Abstract
Accumulating evidence has reported that prolonged periods of sedentary time have been recognized as a risk factor for cardiocerebrovascular disease. However, whether high levels of sedentary behavior are associated with an increased risk of cardiocerebrovascular disease in different regions remains unclear.
The aim of this study was to evaluate the association between sedentary behavior and the risk of myocardial infarction (MI) and stroke in Jiangxi Province of China.
A cross-sectional survey was conducted among 15,364 participants in Jiangxi Province of China from November 2013 to August 2014, using standardized questionnaire forms and physical measurements. Self-reported sedentary behavior in daily life and a history of MI and stroke were conducted by answering the questionnaire. The participants were examined for weight, height, waist circumference (WC), body fat percentage (BFP), visceral fat index (VAI), basal metabolic rate (BMR), and blood pressure (BP). Multivariate logistic regression analysis was performed to evaluate the association between sedentary behavior and the risk of MI and stroke after adjustment for sociodemographic characteristics, lifestyle factors, and disease-related risk factors.
Of the 15,364 eligible participants, 13,710 participants (5604 men and 8106 women, aged 15–97 years) completed the questionnaire. Subjects who had longer sedentary behavior were significantly associated with an increased risk of MI and stroke [odds ratio (OR) = 1.22, 95% confidence interval (95% CI): 1.168–1.281, P < .001; OR = 1.59, 95% CI: 1.50–1.67, P < .001]. After stratification by the categorical variable of sedentary behavior, individuals with a longer time of sedentary behavior (≥8 hours) were also related to a higher risk of MI and stroke than those in the sedentary behavior (<4 hours) group (OR = 176.62, 95% CI: 43.33–719.90, P < .001; OR = 478.52, 95% CI: 118.50–1932.36, P < .001). However, there were no significant differences between individuals in the short time of sedentary behavior (<4 hours) group and the middle time (4–8 hours) group (p > 0.05).
Excessive time spent in sedentary behavior was associated with a higher risk of MI and stroke. The results provide robust evidence to support the guideline recommendations regarding reduction of sedentary behavior in daily life.
Keywords: China, cross-sectional survey, MI, sedentary behavior, stroke
1. Introduction
Since the industrial revolution, the development of new technology has exerted a great impact on people's lifestyles, and the amount of sedentary behavior people engage in is rising not only in high-income areas but also in middle- and low-income areas.[1,2] Growing evidence demonstrated that a large amount of sedentary behavior, independent of physical activity levels, is obviously associated with an increased risk of cardiovascular disease (CVD), stroke, metabolic syndrome, diabetes, obesity, mortality, and some cancers in the general population.[3] The LIFE study team found that there was a 1% increase in CVD risk for every increase of 25 to 30 minutes of daily time spent in sedentary behavior among older adults.[4] On the contrary, recent studies have also shown that individuals who had a CVD, diabetes, obesity, and other diseases often spend over 80% of their daily time in sedentary behavior compared with 50% to 60% in healthy individuals, which caused poorer outcomes during the rehabilitation stage, especially the rehabilitation of myocardial infarction (MI) and stroke.[5–8] The Perth Community Stroke Study, containing 138,708 participants, reported that approximately one-third of stroke survivors might have another stroke within 5 years.[9] Up to now, however, the causal relationship between sedentary behaviors and diseases remains unclear.[10] MI and stroke have become leading health problems worldwide, and they are the most common cause of mortality and long-term disability.[11–15] Physical activity has been identified to decrease the risk of MI and stroke, but the protective effect may be negated by prolonged periods of sedentary behavior. This is also why people in moderate or high physical activity groups also suffer a high prevalence of MI and stroke.[1,2,16] Therefore, it is disturbing that the vicious circle between excessive sedentary behavior and cardiac-cerebral vascular diseases continues, even with moderate or high physical activity.
To the best of our knowledge, most data on sedentary behavior correlations in people are from western and high-income countries, with very little from the low- and middle-income countries of the world.[1,17] Furthermore, sedentary behavior has been recognized as a public health issue only in the past decade, and therefore, few standardized instruments are available for its assessment.[17] China, one of the middle-income countries, has great interregional differences in socioeconomic statuses and the prevalence of CVDs among the different regions. For example, the results from the Prospective Urban and Rural Epidemiological (PURE) Study showed that the prevalence of total CVD was lower in high- and middle-income regions than in low-income regions (7.46%, 7.42%, and 8.36%, respectively).[18] Taken together, it is necessary to assess the relationship between sedentary behavior and MI and stroke in the various domains of China. It may increase awareness of people in understanding the determinants of sedentary behavior in MI and stroke and provide the basis for behavior changing strategies.
2. Methods
2.1. Study design and participants
This cross-sectional survey was supported by the National Key R&D Program in the Twelfth Five-year Plan (No. 2011BAI11B01) from the Chinese Ministry of Science. Using a stratified multistage random sampling method, Jiangxi Province was divided into urban areas and rural areas based on administrative data, including 4 cities and 4 counties. The details of the overall study design are described below. Eight different areas were selected using the probability-proportional-to-size method, in which 2 districts or 2 townships were selected. Next, 3 communities or villages were chosen within each district and township, respectively, using the simple random sampling (SRS) method.[19] Finally, a given number of participants from each of the 14 gender/age strata (men/women and aged 15–24, 25–34, 35–44, 45–54, 55–64, 65–74, and ≥75 years) were chosen according to their economic, physical, and sociocultural environments, balanced by the feasibility of the stratum to achieve representative data and accurate conclusions. Standardized approaches were used for the registry of households, which included information compiled by the local government, identification of individuals, recruitment, and data collection.[19] The design effect was also considered while estimating the sample size. Assuming a design effect of 2.5 and a prevalence of hypertension of 17.7% among the population aged 15 years and older, it was estimated that 15,200 participants were required for the analysis to ensure that the average lengths of the 95% confidence intervals (95% CIs) for prevalence in the entire population and in the subpopulations, defined by age and gender, were less than 0.4% and 1.8%, respectively.[19] As a result, 15,364 residents aged 15 years and older who were intending to stay locally for more than 6 months were approached for this survey from November 2013 to August 2014. After excluding participants with missing data, including MI, stroke, and sedentary behavior, the final sample size for analysis varied by the outcome of interest was 13,710 participants, as shown in Fig. 1.
Figure 1.
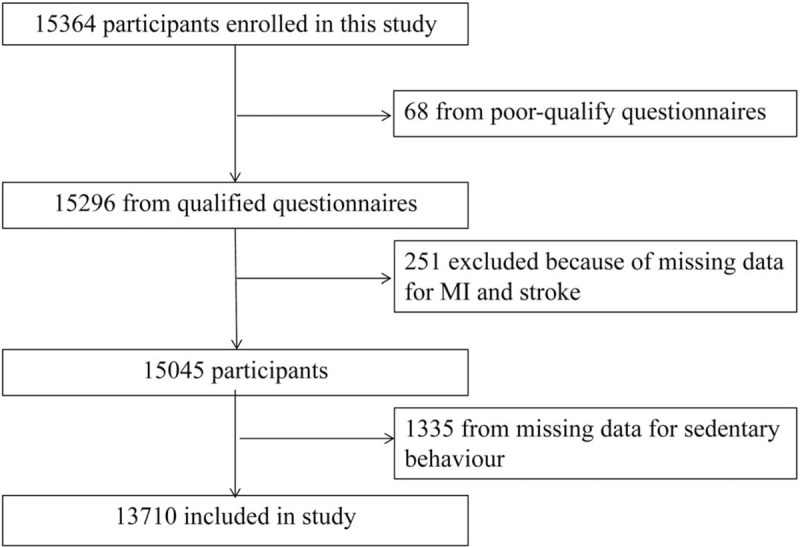
Participant selection for the study.
2.2. Data collection procedures
Standardized interview-based questionnaires developed by the national coordinating center of Fuwai Cardiovascular Hospital (Beijing, China) were administered by trained personnel to participants. The questionnaire included demographic data (such as age, gender, marital status, area, education, and employment status), behavioral characteristics (such as smoking habits, drinking, physical activity, sedentary behavior, and sleeping time), and medical history (hypertension MI and stroke, which was collected and verified with medical or hospital records).
Physical measurements, including body height, weight, waist circumference (WC), body fat percentage (BFP), visceral fat index (VAI), basal metabolic rate (BMR), heart rate (HR), and blood pressure (BP), were collected by standardized methods for anthropometrics. All investigators were medical professionals who were systematically trained, and standard protocols and instruments were used.
To ensure standardization and data quality, comprehensive operations manuals, reinforced by periodic training workshops and regular communication, were used at all sites. Data were entered locally at each site into a customized database programmed with range and consistency checks and transmitted electronically to the coordinating center, where further quality control measures were implemented.
2.3. Anthropometric measurements
Body weight without heavy clothing to the nearest 0.1 kg was measured indoors using an Omron body fat and weight measurement device (V- BODY HBF-371; Omron, Kyoto, Japan). Height was measured without shoes using a standard right-angle device and a fixed measurement tape to the nearest 0.5 cm. WC was obtained to the nearest 0.5 cm by putting the measuring tape at the midpoint between the lower margin of the last rib and the top of the hip bone (at the level of umbilicus) at the end of the expiration. BFP, VAI, and BMR were also measured using an Omron body fat and weight measurement device (V- BODY HBF-371; Omron, Kyoto, Japan). All measurements were taken twice, and the average of the 2 values was used. BP and HR were measured 3 times on the right arm of the participants using an electronic BP monitor (Omron HBP-1300; OMRON, Kyoto, Japan) after a rest of at least 5 minutes, with a 30-second interval between measurements. The process of measuring BP was performed according to the 2010 “Chinese Blood Pressure Measurement Guidelines.”[20] Systolic BP (SBP) and diastolic BP (DBP) were defined as the average of 3 SBP and DBP readings, respectively. Participants were asked to avoid vigorous exercise, smoking, drinking, and consumption of coffee and tea for at least 30 minutes before the measurements.
2.4. Ethics statement
All participants who provided written informed consent were enrolled in the study. If the participants were unable to write, fingerprinting was used. This study was approved by the Medical Research Ethics Committee of the Second Affiliated Hospital of Nanchang University and the Fuwai Cardiovascular Hospital (Beijing, China).
2.5. Definitions
2.5.1. Sedentary behavior
Self-reported sedentary behavior was obtained with the following question: “How long do you spend in your sedentary behavior every day, such as sitting or reclining, including reading, watching TV or working online?” Sedentary behavior is defined as any waking behavior with an energy expenditure ≤1.5 METs, while in a sitting or reclining posture (1 MET is defined as the energy spent when an individual sits quietly).
2.5.2. MI
Self-reported history of MI was obtained with the following question: “Have you been diagnosed with MI by a hospital?” If respondents answered “yes,” they were asked to provide the diagnostic certificate. The electrocardiograms had localized pathological Q waves with or without symptoms; imaging evidence illustrated that the myocardium was thinning or scarring with a loss of contractile force or no viability.
2.5.3. Stroke
Self-reported history of stroke was assessed if respondents answered “yes” to the question, “Have you ever been told by a doctor or other health professional that you had a stroke?” These patients were also asked for symptoms, initial dates, and diagnostic units in order to make a reasonable assessment of the original diagnosis. Stroke included subarachnoid hemorrhage, intracerebral hemorrhage, or cerebral ischemic necrosis, but did not include secondary stroke caused by transient cerebral ischemia, brain tumor, brain metastasis tumor, or trauma.
2.5.4. Hypertension
BP was measured using the Omron HBP-1300 Professional Portable Blood Pressure Monitor (Omron, Kyoto, Japan) 3 times on the right arm supported at the heart level after the participants were allowed to rest for 5 minutes, with a 30-second interval between measurements.[19,21] SBP or DBP was defined as the average of the 3 SBP or DBP readings. Hypertension was defined as SBP ≥140 mm Hg and/or DBP ≥90 mm Hg, and if the individual was on antihypertensive drugs for 2 weeks.[22]
2.5.5. Low income
Low-income group in China refers to those whose income is lower than the annual or monthly income stipulated by the state or province. The urban low-income people are at the bottom of the society and are the vulnerable groups in the urban society. Most of them are unemployed and outside the system (people who have never worked in state-owned units, relying on working and holding small families to support their families), and disabled and widowed elderly people.
2.5.6. Education
Educational level was divided into 3 domains according to the number of years of education, including 0 to 6, 7 to 9, and ≥10 years.
2.5.7. Behavioral characteristics
Smoking habit was defined as never, current (daily smoking, >6 months), and former (cessation of smoking, >6 months). Alcohol drinking was defined as drinking alcohol at least 1 time per week during the previous year.[23–26]
2.5.8. Physical activity
Self-reported physical activity was assessed and classified by the International Physical Activity Questionnaire (IPAQ).[27–30]
2.6. Statistical analysis
All data were established using the EpiData version 3.02 software (Odense, Denmark). After alignment correction, both the Statistical Package for Social Science software 17.0 (SPSS, IL) and Microsoft Excel 2007 were used for statistical analysis. Continuous variables are presented as the mean ± standard deviation and are compared using the t test. Categorical variables are expressed as percentages and were analyzed using the Chi-square test or Fisher exact test, as appropriate. Multivariate logistic regression analysis was performed to evaluate the odds ratio (OR) and 95% CI of MI or stroke being associated with sedentary behavior. Sedentary behavior of < 4 hours/day was chosen as a reference to be consistent with previous studies in the field because most subjects fell in this category.[17] Statistical significance was based on P < .05.
3. Results
3.1. Characteristics of the subjects
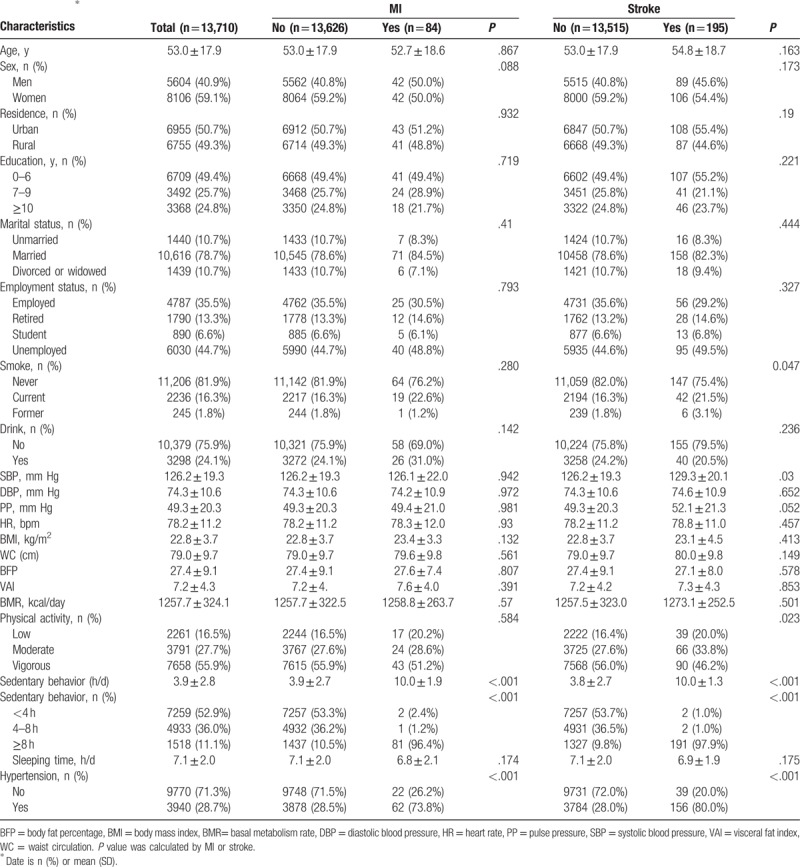
As summarized in Table 1, a total of 13,710 participants of 15,364 eligible participants (5604 men and 8106 women, aged 15–97 years) were included in this analysis. In addition, 1654 participants were excluded due to missing data, including sex, age, sedentary behavior, and history of MI and stroke. Overall, the average age was 53.0 ± 17.9 years. Of the participants, 6955 (50.7%) came from urban areas, and 6755 (49.3%) came from rural areas. The percentages of MI and stroke were 61.3 per 10,000 people (84 cases) and 142.2 per 10,000 people (195 cases), respectively. The mean (SD) values for sedentary behavior were 3.9 ± 2.8, and of the 13,710 participants, 52.9%, 36.0%, and 11.1% reported their sedentary behavior as <4, 4 to 8, and ≥8 hours/day, respectively. Compared with the control group, those who had MI and stroke were more likely to have current habit, history of hypertension, and low physical activity. Overall, there was a significantly increased prevalence of MI and stroke among adults whose sedentary behavior was more than 8 hours. No significant difference in the education, marital status, employment, drink habit, body mass index (BMI), WC, BFP, VAI, BMR, HR, and sleeping time were observed between the control group and the MI or stroke group in this study.
Table 1.
Characteristics of participants.
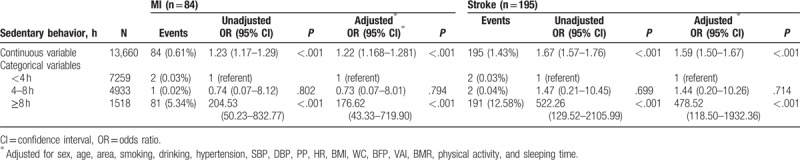
3.2. Association between sedentary behavior and MI and stroke
Table 2 summarizes the association between sedentary behavior and MI and stroke. There were 84 individuals with incidents of MI and 195 individuals with strokes. The logistic regression analysis showed that longer sedentary behavior was associated with a significantly higher risk of MI and stroke (P < .001). In unadjusted logistic regression analysis, continuous sedentary time correlated with the risk of MI and stroke (OR = 1.23, 95% CI: 1.17–1.29, P < .001; OR = 1.67, 95% CI: 1.57–1.76, P < .001). Further adjusted for sex, age, area, smoking, drinking, hypertension, SBP, DBP, PP, HR, BMI, WC, BFP, VAI, BMR, physical activity, and sleeping time, sedentary behavior was still independently correlated to the risk of MI and stroke (OR = 1.22, 95% CI: 1.168–1.281, P < .001; OR = 1.59, 95% CI: 1.50–1.67, P < .001). When stratified by the categorical variable of sedentary behavior, there was a gradual rise in unadjusted event rates for MI and stroke between short time of sedentary behavior (<4 hours) and longer time of sedentary behavior (≥8 hours) (OR = 204.53, 95% CI: 50.23–832.77, P < .001; OR = 522.26, 95% CI: 129.52–2105.99, P < .001). However, there were no significant differences between individuals in the short time of sedentary behavior (<4 hours) and middle time (4–8 hours) groups (P > .05). After adjustment for potential confounders, compared with individuals in the sedentary behavior (<4 hours) group, those with longer times of sedentary behavior (≥8 hours) were still greatly associated with an increased likelihood of MI and stroke (OR = 176.62, 95% CI: 43.33–719.90, P < .001; OR = 478.52, 95% CI: 118.50–1932.36, P < .001). Therefore, in our study, longer times of sedentary behavior were independently associated with risk of MI and stroke.
Table 2.
Association between sedentary behavior and MI and stroke risk.
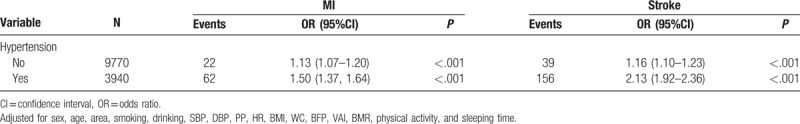
3.3. Association between sedentary behavior and MI and stroke by hypertension
Table 3 summarizes the relationship between sedentary behavior and MI and stroke according to hypertension. When subgroup analyses stratified by hypertension was performed, the logistic regression analysis found that individuals with hypertension had a higher prevalence of MI and stroke as sedentary time increased (OR = 1.50, 95% CI:1.37–1.64, P < .001; OR = 2.13, 95% CI: 1.92–2.36, P < .001), as well as people with normal BP (OR = 1.13, 95% CI: 1.07–1.20, P = .009; OR = 1.16, 95% CI: 1.10–1.23, P < .001). In addition, the results showed that people with hypertension had a higher risk of MI and stroke than those without hypertension at the same sedentary times.
Table 3.
Association between sedentary behavior and MI and stroke by hypertension.
4. Discussion
Findings from the INTER-HEART and INTER-STROKE studies suggested that the risks attributable to the population for MI and stroke had over 90% correlation in each major region of the world, and approaches to prevention could be based on similar principles in high-income as well as low- and middle-income countries worldwide.[31–33] In our study, we evaluated the association between sedentary behavior and the risk of MI and stroke. Increasing sedentary time was related to enhanced risk of MI and stroke. In addition, categories of increasing sedentary time were consistently associated with a higher risk of MI and stroke. Furthermore, the detrimental impacts of sedentary behavior were independent of a range of socioeconomic and cardiocerebrovascular risk factors. The results of our study were similar to the previous findings of the adverse effects of sedentary behavior in high-income areas.[1–3]
Although numerous studies have indicated the negative relationship between sedentary time and MI and stroke, agreement about the levels of sedentary duration has not been established because study results were inconsistent.[6,17,34] Indeed, the study that first highlighted the detrimental effect of sedentary behavior was conducted only in the past decade.[17] The NIH-AARP Diet and Health Study showed that people whose sitting time ≥7 hours had a greater risk of CVD; this was even among adults reporting high levels of moderate-vigorous physical activity (MVPA).[6] Participants with over 9.6 hours sedentary time measured by accelerometer from the National Health and Nutrition Examination Survey were obviously related to CVD,[35] such time that was similar to the conclusion of meta-analysis made by Pandey et al.[34] Paul et al[7] found that stroke survivors had significantly higher sedentary time than the controls (20.4 ± 2.7 vs 17.5 ± 3.8 hours, including sleep time). However, in our analysis, we observed that participants who were sedentary over 8 hours in daily life were significantly associated with an increased risk for MI and stroke after adjusting for confounding factors compared with those whose time less 4 hours. There was no difference in people with a sedentary duration of 4 to 8 hours, which was consistent with the results from Pandey et al.[34] Similar results were also found for continuous sedentary behavior with a significantly higher risk of MI and stroke. The inconsistent association of MI and stroke with sedentary behavior from previous studies may be due to racial differences and differences in population and sample sizes, measurement methods, and diagnosis of MI and stroke. Excessive sedentary behavior has been reported to be the cause of loss of muscle mass and poor cardiopulmonary fitness, which may be one of the main causes of diseases.[36,37] People from different regions and races have their own physical fitness and resistance, particularly in Asia and Europe, as well as different colors. Therefore, it may explain the different sedentary time cutoffs from studies related to the risk of MI and stroke. However, our findings with respect to MI and stroke are consistent with the results from the World Health Organization's study, in which participants whose sedentary time was >8 hours per day had a high risk of stroke.[38] Future studies with respect to the relationship between sedentary behavior and MI and stroke need larger sample sizes and should consider the consistency in measurement and classification methods for sedentary behavior, in greater detail, to increase the reliability and accuracy of the conclusions.
Our study also examined the association between sedentary behavior and MI and stroke according to hypertension. Increasing evidence has demonstrated that excessive sedentary behavior often makes for mass inactivity, which is different from lack of physical activity, decreases aerobic fitness, disturbs metabolism, vascular health, and perfusion, and results in an increased risk of many chronic diseases.[36,39] The formation and progress of hypertension are obviously associated with these facts and lead us to suppose that there was a certain relationship between sedentary time and MI and stroke based on hypertension. Actually, in our analysis, we determined that people with hypertension had a higher risk of MI and stroke at the same sedentary time. Findings from Pandey et al[34] showed that the association between sedentary time and the risk for CVD is nonlinear, with an increased risk only at very high levels. In our survey, we also got the same results: that prolonged periods of sedentary behavior of more than 8 hours might spark a pandemic of MI and stroke, though individuals with hypertension tended to be more obvious and had greater harm. These results may also be caused by long-term loss of muscle mass and low cardiorespiratory fitness, because once they lose the last line of defense, diseases outbreak and the risks continued to increase. Overall, our study demonstrated that people who spent more than 8 hours on sedentary behavior in their daily life may face huge potential risks for MI and stroke events, especially those with hypertension.
This study has several limitations. First, it is a cross-sectional study that cannot establish causal relationships. Prospective longitudinal data are needed for future research. Second, participants in the study were from Jiangxi Province, China, and hence, the generalizability of the results to other populations remains to be verified. Third, sedentary behavior was assessed by self-reporting. Therefore, imprecise reporting of the variables, at least in part, may have occurred, and an overall tendency to overestimate, compared with objective measurements, was inevitable, which may have exaggerated the potential harmful effects of sedentary behavior. Fourth, MI and stroke were also assessed according to the self-reported questionnaire responses. The type and extent of MI and stroke was not evaluated accurately. Finally, although we considered demography, smoking, and drinking habits and several risk factors, such as BMI, WC, and hypertension, the influence of the potential confounding effects cannot be excluded entirely. Despite these limitations, our study has several strengths. An important merit is that this is the first study to assess the association between sedentary behavior and MI and stroke in southern China. Another strength is the prospective study design and inclusion of a large sample from the general population, based on city-gender-age distribution, whereby the validity is improved over that of studies based on hospital data; moreover, the data in our study were obtained from face-to-face interviews, which are more reliable than telephone interviews.
5. Conclusion
Our findings demonstrated that excessive time spent in sedentary behavior was strongly associated with a high risk of MI and stroke events, and this association was independent of demography, physical activity levels, and other risk factors. The results of our study provide robust evidence to support the guideline recommendations regarding the reduction of sedentary behavior in daily life. In addition, given the increasing prevalence of MI and stroke, clinicians should encourage patients who are at risk of developing cardiocerebrovascular diseases to decrease their sedentary behavior.
Acknowledgment
We acknowledge the contributions of the staff members who participated in this study as well as the study participants who shared their time with us.
Author contributions
HHB and XSC conceived the study and revised the manuscript. XSC participated in its design and coordination and helped to draft the manuscript. JXL, PL, YQW, QHW, HHB, XSC participated in its design, performed the statistical analysis, and wrote the manuscript. LLY, QL, LHH, and WZ designed and carried out the questionnaires. LLY, QL, LHH, WZ, XH, CJY collected the samples and did the data clearance. All authors read and approved the final manuscript.
Conceptualization: Lingling Yu.
Data curation: Lingling Yu, Qian Liang, Chunjiao You.
Formal analysis: Qian Liang, Wei Zhou, Xiao Huang.
Funding acquisition: Lingling Yu, Huihui Bao, Xiaoshu Cheng.
Investigation: Lihua Hu, Huihui Bao.
Project administration: Xiaoshu Cheng.
Software: Lingling Yu, Qian Liang, Wei Zhou, Lihua Hu.
Supervision: Juxiang Li, Yanqing Wu, Ping Li, Qinghua Wu, Huihui Bao, Xiaoshu Cheng.
Validation: Huihui Bao, Xiaoshu Cheng.
Visualization: Lingling Yu, Huihui Bao, Xiaoshu Cheng.
Writing – original draft: Lingling Yu, Xiaoshu Cheng.
Writing – review & editing: Lingling Yu, Huihui Bao, Xiaoshu Cheng.
Footnotes
Abbreviations: BFP = body fat percentage, BMI = body mass index, BMR = basal metabolic rate, BP = blood pressure, DBP = diastolic blood pressure, HR = heart rate, MI = infarction, PP = pulse pressure, SBP = systolic blood pressure, VAI = visceral fat index, WC = waist circumference.
LY First author.
Funding/support: This research was supported by the National Key R&D Program in the Twelfth Five-year Plan (No. 2011BAI11B01 and 2014ZX09303305) from the Chinese Ministry of Science and Technology, the National Natural Science Foundation of China (No. 81560051, 81460045, and 81460010), the Significant New Drug Creation (No. 2014ZX09303305) from the Project of National Science and Technology Major Project, the China Postdoctoral Science Foundation Funded Project (No. 2017M622107), and the Graduate Innovation Fund of Jiangxi Province (No. YC2016-B024).
The author(s) of this work have nothing to disclose.
References
- [1].Held C, Iqbal R, Lear SA, et al. Physical activity levels, ownership of goods promoting sedentary behaviour and risk of myocardial infarction: results of the INTERHEART study. Eur Heart J 2012;33:452–66. [DOI] [PubMed] [Google Scholar]
- [2].Hamilton MT, Hamilton DG, Zderic TW. Role of low energy expenditure and sitting in obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease. Diabetes 2007;56:2655–67. [DOI] [PubMed] [Google Scholar]
- [3].Ezeugwu VE, Garga N, Manns PJ. Reducing sedentary behaviour after stroke: perspectives of ambulatory individuals with stroke. Disabil Rehabil 2017;39:2551–8. [DOI] [PubMed] [Google Scholar]
- [4].Fitzgerald JD, Johnson L, Hire DG, et al. Association of objectively measured physical activity with cardiovascular risk in mobility-limited older adults. J Am Heart Assoc 2015;4:e1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Mattlage AE, Redlin SA, Rippee MA, et al. Use of accelerometers to examine sedentary time on an acute stroke unit. J Neurol Phys Ther 2015;39:166–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Matthews CE, George SM, Moore SC, et al. Amount of time spent in sedentary behaviors and cause-specific mortality in US adults. Am J Clin Nutr 2012;95:437–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Paul L, Brewster S, Wyke S, et al. Physical activity profiles and sedentary behaviour in people following stroke: a cross-sectional study. Disabil Rehabil 2016;38:362–7. [DOI] [PubMed] [Google Scholar]
- [8].Tieges Z, Mead G, Allerhand M, et al. Sedentary behavior in the first year after stroke: a longitudinal cohort study with objective measures. Arch Phys Med Rehabil 2015;96:15–23. [DOI] [PubMed] [Google Scholar]
- [9].Hankey GJ, Jamrozik K, Broadhurst RJ, et al. Five-year survival after first-ever stroke and related prognostic factors in the Perth Community Stroke Study. Stroke 2000;31:2080–6. [DOI] [PubMed] [Google Scholar]
- [10].Proper KI, Singh AS, van Mechelen W, et al. Sedentary behaviors and health outcomes among adults: a systematic review of prospective studies. Am J Prev Med 2011;40:174–82. [DOI] [PubMed] [Google Scholar]
- [11].Donnan GA, Fisher M, Macleod M, et al. Stroke. Lancet 2008;371:1612–23. [DOI] [PubMed] [Google Scholar]
- [12].Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2197–223. [DOI] [PubMed] [Google Scholar]
- [13].Feigin VL, Krishnamurthi RV, Parmar P, et al. Update on the global burden of ischemic and hemorrhagic stroke in 1990-2013: the GBD 2013 study. Neuroepidemiology 2015;45:161–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation 2016;133:e38–60. [DOI] [PubMed] [Google Scholar]
- [15].Correction to: heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation 2017;135:e646. [DOI] [PubMed] [Google Scholar]
- [16].van der Ploeg HP, Chey T, Korda RJ, et al. Sitting time and all-cause mortality risk in 222 497 Australian adults. Arch Intern Med 2012;172:494–500. [DOI] [PubMed] [Google Scholar]
- [17].Hallal PC, Andersen LB, Bull FC, et al. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet 2012;380:247–57. [DOI] [PubMed] [Google Scholar]
- [18].Yan R, Li W, Yin L, et al. Cardiovascular diseases and risk-factor burden in urban and rural communities in high-, middle-, and low-income regions of China: a large community-based epidemiological study. J Am Heart Assoc 2017;6:pii: e004445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Wang Z, Zhang L, Chen Z, et al. Survey on prevalence of hypertension in China: background, aim, method and design. Int J Cardiol 2014;174:721–3. [DOI] [PubMed] [Google Scholar]
- [20].Liu LS. [2010 Chinese guidelines for the management of hypertension]. Zhonghua Xin Xue Guan Bing Za Zhi 2011;39:579–615. [PubMed] [Google Scholar]
- [21].Li LM, Rao KQ, Kong LZ, et al. A description on the Chinese national nutrition and health survey in 2002. Zhonghua Liu Xing Bing Xue Za Zhi 2005;26:478–84. [PubMed] [Google Scholar]
- [22].Lenfant C, Chobanian AV, Jones DW, et al. Seventh report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7): resetting the hypertension sails. Hypertension 2003;41:1178–9. [DOI] [PubMed] [Google Scholar]
- [23].Sacco RL, Elkind M, Boden-Albala B, et al. The protective effect of moderate alcohol consumption on ischemic stroke. JAMA 1999;281:53–60. [DOI] [PubMed] [Google Scholar]
- [24].GBD 2015 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016; 388: 1659–1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Je Y, De Vivo I, Giovannucci E. Long-term alcohol intake and risk of endometrial cancer in the Nurses’ Health Study, 1980-2010. Br J Cancer 2014;111:186–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Wang C, Li W, Yin L, et al. Comparison of healthy lifestyle behaviors among individuals with and without cardiovascular diseases from urban and rural areas in China: a cross-sectional study. PLoS One 2017;12:e181981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Bauman A, Bull F, Chey T, et al. The International Prevalence Study on Physical Activity: results from 20 countries. Int J Behav Nutr Phys Act 2009;6:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Pitsavos C, Kavouras SA, Panagiotakos DB, et al. Physical activity status and acute coronary syndromes survival. J Am Coll Cardiol 2008;51:2034–9. [DOI] [PubMed] [Google Scholar]
- [29].Craig CL, Marshall AL, Sjostrom M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003;35:1381–95. [DOI] [PubMed] [Google Scholar]
- [30].Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation 2007;116:1081–93. [DOI] [PubMed] [Google Scholar]
- [31].Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004;364:937–52. [DOI] [PubMed] [Google Scholar]
- [32].O’Donnell MJ, Xavier D, Liu L, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet 2010;376:112–23. [DOI] [PubMed] [Google Scholar]
- [33].O’Donnell MJ, Chin SL, Rangarajan S, et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet 2016;388:761–75. [DOI] [PubMed] [Google Scholar]
- [34].Pandey A, Salahuddin U, Garg S, et al. Continuous dose-response association between sedentary time and risk for cardiovascular disease. JAMA Cardiol 2016;1:575–83. [DOI] [PubMed] [Google Scholar]
- [35].Evenson KR, Butler EN, Rosamond WD. Prevalence of physical activity and sedentary behavior among adults with cardiovascular disease in the United States. J Cardiopulm Rehabil Prev 2014;34:406–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Kortebein P, Ferrando A, Lombeida J, et al. Effect of 10 days of bed rest on skeletal muscle in healthy older adults. JAMA 2007;297:1772–4. [DOI] [PubMed] [Google Scholar]
- [37].Mackay-Lyons MJ, Makrides L. Exercise capacity early after stroke. Arch Phys Med Rehabil 2002;83:1697–702. [DOI] [PubMed] [Google Scholar]
- [38].Vancampfort D, Stubbs B, Hallgren M, et al. Correlates of sedentary behaviour among adults with hazardous drinking habits in six low- and middle-income countries. Psychiatry Res 2018;261:406–13. [DOI] [PubMed] [Google Scholar]
- [39].Verschuren O, Mead G, Visser-Meily A. Sedentary behaviour and stroke: foundational knowledge is crucial. Transl Stroke Res 2015;6:9–12. [DOI] [PubMed] [Google Scholar]


