Supplemental Digital Content is available in the text.
Abstract
Objective:
Pediatric sepsis remains a significant cause of morbidity and mortality despite the development of strategies proven to improve diagnosis and treatment. Specifically, early recognition and urgent therapy initiation are consistently associated with improved outcomes. However, providers bring these principles inconsistently to the bedside. The objective of this study was to describe practitioner knowledge of, and attitudes toward, sepsis as a means of identifying potentially modifiable factors delaying life-saving treatment. We hypothesized there would be difficulties with sepsis recognition and self-reported discomfort with making the diagnosis among all provider groups in a pediatric tertiary care center.
Methods:
Emergency department and inpatient pediatric physicians, nurses, and respiratory therapists in a single, freestanding children’s hospital received an electronic survey. Likert scales permitted anonymous self-reporting of comfort and diagnostic delays. Seven clinical vignettes assessed diagnostic knowledge. Independent sample t tests and Chi-square compared responses.
Results:
Three hundred two staff participated (73% response rate), 41% of whom had at least 10 years of clinical experience. One in 5 was uncomfortable alerting coworkers to a patient with suspected sepsis or septic shock, and almost half were uncomfortable doing so in cases of compensated shock. Every role self-reported diagnostic delays, including faculty physicians. On average, physicians answered a greater percentage of vignette questions correctly (66%), compared with nurses (58%; P = 0.013) and respiratory therapists (52%; P = 0.005).
Conclusions:
Sepsis knowledge deficits, provider discomfort, and diagnostic delays are prevalent within a tertiary care children’s hospital. Their presence and scale suggest areas for future research and targeted intervention.
INTRODUCTION
Each year, the United States alone spends billions of dollars treating pediatric sepsis and its sequelae. Children with the most severe forms (severe sepsis and septic shock) are often treated in a pediatric intensive care unit (PICU) and may be hospitalized for weeks.1–3 By the time they arrive in the PICU, as many as two-thirds of these patients will have sepsis-induced multiorgan dysfunction.4 Given the well-described relationship between time to therapy, and sepsis outcomes, a likely explanation for presenting to the ICU at such an advanced stage of disease is a delay in diagnosis. Whether at the onset of sepsis or during clinical decompensation, such delays may postpone crucial treatment.5–7
Diagnostic errors (including delays) are not uncommon, identified somewhere in the clinical course of approximately 10–20% of patients.8–10 One large, multicenter study of physician errors and delays found that 28% were self-reported as “major.”11 Septic patients may be especially vulnerable to these mistakes, as diagnostic delays are the most commonly cited barrier to timely, life-saving therapy.12 As a result, in this study, we chose to examine why diagnostic delays might occur in these patients in our institution. Specifically, our objective was to describe 2 factors that could be both contributory and modifiable—practitioner knowledge and attitude.
Previous studies describe knowledge deficits on a smaller scale. In 1 single-center audit, fewer than half of nurses could recognize sepsis and septic shock in a vignette series even though almost all (90%) indicated they were comfortable doing so.13 Another survey, of physicians-in-training, found only 38% could identify the diagnostic criteria for sepsis, 20% for septic shock. This improved to 54% and 67%, respectively, with the addition of a “sepsis module” to their curriculum.14
Other initiatives, emphasizing knowledge as a springboard to timely therapy, have also shown success. Improved staff knowledge was credited with helping decrease ICU length of stay and mortality in adult sepsis.15 Early emergency department (ED) recognition of pediatric septic shock has decreased the likelihood of PICU admission and mortality.16 Likewise, a focus on rapid initiation of therapy has also improved outcomes. In 1 adult study, beginning fluid resuscitation within 30 minutes of septic shock recognition decreased mortality and hospital length of stay.17 Practically, breakdowns in provider-to-provider reporting (eg, bedside nurse-to-physician) may be as consequential as diagnostic or therapeutic delays. However, the literature has yet to evaluate their impact on sepsis.
To the best of our knowledge, no study has examined multidisciplinary sepsis knowledge and attitudes in a pediatric tertiary care center—where the expectation is timely, expert diagnosis and therapy. We hypothesized that all provider roles and teams surveyed would show evidence of diagnostic knowledge deficits and discomfort with recognition.
METHODS
We performed this study at the Women and Children’s Hospital of Buffalo (WCHOB), a 200-bed, urban hospital serving Buffalo, New York, and its surrounding counties. As a tertiary care center, it offers general and subspecialty pediatric services to anyone under 21 years of age. WCHOB admits 12,000 children annually, including 90–120 cases of severe sepsis and septic shock. Virtually all these cases come to count among the 1,200 annual PICU admissions, where they have an unadjusted mortality rate of roughly 2%.
Study Impetus
In late 2014, diagnostic delays in a case of septic shock triggered an institution-wide effort to improve recognition and management of sepsis. A statewide, hospital reporting mandate from the Department of Health, beginning in 2015, strengthened its momentum. Over the next year, physicians, registered nurses (RNs) and respiratory therapists (RTs) from the ED, general floors, and PICU participated in a series of focus groups, conducted by PICU physicians and nurse educators, to identify challenges to recognizing sepsis. Feedback from these sessions informed survey development for this study. Of note, WCHOB has had a Severe Sepsis Management Protocol since 2013.
Hospital leadership viewed this survey as one aspect of an institutional needs assessment, to help determine any necessary changes to the protocol, staff education, and provider culture. As such, no formal sepsis education occurred before, or during, its distribution and response window. The sole intervention during this time was the implementation of a cloud-based EHR alert system (St John Sepsis: Cerner Corporation, Kansas City, Mo.) in September 2015. This Electronic Health Record alert provided real-time “Systemic Inflammatory Response Syndrome (SIRS)” and “Sepsis” notifications to nurses whenever their patients met predetermined vital sign or laboratory criteria. Alerts mandated only that an RN notifies a physician provider. There was no structured sepsis education given to staff before its rollout.
Study Subjects and Eligibility Criteria
All physicians, nurses, RTs, physician assistants (PAs), and nurse practitioners (NPs) working in the ED, General Pediatrics floors, and PICU were eligible. RNs and RTs from the Stabilization and Transport (STAT) team were included as the first responders to medical emergencies and sepsis alerts. We excluded Obstetrics/Gynecology, Anesthesia, Surgery, and Neonatology providers.
General Survey Design
Participants indicated their provider role (eg, resident physician), primary team (eg, PICU) and experience (eg, years out of training or postgraduate year). Anyone normally dividing clinical time between teams (eg, RTs rotating in PICU and ED) identified with the team on which they spent over 50% of their time. This study considered any respondent out of training for at least ten years to be “experienced.”
This study divided nondemographic questions into 4 domains: attitude and comfort, knowledge, past behavior, and sepsis education preferences (see Supplemental Digital Content 1 at http://links.lww.com/PQ9/A34). To help ensure content validity, 10 pediatric providers (3 MDs, 3 RNs, 2 RTs, and 2 NPs) initially piloted the survey. All had at least 5 years of critical care experience in an outside tertiary center, and none was an eligible subject.
Survey Development—Attitude and Comfort
The medical literature documents multiple obstacles to “speaking up” for health care providers, even when patient safety concerns arise.18,19 These have the potential to make “comfort” with recognizing sepsis, in and of itself, less pertinent to patient care and our institutional needs assessment. As a result, we assessed comfort with the following statements:
“I feel comfortable alerting other providers that a patient may have SIRS or sepsis based on my own evaluation.”
“I feel comfortable alerting other providers that a patient may have severe sepsis or septic shock based on my own evaluation.”
“I feel comfortable diagnosing a patient with septic shock if they have a blood pressure that is in the ‘normal’ range.”
Participants rated their level of agreement with each on a 5-point Likert scale (from “Strongly Disagree” to “Strongly Agree”). The survey did not explicitly define “comfort” for respondents. We considered any nonneutral reply (ie, “Somewhat” or “Strongly” Agree, “Somewhat” or “Strongly” Disagree) indicative of provider comfort or discomfort, respectively.
Survey Development—Past Behavior
This section used a Likert-scale matrix to allow participants to self-report how often they hesitated to act on suspicion of sepsis or shock. Specifically, they indicated the frequency with which they have hesitated to act for the following reasons: discomfort with giving a patient the “label” of sepsis, worry about a negative response from a colleague, worry about “making a big deal” in case the diagnosis was incorrect, and past discouragement from making the diagnosis. Feedback from multidisciplinary focus groups informed these rationale statements.
Survey Development—Knowledge
Seven clinical vignettes, developed by the principal investigators, assessed diagnostic knowledge. Five were based on cases reviewed by the WCHOB Pediatrics Quality Assurance Committee from 2014 to 2015, including the index case discussed above. The remainder used focus group input on “challenging” patients. Identifying demographics (eg, age, diagnosis, vital signs) were different to limit recall for providers involved in the actual cases.
Each vignette provided a brief history of present illness, primary diagnosis, and physical examination and laboratory findings. Septic shock vignettes included additional information that might be pertinent to diagnosing shock, including urine output, vasopressor requirements and blood gas data. Respondents indicated simply “Yes” or “No” at the end of each vignette, to the question of whether patients met sepsis or septic shock criteria. The pediatric criteria published by Goldstein et al.20 served as the basis for correctness (Supplemental Digital Content 2, available at http://links.lww.com/PQ9/A35).
Survey Development—Future Education
Respondents indicated agreement with various aspects of potential sepsis education, including content, format, and target audience. Rank order lists identified priorities and preferences.
Survey Dissemination
Eligible staff received 4 e-mails over a 10-week span (October through mid-December 2015) asking them to participate. Each contained an electronic link to the survey webpage, instructions for completion, and a description of the study objective and plan for data usage. Respondents gave consent with survey initiation. Participation was voluntary, anonymous, and nonincentivized.
Analyses
Surveys were collected utilizing Question Pro software (Question Pro Inc., Seattle Wash.). Independent sample t tests compared continuous parametric data between categories, with Chi-square used to compare proportions between categories. For analysis purposes, all responses to questions of frequency were subcategorized as “regular” if respondents sometimes chose, frequently, or very frequently. Analyses were performed using IBM SPSS software, version 21 (Chicago, Ill.). Statistical significance was set at a P value of < 0.05.
The Institutional Review Board of the University at Buffalo approved this study.
RESULTS
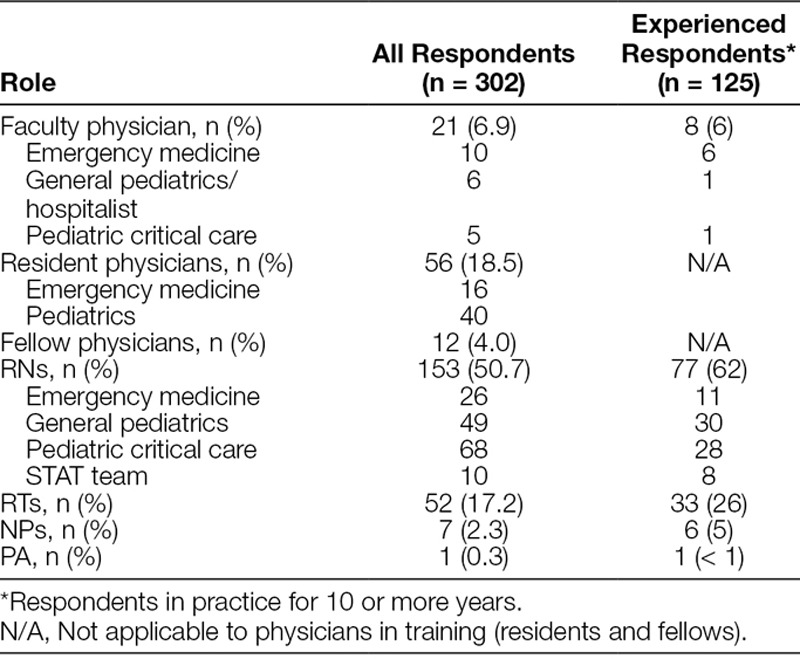
A total of 412 providers were eligible for participation. Approximately 73% (n = 302) completed the survey. Table 1 displays respondent demographics. Approximately half of all responses were from RNs. Based on one-sample, binomial analyses comparing actual to expected participation, the percentage of nurse respondents to the survey was no different than the proportion of nurses among hospital staff (P = 0.28). On the contrary, the percentages of faculty physician, RT, and advanced practitioner (NP and PA) respondents were all higher than their respective proportions among hospital staff (ie, these groups were overrepresented, all P values < 0.001).
Table 1.
Characteristics of Survey Respondents as Stratified by Role and Experience
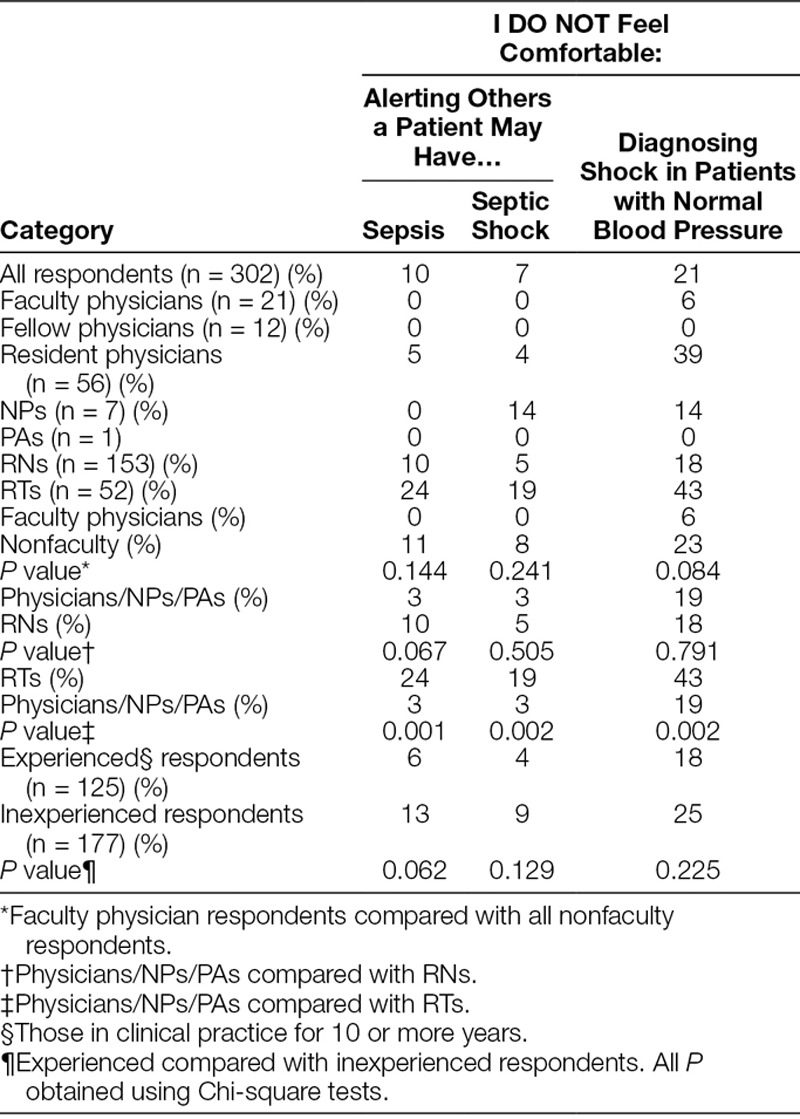
Attitude and Comfort
Most (79%) respondents agreed (“Somewhat” or “Strongly”) with statements of comfort in recognizing SIRS/sepsis and severe sepsis/septic shock and alerting a coworker. However, 1 in 10 disagreed (“Somewhat” or “Strongly”) for cases of SIRS/sepsis and 7% for severe sepsis/septic shock. Only 52% of respondents indicated they were comfortable diagnosing septic shock in patients with normal blood pressure.
Experienced and inexperienced respondents agreed in similar proportions for cases of SIRS/sepsis (P = 0.62), severe sepsis/septic shock (P = 0.13), and septic shock with normal blood pressure (P = 0.23). Likewise, there was no difference among physicians (faculty/housestaff), advanced practitioners, and RNs. However, RT respondents indicated disagreement (ie, discomfort) in greater numbers for both SIRS/sepsis (P = 0.001) and severe sepsis/septic shock (P = 0.002) when compared with other roles (Table 2).
Table 2.
The Proportion of Respondents Indicating Discomfort with Diagnosing or Alerting Others to a Patient with Sepsis or Septic Shock
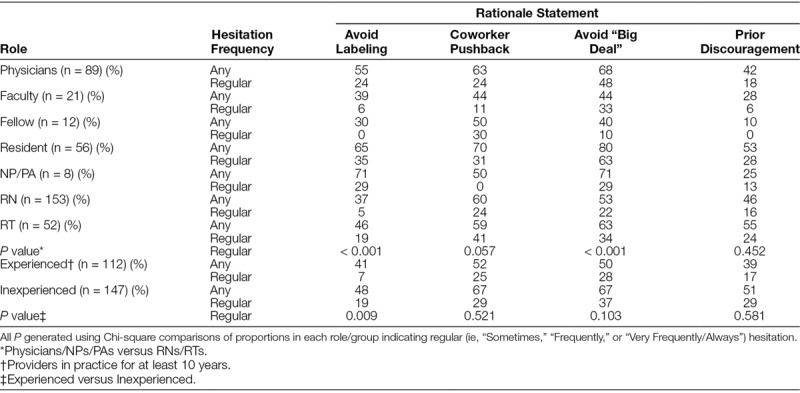
Past Behavior
Table 3 displays the percentage of respondents reporting hesitation with bringing sepsis or septic shock concerns to the care team. Every group (except PAs, n = 1) had members indicating they hesitate regularly for one reason or another, even faculty physicians. All groups reported a similar frequency of hesitation when the rationale was prior discouragement or worry over a negative reaction. A greater percentage of physicians and advanced practitioners, compared with others, reported hesitating regularly when the concern was mistakenly “making a big deal” (P < 0.001) or “labeling” the patient (P < 0.001). Labeling concerns also elicited more regular hesitation from inexperienced (19%) respondents than experienced (7%) respondents (P = 0.009).
Table 3.
Percentage of Respondents Self-reporting Hesitancy to Bring Sepsis or Septic Shock Concerns to their Care Teams
Knowledge
Table 4 displays clinical vignette performance. The overall mean score was 65.8% with no difference between the 7 provider roles (P = 0.132). Faculty physicians (69.6% ± 20.1%) did not perform significantly better than resident physicians (59.1% ± 21.9%; P = 0.065). Likewise, there was no difference in mean score between experienced (57.3% ± 22.8%) and inexperienced (61.8% ± 21.3%) respondents (P = 0.119) or between nurses from different units of the hospital. However, physicians did outperform RNs (P = 0.013) and RTs (P = 0.005). Practitioners indicating awareness of the WCHOB Severe Sepsis Management Protocol answered more questions correctly than the unaware (61.1% versus 51.1%; P = 0.001).
Table 4.
Clinical Vignette Performance, as Determined by Mean Correct Percentage, of and between Survey Respondents
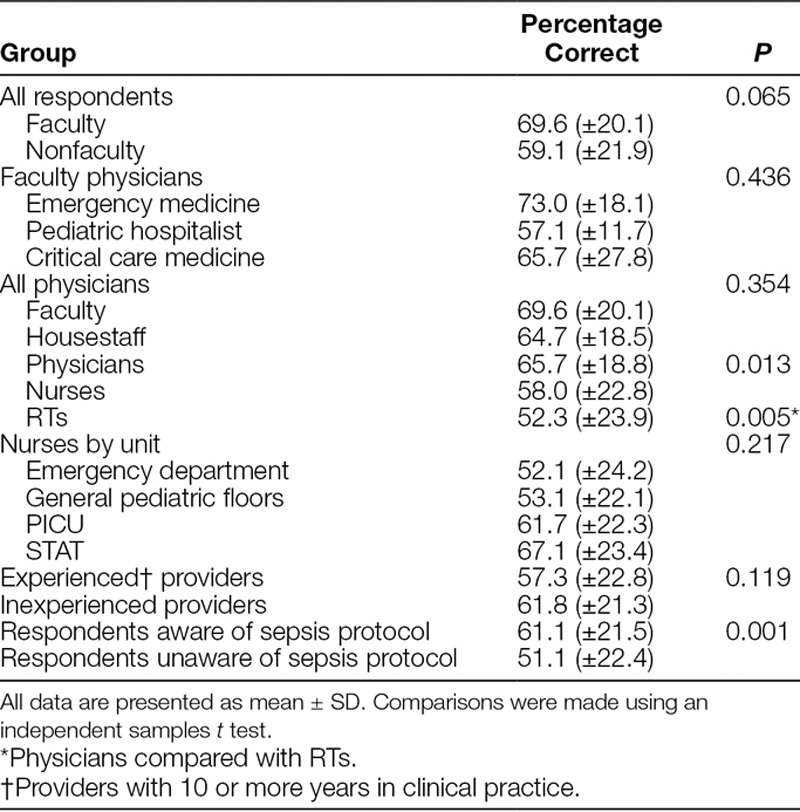
Figure 1 displays performance by individual vignette. Vignette 3—a teenager with Influenza infection, fever, tachycardia, and tachypnea—was correctly identified as septic by fewer RTs (21%) and RNs (25%) than physicians (51%; P < 0.001). This was also the vignette with the lowest overall correct score (34%).
Fig. 1.
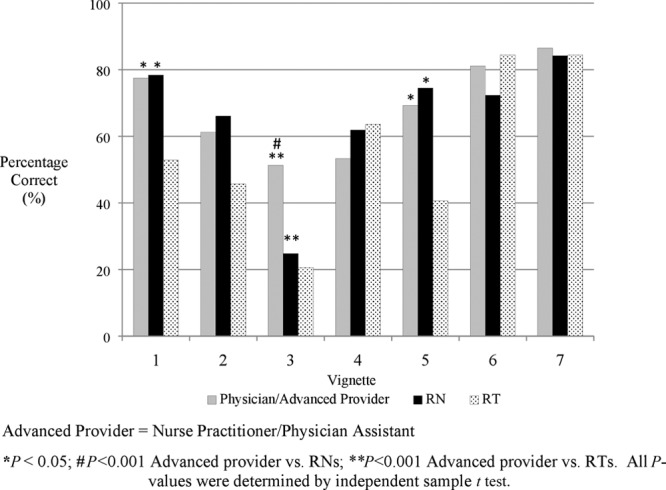
Mean percentage of correct vignette responses by provider group.
Future Education
Most respondents agreed that anyone with a role in patient care at WCHOB should be able to recognize sepsis (95%) and that any future education should be mandatory (90%). There was considerable disagreement with limiting sepsis instruction to physicians and/or ED/PICU providers, especially among RNs (87%) when compared with physicians (63%; P = 0.001). Nurses also favored mandatory education (74%) more than non-RN respondents (58%; P = 0.003). The 3 platforms for education preferred by all groups were (in varying priority) simulation, online modules, and small-group sessions. Early recognition, timely intervention, and review of diagnostic criteria were the content points requested most often.
Institution Assessment
Only 47% of respondents agreed that WCHOB providers diagnose sepsis stringently, based on published criteria. A similar proportion (48%) agreed the institution excels at sepsis recognition. One in 5 inexperienced respondents did not agree with WCHOB’s recognition excellence, compared with 11% of experienced participants (P = 0.039). Most (71%) respondents did agree the institution excels at sepsis treatment, with no difference based on experience.
DISCUSSION
This report is the first multidisciplinary assessment of sepsis-related knowledge, attitude and self-reported behavior of pediatric providers across multiple units of a tertiary care center. Our findings suggest deficiencies in practitioner ability to correctly and confidently identify sepsis and septic shock, and raise concerns that these issues may influence behavior and patient care. No provider group nor level of experience was immune to some degree of deficiency and behavioral impact, not even faculty physicians.
While prior studies have found deficits in the diagnostic knowledge of practitioners, subjects have always belonged to singular groups (eg, nurses only).13,14,21,22 Previous descriptions of provider comfort with sepsis recognition have been similarly focused. Our involvement of multiple disciplines likely makes the results more generalizable to centers comparable with WCHOB. Smaller or more resource-limited hospitals may find relevance as well, as most institutions are shifting the burden of responsibility for sepsis recognition and timely therapy initiation to house staff physicians, RNs or RTs.23
One of the more striking findings was the discomfort that 1 in 10 providers had with either recognizing sepsis outright or with notifying the care team. Perhaps unsurprisingly, given the (mostly) singular focus of their role, RTs reported more discomfort than other groups. We view this as evidence of a need for targeted education, especially in centers such as ours, where RTs are nearly always first to the bedside of a deteriorating patient. Interestingly, experience appeared to be irrelevant in this domain. This observation supports a broad, inclusive outreach for future initiatives, as sepsis recognition may not necessarily be a skill gained through experience.
Another noteworthy finding was that of a regular hesitation to call attention to septic patients by all groups, including faculty physicians. Given our reported data, this is unlikely to be due to a pervasive discomfort with recognizing or acting on sepsis, nor to a significant (and shared) knowledge deficit. Although speculative, we must consider that our institutional culture may not adequately support certain aspects of the diagnosis or initiation of therapy in these patients. Perhaps identifying a patient as “septic,” in the mind of certain WCHOB providers, implies a particular degree of illness, work-up, or care requirement. If so, there might be a general reluctance to raise such an “alarm” for fear of being mistaken. This and other possible contributors to provider hesitation will be the subject of future study.
A validated method for evaluating sepsis diagnostic knowledge has not been published, making it difficult to generalize the results of our vignette scoring. However, the similarity in scores across provider groups does suggest a shared degree of knowledge. Interestingly, this finding held after stratification by experience, even though inexperienced respondents would have trained after the launch of the Surviving Sepsis Campaign (SSC). We hypothesized medical education in the post-Surviving Sepsis Campaign era would lend greater focus to recognizing these patients, conferring a diagnostic advantage to inexperienced participants. This did not materialize in our results, likely indicative of the type of “paper-to-practice” breakdown that prompted the recent efforts of Sepsis-3 to reformat its definitions to more closely mimic what occurs at the bedside.24
Additionally, an understanding of fundamentals may be insufficient to appreciate nuance, which could explain why those with more training on the subject (physicians, advanced practitioners) outscored other roles on certain vignettes.
Most respondents favored multidisciplinary education through simulation, online modules, and small-group discussion, with an emphasis on early recognition and treatment. This approach has proven beneficial, as nurses exposed to simulation and online programs reported improvements in knowledge and performed particular sepsis “competence behaviors” more frequently.25 House staff physicians have likewise demonstrated sustained knowledge improvements after structured education.26 Input from this work will shape similar interventions in our institution.
This study has several limitations. It is single-center, which may compromise the external validity of the findings. The exclusion of certain WCHOB providers (eg, surgery practitioners), who must also recognize and manage sepsis, limits generalizability. Follow-up studies will invite these groups to participate. Those who piloted our survey—with critical and tertiary care experience—may have been biased reviewers of sepsis recognition, influencing our assurance of content validity. Unconsidered confounders, the single-center setting, and hypothesis guessing could all threaten construct validity. The latter may be especially pertinent to our use of vignettes with a “Yes/No” answer format as markers of knowledge. Attitudes and comfort may not have been ideally assessed using scales of agreement, as opposed to explicitly defined and quantified comfort, with given statements. Finally, we rely on self-report, making our results subject to a discrepancy between data and practice. However, factors known to foster this discrepancy, such as social desirability bias, typically skew responses away from less-accepted behaviors (eg, clinical hesitation), making ours more likely to be underestimates of the truth.
CONCLUSIONS
This report is the first multidisciplinary evaluation of sepsis knowledge, attitude, and behavior among pediatric providers of a tertiary care center. The findings indicate some degree of discomfort, knowledge deficiency, and clinical hesitation among all groups. Given thve importance of prompt recognition and treatment in sepsis, such findings are especially noteworthy. Despite its limitations, this work is a first step in understanding, and ultimately overcoming, barriers to such timely management. Our results suggest targets for intervention and future study, such as the phenomenon of provider hesitation.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Supplementary Material
Footnotes
Published online September 5, 2018
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
To cite: Breuer RK, Hassinger AB. Identifying Provider Hesitation and Discomfort with Diagnosing Sepsis: A Multidisciplinary Survey of a Pediatric Tertiary Care Center. Pediatr Qual Saf 2018;3:099.
This study was performed at the Women and Children’s Hospital of Buffalo (now John R. Oishei Children’s Hospital).
REFERENCES
- 1.Ruth A, McCracken CE, Fortenberry JD, et al. Pediatric severe sepsis: current trends and outcomes from the Pediatric Health Information Systems database. Pediatr Crit Care Med. 2014;15:828–838.. [DOI] [PubMed] [Google Scholar]
- 2.Watson RS, Carcillo JA, Linde-Zwirble WT, et al. The epidemiology of severe sepsis in children in the United States. Am J Respir Crit Care Med. 2003;167:695–701.. [DOI] [PubMed] [Google Scholar]
- 3.Watson RS, Carcillo JA. Scope and epidemiology of pediatric sepsis. Pediatr Crit Care Med. 2005;6:S3–S5.. [DOI] [PubMed] [Google Scholar]
- 4.Weiss SL, Fitzgerald JC, Pappachan J, et al. ; Sepsis Prevalence, Outcomes, and Therapies (SPROUT) Study Investigators and Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network. Global epidemiology of pediatric severe sepsis: the sepsis prevalence, outcomes, and therapies study. Am J Respir Crit Care Med. 2015;191:1147–1157.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rivers E, Nguyen B, Havstad S, et al. ; Early Goal-Directed Therapy Collaborative Group. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–1377.. [DOI] [PubMed] [Google Scholar]
- 6.Carcillo JA, Davis AL, Zaritsky A. Role of early fluid resuscitation in pediatric septic shock. JAMA. 1991;266:1242–1245.. [PubMed] [Google Scholar]
- 7.Han YY, Carcillo JA, Dragotta MA, et al. Early reversal of pediatric-neonatal septic shock by community physicians is associated with improved outcome. Pediatrics. 2003;112:793–799.. [DOI] [PubMed] [Google Scholar]
- 8.Shojania KG, Burton EC, McDonald KM, et al. Changes in rates of autopsy-detected diagnostic errors over time: a systematic review. JAMA. 2003;289:2849–2856.. [DOI] [PubMed] [Google Scholar]
- 9.Kirch W, Schafii C. Misdiagnosis at a university hospital in 4 medical eras. Medicine (Baltimore). 1996;75:29–40.. [DOI] [PubMed] [Google Scholar]
- 10.Goldman L, Sayson R, Robbins S, et al. The value of the autopsy in three medical eras. N Engl J Med. 1983;308:1000–1005.. [DOI] [PubMed] [Google Scholar]
- 11.Schiff GD, Hasan O, Kim S, et al. Diagnostic error in medicine: analysis of 583 physician-reported errors. Arch Intern Med. 2009;169:1881–1887.. [DOI] [PubMed] [Google Scholar]
- 12.Balamuth F, Weiss SL, Neuman MI, et al. Pediatric severe sepsis in U.S. children’s hospitals. Pediatr Crit Care Med. 2014;15:798–805.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jeffery AD, Mutsch KS, Knapp L. Knowledge and recognition of SIRS and sepsis among pediatric nurses. Pediatr Nurs. 2014;40:271–278.. [PubMed] [Google Scholar]
- 14.Ziglam HM, Morales D, Webb K, et al. Knowledge about sepsis among training-grade doctors. J Antimicrob Chemother. 2006;57:963–965.. [DOI] [PubMed] [Google Scholar]
- 15.Torsvik M, Gustad LT, Mehl A, et al. Early identification of sepsis in hospital inpatients by ward nurses increases 30-day survival. Crit Care. 2016;20:244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lane RD, Funai T, Reeder R, et al. High reliability pediatric septic shock quality improvement initiative and decreasing mortality. Pediatrics. 2016;138 Available at http://pediatrics.aappublications.org/content/138/4/e20154153. Accessed June 15, 2017. [DOI] [PubMed] [Google Scholar]
- 17.Leisman D, Wie B, Doerfler M, et al. Association of fluid resuscitation initiation within 30 minutes of severe sepsis and septic shock recognition with reduced mortality and length of stay. Ann Emerg Med. 2016;68:298–311.. [DOI] [PubMed] [Google Scholar]
- 18.Etchegaray JM, Ottosen MJ, Dancsak T, et al. Barriers to speaking up about safety concerns. J Patient Saf. Published online ahead-of-print: November 4, 2017 (doi: 10.1097/PTS.0000000000000334). Accessed November 30, 2017. [DOI] [PubMed] [Google Scholar]
- 19.Landgren R, Alawadi Z, Douma C, et al. Barriers of pediatric residents to speaking up about patient safety. Hosp Pediatr. 2016;6:738–743.. [DOI] [PubMed] [Google Scholar]
- 20.Goldstein B, Giroir B, Randolph A, et al. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. 2005;6:2–8.. [DOI] [PubMed] [Google Scholar]
- 21.Poeze M, Ramsay G, Gerlach H, et al. An international sepsis survey: a study of doctors’ knowledge and perception about sepsis. Crit Care. 2004;8:R409–R413.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Assunção M, Akamine N, Cardoso GS, et al. ; SEPSES Study Group. Survey on physicians’ knowledge of sepsis: do they recognize it promptly? J Crit Care. 2010;25:545–552.. [DOI] [PubMed] [Google Scholar]
- 23.Owen JA, Brashers VL, Littlewood KE, et al. Designing and evaluating an effective theory-based continuing interprofessional education program to improve sepsis care by enhancing healthcare team collaboration. J Interprof Care. 2014;28:212–217.. [DOI] [PubMed] [Google Scholar]
- 24.Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315:801–810.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Delaney MM, Friedman MI, Dolansky MA, et al. Impact of a sepsis educational program on nurse competence. J Contin Educ Nurs. 2015;46:179–186.. [DOI] [PubMed] [Google Scholar]
- 26.Tromp M, Bleeker-Rovers CP, van Achterberg T, et al. Internal medicine residents’ knowledge about sepsis: effects of a teaching intervention. Neth J Med. 2009;67:312–315.. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


