recommend caregivers of children with unclassified fever to return for follow-up only if the child’s fever persists (i.e., conditional follow-up).9,10 In both guidelines, caregivers are advised to return immediately if the health status of the child worsens.
No research has been conducted into exploring health worker and caregiver perceptions of the follow-up recommendations. Advising that all children with unclassified fever be brought for follow-up might be unnecessary if many of them have recovered before the assigned day. Furthermore, it can create an additional burden for both families and health workers. On the other hand, it may promote detection of those at risk of developing severe illness. This study therefore aimed to explore how children with fever, particularly unclassified fever, are managed by HEWs and caregivers in rural communities in Ethiopia. In addition, HEWs’ and caregivers’ perceptions of the follow-up recommendations were studied.
MATERIALS AND METHODS
The reporting of the methods has been guided by the criteria for reporting qualitative research (COREQ) guidelines.11
Study context.
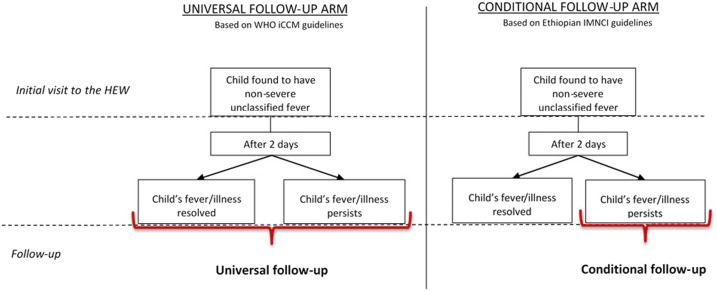
This qualitative study was conducted as part of a cluster-randomized, community-based, controlled non-inferiority trial (cRCT) which compared the safety of a HEW-advised conditional 3-day follow-up visit only in cases where symptoms did not resolve, with a universal follow-up visit at day 3 for all children (Figure 1). In Ethiopia, HEWs follow Integrated Management of Neonatal and Childhood Illnesses (IMNCI) guidelines.9 These are similar to IMCI guidelines in their follow-up recommendation for children with unclassified fever; recommending conditional follow-up. Consequently, in one study arm, HEWs used the country’s IMNCI guidelines as usual, whereas in the other study arm a universal follow-up was introduced. Whether the child is still febrile and should return for the follow-up visit is assessed by the caregivers themselves. Caregivers do not receive any specific instructions on how to assess the child’s temperature. Rather, they assess the child’s health status subjectively, through close contact, for instance, noticing elevated body temperature through touching/body contact or observing differences in the child’s (eating) behavior. Literature suggests that mothers are good at establishing when their children are febrile.12,13 In both arms, caregivers were advised to bring their child back at any time if the condition of the child worsened.14 During the follow-up assessment (day 3), HEWs examine the child using the same procedure as during the initial visit (day 1). If a child is still found to have unclassified fever, it could be an indication of a more severe cause of the fever. Consequently, the child would in this case be referred to the health center for further examination. This is important to keep in mind as not all children with unclassified fever will recover without medical treatment. The fever can also be a result of a more severe infection, such as typhoid fever. However, the follow-up recommendation should then come into play and identify these severe cases during the follow-up visit. The study protocol of the trial and quantitative results of this research project are published elsewhere.15,14
Figure 1.
Summary of the follow-up recommendations for febrile children with unclassified fever used in the two study arms. HEW = Health Extension worker; iCCM = Integrated Community Case Management; IMNCI = Integrated Management of Neonatal and Childhood Illnesses. This figure appears in color at www.ajtmh.org.
Setting.
Interviews were conducted in three woredas (districts) of the Southern Nations, Nationalities, and People’s Region (SNNPR) of Ethiopia: Damot Gale, Boloso Sore, and Halaba Special Woreda. Together, the population of these woredas is projected to be around 750,000, with the vast majority (∼80%) living in rural areas. A total of 284 HEWs work in 144 health posts (HP) in these three woredas. There is one HP in every kebele (smallest administrative unit; subdistrict), serving an estimated 3,000–5,000 people. Two HEWs usually work at one HP together. Health extension workers are trained and employed by the government and receive salaries.16,17
Recruitment and data collection.
The 13 HEWs who had enrolled most children for the cRCT between December 2015 and February 2016 were purposively selected for interviews. In four cases, the selected HEW officially worked together with another HEW, and the two were interviewed as a pair. The 13 interviews, therefore, represent a total of 17 HEWs. The mean age of the HEWs was 26 years (range 20–35 years), with an average of 6.5 years of work experience as a HEW (median 8; range 1–12 years) (Table 1).
Table 1.
Characteristics of study participants
| Health extension workers N = 17 | Caregivers N = 20 | |
|---|---|---|
| Age (years)* | ||
| 19–24 | 3 | 1 |
| 25–29 | 9 | 11 |
| 30–34 | 4 | 5 |
| 35–40 | 1 | 2 |
| Work experience (in years) | ||
| 1–4 | 6 | – |
| 5–9 | 8 | – |
| 10–15 | 3 | – |
| Mean | 6.5 | – |
| Number of children | ||
| 1–3 | – | 13 |
| 4+ | – | 7 |
| Study district | ||
| Boloso Sore | 4 | – |
| Damot Gale | 4#1 | 17 |
| Halaba | 9#3 | 3 |
| Study arm | ||
| Universal follow-up | 8#2 | 10 |
| Conditional follow-up | 9#2 | 10 |
| Mean length of the interview (in min) | 46 | 39 |
Age information of one caregiver missing.
#n Number of interviews conducted in pairs.
Furthermore, 20 caregivers of children enrolled in the study were randomly selected for the interviews in each study arm. All caregivers whose children had been enrolled in the study during the previous 2 weeks (March 29–April 11, 2016) were identified (N = 290). Following this, using Stata, random numbers between 1 and 290 determined which of the caregivers were invited for the interview.
By chance, the vast majority of caregiver interviews were conducted in Damot Gale and only a few in Halaba. All caregivers interviewed were mothers; they were aged between 19 and 35 years and most had three or fewer children (Table 1). Half of the interviews (HEW: N = 6; caregiver: N = 10) were conducted in the study arm using the universal follow-up recommendation, and the other half were conducted in the study arm using the conditional follow-up recommendation. HEWs were contacted via phone, whereas caregivers were reached with the help of the HEW in the respective community.
Semi-structured interview guides were separately prepared for HEWs and caregivers. The guides were formulated in English and then translated into Amharic. They addressed management and treatment practices of children with unclassified fever as well as perceptions and experiences of the follow-up recommendations. Two male, Amharic-speaking interviewers conducted the HEW interviews and one additional male interviewer who was also fluent in the local language Wolaitegna was recruited for the caregiver interviews. The interviewers had a Master’s education in health sciences and experience of conducting studies in rural Ethiopia.
Interviews were conducted between March and April 2016 and took between 22 and 77 minutes. HEW interviews generally took longer. The interviews took place either at the respective HP or, for some HEWs, at the district health office or a quiet place outside. Health extension workers were interviewed in Amharic (official language of Ethiopia), whereas caregiver interviews were conducted in Wolaitegna (in Damot Gale) and Halabigna (in Halaba), local languages of the study districts. Translators who were fluent in these local languages were selected by the Ethiopian research team and were used for most of the caregiver interviews. The interviews were digitally recorded, transcribed, and translated into English by the interviewers. For their participation in the study, HEWs received phone credit of 50 Birr (∼2.20 USD) and caregivers 122.5 Birr in cash (∼5.5 USD), which they were informed of after the interview.
Data analysis.
Each interview transcript was read multiple times by the main author (TF). Content analysis was applied to the interview transcripts.18 Codes were initially assigned freely and then merged and adjusted during the data analysis process using the qualitative data analysis software Nvivo (version 11). HEW and caregiver interviews were coded separately to understand the perceptions of both groups. HEW interviews were analyzed first and a preliminary analysis was discussed among all authors. Caregiver interviews were subsequently compared with and contrasted to the main themes identified in the HEW interviews. The analysis process was data-driven based on all full interview transcripts which finally lead to one common coding scheme (Table 2). Two of the authors (TF and HMA) discussed the categories and themes during an iterative process which took place between April 2016 and January 2017.
Table 2.
Codes, categories, and themes of the study
| Theme | The emergence of unclassified fever as diagnosis | ||||||
|---|---|---|---|---|---|---|---|
| Subthemes | The meaning of “fever” | Changes in fever management | Trade-offs between follow-up recommendations | ||||
| Categories | Visibility of the disease | Fever without malaria | Health workers as focal point for fever management | Renegotiating the need of medicine | Reporting raises attention | Conditional follow-up: Reducing the number of visits to health facilities | Universal follow-up as continuum of care |
| Codes | Caregivers want a malaria diagnosis | Fever not only caused by malaria | HEWs as educators | Never send patients back empty handed | Giving attention to fever | Reduction in visits to health facility | Following process of disease and visibility of diagnostic outcome |
| Fever expected to be malaria | Unclassified fever is no disease | Communication between HEWs and caregivers | Caregivers insist on medicine | HEWs’ desire for knowledge | Possibility for additional services and diagnosis when needed | Reduction in diagnostic uncertainty | |
| Concerns about the child’s illness | Child is free of disease | HEWs play a role as health professionals | Caregivers comply with follow-up recommendation | Fever alone recognized as illness | Separation of illness cases | Possibility for additional services and diagnosis | |
| Blood tests | – | HEWs give advice | Recovery of child equals correct diagnosis | Reporting as a task of HEWs | Recommendation reduces referral and costs | Facilitating mothers to return for follow-up | |
| Disease could not be seen | – | – | No medicine given as treatment at health posts | Conducting follow-ups during outreach activities | – | Seeing the same child twice | |
| – | – | – | Drugs as incentive to seek care at health posts | – | – | – | |
Ethical approval.
This study was approved by the SNNPR Health Bureau Research Ethical Review Committee (P02-6-19/4511). The trial is registered as NCT02926625. Written and oral consent was obtained from all study participants. Confidentiality was ensured and interviewees were informed about the possibility to decline participation or drop out of the interview. Caregivers were informed that nonparticipation would not result in decline in or limited access to care for the child or any family member.
RESULTS
The results are presented under three subthemes: 1) The meaning of “fever,” 2) changes in fever management, and 3) trade-offs between follow-up recommendations. These fed into the overarching theme of this study: The emergence of unclassified fever as possible diagnosis (Table 2).
The meaning of “fever.”
Unclassified fever was often explained to caregivers by HEWs as “fever without malaria” (in Amharic: tekusat weba yaltegegnebet) when a mother brought a febrile child to the HP, but no cause of the fever could be identified. The child was also described to be “free of disease,” to have “no disease symptom,” or simply to have “nothing.” Before the trial was initiated in the area, children presenting with fever alone were often referred to health centers. However, after the start of the cRCT, HEWs acknowledged unclassified fever as a distinct condition that they were able to manage themselves.
One caregiver described this as follows:
(…) previously when my children were sick and I brought them to this health post, they [HEWs] sent me to the health center but now they changed their advice and told me to go back home. (Caregiver ID 1; conditional follow-up)
Mixed feelings about the inability of HEWs to diagnose the febrile child at the HP were reported by caregivers. While some felt that this diagnosis was “not fulfilling,” others expressed their satisfaction with the fact that the child was not diagnosed with any disease and, therefore, was apparently healthy.
At the HP level, malaria rapid diagnostic tests (mRDT) are used by HEWs when children have fever to diagnose or rule out malaria. In this study, one HEW also described the mRDTs’ potential function as a disease visualization tool when handling children with unclassified fever. This helped her to confirm the absence of malaria and to increase caregivers’ understanding of the unclassified fever diagnosis.
When I tell them [caregivers] that the fever has no malaria, (…) I confirm the diagnosis of the blood test by showing them the RDT and tell them: “if the child has malaria, it will be detected by this device [mRDT].” (HEW ID 2; universal follow-up arm)
Most of the mothers recalled that the blood of the child was tested. However, mothers did not specify exactly how the test result was explained to them.
Changes in fever management.
Medicines played a great role in the management of sick children at the HP. “I will not let them [patients] go home without medication” (HEW ID 4; conditional follow-up arm) was a sentence uttered by several HEWs. They explained that before the project they commonly treated febrile children with antipyretics or antimalarials (artemether–lumefantrine and chloroquine), irrespective of the severity of the fever or mRDT result. Factors that contributed to this were the wish of the HEW to provide care and the belief that caregivers might not come back if they were refused medicines. Following up children with unclassified fever at the HP was not a common practice before the trial, even though it is recommended in the national IMNCI guidelines. In only four of the 13 interviews did HEWs mention having recommended some sort of follow-up visit before the trial.
When asked about their current fever management practices, HEWs reported that they now recommend a follow-up visit for children with unclassified fever and withholding medication (unless the child had high fever, in which case they gave antipyretics or referred directly). The mothers confirmed being recommended a follow-up visit.
To compensate for the withholding of medication for unclassified fever cases and to ensure that caregivers accept this, HEWs placed a stronger emphasis on counseling caregivers. This was distinct from the healthcare advice and recommendations included in their HEW work packages. They informed caregivers of the child’s health condition, that the fever was not caused by malaria and the nonnecessity of medical treatment, or potential side effects of medication.
This communication enabled HEWs to withhold medicines from children with unclassified fever, while simultaneously making caregivers feel like their child was being taken care of rather than being left “empty handed.”
One HEW described the expectations of caregivers and patients as follows:
Psychologically they [patients/caregivers] expect that by going to the health post I will have some medical treatment [for them], but if they have no malaria and we give them advice and (…) treat them politely they consider themselves as they got some treatment. (HEW ID 6B; conditional follow-up arm)
A mother also stated that she appreciated the conversations with the HEW and did not feel too concerned about her child not being treated with medication.
Many HEWs mentioned that they now felt that the mothers were more accepting of the diagnosis and the withholding of medicines. Mothers were further described to argue less and to increasingly comply with the follow-up recommendation given.
Trade-offs between follow-up recommendations.
HEWs appreciated both types of follow-up recommendations for ensuring that most of the mothers returned to the HP. HEWs and caregivers appreciated the opportunity provided by the follow-up visits to examine the (possibly still sick) child a second time and potentially diagnose the ailment on this occasion. A universal follow-up was seen by HEWs as valuable because it enabled them to see the outcome of the child’s illness. HEWs declared their interest in knowing whether their diagnosis and case management were correct and whether the child’s health status had in fact improved. HEWs who did not fully trust a negative mRDT result during the initial visit described having a second opportunity to conduct an mRDT during the follow-up. A negative mRDT result during the follow-up confirmed to them the absence of malaria and increased their trust in the test result. The universal follow-up process was viewed as being part of a continuum of care, in which mothers benefit from additional health education by the HEW, even if the child had recovered at the time of the follow-up visit.
(…) the recommendation [universal follow-up] gives us the opportunity to know the outcome of our decision; whether the child improved or not, whether they took it [the child] to other places. So, it is very useful for us. (HEW ID 2; universal follow-up arm)
There were also some concerns raised about the universal follow-up recommendation, as some HEWs felt that the time spent on the follow-up could be used in better ways.
You are seeing the same child two times and the time you spend on this child could be used to see another child or to carry out another activity. (HEW ID 11A; universal follow-up arm)
Such concerns about time and the need to return for a follow-up were not reflected in caregivers’ responses. Rather, caregivers in both study arms saw the follow-up visit as being beneficial to the health of their child.
(…) my wish is to see my child healthy and taking [the child] there [to the HP] again has an advantage. It is for the sake of my child’s health and I want her to be healthy. (Caregiver ID 7)
A conditional follow-up advising mothers to only come back after 2 days if the child’s fever persists was perceived as being valuable in that it reduced the number of visits to health facilities (health center or HP). This was linked to reducing long travels to health facilities, as well as saving time and costs for the caregivers, as this mother explains:
It [the recommendation] was good and I accepted her [HEW’s] advice happily. If she had advised me to go to the [name of] health center or to the other health facility I would have not been happy because I didn’t have money for the transportation. So it would worry me; but rather than referring me to these health facilities, she gave me the service and told me to come back on the second day if the fever is continuing. So when she advised me to come back [to the HP] it saved me from spending my money and it also reduced my worries. (Caregiver ID 1, conditional follow-up arm)
DISCUSSION
The findings of this study indicate that HEWs have begun to recognize unclassified fever as a health condition in its own right and have started to pay more attention to fever in children generally since the project with its clear management guidelines was introduced. Communication about the meaning of an unclassified fever diagnosis and the nonnecessity of medical treatment became increasingly important over the time of the study. The clearer communication enabled HEWs to withhold medicines from children with unclassified fever because caregivers still believed their child was being taken care of.
The communication between health providers and patients about the purpose and result of mRDTs has previously been found to be poor.19,20 In addition, although since 2010 the recommendation has been that antimalarial medication should only be given when a case is confirmed positive,21 health workers still experience mistrust in mRDTs and insecurities about managing febrile children with negative mRDT results, thus often resorting to the use of antimalarials even when unnecessary.22–25 It has been described that showing the test result to patients can help increase patients’ trust and that a lack of communication about the test can lead to a patient misinterpreting its result.20 Thus, particularly for negative malaria test results and low fever, where according to iCCM no medication should be given, clear communication to caregivers of sick children becomes important. This could potentially prevent caregivers from believing that the HEW did not provide proper care and sent them home “empty handed.” An alternative approach to tackling the problem of caregivers perceiving their children to be given inappropriate care could be the provision of antipyretics to all mRDT-negative febrile children at the community level. However, medications are scarce in these settings, which is why this approach could be difficult to implement in practice.
In this study, one HEW described how she used the mRDT to provide a visualization of the results and thereby the absence of malaria to mothers. Furthermore, almost all HEWs named the condition of unclassified fever “fever without malaria” and explained to mothers the non-severity of this condition. Instead of prescribing medication, they advised them to return for a follow-up. Briefly explaining the condition of the child to caregivers in this way seemed to have helped HEWs and made them more satisfied with and confident about managing fever because caregivers were more accepting of what HEWs said and were less demanding about receiving drugs. Learning from this study, future training of health workers should strongly emphasize the importance of communicating with patients, especially when using diagnostic tests. Fever is often believed to be caused by malaria.26,27 Consequently, it is necessary that an explanation of mRDT test results, particularly when negative, becomes common practice. To increase health workers’ confidence in managing children with negative malaria tests, local illness management guidelines should include clear instructions on what to do in cases where no cause of fever can be identified, for instance, explaining to caregivers that the fever is not caused by malaria, that there is no need for medical treatment at the first visit, and that the caregiver should come back for a follow-up visit. The benefits of naming such a condition in which fever is present but no signs of malaria, diarrhea, pneumonia, or danger signs are found should be evaluated and discussed as well as providing caregivers with advice about how to manage it. It should additionally be clarified for these health workers that although unclassified fever mostly resolves itself, it can also be an indication of a more severe illness or infection that requires treatment. Therefore, the importance of the follow-up visit should be emphasized to identify severely ill children during the follow-up and refer them to the health center for further diagnosis and treatment.
Both the universal and the conditional follow-up recommendations were perceived to have advantages. Universal follow-up was described as providing an opportunity for a reassessment of the child’s progress and to provide caregivers with additional healthcare information, whereas conditional follow-up can save time and costs for health workers and caregivers/patients. These benefits are in line with the findings of a qualitative study conducted in the Democratic Republic of Congo in June 2016 (L. C. Mullany, personal communication, 2017), suggesting that the findings of this study are not applicable to the Ethiopian context only. However, statements about preferences for one recommendation over the other cannot be made from this study. Results from the cRCT, in which this study was nested in, will evaluate the safety aspect of these recommendations and further feed into the discussion on the most appropriate follow-up recommendation. The findings are published elsewhere.15
An advantage of this study is that it included HEWs and mothers, providing an insight into similarities and differences between the two perspectives. The occurrence of a desirability bias cannot be excluded with certainty, particularly when asking about the follow-up recommendations within the trial. However, because of the fact that the HEWs’ reported follow-up practices corresponded with caregivers’ responses, we do believe that HEWs largely provided accurate information. Nevertheless, it must be pointed out that almost all HEWs reported only advantages of the two follow-up recommendations and almost none reported flaws. Furthermore, the interviews were conducted by male interviewers, whereas all interviewees (HEWs and caregivers) were female. However, we could not find any indication that this affected the findings of this study. This study provides insights into perceptions and management of children with unclassified fever, as well as corresponding follow-up recommendations. Health workers’ perceptions of healthcare recommendations are important for any guideline’s success. Therefore, these should be considered when reviewing and revising guidelines for the management of unclassified fever.
CONCLUSION
Awareness of the presence of fever not associated with malaria, pneumonia, or diarrhea is important in managing febrile children at community level. Nevertheless, knowledge about unclassified fever can be low in community settings and corresponding guidelines ambiguous, making it more difficult for health workers to appropriately manage these febrile children. Findings of this study show that the recognition of the unclassified fever condition improved and that HEWs became more comfortable communicating the diagnosis to the caregivers and withholding unnecessary medications from these patients. Making amendments to guidelines for unclassified febrile illnesses, by for instance, including a certain diagnostic term and clearer management instructions, could help health workers in rural communities to more confidently manage these cases. The benefits of such amendments should be evaluated to advance fever management in low- and middle-income countries, in particular where malaria prevalence is reducing. Both the universal and conditional follow-up recommendations were seen as beneficial by HEWs and caregivers, although with different perceived advantages. Research findings of the quantitative part of this cRCT indicated that the conditional follow-up is non-inferior with the universal follow-up in this setting. This information, in addition to the perceptions of caregivers and health workers should launch a discussion on the need to revise the follow-up recommendations for different contexts. In Ethiopia, it already is common practice to recommend a conditional follow-up (a follow-up only in case symptoms continue) at community level for children with unclassified fever. It might be a more efficient way of using resources to allow CHWs in countries with similar settings to use this recommendation as well.
Acknowledgments:
We thank the Federal Ministry of Health in Ethiopia, the Regional Health Bureau in SNNPR (in particular, our technical advisor, Habtamu Beyene), and the woreda offices in Damot Gale, Boloso Sore, and Halaba. We extend our thanks to all the health extension workers and mothers we interviewed for granting us their time and sharing their experiences. We would further like to acknowledge Anteneh Sebsibe, Belayneh Fekene, and Misganu Endrias for conducting the interviews.
REFERENCES
- 1.WHO, UNICEF , 2012. WHO/UNICEF JOINT STATEMENT Integrated Community Case Management (iCCM). An Equity-Focused Strategy to Improve Access to Essential Treatment Services for Children. Geneva, Switzerland/New York, NY: Word Health Organization and The United Nations Children’s Fund. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wharton-Smith A, Counihan H, Strachan C, 2014. Implementing Integrated Community Case Management: Stakeholder Experience and Lessons Learned in Three African Countries London, United Kingdom: Malaria Consortium. Available at: http://www.malariaconsortium.org/learningpapers. Accessed August 2, 2017.
- 3.WHO, UNICEF , 2005. Handbook IMCI: Integrated Management of Childhood Illness. Geneva, Switzerland: World Health Organization. [Google Scholar]
- 4.Dagan R, Sofer S, Phillip M, Shachak E, 1988. Ambulatory care of febrile infants younger than 2 months of age classified as being at low risk for having serious bacterial infections. J Pediatr 112: 355–360. [DOI] [PubMed] [Google Scholar]
- 5.Avner JR, 2009. Acute fever. Pediatr Rev 30: 5. [DOI] [PubMed] [Google Scholar]
- 6.Elfving K, Shakely D, Andersson M, Baltzell K, Ali AS, Bachelard M, Falk KI, Ljung A, Msellem MI, Omar RS, 2016. Acute uncomplicated febrile illness in children aged 2–59 months in Zanzibar–aetiologies, antibiotic treatment and outcome. PLoS One 11: e0146054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.D’Acremont V, Kilowoko M, Kyungu E, Philipina S, Sangu W, Kahama-Maro J, Lengeler C, Cherpillod P, Kaiser L, Genton B, 2014. Beyond malaria—causes of fever in outpatient Tanzanian children. N Engl J Med 370: 809–817. [DOI] [PubMed] [Google Scholar]
- 8.WHO, UNICEF , 2011. Caring for the Sick Child. Caring for Newborns and Children in the Community—A Training Course for Community Health Workers. Geneva, Switzerland. [Google Scholar]
- 9.Ethiopia Ministry of Health , 2011. Integrated Management of Newborn and Childhood Illness, Part 1 Addis Ababa, Ethiopia: Ethiopia Federal Ministry of Health. Available at: http://www.open.edu/openlearncreate/pluginfile.php/71990/mod_resource/content/2/IMNCI_Part_1_Final_Print-ready_March_2011_.pdf.
- 10.World Health Organization , 2009. Caring for the Sick Child in the Community: Participant’s Manual Geneva, Switzerland: World Health Organization. Available at: http://apps.who.int/iris/bitstream/10665/44398/1/9789241548045_Manual_eng.pdf.
- 11.Tong A, Sainsbury P, Craig J, 2007. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 19: 349–357. [DOI] [PubMed] [Google Scholar]
- 12.Al-Almaie SM, 1999. The reliability of mothers to assess the presence of fever in their children. Saudi Med J 20: 696–698. [PubMed] [Google Scholar]
- 13.Verhoef H, Hodgins E, West CE, Carter JY, Kok FJ, 1998. Diagnosis of fever in Africa. Lancet 351: 372–373. [DOI] [PubMed] [Google Scholar]
- 14.Källander K, Alfvén T, Abebe A, Hailemariam A, Petzold M, Getachew D, Barat L, Steinhardt LC, Gutman JR, 2018. Universal versus conditional 3-day follow-up visit for children with unclassified fever at the community level in Ethiopia: study protocol for a cluster randomized controlled non-inferiority trial. JMIR Res Protoc 7: e99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Källander K, Alfvén T, Funk T, Abebe A, Hailemariam A, Petzold M, Getachew D, Steinhardt LC, Gutman JR, 2018. Universal versus conditional 3-day follow-up for children with non-severe unclassified fever at the community level in Ethiopia: a cluster randomised, noninferiority trial. PLoS Med 15: e1002553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bilal NK, Herbst CH, Zhao F, Soucat A, Lemiere C, 2011. Health extension workers in Ethiopia: improved access and coverage for the rural poor. Chuhan-Pole P, Angwafo M, eds. Yes Africa Can: Success Stories from a Dynamic Continent. Washington, DC: The World Bank, 433–443. [Google Scholar]
- 17.Legesse H, Degefie T, Hiluf M, Sime K, Tesfaye C, Abebe H, Kebede H, Pearson L, Kassaye A, Taylor M, 2014. National scale-up of integrated community case management in rural Ethiopia: implementation and early lessons learned. Ethiop Med J 52: 15–26. [PubMed] [Google Scholar]
- 18.Elo S, Kyngäs H, 2008. The qualitative content analysis process. J Adv Nurs 62: 107–115. [DOI] [PubMed] [Google Scholar]
- 19.Ansah EK, Reynolds J, Akanpigbiam S, Whitty CJ, Chandler CI, 2013. “Even if the test result is negative, they should be able to tell us what is wrong with us”: a qualitative study of patient expectations of rapid diagnostic tests for malaria. Malar J 12: 258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Altaras R, Nuwa A, Agaba B, Streat E, Tibenderana JK, Martin S, Strachan CE, 2016. How do patients and health workers interact around malaria rapid diagnostic testing, and how are the tests experienced by patients in practice? A qualitative study in western Uganda. PLoS One 11: e0159525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Health Organization , 2010. Guidelines for the Treatment of Malaria. Geneva, Switzerland: WHO. [Google Scholar]
- 22.Manyando C, Njunju EM, Chileshe J, Siziya S, Shiff C, 2014. Rapid diagnostic tests for malaria and health workers’ adherence to test results at health facilities in Zambia. Malar J 13: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mubi M, Kakoko D, Ngasala B, Premji Z, Peterson S, Björkman A, Mårtensson A, 2013. Malaria diagnosis and treatment practices following introduction of rapid diagnostic tests in Kibaha district, coast region, Tanzania. Malar J 12: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johansson EW, 2016. Beyond “test and treat”: malaria diagnosis for improved pediatric fever management in sub-Saharan Africa. Glob Health Action 9: 31744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johansson EW, Kitutu FE, Mayora C, Awor P, Peterson SS, Wamani H, Hildenwall H, 2016. It could be viral but you don’t know, you have not diagnosed it: health worker challenges in managing non-malaria paediatric fevers in the low transmission area of Mbarara district, Uganda. Malar J 15: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hertz JT, Munishi OM, Sharp JP, Reddy EA, Crump JA, 2013. Comparing actual and perceived causes of fever among community members in a low malaria transmission setting in northern Tanzania. Trop Med Int Health 18: 1406–1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baltzell K, Elfving K, Shakely D, Ali AS, Msellem M, Gulati S, Mårtensson A, 2013. Febrile illness management in children under five years of age: a qualitative pilot study on primary health care workers’ practices in Zanzibar. Malar J 12: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]