Abstract
Purpose of review
The underlying mechanisms responsible for chronic and progressive neurological damage after traumatic brain injury (TBI) are poorly understood, and therefore, current treatment options are limited. Proteomics is an emerging methodology to study changes to the TBI proteome in both patients and experimental models.
Recent findings
Although experimentally complex, mass spectrometry-based proteomics approaches are converging on a set of common methods. However, these methods are being applied to an increasingly diverse range of experimental models and types of injury.
Summary
In this review, our aim is to briefly describe experimental TBI models and the underlying methods common to most proteomic approaches. We will then review a series of articles that have recently appeared in which these approaches have been applied to important TBI questions. We will summarize several recent experimental studies, and suggest how the results of these emerging studies might impact future research as well as patient treatment.
Keywords: biochemical pathway identification, biomarkers, experimental traumatic brain injury models, neurodegeneration, proteomics
INTRODUCTION
Current treatment approaches for traumatic brain injury (TBI) patients are limited and the long-term prognosis of those with severe or recurrent injury remains poor. Advances in medical management have been slowed by limited understanding of the underlying pathophysiology. However, one of the very real challenges in TBI research is the heterogeneity of the initial injury which is reflected in the wide array of experimental models currently in use, from in-vitro cell and in-vivo animal models to studies on humans with variable types of injuries and often unknown prior history of injury. Proteomics approaches can reveal changes in protein levels between control and experimental samples which can be used to identify biomarkers as well as reveal potential pathways of tissue damage. Such approaches can be applied to bodily fluids including blood and cerebrospinal fluid (CSF) as well as cultured cells, intact tissues, and most recently exosomes. Although highly complex and technical, there are a common set of steps used in mass spectrometry-based proteomics and we will first provide a brief overview of the essential methods. We will then review a series of articles published between 2017 and 2018, in which these methods have been applied to study different questions in TBI (Table 1). Furthermore, a list of biological process gene ontology terms as well as critical proteins found in each reviewed study is listed in Table 2. Because of the highly diverse experimental models reviewed, it is not yet possible to compare each study with the others. However, common themes are emerging from these studies, including the role of inflammatory responses following TBI.
Table 1.
Proteomic Studies Highlighted in This Review
| Reference | Model | Question/focus |
| [1▪] | 1. In-vitro stretch injurya. B35 cellsb. RN33Bc. SH-SY5Yd. K048 human neural stem cells (hNSCs) | Medium throughput drug screening approach for the identification of compounds that reduce proteome changes associated with cellular damage |
| [2▪▪] | 1. In-vitro stretch injurya. SH-SY5Yb. HT-222. CCI model (rat) 3. Human CSF | Determine the efficacy of hypothermia as a treatment for TBI and the effect on the TBI proteome |
| [3▪▪] | 1. Pendulum injury (rat) | Identification of repetitive TBI-specific proteins/biomarkers |
| [4▪▪] | 1. Stab wound injury (mouse) | Differential proteome response of gray matter injury vs. gray and white matter injury |
| [5▪] | 1. Stab wound injury (mouse) | Effect of monocyte invasion and astrocyte proliferation after TBI on glial scar formation |
| [6▪] | 1. CCI and hemorrhagic shock (porcine) | Determine the efficacy of valproic acid treatment for TBI and effect on the TBI proteome |
| [7▪] | 1. Human serum | Use of serum biomarker profile for defining TBI severity |
| [8▪▪] | 1. Microvesicles/exosomes (derived from human CSF) | Potential utility of microvesicles/exosomes for TBI diagnosis |
| [9▪▪] | 1. Postmortem brain tissuea. CTE (I–IV) b. Alzheimer's diseasec. Control | Differential proteome changes associated with different clinical stages of CTE and comparison of CTE vs. Alzheimer's disease |
| [10▪▪] | 1. Frozen human brain tissuea. iNPHb. TBI | Identification of focal vs. diffuse injury proteome |
CCI, controlled cortical impact; CSF, cerebrospinal fluid; CTE, chronic traumatic encephalopathy; iNPH, idiopathic normal pressure hydrocephalus; TBI, traumatic brain injury.
Table 2.
Critical Gene Ontology Terms and Proteins Identified in the Highlighted Studies
| Reference | Gene ontology terms | Critical proteins |
| [1▪] | StructuralReceptorNucleic acid binding transcription factor (TF)Enzyme regulatorCatalyticTransporter | None reported |
| [2▪▪] | CCI and 37°C vs. 37°C Blood coagulationResponse to wound healingHemostasis CCI and 32°C vs. CCI and 37°C Cellular component organizationResponse to mercury ionMacromolecular complex assembly | Plasminogen (PLG)Antithrombin III (ATIII)Fibrinogen γ chain (FGGa)Transthyretin (TTRa) |
| [3▪▪] | Single vs. repetitive mild traumatic brain injury (mTBI) vs. time points AutophagyCell adhesionGlutathione metabolismMyelinationMicrotubule depolymerizationAxon guidancecentral nervous system (CNS) development | Phosphodiesterase 10a (Pde10a)Guanine nucleotide-binding protein subunit α(GnaI) |
| [4▪▪] | Gray matter and white matter injury vs. gray matter injury only Lipid biosynthesisMyelinationAxon ensheathmentOxidative stressCell redox homeostasisplatelet derived growth factor (PDGF) signaling pathwaytransforming growth factor beta (TGFβ) signaling pathway | Glial fibrillary acidic protein (GFAP)VimentinFibrinogen alpha chain (FGA)Plasminogen (PLG)Antithrombin III (ATIII)von Willebrand factor A domain containing protein8 (vwf8a)Zinc finger MIZ domain-containing protein 1 (Zmiz1) |
| [5▪] | Wild type vs. CCR2-/- mice Glycosaminoglycan synthesisMetabolic processesNegative regulation of: B-cell-mediated immunity, immunoglobulin-mediated immune response, immunoglobulin production | Thymocyte nuclear protein 1 (Thyn1)Bridging integrator 2 (Bin2)Carbonic anhydrase 12 (Ca12)3-betaglucuronosyltransferase 2 (B3gat2)Guanine nucleotide-binding protein subunit α (GnaI)Mannose-1-phosphate guanylyltransferase α (Gmppa)Coiled-coil domain-containing protein 85A (Ccdc85a)Actin-binding LIM protein 3 (Ablim3)Njmu-R1 (5730455P16ik)Mitogen-activated protein kinase kinase kinase kinase 2 (Map4k2) |
| [6▪] | Valproic acid treatment vs. normal saline control Cytoplasmic structural proteinsCell deathNecrosisOrganismal deathEndocytosisCell survival, viability, and proliferationOrganization of cytoplasm | Phenylalanyl-tRNA synthetase α subunit (FARSA)Periplakin (PPL)ArfGAP with RhoGAP domainRho GTPase-activating protein 11 (ARHGAP11)Trafficking protein particle complex 5 (TRAPPC5)Tyrosine 3/tryptophan 5-monooxygenase activation protein β (Ywhab)Vinculin (VCL)Nucleolar protein 11 (NOL11)Canopy FGF signaling receptor |
| [7▪] | Found in mild, moderate, and severe TBI Major acute phase reactantAcute phase responseLipid transportAngiogenesisCell adhesionBlood coagulation hemostasisInflammatory responseCholesterol metabolismLipid metabolismLipid degradationSteroid metabolismSterol metabolism | Serum amyloid A (SAA)bC-reactive protein (CRP)bLeucine-rich α-2-glycoprotein (LRG1)bLipopolysaccharide-binding protein (LBP)bFibronectin (FN)bVitronectin (VN)bα-1-antichymotrypsin (ACT)bKininogen (KNG)Apolipoprotein E (ApoE)Zinc-α-2-glycoprotein (AZGP1) |
| [8▪▪] | Severe TBI CSF vs. control CSF Cytoskeletal proteinsNeurite outgrowthVesicle membrane | SpectrinGlial acidic fibrillary protein (GFAP)Ubiquitin carboxyl terminal hydrolase L1 (UCH-L1)Synaptophysin (SYP)Alix |
| [9▪▪] | None reported | Mitochondrial ribosomal protein L32 (MRPL32)Rho guanine nucleotide exchange factor 25 (ARHGEF25)Neuronal calcium sensor 1 (NCS1)Voltage-dependent anion channel 3 (VDAC-3)Calmodulin 2 (CALM2)Kininogen 1 (KNG1)Proline-rich region containing (RLTPR)NAD(P)H dehydrogenase [quinone] (NQ01) |
| [10▪▪] | Severe TBI vs. iNPH (control) NeurodegenerationCytoskeletal functionCell death or survivalCell signalingTransport or repair pathwaysOxidation or reduction pathwaysEnergy metabolism | Microtubule-associated protein tau (MAPT)FascinPyruvate kinase (PKM)Cathepsin D (CTSD)Prosaposin (PSAP) |
Bold text: proteins identified as elevated relative to control.
Italicized text: proteins identified as decreased relative to control.
CCI, controlled cortical impact; iNPH, idiopathic normal pressure hydrocephalus; TBI, traumatic brain injury.
aProteins found in both human and animal studies.
bElevated in all patients.
Box 1.
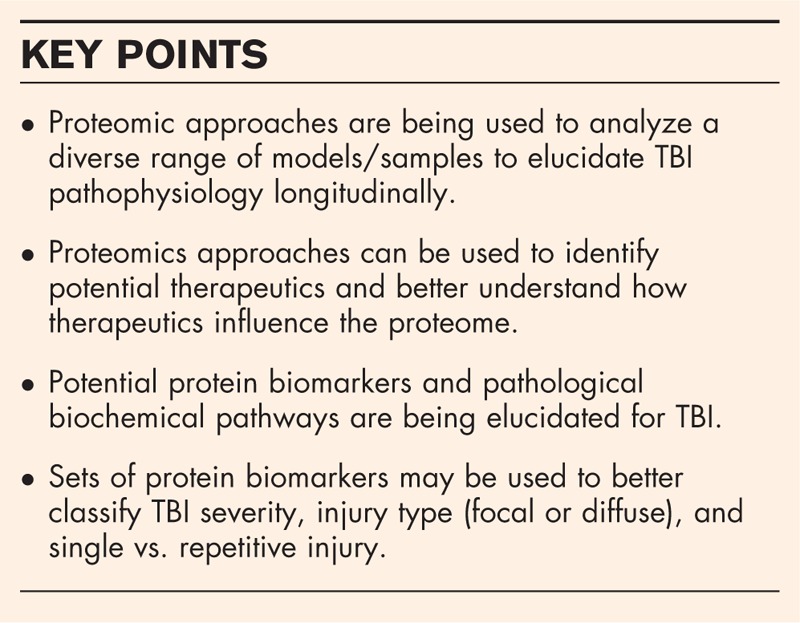
no caption available
OVERVIEW AND CONSIDERATIONS FOR PRECLINICAL MODELS OF TRAUMATIC BRAIN INJURY
Proteomic approaches are well suited for the identification of the mechanisms of injury of TBI and provide a strategy for identifying targets for novel treatments. Preclinical proteomic analysis of the effects of TBI depends on the characterization and validation of reproducible, clinically relevant models. Although rodent brains, unlike human brains, are not gyrencephalic, multiple preclinical rat and mouse models of TBI have been used, in large part because they are cost-effective in comparison with larger animal models. The most common and best characterized rodent models of TBI are fluid percussion injury, controlled cortical impact (CCI), weight drop, and blast-induced neurotrauma. Each of these models is similar to civilian or military TBI in at least some respects but, because human TBI is extremely heterogeneous, no model more than partially simulates clinical TBI.
When studying the proteomic effects of preclinical TBI or reviewing findings from others’ laboratories, several questions should be considered. First, from what source was the sample derived? Peripheral blood samples suggest the possibility of biomarker identification, but the exact origin of a protein is unknowable. CSF contain proteins that are derived from brain tissue, but as with blood samples, the source is unknown. Second, if brain tissue was analyzed, was the tissue from the injury site, from grossly uninjured tissue ipsilateral to the lesion site or tissue contralateral to the injury site? Third, if a relatively large sample was required for analysis, what was the likely heterogeneity of the sampled tissue? Fourth, were samples from multiple animals pooled to increase sample size or reduce the cost of analysis? Fifth, what was the statistical management of the data, that is, are the findings likely to be reproducible?
OVERVIEW OF PROTEOMICS METHODS AND CAVEATS
In current practice, most mass spectrometry-based proteomics studies use a series of common steps as outlined below. Samples for analysis can come from diverse sources including blood, CSF, cultured cells, and intact tissues. Proteins are extracted from these biological sources, and total protein is quantified. Quantification is a critical step because the ensuing procedures have been optimized for a defined amount of protein and a consistent quantity of protein is critical for accurate measurement of changes in protein abundance among samples. Isolated proteins are then subjected to digestion using amino acid sequence-specific proteases, usually trypsin [11].
At this point, ‘isobaric’ reagents can be introduced which are stable isotope-containing molecules that can be used to chemically ‘tag’ peptides. Commonly used isobaric tags include both tandem mass tags and isobaric tags for relative and absolute quantitation reagents, and the use of these tags can allow simultaneous analysis of controls and experimental samples and provide relative quantification with high precision [12,13]. Peptides can then be fractionated by liquid chromatography ‘off-line’ or the peptides can be directly introduced into the mass spectrometer. Peptides are introduced into mass spectrometers as ions, and the masses of the peptide ions are determined. The peptides are then fragmented in the mass spectrometer and the masses of the resulting fragments determined. Upon the basis of the pattern of peptide fragments, the sequence of the original peptide can be established, and its identity confirmed via comparison to several databases (i.e., UniProt) [14]. The entire chromatography run can extend to hours with tens of thousands of mass spectra obtained. Data obtained from proteomic studies are a direct reflection of the starting material composition. Therefore, different brain regions within the brain have different ratios of cell types as well as different functions that result in differential protein expression profiles. This was eloquently illustrated by the study conducted by Sharma et al.[15] where they determined cell type-specific proteins as well as brain region-specific proteins in mouse brain. Finally, the most accepted secondary form of validation of proteomic findings is to use antibody-based assays including western blot and ELISA.
Once the original liquid chromatography-mass spectrometer data file has been obtained, various software approaches can be used to ‘reassemble’ the peptides into proteins. The ‘quality’ for each protein identification can be assessed based upon the number of unique peptides observed. The amount of each protein can be determined by the signal intensity of each peptide observed, and statistical approaches can then be applied to determine which changes in protein levels between experimental and control groups are significant [16].
The endpoint of the initial study is a list of proteins and their relative abundances. Various bioinformatics approaches can then be applied to these lists, grouping proteins by gene ontology terms, interacting networks, and biochemical pathways [17,18]. Upon the basis of the altered pathways or networks, inferences can be made as to the underlying pathophysiology created by a specific type of injury in a specific type of model.
A well-known problem with proteomics studies is for there to be a bias toward highly abundant proteins. Protein digestion of high-abundance proteins results in a greater number of digested peptides more quickly that drown out low-abundance peptides. There are strategies such as those developed by Fonslow et al.[19] to remove the high-abundance protein tryptic peptides to improve the identification of low-abundance proteins within a sample. Another potential issue that could bias the proteomic results is related to protein digestion. For example, membrane proteins require special solubilization techniques to release the integral proteins and allow for their digestion and identification [20]. Furthermore, TBI pathophysiology can lead to aggregation of proteins (i.e., tau) that can be a challenge to identify with standard protease methodologies. The highlighted study by Cherry et al.[9▪▪] (later in this review) developed a strategy for analyzing the detergent-insoluble proteome to gain a more comprehensive understanding of the proteome alteration related to neurodegeneration.
PROGRESS PRIOR TO 2018
Ganau et al. (2018)
Ganau et al.[21] provide a comprehensive summary of work prior to 2018. Their systematic review, which was completed in late 2017, emphasized applications of proteomic profiling to identify potential biosignatures for TBI.
PROGRESS TO DATE IN 2018
López-García et al.(2018)
This study used perhaps the simplest experimental system, cells grown in culture [1▪]. In-vitro models, although lacking the complexity of tissue, anatomic structures and an immune response, can provide high throughput for drug screens. López-García et al. developed an in-vitro model to monitor gene expression changes, proteomic signatures, mitochondrial function, and delayed cell death in neural cell lines subjected to rapid stretch injury followed by oxidant (H2O2) stress [1▪]. This model was then used to screen a library of 3500 drugs, from which five were identified to be beneficial. Of these, the antibiotic rifampicin was identified as a neuroprotectant.
In the proteomics portion of this study, B35 rat neuroblastoma cells, either undifferentiated or differentiated were subjected to stretch injury. Proteins with either increased or decreased abundance were identified that were associated with either cell differentiation or in-vitro stretch injury or both (Table 2). This approach can be used to identify and perhaps retask drugs for use in TBI and potentially to associate biochemical pathways with drug actions.
Cheng et al. (2018)
Using a combination of an in-vitro stretch model, a rat CCI model and CSF from TBI patients, Cheng et al.[2▪▪] investigated the influence of hypothermia on response to TBI. The proteomics portion of this study involved an examination of the influence of hypothermia after CCI. Temperature modulation in sham rats alone and TBI resulted in the upregulation and downregulation of distinct sets of proteins. The Cheng group noted that CCI and 32°C treatment reversed many of the observed protein changes seen in the CCI and 37°C group. Gene ontology analysis of the proteins with altered abundance revealed differences between the CCI and 37°C group vs. the CCI and 32°C group (Table 2).
Proteins were also examined in CSF samples from human TBI patients with mild (7), moderate (5), and severe (8) injury. Levels of plasminogen (PLG), antithrombin III (ATIII), fibrinogen gamma chain (FGG), and transthyretin increased with increasing injury magnitude. When measured at 3 days following injury, hypothermia resulted in lower levels of PLG, ATIII, FGG, and transthyretin. Among the proteins identified in the rat brain tissue and human CSF studies, FGG and PLG appear in both. The authors conclude that inconsistent results from prior hypothermia studies could result from the complexity of variables in TBI, and that combined proteomics and bioinformatics analysis of appropriate biomarkers might improve the selection of patients who would benefit from hypothermia therapy.
Song et al. (2018)
To examine the global proteome effects of repetitive TBI, Song et al.[3▪▪] used a unique rat model of repetitive mild brain injury. The repetitive groups were impacted once per day for 3 consecutive days. Rats were sacrificed 1 day, 7 days, or 6 months following the final strike. Differentially expressed proteins were analyzed by gene ontology annotation (Table 2). At 6 months after injury, two proteins, phosphodiesterase 10a (Pde10a) and guanine nucleotide binding protein subunit α (Gnal), were significantly unregulated in the repetitively injured group compared with the singly injured and sham groups. Both Pde10a and Gnal are proteins involved in cyclic adenosine monophosphate signaling and therefore involved in cell survival and inflammation. An important result of this study is that the levels of both Pde10a and Gnal were significantly elevated in the multiple injury vs. the single injury group 6 months after the initial injury.
Mattugini et al. (2018)
Mattugini et al.[4▪▪] used a proteomics approach to examine differences in stab wound injury in the adult murine cerebral cortex. The focus of the study was to determine if damage resulting from injury to gray matter alone was different from gray matter extending into the underlying white matter 3 days post injury. Punch biopsies were obtained from the gray matter around the lesion site and from a corresponding contralateral site. Lists of proteins significantly different between the two hemispheres were obtained. After gray matter alone and gray matter and white matter injury, levels of glial acidic fibrillary protein and vimentin increased substantially as did proteins involved in blood coagulation (fibrinogen α chain, PLG, ATIII). A cluster of proteins and associated gene ontology terms increased in the gray matter and white matter group, as opposed to the gray matter alone group (Table 2). The authors concluded that there are profound differences resulting from damage to gray matter alone vs. damage to gray matter with white matter injury inducing reactive gliosis that contributes to scar formation and inhibits axonal regeneration.
Frik et al. (2018)
Frik et al.[5▪] also used a stab wound injury model to investigate the importance of monocyte invasion, astrocyte proliferation, and the importance of the C–C–chemokine receptor 2 (CCR2). CCR2 directs monocytes to inflamed tissues, and the loss of CCR2 reduced macrophage infiltration and improved cognitive function after TBI [22]. Frik et al. produced stab wounds in wild-type, mixed-sex, and CCR2-/- mice and examined astrocyte proliferation and immune cell infiltration in wild-type and CCR2-/- mice at intervals up to 90 days following surgery [5▪]. For the proteomics portion of the study, samples were taken at only day 5 post injury. Proteins with significant changes were analyzed with respect to protein network interactions and gene ontology biological processes (Table 2). Proteins associated with the gene ontology terms glycosaminoglycan synthesis and metabolic processes were found to be higher in the wild-type animals, consistent with the decreased extracellular matrix deposition and scar formation in the CCR2-/- group after stab wound injury observed by immunohistochemical methods. This study demonstrates the important role of monocyte invasion and astrocyte proliferation in scar formation following TBI.
Weykamp et al. (2018)
Weykamp et al.[6▪] studied the role of the antiepileptic agent, valproic acid (VPA), in modulating the proteome in a porcine model of TBI. In addition to acting as a γ-aminobutyric acid channel modulator, VPA, at higher concentrations, acts as a histone deacetylase inhibitor. In their study, female Yorkshire swine received CCI and were simultaneously bled 40% of total blood volume to simulate hypovolemic shock that often accompanies TBI in both civilian and military trauma. Peripheral blood monocytic cells were collected at three time points; at baseline, 60 min after VPA infusion, and after resuscitation with normal saline infusion. A series of proteins were identified that distinguished the normal saline from the normal saline and VPA group, most of which were cytoplasmic structural proteins (Table 2). In the VPA-treated animals, proteins associated with cellular compromise were decreased and cellular survival were increased. The induction of VPA-mediated changes was too rapid to be explained by VPA-mediated changes in histone acetylation and transcriptional accessibility. Increases in protein acetylation were observed for histone H3, ras-related protein Rab-14, which is involved in endocytic transport and cell–cell adhesion, and rho guanosine nucleotide dissociation inhibitor, a rho signaling inhibitor. Potential limitations of this study include the small number of experimental animals, and the simultaneous induction of TBI and hemorrhagic shock. The extrapolation of the results obtained here in peripheral blood monocytic cells to neurons and astrocytes found in the brain awaits experimental validation.
Anada et al. (2018)
Anada et al.[7▪] proposed a panel of human serum protein biomarkers to measure the severity of TBI. Although patients with TBI are traditionally stratified based upon the Glasgow Coma Scale (GCS), the authors argued that the increased use prior to arrival at the hospital of intubation and sedation, would eliminate verbal responses and may eliminate eye opening (two of the three components of the GCS), impair assessment of patient status, and could increase the importance of serum biomarkers. Sera were pooled and on the basis of GCS at presentation, generated four groups; mild TBI (GCS: 13–15), moderate TBI (GCS: 9–12), severe TBI (GCS: 3–8), and control. A series of 10 secreted proteins were observed to increase in abundance (Table 2). Increased levels of two proteins, serum amyloid-A and C-reactive protein, were confirmed by ELISA, however, neither protein is specific to TBI.
Overall, the authors showed that increased abundance of seven proteins were elevated in all TBI patients (Table 2). Although individually, these proteins cannot be used as specific TBI biomarkers, collectively they suggest patterns that might distinguish mild, moderate, and severe TBI.
Manek et al. (2018)
This study examined exosomes, isolated from human CSF following TBI, using a proteomics approach [8▪▪]. Exosomes or microvesicles/exosomes (MV/E) are released from brain cells during disease and injury. The MV/E contain products from damaged cells, including proteins. CSF was obtained from normal patients, TBI patients with GSC <8, and from the CSF drainage system in patients with severe blunt head trauma. The number of proteins in MV/E of trauma patients (466) was considerably larger than in human control samples (92). The MV/E from TBI CSF had several proteins not found in the controls, including cytoskeletal proteins, neurite outgrowth-related proteins, and vesicle membrane proteins. Intact spectrin and GFAP, as well as their corresponding breakdown products, and ubiquitin carboxyl terminal hydrolase L1 and Alix, were observed to increase substantially in the MV/E from TBI patients. The authors concluded that CSF from patients contained exosomes derived from multiple cell types in the brain, and that the analysis of these proteins, as well as their breakdown products could have important diagnostic value in TBI.
Cherry et al. (2018)
Cherry et al.[9▪▪] examined detergent-insoluble proteins in postmortem brain tissue from patients with chronic traumatic encephalopathy (CTE). CTE is thought to result from repetitive head trauma, although specific underlying disease mechanisms are currently unknown. Patients diagnosed with CTE (11), Alzheimer's disease (8), and control cases (6) were examined. A series of proteins were identified that distinguished CTE from control and Alzheimer's disease samples, and some proteins common to CTE and Alzheimer's disease were also observed. Among the proteins examined, seven were indicated as proteins of interest including NQO1 (Table 2). The NQO1 gene encodes the protein NAD(P)H dehydrogenase [quinone] 1. The increased abundance of NQO1 was confirmed using immunohistochemistry and its levels were shown to increase with increasing CTE stage. The increased abundance of NQO1 in CTE may suggest activation of a protective response to oxidative stress. It is currently unknown if the proteins extracted from detergent-insoluble precipitates are enzymatically active or if their association with hyperphosphorylated tau indicates they have become a component of pathological aggregates.
Hamdeh et al. (2018)
Hamdeh et al.[10▪▪] focused on elucidating the differences between the focal and diffuse TBI proteome in 16 severe TBI patients presenting with a GSC score ≤8 (average 4.3). A unique aspect of this study was that brain samples were obtained from structurally normal-appearing (by imaging) frontal cortex obtained during insertion of an intracranial pressure (ICP) monitor. Control patients comprised a group of 11 idiopathic normal pressure hydrocephalus (iNPH) patients. Potentially limiting aspects of the study include small patient numbers, small tissue sample amounts, heterogeneity in age (17–83 for the TBI patients and 64–80 for the iNPH patients), and heterogeneity in mechanism of injury for the TBI patients, although most (69%) were injured in a motor vehicle accident. The majority of both TBI (75%) and idiopathic normal pressure hydrocephalus (iNHP) patients (64%) were men.
For the proteomics studies, brain biopsies were taken when the ICP monitor was inserted, between 3 and 175 h post injury. When results of protein levels from a series of six TBI patients, not otherwise distinguished as diffuse or focal TBI, were compared with the iNPH patients, a subset of the identified proteins was found to be altered in a statistically significant number of patients; several of which have been previously shown to be altered in both human and animal TBI proteomic studies (Table 2).
In a second study, proteome differences were examined between patients with focal injury and diffuse axonal injury (DAI) for which several of the altered proteins were similar to those found in the previous comparison between TBI and iNPH controls. It is important to note that the samples in this study were obtained from normal-appearing cortical tissue at the location of the ICP monitor and at a distance from any radiologically apparent brain injury. In previous studies, tissues were obtained closer to the apparent site of injury. More than 20 proteins in the DAI group had altered abundance relative to the iNPH or focal injury groups, suggesting that DAI is associated with more widespread injury (Table 2). The authors suggest that understanding the heterogeneity in injury among TBI patients has implications for individualized therapy for TBI patients. Further, the more widespread and complex alterations in the DAI patients are indicative of a secondary injury cascade that may be related mechanistically to the development of neurodegenerative disorders in TBI patients.
CONCLUSION
Proteomics has emerged as a sophisticated tool with applications in many human diseases, including cancer and neurodegeneration as well as TBI. The field of proteomics is maturing with evolving standards for sample preparation and data analysis that will make the results of such studies available for examination by a much broader range of investigators. Bioinformatics approaches for validation and comparison across multiple studies are in progress. The past year has shown that these methods can be applied in multiple experimental settings from in-vitro models to human studies to ask increasingly complex questions about critical variables in TBI. Although several consistent themes are emerging from these studies, in particular the role of inflammation in post-TBI injury, it is not yet possible to integrate these studies at the level of specific proteins. Future studies will create additional tools and data that will codify mechanistic details resulting in acute and chronic neurodegeneration and hopefully lead to improved methods for patient stratification and treatment methods and agents.
Acknowledgements
The authors would like to thank Lawrence Sowers for his critical reading and editorial assistance in preparation of this manuscript.
Financial support and sponsorship
This work was supported by NIH grant 1R01CA184097 as well as a grant from The Moody Foundation for Translational TBI Research.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1▪.López-García I, Gerő D, Szczesny B, et al. Development of a stretch-induced neurotrauma model for medium-throughput screening in vitro: identification of rifampicin as a neuroprotectant. Br J Pharmacol 2018; 175:284–300. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study showed that proteomics could be used to help screen for/repurpose drugs for TBI.
- 2▪▪.Cheng SX, Xu Z-W, Yi T-L, et al. iTRAQ-based quantitative proteomics reveals the new evidence base for traumatic brain injury treated with targeted temperature management. Neurotherapeutics 2018; 15:216–232. [DOI] [PMC free article] [PubMed] [Google Scholar]; Cheng et al. determined that the use of proteomics and bioinformatics analysis could improve the efficacy of hypothermia treatment and be potentially used for identifying patients for which the therapy might be beneficial.
- 3▪▪.Song H, Fang S, Gao J, et al. Quantitative proteomic study reveals up-regulation of cAMP signaling pathway-related proteins in mild traumatic brain injury. J Proteome Res 2018; 17:858–869. [DOI] [PubMed] [Google Scholar]; This study identified proteins that could help distinguish between single and repetitive head injury.
- 4▪▪.Mattugini N, Merl-Pham J, Petrozziello E, et al. Influence of white matter injury on gray matter reactive gliosis upon stab wound in the adult murine cerebral cortex. Glia 2018; 66:1644–1662. [DOI] [PubMed] [Google Scholar]; Mattugini et al. determined how the proteome response could change so much based upon grey matter injury vs. grey and white matter injury.
- 5▪.Frik J, Merl-Pham J, Plesnila N, et al. Cross-talk between monocyte invasion and astrocyte proliferation regulates scarring in brain injury. EMBO Rep 2018; 19: doi:10.15252/embr.201745294. [DOI] [PMC free article] [PubMed] [Google Scholar]; Frik et al. used proteomics and genetic mouse models to elucidate how monocytes contribute to glial scar formation.
- 6▪.Weykamp M, Nikolian VC, Dennahy IS, et al. Rapid valproic acid-induced modulation of the traumatic proteome in a porcine model of traumatic brain injury and hemorrhagic shock. J Surg Res 2018; 228:84–92. [DOI] [PubMed] [Google Scholar]; Weykamp et al. determined the effects of valproic acid on modulating the porcine proteome after TBI and were able to determine a likely mechanism of action.
- 7▪.Anada RP, Wong KT, Jayapalan JJ, et al. Panel of serum protein biomarkers to grade the severity of traumatic brain injury. Electrophoresis 2018; doi:10.1002/elps.201700407. [DOI] [PubMed] [Google Scholar]; Anada et al. tried to identify a panel of serum biomarkers to better define the severity of TBI.
- 8▪▪.Manek R, Moghieb A, Yang Z, et al. Protein biomarkers and neuroproteomics characterization of microvesicles/exosomes from human cerebrospinal fluid following traumatic brain injury. Mol Neurobiol 2018; 55:6112–6128. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study was one of the first to utilize exosomes to develop novel biomarkers for TBI.
- 9▪▪.Cherry JD, Zeineddin A, Dammer EB, et al. Characterization of detergent insoluble proteome in chronic traumatic encephalopathy. J Neuropathol Exp Neurol 2018; 77:40–49. [DOI] [PMC free article] [PubMed] [Google Scholar]; Cherry et al. conducted a proteomic study on the detergent-insoluble fractions from postmortem brain tissue to identify proteome differences between CTE and Alzheimer's disease.
- 10▪▪.Hamdeh SA, Shevchenko G, Mi J, Musunuri S. Proteomic differences between focal and diffuse traumatic brain injury in human brain tissue. Sci Rep 2018; 8:6807. [DOI] [PMC free article] [PubMed] [Google Scholar]; Hamdeh et al. used proteomics to identify differences between focal and diffuse injury as well as using biopsied brain tissue during the insertion of ICP monitors. Their use of live human brain tissue could prove to be a valuable approach for studying TBI.
- 11.Van Ripper SK, de Jong EP, Carlis JV GT. Mass spectrometry-based proteomics: basic principles and emerging technologies and directions. [date unknown], doi:10.1007/978-94-007-5896-4_1 [DOI] [PubMed] [Google Scholar]
- 12.Thompson A, Schäfer J, Kuhn K, et al. Tandem mass tags: a novel quantification strategy for comparative analysis of complex protein mixtures by MS/MS. Anal Chem 2003; 75:1895–1904. [DOI] [PubMed] [Google Scholar]
- 13.Ross PL, Huang YN, Marchese JN, et al. Multiplexed protein quantitation in Saccharomyces cerevisiae using amine-reactive isobaric tagging reagents. Mol Cell Proteomics 2004; 3:1154–1169. [DOI] [PubMed] [Google Scholar]
- 14.The UniProt Consortium UniProt: the universal protein knowledgebase. Nucleic Acids Res 2017; 45:D158–D169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sharma K, Schmitt S, Bergner CG, et al. Cell type- and brain region-resolved mouse brain proteome. Nat Neurosci 2015; 18:1819–1831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Burger T. Gentle introduction to the statistical foundations of false discovery rate in quantitative proteomics. J Proteome Res 2018; 17:12–22. [DOI] [PubMed] [Google Scholar]
- 17.Ashburner M, Ball CA, Blake JA. Gene ontology: tool for the unification of biology. The Gene Ontology Consortium. Nat Genet 2000; 25:25–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.The Gene Ontology Consortium Expansion of the gene ontology knowledgebase and resources. Nucleic Acids Res 2017; 45:D331–D338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fonslow BR, Stein BD, Webb KJ, et al. Digestion and depletion of abundant proteins improves proteomic coverage. Nat Methods 2013; 10:54–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chandramouli K, Qian PY. Proteomics: challenges, techniques and possibilities to overcome biological sample complexity. Hum Genomics Proteomics 2009; 2009: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ganau M, Syrmos N, Paris M, et al. Current and future applications of biomedical engineering for proteomic profiling: predictive biomarkers in neuro-traumatology. Medicines (Basel) 2018; 5: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hsieh CL, Niemi EC, Wang SH, et al. CCR2 deficiency impairs macrophage infiltration and improves cognitive function after traumatic brain injury. J Neurotrauma 2014; 31:1677–1688. [DOI] [PMC free article] [PubMed] [Google Scholar]


