Abstract
Objective. To design and evaluate the use of simulations in preparing students to identify and reduce medication errors and promote patient safety.
Methods. Third-year pharmacy students used methods of root cause analysis (RCA) to determine the cause of a medication error in three simulated pharmacy settings. Before and after the activity, students completed an anonymous survey. They also completed a modified Healthcare Professionals Patient Safety Assessment instrument to measure changes in their knowledge, skills, and attitudes.
Results. Ninety out of 165 students submitted complete data sets for analysis. Students demonstrated significant changes in knowledge, skills, and attitudes regarding medication errors. They felt they could find the cause of an error, identify factors leading to an error, and work with a team to prevent error recurrence. They also demonstrated an increase in knowledge about medication-related errors and the root cause analysis process.
Conclusion. Students used RCA methods to discover medication errors in three simulated pharmacy settings. Students improved their knowledge, skills, and attitudes regarding medication errors through this process.
Keywords: simulation, pharmacy skills, medication errors, patient safety, root cause analysis
INTRODUCTION
Graduates must be prepared to create and maintain a safe health care environment for patients. To do this, students must be trained to work effectively as a member of a team, communicate with health care providers and patients regarding medication errors, use root cause analysis (RCA) to evaluate medication errors, recognize the role of technology in improving medication safety, and believe that their efforts to advance medication safety are essential.1-3
In 2002, Johnson and colleagues conducted a survey and found that medication error curricula within colleges and schools of pharmacy lacked standardization and were missing important patient safety topics such as human error and medical errors.4 In 2008, the U.S. Food and Drug Administration (FDA) developed a Science of Safety (SoS) curriculum and collaborated with the American Association of Colleges of Pharmacy to integrate the curriculum into pharmacy education across the United States. In 2011, West-Strum and colleagues found that most pharmacy schools were using the curriculum; however, students were not learning how to use patient databases or electronic decision-support tools. They were also not introduced to the role of the FDA in risk management.5 Recommendations generated from their survey results included increasing opportunities for interprofessional and experiential education focused on safety topics as well as increasing faculty use of the SoS curriculum through training workshops and continuing education programs.5
In 2012, the Pharmacy Quality Alliance provided resources for the development of the Educating Pharmacy Students and Pharmacists to Improve Quality (EPIQ) program.6 The goal of the program was to increase student knowledge and skills needed for decreasing medication errors and improving patient safety.6 A 2012 survey by Gilligan and colleagues found that EPIQ was perceived as a quality program and, overall, the program positively affected student confidence in their ability, knowledge, motivation, and awareness of reducing medication errors and quality improvement.6
Other educational interventions related to medication safety have focused on pharmacy students’ knowledge and communication of medication errors, the role of the pharmacist in medication error reduction, integration of patient safety education into introductory pharmacy practice experiences, and the use of independent and team-based RCA projects.7-11
Hearing the call for improved preparedness of graduates to be able to reduce medication errors and promote patient safety, faculty members at North Dakota State University’s College of Health Professions created a capstone experience for students enrolled in a pharmacy skills laboratory. As most students will not be a part of an RCA during advanced pharmacy practice experiences (APPEs), it has been recommended that the RCA approach be taught to students through the use of detailed cases.11 Faculty members developed simulations to meet a perceived curricular gap and Accreditation Council for Pharmacy Education Standards.12 Prior to implementation of the simulations, students received minimal didactic instruction and no hands-on application of medication errors and patient safety topics. Appendix 1 of Standards 2016 outlines the didactic requirement for students to be able to analyze causes of medication errors and explore ways to reduce errors to increase patient safety.12 Simulations can be used to teach students how to identify, report, and communicate information regarding medication errors.13-15 Faculty members created three innovative medication error simulations highlighting teamwork, communication, the RCA process in an institutional setting, and use of the Institute for Safe Medication Practices (ISMP) fact gathering worksheet in both long-term care and community pharmacy settings.16 Students’ change in knowledge, skills, and attitudes regarding medication errors and patient safety were assessed before and after the simulations.
METHODS
This study took place at a single pharmacy school campus located at a public land grant institution. Pharmaceutical Care Laboratory IV is part of a four-semester course series designed to teach and assess the practical application of skills needed for students to practice at the top of their license. The course is offered in the spring semester of the third professional year within a four-year professional curriculum. Data represents findings from two cohorts of students collected during two consecutive years (N=165). Two pharmacist faculty trained up to 16 third-year pharmacy students enrolled in each of the six sections about medication errors and patient safety. Prior to enrolling in the laboratory, students discussed and used RCA in two didactic courses, Interprofessional Health Care Practice in the prior year, and Pharmacy Practice Improvement and Project Management during the same semester. To apply information learned in these courses about investigating sentinel events, three simulations were developed to further prepare students to identify, report, and communicate information regarding medication errors. Prior to the simulations and independent of class time, students completed readings from the ISMP Root Cause Analysis Workbook for Community/Ambulatory Pharmacy and viewed a video in which a parent recounts the medication error that occurred during the hospitalization of his newborn children.16,17 While watching the video, students completed a cause-and-effect diagram to identify potential causes of the medication error. To ensure students had completed and understood the independent class assignments, faculty members led a pre-activity discussion at the beginning of each laboratory section during which the students collectively completed the same assigned cause-and-effect diagram. Faculty members facilitated the diagramming and led a detailed discussion on the cause of the medication error and possible process improvements to prevent similar medication errors.
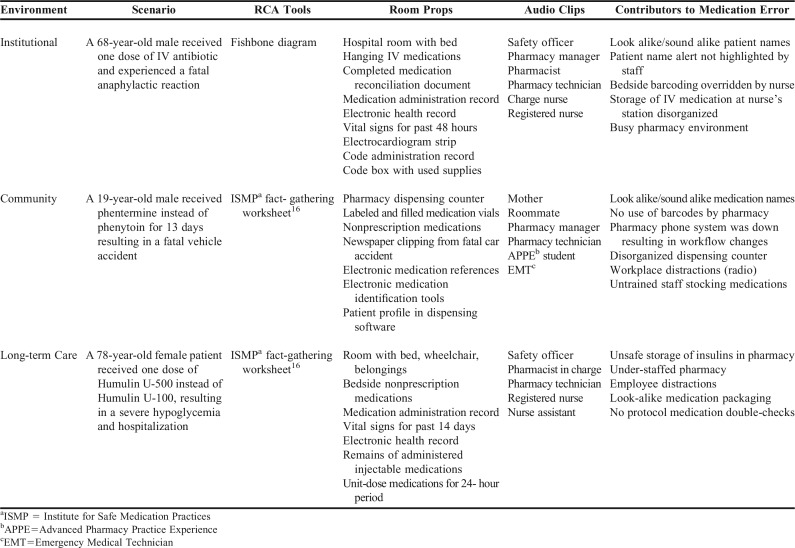
Faculty members developed three medication error simulations taking place in institutional, community, and long-term care settings (Table 1). Students were randomly divided into three groups. For each setting, students had to investigate a staged room, both independently and as a group, to determine the cause of the medication error. All rooms had audio recordings of individuals who had been interviewed regarding the medication error. Students were asked to listen to the audio clips to gather additional information needed for their investigation. As determined by the scenario, students could listen to audio clips of detailed interviews from the pharmacy manager, pharmacist, pharmacy technician, charge nurse, nurse, certified nurse assistant, safety officer, mother, roommate, APPE student, or emergency medical technician. For example, when listening to a clip of the pharmacist in the institutional simulation, students learned that the pharmacist was tired, and her workflow was repeatedly interrupted by telephone calls, technician requests, and a spilled cup of coffee. The students then had to evaluate if this information was important to their investigation. As the students investigated the room, they were to independently complete an RCA using either a cause-and-effect diagram or fact-gathering worksheet. Investigation of each room took approximately 25 minutes.
Table 1.
Description of Medication Error and Patient Safety Simulations
For the institutional simulation, a room was staged as a hospital room with a bed, intravenous medications hanging at the bedside, pharmacy medication code box, and evidence of a recent code. Students had access to the patient’s electronic medical record, medication administration record, prescribed medications, and equipment or supplies used to administer code medications. Students were to identify that the patient received an antibiotic prepared for a different patient with a name alert. The error caused a sentinel event which the patient did not survive. Through their fact-finding, students were to recognize that automation failure, medication storage, name alert failure, and an overworked staff may have contributed to the error. During the institutional simulation, students used a cause-and-effect diagram to independently collect their findings. The diagram facilitated the collection of information regarding the sentinel event using the headings of equipment, process, people, materials, environment, and management.
For the community simulation, a room was staged as a community pharmacy. Students had access to the patient’s dispensing profile and recently dispensed medications, the pharmacy’s medication stock, and a newspaper article detailing a car accident involving the patient. Students were to identify that the patient had been dispensed phentermine instead of phenytoin. The error caused a sentinel event which the patient did not survive. Through their fact-finding, students were to recognize that lack of separation of look-alike, sound-alike medication stock bottles, technology malfunction, and untrained staff may have contributed to the error. During the community simulation, students used the ISMP fact-gathering worksheet to independently collect their findings.16 The worksheet outlines how to begin an investigation and guides students in their documentation of information about a sentinel event, including patient information, drug information, communication of drug orders, drug labeling, packaging, and nomenclature, drug standardization, storage and distribution, environmental factors, workflow and staffing patterns, staff competency and education, patient education, and quality processes and risk management. In comparison to the cause-and-effect diagram, the workbook provides more direction during the data collection using guiding questions. Guiding questions are used in each of the topic areas to help the investigator determine what may have contributed to the event.16
For the long-term care simulation, a room was staged as a long-term care patient room with a bed, wheelchair, nonprescription medications at bedside, and remnants of prescription medications recently administered. Students had access to the patient’s electronic medical record, medication administration record, prescribed medications, and equipment or supplies used to administer medication. Students were to identify that the patient received Humulin U-500 instead of Humulin U-100. The error caused a sentinel event resulting in the transfer of the patient to a critical care unit. Through their fact finding, students were to recognize that a change in workflow, overworked staff, medication storage, packaging, and labeling may have contributed to the error. Students used the ISMP fact-gathering worksheet to independently collect their findings.16
Once the students independently identified the errors, they discussed their findings with their group. When group consensus was met, the group created one document with their collective findings for each simulation. A group cause-and-effect diagram was completed for the institutional simulation, and group ISMP fact-gathering worksheets were completed for the community practice simulation and long-term care simulations.16 After students rotated through all three simulations, faculty members facilitated a debriefing for each of the simulations. The debriefing was used to discuss potential causes of each medication error, strategies to prevent similar errors in the future, and ways to communicate medication errors with patients and providers. It also included a reflective discussion on how medication errors are prevented in pharmacies as seen during internships or introductory pharmacy practice experiences. Reflective discussions focused on job roles, workflow, technology, culture of safety, and disclosure of errors to patients.
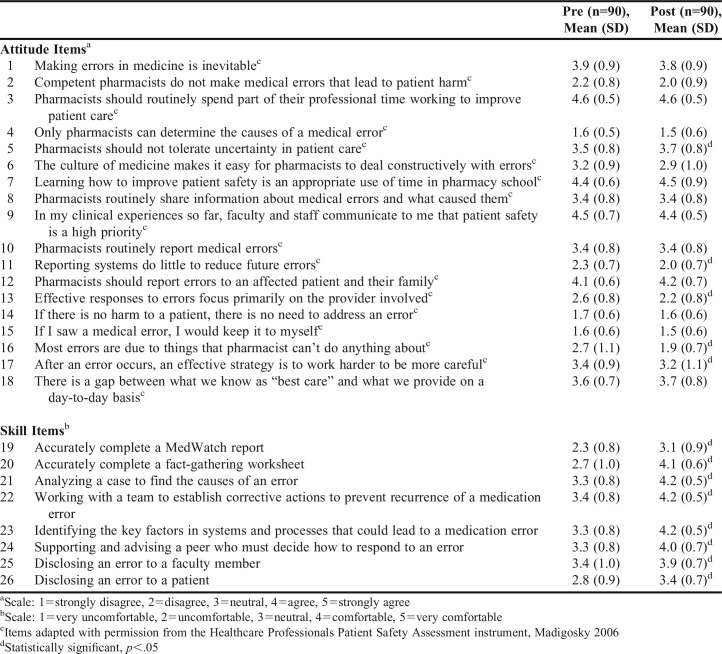
With permission, faculty members adapted the Healthcare Professionals Patient Safety Assessment instrument, a survey used to evaluate the impact of a patient safety and medical fallibility curriculum on medical students’ knowledge, skills, and attitudes.18 Researchers who developed the questionnaire found that a patient safety and medical fallibility curriculum affected the knowledge, skills, and attitudes of medical students, and students demonstrated sustained improvement when required to apply knowledge and practice skills in interactive sessions or role-playing.18 Researchers piloted the survey for comprehensibility and applicability with first- and second-year medical students prior to its use.18 For this study, all 26 survey items were modified for use in evaluating a pharmacy curriculum and to reflect the survey audience of pharmacy students. (Table 2). The original version of the tool used the term medical error vs medication error. Although this research is focused on medication errors, the wording was maintained, as the term medical error is a broader term. Items 1 to 18 measured student attitudes regarding medication errors, and items 19 to 26 measured students’ perceived skill with identification and communication of medication errors.
Table 2.
Improvement in Attitudes and Skills Before and After Medication Error Simulation
In addition to the 26 established and adapted survey questions, 11 items were added to the survey to measure knowledge of and personal experience with medical errors. Knowledge items were developed by faculty members using the ISMP workbook.16 All pre-survey items were included on the post-survey. One additional item was added only to the post-survey to collect student preference for use of a cause-and-effect diagram vs a fact-gathering worksheet when collecting data. Face validity was established through faculty review. Three faculty members reviewed the instrument for readability and clarity.
The North Dakota State University Institutional Review Board approved the informed consent document and survey used in this study. Students were asked to complete the survey before and after the learning experience, anonymously and online, using Qualtrics (Provo, UT). All data was entered and analyzed using Microsoft Excel v. 2013 (Redmond, WA). Students were asked to generate a personal code used to match pre-survey and post-survey responses. Student data was pooled as two iterations of the activity over the course of two academic years.
From the two cohorts of students, 90 out of 165 (54%) students submitted complete pre-surveys and post-surveys for analysis. A 5-point Likert scale (1=strongly disagree and 5=strongly agree) was used to assess items 1 through 26 focused on student attitudes regarding medication errors and their perceived skill with identification and communication of medication errors (Table 2). Using personal codes, individual student data from the pre-survey and the post-survey were matched. Using matched student data allowed the researchers to evaluate actual gain in attitude and perceived skill for each individual student. Matched data were analyzed using a paired t-test for each individual student. Overall student performance on knowledge-based questions was analyzed using a paired t-test to evaluate if the simulation led to a statistically significant increase in overall knowledge.
RESULTS
When comparing the matched responses for the pre-survey and post-survey regarding attitudes, five items showed significant improvement (p<.05). After the activity, students felt that pharmacists should not tolerate uncertainty in patient care, reporting systems can reduce future errors, responses to errors must be addressed by more than just the responsible provider, and pharmacists can reduce medication errors. Self-reported skill items also showed statistically significant improvements. Students felt they could find the cause of an error, identify factors that led to a medication error, and could work with a team to prevent medication error recurrence. Students also felt they could communicate with a peer, faculty member, or patient regarding an error (Table 2). Students (N=90) demonstrated a statistically significant gain in knowledge regarding types of medication errors, investigation of medication errors, and reporting medication errors as seen in an increase in overall knowledge assessment scores (p<.01). The mean pre-treatment overall knowledge score was 81.5% (SD 7.4). The mean post-treatment overall knowledge score was 83.9% (SD 5.8). Specific to the post-survey, 75 out of 117 (64.1%) students preferred using a cause-and-effect diagram vs a fact-gathering worksheet to identify a medication error. Students also were asked to describe their personal experience with medication errors. Within two years prior, 94 out of 117 (80.3%) students had observed a medical error in their clinical experiences, 38 (32.2%) had disclosed a medical error to a faculty member, and 86 (73.5%) had disclosed a medical error to a pharmacist.
DISCUSSION
Pharmacists play a pivotal role in the prevention of medication errors through their interactions with the health care team, medication review, consultation, and follow-up.19-26 Three medication error simulations were developed and used to improve pharmacy students’ knowledge, skills, and attitudes in the prevention of medication errors and promotion of patient safety. The results of this study indicate that the use of medication error simulations in a pharmacy curriculum led to changes in students’ knowledge, attitudes, and skills.
As a result of participating in three medication error simulations, students showed significant improvement in their attitudes and skills regarding medication errors. They recognized that pharmacists do play a role in reducing and preventing medication errors. They also acknowledged the importance of reducing ambiguity in the workplace, use of medication reporting systems, and use of strategies to prevent medication errors.
After the simulations, students felt they could find the cause of an error, identify factors that contributed to an error, complete a cause-and-effect diagram and a fact-gathering worksheet, and work on a team to prevent errors from recurring. Students preferred using the cause-and-effect diagram vs the fact-gathering worksheet to identify a medication error. This may be due to ease of use of the diagram. The worksheet is very descriptive in the information that needs to be collected in comparison to the diagram. Faculty members emphasized to students the importance of being able to accurately complete both types of data collection. This data also highlights the continued need for educating students about medication and medical errors.
Students responded neutrally when asked if pharmacists routinely share information about medical errors or routinely report medical errors. These items became important to the debriefing. Faculty members facilitated a discussion with the students focused on culture of safety and used examples from their own practice experience to support the pharmacist’s role in sharing and reporting information about medical errors.
The results of this pilot study add to the findings of previous studies by further confirming that integrating patient safety education into a curriculum is valuable.9,10 In particular, students improved in knowledge and confidence regarding the ability to conduct a root cause analysis when allowed to practice the process.9,10,27 This process also helps students to identify problems and solutions within their work environment and promotes teamwork and a culture of safety.9,10,27
Unexpectedly, most students had observed a medical error during their clinical experiences, and many had disclosed a medical error to a faculty member or pharmacist. Additional information could have been collected regarding the type of error observed. However, this finding further substantiates the need for medication error and patient safety curricular initiatives.
These simulations could easily be executed at other universities. Immersive rooms are not needed for the simulation but add to increased student engagement. Similar simulations have been deployed by the authors to an audience of pharmacists, technicians, and pharmacy students. A mix of participants worked in groups of 10 to evaluate simulation materials at a tabletop (eg, a medication printout or labeled products) and used a cause-and-effect diagram to identify the medication error.
Simulations help students to develop knowledge, attitudes, and skills regarding medication errors. Medication error simulations are easily implemented and customizable to meet the needs of students and pharmacy curricula. Unique to this pharmacy curriculum is the use of simulations in three different pharmacy settings. Students identified medication errors in an institutional, long-term care, and community pharmacy setting. In addition, they used both the cause-and-effect diagramming technique and the ISMP Root Cause Analysis Workbook for Community/Ambulatory Pharmacy to document their findings.16 This resulted in a comprehensive training experience ensuring that students are prepared to prevent medication errors and promote patient safety in both inpatient and outpatient pharmacy settings.
Limitations to the study include the response rate, survey instrument, and evaluation methods. Students were not required to take the pre- and post-surveys, and participation in the study did not affect their course grade. In the future, faculty members may consider using an incentive to increase survey participation. Although, the survey instrument had been piloted previously for comprehensibility and applicability in medical students, the tool has not undergone formal validation and reliability testing, nor has it been previously piloted with pharmacy students. Items only measured by the post-survey could have been measured prior to the simulations to more accurately capture student changes in knowledge and skill. Lastly, the study is limited by reliance of students self-reporting their perceived skills and behaviors. However, the results from two student cohorts illustrate the effectiveness of simulations to change student knowledge and attitudes about medication errors and patient safety. As the topics of medication errors and patient safety are important to all students, innovative approaches to teaching such topics can be useful to all faculty and should be included in the curriculum.
CONCLUSION
Simulations used to teach students how to identify, report, and communicate information regarding medication errors were successfully piloted for third-year students in a pharmacy skills laboratory course. Students worked as a team to investigate three different pharmacy settings in which a medication error occurred. They used cause-and-effect diagrams and fact-gathering worksheets to collect information in each setting, leading to discovery of the simulated medication errors. Students improved their knowledge, skills, and attitudes regarding medication errors through this process.
ACKNOWLEDGMENTS
The authors thank Dan Freisner, PhD, and Dan Cernusca, PhD, for their assistance with data analysis, and Alicia Fitz, PharmD, for her support of the project at North Dakota State University, Fargo. The authors also thank Michael Neville, PharmD, BCPS, FASHP, for sharing his medication error curriculum for further development.
REFERENCES
- 1.Alldredge BK, Koda-Kimble MA. Count and be counted: preparing future pharmacists to promote a culture of safety. Am J Pharm Educ. 2006;70(4) doi: 10.5688/aj700492. Article 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu AW, Lipshutz AKM, Pronovost PJ. Effectiveness and efficiency of root cause analysis in medicine. JAMA. 2008;299(6):685–687. doi: 10.1001/jama.299.6.685. [DOI] [PubMed] [Google Scholar]
- 3.Lang W. The role of academic pharmacy to influence safety through science and education. Am J Pharm Educ. 2011;75(4) doi: 10.5688/ajpe75478. Article 78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Johnson MS, Latif DA, Gordon B. Medication error instruction in schools of pharmacy curricula: a descriptive study. Am J Pharm Educ. 2002;66(4):364–371. [Google Scholar]
- 5.West-Strum D, Basak R, Bentley JP, et al. The science of safety curriculum in US colleges and schools of pharmacy. Am J Pharm Educ. 2011;75(7) doi: 10.5688/ajpe757141. Article 141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gilligan AM, Myers J, Nash JD, et al. Educating pharmacy students to improve quality (EPIQ) in colleges and schools of pharmacy. Am J Pharm Educ. 2012;76(6) doi: 10.5688/ajpe766109. Article 109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rickles NM, Noland CM, Tramontozzi A, Vinci MA. Pharmacy student knowledge and communication of medication errors. Am J Pharm Educ. 2010;74(4) doi: 10.5688/aj740460. Article 60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kiersma ME, Darbishire PL, Plake KS, Oswald C, Walters BM. Laboratory session to improve first-year pharmacy students' knowledge and confidence concerning the prevention of medication errors. Am J Pharm Educ. 2009;73(6) doi: 10.5688/aj730699. Article 99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Trinkley KE, Van Matre ET, Mueller SW, Page RL, Nair K. Perceived benefit of teaching patient safety to pharmacy students by integrating classroom teaching with introductory (IPPE) visits. J Pharm Pract. 2017;30(1):115–120. doi: 10.1177/0897190015614478. [DOI] [PubMed] [Google Scholar]
- 10.Holdsworth MT, Bond R, Parikh S, Yacop B, Wittstrom KM. Root cause analysis design and its application to pharmacy education. Am J Pharm Educ. 2015;79(7) doi: 10.5688/ajpe79799. Article 99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fassett WE. Key performance outcomes of patient safety curricula: Root cause analysis, failure mode and effects analysis, and structured communications skills. Am J Pharm Educ. 2011;75(8) doi: 10.5688/ajpe758164. Article 164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. Standards 2016. https://www.acpe-accredit.org/pdf/Standards2016FINAL.pdf. Accessed July 11, 2017.
- 13.Sanko J, Mckay M, De Santis JP, Solle NS. Learning from simulation-based medication event reporting: a mixed methods analysis. Clin Simul Nursing. 2015;11(6):300–308. [Google Scholar]
- 14.Durham CF, Alden KR. Enhancing patient safety in nursing education through patient simulation. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville, MD: Agency for Healthcare Research and Quality; 2008. [PubMed] [Google Scholar]
- 15.Warholak TL, Queiruga C, Roush R, Phan H. Medication error identification rates by pharmacy, medical, and nursing students. Am J Pharm Educ. 2011;75(2) doi: 10.5688/ajpe75224. Article 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Institute for Safe Medication Practices. Root cause analysis workbook for community/ambulatory pharmacy. https://www.ismp.org/tools/rca/RCA-Complete.pdf. Accessed July 11, 2017.
- 17.Stop MICRA. “Dennis Quaid talks about his twins and medical negligence.” Online video clip. YouTube, https://www.youtube.com/watch?v=GEDMYsm3Nxs. Published October 13, 2014. Accessed July 11, 2017.
- 18.Madigosky WS, Headrick LA, Nelson K, Cox KR, Anderson T. Changing and sustaining medical students’ knowledge, skills, and attitudes about patient safety and medical fallibility. Acad Med. 2006;81(1):94–101. doi: 10.1097/00001888-200601000-00022. [DOI] [PubMed] [Google Scholar]
- 19.Leape LL, Cullen DJ, Clapp M, et al. Pharmacist participation on physician rounds and adverse drug events in the intensive care unit. JAMA. 1999;282(3):267–270. doi: 10.1001/jama.282.3.267. [DOI] [PubMed] [Google Scholar]
- 20.Schnipper JL, Kirwin JL, Cotugno MC, et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Arch Intern Med. 2006;166(5):565–571. doi: 10.1001/archinte.166.5.565. [DOI] [PubMed] [Google Scholar]
- 21.Rothschild JM., Churchill W, Erickson A, et al. Medication errors recovered by emergency department pharmacists. Ann Emerg Med. 2010;55(6):513–521. doi: 10.1016/j.annemergmed.2009.10.012. [DOI] [PubMed] [Google Scholar]
- 22.Kaboli PJ, Hoth AB, McClimon BJ, Schnipper JL. Clinical pharmacists and inpatient medical care: a systematic review. Arch Intern Med. 2006;166(9):955–964. doi: 10.1001/archinte.166.9.955. [DOI] [PubMed] [Google Scholar]
- 23.Khalili H, Farsaei S, Rezaee H, Dashti-Khavidaki S. Role of clinical pharmacists’ interventions in detection and prevention of medication errors in a medical ward. Int J Clin Pharm. 2011;33(2):281–284. doi: 10.1007/s11096-011-9494-1. [DOI] [PubMed] [Google Scholar]
- 24.Scarsi KK, Fotis MA, Noskin GA. Pharmacist participation in medical rounds reduces medication errors. Am J Health Syst Pharm. 2002;59(21):2089–2092. doi: 10.1093/ajhp/59.21.2089. [DOI] [PubMed] [Google Scholar]
- 25.Kaushal R, Bates DW, Abramson EL, Soukup JR, Goldmann DA. Unit-based clinical pharmacists’ prevention of serious medication errors in pediatric inpatients. Am J Health Syst Pharm. 2008;65(13):1254–1260. doi: 10.2146/ajhp070522. [DOI] [PubMed] [Google Scholar]
- 26.Murray MD, Ritchey ME, Wu J, Tu W. Effect of a pharmacist on adverse drug events and medication errors in outpatients with cardiovascular disease. Arch Intern Med. 2009;169(8):757–763. doi: 10.1001/archinternmed.2009.59. [DOI] [PubMed] [Google Scholar]
- 27.Dolansky MA, Druschel K, Helba M, Courtney K. Nursing student medication errors: a case study using root cause analysis. J Prof Nurs. 2013;29(2):102–108. doi: 10.1016/j.profnurs.2012.12.010. [DOI] [PubMed] [Google Scholar]