Overview
Introduction
The correct usage of preoperative and intraoperative imaging allows fixation of posterior pelvic ring injuries with safely positioned iliosacral screws in the setting of sacral dysmorphism.
Step 1: Preoperative Planning
Obtain CT reformats along the longitudinal axis of the sacrum to determine the orientation and diameter of the osseous corridor for selection of the ideal screw size, length, and trajectory.
Step 2: Patient Positioning
Proper positioning enables reduction and accurate iliosacral screw placement.
Step 3: Fracture Reduction
Reduction of the posterior pelvic ring confers stability; if closed reduction is unsuccessful, proceed with open reduction.
Step 4: Identification of the Entry Point
The entry point for an iliosacral screw into the upper sacral segment of a dysmorphic pelvis lies more posterior and caudal on the outer table of the posterior ilium than does a transsacral screw; adjust the entry point on the basis of inlet and outlet fluoroscopic views.
Step 5: Drilling Technique
Insert a stout cannulated drill bit of 4.5 to 5 mm (depending on the core diameter of the intended iliosacral screw) over the Kirschner wire and drill it into the sacral body under fluoroscopic guidance, in accordance with the preoperative plan.
Step 6: Screw Insertion
With the guidewire in the ideal position, measure the screw length off the inserted guidewire and advance a tap into the pathway; insert the screw and verify its position on the inlet, outlet, and lateral sacral views.
Results
Understanding the three-dimensional anatomy of the posterior pelvic ring is essential to successful reduction and fixation of unstable pelvic injuries with use of percutaneous iliosacral screws.
Introduction
The correct usage of preoperative and intraoperative imaging allows fixation of posterior pelvic ring injuries with safely positioned iliosacral screws in the setting of sacral dysmorphism.
Percutaneous treatment of unstable pelvic ring injuries is a technically demanding procedure with a steep learning curve. An in-depth understanding of pelvic osseous, vascular, and neural anatomy is vital to prevent serious complications. The surgeon must feel comfortable translating difficult fluoroscopic imaging into a three-dimensional spatial visualization to attain reduction and establish an effective and safe screw trajectory. Even surgeons experienced in the use of percutaneous iliosacral screws must be ready to adjust their technique when confronted with a dysmorphic anatomic phenotype (Video 1).
Video 1.
Case example of preplanning and the surgical technique for the percutaneous iliosacral screw fixation of an unstable pelvic fracture.
Sacral dysmorphism has been shown to be present in 40% of the general population1,2. The dysmorphic sacrum differs from a nondysmorphic sacrum in the morphology of the osseous corridors that connect the posterior ilium to the sacral bodies via the sacroiliac joint. In the dysmorphic upper sacral segment, this corridor has a smaller cross-sectional area and a more acute angle in the coronal and axial planes than are seen in a nondysmorphic sacrum3,4.The morphology of the osseous corridor in sacral dysmorphism has been previously described as having five associated qualitative characteristics identifiable on the outlet radiograph5. A transiliac, transsacral screw confers the greatest resistance to vertical displacement; however, it is not possible to use such a screw in certain patients with upper sacral segment dysplasia5-11. Preoperative planning involves coronal and axial reformats of a 0.0625-mm-slice computed tomography (CT) scan along the longitudinal axis of the sacrum. These reformats define the morphology and ideal trajectory of iliosacral screw placement, and use of the sacral dysmorphism score can identify patients in whom use of a transiliac, transsacral screw is highly risky or impossible1.
The surgical procedure starts with appropriate supine positioning and verification of adequate fluoroscopic inlet, outlet, and lateral sacral views. The coronal and axial angulation measured during preoperative planning can then be used to determine the best insertion site and trajectory of the iliosacral screw. Reduction of the fracture is enabled by positioning with a longitudinal central bump underneath the sacrum. Careful assessment of the trajectory of the guidewire and drill on outlet, inlet, and lateral sacral fluoroscopic views is necessary to ensure an intraosseous trajectory of each iliosacral screw12,13. Alternatively, surgical navigation, which allows real-time visualization of screw placement without radiation, can be used when combined with intraoperative CT for registration; however, the same principles regarding accurate screw placement apply (see Clinical Comments section below). The drill can be used to subtly change the guidewire trajectory. During screw placement, outlet, inlet, and lateral sacral views confirm the final trajectory, and the obturator outlet view can verify cortical seating of the iliosacral screw.
Step 1: Preoperative Planning
Obtain CT reformats along the longitudinal axis of the sacrum to determine the orientation and diameter of the osseous corridor for selection of the ideal screw size, length, and trajectory.
When a pelvic outlet radiograph demonstrates signs of sacral dysmorphism (Fig. 1), obtain a fine-cut (0.625-mm-slice-thickness) CT scan through the sacrum to confirm these findings and aid in surgical planning.
Reformat the CT scan in the true coronal and axial planes by defining the sagittal axis of the reformats as the posterior border of the sacrum and the axial axis of the reformats along the upper end plate of the second sacral segment. This will provide coronal and axial cuts that accurately represent the trajectory of the upper and second sacral osseous corridors (Figs. 2-A through 2-D) and correspond with intraoperative inlet and outlet fluoroscopic projections.
Select an axial reformat that maximizes the length of bone perpendicular to the axis of the osseous corridor between the ipsilateral ala and the first neural foramen. This represents the diameter of the upper sacral segment corridor. Given that this is not a perfect cylinder, if the diameter is <10 mm, take caution with insertion of a screw 6.5 mm in diameter or larger.
Measure the coronal angulation of the upper sacral segment corridor, defined as the angle subtended by a line connecting the iliac crests and a second line along the axis of the upper sacral segment osseous corridor (Fig. 3-A).
Measure the axial angulation of the upper sacral segment corridor, defined as the angle subtended by a line connecting the posterior iliac spines and a second line along the axis of the upper sacral segment osseous corridor (Fig. 3-B).
Calculate the sacral dysmorphism score with the formula: (first sacral coronal angle) + 2(first sacral axial angle). The higher the score, the less likely there is a safe transsacral osseous corridor.
The ideal screw is one that best augments stability. The entry site can vary depending on the injury pattern. With an entry site centered on the axis of the ipsilateral osseous corridor, the measured coronal angulation estimates the angle of screw insertion relative to a horizontal line parallel to the superior end plate of the upper sacral segment in the coronal plane of the sacrum on the outlet image. The measured axial angulation estimates the angle between the longitudinal axis of the osseous corridor and the horizontal in the axial plane of the sacrum visualized on the inlet projection.
Analyze the second sacral segment in the same manner as the upper sacral segment. In many dysmorphic sacra, the size and orientation of the second sacral segment are increased, enabling placement of one or two transsacral screws.
Fig. 1.
A three-dimensional reconstruction and holographic reconstruction of an outlet image that show all of the morphologic characteristics of sacral dysmorphism: (1) a first sacral segment not recessed in the pelvis, (2) an acute alar slope to the first sacral segment, (3) mamillary processes, (4) noncircular sacral foramina, and (5) a residual disc between the first and second sacral segments. There is a zone-222 sacral fracture.
Fig. 2-A.
A mid-corridor coronal cut of the CT scan reformatted along the axis of the upper sacral segment, which demonstrates a zone-222 sacral fracture and the true coronal angulation of the first sacral segment.
Fig. 2-B.
A mid-corridor coronal cut of the CT scan reformatted along the axis of the second sacral segment.
Fig. 2-C.
A mid-corridor axial cut of the CT scan reformatted along the axis of the upper sacral segment, which demonstrates a zone-222 sacral fracture and the true axial angulation of the first sacral osseous corridor.
Fig. 2-D.
A mid-corridor axial cut of the CT scan reformatted along the axis of the second sacral segment.
Fig. 3-A.
The method for determining the coronal angulation of the upper sacral segment begins with a line drawn to connect the iliac crests. A line is then drawn along the axis of the upper sacral segment. The coronal angulation is the angle subtended by these lines.
Fig. 3-B.
The method for determining the axial angulation of the upper sacral segment begins with a line drawn to connect the posterior iliac spines. A line is then drawn along the axis of the upper sacral segment. The axial angulation is the angle subtended by these lines.
Step 2: Patient Positioning
Proper positioning enables reduction and accurate iliosacral screw placement.
Position the patient supine on a radiolucent table. Slide the patient toward the table edge ipsilateral to the injured side to allow the surgeon’s hand to drop below the level of the table, thus directing the screw anteriorly in order to achieve proper placement into the upper sacral segment. There must be adequate clearance beneath the table for the full range of fluoroscopic imaging. Some patients require extreme angulation of the fluoroscopic unit to obtain a true outlet image.
Place a central sacral support underneath the sacrum. This positioning aid is typically made from two or three folded sheets or blankets wide enough to support the posterior superior iliac spines and long enough to elevate the ischial tuberosities. This central sacral support lifts the pelvis evenly off the operating table to allow for unobstructed angled trajectories for placement of iliosacral screws in accordance with Step 1. This facilitates reduction and access to the posterior pelvic ring (Fig. 4).
Confirm the adequacy of outlet, inlet, and lateral sacral views prior to sterile skin preparation.
Place adhesive drapes transversely along the inferior costal margin to meet a drape placed longitudinally along the posterior aspect of the buttock where it is in contact with the table. Proper draping allows sterile preparation of skin caudal to the inferior costal margin anteriorly and laterally. Maintain the posterior sterile margin as close to the table as possible, to take advantage of the elevated position of the pelvis on the central sacral support and to allow as much freedom as possible for the insertion angle of the iliosacral screw. The inferior extent of the skin preparation is a horizontal line at or just below the anterosuperior aspect of the symphysis pubis. The skin preparation can be extended distally to incorporate the hindquarter ipsilateral to the injured hemipelvis should access to the limb be required to achieve a manipulative reduction intraoperatively (Figs. 5-A and 5-B).
Fig. 4.
A central sacral support, fashioned from two or three folded sheets or blankets, allows access to unobstructed angled trajectories for placement of iliosacral screws along the true axis of the osseous corridor.
Fig. 5-A.
Adhesive drapes are placed along the inferior costal margin and along the posterior aspect of the buttock where it is in contact with the table to maximize the freedom and potential angles of approach to the sacral corridors.
Fig. 5-B.
The prepared field can include the ipsilateral hindquarter to allow sterile traction and intraoperative manipulation. In this case, Schanz pins have been placed in both anterior inferior iliac spines to augment reduction maneuvers.
Step 3: Fracture Reduction
Reduction of the posterior pelvic ring confers stability; if closed reduction is unsuccessful, proceed with open reduction.
Verify the vertical displacement of the posterior pelvic ring on the outlet view and the rotational and anterior-posterior translation on the inlet view.
A distal femoral traction pin may be placed to facilitate reduction. If the anesthetist induces adequate paralysis by using muscle relaxant agents, >15 lb (>6.8 kg) of traction is seldom necessary. Other augments to reduction may include manipulation by placing a percutaneous Schanz pin in the gluteus medius tubercle, the anterior inferior iliac spine, and/or the trochanteric line of the femur, with or without use of external fixation or a universal distractor.
When the symphysis pubis is displaced in conjunction with the posterior pelvic ring, perform an open reduction of the symphysis pubis through a Pfannenstiel approach to aid in the indirect reduction of the posterior pelvic ring.
If closed reduction of the posterior pelvic ring is unsuccessful, perform an open reduction via an anterior or posterior approach, according to your preference. Reduction both confers stability and is vital to safe iliosacral screw placement14.
Step 4: Identification of the Entry Point
The entry point for an iliosacral screw into the upper sacral segment of a dysmorphic pelvis lies more posterior and caudal on the outer table of the posterior ilium than does a transsacral screw; adjust the entry point on the basis of inlet and outlet fluoroscopic views.
Obtain an inlet view centered on the anterior aspect of the sacroiliac joint on the side of the injury. This image plane corresponds to the CT axial reformat. In order to move the entry point anterior or posterior, or alter the trajectory to aim obliquely anterior and medial (Step 1: axial angle), move in the plane orthogonal to the fluoroscopy beam.
Obtain an outlet view centered on the superior aspect of the sacroiliac joint on the side of the injury. This image plane corresponds to the CT coronal reformat. In order to move the entry point cephalad or caudal, or alter the trajectory to aim obliquely superior and medial (Step 1: coronal angle), move in the plane orthogonal to the fluoroscopy beam.
Place a 1.6-mm Kirschner wire percutaneously through the gluteal musculature to rest on the lateral cortex of the posterior ilium. Evaluate the location and trajectory of the Kirschner wire on the inlet (Fig. 6-A) and outlet (Fig. 6-B) projections and reorient it iteratively until the wire is satisfactorily aimed into the body of the upper sacral segment by way of the osseous corridor of bone superior and anterior to the first neural foramen.
The entry point in a dysmorphic pelvis will be more posterior and caudal than that in a nondysmorphic pelvis, in which a transiliac, transsacral corridor may be present. The lateral view is of less value for identification of the entry point in a dysmorphic pelvis given the obliquity of the orientation of the safe zone and its superimposition on the iliac cortical density.
Fig. 6-A.
The entry point is demonstrated on this inlet view. It is positioned central along the osseous corridor of the first sacral segment and is targeted along the axis of the corridor in the anterior-to-posterior plane.
Fig. 6-B.
The entry point is demonstrated on this outlet view. It is positioned central along the osseous corridor of the first sacral segment and is targeted along the axis of the corridor in the superior-to-inferior plane.
Step 5: Drilling Technique
Insert a stout cannulated drill bit of 4.5 to 5 mm (depending on the core diameter of the intended iliosacral screw) over the Kirschner wire and drill it into the sacral body under fluoroscopic guidance, in accordance with the preoperative plan.
Make a 1-cm longitudinally oriented incision through the skin and subcutaneous tissue centered on the properly positioned Kirschner wire.
Insert the cannulated pin sleeve for the screw system of choice (6.5 to 7.5 mm is most common) over the Kirschner wire and stabilize it on the outer table of the ilium. Remove the Kirschner wire and replace it with a terminally threaded guidewire from the chosen screw system. Using the solid pin-sleeve soft-tissue protector, small additional adjustments to the entry point and trajectory can still be made.
Once the entry point is optimized, insert the Kirschner wire 5 mm, taking care not to enter the sacroiliac joint. While it is possible to advance the guidewire to its target in the sacral body, we find that guidewires tend to wander off course through long osseous corridors. In dysmorphic sacra, where the safe zone may be particularly narrow and the risk of cortical perforation high, we recommend an alternative drilling technique.
The terminally threaded guidewire serves as an anchor for the cannulated drill bit, which is advanced over it in a drill-forward mode.
Prior to advancing the drill into the sacroiliac joint, use inlet and outlet views to confirm the intended trajectory. When the drill crosses the sacroiliac joint, the cortex of the medial aspect of the ilium and lateral aspect of the sacrum set the screw trajectory. Even small changes in the trajectory are more difficult to achieve after the sacroiliac joint has been crossed.
A marked decrease in resistance is encountered in the sacral ala as a result of its lower-density bone, even in the absence of a fracture at this site. Check inlet and outlet projections repeatedly to confirm proper positioning and avoidance of any deflection (Figs. 7-A and 7-B).
Advance the drill in oscillation mode to avoid etching or perforating the thin anterior cortex of the sacral ala or neural foramen.
When the drill approaches the area of bone just above the first neural foramen, a lateral image of the sacrum and pelvis is recommended (Fig. 8).
Preoperative planning should alert you to the fact that, in the dysmorphic upper sacral segment, the sacral ala and most of the body may be anterior and superior to the iliac cortical density. Therefore, the lateral projection should demonstrate the tip of the cannulated drill bit aimed through the iliac cortical density, for the upper sacral segment body.
Return to alternating between inlet and outlet fluoroscopic projections, if the lateral image confirms proper execution. Advance the drill above the first neural foramen and into the sacral body in oscillation mode. The bone in the body of the sacrum is denser so you will encounter greater resistance. However, excessive resistance should prompt concern about impending cortical perforation and all fluoroscopic views should again be evaluated prior to continuing.
Stop advancing the drill when you encounter increased resistance or come close to (within 2 mm of) either the superior end plate (as seen on the outlet view) or the anterior cortex (as seen on the inlet view) of the contralateral aspect of the sacral body (Figs. 9-A and 9-B).
Remove the drill and use another guidewire to “sound” and palpate the path of the intended screw to evaluate for cortical perforation. If none is found, insert the guidewire in reverse with its blunt end gently lodged in the cancellous bone of the sacral body at the end of the drilled path (Figs. 10-A and 10-B).
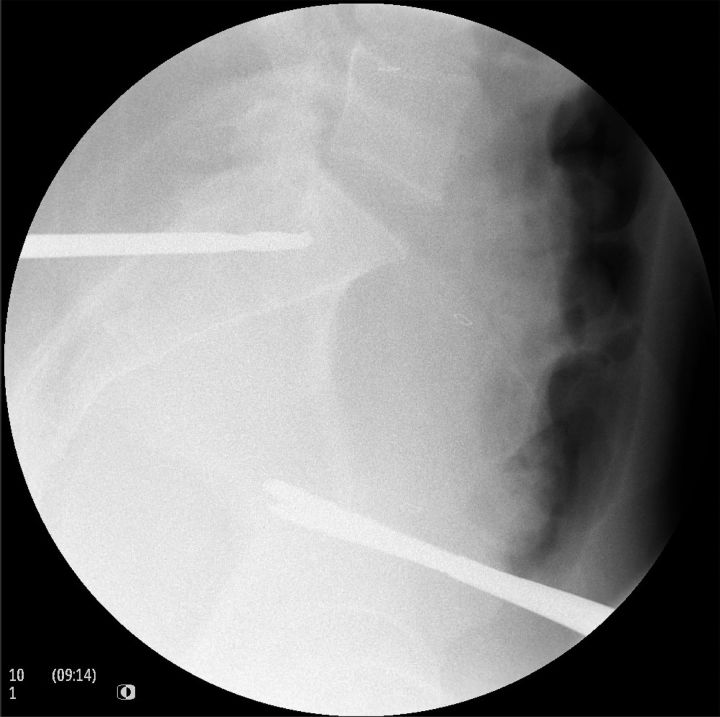
Fig. 7-A.
Drilling technique demonstrated on the inlet view. The cannulated drill is advanced along the desired trajectory, along the axis of the osseous corridor and along the trajectory of the guidewire, with a drill-forward technique. This enables subtle adjustments in the trajectory, which can be confirmed on alternating inlet and outlet views, before the drill traverses the sacroiliac joint.
Fig. 7-B.
The outlet view confirms the trajectory of the drill in the superior-to-inferior plane. Advancing the drill in oscillation mode provides good tactile feedback and reduces etching to prevent perforation through the narrow anterior cortex of the sacral ala.
Fig. 8.
The lateral sacral view is recommended to reduce the risk of perforation into the nerve root tunnel or sacral spinal canal. This is most illustrative when, as seen in Fig. 7-B, the drill has reached a point superior to the neural foramen on the outlet view. At this point, the lateral projection should demonstrate the tip of the cannulated drill bit aimed through the iliac cortical density, for the upper sacral segment body.
Fig. 9-A.
As visualized on the inlet view, the drill should be advanced until the surgeon encounters increased resistance or comes into close proximity to the anterior cortex of the contralateral sacral ala.
Fig. 9-B.
As visualized on the outlet view, the drill should be advanced until the surgeon encounters increased resistance or comes into close proximity to the superior end plate.
Fig. 10-A.
The drill has been removed, and the guidewire has been inserted with its blunt end leading. The drilled path can be sounded to check for perforation. The inlet view is shown here with the guidewire gently lodged at the end of the drilled path.
Fig. 10-B.
This outlet view shows the guidewire gently lodged at the end of the drilled path.
Step 6: Screw Insertion
With the guidewire in the ideal position, measure the screw length off the inserted guidewire and advance a tap into the pathway; insert the screw and verify its position on the inlet, outlet, and lateral sacral views.
With the desired trajectory confirmed, use the guidewire to determine the ideal screw length either by employing a depth gauge or by measuring the difference in length using a second guidewire placed adjacent and parallel to the first, onto the outer table of the ilium.
Advance a tap into the pathway, if necessary, and then insert the screw. As it is advanced along the guidewire, use biplanar fluoroscopy to confirm that the pin is not binding and is advancing properly (Figs. 11-A and 11-B).
Depending on whether a neutralization screw (used to hold the sacroiliac joint without obtaining compression) or a lag screw (used to compress the sacroiliac joint) is desired, a fully or partially threaded screw may be chosen.
A washer may be used to increase the surface area of contact between the screw head and the lateral cortex of the ilium, and will be well visualized as flush on the obturator inlet view (Fig. 12).
Again verify the final screw position on the lateral sacral fluoroscopic view (Fig. 13) as well as on inlet and outlet imaging (Fig. 14). Use of a CT scan may be desirable to assess screw placement more accurately.
Fig. 11-A.
The screw is inserted along the guidewire after advancement of the cannulated tap. Note the axial orientation on the inlet view along the axis of the upper sacral segment osseous corridor. Shown here also is the entry point for a second screw placed through the safe transsacral corridor in the second sacral segment.
Fig. 11-B.
The screw is inserted along the guidewire after advancement of the cannulated tap. Note the coronal orientation on the outlet view along the axis of the upper sacral segment osseous corridor. Shown here also is the entry point for a second screw placed through the safe transsacral corridor in the second sacral segment.
Fig. 12.
A washer may be used to increase cortical contact. The obturator inlet view provides verification of seating of the screw and washer against the iliac cortex.
Fig. 13.
The final screw position should always be confirmed on the lateral sacral view.
Fig. 14.
Final radiographs showing the upper sacral segment screw along the axis of the safe corridor and the transsacral second sacral segment screw.
Results
Understanding the three-dimensional anatomy of the posterior pelvic ring is essential to successful reduction and fixation of unstable pelvic injuries with use of percutaneous iliosacral screws4,14-16. The key to success is the execution of a detailed preoperative plan based on an appropriately reformatted CT image and an understanding of information provided by intraoperative fluoroscopic imaging. This becomes a greater challenge in the setting of sacral dysmorphism. In a study of 104 uninjured pelves, we found the prevalence of sacral dysmorphism to be 41% and that the two most important predictors of a safe transsacral corridor were the true coronal and axial angulation measurements of the upper sacral segment1. These two measurements must be made on true axial and coronal images, which require reformatting of the CT scan perpendicularly along the plane of the sacrum.
In our study1, we determined that the relationship between the coronal and axial orientation of the upper sacral segment could be used to predict the presence of a safe osseous tunnel for the placement of a transsacral screw. The coronal and axial angles are measured from the reformatted CT scan, after which the sacral dysmorphism score can be calculated with the formula: (first sacral coronal angle) + 2(first sacral axial angle). The greater the sacral dysmorphism score, the lower the prevalence of an osseous corridor sufficient for transsacral fixation.
Our recent study1 suggests that >80% of sacra with a sacral dysmorphism score of <30 have a safe transsacral corridor, whereas fewer than half of sacra with a score of >30 have a safe transsacral corridor. Specific data by quintile are presented in Table I.
TABLE I.
Sacral Dysmorphism Scores by Quintile in the Cohort
| Quintile | With Safe Transsacral Corridor (%) | Minimum Score | Maximum Score |
| 1 | 95 | 1.8 | 18 |
| 2 | 80 | 18.6 | 32.3 |
| 3 | 45 | 34.3 | 43.4 |
| 4 | 15 | 44.6 | 70.4 |
| 5 | 0 | 72.2 | 116.5 |
The goal of iliosacral screw fixation is maintaining reduction with safe intraosseous fixation that can resist physiologic loading of the injured posterior pelvic ring. The safest trajectory of an iliosacral screw is along the central axis of the ipsilateral osseous corridor. This trajectory can be determined with use of appropriate preoperative imaging and calculation. Adjustments to this trajectory can be made cautiously when the anatomy permits. In the dysmorphic sacrum, the trajectory is more angulated caudal to cephalad and posterior to anterior, and the anatomy is less forgiving of adjustments. The steep and angulated anterior cortex of the sacral ala can be difficult to assess on intraoperative fluoroscopy.
What to Watch For
Indications
Contraindications
A small osseous corridor (<10 mm in its largest diameter) between the neural foramen and anterior cortex of the sacrum on axial reformats or between the upper and second neural foramina on coronal reformats4.
Inability to attain an adequate reduction.
Fluoroscopic imaging that is not adequate to accurately discern the complex osseous anatomy of the sacrum intraoperatively. Factors that limit the quality of fluoroscopic imaging are large body habitus, bowel gas, pneumoperitoneum, and contrast in the bowel or bladder.
Pitfalls & Challenges
Improper positioning and draping can prevent access and limit imaging, increasing the technical difficulty and increasing the risk of extraosseous screw placement.
The iliac cortical density, seen on the lateral sacral view, is an excellent landmark for iliosacral screw placement5,16. In patients without dysmorphic sacral features, the entire screw trajectory should remain posterior to this line. This prevents anterior and superior screw placement, which can perforate the superoanterior cortex of the sacrum and injure the L5 nerve root. Unfortunately, in a dysmorphic sacrum, this line may be poorly defined, and the angle necessary to prevent posterior penetration into the spinal canal may require the tip of the screw to be anterior to the iliac cortical density.
Given the ovoid shape of the osseous corridor for iliosacral screw placement, it is impossible to rule out cortical perforation with orthogonal radiographs or fluoroscopy, especially when the axis of screw placement is not parallel to the beam. Therefore, we recommend using techniques described above that augment the surgeon’s tactile feedback and control of instrumentation to improve the safety of this procedure.
Clinical Comments
The goal of iliosacral screw fixation is stabilization of the pelvic ring after reduction is achieved, in order to prevent late displacement. Increased length and diameter of screws, and transiliac, transsacral screw placement, provide increased stability. Ideally, multiple long screws would be placed in both the upper and the second sacral segment. However, screws must be placed safely, meaning that they must be fully contained within the osseous corridors that traverse the sacrum. There is an inherent balance between attempting to achieve maximum fixation and ensuring osseous containment. Use of the proposed preoperative planning techniques as well as adequate quality of, and careful attention to, intraoperative fluoroscopic imaging minimize the risk of extraosseous screw placement and neurovascular injury.
While these techniques described here are primarily for instrumentation of the upper sacral segment of a dysmorphic sacrum, they are generalizable to iliosacral screw placement in nondysmorphic pelves as well.
Intraoperative CT and navigation technologies are likely to facilitate, and improve the accuracy of, placement of internal fixation, as has already been shown for internal fixation of the spine. However, we caution surgeons against becoming reliant on these tools at the expense of a detailed understanding of the surgical and radiographic anatomy and a thoughtful preoperative plan. Understanding the principles defined and illustrated in this technique paper and video are paramount to obtaining an optimal outcome when treating posterior pelvic ring injuries with percutaneous techniques.
Footnotes
Based on an original article: J Bone Surg Am. 2014 Jul 16;96(14):e120.
Disclosure: None of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of any aspect of this work. None of the authors, or their institution(s), have had any financial relationship, in the thirty-six months prior to submission of this work, with any entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. Also, no author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Kaiser SP, Gardner MJ, Liu J, Routt MLJ, Jr, Morshed S. Anatomic determinants of sacral dysmorphism and implications for safe iliosacral screw placement. J Bone Joint Surg Am. 2014. July 16;96(14):e120. [DOI] [PubMed] [Google Scholar]
- 2.Miller AN, Routt MLJ., Jr Variations in sacral morphology and implications for iliosacral screw fixation. J Am Acad Orthop Surg. 2012. January;20(1):8-16. [DOI] [PubMed] [Google Scholar]
- 3.Conflitti JM, Graves ML, Chip Routt MLJ., Jr Radiographic quantification and analysis of dysmorphic upper sacral osseous anatomy and associated iliosacral screw insertions. J Orthop Trauma. 2010. October;24(10):630-6. [DOI] [PubMed] [Google Scholar]
- 4.Gardner MJ, Morshed S, Nork SE, Ricci WM, Chip Routt MLJ., Jr Quantification of the upper and second sacral segment safe zones in normal and dysmorphic sacra. J Orthop Trauma. 2010. October;24(10):622-9. [DOI] [PubMed] [Google Scholar]
- 5.Routt MLJ, Jr, Simonian PT, Agnew SG, Mann FA. Radiographic recognition of the sacral alar slope for optimal placement of iliosacral screws: a cadaveric and clinical study. J Orthop Trauma. 1996;10(3):171-7. [DOI] [PubMed] [Google Scholar]
- 6.Simonain PT, Routt C, Jr, Harrington RM, Tencer AF. Internal fixation for the transforaminal sacral fracture. Clin Orthop Relat Res. 1996. February;(323):202-9. [DOI] [PubMed] [Google Scholar]
- 7.Yinger K, Scalise J, Olson SA, Bay BK, Finkemeier CG. Biomechanical comparison of posterior pelvic ring fixation. J Orthop Trauma. 2003. August;17(7):481-7. [DOI] [PubMed] [Google Scholar]
- 8.Routt MLJ, Jr, Simonian PT, Mills WJ. Iliosacral screw fixation: early complications of the percutaneous technique. J Orthop Trauma. 1997. November;11(8):584-9. [DOI] [PubMed] [Google Scholar]
- 9.Keating JF, Werier J, Blachut P, Broekhuyse H, Meek RN, O’Brien PJ. Early fixation of the vertically unstable pelvis: the role of iliosacral screw fixation of the posterior lesion. J Orthop Trauma. 1999. February;13(2):107-13. [DOI] [PubMed] [Google Scholar]
- 10.Griffin DR, Starr AJ, Reinert CM, Jones AL, Whitlock S. Vertically unstable pelvic fractures fixed with percutaneous iliosacral screws: does posterior injury pattern predict fixation failure? J Orthop Trauma. 2003. July;17(6):399-405. [DOI] [PubMed] [Google Scholar]
- 11.Gardner MJ, Routt MLJ., Jr Transiliac-transsacral screws for posterior pelvic stabilization. J Orthop Trauma. 2011. June;25(6):378-84. [DOI] [PubMed] [Google Scholar]
- 12.Xu R, Ebraheim NA, Robke J, Yeasting RA. Radiologic evaluation of iliosacral screw placement. Spine. 1996. March 1;21(5):582-8. [DOI] [PubMed] [Google Scholar]
- 13.Graves ML, Routt MLJ., Jr Iliosacral screw placement: are uniplanar changes realistic based on standard fluoroscopic imaging? J Trauma. 2011. July;71(1):204-8; discussion 208. [DOI] [PubMed] [Google Scholar]
- 14.Reilly MC, Bono CM, Litkouhi B, Sirkin M, Behrens FF. The effect of sacral fracture malreduction on the safe placement of iliosacral screws. J Orthop Trauma. 2003. February;17(2):88-94. [DOI] [PubMed] [Google Scholar]
- 15.Karachalios T, Zibis AH, Zintzaras E, Bargiotas K, Karantanas AH, Malizos KN. An anatomical update on the morphologic variations of S1 and S2. Orthopedics. 2010. October;33(10):733 Epub 2010 Oct 11. [DOI] [PubMed] [Google Scholar]
- 16.Ziran BH, Wasan AD, Marks DM, Olson SA, Chapman MW. Fluoroscopic imaging guides of the posterior pelvis pertaining to iliosacral screw placement. J Trauma. 2007. February;62(2):347-56; discussion 356. [DOI] [PubMed] [Google Scholar]
- 17.Routt MLJ, Jr, Kregor PJ, Simonian PT, Mayo KA. Early results of percutaneous iliosacral screws placed with the patient in the supine position. J Orthop Trauma. 1995. June;9(3):207-14. [DOI] [PubMed] [Google Scholar]
- 18.Osterhoff G, Ossendorf C, Wanner GA, Simmen HP, Werner CM. Posterior screw fixation in rotationally unstable pelvic ring injuries. Injury. 2011. October;42(10):992-6. Epub 2011 May 6. [DOI] [PubMed] [Google Scholar]
- 19.Mullis BH, Sagi HC. Minimum 1-year follow-up for patients with vertical shear sacroiliac joint dislocations treated with iliosacral screws: does joint ankylosis or anatomic reduction contribute to functional outcome? J Orthop Trauma. 2008. May-Jun;22(5):293-8. [DOI] [PubMed] [Google Scholar]
- 20.Schweitzer D, Zylberberg A, Córdova M, Gonzalez J. Closed reduction and iliosacral percutaneous fixation of unstable pelvic ring fractures. Injury. 2008. August;39(8):869-74. Epub 2008 Jul 14. [DOI] [PubMed] [Google Scholar]
- 21.Cole JD, Blum DA, Ansel LJ. Outcome after fixation of unstable posterior pelvic ring injuries. Clin Orthop Relat Res. 1996. August;(329):160-79. [DOI] [PubMed] [Google Scholar]
- 22.Denis F, Davis S, Comfort T. Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop Relat Res. 1988. February;(227):67-81. [PubMed] [Google Scholar]