Abstract
This study was designed to compare postoperative complications and postoperative discomfort when using glue combined with nasal margin suture fixation versus fibrin glue or sutures alone to attach conjunctival autografts among Chinese patients during pterygium excisions.
We analyzed the medical records of 150 eyes of 150 patients with primary pterygium, in which the autografts were secured by 3 different methods after pterygium excision: 50 eyes were secured with fibrin glue, 50 eyes were secured with glue + nasal sutures, and 50 eyes were secured with sutures. The more than 6 months of follow-up observation data included postoperative complications (graft loss/displacement, dehiscence, proliferative granuloma, inflammation, and hemorrhage), recurrence, and postoperative discomfort. A logistic regression procedure was conducted to evaluate the relationship between graft complications and the pterygium grade.
Graft loss/displacement occurred in 3 patients (6%) in the glue group. Graft dehiscence occurred in 8 patients (16%) in the glue group (P < .001), with 2 developing into proliferative granuloma, compared with none in the glue + nasal sutures group and the sutures group at the 3-month postoperative follow-up. Pterygium recurrence occurred in 1 patient (2.2%) in the glue group and 2 patients (4.4%) in the sutures group, compared with none in the glue + nasal sutures group at the 6 to 9 month postoperative follow-up (P = .315). There were fewer postoperative symptoms (pain, foreign body sensation, and tearing) at days 1 and 7 in the fibrin glue and glue + nasal sutures groups than in the sutures group (P < .01). The pterygium grade was a significant risk factor for graft complications (Odd ratio, OR: 5.98, Confidence interval, CI: 1.193–29.992, P = .03) in the glue group.
The modified conjunctival autograft fixation with glue + sutures on the nasal margin resulted in more stable grafts and less graft-associated complications. There was a low level of postoperative patient discomfort in the glue + sutures group. A higher grade of pterygium led to an increased rate of complications in the glue group.
Keywords: complication, dehiscence, discomfort, fibrin glue, granuloma, pterygium, suture
1. Introduction
A pterygium is defined as fibrovascular overgrowth of the Tenon's capsule and bulbar conjunctiva onto the cornea, with an incidence ranging from 0.7% to 31%.[1–3] Pterygium excision together with autologous conjunctival grafting has been suggested as the best treatment, with high safety and a low recurrence rate.[4,5]
Traditionally, the conjunctival autograft (CAG) is most commonly fixated to the sclera by suture. However, the use of suture material can be associated with a number of complications, including infections, inflammation, suture abscesses, button holes, prolonged operative time, and postoperative discomfort.[6,7] Fibrin glue has been reported as an alternative to sutures for fixation of conjunctival grafts and can improve postoperative comfort and reduce the surgical time, complications, recurrence rates, and inflammation.[8–10]
To our knowledge, there are few reports about CAGs using fibrin glue in the Chinese population or Asian society. It is a challenge to treat Chinese pterygium patients using only glue to fix a CAG because of the high grade and large size of pterygiums in the patients being treated, which may meet severe postoperative inflammation and unstable CAG. Mahar and Manzar[11] and Sandra et al[12] reported that there was a definite trend of increased postoperative complication such as recurrence with higher grade of pterygium when autografting with fibrin glue.[11,12] In our Institution, we began using fibrin glue in CAGs in 2014 and have found several complications, such as graft loss/displacement, dehiscence, proliferative granuloma, and pterygium recurrence, which may be due to the abovementioned reason. Therefore, we tried to improve the graft stability and reduce graft related complication by combining fibrin glue and sutures in the nasal margin to fix the conjunctiva graft.
In this study, the postoperative complications of CAG fixation using a combination of fibrin glue and nasal sutures were compared with the use of fibrin glue or sutures in the management of primary pterygium in Chinese patients. First day, as well as the one-week, one-month, 3-month, and 6–9 month postoperative follow-ups data were collected, including the conjunctival graft stability (graft loss, graft displacement, and dehiscence), pterygium recurrence, and other postoperative complications (hemorrhage, inflammation, proliferative granuloma, and corneal epitheliopathy). Postoperative discomfort (foreign body sensation, epiphora, pain, and irritation) was also evaluated.
2. Patients and methods
We retrospectively reviewed the medical records of one hundred fifty consecutive patients (150 eyes) undergoing primary nasal pterygium excision with 3 different surgical methods of conjunctival autograft fixation at Affiliated Second Hospital of Zhejiang University between February 2016 and June 2017. Comprehensive medical and ocular histories were obtained, including patient gender, age, and ocular and medical history. A detailed ocular examination was performed preoperatively. In the study, pterygium size and grade were assessed by the same surgeon by slit lamp. The pterygia were preoperatively graded according to the Tan system,[13] grade 1 (atrophic), grade 2 (intermediate) and grade 3(fleshy). The inclusion criterion was primary pterygium of grade 2 or grade 3 and had an extension of at least 2 mm from the limbus. Patients with ocular surface disorders, pseudopterygium, ocular surgery or trauma history, symblepharon, or known hypersensitivity to any component of fibrin glue were excluded. Z-Pooled normal approximation method is used to estimate sample size. Power calculations with a type I error of 0.05 and type II error of 0.8 were executed. Assuming that the graft complications of the groups were 35% and 10%, respectively, each group needed at least 43 patients. The study was performed following the Declaration of Helsinki and was approved by the ethical committee at the Affiliated Second Hospital, School of Medicine, Zhejiang University in Hangzhou, China.
Fifty consecutive patients (50 eyes) that had pterygium surgery with CAG fixation using fibrin glue (Group 1) who underwent surgery between February 2016 and July 2016, fifty consecutive patients (50 eyes) that had CAG fixation using glue plus nasal sutures (Group 2) who underwent surgery between August 2016 and January 2017, and fifty consecutive patients (50 eyes) that had CAG fixation using sutures (Group 3) who underwent surgery between February 2017 and June 2017. The surgical method was decided by surgeon and treatment period. The outcome measures included postoperative complications and postoperative discomfort. Postoperative complications, such as graft loss/displacement, dehiscence, hemorrhage, inflammation, proliferative granuloma, recurrence of pterygium were examined by slit lamp examination. Postoperative discomfort (pain, foreign body sensation, and tearing) were collected by a questionnaire.
All of the surgeries were performed by one surgeon (Huang) using peribulbar anesthesia (2% lidocaine). The pterygium body was first separated and removed from the underlying sclera and the surrounding conjunctiva by scissors using blunt and sharp dissections. Then the pterygium head was torn off the cornea using forceps and a knife blade. The area of the bare scleral bed was measured. A conjunctival graft of the same size was then carefully obtained from the superior bulbar conjunctiva.
In Group 1 (fibrin glue group), the conjunctival autograft was immediately transferred onto the bare sclera with fibrin glue (SHANGHAI RAAS, China) as described by Sati.[14] In Group 2 (glue + nasal sutures group), three 10–0 sutures in the nasal margin and fibrin glue adhesive were combined to fix the graft (Fig. 1). Before the glue application, 3 nylon 10–0 sutures (Alcon Laboratories Incorporated, Fort Worth, TX) were used to anchor the nasal margin of the graft to the episclera and recipient conjunctiva. Then, the graft was reversed with the 3 sutures to the nasal side, and fibrin glue was added to the bare sclera. The graft was quickly overturned to cover the bare sclera and was adhered by glue. In Group 3 (sutures group), 5–8 interrupted 8–0 Vicryl sutures (Ethicon, Inc.) were used to suture the graft to the surrounding conjunctiva, including anchoring grafts at the 4 corners of the episclera. A bandage lens was placed after the operation in all the 3 groups.
Figure 1.
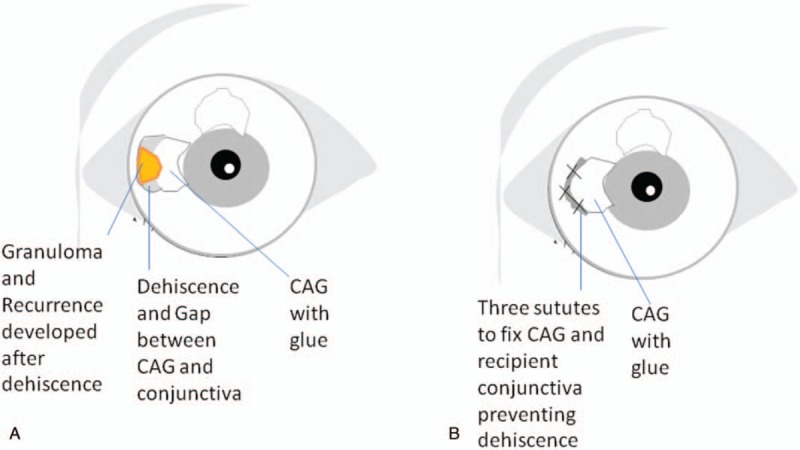
Schematic representation of a modified surgical method in which three 10–0 sutures are placed in the nasal margin to fix the graft and nasal conjunctiva after fibrin glue adhesive to prevent dehiscence and graft-associated complications. (A) In the conjunctival autografts (CAGs) sealed with glue, the dehiscence and gap between the CAG and conjunctiva easily developed granuloma and recurrence because of an epithelial defect. (B) Three sutures were used to fix the CAG and recipient conjunctiva in the graft nasal margin, preventing dehiscence and graft-associated complications. CAGs = conjunctival autografts.
Tobramycin and dexamethasone ointment (TobraDex; Alcon) was placed in each of the eyes, and a pressure patch was applied over night. All patients were treated with tobramycin and dexamethasone eye drops 4 times daily during the first week; then, the eye drops dosage was tapered during the next 3 weeks. In Group 2, the sutures were removed on postoperative day 7 ± 1. The bandage lens was removed on day 7 ± 1 in all the 3 groups.
The records included follow-ups on the first day after surgery, as well as the 1-week, 1-month, 3-month, and 6 to 9 month follow-ups after the surgery. All patients were examined by slit lamp at every visit to monitor the autograft, ocular surface, and development of any complications, such as graft loss/displacement, dehiscence, hemorrhage, inflammation, proliferative granuloma, and corneal epitheliopathy. The degree of postoperative inflammation was classified into 3 grades: mild, moderate, and severe according to Cha et al's study.[15] Recurrence of the pterygium was defined as any regrowth of the conjunctiva onto the cornea. For the postoperative graft displace cases, we replaced the displaced graft using suture fixation, and we covered the bare sclera of the graft loss with amniotic membrane, as in the preceding surgery. In addition, any records of postoperative discomfort (pain, foreign body sensation, and tearing) were collected. In order to grade the symptoms, the patients were asked to fill out a questionnaire on postoperative days 1, 7, and 30 using a 5-point scale adapted from Lim-Bon-Siong and associates.[16]
2.1. Statistical analysis
All continuous data were expressed as the mean ± standard error and analyzed using a one-way ANOVA test. The categorical data were examined by Pearson's chi-squared test. The complications and recurrence data were analyzed by the Fisher's exact test. A logistic regression analysis was used to evaluate the relationship between the complications and the variables (age, gender, grade, surgical type).
3. Results
3.1. Patients’ characteristics
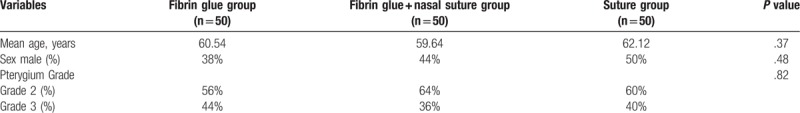
All 150 patients completed the 3-month clinic follow-up, and 138 patients finished the last 6 to 9 month (6.96 ± 0.96) follow-up after the surgery to evaluate the presence of recurrence. The patients’ ages (P = .37) and sex ratio (P = .48) did not have statistically significant differences across the 3 groups (Table 1). The distribution of the pterygium grading was no different among the 3 groups (P = .82).
Table 1.
Patient demographics and variables in 3 groups.
3.2. Postoperative complications and recurrence
Graft loss occurred in one patient (Grade 2), and graft displacement was seen in 2 patients (Grade 3) in Group 1 at the day 1 follow-up (Table 2). The rates of graft dehiscence (8 patients in Group 1 [16%], compared with none in Groups 2 and 3 [0%]) were significantly higher for the patients in the glue group (P < .001). This dehiscence was mostly (7 cases) seen between the conjunctiva and the nasal margin of the graft. Only one case of dehiscence was seen on both nasal and temporal side of the graft. The dehiscence was completely epithelized within one month in 5 patients in Group 1 for the small and linear gap (Fig. 2A). However, proliferative granuloma was present in 2 patients in Group 1 (all Grade 3) from graft dehiscence from Day 7 to Day 30 (Fig. 2B). The granuloma could not been resolved with topical corticosteroid and had to been excised in a second surgery. There were more graft related complications (graft loss/displacement, dehiscence, proliferative granuloma) in glue group (n = 11) when compared to glue + sutures group (n = 0) and sutures group (n = 0) (P < .001). Inflammation was seen in 10 patients (20%) in Group 3 at one month (Fig. 2C), which was more than Groups 1(n = 0 0%) and 2 (n = 0 0%) (Table 2) (P < .001). An extensive subconjunctival hemorrhage was seen in 2 patients in Group 1, 5 patients in Group 2, and 6 patients in Group 3, which spontaneously resolved within 1 month without any intervention.
Table 2.
Comparison of complication and recurrence in 3 groups.
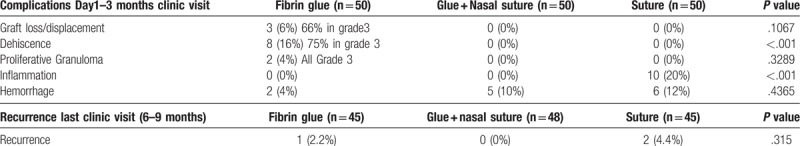
Figure 2.
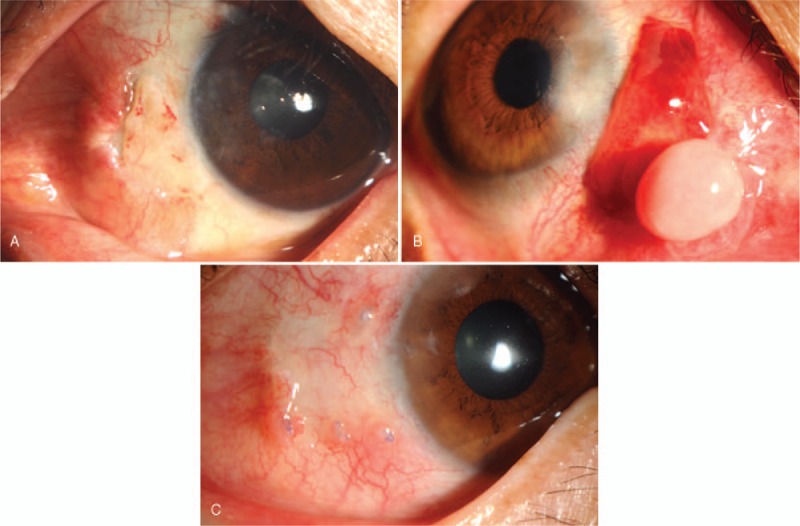
Complication demonstration. (A) Dehiscence in group 1 resulting in complete epithelization. (B) Dehiscence in group 1 developing into proliferative granuloma. C: Sutures associated with inflammation in group 3 at the 1 month follow-up.
Recurrence was seen in one patient on one-month in Group 1 (2.2%) and 2 patients in Group 3 (4.4%) on 3-month, compared with none in Group 2 (0%) during the 6–9 month postoperative follow-up (P = .315). Second surgeries were performed to excise the pterygia for these recurrent patients.
We analyzed relations between variables (age, gender, grade, surgical type) and the probability for postoperative complications. The type of surgical technique (glue vs glue-suture vs suture) (P = .033) were statistically significant in multivariate analyses using logistic regression. After adjusting for age and gender, our results indicated that the grade of the pterygium was a significant risk factor for graft-associated postoperative complications, including graft loss/displacement, dehiscence, granuloma, and recurrence in the glue group (OR: 5.98, CI: 1.193–29.992, P = .03).
3.3. Postoperative symptoms
The pain levels were significantly higher in Group 3 than in Groups 1 and 2 on postoperative days 1 and 7 (P < .01, Fig. 3A). Across the groups, on postoperative days 1 and 7, the foreign body sensation symptom was significantly greater in Group 3 when compared with Groups 1 and 2 (P < .01, Fig. 3B). The intensity of the tearing symptoms was significantly lower in Groups 1 and 2 than in Group 3 on postoperative days 1 and 7 (P < .01, Fig. 3C). On postoperative day 30, the symptoms of pain and tearing presented no significant difference among the 3 groups. However, the intensity of foreign body sensations was still higher in Group 3 than in Groups 1 and 2 until Day 30 (P < .05).
Figure 3.
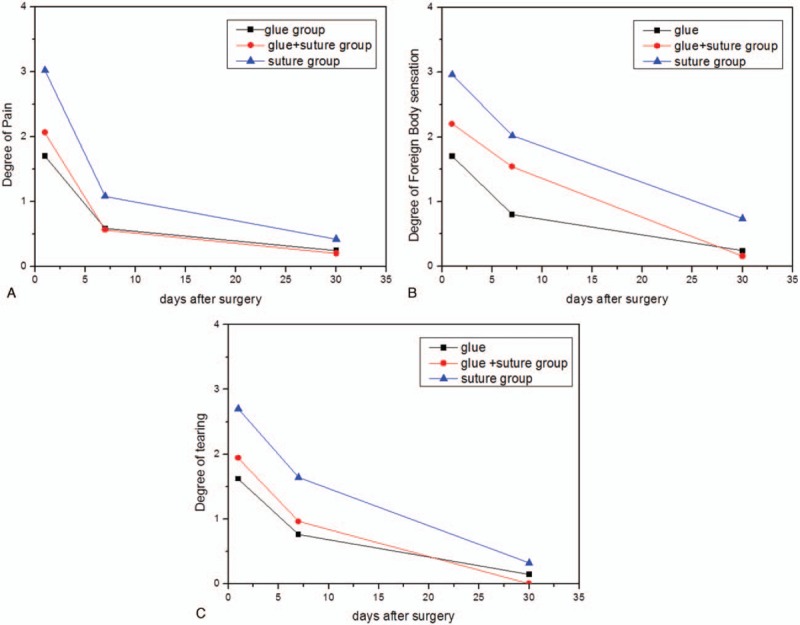
Comparisons of postoperative symptoms among the 3 groups. (A) Pain. (B) Foreign body sensation. (C) Tearing.
4. Discussion
Conjunctival autografting is suggested to be the best choice for pterygium surgery, which has been reported to reduce recurrence rates and present high safety.[17,18] There are 2 main methods, sutures or glue to fix the CAG. Sutures are usually associated with more discomfort and inflammation, on the other hand, fibrin glue improved the comfort but has been reported to associated with more unstable graft.[19,20] Therefore, we designed a modified surgical method which combined fibrin glue and nasal margin suture fixation to make a more stable graft and minimize the sutures associated problem. In our study, we observed postoperative complications and discomfort for CAG fixation in the fibrin glue group and the glue + sutures group in Chinese high-grade pterygium excision when compared with the traditional sutures group. We used questionnaires to evaluate the degree of postoperative symptoms and found that the patient's postoperative discomfort (pain, foreign body sensation, and tearing) was less in the fibrin glue group when compared with the sutures group, which is similar to the existing literature.[14,19] In addition, fewer postoperative symptoms were reported, even though 3 sutures were added to anchor the nasal margins of the grafts in the glue + nasal sutures group when compared with the sutures group. The sutures in Group 2 did not increase the pain and inflammation, which may be due to the minimum of 3 sutures put in the nasal side of the graft, far away from the sensitive corneal limbus area. These were taken out quickly, during the one-week follow-up, while the more interrupted 8–0 Vicryl sutures in Group 3 were slowly resorbed over time, which could be a potential reason for chronic inflammation. Moreover, the 8–0 Vicryl sutures in Group 3 may cause a higher grade of inflammation than that of the 10–0 nylon sutures in Group 2 due to the differences between the 2 materials.
Although the fibrin tissue glue used in pterygium can significantly improve the patient comfort and reduce the surgical time, the technique is open to various complications, such as graft loss, graft displacement, wound dehiscence, and Tenon's cysts.[20] In addition, the rates of graft retraction, dehiscence, and granuloma were higher in the fibrin glue group than in the sutures group.[15,19,20] Cagatay et al[20] reported that the rate of Tenon's cysts (9.4%) in the fibrin glue group was not resolved with topical corticosteroid treatment after 14 days and, therefore, had to been excised in a second surgery. In one Korean pterygium study, Cha reported that the rate of dehiscences (32%) and granulomas (14%) were predominantly observed in the fibrin glue group, even though they transplanted an oversized graft that was 1 mm larger than the size of the bearing area.[15] Our study found that the rate of dehiscence was greater in the glue group. Eight cases of dehiscence were observed between the nasal margin of the graft and the adjacent conjunctiva in the glue group due to wound contraction or ocular horizontal movement. Five cases of dehiscence resulted in a gap that was small and linear and completely epithelized within one month. However, 2 cases of dehiscence developed into proliferative granuloma, with one developing into recurrence. Surgical intervention was required because the granuloma and recurrence were so proliferative that they did not regress with topical and systemic medical treatment.
We analyzed the granuloma and recurrence development in our glue group and believe that the dehiscences observed between the nasal margin of the CAG and the adjacent conjunctiva in the glue group caused an epithelial defect and induced serious fibrovascular proliferation, which may be related to the postoperative granuloma and recurrence. Therefore, we designed a modified surgical method in which we put three 10–0 sutures in the nasal margin to fix the graft and nasal conjunctiva after fibrin glue adhesive to prevent dehiscence after wound contraction or ocular horizontal movement (Fig. 1). There were no graft-related complications or dehiscence, granuloma, or recurrence found in our glue + nasal sutures group in our more than 6 months of follow-up. When compared with the simple glue group, we believe that the modified surgical method inhibits the dehiscence and proliferative granuloma to a great degree. These results are in accordance with the studies that analyzed the recurrence patterns following pterygium surgeries with CAGs and concluded that wound dehiscence, pyogenic granuloma, and graft hemorrhage caused epithelial defects, and that the resulting uncontrolled inflammation was related to the triggering of recurrent growth.[21–24] Our study demonstrated no recurrence (0%) in the glue + nasal sutures group and less recurrence in the glue group (2.2%) when compared with the sutures group (4.4%), though there was no significant difference because of the small number of cohort patients and the short follow-up period in our study. Nevertheless, we believe that the lesser inflammation in the earlier postoperative stage following glue-assisted autografting may be related to a small chance of recurrence. Moreover, we firmly believe that the sutures anchoring the nasal margin of the graft and the adjacent conjunctiva following the glue fixation prevented dehiscence and graft retractions and avoided conjunctival epithelial defects. This played a crucial role in inhibiting the triggering of fibrovascular proliferation and recurrent growth in the glue + nasal sutures group.
There are some research literature reported results with respect to complication and recurrences rates. Hall et al[25] published a RCT with 25 patients in glue group and 25 patients in suture group, they reported 2 case (8%) severe dehiscence in glue group after pterygium surgery which need repeat operation for sutures and 3 case (12%) granuloma and 8 case (32%) retraction of the nasal edge of the graft. They concluded that conjunctival autograft with fibrin glue in pterygium surgery decreased surgical time and resulted in less postoperative pain in the first 48 hours but had a higher complication rate when compared with sutures. Karalezli et al[21] published a RCT to compare fibrin glue versus sutures for conjunctival autografting. The graft dehiscence was observed in 2 eyes (8%) in the fibrin glue group and none (0%) in suture group, while recurrence was observed in 1 eye (4%) in the fibrin glue group and in 3 eyes (12%) in the suture group in 12 months follow-up. Sati et al[14] reported the rate of recurrence 6.67% for glue group and 10% for suture group 12 months follow-up after pterygium surgery in RCT study. Our postoperative complication and recurrence results for glue group and suture group were close to the other published studies, while results for glue + nasal suture group compared favourably with the other studies.
We used the grading system based on the fleshiness and clinical morphology of the pterygia by Tan et al.[13] In our study groups, the preoperative grade of the pterygia included Grade 2 (60%) and Grade 3 (40%).
The high grades in the Chinese preoperative pterygium population may relate to various factors, such as economics and medical condition. We found a 66% graft loss/displacement in Grade 3, 75% dehiscence in Grade 3, and all of the granulomas and recurrences occurred in Grade 3 in the glue group. Our results suggested that the grade of the pterygium was a significant risk factor for graft-associated postoperative complications, including graft loss/displacement, dehiscence, granuloma, and recurrence, in the glue group. These results are in accordance with studies showing that the grade and morphology of pterygium influences recurrence rates when autografting with fibrin glue, in addition, studies showed that there appeared to be significantly more recurrences in the high grade group than the low grade group.[11,12] Our postoperative complication and recurrence results after pterygium surgery compared favourably with the other published studies.
In conclusion, the modified method of putting 3 sutures in the nasal margin to fix the graft and adjacent conjunctiva following fibrin glue adhesive for attaching CAGs could prevent postoperative graft related postoperative complications (graft loss/displacement, dehiscence, proliferative granuloma) after pterygium surgery in Chinese pterygium cases. In addition, it could improve the postoperative comfort when compared with the traditional sutures group. However, further studies with a larger population and longer follow-up period are needed to supplement this report.
Author contribution
Xiaodan Huang conceived of the study and drafted the manuscript. Binbin Zhu and Lin Lin collected the data and revised the manuscript. Xiuming Jin participated in the design of the study and critically revised the manuscript. All authors read and approved the final manuscript.
Conceptualization: Xiaodan Huang.
Data curation: Xiaodan Huang, Binbin Zhu.
Formal analysis: Xiaodan Huang, Binbin Zhu.
Funding acquisition: Xiaodan Huang, Xiuming Jin.
Investigation: Xiaodan Huang, Lin Lin.
Methodology: Xiaodan Huang, Lin Lin.
Project administration: Xiaodan Huang, Binbin Zhu, Lin Lin.
Resources: Xiaodan Huang, Lin Lin.
Software: Xiaodan Huang, Binbin Zhu, Lin Lin.
Supervision: Xiuming Jin.
Validation: Binbin Zhu.
Visualization: Binbin Zhu.
Writing – original draft: Xiaodan Huang.
Writing – review & editing: Xiuming Jin.
Footnotes
Abbreviations: CAG = conjunctival autograft, CI = confidence interval, OR = odd ratio.
Ethics approval and consent to participate: This study followed the tenets of the Declaration of Helsinki and was approved by the ethics committee of the Second Affiliated Hospital, School of Medicine, Zhejiang University. Informed written consent was obtained from all participants.
Fundings: The authors acknowledge the financial support of the National Natural Science Foundation of China (Project number: 81870624); Major Science and Technology Projects of Zhejiang Province (No.2017C03046).
Competing Interests: The authors declare that they have no competing interests.
The authors have no conflicts of interest to disclose.
References
- [1].Hirst LW. Recurrent pterygium surgery using pterygium extended removal followed by extended conjunctival transplant: recurrence rate and cosmesis. Ophthalmology 2009;116:1278–86. [DOI] [PubMed] [Google Scholar]
- [2].Shiroma H, Higa A, Sawaguchi S, et al. Prevalence and risk factors of pterygium in a southwestern island of Japan: the Kumejima Study. Am J Ophthalmol 2009;148:766–71. [DOI] [PubMed] [Google Scholar]
- [3].Srinivasan S, Dollin M, McAllum P, et al. Fibrin glue versus sutures for attaching the conjunctival autograft in pterygium surgery: a prospective observer masked clinical trial. Br J Ophthalmol 2009;93:215–8. [DOI] [PubMed] [Google Scholar]
- [4].Prabhasawat P, Barton K, Burkett G, et al. Comparison of conjunctival autografts, amniotic membrane grafts, and primary closure for pterygium excision. Ophthalmology 1997;104:974–85. [DOI] [PubMed] [Google Scholar]
- [5].Al Fayez MF. Limbal versus conjunctival autograft transplantation for advanced and recurrent pterygium. Ophthalmology 2002;109:1752–5. [DOI] [PubMed] [Google Scholar]
- [6].Allan BD, Short P, Crawford CJ, et al. Pterygium excision with conjunctival autografting: an effective and safe technique. Br J Ophthalmol 1993;77:698–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Tan D. Conjuctival grafting for ocular surface disease. Curr Opin Ophthalmol 1999;10:227–81. [DOI] [PubMed] [Google Scholar]
- [8].Koranyi G, Seregard S, Kopp ED. Cut and paste: anosuture, small incision approach to pterygium surgery. Br J Ophthalmol 2004;88:911–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Koranyi G, Seregard S, Kopp ED. The cut-and-paste method for primary pterygium surgery: long-term follow-up. Acta Ophthalmo l Scand 2005;83:298–301. [DOI] [PubMed] [Google Scholar]
- [10].Ayala M. Results of pterygium surgery using a biologic adhesive. Cornea 2008;27:663–7. [DOI] [PubMed] [Google Scholar]
- [11].Mahar PS, Manzar N. The study of etiological and demographic characteristics of pterygium recurrence: a consecutive case series study from Pakistan. Int Ophthalmol 2014;34:69–74. [DOI] [PubMed] [Google Scholar]
- [12].Sandra S, Zeljka J, Zeljka VA, et al. The influence of pterygium morphology on fibrin glue conjunctival autograft pterygium surgery. Int Ophthalmol 2014;34:75–9. [DOI] [PubMed] [Google Scholar]
- [13].Tan DT, Chee SP, Dear KB, et al. Effect of pterygium morphology on pterygium recurrence in a controlled trial comparing conjunctival autografting with bare sclera excision. Arch Ophthalmol 1997;115:1235–40. [DOI] [PubMed] [Google Scholar]
- [14].Sati A, Shankar S, Jha A, et al. Comparison of efficacy of three surgical methods of conjunctival autograft fixation in the treatment of pterygium. Int Ophthalmol 2014;34:1233–9. [DOI] [PubMed] [Google Scholar]
- [15].Cha DM, Kim KH, Choi HJ, et al. A comparative study of the effect of fibrin glue versus sutures on clinical outcome in patients undergoing pterygium excision and conjunctival autografts. Korean J Ophthalmol 2012;26:407–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Lim-Bon-Siong R, Valluri S, Gordon ME, et al. Efficacy and safety of the ProTek (Vifilcon A) therapeutic soft contact lens after photorefractive keratectomy. Am J Ophthalmol 1998;125:169–76. [DOI] [PubMed] [Google Scholar]
- [17].Sanchez-Thorin JC, Rocha G, Yelin JB. Meta-analysis on the recurrence rates after bare sclera resection with and without mitomycin C use and conjunctival autograft placement in surgery for primary pterygium. Br J Ophthalmol 1998;82:661–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Young AL, Leung GY, Wong AK, et al. A randomised trial comparing 0.02% mitomycin C and limbal conjunctival autograft after excision of primary pterygium. Br J Ophthalmol 2004;88:995–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Choudhury S, Dutta J, Mukhopadhyay S, et al. Comparison of autologous in situ blood coagulum versus sutures for conjunctival autografting after pterygium excision. Int Ophthalmol 2014;34:41–8. [DOI] [PubMed] [Google Scholar]
- [20].Cagatay HH, Gokce G, Ekinci M, et al. Long-term comparison of fibrin tissue glue and vicryl suture in conjunctival autografting for pterygium surgery. Postgrad Med 2014;126:97–103. [DOI] [PubMed] [Google Scholar]
- [21].Karalezli A, Kucukerdonmez C, Akova YA, et al. Fibrin glue versus sutures for conjunctival autografting in pterygium surgery: a prospective comparative study. Br J Ophthalmol 2008;92:1206–10. [DOI] [PubMed] [Google Scholar]
- [22].Wang X, Zhang Y, Zhou L, et al. Comparison of fibrin glue and Vicryl sutures in conjunctival autografting for pterygium surgery. Mol Vis 2017;23:275–85. [PMC free article] [PubMed] [Google Scholar]
- [23].Lan A, Xiao F, Wang Y, et al. Efficacy of fibrin glue versus sutures for attaching conjunctival autografts in pterygium surgery: a systematic review with meta-analysis and trial sequential analysis of evidence. Oncotarget 2017;8:41487–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Kwon SH, Kim HK. Analysis of recurrence patterns following pterygium surgery with conjunctival autografts. Medicine (Baltimore) 2015;94:e518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Hall RC, Logan AJ, Wells AP. Comparison of fibrin glue with sutures for pterygium excision surgery with conjunctival autografts. Clin Exp Ophthalmol 2009;37:584–9. [DOI] [PubMed] [Google Scholar]


