Overview
Introduction
We describe the surgical technique and the pitfalls of French-door laminoplasty.
Step 1: Patient Positioning
Position the patient to keep the cervical spine “parallel to the floor” or in the “reverse Trendelenburg position” with only a slight incline and place intraoperative neurological monitors to prevent intraoperative neurological deterioration.
Step 2: Surgical Approach
Use the common cervical posterior approach to expose the lamina and ligamentum flavum.
Step 3: Create Grooves
Cut the center of each lamina and create bilateral grooves using a high-speed burr.
Step 4: Open the Lamina
Open the lamina bilaterally and create a small hole in each one using a high-speed burr.
Step 5: Create Bone Struts
Create bone struts from the spinous processes and tie them to each lamina.
Step 6: Wound Closure
Perform meticulous closure of the wound to avoid wound-healing complications.
Results
In our original study12, we treated forty-six patients with French-door laminoplasty and compared the surgical results of this procedure with those of open-door laminoplasty in a prospective, randomized controlled manner.
Introduction
We describe the surgical technique and the pitfalls of French-door laminoplasty.
Cervical laminoplasty was developed in the 1970s as an alternative to laminectomy for treating multilevel cervical compressive myelopathy1. The proposed advantages of laminoplasty are that it achieves expansion of the spinal canal and preserves spinal stability2. Posterior laminectomy with fusion with use of instrumentation is also an effective alternative, especially for patients with kyphosis or instability. However, it is less cost-effective and a variety of complications have been reported3. Anterior discectomy and fusion could provide better surgical outcomes than posterior decompression, but the complications at an early stage after the surgery are more common in patients with multilevel cervical myelopathy4.
Various modified methods of laminoplasty have been developed and the procedures are primarily classified as either open-door5,6 or French-door (double-door)7 laminoplasty. The spinal canal is opened on one side of the lamina and is hinged on the contralateral side in open-door laminoplasty, whereas the door is opened from the midline of the lamina and is hinged in the transitional area between the facet joints and the laminae in French-door laminoplasty.
A laminoplasty can reportedly provide satisfactory long-term results with an acceptable complication rate in patients with cervical spondylotic myelopathy and ossification of the posterior longitudinal ligament8-11. However, only a few studies have compared the French-door and open-door techniques. We conducted a prospective randomized study and found that postoperative cervical alignment and range of motion were better with French-door laminoplasty than with open-door laminoplasty12. In this surgical techniques article, we note some tips for intraoperative exposure and how to open the lamina by creating grooves to obtain a satisfactory surgical outcome.
We perform this surgery with modifications of the method reported by Kurokawa et al.7,13. We describe a C3-C6 laminoplasty technique. After exposure of the lamina, we resect the spinous processes at their bases. The center of each lamina is cut and bilateral grooves are created with a high-speed burr. The gap between the laminae is then bridged by bone struts from the spinous processes.
Step 1: Patient Positioning
Position the patient to keep the cervical spine “parallel to the floor” or in the “reverse Trendelenburg position” with only a slight incline and place intraoperative neurological monitors to prevent intraoperative neurological deterioration (Video 1).
Apply a Mayfield or Sugita head clamp14 (Fig. 1) with the patient in the supine position.
Place the patient in the prone position on rolls or a positioning frame with the arms parallel to the body.
Fix the clamp to the holder with the head and cervical spine in the neutral position.
Support the patient’s feet and fix the thighs to the table using a strap.
Tilt the table such that the cervical spine is in the horizontal position.
Place intraoperative neurological monitors to record motor evoked potentials and sensory evoked potentials.
Fig. 1.

Sugita head clamp14.
Video 1.
Positioning of a patient for cervical laminoplasty.
Step 2: Surgical Approach
Use the common cervical posterior approach to expose the lamina and ligamentum flavum.
Make a longitudinal midline incision from the spinous process of C2 to the C7 spinous process.
Incise the nuchal ligament and the fascia.
Identify the spinous processes of C2 and C7.
Perform subperiosteal dissection of the muscles along the C3-C6 laminae from medial to lateral to reach the medial border of the facet joints.
When the upper end of the laminoplasty is C3, the semispinalis cervicis should be minimally detached from the C2 spinal lamina. Excising too much muscle from C2 may cause postoperative cervical kyphotic changes or axial pain.
Resect the C3-C6 spinous processes at their bases for later use as strut bone grafts to hold the elevated lamina in position.
Remove soft tissues from the bone with punches and rongeurs until the yellow ligaments are clearly seen in between the laminae.
Step 3: Create Grooves
Cut the center of each lamina and create bilateral grooves using a high-speed burr (Fig. 2 and Video 2).
Ensure the functioning of the high-speed burr before use. We generally use a 4 or 5-mm steel high-speed burr.
Make the center of the lamina very thin using the high-speed burr.
Stop bleeding from the bone using bone wax.
Do not cut the lamina completely with the high-speed burr. Instead split the last thin cortex carefully by scoring with a mucosal elevator.
Carefully create bilateral grooves for the hinges using the high-speed burr at the transitional area between the facet joints and the laminae. Ensure the flexibility of the lamina with a mucosal elevator while creating the grooves.
Fig. 2.

Lateral grooves should be created in the transitional area between the facet joints and the laminae.
Video 2.
Central and lateral groove creation with use of a high-speed surgical burr.
Step 4: Open the Lamina
Open the lamina bilaterally and create a small hole in each one using a high-speed burr (Video 3).
The spinal canal is enlarged by opening the split lamina bilaterally.
We generally use a mucosal elevator for separating the lamina and Metzenbaum scissors for cutting the ligamentum flavum.
Provide hemostasis with a bipolar cauterizer.
Grasp the separated lamina using forceps and create a small hole in each one using a 2-mm high-speed burr. These holes are used to suture the spacers to the lamina, as described in Step 5.
Video 3.
Separating the cervical lamina and making a small hole in each side.
Step 5: Create Bone Struts
Create bone struts from the spinous processes and tie them to each lamina (Figs. 3 and 4 and Video 4).
Create bone graft struts from the spinous processes of C6 and/or C7. The length of these struts should be 16 to 18 mm.
If the spinous process is not sufficiently large to create the necessary number of bone struts, use hydroxyapatite spacers (Apacerum; Asahi Optical, Tokyo, Japan)15.
Suture the bilateral edges of the lamina to the corresponding edges of the struts, and tie the remaining suture at the center of the strut (Figs. 5-A and 5-B).
Ensure the stability of the grafted struts.
Fig. 3.
Application of the bone strut, the edges of which should be cut obliquely.
Fig. 4.
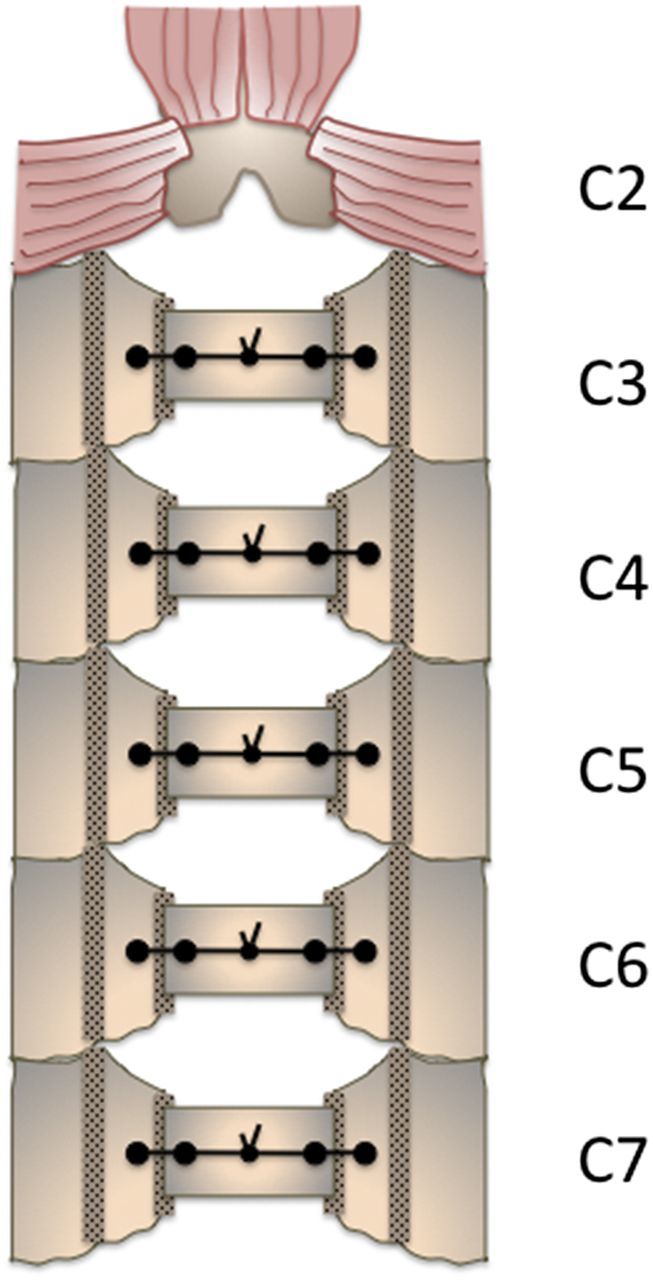
Cervical French-door laminoplasty.
Fig. 5-A.
Preoperative CT (computed tomography) axial image (C4-C5).
Fig. 5-B.
Postoperative CT axial image (C4-C5).
Video 4.
Creating bone struts and suturing the bone struts to the lamina.
Step 6: Wound Closure
Perform meticulous closure of the wound to avoid wound-healing complications.
Thoroughly irrigate the wound.
We generally insert a suction drain, but this is optional.
Close the muscle to decrease dead space.
Close the fascia with single stitches, which should be tight.
Close the subcutaneous layer by firmly apposing the edges.
Close the skin with single stitches; we generally use a stapler.
Results
In our original study12, we treated forty-six patients with French-door laminoplasty and compared the surgical results of this procedure with those of open-door laminoplasty in a prospective, randomized controlled manner. There were no differences in perioperative complications or neurological outcomes (Japanese Orthopaedic Association [JOA] scores) between the two groups. However, the postoperative cervical sagittal alignment and range of motion one year after surgery were better with French-door laminoplasty than with open-door laminoplasty. Compared with open-door laminoplasty, French-door laminoplasty resulted in a significantly smaller mean reduction in the cervical lordotic angle (3.0° compared with 5.6°), a significantly greater cervical range of motion (26.0° compared with 19.3°), and a significantly greater cervical lordotic angle in extension (14.1° compared with 7.9°).
In general, surgical decompression for the treatment of cervical compressive myelopathy is effective and improves functional, disability-related, and quality-of-life outcomes for all disease-severity categories16. The long-term results of laminoplasty have been satisfactory, and the rate of additional cervical surgery is low (2%), even in patients with ossification of the posterior longitudinal ligament9. Postoperative neurological deterioration occurs in 14% of patients from five to fifteen years after surgery, but the most common causes are lumbar or thoracic disease8,9.
What to Watch For
Indications
Patients with multilevel cervical compressive myelopathy (cervical spondylotic myelopathy or ossification of the posterior longitudinal ligament) are good candidates for cervical laminoplasty.
Patients with (1) single-level or two-level canal stenosis without developmental cervical canal stenosis or (2) ossification of the posterior longitudinal ligament with the ossification occupying ≥60% of the spinal canal could be better candidates for anterior surgery than for laminoplasty17. In patients with multilevel cervical myelopathy, spine surgeons should select anterior surgery in accordance with their surgical skills because surgical complications might be high18.
Developmental canal stenosis.
Contraindications
Substantial kyphosis of the cervical spine.
Preoperative local cervical kyphosis (>13°) results in a poor neurological outcome19.
Preoperative cervical lordosis of <10° or kyphosis and preoperative ossification of the posterior longitudinal ligament with a thickness of >7 mm could be a risk factor for a poor surgical outcome20.
The K-line, a straight line that connects the midpoints of the spinal canal at C2 and C7 on a lateral cervical radiograph, could be a practical tool for determining the cervical approach in patients with cervical ossification of the posterior longitudinal ligament21. Patients with cervical ossification of the posterior longitudinal ligament are divided into two groups according to the K-line. Ossification of the posterior longitudinal ligament does not exceed the K-line in the K-line (+) group and does exceed it in the K-line (−) group. Patients with ossification of the posterior longitudinal ligament in the K-line (−) group should not be treated with the posterior approach because sufficient decompression cannot be achieved with the posterior approach.
Substantial instability of the cervical spine (>20% slip or >4 mm of spondylolisthesis)22.
Severe cervical canal compression due to ossification of the posterior longitudinal ligament with the ossification occupying ≥60% of the spinal canal23.
Pitfalls & Challenges
Complications include segmental motor palsy (C5 palsy)24,25, postoperative kyphosis26-28, a reduced range of motion26-28, progression of ossification of the posterior longitudinal ligament, and axial pain29.
The average prevalence of C5 palsy is 4.6% (range, 0% to 30%)24,25. Various etiologies of segmental motor palsy, including tethering of the C5 roots and/or damage to the spinal cord, have been reported24,25. Some investigators have advocated prophylactic decompression of the C5 roots at the time of laminoplasty30. If the created lateral grooves are extremely wide (at the inner margin of the lateral mass), there might be a higher risk of C5 palsy because of excessive posterior spinal cord shift31.
The postoperative reduction in the range of motion has been reported to range from 30% to 70% of the preoperative range of motion26-28; however, we previously reported a reduction in the range of motion of 26%3. Damage to the posterior muscles and facet joints, and spontaneous laminar fusion, can be the causes of a reduced postoperative range of motion32,33. Attention should be paid to the intraoperative muscle dissection area and the placement of the lateral grooves (to avoid damaging the facet joint). Postoperative cervical collars are not necessarily required. Early removal of the cervical collar prevents contraction of the facet joints, postoperative atrophy, and dysfunction of the extensor muscles of the cervical spine33.
Clinical Comments
We believe that, among the available techniques (posterior, anterior, and combined anterior-posterior fusions), laminoplasty has the fewest complications, especially for patients with multilevel cervical compressive myelopathy. There were no significant differences in the rate of complications between posterior and anterior surgery in a large-scale study34. However, perioperative complications occurred more frequently in patients with longer (four or five-level) anterior fusions4,18. Even if the anterior fusion area was short, adjacent-segment disease frequently occurred and there was an increased risk that additional surgery would be required35.
Anterior and posterior surgical procedures are equally effective for the treatment of cervical spondylotic myelopathy36. Anterior surgery has a better clinical outcome in the early stages after surgery; however, posterior surgery has a similar clinical outcome in the later stages4. Anterior surgery was found to have a better neurological outcome in patients with severe ossification of the posterior longitudinal ligament (≥60%), although the complication rate remained high23.
Is French-door laminoplasty more beneficial than open-door laminoplasty? Neurological recovery is almost the same after both procedures. However, after conventional open-door laminoplasty, postoperative neurological deterioration might occur more frequently, due to laminar closure, than it does after French-door laminoplasty37.
Are autologous bone struts or hydroxyapatite spacers better? Hydroxyapatite is reportedly costlier and associated with postoperative complications15. The average nonunion rates of hydroxyapatite spacers were 21% in patients with cervical spondylotic myelopathy and 17% in those with ossification of the posterior longitudinal ligament15. Autologous bone struts are better; however, if we do not cut the C7 spinous process, it can be difficult to create sufficient bone struts. We use hydroxyapatite spacers as an alternative material only when there is not sufficient bone available to create the bone struts.
Footnotes
Based on an original article: Spine (Phila Pa 1976). 2014 Apr 15;39(8):642-7.
Disclosure: None of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of any aspect of this work. None of the authors, or their institution(s), have had any financial relationship, in the thirty-six months prior to submission of this work, with any entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. Also, no author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Oyama M, Hattori S, Moriwaki N. [A new method of cervical laminectomy]. The Central Japan Journal of Orthopaedic Surgery. 1973;16:792-4. Japanese. [Google Scholar]
- 2.Hirabayashi K, Satomi K. Operative procedure and results of expansive open-door laminoplasty. Spine (Phila Pa 1976). 1988. July;13(7):870-6. [DOI] [PubMed] [Google Scholar]
- 3.Nakashima H, Yukawa Y, Imagama S, Kanemura T, Kamiya M, Yanase M, Ito K, Machino M, Yoshida G, Ishikawa Y, Matsuyama Y, Ishiguro N, Kato F. Complications of cervical pedicle screw fixation for nontraumatic lesions: a multicenter study of 84 patients. J Neurosurg Spine. 2012. March;16(3):238-47. Epub 2011 Dec 16. [DOI] [PubMed] [Google Scholar]
- 4.Liu T, Xu W, Cheng T, Yang HL. Anterior versus posterior surgery for multilevel cervical myelopathy, which one is better? A systematic review. Eur Spine J. 2011. February;20(2):224-35. Epub 2010 Jun 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hirabayashi K. [Expansive open-door laminoplasty for cervical spondylotic myelopathy]. Shujutsu. 1978;32:1159-63. Japanese. [Google Scholar]
- 6.Hirabayashi K, Miyakawa J, Satomi K, Maruyama T, Wakano K. Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament. Spine (Phila Pa 1976). 1981. Jul-Aug;6(4):354-64. [DOI] [PubMed] [Google Scholar]
- 7.Kurokawa T, Tsuyama N, Tanaka H, Kobayashi M, Machida H, Izuka T, Hoshino Y, Hatsuyama Y. [Enlargement of the spinal canal by the sagittal splitting of the spinous processes]. Bessatsu Seikeigeka. 1982;2:234-40. Japanese. [Google Scholar]
- 8.Chiba K, Ogawa Y, Ishii K, Takaishi H, Nakamura M, Maruiwa H, Matsumoto M, Toyama Y. Long-term results of expansive open-door laminoplasty for cervical myelopathy—average 14-year follow-up study. Spine (Phila Pa 1976). 2006. December 15;31(26):2998-3005. [DOI] [PubMed] [Google Scholar]
- 9.Iwasaki M, Kawaguchi Y, Kimura T, Yonenobu K. Long-term results of expansive laminoplasty for ossification of the posterior longitudinal ligament of the cervical spine: more than 10 years follow up. J Neurosurg. 2002. March;96(2)(Suppl):180-9. [PubMed] [Google Scholar]
- 10.Satomi K, Nishu Y, Kohno T, Hirabayashi K. Long-term follow-up studies of open-door expansive laminoplasty for cervical stenotic myelopathy. Spine (Phila Pa 1976). 1994. March 1;19(5):507-10. [DOI] [PubMed] [Google Scholar]
- 11.Seichi A, Takeshita K, Ohishi I, Kawaguchi H, Akune T, Anamizu Y, Kitagawa T, Nakamura K. Long-term results of double-door laminoplasty for cervical stenotic myelopathy. Spine (Phila Pa 1976). 2001. March 1;26(5):479-87. [DOI] [PubMed] [Google Scholar]
- 12.Nakashima H, Kato F, Yukawa Y, Imagama S, Ito K, Machino M, Ishiguro N. Comparative effectiveness of open-door laminoplasty versus French-door laminoplasty in cervical compressive myelopathy. Spine (Phila Pa 1976). 2014. April 15;39(8):642-7. [DOI] [PubMed] [Google Scholar]
- 13.Machino M, Yukawa Y, Hida T, Ito K, Nakashima H, Kanbara S, Morita D, Kato F. Modified double-door laminoplasty in managing multilevel cervical spondylotic myelopathy: surgical outcome in 520 patients and technique description. J Spinal Disord Tech. 2013. May;26(3):135-40. [DOI] [PubMed] [Google Scholar]
- 14.Singh AK, Okudera H, Kobayashi S, Osawa M, Tokushige K. A newly designed attachment device of multipurpose frame for neuronavigator. Technical note. Acta Neurochir (Wien). 1994;129(1-2):97-9. [DOI] [PubMed] [Google Scholar]
- 15.Kimura A, Seichi A, Inoue H, Hoshino Y. Long-term results of double-door laminoplasty using hydroxyapatite spacers in patients with compressive cervical myelopathy. Eur Spine J. 2011. September;20(9):1560-6. Epub 2011 Feb 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fehlings MG, Wilson JR, Kopjar B, Yoon ST, Arnold PM, Massicotte EM, Vaccaro AR, Brodke DS, Shaffrey CI, Smith JS, Woodard EJ, Banco RJ, Chapman JR, Janssen ME, Bono CM, Sasso RC, Dekutoski MB, Gokaslan ZL. Efficacy and safety of surgical decompression in patients with cervical spondylotic myelopathy: results of the AOSpine North America prospective multi-center study. J Bone Joint Surg Am. 2013. September 18;95(18):1651-8. [DOI] [PubMed] [Google Scholar]
- 17.Matsumoto M, Chiba K, Toyama Y. Surgical treatment of ossification of the posterior longitudinal ligament and its outcomes: posterior surgery by laminoplasty. Spine (Phila Pa 1976). 2012. March 1;37(5):E303-8. [DOI] [PubMed] [Google Scholar]
- 18.Koller H, Hempfing A, Ferraris L, Maier O, Hitzl W, Metz-Stavenhagen P. 4- and 5-level anterior fusions of the cervical spine: review of literature and clinical results. Eur Spine J. 2007. December;16(12):2055-71. Epub 2007 Jun 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Suda K, Abumi K, Ito M, Shono Y, Kaneda K, Fujiya M. Local kyphosis reduces surgical outcomes of expansive open-door laminoplasty for cervical spondylotic myelopathy. Spine (Phila Pa 1976). 2003. June 15;28(12):1258-62. [DOI] [PubMed] [Google Scholar]
- 20.Yamazaki A, Homma T, Uchiyama S, Katsumi Y, Okumura H. Morphologic limitations of posterior decompression by midsagittal splitting method for myelopathy caused by ossification of the posterior longitudinal ligament in the cervical spine. Spine (Phila Pa 1976). 1999. January 1;24(1):32-4. [DOI] [PubMed] [Google Scholar]
- 21.Fujiyoshi T, Yamazaki M, Kawabe J, Endo T, Furuya T, Koda M, Okawa A, Takahashi K, Konishi H. A new concept for making decisions regarding the surgical approach for cervical ossification of the posterior longitudinal ligament: the K-line. Spine (Phila Pa 1976). 2008. December 15;33(26):E990-3. [DOI] [PubMed] [Google Scholar]
- 22.Reiter MF, Boden SD. Inflammatory disorders of the cervical spine. Spine (Phila Pa 1976). 1998. December 15;23(24):2755-66. [DOI] [PubMed] [Google Scholar]
- 23.Fujimori T, Iwasaki M, Okuda S, Takenaka S, Kashii M, Kaito T, Yoshikawa H. Long-term results of cervical myelopathy due to ossification of the posterior longitudinal ligament with an occupying ratio of 60% or more. Spine (Phila Pa 1976). 2014. January 1;39(1):58-67. [DOI] [PubMed] [Google Scholar]
- 24.Sakaura H, Hosono N, Mukai Y, Ishii T, Yoshikawa H. C5 palsy after decompression surgery for cervical myelopathy: review of the literature. Spine (Phila Pa 1976). 2003. November 1;28(21):2447-51. [DOI] [PubMed] [Google Scholar]
- 25.Imagama S, Matsuyama Y, Yukawa Y, Kawakami N, Kamiya M, Kanemura T, Ishiguro N; Nagoya Spine Group. C5 palsy after cervical laminoplasty: a multicentre study. J Bone Joint Surg Br. 2010. March;92(3):393-400. [DOI] [PubMed] [Google Scholar]
- 26.Kawaguchi Y, Kanamori M, Ishihara H, Ohmori K, Nakamura H, Kimura T. Minimum 10-year followup after en bloc cervical laminoplasty. Clin Orthop Relat Res. 2003. June;411:129-39. [DOI] [PubMed] [Google Scholar]
- 27.Hase H, Watanabe T, Hirasawa Y, Hashimoto H, Miyamoto T, Chatani K, Kageyama N, Mikami Y. Bilateral open laminoplasty using ceramic laminas for cervical myelopathy. Spine (Phila Pa 1976). 1991. November;16(11):1269-76. [DOI] [PubMed] [Google Scholar]
- 28.Hyun SJ, Rhim SC, Roh SW, Kang SH, Riew KD. The time course of range of motion loss after cervical laminoplasty: a prospective study with minimum two-year follow-up. Spine (Phila Pa 1976). 2009. May 15;34(11):1134-9. [DOI] [PubMed] [Google Scholar]
- 29.Wang SJ, Jiang SD, Jiang LS, Dai LY. Axial pain after posterior cervical spine surgery: a systematic review. Eur Spine J. 2011. February;20(2):185-94. Epub 2010 Oct 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Katsumi K, Yamazaki A, Watanabe K, Ohashi M, Shoji H. Can prophylactic bilateral C4/C5 foraminotomy prevent postoperative C5 palsy after open-door laminoplasty?: a prospective study. Spine (Phila Pa 1976). 2012. April 20;37(9):748-54. [DOI] [PubMed] [Google Scholar]
- 31.Xia Y, Xia Y, Shen Q, Li H, Xu T. Influence of hinge position on the effectiveness of expansive open-door laminoplasty for cervical spondylotic myelopathy. J Spinal Disord Tech. 2011. December;24(8):514-20. [DOI] [PubMed] [Google Scholar]
- 32.Fujimura Y, Nishi Y. Atrophy of the nuchal muscle and change in cervical curvature after expansive open-door laminoplasty. Arch Orthop Trauma Surg. 1996;115(3-4):203-5. [DOI] [PubMed] [Google Scholar]
- 33.Iizuka H, Nakagawa Y, Shimegi A, Tsutsumi S, Toda N, Takagishi K, Shimizu T. Clinical results after cervical laminoplasty: differences due to the duration of wearing a cervical collar. J Spinal Disord Tech. 2005. December;18(6):489-91. [DOI] [PubMed] [Google Scholar]
- 34.Fehlings MG, Smith JS, Kopjar B, Arnold PM, Yoon ST, Vaccaro AR, Brodke DS, Janssen ME, Chapman JR, Sasso RC, Woodard EJ, Banco RJ, Massicotte EM, Dekutoski MB, Gokaslan ZL, Bono CM, Shaffrey CI. Perioperative and delayed complications associated with the surgical treatment of cervical spondylotic myelopathy based on 302 patients from the AOSpine North America Cervical Spondylotic Myelopathy Study. J Neurosurg Spine. 2012. May;16(5):425-32. Epub 2012 Feb 10. [DOI] [PubMed] [Google Scholar]
- 35.Matsumoto M, Okada E, Ichihara D, Watanabe K, Chiba K, Toyama Y, Fujiwara H, Momoshima S, Nishiwaki Y, Iwanami A, Ikegami T, Takahata T, Hashimoto T. Anterior cervical decompression and fusion accelerates adjacent segment degeneration: comparison with asymptomatic volunteers in a ten-year magnetic resonance imaging follow-up study. Spine (Phila Pa 1976). 2010. January 1;35(1):36-43. [DOI] [PubMed] [Google Scholar]
- 36.Fehlings MG, Barry S, Kopjar B, Yoon ST, Arnold P, Massicotte EM, Vaccaro A, Brodke DS, Shaffrey C, Smith JS, Woodard E, Banco RJ, Chapman J, Janssen M, Bono C, Sasso R, Dekutoski M, Gokaslan ZL. Anterior versus posterior surgical approaches to treat cervical spondylotic myelopathy: outcomes of the prospective multicenter AOSpine North America CSM study in 264 patients. Spine (Phila Pa 1976). 2013. December 15;38(26):2247-52. [DOI] [PubMed] [Google Scholar]
- 37.Matsumoto M, Watanabe K, Hosogane N, Tsuji T, Ishii K, Nakamura M, Chiba K, Toyama Y. Impact of lamina closure on long-term outcomes of open-door laminoplasty in patients with cervical myelopathy: minimum 5-year follow-up study. Spine (Phila Pa 1976). 2012. July 1;37(15):1288-91. [DOI] [PubMed] [Google Scholar]





