ABSTRACT
Introduction
This guideline was developed to present current evidence and to provide associated clinical recommendations on prosthetic foot selection for individuals with lower-limb amputation.
Materials
NA
Methods
The guideline is based upon the best available evidence as it relates prosthetic foot selection during the provision of definitive lower-limb prostheses. Where possible, recommendations are drawn from Cochrane Review, meta-analysis, systematic and narrative literature reviews, and published evidence-based guidelines. Where this standard is unavailable, alternate academic literature has been used to support individual recommendations.
Results
Recommendation 1: For patients ambulating at a single speed who require greater stability during weight acceptance because of weak knee extensors or poor balance, a single-axis foot should be considered. Recommendation 2: Patients at elevated risks for overuse injury (i.e., osteoarthritis) to the sound-side lower limb and lower back are indicated for an energy-storage-and-return (ESAR) foot to reduce the magnitude of the cyclical vertical impacts experienced during weight acceptance. Recommendation 3: Neither patient age nor amputation etiology should be viewed as primary considerations in prosthetic foot type. Recommendation 4: Patients capable of variable speed and/or community ambulation are indicated for ESAR feet.
Conclusions
These clinical practice guidelines summarize the available evidence related to prosthetic foot selection for individuals with lower limb amputation. The noted clinical practice guidelines are meant to serve only as “guides.” They may not apply to all patients and clinical situations.
KEY INDEXING TERMS: prosthetic foot, lower-limb amputation, transtibial, transfemoral, practice guideline, systematic review, energy storing foot
Of the 1.6 million persons living in the United States with limb loss, approximately 1.3 million (86%) have an amputation of the lower limb.1,2 These individuals vary tremendously with respect to age, sex, amputation level, and etiology, comorbid health conditions, physical presentation, ambulatory potential, and daily activity levels. Accordingly, a range of prosthetic foot types have been developed to reflect this variation, allowing for the appropriate pairing of prosthetic foot type to end user.
The prosthetic foot is an integral component of any lower-limb prosthesis after major lower-limb amputation (i.e., ankle disarticulation level or proximal). In attempting to best restore the functionality previously provided by the anatomical foot and ankle, prosthetic feet have many mechanical design variations. For example, design features attempt to replicate the shock absorption associated with loading response, the coronal adaptations experienced in midstance, the rigid forefoot leverage required in terminal stance, and the propulsion associated with terminal stance through preswing. These functions are pursued through a number of mechanisms, including mechanical joint axes, compressive foams, and bumpers. In addition, many feet now have elastic materials designed to deform under load and then return to their original shape, releasing the energy stored during deformation to provide power to the gait cycle. The costs associated with prosthetic foot types vary with the technologies used to meeting these functional goals.
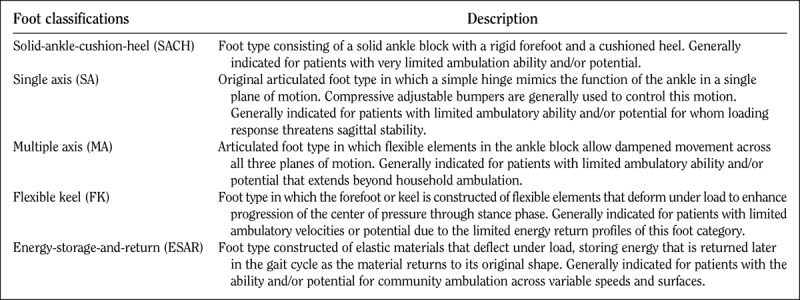
The number of prosthetic feet available within the rehabilitation community can be overwhelming. However, prosthetic feet are generally classified into several key categories reflecting basic differences in technologies, functional performance limitations, and costs (Table 1).3 The solid-ankle-cushion-heel (SACH) foot is the simplest category of prosthetic foot consisting of a solid ankle block with a rigid forefoot and a compressive material within the heel. The single-axis foot integrates a single mechanical hinge to replicate the function of the ankle joint in the sagittal plane. The multiple-axis foot includes flexible elements to allow dampened movement in all planes of motion. The flexible-keel foot introduces flexible elements to the forefoot of the prosthesis to enhance the sagittal progression of the center of pressure through stance phase. A broad category of energy-storage-and-return (ESAR) feet is constructed of elastic materials that deform under load, storing potential energy that is released later in the gait cycle when these elements return to their original shape.3
Table 1.
Basic prosthetic foot categories for lower-limb prostheses3
Clinical practice guidelines (CPGs) are increasingly common in health care, with the US Agency for Healthcare Research and Quality (AHRQ) now housing over 1700 practice guidelines in its National Guideline Clearinghouse.4 Yet, the field of orthotics and prosthetics is underrepresented in this area, with only a single CPG listed in the AHRQ database. Encouragingly, the field has begun to develop and publish practice guidelines across a range of care episodes including the management of plagiocephaly,5 postoperative care after transtibial amputation,6 prosthetic foot selection for individuals with lower-limb amputation,7 prescription guidelines for microprocessor-controlled prosthetic knees in the South East England,8 and a two-part “Dutch evidence-based guidelines of amputation and prosthetics of the lower extremity.”9,10
The scope and depth of CPGs are variable, with direct implications on their resultant clinical relevance and ultimate incorporation into practice. The current effort is modeled after the CPGs of the American College of Physicians,11 with necessary adaptations to accommodate the emerging evidence base of orthotic and prosthetic care. The stated goals of this approach are to “provide clinicians with clinical based guidelines based upon the best available evidence; to make recommendations on the basis of that evidence; to inform clinicians of when there is no evidence; and finally, to help clinicians deliver the best health care possible.”11(p194)
Clinical utility is of paramount importance in this effort, culminating in a small number of succinct, actionable, evidence-based recommendations.12 Notably, within this framework, although the resultant CPGs represent a comprehensive overview of available literature, deficits in the available literature preclude CPGs within this framework from providing comprehensive clinical guidance.
The purpose of this guideline is to present the available evidence with respect to determining the most appropriate prosthetic foot type for individuals with lower-limb amputation in consideration of their clinical presentation. The target audience for this guideline includes prosthetists, surgeons, physicians, physical therapists, and policy makers. The target patient population comprises individuals who have experienced major lower-limb amputation (i.e., ankle-disarticulation level or proximal), who have experienced adequate healing at the primary wound site to permit prosthetic fitting, and who have the desire and potential or demonstrated ability to ambulate with a prosthesis.
A Medline search was conducted on through April 2016 to locate sources of evidence statements within the published literature. The following search terms were used: “lower limb amputation” AND “prosthesis,” “prosthetic feet” OR “components,” AND “systematic review” OR “meta-analysis.” This search yielded 96 abstracts. Of these, four papers were identified as secondary knowledge sources (i.e., meta-analysis, systematic review, or evidence-based guidelines) that synthesized published findings of primary knowledge related to the performance characteristics of prosthetic foot types. These publications include a Cochrane Review,13 published national evidence-based guidelines,10 a systematic review,6 and an evidence-based narrative review and meta-analysis.14 An additional recent systematic review with meta-analysis that had not yet been indexed but had been published was also identified and included.15
In more recent publications, where authors provided explicit evidence statements, these were extracted for subsequent synthesis. If explicit evidence statements were not provided, well-supported narrative statements were extracted. Extracted statements are summarized in Table 2. Statements addressed the following key considerations:
Table 2.
Evidence statements taken from secondary knowledge sources
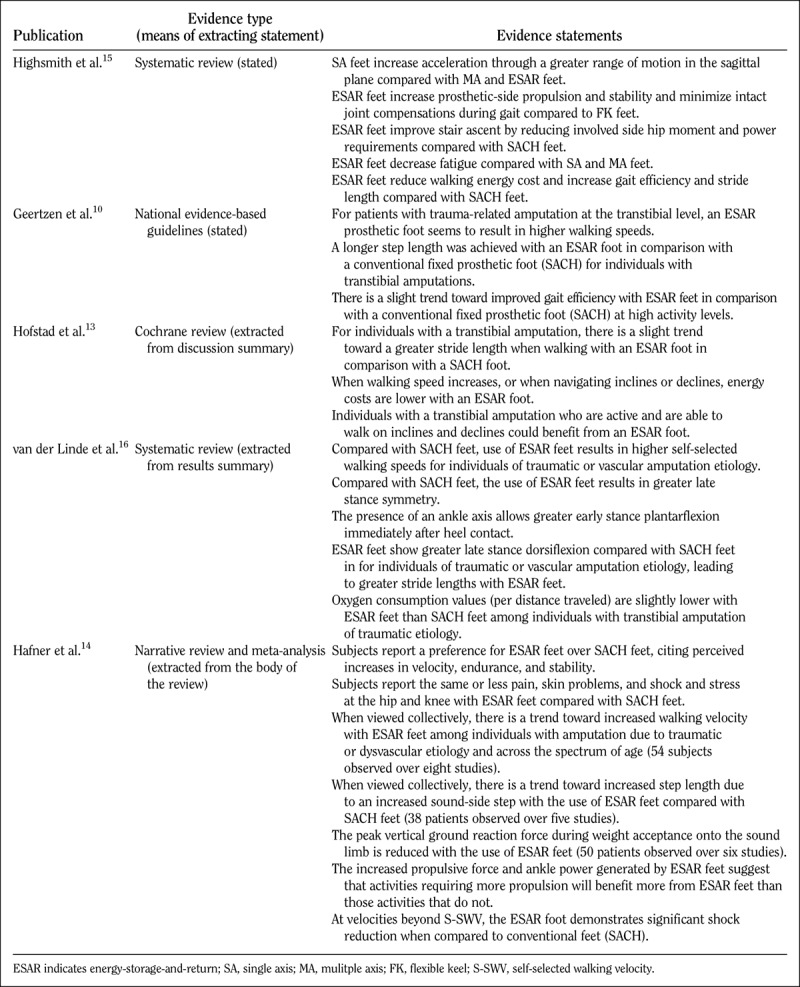
Comparative effectiveness: Where available, statements related to the comparative efficacy of various foot types were extracted from secondary knowledge sources.
Benefits of treatments: Benefits described in the evidence base include such considerations as self-selected walking velocity, increased stride length, favorable kinematics and kinetics, metabolic improvements, and subjective benefits and preferences.
Harms of treatments: Harms described in the evidence base include the peak vertical impact forces experienced by the sound-side limb, residual limb pain, skin problems and shock and stress at the hip and knee.
COMPARATIVE EFFECTIVENESS
Statements of comparative efficacy have largely been drawn between ESAR feet and the other foot types described above and contained in Table 1.
BENEFITS
The benefits associated with prosthetic foot types are shown in Table 2 with their sources of evidence. In general, the SACH foot has served as the base of comparison for other foot types. The benefits associated with the single-axis foot type include its ability to rapidly accommodate the ground in the sagittal plane with attendant benefits to stability during loading response.15,16 To the extent that multiple-axis and flexible-keel feet have been represented in secondary knowledge sources, they are seen as a base of comparison for ESAR feet. A single secondary knowledge publication has addressed the benefits of multiaxial ankle function when such elements are attached proximally to a range of prosthetic feet.15
The benefits of ESAR feet include increases in self-selected walking speed10,14,16 and both perceived and measured improvements in walking efficiency.14–16 Favorable gait measures include an extended stride length.10,14–16 Favorable kinetics include increased propulsive properties and walking efficiency during level-ground ambulation,15 the negotiation of environmental obstacles such as stairs and ramps,13,15 and at elevated activity levels.10,13,14
HARMS
The potential harms associated with prosthetic foot type in secondary knowledge sources include both objective measurements and patient-reported outcomes. The magnitude of the initial peak vertical ground reaction force on the sound-side limb has been observed to decrease with the use of ESAR feet.14 Such forces have been often associated with overuse strain and injury to the contralateral limb.17 These objective findings are reinforced by patient-reported outcomes of decreased limb pain, skin problems, and shock or stress at the hip and knee with the use of ESAR feet.14
CONSIDERATIONS BY PATIENT TYPE
The benefits ascribed to single-axis feet are limited to those patients with limited ambulatory ability and/or potential whose sagittal plane stability is threatened during loading response. There is no evidence to suggest that this is a beneficial characteristic for more active walkers with adequate strength and balance. Similarly, the benefits of ESAR feet are largely confined to observations during level-ground walking at active walking velocities, elevated walking speed and activity levels, or during the negotiation of ramps and stairs.
RECOMMENDATIONS
Recommendation 1: For patients ambulating at a single speed who require greater stability during weight acceptance because of weak knee extensors or poor balance, a single-axis foot should be considered.
Studies suggest a more rapid sagittal plane rotational acceleration of the foot about the ankle during weight acceptance with the use of a single-axis foot, bringing the prosthetic foot into full contact with the floor more quickly than other prosthetic foot options.15,16 This increased surface area may provide greater stability to those patients with poor balance. In addition, this ankle movement draws the ground reaction force anteriorly, reducing the magnitude of the external knee flexion moment during weight acceptance. This reduces the likelihood of a knee-buckling event, creating a more stable environment for users with weak knee extensors or transfemoral prostheses. However, the abrupt plantarflexion observed with simple single-axis feet may compromise the progression of the center of pressure through stance phase, disrupting the smoothness of gait among patients capable of elevated and/or variable speeds of ambulation.
Recommendation 2: Patients at elevated risks for overuse injury (i.e., osteoarthritis) to the contralateral lower limb and lower back are indicated for an ESAR foot to reduce the magnitude of the cyclical vertical impact forces experienced during weight acceptance.
Studies suggest consistent reductions in the peak ground reaction force experienced by the sound-side limb during weight acceptance with the use of ESAR feet.14 Patients with higher risks for overuse injury because of elevated activity levels, greater self-selected walking velocities, or younger age (thus anticipating comparatively more years of prosthetic ambulation) stand to benefit the most from the reduced loading forces associated with ESAR feet. Self-report outcomes of decreased pain, skin problems, shock, and stress at the hip and knee with the use of ESAR feet are consistent with these laboratory findings.14 The shock-absorbing characteristics of ESAR feet seem to be more apparent at speeds exceeding self-selected walking velocities.14 Likely contributions to the mechanism of impact reduction include consistent observations of increased propulsion from ESAR feet14,15 and greater tibial progression into terminal stance without sacrificing ankle moment,16 both of which collectively reduce the dropoff from the prosthetic foot onto the contralateral limb at the conclusion of the prosthetic step.
Recommendation 3: Neither patient age nor amputation etiology should be viewed as primary considerations in prosthetic foot type.
Several of the comparative benefits associated with ESAR feet relative to alternate feet designs, including elevated self-selected walking speeds and greater limb symmetry in terminal stance, have been observed among patients with both traumatic and dysvascular amputation etiologies.14,16 Therefore, amputation etiology does not in itself seem to limit the potential beneficial effects associated with ESAR feet. Similarly, studies suggest that the benefits of ESAR feet in increasing self-selected walking speed seem to encompass a broad age range and may be independent of either amputation etiology or age.14
Recommendation 4: Patients capable of variable speed and/or community ambulation are indicated for ESAR feet.
Compared with the other foot designs described in Table 1, ESAR feet have been associated with both perceived and measured increases in self-selected walking speeds.10,14,16 Studies suggest that this may be the result of increased step length, predominantly in the step length of the contralateral limb.10,13,14 Users have subjectively reported increased stability with this foot type relative to other prosthetic foot categories.14,15 This willingness to increase contralateral step length relative to other foot designs may reflect the user's increased perceived stability when using an ESAR feet.
Lengthening the contralateral step may partially explain the modest reductions experienced in reported and measured oxygen cost, which is the energy expelled to traverse a given distance.14–16 The comparative benefits of ESAR feet with respect to reduced energy costs of ambulation are more pronounced at elevated walking speeds,13 during the negotiation of inclines and declines,13 and during stair ascent.15
INCONCLUSIVE AREAS OF EVIDENCE
Most of the published literature on prosthetic foot design consists largely of comparative efficacy trials between SACH feet and ESAR feet. Single-axis, multiple-axis, and flexible-keel feet, although utilized in prosthetic rehabilitation, are underrepresented in the academic literature. Despite high volumes of use of these foot types, the scientific community has lagged behind in reporting empirical evidence that may coincide or refine anecdotal evidence. Lacking any empirical evidence, the flexible-keel foot type in particular lacks the objective support to justify its specific mention in the guideline beyond its current mention as an existing category of prosthetic foot.
More recent prosthetic foot technologies, including hydraulic ankle-foot units, microprocessor-regulated ankle/feet, and externally powered propulsive ankle/feet continue to emerge in both prosthetic rehabilitation and its associated evidence base. However, these were not included within the scope of the source publications or the resultant CPG. Supplements to prosthetic feet, including vertical shock pylons and multiple-axis ankle units, have received limited treatment within secondary knowledge sources but were not included within the scope of this review.
Importantly, it is recognized that patients are individuals with unique presentations. As such, the noted clinical practice guidelines are meant to serve only as “guides.” They may not apply to all patients and clinical situations. Thus, they are not intended to replace clinical judgment. In addition, it is recognized and planned that the clinical practice guidelines will need to be updated as new evidence emerges surrounding prosthetic feet.
Footnotes
Disclosures: The authors are current employees of Hanger Clinic and received no external funding for the purposes of this work.
REFERENCES
- 1.Dillingham T, Pezzin L, MacKenzie EJ. Limb amputation and limb deficiency: epidemiology and recent trends in the United States. South Med J 2002;95:875–883. [DOI] [PubMed] [Google Scholar]
- 2.Ziegler-Graham K, MacKenzie EJ, Ephraim PL, et al. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil 2008;89(3):422–429. [DOI] [PubMed] [Google Scholar]
- 3.Michael JW, Stevens PM. Lower limb prosthetic components: updated classification and passive, body-powered components. In: Krajbich JI, Pinzur MS, Potter BK, Stevens PM. (Eds.) Atlas of Amputations and Limb Deficiencies: Surgical, Prosthetic, and Rehabilitation Principles. 4th Ed American Academy of Orthopedic Surgeons: Rosemont, IL; 2015:429–443. [Google Scholar]
- 4.US Department of Health and Human Services, Agency for Healthcare Quality and Research. National Guideline Clearinghouse. Available at: https://www.guideline.gov/browse/clinical-specialty. Accessed September 8, 2017.
- 5.Lin RS, Stevens PM, Wininger M, Castiglione CL. Orthotic management of deformational plagiocephaly: consensus clinical standards of care. Cleft Palate Craniofac J 2016;53(4):394–403. [DOI] [PubMed] [Google Scholar]
- 6.Stevens P, Rheinstein J, Campbell J. Acute postoperative care of the residual limb following transtibial amputation: a clinical practice guideline. Arch Phys Med Rehabil 2016;97:e21. [Google Scholar]
- 7.Stevens P, Rheinstein J, Wurdeman S. Prosthetic foot selection for individuals with lower limb amputation: a clinical practice guideline. Arch Phys Med Rehabil 2016;97:e21–e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sedki I, Fisher K. Developing prescribing guidelines for microprocessor-controlled prosthetic knees in the South East England. Prosthet Orthot Int 2015;39(3):250–254. [DOI] [PubMed] [Google Scholar]
- 9.Geertzen J, van der Linde H, Rosenbrand K, et al. Dutch evidence-based guidelines for amputation and prosthetics of the lower extremity: amputation surgery and postoperative management. Part 1. Prosthet Orthot Int 2015;39(5):351–360. [DOI] [PubMed] [Google Scholar]
- 10.Geertzen J, van der Linde H, Rosenbrand K, et al. Dutch evidence-based guidelines for amputation and prosthetics of the lower extremity: rehabilitation process and prosthetics, part 2. Prosthet Orthot Int 2015;39(5):361–371. [DOI] [PubMed] [Google Scholar]
- 11.Qaseem A, Snow V, Owens DK, et al. The development of clinical practice guidelines and guidance statements of the American College of Physicians: summary of methods. Ann Intern Med 2010;153:194–199. [DOI] [PubMed] [Google Scholar]
- 12.Qaseem A, Humphrey LL, Forciea MA, et al. Treatment of pressure ulcers: a clinical practice guideline from the American College of Physicians. Ann Intern Med 2015;162:370–379. [DOI] [PubMed] [Google Scholar]
- 13.Hofstad CJ, Linde H, Limbeek J, Postema K. Prescription of prosthetic ankle-foot mechanisms after lower limb amputation (Review). Cochrane Database Syst Rev 2004;(1):CD003978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hafner BJ, Sanders JE, Czerniecki J, Fergason J. Energy storage and return prostheses: does patient perception correlate with biomechanical analysis? Clin Biomech (Bristol, Avon) 2002;17:325–344. [DOI] [PubMed] [Google Scholar]
- 15.Highsmith MJ, Kahle JT, Miro RM, et al. Prosthetic interventions for people with transtibial amputation: systematic review and meta-analysis of high-quality prospective literature and systematic reviews. J Rehabil Res Dev 2016:53(2):157–184. [DOI] [PubMed] [Google Scholar]
- 16.van der Linde H, Hofstad CJ, Geurts AC, et al. A systematic literature review of the effect of different prosthetic components on human functioning with a lower-limb prosthesis. J Rehabil Res Dev 2004;41(4):555–570. [DOI] [PubMed] [Google Scholar]
- 17.Gailey R, Allen K, Castles J, et al. Review of secondary physical conditions associated with lower-limb amputation and long-term prosthesis use. J Rehabil Res Dev 2008;45(1):15–29. [DOI] [PubMed] [Google Scholar]


