Abstract
Aim:
We created a Learning Health System, the “Learn From Every Patient” program, embedded in our cerebral palsy team clinic. This program was designed to simultaneously provide clinical care while systematically collecting data for quality improvement and research projects on all patients.
Method:
Clinicians created tools within the Electronic Health Record to discretely capture data for clinical use which was also available for quality improvement/research efforts. At baseline, all patients in our clinic received annual hip x-rays to screen for hip displacement. Using our “Learn From Every Patient” database, we reviewed the outcomes for the most mildly affected patients, Level I on the Gross Motor Functional Classification System.
Results:
One hundred thirty-two patients were classified as Gross Motor Functional Classification System Level I. During the study period, these patients received 212 pelvis x-rays, viewing 424 hips, of which 419 (98.8%) were normal. Five hips (1.2%) had < 30% displacement. None had any hip-related symptoms nor required any procedures during the period. We used these data to create an evidence-based change in our standardized hip screening procedure by eliminating annual screening x-rays for this population.
Interpretation:
This implementation of a local learning health system approach to systematically collect research data simultaneously with routine clinical care enabled us to implement an evidence-based improvement in clinical practice. This complete integration of research into clinical care improved care by reducing radiation exposure, while simultaneously reducing health care costs.
INTRODUCTION
A Learning Health System (LHS) incorporates “a continuous cycle of systematic care improvement by coupling evidence generation with evidence application to health care.”1 We recently reported on the implementation of such a system, the “Learn From Every Patient” (LFEP) Program in the Cerebral Palsy (CP) program at Nationwide Children’s Hospital.2 In the LFEP Program, the Electronic Health Record (EHR) supports the systematic collection of discrete data during all clinical encounters, which simultaneously meets clinical documentation requirements while informing quality improvement (QI) and research efforts (Fig. 1). Our early results confirmed significant improvements in the value of care, with decreased inpatient and emergency care utilization, while increasing the number of patients served. In an editorial,1 we discussed the promise of an LHS, which could fully integrate clinical care and research data collection on all patients, and systematically improve outcomes. We report here additional evidence demonstrating that our local LHS program can “learn” by systematically producing evidence during routine clinical care that directly improves outcomes.
Fig. 1.
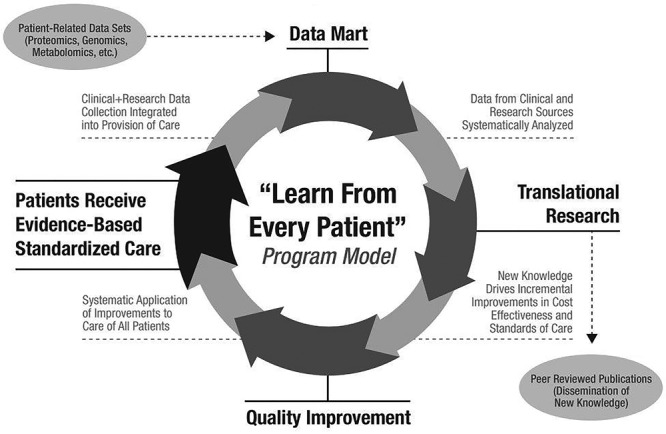
The LFEP Model for the Systematic Improvement of Evidence-Based Clinical Care. Starting with the introduction of a standardized “evidence + expert-opinion-based clinical protocol,” each patient encounter includes the collection of combined “clinical + research data,” which is transferred to a data mart, where it is integrated with other patient-related datasets (proteomics, genomics, metabolomics, etc.). These data can then be queried to address specific clinical or translational research questions. The analyzed data are submitted for publication in peer-reviewed journals (ie, dissemination of new knowledge), and the new knowledge used to drive incremental improvements in cost-effectiveness, and standards of care. This “QI” is then applied systematically to the care of all patients in the form of specific evidence-based improvements in the original standardized clinical protocol. Continued iterations of this “improvement cycle” then drive continuous, systematic improvements in future evidence-based clinical care. (Modified with permission).2
CP is a group of permanent, nonprogressive disorders of the motor system that are caused by disturbances in the developing brain.3 Clinicians classify patients with CP according to motor ability by the Gross Motor Functional Classification System (GMFCS), in which patients who are Level I are the most mildly affected and do not require adaptive devices for ambulation, whereas patients with more severe motor problems are classified at Levels II–V.4 Patients with CP frequently experience subluxation or dislocation of the hips due to lower limb spasticity,5 leading to pain, decreased ambulation, and lower quality of life.6 The frequency of significant hip dislocation increases with the severity of CP, and multiple strategies exist to radiographically screen for hip subluxation in hopes of reducing the likelihood of painful dislocation.7,8
Despite the previously published strategies, our clinic practice at baseline was to screen every patient with an anteroposterior x-ray of both hips every year, regardless of GMFCS level. This LHS initiative was designed to use our EHR to review outcomes for our patients mildly affected with CP and “learn” if this level of screening was warranted.
METHODS
The LFEP Program uniquely incorporates discrete research data collection into the clinical EHR through data capture that is driven by physician-inspired research questions that are expected to improve patient care. Lowes et al.2 described this process in detail elsewhere. The interdisciplinary CP team instituted the LFEP Program in the clinic at Nationwide Children’s Hospital, Columbus, Ohio, in 2011. It includes an annual visit with specialists in 8 medical and allied disciplines. The team meets after each clinic to construct an interdisciplinary care plan for each patient. This practice increases team communication and minimizes patient care fragmentation.
The clinical team identified the discrete clinical data that would be collected during the provision of all routine (billable) clinical care, keeping in mind that these same data points would provide prospective disease-specific data for identified clinical research and QI projects. Within the EHR (Epic, Epic Systems Corp, Verona, Wis.) the clinical team created 3 key components of the LFEP program: (1) a list of discrete clinical data elements to fully document routine clinical care; (2) a prioritized list of research/QI questions designed to drive specific improvements in clinical care; and (3) a list of discrete research data elements able to answer these questions.
EHR tools, such as “drop down boxes” and “flowsheets” support discrete data collection to allow the clinical providers to select specific values. These discretely recorded data then populate the clinical note and are sent to the enterprise data warehouse, eliminating duplicate information entry (Fig. 2). Though the use of free text is minimized because it is not discrete, it can still be added to the clinical note as desired.
Fig. 2.
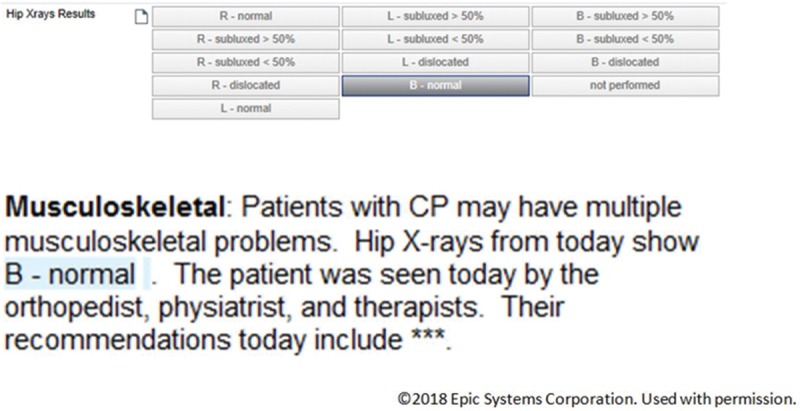
Example of the Epic Smartform (top) and Notewriter (bottom). The provider enters data in the flowsheet during regular clinic care, which helps the provider write the clinical note and capture data for later research or QI use.
The QI question of the current study was to examine the current practice of screening for hip displacement in patients mildly affected by CP. When the LFEP Program began, our practice included annual screening hip radiographs on every patient, with results entered into the EHR for inclusion in the clinical note (in addition to ~250 other clinical data points). One of the physicians (Orthopedist, Physiatrist, or Pediatrician) entered this data point based on his/her interpretation of the hip radiograph. Using Reimer’s method of measuring hip migration,9 the physician classified each hip as normal, displaced < 50%, displaced > 50%, or dislocated. The team assigned GMFCS level by consensus. This study, in which data collection occurred entirely within the EHR during routine care, was approved by the Nationwide Children’s Hospital Institutional Review Board.
RESULTS
Between 12/13/2011 and 7/1/2014, the team classified 132 patients as GMFCS Level I, with a mean age of 7.8 years (SD, 4.9; range, 1–22 years). These patients received 212 pelvis x-rays, viewing 424 hips, of which 419 (98.8%) were normal. Five hips (1.2%) had < 50% displacement. These x-rays were re-reviewed by the study team, and all were minimally (< 30%) displaced. Further examination of the medical records revealed that none of these patients had any hip-related symptoms nor required any procedures on the hips during the period.
Based on this evidence systematically generated during routine clinical care, the physicians on our team determined that screening hip radiographs for patients with Level I CP were not warranted. Analysis of these data, collected entirely during routine clinical care, enabled our team to simultaneously introduce an evidence-based care improvement for current and future patients. Patient safety was improved by reducing radiation exposure (42–254 mRad per x-ray per year, depending on patient size) and costs (average $66 per x-ray per child per year, collected from family, and/or insurance company).
DISCUSSION
The systematic collection of research and clinical data together in the EHR during routine clinical care, as part of the Learn From Every Patient program, enabled the collection of robust research-quality data that directly enabled an evidence-based improvement in care. Importantly, it also simultaneously reduced the cost of care, and potential treatment-related morbidity (radiation exposure).
Although hip screening protocols had been previously published,7,8 our local practice did not yet reflect the recommendation to limit hip X-rays in mildly affected children with CP. In fact, we needed to be convinced by our data to make such a change in practice. This is a strength of a Learning Health System, where local observations can lead directly to implementation. We found that our local data also strongly supported the previously suggested strategies, in which patients with Level I CP receive a single screening hip x-ray upon diagnosis of CP, and are only re-imaged if symptoms referable to the hip develop.
To perform this study as a traditional chart review, we would have had to abstract every patient’s chart to record GMFCS level and hip film results. This requirement would have been a time-consuming process of reading through the written chart notes and radiology reports. In marked contrast, the LFEP process of systematic collection of data enabled a simple computer search of existing records, generating both patients of interest and their x-ray results. The only active chart review required was a review of a small number of abnormal radiographs.
Clinician-researchers can easily access clinical and research data for “learning projects” such as the 1 detailed above. Importantly, this large and growing dataset is also available for all team members to perform future collaborative research and QI projects to generate evidence to improve clinical care. Other ongoing learning projects at our institution include an examination of caregiver experience among parents of children with CP;10 an examination of obesity in tube-fed children with CP;11 and factors associated with changing communication skills in children with CP (in process).
This study provided an example of how an LHS can contribute to improving health care value by improving quality and reducing costs, in this case by eliminating a common screening procedure (hip radiographs) for a specific group of patients. Although a relatively low cost to the patient or insurance company (average $66), this is an annual saving for each patient for each year. Because the patients studied are children, these savings accrue over the lifetime of children with CP. Future LFEP QI and/or research projects can continue to examine other methods to improve health care value.
Although this example of an LHS was specifically created in a CP program in a pediatric hospital, similar projects could be undertaken in any program with any patient population. As we discussed in our previous article,2 requirements for a robust LHS include active involvement of the clinical team in identification of the relevant data elements, smart forms, and templates; note templates that ease the process of data entry, making use of the smart forms a quicker way to document; regular review of the smart forms to ensure continued relevance; and the ability for clinicians to easily review their own data for research and QI. We believe such an LHS could be scaled up to larger programs, even system-wide initiatives, provided that EHR tools are easier to use than other methods of documentation. Also, clinician buy-in and participation from the beginning is crucial.
A limitation of this study method is that data are collected during regular clinical care by clinicians, with potential errors in data entry. In the small number of hip x-rays that were re-reviewed for this study, we found all of that data to be accurate. However, to ensure that all data collected during routine care are both complete and accurate, we believe that review of these data by a provider with content area expertise is necessary.2
In summary, although we previously reported that the LFEP Program could be implemented cost-effectively to improve care and reduce costs,1,2 this report extends those early findings by now demonstrating a specific example of how such an LHS can indeed “learn” to systematically improve future care.
ACKNOWLEDGMENTS
The authors acknowledge the Meuse Family Foundation and the Pedal-with-Pete Foundation, Inc., for their support of the LFEP Program. The funders had no role in the study design, data collection, data analysis, article preparation, or publication decision.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Footnotes
Published online September 5, 2018
To cite: Noritz G, Boggs A, Lowes LP, Smoyer WE. Evidence That Local Learning Health Systems Can Systematically Learn and Improve Patient Care: A Report from the “Learn From Every Patient” Program. Pediatr Qual Saf 2018;3:100.
REFERENCES
- 1.Smoyer WE, Embi PJ, Moffatt-Bruce S. Creating local learning health systems: think globally, act locally. JAMA. 2016;316:2481–2482.. [DOI] [PubMed] [Google Scholar]
- 2.Lowes LP, Noritz GH, Newmeyer A, et al. ; ‘Learn from Every Patient’ Study Group. ‘Learn From Every Patient’: implementation and early results of a learning health system. Dev Med Child Neurol. 2017;59:183–191.. [DOI] [PubMed] [Google Scholar]
- 3.Rosenbaum P, Paneth N, Leviton A, et al. A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl. 2007;109:8–14.. [PubMed] [Google Scholar]
- 4.Palisano R, Rosenbaum P, Walter S, et al. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39:214–223.. [DOI] [PubMed] [Google Scholar]
- 5.Soo B, Howard JJ, Boyd RN, et al. Hip displacement in cerebral palsy. J Bone Joint Surg Am. 2006;88:121–129.. [DOI] [PubMed] [Google Scholar]
- 6.Ramstad K, Jahnsen RB, Terjesen T. Severe hip displacement reduces health-related quality of life in children with cerebral palsy. Acta Orthopaedica. 2016;88:1–6.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dobson F, Boyd RN, Parrott J, et al. Hip surveillance in children with cerebral palsy. Impact on the surgical management of spastic hip disease. J Bone Joint Surg Br. 2002;84:720–726.. [DOI] [PubMed] [Google Scholar]
- 8.Wynter M, Gibson N, Willoughby KL, et al. ; National Hip Surveillance Working Group. Australian hip surveillance guidelines for children with cerebral palsy: 5-year review. Dev Med Child Neurol. 2015;57:808–820.. [DOI] [PubMed] [Google Scholar]
- 9.Reimers J. The stability of the hip in children. A radiological study of the results of muscle surgery in cerebral palsy. Acta Orthop Scand Suppl. 1980;184:1–100.. [DOI] [PubMed] [Google Scholar]
- 10.Lowes L, Clark TS, Noritz G. Factors associated with caregiver experience in families with a child with cerebral palsy. J Pediatr Rehabil Med. 2016;9:65–72.. [DOI] [PubMed] [Google Scholar]
- 11.Noritz G, Lowes L, Johnson L, et al. Overweight status in children with cerebral palsy. Dev Med Child Neurol. 2016;58:24–25.. [Google Scholar]


