Abstract
This study was conducted to compare the survival rate and the influencing factors between women and men following ST-elevation myocardial infarction (STEMI) treated with primary percutaneous coronary intervention (PCI).
A national-wide Acute Coronary Syndrome Full Spectrum Registry conducted by the Taiwan Society of Cardiology was used for data collection between October 2008 and January 2010. Details of 1621 patients with STEMI treated with primary PCI, including 1350 (83%) men and 271 (17%) women, were collected. Composite outcomes included all-cause death, myocardial reinfarction, and an ischemic stroke. Demographic data, comorbidities, clinical presentations, details of treatment received, and outcomes were recorded at 3-month intervals for 1 year.
No significant difference was observed between men and women in the composite endpoints after STEMI during their hospital stay (5.5% vs 2.5%, P = .07). However, women showed significantly higher in-hospital and 1-year mortality rates than those of men (4.1% vs 1.8%, P = .008; 11.0% vs 4.1%, P = .000, respectively). Compared with men, women presented with higher age (mean age 68.9 vs 58.9 years, P = .001), less body weight (58.7 vs 70.9 kg, P < .001), more number of risk factors, delayed diagnosis, and more number of inadequate medical treatments. After adjusting for age and cardiovascular risk factors, the difference in mortality ceased to exist between men and women.
Although female patients with STEMI-treated primary PCI had higher in-hospital and 1-year mortality rates than those of males in Taiwan, there was no gender difference after adjusting for age and cardiovascular risk factors.
Keywords: cardiovascular outcome, gender difference, mortality, primary PCI, STEMI
1. Introduction
Gender difference has been observed in several diseases in terms of their prevalence and outcomes. Among such diseases, coronary artery disease has been reported to present a delayed onset for 10 years in women, with increased mortality and morbidity rates after acute coronary events compared with the rates among their comparators in many countries.[1]
There is extensive evidence delineating the relationship of gender difference in acute coronary syndrome (ACS).[2,3] However, after adjusting for confounding factors, the gender difference ceased to exist. In general, studies on outcomes have reported higher crude mortality rates in women after ACS, which have been primarily explained by differences in age, management, and comorbidities between men and women. In addition, these studies have identified an age–sex interaction, wherein older age women have a particularly high risk of mortality after ACS even after adjusting for other risk factors.[4–6]
Limited data from the world have also demonstrated that women have worse outcomes after ACS treated with primary percutaneous coronary intervention (PCI)[7,8]; however, to our knowledge, there have been no such reports from Asia. Therefore, we conducted this study to compare the short-term major cardiovascular outcomes and determine the influencing factors between men and women after ST-elevation myocardial infarction (STEMI) treated with primary PCI.
2. Materials and methods
2.1. Study participants
An ACS Full Spectrum Registry was conducted by the Taiwan Society of Cardiology and implemented between October 2008 and January 2010. A total of 39 tertiary hospitals were included in this registry, all of which have the availability of on-site thrombolytic therapy and on-site cardiac catheterization facility. Details regarding patient recruitment, definition of ACS, and inclusion and exclusion criteria have been previously described.[9]
2.2. Study design
It was mandatory for each hospital to provide data on demographics, clinical characteristics, comorbid conditions, clinical presentations, medical and therapeutic information, and complications or outcomes. Patient details regarding medical interventions and clinical events such as death, myocardial infarction, stroke, and rehospitalization after their discharge were collected and were followed up for 1-year at 3-month intervals through clinical visits. Data collected in this study were entered into a standardized report form, and source documentation and accuracy were monitored in 5% of all case report forms at each recruiting site. The study protocol was approved by the ethics committee of the Sin-Lau Hospital (SL-2012–18) and was performed in accordance with the local regulatory guidelines and the international guidelines for good clinical practice.[10] All the patients provided an informed consent, although it can be waived if they were not willing.
2.3. Cardiovascular outcomes
The endpoint of this study was to assess major adverse cardiac events (MACE) during hospitalization and 1 year after discharge, a composite of all-cause death, myocardial reinfarction, and an ischemic stroke.
2.4. Statistical analysis
Continuous variables were summarized as mean values and standard deviations, whereas categorical variables were summarized as numbers and percentages. Student t test was used for comparing continuous variables and Chi-square test was used for comparing categorical variables between males and females. Non-normally distributed continuous variables were summarized using median and interquartile range and were analyzed using the Mann–Whitney test. The association between in-hospital or 1-year outcome and gender after adjusting for various confounders (age, body mass index, diabetes, current smoking status, dyslipidemia, and hypertension) was analyzed using multivariable logistic regression. Finally, time-to-event comparisons among the 2 groups were performed using Kaplan–Meier survival curve analysis. A P value of < .05 was considered as statistically significant. SAS software version 9.2 (SAS Institute Inc., Cary, NC) was used for performing all statistical analyses.
3. Results
3.1. Study participants
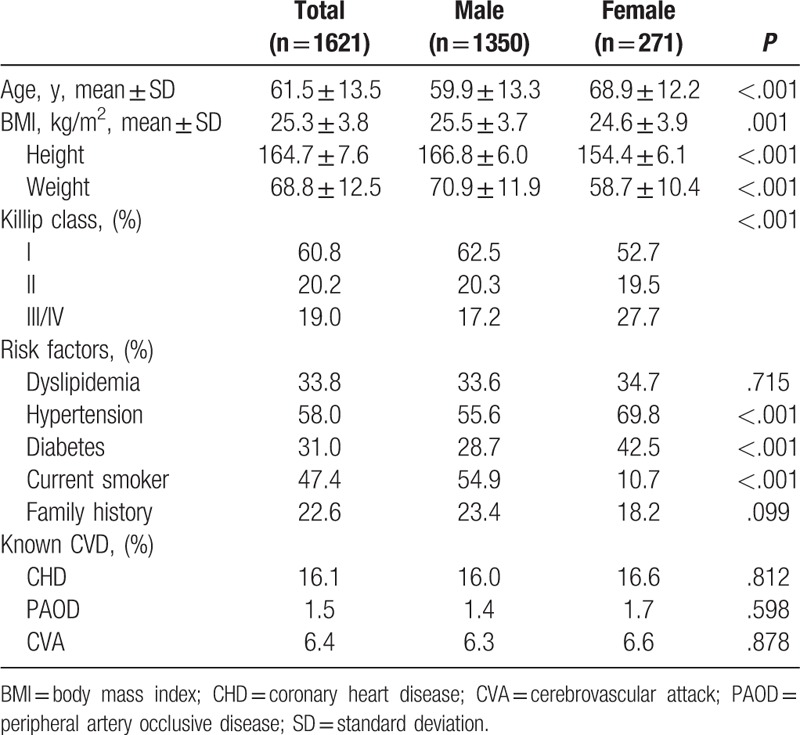
Baseline characteristics of the enrolled patients are depicted in Table 1. A total of 1621 patients, including 1350 men and 271 women, were recruited in this study. Mean age of the patients was 62 years, with female patients being 9 years older than male patients (P < .001). Female patients also had significantly lower body weight, shorter body height, and lower body mass index than those of male patients. Analysis of disease severity in terms of STEMI presentation revealed that female patients had a higher incidence of Killip III/IV class than that of male patients (27.7% vs 17.2%, P < .001). Female patients also had a significantly higher prevalence of hypertension and diabetes mellitus but a lower prevalence of current smoking status. Both genders showed equal prevalence of coronary heart disease, peripheral artery occlusive disease, and cerebrovascular attack.
Table 1.
Baseline characteristics of patients enrolled in the registry.
3.2. Evaluation and diagnostic procedure in emergent department
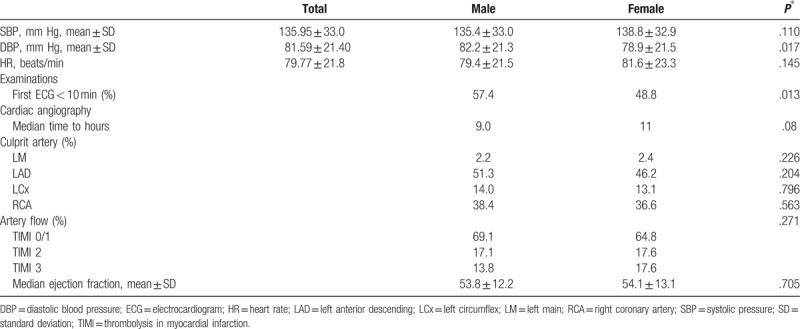
During presentation in the emergency room, female patients showed a significantly lower diastolic blood pressure. Male patients comprised a significantly higher proportion than female patients in undergoing the first electrocardiogram (ECG) within 10 minutes (57.4% vs 48.8%, P = .013). No statistical difference was observed between men and women in terms of culprit arteries, severity of TIMI flow in the culprit arteries, and left ventricular (LV) systolic function (Table 2).
Table 2.
Evaluation in the ED, diagnostic, and angiographic procedures.
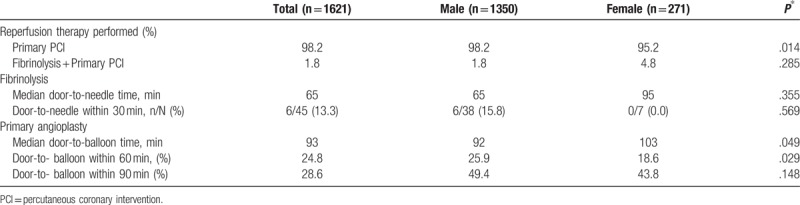
3.3. Reperfusion in STEMI patients
Table 3 summarizes the details of comparison of reperfusion therapy in patients with STEMI between the 2 genders. The probability of undergoing primary PCI was higher among both genders, although female patients comprised a significantly lower proportion than that of male patients in this context (95.2% vs 98.2%, P = .014). Female patients had a longer door-to-balloon time than that of male patients (103 vs 92 minutes, P = .049). Guideline-derived door-to-balloon time was less among female patients within 60 or 90 minutes compared with that in male patients (18.6% vs 25.9%, P = .029; 43.8% vs 49.4%, P = .148, respectively).
Table 3.
Reperfusion status in patients diagnosed with STEMI at the time of admission.
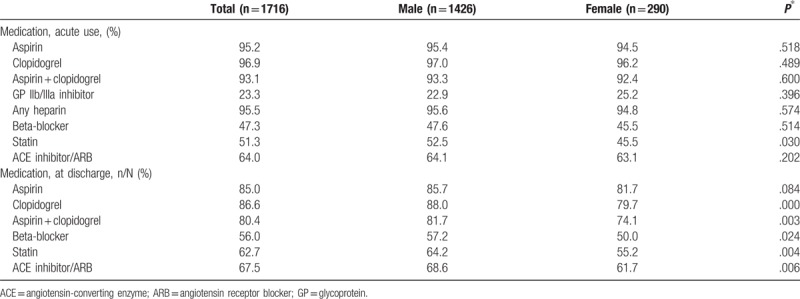
3.4. Pharmacological management of STEMI for acute use and at discharge
No significant gender differences were observed in medication for acute use (within the first 24 hours of admission) of aspirin, clopidogrel, GP IIb/IIIa inhibitors, heparin, beta-blockers, angiotensin-converting enzyme inhibitors (ACEIs), and angiotensin receptor blockers (ARBs). The proportion of acute use of statins was significantly less in women than that in men (45.5% vs 52.5%, P = .030). Furthermore, compared with male patients, female patients received significantly less medications at discharge such as clopidogrel (88.7% vs 79.0%, P = .000), aspirin + clopidogrel (81.7% vs 74.1%, P = .003), beta-blockers (57.2% vs 50.0%, P = .027), statins (64.2% vs 55.2%, P = .004), and ACEIs/ARBs (68.6% vs 61.7%, P = .006) (Table 4).
Table 4.
Medication prescription for acute use and at patient discharge.
3.5. In-hospital and 1-year cardiovascular outcomes
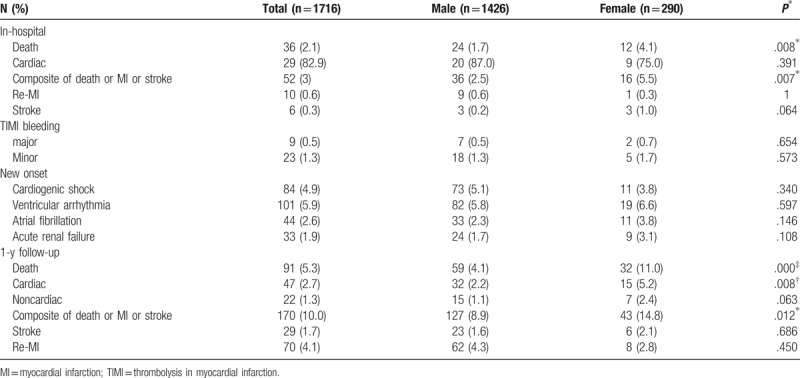
Table 5 summarizes the details of in-hospital and 1-year follow-up cardiovascular outcomes. There was no significant difference in composite endpoints (males 2.5% vs females 5.5%, P = .07); however, compared with male patients, females had significantly higher rates of total mortality (1.7% vs 4.1%, P = .004) and cardiac mortality (1.4% vs 3.1%, P = .027) among the in-hospital cardiovascular outcomes. No difference was observed between both genders in terms of TIMI major or minor bleeding, new onset of cardiogenic shock, ventricular arrhythmia, atrial fibrillation, and acute renal failure.
Table 5.
In-hospital and at discharge outcomes according to gender.
After STEMI, a lower mortality rate that persisted till 1 year was observed in male patients [hazard ratio: 0.36%, 95% confidence interval (95% CI): 0.23–0.55] (Fig. 1). The gender difference in terms of in-hospital and 1-year cardiac mortality after STEMI was still existent; however, after adjusting for sex and age (model 1) or by age, sex, and other cardiovascular risk factors (model 2), the difference became nonsignificant (Table 6).
Figure 1.
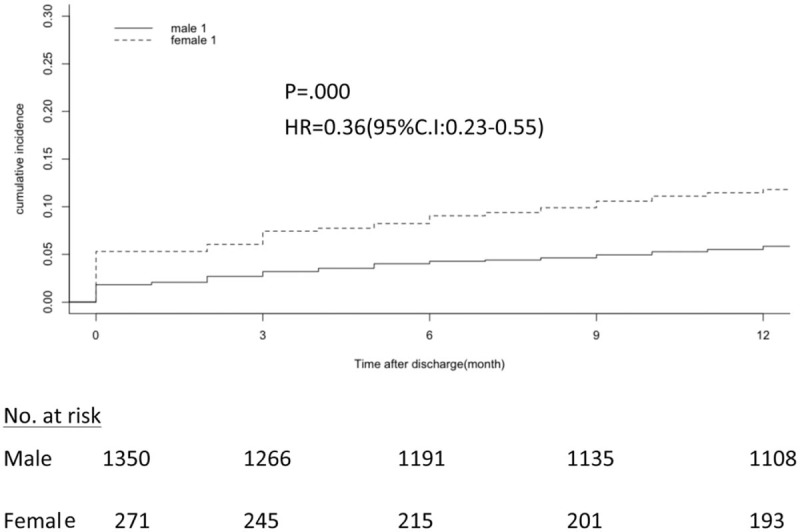
Comparison 1-year mortality rate by Kaplan–Meir method between males and females after STEMI.
Table 6.
Multivariable-adjusted odds ratios for the association between gender and outcome.

4. Discussion
From this study, we found that gender disparities exist in terms of age, comorbidities, medication management, primary PCI, and in-hospital and 1-year mortality rates among patients with STEMI. However, after adjusting for age and cardiovascular risk factors, there was no gender difference in the in-hospital and 1-year mortality rates among patients with STEMI.
This study on the role of gender in patients with STEMI treated with primary PCI in Taiwan has demonstrated inconsistent results compared with those of previous studies.[4,5,11–14] Female patients with STEMI were older and had a higher prevalence of hypertension and diabetes mellitus than those of male patients, which is consistent with the results of previous studies[15–18] and might also explain the poorer prognosis. The time to first ECG at the emergency department was longer among women, which might delay receiving appropriate treatment for STEMI. A possible delay for performing ECG in women could be attributed to a lack of STEMI symptoms and atypical angina presentation when symptoms occur. [15] Our data also revealed a significant underutilization of dual antiplatelet therapy and statins when women are discharged from the hospital. These results are in accordance with previous studies that found a consistent lower utilization rate of medications in women.[15,19] A study based on a large Canadian registry found that women had lower chances of receiving lipid-lowering agents, even after adjustment for all relevant variables.[20] Moreover, similar results with lower rates of treatment with aspirin and statins were reported in a study based on the American College of Cardiology-National Cardiovascular Data Registry.[21] Underutilization of antiplatelet therapy could be justified by higher rates of nonobstructive coronary artery disease in women. This notion is supported by a previous study based on the 2004 to 2010 ACSIS surveys that showed underutilization of evidence-based medications in patients with nonobstructive coronary artery disease.[22]
Women were also less likely to undergo primary PCI, had longer door-to-balloon time, and a higher Killip class (3 and 4) compared with those among men. Our results are consistent with those of several previous studies.[5,11,14,23,24] and can be explained by the observation that women of older age and having more number of comorbidities are probably at a higher risk for undergoing primary PCI. The fact that women experienced a longer median time to have a coronary angiography than men could be related to the fact that women are less likely to experience symptoms of STEMI, and when they develop such symptoms, they are often present as atypical angina, which complicates the STEMI diagnosis. [15,19–21]
Finally, although female patients had higher in-hospital and 1-year mortality rates than those of males, no gender difference was observed after adjusting for age and cardiovascular risk factors. Although previous studies have shown that women tend to develop worse outcomes, the role of gender in mortality has been controversial in several studies.[3,10,11,21,25,26] Our study has shown that women tend to have higher in-hospital and 1-year mortality rates, which is consistent with the results of most of the previous studies.[27–30] This poorer cardiovascular outcome in females could most probably be related to the higher age of females and the higher incidence rates of coronary risk factors such as diabetes mellitus and hypertension, as well as the higher incidence rates of Killip class 3 and cardiogenic shock. However, after adjusting for age and cardiovascular risk factors, the difference in mortality between both genders became nonsignificant, which is consistent with the result of previous studies[15–18] and further suggests the significance of age and cardiovascular risk factors in this context.
There are 3 limitations in this study. First, it is a nonrandomized and an observational study, which thus makes it difficult to determine the cause-and-effect relationships between cardiovascular outcomes and STEMI. However, the results of this study provide valuable real-world data regarding the current clinical practices across the full spectrum of STEMI, which could help improve the management of STEMI in Taiwan. Second, unmeasured sex-specific differences may also exist. The database lacks details of family history and unmeasured confounders. Therefore, caution must be exercised while interpreting our data. Third, all the patient details in this study were collected from 39 general hospitals equipped with catheterization rooms in Taiwan; therefore, it is unclear how our findings can be generalized to patients in different areas.
Despite some limitations, this study has 2 aspects of strength. First, the data used in this study represent > 90% of the hospitals equipped with catheterization rooms in Taiwan. This study also provides valuable real-world data regarding the current clinical practices in Taiwan. Second, the collected data are prospective and allow better observation of the results over a 1-year follow-up period in this study.
5. Conclusion
Gender disparities exist in terms of age, comorbidities, medication management, primary PCI, and in-hospital and 1-year mortality rates among patients with STEMI in Taiwan. However, after adjusting for age and cardiovascular risk factors, there was no gender difference in the in-hospital and 1-year mortality rates among patients with STEMI in Taiwan. With potential prognostic importance, these findings call for more work to evaluate the role of gender among patients with STEMI treated with primary PCI to reduce gender difference in contemporary care.
Acknowledgment
We thank all the investigators and nurses participating in this registry.
Author contributions
Conceptualization: Li-Ping Chou, Ping Zhao, Gwo-Ping Jong.
Funding acquisition: Li-Ping Chou, Gwo-Ping Jong.
Investigation: Li-Ping Chou, Yen-Hsun Chen.
Methodology: Li-Ping Chou, Ping Zhao, Gwo-Ping Jong.
Project administration: Li-Ping Chou, Gwo-Ping Jong.
Resources: Li-Ping Chou, Chieh Kao, Yen-Hsun Chen.
Supervision: Gwo-Ping Jong.
Visualization: Li-Ping Chou, Ping Zhao.
Writing – original draft: Li-Ping Chou, Gwo-Ping Jong.
Writing – review & editing: Li-Ping Chou, Gwo-Ping Jong.
Gwo-Ping Jong orcid: 8889-8889-8889-888X.
Footnotes
Abbreviations: ACS = acute coronary syndrome, ECG = electrocardiogram, PCI = primary percutaneous coronary intervention, STEMI = ST-elevation myocardial infarction.
L-PC and PZ authors contributed equally to this work.
Funding/support: This study was funded by Sanofi Taiwan Co., Ltd. and Bristol-Myers Squibb (Taiwan) Ltd (CV-2010-001 and CV-2010-002).
The authors have declared that no competing interests exist.
References
- [1].Rosengren A, Wallentin L, Simoons M, et al. Age, clinical presentation, and outcome of acute coronary syndromes in the Euroheart acute coronary syndrome survey. Eur Heart J 2006;27:789–95. [DOI] [PubMed] [Google Scholar]
- [2].Steg P, Goldberg R, Gore J. Baseline characteristics, management practices, and in-hospital outcomes of patients hospitalized with acute coronary syndromes in the global registry of acute coronary events (GRACE). Am J Cardiol 2002;90:358–63. [DOI] [PubMed] [Google Scholar]
- [3].Dey S, Flather MD, Devlin G, et al. Sex-related differences in the presentation, treatment and outcomes among patients with acute coronary syndromes: the global registry of acute coronary events. Heart 2009;95:20–6. [DOI] [PubMed] [Google Scholar]
- [4].Vaccarino V, Krumholz HM, Berkman LF, et al. Sex differences in mortality after myocardial infarction: is there evidence for an increased risk for women? Circulation 1995;91:1861–71. [DOI] [PubMed] [Google Scholar]
- [5].Nohria A, Vaccarino V, Krumholz HM. Gender differences in mortality after myocardial infarction: why women fare worse than men. Cardiol Clin 1998;16:45–57. [DOI] [PubMed] [Google Scholar]
- [6].Bucholz EM, Butala NM, Rathore SS, et al. Sex differences in long-term mortality after myocardial infarction: a systematic review. Circulation 2014;130:757–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Zubaid M, Rashed WA, Al-Khaja N, et al. Clinical presentation and outcomes of acute coronary syndromes in the gulf registry of acute coronary events (Gulf RACE). Saudi Med J 2008;29:251–5. [PubMed] [Google Scholar]
- [8].Kosuge M, Kimura K, Kojima S, et al. Sex differences in early mortality of patients undergoing primary stenting for acute myocardial infarction. Circ J 2006;70:217–21. [DOI] [PubMed] [Google Scholar]
- [9].Shyu KG, Wu CJ, Mar GY, et al. Clinical characteristics, management and in-hospital outcomes of patients with acute coronary syndrome: observations from the Taiwan ACS full spectrum registry. Acta Cardiol Sin 2011;27:135–44. [Google Scholar]
- [10].International Epidemiological Association Guidelines. Available at: http://www.ieaweb.org/index.php?option=com_content&view=article&id=15%3Agoodepidemiological-practice-gep&catid=20%3Agood-epidemiologicalpracticegep&Itemid=43&limitstart=1 Accessed January 28, 2011. [Google Scholar]
- [11].Yan AT, Tan M, Fitchett D, et al. One-year outcome of patients after acute coronary syndromes (from the Canadian Acute Coronary Syndromes Registry). Am J Cardiol 2004;94:25–9. [DOI] [PubMed] [Google Scholar]
- [12].Chew DP, Amerena JV, Coverdale SG, et al. Invasive management and late clinical outcomes in contemporary Australian management of acute coronary syndromes: observations from the ACACIA registry. Med J Aust 2008;188:691–7. [DOI] [PubMed] [Google Scholar]
- [13].Bruins Slot MH, Rutten FH, van der Heijden GJ, et al. Gender differences in pre-hospital time delay and symptom presentation in patients suspected of acute coronary syndrome in primary care. Fam Pract 2012;29:332–7. [DOI] [PubMed] [Google Scholar]
- [14].Shehab A, Al-Dabbagh B, AlHabib KF, et al. Gender disparities in the presentation, management and outcomes of acute coronary syndrome patients: data from the 2nd gulf registry of acute coronary events (Gulf RACE-2). PLoS One 2013;8:e55508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Sabbag A, Matetzky S, Porter A, et al. Sex differences in the management and 5-year outcome of young patients (<55 years) with acute coronary syndromes. Am J Med 2017;130:1324.e15–22. [DOI] [PubMed] [Google Scholar]
- [16].Kuhn L, Page K, Rahman MA, et al. Gender difference in treatment and mortality of patients with ST-segment elevation myocardial infarction admitted to Victorian public hospitals: a retrospective database study. Aust Crit Care 2015;28:196–202. [DOI] [PubMed] [Google Scholar]
- [17].Duraes AR, Bitar YS, Freitas ACT, et al. Gender differences in ST-elevation myocardial infarction (STEMI) time delays: experience of a public health service in Salvador-Brazil. Am J Cardiovasc Dis 2017;7:102–7. [PMC free article] [PubMed] [Google Scholar]
- [18].Lansky AJ, Pietras C, Costa RA, et al. Gender differences in outcomes after primary angioplasty versus primary stenting with and without abciximab for acute myocardial infarction: results of the Controlled Abciximab and Device Investigation to Lower Late Angioplasty Complications (CADILLAC) trial. Circulation 2005;111:1611–8. [DOI] [PubMed] [Google Scholar]
- [19].Blomkalns AL, Chen AY, Hochman JS, et al. Gender disparities in the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes: large-scale observations from the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the American College of Cardiology/American Heart Association Guidelines) National Quality Improvement Initiative. J Am Coll Cardiol 2005;45:832–7. [DOI] [PubMed] [Google Scholar]
- [20].Bugiardini R, Yan AT, Yan RT, et al. Factors influencing underutilization of evidence-based therapies in women. Eur Heart J 2011;32:1337–44. [DOI] [PubMed] [Google Scholar]
- [21].Hess CN, McCoy LA, Duggirala HJ, et al. Sex-based differences in outcomes after percutaneous coronary intervention for acute myocardial infarction: a report from TRANSLATE-ACS. J Am Heart Assoc 2014;3:e000523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Minha S, Gottlieb S, Magalhaes MA, et al. Characteristics and management of patients with acute coronary syndrome and normal or non-significant coronary artery disease: results from Acute Coronary Syndrome Israeli Survey (ACSIS) 2004–2010. J Invasive Cardiol 2014;26:389–93. [PubMed] [Google Scholar]
- [23].Chang WC, Kaul P, Westerhout CM, et al. Impact of sex on long-term mortality from acute myocardial infarction vs unstable angina. Arch Intern Med 2003;163:2476–84. [DOI] [PubMed] [Google Scholar]
- [24].Dreyer RP, Ranasinghe I, Wang Y, et al. Sex differences in the rate, timing, and principal diagnoses of 30-day readmissions in younger patients with acute myocardial infarction. Circulation 2015;132:158–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Akhter N, Milford-Beland S, Roe MT, et al. Gender differences among patients with acute coronary syndromes undergoing percutaneous coronary intervention in the American College of Cardiology-National Cardiovascular Data Registry (ACC-NCDR). Am Heart J 2009;157:141–8. [DOI] [PubMed] [Google Scholar]
- [26].Koek HL, de Bruin A, Gast F, et al. Short- and long-term prognosis after acute myocardial infarction in men versus women. Am J Cardiol 2006;98:993–9. [DOI] [PubMed] [Google Scholar]
- [27].Berger JS, Elliott L, Gallup D, et al. Sex differences in mortality following acute coronary syndromes. JAMA 2009;302:874–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Fath-Ordoubadi F, Barac Y, Abergel E, et al. Gender impact on prognosis of acute coronary syndrome patients treated with drugeluting stents. Am J Cardiol 2012;110:636–42. [DOI] [PubMed] [Google Scholar]
- [29].Alabas OA, Gale CP, Hall M, et al. Sex differences in treatments, relative survival, and excess mortality following acute myocardial infarction: National Cohort Study Using the SWEDEHEART Registry. J Am Heart Assoc 2017;6:e007123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Piackova E, Jäger B, Farhan S, et al. Gender differences in short- and long-term mortality in the Vienna STEMI registry. Int J Cardiol 2017;244:303–8. [DOI] [PubMed] [Google Scholar]


