Abstract
Objective. To determine the impact of a vaccine hesitancy learning unit on student knowledge, attitudes, and ability to address vaccine hesitancy and/or refusal.
Methods. The learning unit consisted of two standardized patient simulation encounters performed one week apart. A 13-item attitudes survey was administered prior to the simulations to determine student confidence and knowledge regarding vaccine hesitancy. Students then participated in an encounter with a simulated patient who assessed the students’ abilities using a 16-item grading rubric related to the art of the rhetoric, communication skills, and social, emotional competence. Post-simulation, students received feedback, completed a self-reflection exercise, and received formal coursework on addressing vaccine hesitancy. The following week, students participated in a second simulated patient encounter and thereafter completed the same attitudes and satisfaction surveys.
Results. There were 203 students who went through the learning unit, with 180 (88.6% response rate) completing all the survey tools. The results showed significant improvements in all 16 items of the assessment rubric. On the pre/post attitudes questions, 9 out of 13 items showed significant improvement. Gains were largest for knowledge on the use of thimerosal as a preservative, speaking about how vaccines will not overwhelm a child’s immune system, and knowledge about vaccinations not overwhelming a child's immune system. Overall, 94% of students were satisfied with the learning unit.
Conclusion. This learning unit was effective in improving student confidence and ability to address vaccine hesitancy.
Keywords: vaccine hesitancy, vaccine myths, simulation, art of persuasion, vaccine refusal
INTRODUCTION
The number of cases of vaccine-preventable diseases in the United States is on the rise. In 2014, there were 644 reported cases of measles, which was three times higher than reports in 2013. In 2010, the state of California reported more than 9000 cases of pertussis, a historic rise in numbers, and the highest since 1947.1-3 These cases occurred mainly in infants who were not yet vaccinated and therefore relied on herd immunity for protection. Vaccination rates appear to be about 90% for most preventable childhood diseases, but these statistics may mask a subset of communities that may not routinely vaccinate their children or who may have similarly held beliefs regarding the dangers of vaccinations.1 This subset of communities represent the likely gaps in herd immunity and a source for disease outbreaks. A review of recent outbreaks of vaccine-preventable diseases suggests that US vaccination rates may still be inadequate with large regional variation.1,4 Another recent study estimated that 2009 immunization rates of children in California ranged from 64% to 92% for measles, mumps, and rubella 1 (MMR1) and from 25% to 58% for MMR2 in typical schools, and from 49% to 90% for MMR1 and from 16% to 63% for MMR2 in schools with high personal belief exemptions for vaccinations – with all these ranges being lower than the herd immunity threshold range of 88% to 95% for MMR.5 Among adults, the rates of vaccinations are even more alarming with tetanus-diphtheria-acelluar pertussis (Tdap) and pneumococcal (high-risk populations) vaccination rates around 20% of populations that should be immunized.6 These and other reports provide evidence of a growing number of patients who refuse to get themselves and their children vaccinated due to a belief that vaccines can cause harm.
Study of vaccine refusal among parents and patients reveals a deep-rooted mistrust of medicine and fear that vaccines may cause more harm than good. This subset of the population is either anti-vaccine or vaccine-hesitant.7-12 The vaccine-hesitant group may under-vaccinate their children or may request delays in the vaccine schedule. Even in cases where they get vaccinations on time, they may have serious doubts about the safety and efficacy of vaccines.1
Various factors appear to influence parental vaccine hesitancy, including parent-specific factors (knowledge of vaccines, past experiences, socioeconomic status, education level, and demographics), vaccine-related factors (perceived vaccine efficacy, vaccine safety, and disease susceptibility), and external factors (policies, requirements, norms, media, and patient-provider relationships).13 Public concerns range from anxiety about vaccines causing autism, vaccines overloading a child’s immune system, harmful ingredients in vaccines such as thimerosal and aluminum, to a general mistrust of the health care system. This public misperception needs to be addressed quickly and strategically by public health officials, professional organizations, and individual health care providers.1 Two recent systematic reviews revealed that while the evidence is low to moderate on the effectiveness of individual strategies to address parental vaccination hesitancy or refusal, an approach employing multiple strategies may be effective.14,15
Available strategies include targeting under-vaccinated populations, enhancing awareness and education, improving access, mandating vaccinations or enforcing sanctions for those not vaccinated, and engaging religious and other community leaders in promoting vaccination.14 On a personal level, educating parents on the impact of childhood diseases may also present a viable strategy for addressing vaccine hesitancy.16 The Centers for Disease Control and Prevention (CDC) outlined a series of facts designed to counter most common vaccine myths and address likely causes of vaccine hesitancy. This may be a useful tool for providers who need talking points when counseling a parent on vaccine use. However, simply countering vaccine myths may not be effective.1 It is imperative for vaccine promoters to use a multifaceted strategy for promoting vaccine use.
The first prong of this multifaceted approach would be for health care providers to master the art of rhetoric or persuasion so as to have meaningful and personal conversations with patients and parents. As Aristotle stated, an effective strategy in persuading another individual is to employ the art of rhetoric.17 The foundation of which is building trust and a sense that the messenger is listening, truly attentive, and credible. The tenets of persuasion require that the individual have an open and credible stance, an emotional connection to their audience, display a command over their content and offer logical argumentation. In the context of vaccine hesitancy, components of the art of persuasion should include a genuine interest in the child/patient, acknowledgment of any concerns regarding vaccines, provision of accurate information on both risks and benefits of vaccines, and the overall social-emotional competence of the provider. The second prong would be to employ a clinical perspective on vaccine hesitancy. This strategy would include recognizing and identifying the patient’s concerns and then using strategies that would target those specific concerns. This technique could avoid information overload and focus the conversation between the patient and provider.18 For vaccine-hesitant parents, the third and last prong would be to use social and emotional skills to arouse emotions to relay the importance and immediacy of vaccinating young children. Highlighting personal stories of tragedies related to this illness may have an emotional impact on parents, unparalleled to any statistical data or regulatory strategies.
Pharmacists play an important role in educating patients, dispensing, and administering immunizations and are central to promoting this public health measure. It is important to educate pharmacists to recognize and respond to vaccine hesitancy. Like medication adherence, convincing patients of the importance of vaccinating themselves and their children requires good communication skills and the use of individualized strategies that target the root of that patient’s hesitancy. However, even with optimal communication strategies, some patients/parents may remain unconvinced. Pharmacists must focus on maintaining the patient-provider relationship despite disagreement. The inclusion of these vital humanistic communication strategies along with the clinical aspects of immunizations is imperative for the pharmacy curriculum. The 2016 ACPE Standards support this by stating that the graduating pharmacist should be a patient advocate, understand and respect a patient’s health beliefs, and promote population-based health.19
Traditional pharmacy education regarding vaccines has been based on providing clinical information about vaccines and the proper administration technique. The authors are not aware of any published research in pharmacy education that describes the development and assessment of student ability to understand and apply strategies to address vaccine hesitancy and refusal. The only reference found was an abstract in the nursing education literature.20 This paper describes a two-week learning unit that focused on teaching pharmacy students the art of persuasion (rhetoric) as related to vaccine hesitancy. The objective of this study is to determine the impact of this learning unit on student knowledge, attitudes, perceptions, and the ability to address vaccine hesitancy and refusal.
METHODS
At the University of the Pacific, students complete the American Pharmacist Association (APhA) Immunization Training Certification Program as part of a required Practicum I course in the first semester of the program. In 2016, during the third semester of the program, a two-week vaccine hesitancy learning unit was added to the required Practicum II course as a formative component that was not part of the students’ summative grade in the course. Practicum II is a course designed to provide hands-on learning activities in the area of developing subjective, objective, assessment, and plan (SOAP) notes, laboratory diagnosis, diagnostic tests, physical assessment and professional communication. The course is divided into small discussion groups that are led by trained teaching assistants. The goal of the learning unit was to build upon the material learned in the APhA certificate program and provide practice in counseling vaccine-hesitant patients. The objectives of the learning unit were to enable a student to identify common myths associated with vaccine use, identify a patient/parent who is vaccine-hesitant, apply counter strategies in communicating with a patient/parent who is vaccine-hesitant, and apply the art of rhetoric when communicating with a patient/parent who is vaccine-hesitant.
The vaccine hesitancy unit consisted of two standardized patient (SP) simulations scheduled one week apart with a self-study module in between simulations. Twenty actors were hired and trained for 4 hours to serve as SPs for the simulation. Each scenario began with an SP who approached the student pharmacist and expressed a vague concern about getting themselves or their child vaccinated. Scenarios were conducted in a small classroom. Four common vaccine myths as identified by the World Health Organization (WHO) were selected for this exercise: vaccines overwhelming a child’s immune system, vaccines causing the illness they are supposed to prevent, vaccines containing harmful additives such as thimerosal, and vaccines causing side effects.21
Faculty members developed the scenarios and scripts for the SPs based on these myths. During each one-on-one simulated interaction, the SP brought up two of the selected vaccine myths. Students were not informed ahead of time what concerns the SP would have. The scenario was deliberately vague as students were expected to evaluate the patient by asking questions, providing counseling, mediating any conflict, and maintaining the patient-provider relationship despite possible disagreements. A conflict escalation clause was put into each script to allow the SP to escalate the situation to a conflict scenario. This would be triggered if the SP felt the pharmacy student was not listening, not being properly empathetic, or exhibiting a condescending or dismissive attitude toward them and/or their concerns. If the SP escalated the script to the conflict scenario, the student was given immediate feedback (at the end of the simulation) on the behavior that triggered the escalation. The total time given for the simulation and feedback was 20 minutes.
Students completed a self-reflection essay after the first SP interaction. The prompt for the self-reflection was “Please reflect on how you would address any communication deficiencies pointed out by your patient.” To further prepare students, the researchers developed an online module and two YouTube videos (referred to as the intervention in future sections). The YouTube videos were created by the researchers to demonstrate the differences between “poor” and “effective” techniques when addressing a vaccine-hesitant patient/parent. The online module was an hour long, and each YouTube video was 6 minutes long with captions to highlight areas of importance (YouTube video links are available upon request). The module provided information on how to counter vaccine myths, impact of common vaccine-preventable diseases, using the art of persuasion, and common vaccine side effects. The YouTube videos provided instruction on how to recognize the patient’s exact concerns, how to quickly counter any vaccine hesitancy, how to use disease facts to develop an emotional tie to the patient and how to employ a multimodal approach that does not rely on any one strategy. The second simulated interaction was conducted the following week. The scenario and script setup was similar to the first but focused on two different vaccine concerns. The students did not know ahead of time what concerns the patient would have. The second simulation gave students the opportunity to use and practice the new techniques introduced in the online module and videos. Following each simulation, SPs provided formative feedback with the help of a grading rubric developed by faculty.
The grading rubric was divided into three components: the art of the rhetoric, communication skills, and social-emotional competence. The components of social-emotional competence (consideration, connection, influence, and self-awareness) were adapted from the Personal-Interpersonal Competence Assessment (PICA).22 Students could receive up to 48 points on 16 items with a maximum score of 3 on each item. The performance scale ranged from 0=none, 1=insufficient, 2=adequate, to 3=thorough. Definitions were provided for each performance scale.
SPs received extensive training to serve as patients and as graders to ensure grading consistency. The training consisted of an hour long online training in which SPs viewed a PowerPoint (Microsoft, Redmond, WA) presentation developed by faculty on the vaccine myths, how to assess student performance, and finally how to give constructive feedback. SPs were also instructed to read and familiarize themselves with the script and grading rubric. Before each simulation, SPs were also provided 2 hours of face to face training during which a vaccine hesitancy consultation video was viewed and SPs were asked to graded it using the rubric. A group discussion followed to ensure consistency with grading. SPs were also trained on how to escalate the script to a conflict scenario if necessary, and to provide feedback on areas of improvement (Appendix 1). SPs were trained to provide feedback on a student’s use of the art of rhetoric, communication skills, and social, emotional competence. The SPs used components of the grading rubric to provide targeted feedback to the students. SPs were trained to provide a patient’s perspective of the student’s interaction with them. SPs were blinded to any pre/post student intervention and data collection to prevent bias toward the intervention.
Assessment data was collected throughout this unit. Before beginning the unit, students completed a 13-item attitudes survey designed to measure baseline confidence in their knowledge of, and ability to, address vaccine hesitancy. The survey used a 5-point Likert scale (1=not at all confident, 5=extremely confident). Students were given the same 13-item attitudes survey after the completion of the second simulation to measure any differences in student self-perception. A satisfaction survey was also administered to evaluate student attitudes toward the learning unit. The satisfaction survey used a 5-point Likert scale to measure student satisfaction and agreement on 11 items.
Wilcoxon signed-rank test was applied to the attitudes survey and assessment data due to the ordinal nature of the data. Descriptive statistics were used to describe the self-reflection and satisfaction survey. Statistical significance was set at p≤.05. SPSS Statistics 23 (IBM, Armonk, NY) and Excel 2013 (Microsoft, Redmond, WA were used for data collection, storage, and analysis.
This study was deemed exempt by the institutional review board at the University of the Pacific.
RESULTS
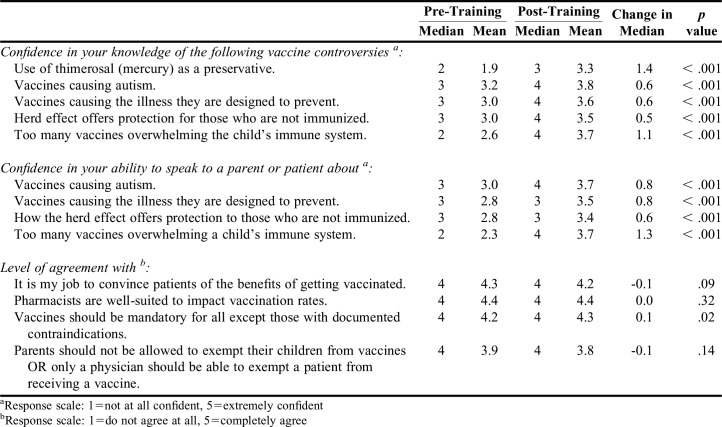
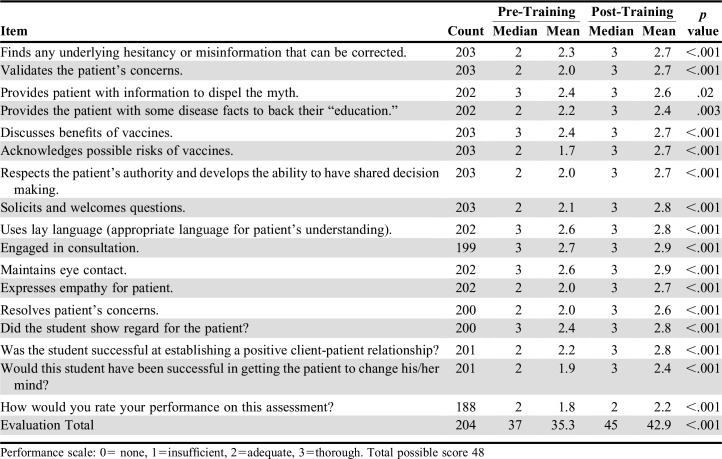
There were 203 students who participated in both phases of the learning unit. Only 180 students (88.6% response rate) completed both the pre- and post-attitudes surveys, with nine items showing significant improvement. The largest changes were seen in Q1 (knowledge about the use of thimerosal as a preservative), Q9 (speaking about how too many vaccines do not overwhelm a child’s immune system), and Q5 (knowledge about vaccinations not overwhelming a child's immune system) (Table 1). Of note, no gains were noted in student attitudes regarding pharmacist roles and vaccine exemptions due to a high level of agreement with the statements prior to the intervention (Q10-Q13). Table 2 shows the mean increase on each of the 16 rubric assessment questions as graded by the SP. By far, the greatest gain (pre-training mean=1.7, post-training mean=2.7, p<.001) was seen in students' ability to acknowledge risks. The other items with larger gains all dealt with creating a positive environment for patient-consultant interactions (eg, soliciting questions, expressing empathy, validating concerns). The smallest gain was in providing the patient with information to dispel the myth, however, even here, the gain was significantly positive (p<.05). Of note, conflict escalation occurred in 15.7% of SP encounters pre-intervention and only 5% of encounters post-intervention. Total mean scores improved from 35.3/48 for the initial activity to 42.9/48 post-intervention. Additionally, students were more likely to change an SP’s mind, post-intervention (1.87 vs 2.42, p<.001).
Table 1.
Comparison of Students’ Pre- and Post-intervention Confidence in Their Knowledge of Common Vaccination Controversies, Communication Abilities, and Roles and Responsibilities (N=180)
Table 2.
Comparison of Students’ Pre- and Post-intervention Rubric Scores of the Simulated Patient Encounters
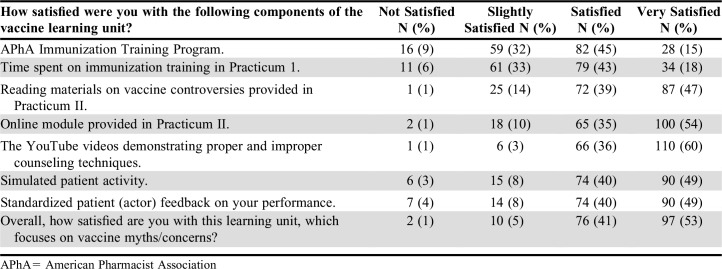
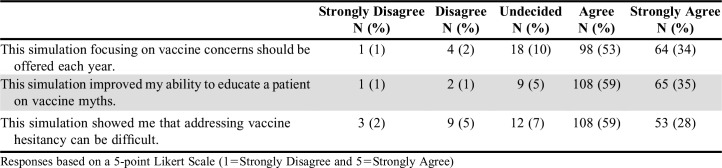
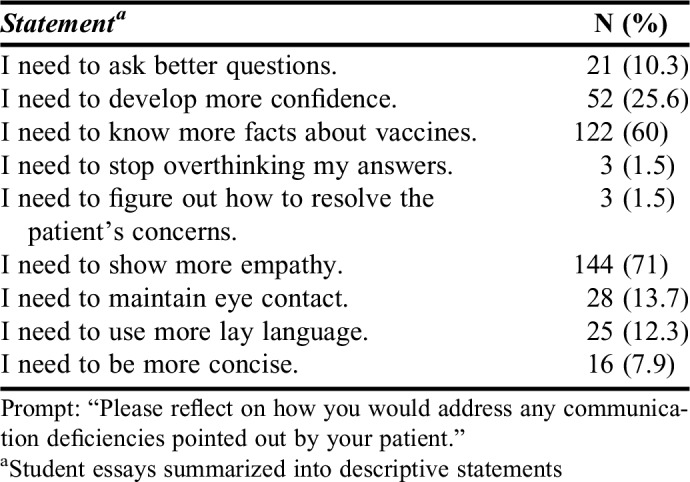
Overall, 94% of students were satisfied with this unit on vaccine myths and concerns (Tables 3 and 4). For individual activities offered in the unit, a majority (average of 78.5%) of the students who responded to the survey were “satisfied or very satisfied” with the offerings. In addition, 85% of students believed that the simulation improved their ability to educate a patient on vaccine myths and 87% believed the simulation should be offered each year. The reflection exercises revealed that more than 70% of students felt that they needed to increase their empathy toward patients, almost 60% of respondents felt that they needed to know more facts to properly counsel a vaccine-hesitant patient, and about 25% felt that they needed to increase their confidence levels (Table 5).
Table 3.
Satisfaction with the Vaccine Learning Unit (N=185)
Table 4.
Student Agreement with Statements Regarding the Vaccine Learning Unit (N=185)
Table 5.
Summary of Student Reflection Exercise (N=203)
DISCUSSION
Vaccine hesitancy is a patient behavior that can have serious consequences for the patient and the population at large. Assessing and addressing the reasons for it is an important aspect of public health and pharmacists should be prepared to intervene.
To the authors’ knowledge, this is the first study that looked at pharmacy students’ ability to identify and address vaccine hesitancy. Changing a patient’s mind requires communication skills that can only be developed through practice and the possession of critical knowledge of how to persuade a hesitant individual. The APhA certification program provides important foundational knowledge on vaccinations, screening procedures, contraindications, adverse reactions, and vaccine myths. However, the pre-intervention data showed deficiencies in student skills and self-confidence, proving a need for more hands-on application of this foundational knowledge. By assessing student abilities in dealing with vaccine hesitancy before and after completing an active learning exercise, this study was able to show significant increases across all areas of confidence, knowledge, and student skill. The simulated exercise, when paired with standard didactic teaching materials, provided a conceptual model of how to teach critical communication skills to improve students’ ability to address vaccine hesitancy.
Programs looking to incorporate such an exercise to their curricula should consider the significant resource costs of SPs and the time needed to schedule and execute simulated patient interactions. In total, it took about 5 hours of SP training and the simulations took approximately 5 hours. In addition, significant effort needs to be put into improving the realism of each simulation, so that students take it seriously and learn from any feedback. The use and adequate training of SPs proved to be effective in providing a realistic simulation for the students. The satisfaction survey results indicated that 89% of the students were “satisfied or very satisfied” with the simulated patient encounter, which is encouraging.
An extensive effort was made to make sure that there was no inter-rater variability by training the SPs using mock video consults. There was no difference in grading among 18 out of 20 SPs; however, two of the 20 had consistently lower scores on the grading rubrics compared to their peer evaluators on both pre- and post- assessment. To further limit inter-rater variability in the future, an assessment and analysis of grading rubrics completed by SPs during the training can take place as a function of the training itself.
Pre/post-simulation data suggest significant improvement in student confidence and improved abilities to persuade a vaccine-hesitant patient. In reviewing the assessment data, students were more likely to change the SPs’ mind, post-intervention. On questions related to attitudes on pharmacist roles and exemptions, no improvements were seen with a slight recession post-intervention on Q10: It is my job to convince patients of the benefits of getting vaccinated and Q13: Parents should not be allowed to exempt their children from vaccines, or only a physician should be able to exempt a patient from receiving a vaccine (Table 1). The recession post-intervention was not statistically significant. Total scores on the grading rubric were significantly improved post-intervention indicating overall skills improvement most notably in social-emotional competence, a critical component of relationship building. The weakest gains were in the students’ provision of information to dispel the myth. Student reflections also indicated that they felt they needed to know more facts about vaccine myths and how to address those myths with practical and persuasive counterpoints. This indicates a need for more time to teach students about vaccines, vaccine hesitancy, and disease prevalence, including a historical perspective. However, despite this, results show significant gains in skills and knowledge.
While this study showed significant short-term gains, further study needs to be done to confirm long-term gains in knowledge and skills. Since survey completion was voluntary, the overall study completion rate was only 88.6%, which is a limitation of the study. Gains in confidence were also seen in students’ perception of their own knowledge versus actual gains in knowledge. A pre/post knowledge quiz could have provided important supportive data. In addition, gains in skills do not necessarily translate to clinical adequacy. Further research on student performance on advanced pharmacy practice experiences (APPEs) and post-graduation in practice would provide powerful data to support this strategy in improving student ability to address vaccine hesitancy. In addition, including students from other health care professions would make this a powerful interprofessional education.
CONCLUSION
Countering vaccine myths and concerns is an important public service that pharmacists are well- suited to performing. Pharmacy students should be systematically taught how to identify, address and counter any vaccine hesitancy. Implementing a learning unit focusing on the use of interpersonal communication skills to counter vaccine hesitancy among patients and parents was successful at improving student knowledge, attitudes, and skills regarding vaccine concerns.
Appendix 1. Example Script
REFERENCES
- 1.Diekema DS. Improving childhood vaccination rates. New Engl J Med. 2012;366(5):391–393. doi: 10.1056/NEJMp1113008. [DOI] [PubMed] [Google Scholar]
- 2.Horne Z, Powell D, Hummel JE, Holyoak KJ. Countering antivaccination attitudes. PNAS. 2015;112(33):10321–10324. doi: 10.1073/pnas.1504019112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and PreventionMeasles in the United States, 2015. www.cdc.gov/media/releases/2015/t0129-measles-in-us.html. Accessed February 12, 2015
- 4.Centers for Disease Control and Prevention. National Immunization Survey. Immunization Coverage in the US. http://www.cdc.gov/media/releases/2015/p0827-vaccination-rates.html. Accessed July 12, 2016.
- 5.Buttenheim AM, Sethuraman K, Omer SB, Hanlon AL, Levy MZ, Salmon D. MMR vaccination status of children exempted from school-entry immunization mandates. Vaccine. 2015;33(46):6250–6256. doi: 10.1016/j.vaccine.2015.09.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Williams WW, Lu PJ, O’Halloran A, et al. Surveillance of vaccination coverage among adult populations – United States, 2014. MMWR. 2016;65(1):1–36. doi: 10.15585/mmwr.ss6501a1. [DOI] [PubMed] [Google Scholar]
- 7.Ruijs WL, Hautvast JL, van Ijzendoorn G, van Ansem WJ, van der Velden K, Hulscher ME. How orthodox protestant parents decide on the vaccination of their children: a qualitative study. BMC Public Health. 2012;12:408. doi: 10.1186/1471-2458-12-408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hilton S, Petticrew M, Hunt K. Combined vaccines are like a sudden onslaught to the body’s immune system’: parental concerns about vaccine ‘overload’ and ‘immune-vulnerability. Vaccine. 2006;24(20):4321–4327. doi: 10.1016/j.vaccine.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 9.Kennedy A, LaVail K, Novak G, Basket M, Landry S. Confidence about vaccines in the United States: understanding parents’ perceptions. Health Aff. 2011;30(6):1151–1159. doi: 10.1377/hlthaff.2011.0396. [DOI] [PubMed] [Google Scholar]
- 10.Cooper LZ, Larson HJ, Katz SL. Protecting public trust in immunization. Pediatrics. 2008;122(1):149–153. doi: 10.1542/peds.2008-0987. [DOI] [PubMed] [Google Scholar]
- 11.Kennedy A, Basket M, Sheedy K. Vaccine attitudes, concerns, and information sources reported by parents of young children: results from the 2009 HealthStyles survey. Pediatrics. 2011;127(Suppl 1):S92–S99. doi: 10.1542/peds.2010-1722N. [DOI] [PubMed] [Google Scholar]
- 12.Kennedy A, Lavail K, Nowak G, Basket M, Landry S. Confidence about vaccines in the United States: understanding parents’ perceptions. Health Aff. 2011;30(6):1151–1159. doi: 10.1377/hlthaff.2011.0396. [DOI] [PubMed] [Google Scholar]
- 13.Gowda C, Dempsey AF. The rise (and fall?) of parental vaccine hesitancy. Hum Vaccin Immunother. 2013;9(8):1755–1762. doi: 10.4161/hv.25085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jarrett C, Wilson R, O’Leary M, Eckersberger E, Larson HJ SAGE Working Group on Vaccine Hesitancy. Strategies for addressing vaccine hesitancy – a systematic review. Vaccine. 2015;33(34):4180–4190. doi: 10.1016/j.vaccine.2015.04.040. [DOI] [PubMed] [Google Scholar]
- 15.Sadaf A, Rihcards JL, Glanz J, Salmon DA, Omer SB. A systematic review of interventions for reducing parenteral vaccine refusal and vaccine hesitancy. Vaccine. 2013;31(40):4293–4304. doi: 10.1016/j.vaccine.2013.07.013. [DOI] [PubMed] [Google Scholar]
- 16.Horne Z, Powell D, Hummel JE, Holyoak KJ. Countering antivaccination attitudes. Proceedings of the National Academy of Sciences of the United States of America. 2015;112(33):10321–10324. doi: 10.1073/pnas.1504019112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Aristotle. On Rhetoric: A Theory of Civic Discourse. 2nd ed. Translated by George A. Kennedy. Oxford, UK: Oxford University Press; 2006.
- 18.Diekema DS. Responding to parental refusals of immunization of children. Pediatrics. 2005;115(5):1428–1431. doi: 10.1542/peds.2005-0316. [DOI] [PubMed] [Google Scholar]
- 19.Accreditation Council for Pharmacy Education. Standards and key elements for the professional program in pharmacy leading to the doctor of pharmacy degree. Standards 2016. https://www.acpe-accredit.org/pdf/Standards2016FINAL.pdf. Accessed December 1, 2016.
- 20.Venzke MH, Pintz C, Posey L. Evaluation of a learning module for nurse practitioner students: strategies to address patient vaccine hesitancy/refusal. Nursing Education Research Conference 2016, Poster. http://www.nursinglibrary.org/vhl/handle/10755/603793. Accessed January 1, 2017.
- 21. Question and Answer: Vaccination.World Health Organization. 2016. Accessed January 23, 2017.
- 22.Seal CR, Miguel K, Alzamil A, Naumann SE, Royce-Davis J, Drost D. Personal-interpersonal competence assessment: a self-report instrument for student development. Res High Educ J. 2015;27:1–10. [Google Scholar]