Abstract
Posttraumatic bone defects (BDs) remain a difficult complication for orthopaedic surgeons. Surgical goals in these reconstructive cases are to create stable limb fixation, maintain limb length, and provide adequate soft-tissue coverage. Historically, surgical approaches in these cases have required the use of an external fixator, which is associated with several postoperative complications. A plate-assisted bone segment transport (PABST) technique using a magnetic limb lengthening system eliminates the need for an external fixator and is effective for these reconstructive cases. A 51-year-old male patient presented as a category I trauma after a motorcycle collision. Osseous injury was defined as Gustilo-Anderson type IIIB distal tibia and fibula fracture (AO 42-C2). After fixation failure, the PABST technique was performed using a magnetic intramedullary limb lengthening system. Radiographic union was achieved 18 months postoperatively. This innovative surgical technique is effective in treating posttraumatic BDs without the need for limb shortening or the use of an external fixator. PABST has the potential to decrease postoperative complications in BD reconstructive cases using all-internal technology designed for limb lengthening. PABST, in this instance, uses a magnetic intramedullary nail that is controlled with a hand-held external remote to allow for precise, adjustable, and bidirectional bone segment transport.
Long bone defects (BDs) usually follow high-energy trauma and are often associated with notable soft-tissue injury. Historically, the reconstruction of posttraumatic BD has relied on a number of surgical techniques including conventional and vascularized bone grafting, induced-membrane techniques, and several variations of bone transport.1,2,3 These variations of bone transport were developed on the principles of distraction osteogenesis pioneered by Ilizarov and refined by Cattaneo et al and Catagni et al.4,5,6 Since its inception, the Ilizarov method of bone transport has become common practice in reconstructive surgery for limb lengthening and management of BD. However, despite the physiologic nature of this method of bone transport, it involves the use of an external fixation device, which is associated with pin tract infections and decreased range of motion secondary to joint contractures.1,7,8,9
Recent advances in technology have allowed for less invasive approaches. To eliminate the need for external fixation devices, several intramedullary (IM) nail lengthening systems have been developed. However, issues have been encountered with these devices related to weakness or mechanical instability of the IM nail, difficulty controlling rate of lengthening, pain with distraction, or deep bone infections.8,9,10,11,12 Other described techniques for managing long BDs include lengthening over a nail, lengthening over a plate, definitive external fixation, conventional and vascularized bone grafting, and the Masquelet technique.1,2,3,10,11,12,13,14
Recently, the PRECICE 2 IM Limb Lengthening System (NuVasive), which relies on a noninvasive magnetic interaction between the IM nail and an external, portable, hand-held remote controller, was designed to allow for accurate lengthening of the tibia or femur.15 The PRECICE 2 IM nail is available in four predistraction lengths: 195, 215, 230, and 245 mm. The 245 mm nail has a telescoping rod that allows for 80 mm of lengthening; the remaining nails have a telescoping rod that allows for 50 mm of lengthening. In contrast to previous approaches using motorized IM nails and skeletal kinetic distractors,16,17 this system may prove to be a more precise distraction system and is capable of bidirectional control, which allows for distraction and also compression of the bone regenerate (ie, the accordion technique).4,18,19,20 However, to the knowledge of the authors, there has been no documented use of the PRECICE 2 IM Limb Lengthening System to correct a BD via segmental bone transport without shortening or concurrent use of an external fixation device. This case report is an account of a novel, plate-assisted bone segment transport (PABST) technique using the only IM limb lengthening system currently approved for use in the United States.
Case Report
The patient is a 51-year-old man with no notable medical history who was admitted as a category I trauma after a motorcycle versus car collision. The patient's injuries included a Gustilo-Anderson type IIIB distal tibia and fibula fracture (AO 42-C2) with intact neurovascular examination (Figure 1). Soft-tissue injury included a posteromedial wound at the distal third of the tibia measuring approximately 14.5 × 10 cm with exposed bone. Many surgical interventions were needed to achieve soft-tissue coverage, and a Synthes IM nail was placed during the course of management to provide skeletal stability, maintain length, and allow for unobstructed flap placement. At the patient's request for no further surgery, he was allowed to weight bear as tolerated and gradually return to activities, but he was informed that the nail would likely fail, and if this were to happen, some type of bone graft or transport would be required in the future. Ultimately, there was minimal callus formation, and failure of distal tibia fixation occurred 2 years after the original injury. The defect was estimated to be 3.0 cm after removal of hardware (Figure 2, A and B). Surgical options were discussed, and PABST was chosen.
Figure 1.
AP (A) and lateral (B) radiographs at initial injury.
Figure 2.
A, AP radiograph showing nail fixation failure. B, Intraoperative fluoroscopic image showing residual tibial defect after fibula fixation.
One week after fixation failure, the patient presented for removal of his failed IM nail, débridement of his nonunion, open reduction and internal fixation of his tibia, and fibula and placement of the PRECICE 2 IM Limb Lengthening System (Figure 3).
Figure 3.
AP (A) and lateral (B) radiographs of the plate-assisted bone segment transport construct with the PRECICE 2 IM nail in place.
Description of the Plate-assisted Bone Segment Transport Technique
The proximal portion of the nail was explanted without complications. An anterior incision was made over the tibial nonunion site medial to the flap, and dissection was continued down to the fracture site. The distal interlock bolts were removed, and the distal nail was explanted. An osteotomy of the distal tibial nonunion was then performed using an oscillating saw on low speed with continuous irrigation and frequent breaks to minimize thermal necrosis. The distal osteotomy sites (ie, the docking surfaces) should be flat and parallel with the ankle joint to improve surface area contact on docking and to help with proper alignment. Callus over the fibula was then carefully débrided with a rongeur. The fibular ends were then débrided to provide a good compressible construct. Alignment of the fibula helped establish the length, alignment, and rotation for the construct. A Synthes 10-hole limited-contact dynamic compression plate was applied in compression with two cortical and two locking screws at each end of the fracture site. After débridement and reduction of the fibula, the residual tibial defect was measured at 2.5 cm (Figure 2, B). Next, a medial Synthes distal tibia plate was placed across the fracture, sliding this proximal in a subcutaneous fashion to maintain soft-tissue integrity. The purpose of the plate was to maintain limb alignment during transport. A Synthes 16-hole variable-angle limited contact plate was the longest plate available to span the defect. The plate was secured distally with a combination of cortical and locking screws but was not yet fixed proximally to allow for the proximal corticotomy. With the fibula fixed and residual tibial defect established, nail parameters were then determined. The authors planned to place the distal interlock as close to the defect as possible to reduce the potential of transport segment drift. Therefore, a 245-mm nail with an 80-mm telescoping rod was selected to place the distal interlock as close to the defect as possible without sacrificing lengthening reserve. Nail diameter was chosen to achieve a good IM fit and reduce friction for the transport segment. With an infrapatellar approach, the tibial canal was reamed up to 10.5 mm, and an 8.5-mm-diameter nail was selected. A diaphyseal corticotomy was then performed, as described by De Bastiani et al,18 using a 3.5-mm drill bit and finishing with an osteotome to prevent thermal injury. This procedure was performed 8 cm proximal to the defect site to allow for placement of four tibia plate proximal locking screws in the stationary piece. The nail was then placed in the canal and advanced distally past the corticotomy site, and a proximal interlock bolt was placed. The PRECICE 2 IM nail has three distal locking options: one AP and two medial-lateral (ML). The plan for the medial plate precluded the ML screws. Rotating the nail was considered; however, we chose not to place the ML screws because of the potential for contact between the screws and the medial plate during transport and the possibility of creating a proximal deformity. Therefore, a single AP distal interlocking bolt was placed to engage the transport segment. With distal locking screws already in place, the medial tibia plate was secured proximally with four bicortical locking screws that were placed anterior to the nail. To assess completion of the corticotomy, the nail was lengthened intraoperatively, and the transport segment was confirmed to move by comparing pre- and post-distraction fluoroscopic images.
Patient Progress
The patient was given instructions to be non–weight bearing on his surgical leg after surgery. His surgical wounds healed uneventfully. Lengthening began on postoperative day (POD) 7 and proceeded at a rate of 0.75 mm per day for 32 days (2.4 cm). The regenerate appeared underdeveloped, and on POD 39, the accordion technique as described by Makhdom19 was performed by placing the magnet in the reverse direction at a rate of 0.5 mm per day for 40 days (2.0 cm). Once that was done, distraction was resumed at a rate of 0.5 mm per day for 40 days (2.0 cm). On POD 120, the docking site was then prepared by débridement with a curet and rongeur without complications. The final rate of distraction was slowed to 0.25 mm per day to maximize regenerate development and was continued until POD 128 when the distal interlocking bolt was seen to have a bend in it. The patient was permitted to return to weight-bearing activities with physical therapy on POD 156 when the regenerate appeared mature.
Bone segment docking was noted radiographically on POD 128; however, 6 months later, the docking site showed resorption, indicating a nonunion. The regenerate was mature, and it was determined that compression with the PRECICE 2 nail would not work at this point. Ten months after placement, the PRECICE 2 nail was removed along with the medial plate, and a Synthes IM nail was placed along with iliac crest autograft to augment docking site consolidation. The patient showed increased callus formation at every visit following this procedure up until radiographic union. The consolidation index was 56.9 (d/cm) as assessed on plain radiographs, and radiographic union of the docking site occurred at 18 months after PRECICE 2 IM nail placement (Figure 4).
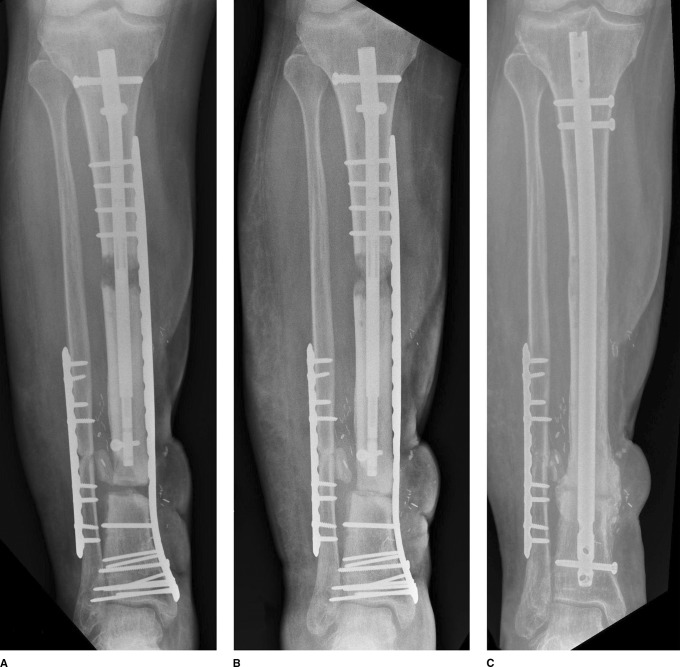
Figure 4.
Radiographs showing stages of healing at 3 months (A), 8 months (B), and 18 months (C), as seen on AP radiographs.
Discussion
The BD described in this report was noted initially to be 4.2 cm, which if managed according to the criteria outlined by Rigal et al1 could have been initially shortened and then lengthened by distraction osteogenesis with a distant corticotomy site. However, in this case, the length and alignment were maintained by plate fixation, and transport was performed using the PRECICE 2 IM Limb Lengthening System. This technique has several advantages: (1) it reduces the risk of joint stiffness and muscle contracture associated with an initial shortening and secondary lengthening;1,7,9 (2) it eliminates the need for an external fixation device, which is uncomfortable to patients and associated with several postoperative surgical complications; and (3) the magnetic device removes the need for a subcutaneous receiver antenna, therefore potentially removing a known source of failure.21,22
The PRECICE 2 magnetic IM nail allows for precision distraction and bidirectional control, which may allow for better control of the transport segment and a more successful bone regenerate outcome. The authors recognize that the PABST technique will continue to be refined but feel that the technique offers a feasible and effective solution to a complex posttraumatic condition for surgeons confronted with challenging BDs.
The PABST technique was successful in treating the segmental BD in this case. However, complications and areas for improvement have been identified. Poor growth in the regenerate was noted early in treatment, and one potential contributor was the diaphyseal location of the corticotomy. With this technique, the corticotomy site is dependent on the length of the plate. With the need to maintain the stationary and docking segments in proper alignment with the plate, the corticotomy site must be more distal than an ideal metaphyseal location. Another reason for slow regenerate development could have been that the transport rate was too fast in the beginning (0.25 mm 3 times daily), outrunning the regenerate, resulting in the need for the accordion technique. Ultimately, the regenerate did consolidate but took longer than anticipated. The second recognized complication was in achieving union at the docking site, and several issues may have contributed to this difficulty. In the initial procedure, an oscillating saw was used to osteotomize the nonunion site. Despite great care for bone biology and soft tissues, using an oscillating saw likely caused thermal necrosis at the docking site. Second, placing the nail as distal as possible may have reduced drift of the transport segment but may have also devitalized the endosteal blood supply needed for optimal health at the docking site. Third, the placement of only one screw in the transport segment may have also contributed to this issue. Although one screw was sufficient to support transport, more screws may have allowed for better compression once docked. Finally, in the procedure to prepare the docking site, iliac crest bone graft was not used. Autograft with iliac crest bone graft may have improved the chance of union at the docking site. The authors also feel that host factors may have played a notable role in the poor regenerate. Optimizing host biology by reviewing laboratory markers (vitamin D and calcium levels) and smoking cessation are important for success. Fortunately, this patient did comply with smoking cessation and dietary supplementation of vitamin D/calcium.
Ultimately, PABST offers surgeons an alternative approach to managing BDs. The use of a magnetic nail with bidirectional control has the potential to reduce complications regarding nail escape and early consolidation. It also allowed for precise monitoring and control of the regenerate and eliminated the need for external fixation devices. Future cohort studies will be needed to determine the reliability, complications, and advantages of this technique.
Footnotes
Dr. Gardner or an immediate family member is a member of a speakers' bureau or has made paid presentations on behalf of NuVasive and serves as a paid consultant to NuVasive. Neither of the following authors nor any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article: Dr. Barinaga and Dr. Beason.
References
References printed in bold type are those published within the past 5 years.
- 1.Rigal S, Merloz P, Le Nen D, Mathevon H, Masquelet AC: French Society of Orthopaedic Surgery and Traumatology (SoFCOT). Bone transport techniques in posttraumatic bone defects. Orthop Traumatol Surg Res 2012;98:103-108. [DOI] [PubMed] [Google Scholar]
- 2.Paley D, Catagni MA, Argnani F, Villa A, Benedetti GB, Cattaneo R: Ilizarov treatment of tibial nonunions with bone loss. Clin Orthop Relat Res 1989;241:146-165. [PubMed] [Google Scholar]
- 3.Masquelet AC, Begue T: The concept of induced membrane for reconstruction of long bone defects. Orthop Clin North Am 2010;41:27-37. [DOI] [PubMed] [Google Scholar]
- 4.Catagni MA, Geurreschi F, Lovisetti L: Distraction osteogenesis for bone repair in the 21st century: Lessons learned. Injury 2011;42:580-586. [DOI] [PubMed] [Google Scholar]
- 5.Ilizarov GA: Basic principles of transosseous compression and distraction osteosynthesis [Russian]. Ortop Traumatol Protez 1971;32:7-15. [PubMed] [Google Scholar]
- 6.Cattaneo R, Villa A, Catagni M, Tentori L: Treatment of septic or non-septic diaphyseal pseudoarthroses by Ilizarov's monofocal compression method. Rev Chir Orthop Reparatrice Appar Mot 1985;71:223-229. [PubMed] [Google Scholar]
- 7.Iacobellis C, Berizzi A, Aldegheri R: Bone transport using the Ilizarov method: A review of complications in 100 consecutive cases. Strategies Trauma Limb Reconstr 2010;5:17-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Paley D: Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res 1990;250:81-104. [PubMed] [Google Scholar]
- 9.Dahl MT, Gulli B, Berg T: Complications of limb lengthening: A learning curve. Clin Orthop Relat Res 1994;301:10-18. [PubMed] [Google Scholar]
- 10.EL-Husseini TF, Ghaly NAM, Mahran MA, Al Kersh MA, Emara KM: Comparison between lengthening over nail and conventional Ilizarov lengthening: A prospective randomized clinical study. Strategies Traum Limb Reconstr 2013;8:97-191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mahboubain S, Seah M, Fragomen AT, Rozbruch R: Femoral lengthening with lengthening over a nail has fewer complications than intramedullary skeletal kinetic distraction. Clin Orthop Relat Res 2012;470:1221-1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Song HR, Oh CW, Mattoo R, et al. : Femoral lengthening over an intramedullary nail using the external fixator: Risk of infection and knee problems in 22 patients with a follow-up of 2 years or more. Acta Orthop 2005;76:245-252. [DOI] [PubMed] [Google Scholar]
- 13.Paley D, Herzenberg JE, Paremain G, Bhave A: Femoral lengthening over an intramedullary nail: A matched-case comparision with Ilizarov femoral lengthening. J Bone Joint Surg Am 1997;79-A:1464-1480. [DOI] [PubMed] [Google Scholar]
- 14.Kosuge DD, Pugh H, Timms A, Barry M: Limb lengthening for post-traumatic shortening over a pre-implanted femoral locking plate. J Orthop Trauma 2013;27:e57-e64. [DOI] [PubMed] [Google Scholar]
- 15.Paley D: PRECICE intramedullary limb lengthening system. Expert Rev Med Devices 2015;12:231-249. [DOI] [PubMed] [Google Scholar]
- 16.Cole JD, Justin D, Kasparis T, DeVlught D, Knobloch C: The intramedullary skeletal kinetic distractor (ISKD): First clinical results of new intramedullary nail for lengthening of the femus and tibia. Injury 2001;32(suppl 4):SD129–SD139. [DOI] [PubMed] [Google Scholar]
- 17.Rozbruch SR, Birch JG, Dahl MT, Herzenberg JE: Motorized intramedullary nail for management of limb-length discrepancy and deformity. J Am Acad Orthop Surg 2014;22:403-409. [DOI] [PubMed] [Google Scholar]
- 18.De Bastiani G, Aldegheri R, Renzi-Brivio L, Trivella G: Limb lengthening by callus distraction. J Pediatr Orthop 1987;7:129-134. [DOI] [PubMed] [Google Scholar]
- 19.Makhdom AM, Cartaleanu AS, Rendon JS, Villemure I, Hamdy RC: The accordion maneuver: A noninvasive strategy for absent or delayed formation in cases of limb lengthening. Adv Orthop 2015;2015:912790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ilizarov GA: Clinical application of the tension-stress effect for limb lengthening. Clin Orthop Relat Res 1990;250:8-26. [PubMed] [Google Scholar]
- 21.Dincyurek H, Kocaoglu M, Eralp IL, Bilen FE, Dikmen G, Eren I: Functional results of lower extremity lengthening by motorized intramedullary nails. Acta Orthop Traumatol Turc 2012;46:42-49. [DOI] [PubMed] [Google Scholar]
- 22.Krieg AH, Lenze U, Speth BM, Hasler CC: Intramedullary leg lengthening with a motorized nail. Acta Orthop 2011;82:344-350. [DOI] [PMC free article] [PubMed] [Google Scholar]